Abstract
This paper focuses on acute-care local public hospitals in Japan and evaluates differences in hospital technology, as reflected in the productivity of labor specialties, physical capital and medicines, and in the impact of teaching activities and other hospital characteristics on hospital output. We use panel data quantile regressions with fixed effects to model a range of technologies for the multi-product output function of hospitals. The analysis reveals technological heterogeneity across high-output and low-output hospitals. We discover inexpedient labor/capital and labor/medicines mix, and vast opportunities for cost savings. The results contribute to scant empirical literature on variation in the hospital production.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
The rapidly growing field of productivity analysis in health economics tends to neglect heterogeneity in hospital technology by focusing on mean tendencies or on most efficient hospitals (Hollingsworth 2008). Accordingly, evidence on input productivity, defined as marginal product of output with respect to a given input (Jensen and Morrisey 1986), is barely documented in the literature for hospitals with different output levels. However, variations in practices for managing human resources, for providing clinical procedures and for operating a hospital as an economic unit were recently quantified at large samples of hospitals in different countries (Bloom et al. 2014, 2015; Dorgan et al. 2010). Combined with the finding of a direct association between management and productivity (Bloom et al. 2007; Bloom 2019; Cleverley and Harvey 1992; Hames 1991; Lee et al. 2013; Otto 1996; Tersigni 1992), heterogeneity in managerial practices points to different values of input productivity at hospitals with different level of output.
The recent technique of quantile regression analysis may be viewed as a convenient tool for formal quantification of heterogeneity of technology in hospital production. The analysis is based on the premise that different types of technology (interpreted as productivity of hospital inputs and as partial effects of hospital characteristics) correspond to different output quantiles, so hospital technology has consequences for the ability to maximize output. Statistically different values of the coefficients for hospital inputs and hospital characteristics, obtained in regressions for low-output and high-output quantiles, would indicate the presence of different types of hospital technology (Koenker 2005). The quantile regression approach does not extrapolate the mean tendency to the tails of the distribution and thereby avoids bias, which is inherent to groupwise post-estimation under conventional mean regression (Hendricks and Koenker 1992; Koenker and Bassett 1978). Another merit of the approach is equivalence of the linear quantile regression to a monotonically increasing transformation, which is a useful feature for estimating log-linearized production functions.Footnote 1 Despite its advantages, the use of quantile regression for purposes of productivity analysis in health economics has to date been limited to studies of the highest output quantiles and has concentrated primarily on nursing homes, which are a very specific type of healthcare facility (Christensen 2004; Knox et al. 2007; Liu et al. 2008; Martin and Jérôme 2016). Another shortcoming of the existing health economics literature is the inability to deal with panel data quantile regression models without imposing any restrictions: either the data are only pooled (Knox et al. 2007) or hospital effects are introduced in the model as a function of a potentially misspecified list of covariates (Hsu et al. 2017).
The purpose of this paper is to measure heterogeneity in hospital productivity by estimating the longitudinal production function of hospitals and evaluating marginal products of labor, capital, and medicines across conditional quantiles of output. The novelty of the present paper is severalfold. To the best of our knowledge, the paper is the first application of a quantile regression approach for measuring a general form of longitudinal production function in the hospital industry. We use a panel data quantile regression model with fixed effects for estimating productivity of capital, medicines, physicians, nurses, technicians, administrators and other staff. Next, the paper assesses optimality of input mix and quantifies potential cost savings across conditional quantiles of hospital output. Finally, using a second-stage sensitivity analysis, the paper ties public regulation, demand patterns and heterogeneity to the production function. For this purpose, we examine the association between production efficiency and a range of regional and municipal variables.
Our sample consists of acute-care regional and municipal public hospitals in Japan in 1999–2018. It should be noted that many productivity studies estimate hospital cost functions, but their approach is based on the assumption of cost minimizing behavior which is not necessarily exhibited by public hospitals (Blank and van Hulst 2017). Therefore, our paper follows the strand in the health economics literature that estimates input productivity through the analysis of production function (Jensen and Morrisey 1986; Thurston and Libby 2002).
Japanese local public hospitals are often criticized for inefficient models of production, and in particular, for an excessive emphasis on capital and medicines. On average total factor productivity and labor productivity have changed negligibly or decreased at these hospitals in the past decade (Kaneko et al. 2018; Zhang et al. 2018) and there has been little if any improvement in the average measures of technical efficiency (Kawaguchi et al. 2014; Kawaguchi 2008). However, this analysis is vitiated by not focusing on productivity of capital and medicines and it lacks estimations that would quantitatively address suboptimality of the labor-capital or labor-medicines mix.
Our findings are novel in establishing technological heterogeneity of Japanese local public hospitals, reflected in different relationships between the quantile index of hospital output, on the one hand, and, on the other hand, hospital technology (proxied by productivity of labor specialties, physician capital and medicines), quality (the fact of hospital accreditation and the status of a designated hospital as a reflection of the high referral rate), and teaching activity (training of nurse students and internship of young doctors).
The results of the statistical tests show that there is a more efficient production path (high-output quantiles) and a less efficient production path (low-output quantiles), and that there is a statistical difference in the values of input elasticities, input productivities and the partial effects of hospital variables across high- and low-output hospitals. Our analysis demonstrates that technological heterogeneity may be linked to different values of potential cost savings in the changeover to optimal combination of hospital inputs.
A possible explanation for the technological heterogeneity is a higher degree of labor specialization and better assignment of labor tasks at high-output hospitals, which serve larger local markets. Technology differences are also associated with managerial opportunities for efficient production. Indeed, we find that the values and time profiles of many managerial performance indicators, which are monitored as part of the managerial reform of Japanese local public hospitals, differ statistically across high-output and low-output hospitals.
The findings may be employed for answering a range of questions on the role of physicians and nurses at high-output and low-output hospitals and on the effective use of the labor of medical specialties, physical capital and medicines. The results about excess (or lack) of certain hospital inputs and of potential cost savings at each quantile of hospital output in each year over the past two decades may provide recommendations for adjusting the policy reforms by diversifying the regulation for high-output and low-output hospitals.
The remainder of this paper is structured as follows. The section “Background on Japanese prefectural and municipal hospitals” reviews the institutional background for Japanese local public hospitals. The section “Methodology” outlines the quantile regression model with fixed effects for estimating the longitudinal hospital production function. The explanation of data and variables is provided in the section “Data”. The section “Results” presents the findings on the typology of hospitals technologies, which are discussed in the section “Discussion”.
2 Background on Japanese prefectural and municipal hospitals
Japanese local public hospitals are operated by local governments of prefecture, city, town, village or a union of towns and villages. Local public hospitals show the highest deficit of all industries run by local government in Japan. The poor financial performance of these healthcare institutions has two main causes. Firstly, in an attempt to compensate for lack of physicians, Japanese local public hospitals overinvest in capital by acquiring expensive equipment, which is often underutilized (Campbell and Ikegami 1998; Kawabuchi and Kajitani 2003; Yamada et al. 1997). Moreover, hospitals often spend funds for unnecessary improvements to facilities (Hisamichi 2010). Secondly, local public hospitals suffer from ineffective management (Ikegami and Campbell 1999; Iwane 1976), reflected in large potential to improve the efficiency of capital accounting (Hisamichi 2010), to review structure of hospital beds (Kanagawa 2008) and speed up healthcare provision (Higuchi 2010; Kumazawa 2010; Nabemi 2010).
In line with the hospital productivity literature, Japanese local public hospitals have attracted academic and policy attention in respect of their undesirable trends in productive efficiency (Besstremyannaya 2013; Kawaguchi et al. 2014; Kawaguchi 2008; Takatsuka and Nishimura 2008). However, estimates of input productivity are commonly based on mean tendencies (Kaneko et al. 2018; Morikawa 2010), which do not fully capture differences between high- and low-output hospitals.
In a regulatory attempt to improve managerial performance of Japanese local public hospitals round-table discussions were held by the Ministry of Internal Affairs and Communications in 2007 and led to the ratification of guidelines for a first wave of reform of these healthcare institutions, which was launched in 2008–2013 (Ministry of Internal Affairs and Communications 2007).
The reform aimed to raise productivity and weaken the soft budget constraints of local public hospitals. A list of managerial performance indicators was designed in order to monitor hospital improvement: (1) share of ordinary revenues in ordinary expenses; (2) share of medical revenues in medical expenses; (3) share of the cost of medicines and medical materials in medical revenues; (4) share of the labor cost in medical revenues; (5) bed occupancy. The share of ordinary revenues in ordinary expenses and the share of medical revenues in medical expenses, which varied at local public hospitals from 70 to 99%, were recommended to be raised to 100% (the level, achieved at private hospitals). Bed occupancy was to be increased. At the same time, hospitals were expected to cut the shares of cost of medicines/medical materials and labor costs in medical revenues.
The reform was only partially successful, so it was followed by a second wave in 2015–2020, and new guidelines emphasized the continuation of performance monitoring (Ministry of Internal Affairs and Communications 2015). Specifically, the share of the cost of capital depreciation in medical revenues and the share of consignment fee in medical revenues were added to the list of monitored indicators. The values of both indicators were to be lowered to the levels achieved at private hospitals.
