Abstract
Background
Ectopic ACTH-secreting pituitary adenoma (EAPA) are a rare cause of Cushing’s disease. Due to the lack of consensus and experience in terms of the diagnosis and treatment of EAPAs, preoperative identification and optimal treatment remain challenging.
Purpose
To investigate the characteristics of EAPAs and offer some proposals for the diagnosis and management of this uncommon disease, the EAPA patients admitted to our center and all of the EAPA cases reported in the literature were reviewed.
Methods
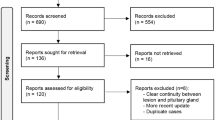
In a retrospective electronic medical chart review, 6 patients (0.39%) with EAPAs were identified from 1536 consecutive patients who were admitted to our hospital with a diagnosis of Cushing’s syndrome between January 2000 and August 2019. A literature review was performed on the online databases PubMed and EMBASE, and 52 cases conformed to the criteria. The data regarding biochemical tests, imaging examinations and follow-ups were analyzed.
Results
The mean age of patients with EAPAs was 37.7 years old, and an obvious female predominance (3.5: 1) was demonstrated. The most common location of EAPAs was the cavernous sinus (34.5%), followed by the sphenoid sinus (31.0%) and the suprasellar region (20.7%). No significant differences in the biochemical test results were found among tumors in different locations. Except for sex, no risk factors related to remission were found. Although no significant differences among different locations were found, the tumors in the cavernous sinus had a relatively higher rate of invisibility in terms of imaging and a higher non-remission rate than tumors in other locations.
Conclusions
In patients with negative intrasellar findings, the uncommon disease of EAPA should be considered. Due to the endocrine similarity between intrasellar pituitary corticotrophin adenoma and EAPA, the preoperative identification of EAPA depends on a careful review of the imaging examinations. Locations such as the cavernous sinus, sphenoid sinus and suprasellar region should be considered first. Tumor resection is recommended when the diagnosis is confirmed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cushing’s syndrome is caused by chronic exposure to excess glucocorticoids. Endogenous Cushing’s syndrome can be classified into adrenocorticotrophic hormone (ACTH)-dependent and ACTH-independent causes [1]. ACTH-dependent Cushing’s syndrome, accounting for approximately 80% of the total causes, includes excess secretion of adrenocorticotrophic hormone (ACTH) from a pituitary tumor (Cushing’s disease, CD) or an ectopic ACTH-producing tumor (ectopic ACTH syndrome) [1, 2]. In addition, there are some cases of ectopic ACTH-secreting pituitary adenomas (EAPAs), which are a rare cause of CD [3, 4].
Cushing’s syndrome is associated with increased mortality and results in poor prognosis, especially for non-remission cases of Cushing’s syndrome, which can lead to a 50% mortality rate at 5 years [2] and impaired health-related quality of life [1, 2, 5]. As a result, it is crucial to make specific diagnosis as early as possible. Rapid and effective treatment is also important for reducing long-term morbidity and mortality.
However, for Cushing’s syndrome, the high prevalence of unspecific manifestations such as obesity, hypertension, diabetes, and osteoporosis in the general population often makes it very difficult to identify, and there is always a considerable delay in diagnosis after the onset of symptoms [5, 6]. Compared to the difficult identification of Cushing’s syndrome, localization diagnosis can be much more difficult, especially for identifying a patient with EAPA. There are no specific endocrinological tests for diagnosing EAPAs, and the unspecific or negative results of MRI makes a precise diagnosis much more difficult [7].
Because of the high possibility of misdiagnosis of EAPAs, pituitary exploration always yields negative results, and initial treatments such as bilateral adrenalectomy or total hypophysectomy will lead to poor outcomes, such as Nelson syndrome or irreversible hypopituitarism [8,9,10,11]. Therefore, it is crucial to distinguish this rare disease from Cushing’s disease and to choose an appropriate initial treatment.
No more than sixty cases of EAPAs have been reported so far, so there is still a lack of data and experience for making a consensus in terms of the management of EAPAs. We present 6 patients who were diagnosed with EAPAs in our center, one of the largest pituitary centers in China, and we review all 58 reported patients (including the 6 patients from our center). This study aimed to describe the characteristics of EAPAs and sought to raise some opinions and advice about the diagnosis and treatment of EAPAs.
Methods
Diagnostic method for Cushing’s syndrome
The preoperative diagnosis of Cushing’s syndrome in our hospital was established on the basis of clinical manifestations as well as endocrine and radiological findings as follows: (1) the clinical manifestations of Cushing’s syndrome include weight gain, fat redistribution, facial rounding, plethora, and comorbidities such as diabetes mellitus, hypertension, and osteoporosis; (2) the biochemical results associated with hypercortisolism include elevated serum midnight cortisol, 24 h urine free cortisol (UFC) and the unsuppressed low-dose dexamethasone suppression test (DST), which are important for confirming the diagnosis of Cushing’s syndrome, and the endocrine tests for differential diagnosis include ACTH and high-dose DST; (3) the radiological examinations include dynamic enhanced pituitary magnetic resonance imaging (MRI), computed tomography (CT) of the bilateral adrenal glands, inferior petrosal sinus sampling (IPSS) and octreotide imaging, which are helpful for differential diagnosis [1, 12].
For patients who were suspected to have Cushing’s syndrome in our center, all or a portion of these tests or examinations were performed to make the most possible preoperative diagnosis. Most patients without absolute contraindications received surgery, and a confirmed final diagnosis was made based on the postoperative histopathological examination and postoperative follow-up.
Patient collection
We retrospectively reviewed patients in Peking Union Medical College Hospital using the electronic medical record of hospital information system.
The inclusion criteria were as follows: (1) patients were identified as ACTH-dependent Cushing’s syndrome by clinical manifestations, unsuppressed low-dose DST and normal or increased ACTH levels; (2) the imaging examinations showed an sella lesion without connection to the pituitary gland; and (3) the diagnosis of EAPA was confirmed by pathological examination after surgery.
The exclusion criteria included the following: (1) patients with lesions of the pituitary gland; (2) ectopic ACTH syndrome confirmed by imaging examination or octreotide imaging; and (3) lesions diagnosed as other diseases rather than pituitary adenomas by histological examination.
Of 1536 patients admitted to our hospital because of Cushing’s syndrome between January 2000 and August 2019, 7 patients were identified with EAPAs, but one was excluded because an intrasellar pituitary lesion was found. Finally, data from 6 patients (0.39%) were collected, which included clinical manifestation, biochemical, imaging, treatment and follow-up data.
Literature review
Since EAPA is a rare disease, a literature review was performed to find all published cases of EAPAs. The online databases PubMed and EMBASE were searched on August 16, 2019, for all articles containing the words “ectopic pituitary adenomas”; this search returned 1208 and 381 results, respectively, from all time periods. Articles were excluded if (1) the articles were reviews without new cases, (2) the cases were not ACTH-secreting pituitary adenomas, (3) the diagnosis was not histologically confirmed, (4) the location of the adenomas was not explicit or (5) cases were reported in non