It should be noted that both the first and the second reform waves put insufficient emphasis on heterogeneity in hospital production. Target values differed only based on hospital size (total number of beds) and acute-care status.
Each hospital was obliged to develop its own plan and set its own targets. A case-by-case evaluation of the early effect of reform in a survey by Ministry of Internal Affairs and Communications showed that most hospitals did not achieve their target values (Kawaguchi et al. 2014). The reform also had only a short-term effect on hospital solvency: the share of local public hospitals with deficits dropped from 71% in 2008 to 48% in 2011, but subsequent years saw a steady reverse trend, reaching 63% by 2016 (Mandai and Watanabe 2019).
3 Methodology
3.1 Panel data smoothed quantile regression with quantile-dependent fixed effects
In this paper we employ panel data quantile regression model with fixed effects. These fixed effects reflect the unobserved characteristics of Japanese local public hospitals, such as treatment styles or managerial practices (Ikegami and Campbell 1999; Ikegami et al. 2011; Kawabuchi and Kajitani 2003; Kodera and Yoneda 2019), which could not be fully captured by the covariates available in the data. The fixed effects may be expressed in different ways for more productive and less productive hospitals, so we adhere to a general model which allows for potentially different values of fixed effects across output quantiles (i.e., quantile-dependent fixed effects).
It should be noted that the asymptotic theory for the panel data quantile regression with quantile-dependent fixed effects requires long panels (Koenker 2004) and the ratio n/T of sample size to the length of panel must be small. In this case the bias of the estimator may be neglected in inference procedures. At the same time, relatively short panels are commonly available for analysis of hospital production, and as the number of hospitals in the industry tends to be large, the ratio n/T becomes large. So the bias of the estimator in quantile regression analysis in short panels would lead to incorrect inference. Accordingly, it becomes necessary to eliminate or reduce the bias. But the usual approach to modeling quantile-dependent fixed effects (e.g., Kato et al. 2012; Koenker 2004; Harding and Lamarche 2014) does not derive the rate of convergence of the bias to zero and hence does not provide the knowledge, which would enable reduction of the bias.
Therefore, most attempts to incorporate short panels in the quantile regression analysis with quantile-dependent fixed effects impose restrictions on the model. For instance, Li et al. (2003) require strong assumptions about the distribution of the dependent variable. Other approaches require that the expected value and standard deviation of the dependent variable were linear in covariates (Machado and Santos Silva 2019) or that the fixed effects were functions of covariates (Harding and Lamarche 2016; Hsu et al. 2017).
The methodology of Galvao and Kato (2016) offers a solution to the problem of estimating quantile-dependent fixed effects in case of short panels without imposing any restrictions on the model: the Koenker (2004) quantile regression objective function is modified through smoothing, and this method of estimation enables computation of the bias and provides an approach for eliminating bias. Specifically, the Dhaene and Jochmans (2015) jackknife split-panel correction is proposed for dealing with the problem of asymptotic bias, arising from the short length of panel.Footnote 2
In this paper we employ the Galvao and Kato (2016) approach which can be formulated as follows. Consider the model
where τ ∈ (0, 1), mapping (2) is the conditional quantile of the dependent variable yit, xit is a vector of covariates and αi(τ) are fixed effects, which vary across quantiles. The estimates of the fixed effects \({\hat{\alpha }}_{i}(\tau )\) and of the coefficients \(\hat{{{{\boldsymbol{\beta }}}}}(\tau )\) are found by solving the Galvao and Kato (2016) optimization problem:
where \(G(v)=\int\nolimits_{u}^{\infty }K(v)dv\) is a smoothed analog of the step function I(u ≤ 0), K(v) is a kernel function, and h is a suitable bandwidth.Footnote 3
In order to reduce the bias of the estimator above obtained in case of short panels Galvao and Kato (2016) suggest using the split-panel jackknife estimator from Dhaene and Jochmans (2015). In case of balanced panels the Dhaene and Jochmans (2015) procedure requires splitting the panel into two: i ∈ {1, … , n} in each panel, while the time index is t ∈ {1, … , T/2} in the first panel and t ∈ {T/2 + 1, … , T} in the second panel. The split-panel estimator is computed as
where \(\hat{{{{\boldsymbol{\beta }}}}}(\tau )\), \({\hat{{{{\boldsymbol{\beta }}}}}}_{1}(\tau )\), \({\hat{{{{\boldsymbol{\beta }}}}}}_{2}(\tau )\) are respectively, estimators for the full panel, the first part of the panel and the second part of the panel. The split-panel estimator under the Dhaene and Jochmans (2015) approach has the same asymptotic variance as the original \(\hat{{{{\boldsymbol{\beta }}}}}\) estimator and allows for reliable inference under short panels.
Dhaene and Jochmans (2015) generalize the approach for the unbalanced panels as follows. Suppose there are Ti longitudinal observations for each i. For each \(T\in \{\mathop{\min }\nolimits_{1\,\le \,i\,\le \,n}{T}_{i},\ldots ,\mathop{\max }\nolimits_{1\,\le \,i\,\le \,n}{T}_{i}\}\) a balanced panel PT = {(i, t): Ti = T} is chosen and an estimate \({\hat{{{{\boldsymbol{\beta }}}}}}_{1/2,T}(\tau )\) is computed for this panel. Note that each panel PT includes all individuals with observations over T periods. Weights, which are equal to the shares of observations of each panel PT in the total sample (i.e., NT/N), are applied to \({\hat{{{{\boldsymbol{\beta }}}}}}_{1/2,T}(\tau )\). The estimator becomes:
where NT is the number of observations in panel PT and N is the total number of observations. The asymptotic variance matrix of the estimator is computed as the sum of the covariance matrices for each estimate with weights equal to \({({N}_{T}/N)}^{2}\).
3.2 Production function, input elasticities, marginal products and input mix
It should be noted that public hospitals commonly operate under soft budget constraints. So models which focus on the hospital production function and do not impose solution of the cost optimization problem seem better suited for the analysis of these institutions (Biorn et al. 2003). This approach also permits us to test whether hospitals choose their inputs optimally under given input prices.
To estimate input elasticities in a multi-product hospital we use the Panzar and Willig (1977) production transformation function F(y, x) = 1, which specifies the production possibilities frontier. It can be treated as an output distance function under the Coelli and Perelman (1999) restriction of F(y, x) being homogeneous of degree 1 in y.Footnote 4 We employ the translogarithmic form of F(y, x), which is a widely used example of a flexible function for the analysis of hospital production (Vita 1990).
where m is the index for output, \(M=\dim ({{{\bf{y}}}})\), k indicates inputs, \(K=\dim ({{{\bf{x}}}})\), h are hospital control variables, and α is a constant. After rearranging terms in (4) under conditions (5) we obtain:Footnote 5
Equation (6) can be used to calculate the elasticity of the production function with respect to a given input:
Marginal product of an input k, which is interpreted as productivity of input k, is derived as \({{{{\rm{MP}}}}}_{k}=-\frac{\partial {y}_{M}}{\partial {x}_{k}}=-\frac{\partial \ln {y}_{M}}{\partial \ln {x}_{k}}\cdot \frac{{y}_{M}}{{x}_{k}}={\epsilon }_{k}\cdot \frac{{y}_{M}}{{x}_{k}}\). The marginal rate of technical substitution between inputs \({x}_{{k}_{1}}\) and \({x}_{{k}_{2}}\), which is defined as \({{{{\rm{MRTS}}}}}_{{k}_{1},{k}_{2}}={{{{\rm{MP}}}}}_{{k}_{1}}/{{{{\rm{MP}}}}}_{{k}_{2}}\) (Mas-Colell et al. 1995, p. 130; Chiang 1984, p. 210), becomes
Under the assumption of cost minimization behavior by hospitals, the marginal rate of technical substitution equals the ratio of input prices (Mas-Colell et al. 1995, p. 137; Chiang 1984, p. 419). The inequality implies that Japanese hospitals do not minimize costs through the optimal choice of inputs. For instance, if \({{{{\rm{MRTS}}}}}_{{k}_{1},{k}_{2}} > \frac{{p}_{{k}_{1}}}{{p}_{{k}_{2}}}\), then the ratio \(\frac{{x}_{{k}_{1}}}{{x}_{{k}_{2}}}\) is less than optimal and input k2 is overutilized relative to input k1.
3.3 Empirical model
3.3.1 Specification for quantile regression analysis
For a given hospital i at time t the value Fit = F(yit, xit) ∈ (0, 1]. Treating \(\ln {F}_{it}\) as a random error term (Coelli and Perelman 2000), (6) can be transformed into the regression specification, where the higher the quantile index, the larger the hospital’s output:Footnote 6
Here \({Q}_{\tau }(\ln {y}_{M}| {{{\bf{x}}}},{{{\bf{h}}}})\) is the conditional τth quantile of \(\ln {y}_{M}\), αi(τ) denotes fixed effects and dt(τ) are annual dummies which capture time effects associated with technological progress in the hospital industry. Control variables hjit include the binary variable for the use of electronic data systems,Footnote 7. We also add the interaction terms for Tohoku region and 2010 year, as well as the interaction term for Tohoku region and 2011 year to capture potential impact on production of the Great East Japan Earthquake of March 2010.
3.3.2 Estimation and inference
Equation (9) is used to estimate the conditional quantile of the dependent variable for each value of τ.Footnote 8 This way we avoid a multiple testing issue inherent to multiple quantile models and the estimates at quantiles outside of the extreme of (0,1) are not influenced by potential failure of the standard asymptotic theory to provide an accurate representation of the finite sample distribution. We use 13 values of τ ∈ [0.2, 0.8], starting with τ = 0.2 at the 0.05–step for detailed analysis. The potential tendencies across quantiles are established by consideration of the relative values of coefficients at several quantile points, adjacent to the extremes of this interval. The size of our sample (5845 observations) together with the total count of parameters (382 comprising 32 coefficients for covariates in the translog specification, 330 fixed effects for each hospital and 20 time effects for each year) restrict the expansion of the interval’s bounds, so we are unable to consider τ < 0.2 or τ > 0.8.Footnote 9
The fit of each regression is assessed using an equivalent of the R2 statistic computed for pairs of quantile regressions: with a restricted set of covariates and with a full set of covariates (Koenker and Machado 1999). Owing to the panel data structure of our model, we compute two variants of this pseudo R2 statistic, which resemble the within R2 for the linear model for panel data: the first compares the full model with the model with only hospital fixed effects, and the second contrasts the full model to the model with hospital fixed effects and time effects.Footnote 10
The Galvao and Kato (2016) asymptotic variance matrix is used for making inference about the coefficients. Standard errors for elasticities and other indicators which are functions of the coefficients are computed using the delta method.
The Wald test is employed to assess hypotheses about the differences between coefficients estimated in regressions for different values of τ. Specifically, we use the Koenker (2005) approach for applying Wald tests in order to assess linear hypotheses in quantile regressions.Footnote 11
3.3.3 Second-stage analysis
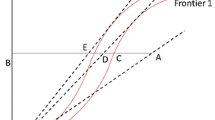
The value of the log distance function \(\ln {F}_{it}\) can be interpreted as productive efficiency of hospital i at time t (Knox et al. 2007), and higher values represent higher efficiency. The approach provides more robust estimates than the classic methods of efficiency analysis, which model optimal technology with nonparametric or parametric frontier analysis (Bernini et al. 2004; Liu and Tone 2008).Footnote 12
We use the estimated distance function for high quantile values (0.75, 0.8) as an approximation of the production possibility frontier (Koenker 2005; Liu and Tone 2008), and calculate the residuals
Note that the residuals correspond to the value of the log distance function together with the individual effects and annual effects, since these quantile-dependent effects cannot be identified separately in the analysis that has the general form of the fixed-effect panel data quantile regression model.
The second-stage analysis of hospital productive efficiency scores \({\hat{u}}_{it}\) employs covariates that are associated with competition, regulation and demand patterns in the hospital industry (Blank and Valdmanis 2010; Ferrier and Valdmanis 1996; Jacobs et al. 2006; Rosko 1999, 2004). The variables for regulation proxy the stringency of financial constraints of the hospital: specifically, we use the share of subsidies and transfers in hospital medical revenues (Yamada et al. 1997) (denoted in the equation below subsidiessh) and the binary variable dpc for involvement in the prospective payment system (Rosko 1999).Footnote 13 The available data do not allow construction of the Herfindahl–Hirschman index, but we proxy the index by the share of the hospital’s beds in the total number of beds in a municipality (bedshare) and by the share of the hospital’s doctors in the total number of doctors in the municipality (docshare). The demographic component of demand pattern is proxied by the share of the population over 65 (shareover65) in the total population of the municipality (Morikawa 2010) while the socio-economic and geographic components are proxied by the standard financial need, which is the product of unit cost of public services, demand for public services and an adjustment coefficient which accounts for socio-economic and geographic factors. (We use log of per capita standard financial need, which is denoted lpstfinneed.)
The estimated equation becomes:
where κi are hospital effects, μt are time effects and εit is a stochastic error term.
3.4 Counterfactual policy analysis: optimal values of inputs and potential cost savings
Suboptimal choice of inputs is associated with excessive costs of a hospital. So using the results of estimation of Eq. (9), we conduct a counterfactual policy analysis: an evaluation of potential cost savings in case of changeover from the values of inputs observed in the data to optimal values.
The optimal values are defined as follows: these values minimize total cost of inputs and provide for the production of a given amount of output under fixed elasticities of the production function and under fixed values of the hospital control variables.
Consider a quantile τ ∈ (0, 1). The following approach is used to find the optimal values of inputs.Footnote 14 Using Eq. (11), we compute the mean elasticities for each input in the regression for conditional τth quantile of hospital output.
Next we focus on a given hospital i and find its optimal amount of inputs through a two-step procedure. (For brevity we omit argument τ in all variables in the description.) First, we compute the residual \({\hat{A}}_{it}\) left after subtracting the linear combination of log inputs \(\ln {x}_{kit}\) with corresponding coefficients \({\hat{\epsilon }}_{k}\) from log output:Footnote 15
(note that hospital controls are included in \(\hat{A}\)).
The mean elasticity \({\hat{\epsilon }}_{k}\) comes from the estimates of Eqs. (7) and (9) as follows.
Second, we solve the cost minimization problem:
where p1it, … , pKit are the values of input prices at the hospital. Here the boundary condition ensures that the hospital produces the same amount of output as is found in the data.Footnote 16
The solution of the cost minimization problem constitutes the optimum tuple of inputs \({x}_{1it}^{* }\), … , \({x}_{Kit}^{* }\).
The optimum value of the hospital costs is calculated as:
So the potential percentage reduction in hospital costs in case of changeover from the actually employed amounts of inputs to the optimal values becomes
where the cost of actually used inputs Cit is computed as
Similarly to the input elasticities, we report the values of cost savings for 1999–2018 and for the whole period.
For each τ, the optimal costs are compared with the factual costs through the standard t-test. For this purpose, we find hospitals where production is close to production in the τth quantile. This is done by considering the group of hospitals in (τ − 0.1, τ + 0.1) according to residuals obtained in the regression for the conditional τth quantile of hospital output. For example, for τ = 0.2 we consider the interval of hospitals with residuals in (0.1, 0.3). The point of the intervals is to avoid unstable results due to small subsamples of hospitals. Similarly, the t-test is applied to hospitals in (τ − 0.1, τ + 0.1) to evaluate the hypothesis about the equality of %ΔC to zero.
4 Data
4.1 Sources
The analysis uses data for Japanese local public hospitals from several sources. The main data source is annual surveys of all local public hospitals in Japan, published in digital form by the Department of Local Finance of the Ministry of Internal Affairs and Communications (Chihou Kouei Kigyou Kessan), with available variables for fiscal years 1999–2018. Participation in the prospective payment system is taken from an administrative database by the Ministry of Health, Labor and Welfare (2020). We use the Japan Council for Quality Health Care (2020) data on hospital accreditation. The names of designated local hospitals (hospitals with high referral rate and an additional subsidy per inpatient)Footnote 17 and the dates when they obtained this status come from the Ministry of Health, Labor and Welfare (2012) and the annual Survey of Finances of Hospital Enterprises (Byouin Jigyou Kessan Joukyou) by the Ministry of Internal Affairs and Communications (2020). We use hospital participation on the market for medical school graduates, taking data from the web portal of the Japan Residency Matching Program (2020). The binary variable for the use of electronic data systems—electronic medical records or electronic ordering system—is constructed using the date of the introduction of these systems at hospitals, published on the web portal of Software Service, Inc. (2021).
The data for Japanese prefectures and municipalities (population, number of acute-care beds and number of physicians at prefectural and municipal healthcare facilities) come from the Statistics Bureau of Japan, the Portal Site of Official Statistics of Japan (2020). The standard financial need of the prefecture or municipality (Kijun Zaisei Juuyougaku)Footnote 18 is taken from the annual Surveys of Prefectural and Municipal Finances (Toudoufuken Kessan Joukyouchou. Shichouson-betsu) carried out by the Ministry of Internal Affairs and Communications (2020). Data on the budgets of prefectures and municipalities from the annual Surveys of Local Public Finance (Chihou Zaisei Joukyouchousa), reported by the Statistics Bureau of Japan, are used to construct the prefectural/municipal profitability variable.
Hospital addresses are retrieved from the Tokyo’s Institute for Health Economics and Policy database on healthcare providers in Japan (Zenkoku Hokensya Iryoukikan. Byouin, Shinryoujo), available since 2015. Websites of hospitals which has ceased to exist by 2015 were used to restore the historic data on hospital location.
4.2 Sample
The non-anonymous character of the databases allows us to merge them by year, hospital name and the name of the prefecture or municipality.
The universe of Japanese local public hospitals includes 884–1007 institutions in 1999–2018.Footnote 19 To guarantee a certain homogeneity of hospital production in the absence of any variable directly related to the prevalence of patients with different diagnoses (case mix) we follow the common strategy of taking only hospitals with acute-care beds (Fujii 2001; Kawaguchi et al. 2014; Yamada et al. 1997). The group of hospitals with only acute-care beds constitutes 615–636 healthcare institutions in 1999–2003, but only 310–426 institutions in subsequent years. This fall in numbers since 2003 reflects the introduction of a long-term care bed category, which was formally embedded into the acute-care beds (Table 1).
We discard hospitals which fail to report the numbers of outpatients or hospital discharges. Next, we exclude data with missing numbers of doctors, nurses and other hospital staff (missing values for these hospital inputs account for 5–6% of observations), and where the values depreciable fixed capital or of on medicines are not reported (5–9% of observations in various years).
Furthermore, we omit data with average length of stay below 6 daysFootnote 20 or over 90 daysFootnote 21 (1% of the sample), and data with bed occupancy falling below 0.1.Footnote 22 Finally, we impose a technical condition by which a hospital must be present in the database of at least 11 years out of the analyzed 20. The condition enables identification of hospital fixed effects. Note that imposing this condition automatically adjusts for the change in the definition of acute-care beds in 2003: hospitals that where classified as having only acute-care beds in 1999–2002 but lost this classification in 2003 (after a part of these beds became long-term care) would not have T ≥ 11 and would not be included in our sample. Our final sample consists of 246–322 hospitals in various years (5845 longitudinal observations with 330 hospital clusters).
4.3 Variables
Since administrative databases commonly suffer from lack of hospital-level variables on the actual outputs of hospital activity (such as improvement of patient’s health after completion of medical treatment), we follow a common approach in the hospital productivity literature and use proxies for hospital outputs. A list of such proxies often includes outpatient visits, inpatient admissions and discharges (Jacobs et al. 2006; Rosko and Mutter 2008; Worthington 2004). The Japanese local public hospital database reports the daily number of outpatients which we use as an output in the absence of other, more detailed data. Following the approach by Takatsuka and Nishimura (2008) we compute another output as the mean of admissions and discharges for acute-care hospitals with acute-care beds.Footnote 23 It should be noted that hospitals may pursue other activities as well as treating patients, notably scientific research, and we follow the Jacobs et al. (2006) approach, which captures it by adding the share of research expenditure in hospital revenues.
Labor inputs are doctors, nurses and other hospital staff.Footnote 24 The number of nurses is the sum of licensed practical nurses (the Japanese term is “assistant nurses”) and registered nurses.Footnote 25 Other hospital staffFootnote 26 includes technicians (59%), administrative personnel (29%) and all other staff (12%).
Capital input is depreciable fixed capital (buildings and equipment). Owing to the emphasis of Japanese healthcare on pharmaceuticals, medicines (medical materials and medicines per se, proxied by their costs) are treated as an additional input (Motohashi 2009). This approach follows studies using data from the US and UK, where medicines are viewed as an input in the production function (Pauly 1980; Feldstein et al. 1974).
Regarding input prices, the proxy for labor price is total labor cost of a given labor input divided by the amount of this input. Capital price is proxied by the share of depreciation and real interest expenditure in the book value of depreciable fixed capital (Fujii 2001). The data allow us to construct the proxy for the price of a component of medical materials (medicines per se). The proxy is the retail cost divided by revenue – the inverse of the so-called drug margin rate (Yamada et al. 1997). We implicitly assume that managerial attitude towards medicines and medical materials is similar, so this proxy price for medicines is expanded in our analysis to relate to all medical materials.Footnote 27
As regards hospital characteristics, the quality of care can be proxied by the referral rate. The values of the variable are unavailable, but we use data for the binary status of designated local hospitals (such hospitals must have a referral rate above 60–80%). Other dichotomous hospital characteristics are binary variables for having student nurses and for attracting residents through participating in the Japan Residency Matching Program.
We use bed occupancy to proxy a hospital’s uncertainty about output and openness for emergency care. Bed occupancy may be viewed as “a measure of demand for hospital services” (Ferrier and Valdmanis 1996) and lower bed occupancy indicates willingness to accept more emergency patients (Doi et al. 2005; Yamada et al. 1997).
As regards patient characteristics, we follow Yamada et al. (1997) and use the mean number of examinations per patient as the only available proxy for the severity of diagnosis. The list of variable names and the descriptive statistics are given in Table 2.
We add binary variables for each year to account for annual effects. Annual changes in aggregate medical prices are negligible within the analyzed period, so explicit introduction of a medical consumer price index along with annual dummies would not affect our results.
5 Results
5.1 Typology of technologies
The results of estimating Eqs. (9), (11), (8), (12), (13) for different quantiles τ are given in Table A.1 (coefficients for inputs and hospital characteristics), Table A.2 (input elasticities), Table A.3 (marginal products), Table B.3 (marginal rate of technical substitution), Supplementary Tables S46–S47, and Figs. 4 and 5 (optimal values of inputs and potential cost savings).
To establish technological heterogeneity we test for the statistical difference of the values of coefficients, obtained in quantile regression for pairs of low- and high-output quantiles (0.2 and 0.8, 0.25 and 0.75). We also test whether the coefficients in each of these low- and high-output quantiles differ from the estimates in the median regression. Similar comparison is conducted for input elasticities, input productivity (evaluated at sample means) and potential cost savings.
The results of the tests, which are given in Supplementary Tables S5–S24 and summarized in Table 3, show technological distinctions across high-output and low-output hospitals, reflected in the effect of the hospital control variables (teaching activity, accreditation, the status of designated hospital, the use of electronic data), in elasticity and productivity of labor of technicians, administrators and other staff, capital and medicines, and in potential cost savings.
5.2 Input productivity
5.2.1 Labor specialties
Physicians are most productive among labor specialties at Japanese local public hospitals, which differs from findings in US and European data, where the highest productivity is observed among nurses (Blank and van Hulst 2017; Jensen and Morrisey 1986). Production at the highest quantiles of hospital output is associated with lower elasticity of physician labor but higher elasticity of technicians, administrators and other staff. However, the labor of technicians and other staff is insignificant in explaining hospital output in low-output quantiles.
5.2.2 Capital and medicines
There is an inverse relationship between productivity of capital and hospital output: the higher the output, the lower the returns to capital. An inverse relationship is observed between productivity of medicines and hospital output.
Arguably, high-output hospitals do not overinvest in capital and medicines for treating patients. Instead, they demonstrate higher labor productivity, which is largely attributed to the highest productivity of technicians, administrators and other staff.
5.2.3 Time profiles
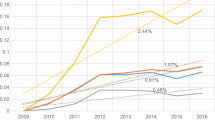
Note that input elasticity as well as marginal product of each input are functions of the estimated coefficients in Eq. (11) and the time-varying variables (outputs, inputs, input prices, hospital characteristics). Evaluation of time-varying variables at annual values of the sample means enables the computation of input elasticities (Supplementary Tables S7, S10, S13, S19 and S22), input productivities (Fig. 1 and Supplementary Tables S26, S29, S32, S38 and S41), marginal rate of technical substitution (Table B.3), optimal inputs (Fig. 4 and Supplementary Table S47) and potential cost savings in 1999–2018 (Fig. 5 and Supplementary Table S46).
As regards time profiles of productivity of physicians and nurses, the patterns below are generally observed at all quantiles of hospital output. The marginal product of physician labor goes up in 1999–2004.Footnote 28 The rise in productivity may be linked to the biennial revisions of the unified fee schedule in 2002 and 2004, which were the first historic instances of reduction of the price for healthcare services. However, the productivity of physicians has seen a steady fall since 2004.
Productivity of nurses declines over the analyzed period. Falling productivity of doctors and nurses at Japanese local public hospitals can be largely explained by shortage of specialized personnel and resulting excessive workloads. Number of nurses in Japanese local public hospitals in the 1900s and 2000s were insufficient by international standards and there was a particular shortage of highly qualified and experienced nurses with lengthy tenure (Ikegami and Buchan 2014). Shortages of doctors at Japanese local public hospitals has been long observed in the academic and policy literature (Ikegami 2014).
Hospitals vary as to annual trends in the productivity of technicians, administrators and other staff, as well as productivity of capital and medicines. The productivity of technicians, administrators and other staff at high- and median-output hospitals increases in 1999–2011 and then falls in subsequent years. However, the productivity of this input at high-output hospitals declines throughout the period 1999–2018. Nonetheless, the value at high-output hospitals is several times larger than at low-output hospitals.
Productivity of capital decreases in 1999–2002 but then remains flat in low-output quantiles. High-output quantiles show a rise in the productivity of this input in 1999–2004, followed by steady values in subsequent years (Supplementary Tables S38, S39, S41 and S42).
Productivity of medicines goes up in 1999–2002, but then falls in 2003 and remains steady at median- and low-output hospitals. At high-output hospitals, the fall in productivity of medicines continues from 2003 until 2018.
The reform of local public hospitals launched in 2008 must have had a temporary positive effect by increasing the elasticity of physicians, technicians, administrators and other staff in 2008–2013. But the elasticity either remained flat or fell in subsequent years. As regards input productivity, the reform only succeeded in boosting productivity of technicians, administrators and other staff at median- and low-output hospitals in 2008–2011. The temporary effect of the reform on productivity is similar to temporary improvement of solvency of local public hospitals in 2008–2013 (Mandai and Watanabe 2019).
Significant changes in technology over time are observed with respect to the productivity of physicians and aggregate labor at both high- and low-output quantiles: there is statistical difference in the values of productivity of these inputs in case of each group of hospitals.
The finding contrasts with absence of differences in labor productivity at US hospitals from the mid-1960s to the late 1980s (Thurston and Libby 2002).
In addition, statistically significant annual changes in productivity of nurses and capital are observed at low-output quantiles, while high-output quantiles show annual changes in productivity of technicians, administrators and other staff.Footnote 29
5.3 Effect of hospital characteristics
Estimation of the Eq. (9) shows that each of the teaching variables—the fact of having student nurses and participation in the Japan Residency Matching Program—has a negative effect on production in the first-stage Eq. (9). The result is in line with the findings for US hospitals and may be explained by additional workload on physicians and nurses, who have to act as supervisors (Jensen and Morrisey 1986). However, the negative effect is less pronounced in high-output hospitals than in low-output hospitals.
The use of electronic data systems has a positive and significant effect on production at low-output quantiles. But the effect of the variable is insignificant at high-output hospitals and at some hospitals with medium values of the quantile index. Arguably, these hospitals have already employed efficient patterns of medical treatment, so the introduction of electronic data systems did not have an additional impact on productivity. Our result that finds heterogeneity of the effect of the variable is in line with the findings about differential impact of the use of electronic medical records on labor productivity at groups of Japanese local public hospitals and absence of the positive mean effect on multi-factor productivity (Kaneko et al. 2018).
Research activity reduces hospital output in low- and median-output quantiles, but does not affect production at high-output quantiles. Similarly, binary variables for healthcare quality—hospital accreditation and designation—have negative estimated coefficients. Arguably, higher quality care requires additional workload and intensive diagnostics, so ceteris paribus the number of treated inpatients and outpatients may decrease.
The results of the second-stage regression (10) reveal that productive efficiency is negatively affected by the share of subsidies in hospital revenue and by profitability of local government (Table B.2). Concerning the demographic component of the demand for healthcare at local public hospitals, the share of people below 65 in the total population of a municipality is negatively significant in explaining productive efficiency of a hospital. This result may be linked to relatively higher severity of medical cases among the elderly population, leading to loss of productive efficiency. Per capita standard financial need, embracing the demand for public services, adjusted for socio-economic and geographic factors, has a negative effect on efficiency. So hospitals may demonstrate lower efficiency in conditions of higher demand for their services.
As regards the proxy variable for the Herfindahl–Hirschman index, there is a positive relationship between the share of the hospital’s beds in the total number of beds of a municipality and the hospital’s productive efficiency. The findings is in line with the results of studies using the US data (Blank and Valdmanis 2008; Rosko 1999) and may be explained by the fact that healthcare markets are seldom competitive (Hollinsworth and Peacock 2008).
5.4 Optimal amounts of inputs and potential cost savings
The difference between marginal rate of technical substitution and price ratios is not statistically significant for pairs of labor inputs (doctors, nurses, technicians, administrators and other staff), so the mix of labor specialties does not statistically differ from optimal in all quantiles. However, the input mix between physical capital and total labor staff, between physical capital and medicines, and between medicines and total labor staff is suboptimal (Table B.3).Footnote 30
Accordingly, there are substantial opportunities for cost savings through changeover to an optimal combination of inputs. Decrease of the amount of capital is required for this purpose at all quantiles (Supplementary Table S47). High-output hospitals need to increase the number of technicians, administrators and other staff, but cut the amount of medicines and slightly reduce the number of doctors. Low- and median-output hospitals needed to increase the number of doctors, reduce the number of technicians, administrators and other staff, reduce the amount of medicines in 1999–2014 but increase the amount of medicines in 2015–2018.
For each output quantile the number of nurses required in the optimal combination of inputs is smaller than the actual number, so the number of nurses has to be reduced. This apparently counterintuitive finding might be explained if, due to the shortage of physicians at Japanese local public hospitals,Footnote 31 nurses have to take on the role of physicians, at least in part. This could explain the shortage of nurses in the current situation. But in the optimum situation the number of doctors is increased, so the number of nurses may need to be reduced.
Potential reduction of hospital costs thanks to changeover to optimal inputs varies from 10 to 25%, and the largest cost reductions in percentage terms may be expected at the lowest output quantile. However, high-output quantiles also have vast opportunities for cost reduction. In some years the potential percentage reduction of their costs exceeds that of low- and median-output hospitals.
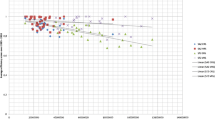
5.5 Performance indicators in the reform of local public hospitals
To examine the impact of technological heterogeneity in hospital response to the reform, we estimate average values of the performance indicators at high-, low- and median-output quantiles.
With the exception of the share of depreciation in medical revenues, differences across high- and low-output quantiles are observed for all managerial indicators (Figs. 2 and 3 and Table 4). The differences are most salient for the share of medical revenues in medical expenses and the share of labor costs in medical revenues. For both indicators, the higher the output quantile, the closer the value of the indicator to the recommended target.
As regards time profiles of the indicators, the reform of local public hospitals can be regarded as successful with respect to the share of cost of medicines in medical revenues. The indicator, which was considered to be excessively high, is decreasing and falls below the recommended target in the groups of high- and median-output hospitals in 2009 and in the group of low-output hospitals in 2016.
Desirable trends were observed for a time in the share of ordinary revenues in ordinary expenses, which was below 100% and needed to increase. It rose in all quantile groups in 2006–2011. However, the values remained below the recommended targets and started falling slightly in later years. As stated by the reform guidelines, the share of labor costs in medical revenues decreased in 2008–2012. But the trend was then reversed: the value of the indicator began to increase from 2011 to 2015 in different output quantiles.
5.6 Analysis for hospitals of different size
Since the fixed-effect model does not enable us to explicitly include time-invariant covariates, such as groups of hospitals by size, we classified hospitals according to the number of their beds for purposes of the post-estimation analysis: small (20–99), medium-sized (from 100 to 299) and large (300 and above).Footnote 32 We then estimated average values of input elasticities, input productivities and other parameters for high-, low- and median-output quantile in groups of small, medium-sized and large hospitals.
The results show that difference in the productivity of inputs at large hospitals exists across high- and low-output quantiles for the labor of technicians, administrators and other staff, and across high- and median-output quantiles for capital. Medium-sized hospitals show differences in the values of productivity of both capital and the labor of technicians, administrators and other staff inputs across high- and low-output hospitals as well as across high- and median-output hospitals (Supplementary Tables S59–S64 and Supplementary Figs. S1–S3). The values of potential cost savings after changeover to an optimal amount of inputs differ between high-output and low-output hospitals within each category of small, medium-sized and large hospitals (Supplementary Tables S77, S79 and S81).
Statistically significant differences in the values and time profiles of five managerial indicators, monitored since the first wave of the reform of local public hospitals, are observed at high- and low-output hospitals in each category of hospitals, classified by their size. These indicators are: the share of ordinary revenues in ordinary expenses, the share of medical revenues in medical expenses, the share of labor costs in medical revenues, the share of costs of medicines in medical revenues, and bed occupancy. The finding supports the cause of further policy diversification, since currently the reform guidelines set different targets only for groups of hospitals of different size (Supplementary Tables S83–S109 and Supplementary Figs. S10–S15).
5.7 Limitations
We note several limitations of the analysis. Firstly, we follow the common approach in health productivity analysis to use a multi-output production function (Hollinsworth and Peacock 2008; Jacobs et al. 2006), which imposes assumptions about additivity across inputs. However, the alternatives of combining all outputs (e.g., adding inpatients and outpatients) or concentrating on one output only may not fully capture the multi-product character of hospital operations. Secondly, inability to directly observe the quality of labor may result in underestimation of labor returns in high-output hospitals, where human capital is substantial. Thirdly, there is no variable directly related to the case mix of Japanese hospitals, except for those which are involved in the prospective payment system. To proxy homogeneity of patient cases, we follow the general trend in the Japanese hospital literature and limit our sample to hospitals with acute-care beds.
6 Discussion
The results of the estimations point to technology distinctions across high- and low-output acute-care local public hospitals in Japan. Specifically, heterogeneity in hospital technology is reflected in statistically different values of productivity of physicians, technicians, administrators and other staff, physical capital and medicines; it is also apparent in partial effects on production of teaching variables, the status of accreditation and designation; and also in cost savings after changeover to optimal input mix.
The discrete typology of technologies associated with production at Japanese local public hospitals goes in line with findings about the discrete typology of hospital managerial practices (Bloom et al. 2015). Indeed, input productivity can be regarded as a function of managerial efforts (Bloom et al. 2017), and poor management and lack of information can be viewed as major reasons for the existence of inferior technologies (Tsionas 2002).
High-output hospitals are characterized by higher productivity of the labor of technicians, administrators and other staff, probably explained by managerial efforts such as organizational support for team work of physicians and technicians on data management and diagnosis coding (Saito 2007; Shima et al. 2006), revision of occupancy of operating theatres and of the workload at inpatient/outpatient divisions (Doi et al. 2005; Tomioka et al. 2008), and faster reporting of the results of medical tests (Suwabe 2004).
Lower productivity of physicians’ labor at high-output hospitals may be related to a higher degree of labor specialization, possibly owing to larger size of the local market. This supposition can be linked to the theory of local demand shifters of labor specialization in service industries, developed in Baumgardner (1988a) as an extension of the Stigler (1951) model of the impact of market size, originally stemming from the seminal theorem of Adam Smith. The empirical proof for the hospital industry can be found in Baumgardner (1988b).Footnote 33 Similarly, Acemoglu and Autor (2011) allow for an assignment of labor tasks, which may be linked to labor specialization.
High-output hospitals show better values of many managerial performance indicators that were monitored during the reform of local public hospitals in Japan. The values of these indicators are statistically different between groups of high- and low-output hospitals. The finding supports the argument about interrelation between management and production.
Low-output hospitals show higher productivity of capital and medicines, while the productivity of technicians, administrators and other staff is most often insignificant.
7 Conclusion
Innovations in hospital technology are often targeted at a particular input, so it is important to examine the productivity of labor specialties, capital and medicine at hospitals (Blank and van Hulst 2017). Moreover, the technology distinction caused by the productivity of labor specialties, capital and medicines is crucial for disentangling best and worst practices and for making judgments about the differential impact of policy reforms (Acemoglu and Finkelstein 2008; Weisbrod 1992). However, empirical evidence on the issue is insufficient and there is a gap in the literature as regards quantification of differences in input productivity across groups of hospitals.
Our paper addresses technology differences at hospitals using a conditional quantile regression approach applied to analysis of the production function. The novel finding of the paper, which employs longitudinal data for Japanese local public hospitals in 1999–2018, is technological heterogeneity expressed as different levels of productivity of labor, capital and medicines at high- and low-output hospitals. Secondly, changes in the values of productivity of labor and capital are discovered over the analyzed period. Finally, differences in the values of input productivity, potential cost savings in case of changeover to optimal amount of inputs, and managerial performance indicators across high- and low-output hospitals persist even after controlling for hospital size.
The establishment of technological heterogeneity underlines the importance of input productivity analysis in the hospital sector. We believe that the quantification of technological heterogeneity of Japanese local public hospitals offers helpful guidance for regulatory changes. In particular, different values of the productivity of labor, capital and medicines at high-output and low-output hospitals may imply different values for the marginal rate of technical substitution and hence different conclusions about the optimality of input mix and potential cost savings.
Data availability
The links to all publicly available datasets used in the current paper and the list of variables are provided in the appendices. The data on financial information of Japanese local public hospitals (Annual Surveys of Local Public Enterprises. Hospitals) have been publicly available on the website of the Japanese Ministry of Internal Affairs and Communications on a rolling basis for most recent years (2014 onwards as of July 2021). The data for 2002–2013 are publicly available through the Web Archiving Project of the National Diet Library (Tokyo) https://warp.da.ndl.go.jp/?_lang=en. Data for earlier years can be obtained from the Statistics Department of the Japanese Ministry of Internal Affairs and Communications upon request: https://www.stat.go.jp/library/faq/faq05/faq05b06.html. The publicly available data used in the current paper can be requested from the corresponding author.
Notes
Specifically, in this paper we use the fact that \({Q}_{\tau }(\ln y| x)=\ln ({Q}_{\tau }(y| x))\), where Qτ is the conditional τth quantile of the dependent variable y under fixed x.
The Galvao and Kato (2016) smoothing technique for reducing the asymptotic bias of the estimator is applicable for a more restricted model with quantile-independent fixed effects: it is used in the Chen and Huo (2020) estimator. Note that a different approach for creating a quantile-independent fixed effects estimator, which could apply to short panels, was proposed by Canay (2011), but the estimator was shown to have asymptotic bias (Besstremyannaya and Golovan 2019).
Galvao and Kato (2016) do not touch on the choice of the bandwidth. So our estimations follow the methodology of Koenker (2005), section 4.10.1 for computing the asymptotic covariance matrix, which specifies the bandwidth as h = κ(Φ(τ + h1) − Φ(τ − h1)). We take h1 from Bofinger (1975) and κ from Koenker (2005).
An alternative approach is the use of normalization that requires homogeneity of degree 1 in inputs. Consideration of an input distance function under this approach leads to very similar results, as both approaches approximate the same production possibility frontier.
The numerical values of the estimated coefficients depend on the order of outputs, but qualitative results concerning the typology of technologies and other findings related to the analysis with the output distance function hold regardless of the order of outputs.
The use of the translog function may cause a multicollinearity problem. Our analysis deals with the panel data regression with fixed effects, so to assess the problem we compute correlation coefficients after the within-group transformation: the subtraction of the per-hospital mean from each regressor. The values of the correlation coefficients do not exceed 0.48.
The approach assumes that the use of an electronic data system has a multiplicative effect on production. A more detailed analysis requires the inclusion of interaction terms of the variable and each input (as well as the products of pairs of inputs). However, it substantially increases the degrees of freedom and so the approach becomes unfeasible given the size of the sample available for estimations.
The asymptotic inference works poorly for extreme quantiles outside the (0.2, 0.8) range, as it is shown in Chernozhukov (2005).
Additionally, we compute the pseudo R2 statistic, which compares the full model with the model with only a constant term (the statistic is employed for evaluating the fit of pooled models in the quantile regression approach and is calculated solely for reference purposes).
The general linear hypothesis \({{{{\rm{H}}}}}_{0}:R[{{{\boldsymbol{\beta }}}}{^\prime} (\tau ),{{{\boldsymbol{\beta }}}}{^\prime} (\tau {^\prime} )]{^\prime} =r\) can be evaluated using the Wald statistic (Koenker 2005; section 3.3): \(W=(R[{{{\boldsymbol{\beta }}}}{^\prime} (\tau ),{{{\boldsymbol{\beta }}}}{^\prime} (\tau {^\prime} )]{^\prime} -r){^\prime} {(R\hat{VR}{^\prime} )}^{-1}(R[{{{\boldsymbol{\beta }}}}{^\prime} (\tau ),{{{\boldsymbol{\beta }}}}{^\prime} (\tau {^\prime} )]{^\prime} -r)\), where the matrix \(\hat{V}\) is constructed by estimating the covariance function of the stochastic process β(τ): \(\hat{V}=\left(\begin{array}{ll}\hat{V}(\tau ,\tau )&\hat{V}(\tau ,\tau {\prime} )\\ \hat{V}(\tau {\prime} ,\tau )&\hat{V}(\tau {\prime} ,\tau {\prime} )\end{array}\right)\).
Nonparametric methods construct a hull of observations (Charnes et al. 1978) and hence consider the observations on the constructed frontier as fully efficient, do not account for measurement error, are sensitive to outliers and require large samples estimations. An alternative parametric method, that of stochastic frontier analysis, imposes distributional or other restrictions on the error term (Aigner et al. 1977). See the debate in the Journal of Health Economics 1994:13(3).
Japanese per diem variant of the prospective payment system, based on diagnosis-procedure combinations, DPCs.
We focus on a group of hospitals, which may comprise the whole sample or a certain category of hospitals in terms of the number of beds: small, medium-sized, and large.
This residual is the log of total factor productivity.
The boundary condition in the cost minimization problem is essentially the equation for the production function and it ensures the production of a given amount of output. It should be noted that the estimated log of the translog production function is not globally quasiconvex, so the optimum allocation of inputs in the cost minimization problem with translog production function does not exist (Boisvert 1982). Accordingly, the approximation of the translog production function is employed in the cost minimization problem: we use the Cobb–Douglas production function which has the returns to each input equal to the mean factor returns estimated under the translog model.
The prefecture grants the status of designated hospital and financial support of 10,000 yen per each admission to a local hospital that satisfies the following requirements: (1) has over 200 beds; (2) the share of patients referred from other facilities is over 60–80%; (3) shares its beds and expensive equipment (e.g., MRI and CT scanner) with other hospitals; (4) trains local healthcare officials; and (5) has emergency status.
The standard financial need is the product of unit cost of public services, the demand for public services and adjustment coefficient (which accounts for socio-economic and geographic factors), see https://www.soumu.go.jp/main_content/000363663.pdf.
The number of hospitals is steadily decreasing since 2003 owing to merging of municipalities and restructuring of hospitals.
Commonly, hospitalization in Japan lasts no less than a week, so shorter hospital stays may reflect only preliminary diagnostics or an anticipated transfer to specialized hospital facility (Nawata et al. 2006).
Hospital stays corresponding to long-term care.
We choose 0.1 as the minimal bound for bed occupancy in order for a hospital to be considered as providing inpatient care. Mean bed occupancy in our sample is 0.75.
Takatsuka and Nishimura (2008) propose reconstructing the arithmetic mean of the number of admissions and discharges using the MHLW definitions of average length of stay (available for acute-care beds only) and bed occupancy.
Our data show that pairwise correlation coefficients between the logarithms of the numbers of physicians, nurses and other staff—after subtraction of hospital means from each variable as we deal with panel-data fixed effects regression—are in a range of 0.33–0.48 in various years.
According to Ikegami and Buchan (2014), there are certain differences in requirements for qualifying as a registered nurse or a licensed practical nurse (3 years of medical education and a national exam versus 2 years of education and a prefectural exam), but the skills of the two types are very similar overall.
This composite group of all non-doctor and non-nurse labor specialties is used in the analysis owing to the size of our sample and the total count of estimated parameters: the inclusion of technicians, administrative personnel and other workers as separate inputs would considerably increase the number of covariates due to the appearance of numerous interaction terms.
The cost of medicines per se constitutes about 70% of all medical materials at local public hospitals, and the correlation between cost of medicines and cost of all medical materials is 0.96.
Although there is a slight fall in 2003.
See Supplementary material: productivity of physicians (Supplementary Tables S26 and S27), other staff (Supplementary Tables S32 and S33), capital (Supplementary Tables S38 and S39), medicines (Supplementary Tables S41 and S42). We use the criterion that the differences across the values in adjacent years were observed at least 7 pairs of years out of 19. This way the differences across annual values cannot be attributed to random variation.
The only exception is one value of the highest output quantile for two input pairs: total labor and physical capital; and physical capital and medicines.
Observed in all output quantiles with the exception of τ = 0.8
The choice of only three groups is justified by the desire to have a sufficient number of observations in each group and to make the size of groups comparable in terms of number of hospitals.
Additionally, Becker and Murphy (1994) state that the extent of labor specialization is explained by the balance between higher productivity (owing to the division of labor) and increased costs of labor coordination.
References
Acemoglu D, Autor D (2011) Skills, tasks and technologies: implications for employment and earnings. In Card D, Ashenfelter O (eds.) Handbook of labor economics, vol 4, Part B. Elsevier, Amsterdam, p 1043–1171
Acemoglu D, Finkelstein A (2008) Input and technology choices in regulated industries: Evidence from the health care sector. J Political Econ 116:837–880
Aigner D, Lovell C, Schmidt P (1977) Formulation and estimation of stochastic frontier production function models. J Econom 6:21–37
Baumgardner JR (1988) The division of labor, local markets, and worker organization. J Political Econ 96:509–527
Baumgardner JR (1988) Physicians’ services and the division of labor across local markets. J Political Econ 96:948–982
Becker GS, Murphy KM (1994) The division of labor, coordination costs, and knowledge. In Becker GS (ed.) Human capital: a theoretical and empirical analysis with special reference to education, 3rd ed. The University of Chicago Press, p 299–322
Bernini C, Freo M, Gardini A (2004) Quantile estimation of production function. Empir Econ 29:373–381
Besstremyannaya G (2013) The impact of Japanese hospital financing reform on hospital efficiency. Jpn Econ Rev 64:337–362
Besstremyannaya G, Golovan S (2019) Reconsideration of a simple approach to quantile regression for panel data. Econom J 22:292–308
Biørn E, Hagen TP, Iversen T, Magnussen J (2003) The effect of activity-based financing on hospital efficiency: A panel data analysis of DEA efficiency scores 1992–2000. Health Care Manag Sci 6:271–283
Blank JLT, Valdmanis VG (2008) Evaluating hospital policy and performance: Contributions from hospital policy and productivity research, Amsterdam: Elsevier JA
Blank JLT, Valdmanis VG (2010) Environmental factors and productivity of Dutch hospitals: A semi-parametric approach. Health Care Manag Sci 13:27–34
Blank JLT, van Hulst BL (2017) Balancing the health workforce: Breaking down overall technical change into factor technical change for labour: An empirical application to the Dutch hospital industry. Hum Resour Health 15:1–14
Bloom N et al. (2017) What drives differences in management? Working Paper, National Bureau of Economic Research
Bloom N et al. (2019) What drives differences in management practices? Am Econ Rev 109:1648–83
Bloom N, Dorgan S, Dowdy J, Van Reenen J (2007) Management practice and productivity: Why they matter. Working Paper, McKinsey&Company, LSE. https://cep.lse.ac.uk/management/Management_Practice_and_Productivity.pdf
Bloom N, Propper C, Seiler S, Van Reenen J (2015) The impact of competition on management quality: Evidence from public hospitals. Rev Econ Stud 82:457–489
Bloom N, Sadun R, Van Reenen J (2014) Does management matter in healthcare? In Chandra A, Cutler D, Huckman R, Martinez E (eds) Hospital organization and productivity. NBER Conference. https://prod-edxapp.edx-cdn.org/assets/courseware/v1/dd428dcc44daa742d5c5c91aeb9dcd21/c4x/HarvardX/PH555x/asset/Management_Healthcare_June2014.pdf
Bofinger E (1975) Optimal condensation of distributions and optimal spacing of order statistics. J Am Stat Assoc 70:151–154
Boisvert RN (1982) The translog production function: Its properties, its several interpretations and estimation problems. Working Paper, Charles H. Dyson School of Applied Economics and Management, Cornell University
Campbell J, Ikegami N (1998) The art of balance in health policy. Maintaining Japan’s low-cost, egalitarian system. Cambridge University Press, Cambridge
Canay I (2011) A simple approach to quantile regression for panel data. Econom J 14:368–386
Charnes A, Cooper W, Rhodes E (1978) Measuring the efficiency of decision making units. Eur J Oper Res 2:429–444
Chen L, Huo Y (2020) A simple estimator for quantile panel data models using smoothed quantile regressions. Econom J 24:247–263
Chernozhukov V (2005) Extremal quantile regression. Ann Stat 33:806–839
Chiang AC (1984) Fundamental methods of mathematical economics. McGraw-Hill
Christensen EW (2004) Scale and scope economies in nursing homes: A quantile regression approach. Health Econ 13:363–377
Cleverley WO, Harvey RK (1992) Competitive strategy for successful hospital management. J Healthc Manag 37:53
Coelli T, Perelman S (1999) A comparison of parametric and non-parametric distance functions: With application to European railways. Eur J Oper Res 117:326–339
Coelli T, Perelman S (2000) Technical efficiency of European railways: A distance function approach. Appl Econ 32:1967–1976
Dhaene G, Jochmans K (2015) Split-panel jackknife estimation of fixed-effect models. Rev Econ Stud 82:991–1030
Doi S, Ryubori M, Umetsuna K, Hayashi S (2005) DPC dounyu-ga oyobosu kyuuseikibyouin-no eikyou-to kongo-no kadai [The impact of DPC introduction on emergency hospitals and future issues. in Japanese]. Nihon Byouin Gakkaishi 52:72–79
Dorgan S et al. (2010) Management in healthcare: Why good practice really matters. Working Paper, McKinsey&Company, LSE. https://cep.lse.ac.uk/textonly/_new/research/productivity/management/PDF/Management_in_Healthcare_Report.pdf
Feldstein M (1974) Econometric studies of health economics., in Frontiers of Quantitative Econometrics, vol. 2, eds. Intriligator M, Kendrick D, Amsteram: North-Holland, 377–434
Ferrier GD, Valdmanis V (1996) Rural hospital performance and its correlates. J Product Anal 7:63–80
Fujii A (2001) Stochastic cost frontier and cost inefficiency of Japanese hospitals: A panel data analysis. Appl Econ Lett 8:801–812
Galvao AF, Kato K (2016) Smoothed quantile regression for panel data. J Econom 193:92–112
Hames DS (1991) Productivity-enhancing work innovations: Remedies for what ails hospitals? J Healthc Manag 36:545
Harding M, Lamarche C (2014) Estimating and testing a quantile regression model with interactive effects. J Econom 178:101–113
Harding M, Lamarche C (2016) Penalized quantile regression with semiparametric correlated effects: An application with heterogeneous preferences. J Appl Econ 32:342–358
Hendricks W, Koenker R (1992) Hierarchical spline models for conditional quantiles and the demand for electricity. J Am Stat Assoc 87:58–68
Higuchi S (2010) Chuusho jichitai byouin-no genjo-to kadai (current situation and tasks for small and medium local public hospitals). J Jpn Hosp Assoc 5:95–101
Hisamichi S (2010) Byouin keiei koto hajime. Byouin jigyou kanri-no tachiba kara. (Starting hospital management. Point of view of a hospital manager). J Jpn Hosp Assoc 2:98–119
Hollingsworth B (2008) The measurement of efficiency and productivity of health care delivery. Health Econ 17:1107–1128
Hollinsworth B, Peacock S (2008) Efficiency measurement in health and health care. Routledge
Hsu A, Dass AR, Berta W, Coyte P, Laporte A (2017) Efficiency estimation with panel quantile regression: An application using longitudinal data from nursing homes in Ontario, Canada. Working Paper No. 170003. Canadian Centre for Health Economics
Ikegami N (ed.) (2014) Universal health coverage for inclusive and sustainable development: Lessons from Japan. The World Bank
Ikegami N, Buchan J (2014) Licensed practical nurses: One option for expanding the nurses workforce in Japan. In Ikegami N (ed.) Universal health coverage for inclusive and sustainable development: Lessons from Japan. The World Bank, p 133–148
Ikegami N, Campbell JC (1999) Health care reform in Japan: The virtues of muddling through. Health Aff 18:56–75
Ikegami N et al. (2011) Japanese universal health coverage: Evolution, achievements, and challenges. Lancet 378:1106–1115
Iwane T (1976) Wa-ga kuni-no kouritsu byouin-ni tsuite. Byouin koudou-no riron-to jisshotekikenkyu (on the public hospitals in Japan: a behavior model of hospitals and some empirical studies). Osaka Economic Papers. p 35–54
Jacobs R, Smith P, Street A (2006) Measuring efficiency in health care. Analytic techniques and health policy. Cambridge University Press
Jensen GA, Morrisey MA (1986) Medical staff specialty mix and hospital production. J Health Econ 5:253–276
Kanagawa Y (2008) Chiikiiryouwo Mamoru. Jichitaibyouin Keiei Bunseki. (Defending Local Health Care. Management Analysis of Local Public Hospitals). Jichitai kenkyusha, Tokyo
Kaneko K, Onozuka D, Shibuta H, Hagihara A (2018) Impact of electronic medical records (EMRs) on hospital productivity in Japan. Int J Med Inform 118:36–43
Kato K, Galvao Jr AF, Montes-Rojas GV (2012) Asymptotics for panel quantile regression models with individual effects. J Econom 170:76–91
Kawabuchi K, Kajitani K (2003) Time of changes–health care reform in Japan. Jpn Hosp 22:11–18
Kawaguchi H, Tone K, Tsutsui M (2014) Estimation of the efficiency of Japanese hospitals using a dynamic and network data envelopment analysis model. Health Care Manag Sci 17:101–112
Kawaguchi K (2008) Iryo-no Koritsusei Sokutei. Keisoushobou [Estimating Healthcare Efficiency, in Japanese]. Keisoshobo Publishing House, Tokyo
Knox K, Blankmeyer E, Stutzman J (2007) Technical efficiency in Texas nursing facilities: A stochastic production frontier approach. J Econ Finance 31:75–86
Kodera T, Yoneda K (2019) Efficiency and the quality of management and care: Evidence from Japanese public hospitals. App Econ Lett 26:1418–1423
Koenker R (2004) Quantile regression for longitudinal data. J Multivar Anal 91:74–89
Koenker R (2005) Quantile regression. Cambridge University Press
Koenker R, Bassett G (1978) Regression quantiles. Econometrica 46:33–50
Koenker R, Machado JA (1999) Goodness of fit and related inference processes for quantile regression. J Am Stat Assoc 94:1296–1310
Kumazawa M (2010) Kouei-kara minei-he. Ayumi-no shokai. (From public to private management. Description of the change). J Jpn Hosp Assoc 5:88–95
Lee J, McCullough JS, Town RJ (2013) The impact of health information technology on hospital productivity. RAND J Econ 44:545–568
Li H, Lindsay BG, Waterman RP (2003) Efficiency of projected score methods in rectangular array asymptotics. J R Stat Soc Series B (Stat Methodol) 65:191–208
Liu C, Laporte A, Ferguson BS (2008) The quantile regression approach to efficiency measurement: Insights from Monte Carlo simulations. Health Econ 17:1073–1087
Liu J, Tone K (2008) A multistage method to measure efficiency and its application to Japanese banking industry. Socio-Econ Plan Sci 42:75–91
Machado JAF, Santos Silva JMC (2019) Quantiles via moments. J Econom 213:145–173
Mandai N, Watanabe M (2019) Relationship between current account balance ratio and salary ratio in Japanese municipal hospitals. Health 11:1591–1597
Martin C, Jérôme T (2016) Cost (in) efficiency and institutional pressures in nursing home chains. Eur Account Rev 25:687–718
Mas-Colell A, Whinston MD, Green JR (1995) Microeconomic theory. Oxford University Press
Ministry of Health, Labor and Welfare (2012) Heisei 24nendo sinryouhoushuu kaitei-niokeru DPC seido (DPC/PDPS)-no taiyou-nitsuite (gaiyou) (An outline of DPC/PDPS system within the 2012 revision of fee schedule, Mar 28). http://www.mhlw.go.jp/stf/shingi/2r98520000025zci-att/2r98520000025zn7.pdf
Ministry of Internal Affairs and Communications (2007) Kouritsubyouin kaikaku gaidorain [Guidelines for the reform of local public hospitals, in Japanese]. https://www.soumu.go.jp/main_sosiki/c-zaisei/hospital/guidline.html
Ministry of Internal Affairs and Communications (2015) Shinkouritsubyouin kaikaku gaidorain [New guidelines for the reform of local public hospitals, in Japanese]. https://www.soumu.go.jp/main_sosiki/c-zaisei/hospital/guidline.html
Morikawa M (2010) Economies of scale and hospital productivity: An empirical analysis of medical area level panel data. RIETI Discussion Paper Series 10-E-050. The Research Institute of Economy, Trade and Industry
Motohashi H (2009) Productivity of medical services: TFP (total factor productivity) and DEA (data envelopment analysis) of Japanese hospitals. ESRI Discussion Paper Series 210, Economic and Social Research Institute Cabinet Office
Nabemi K (2010) Seimei kagayakasou nihon-no byouincho. (Head of Japanese hospital, which lights up the life). J Jpn Hosp Assoc 1:29–38
Nawata K, Nitta A, Watanabe S, Kawabuchi K (2006) An analysis of the length of stay and effectiveness of treatment for hip fracture patients in japan: Evaluation of the 2002 revision of the medical service fee schedule. J Health Econ 25:722–739
Otto AK (1996) Management style, decision processes, and hospital effectiveness. PhD thesis. Kent State University
Panzar JC, Willig RD (1977) Economies of scale in multi-output production. Q J Econ 91:481–493
Pauly M (1980) Doctors and their workshops: Economic models of physician behavior. University of Chicago Press, A National Bureau of Economic Research Monograph
Rosko M, Mutter R (2008) Stochastic frontier analysis of hospital inefficiency. A review of empirical issues and an assessment of robustness. Med Care Res Rev 65:131–166
Rosko MD (1999) Impact of internal and external environmental pressures on hospital inefficiency. Health Care Manag Sci 2:63–74
Rosko MD (2004) Performance of us teaching hospitals: a panel analysis of cost inefficiency. Health Care Manag Sci 7:7–16
Saito J (2007) DPC-to kyuuseiki byouin-no iryou (DPC and health care at acute hospitals). J Jpn Hosp Assoc 4:12–26
Shima Y et al. (2006) DPCdounyugo-no shinryouhouyshuu seikyuu-no genjou-to mondaiten [Current situation and issues with the fee schedule claims after the introduction of DPCs, in Japanese]. Nihon Byouin Gakkaishi 53:67–71
Stigler GJ (1951) The division of labor is limited by the extent of the market. J Political Econ 59:185–193
Suwabe A (2004) Our efforts on DPC in Iwate Medical University hospital. Rinsho Byouri 52:1011–1014
Takatsuka N, Nishimura S (2008) Oderingu shistemu ga byoinseisansei, kouristusei nioyobosu eikyono hyouka. (Effect of order entry system on hospital productivity and efficiency for inpatient care in Japan). Jpn J Health Econ Policy 20:15–33
Tersigni AR (1992) The effect of leadership styles on hospital labor productivity. PhD thesis. Western Michigan University
Thurston NK, Libby AM (2002) A production function for physician services revisited. Rev Econ Stat 84:184–191
Tomioka T, Mano T, Yamada Y (2008) Medico-economic evaluation on efficient management of large acute care hospitals [in Japanese]. Nihon Iryou Byouin Kanri Gakkaishi 45:55–63
Tsionas EG (2002) Stochastic frontier models with random coefficients. J Appl Econ 17:127–147
Vita MG (1990) Exploring hospital production relationships with flexible functional forms. J Health Econ 9:1–21
Wang H, He X (2007) Detecting differential expressions in GeneChip microarray studies: A quantile approach. J Am Stat Assoc 102:104–112
Weisbrod BA (1992) Productivity and incentives in the medical care sector. Scand J Econ 94:S131–S145
Wooldridge J (2007) Quantile methods. NBER Summer Institute, Lecture Notes 14. http://www.nber.org/WNE/lect_14_quantile.pdf
Worthington A (2004) Frontier efficiency measurement in healthcare: A review of empirical techniques and selected applications. Med Care Res Rev 61:135–170
Yamada T, Yamada T, Kim C, Noguchi H (1997) Efficiency and costs in hospitals: A stochastic frontier approach. Discussion Paper 748. University of Tsukuba, Institute of Policy and Planning Sciences
Zhang X, Tone K, Lu Y (2018) Impact of the local public hospital reform on the efficiency of medium-sized hospitals in Japan: An improved slacks-based measure data envelopment analysis approach. Health Serv Res 53:896–918
Acknowledgements
The paper originated from the PhD dissertation in Economics, defended by the corresponded author at Keio University, Tokyo. Access to the Annual Surveys of Local Public Enterprises (fiscal years 1999–2001) was granted to the corresponding author by Keio University Library in 2008–2010.
Funding
The paper was prepared in the framework of the Basic Research Program of the National Research University HSE.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study design, data collection, data analysis and writing the earlier versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Appendix
Appendix
1.1 Data sources
Figures 4 and 5 and Tables A.1, A.2 and A.3
1.2 Results of the estimation
Tables B.1, B.2, B.3, B.4, B.5, B.6, B.7, B.8 and B.9
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Besstremyannaya, G., Golovan, S. Measuring heterogeneity in hospital productivity: a quantile regression approach. J Prod Anal 59, 15–43 (2023). https://doi.org/10.1007/s11123-022-00650-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11123-022-00650-3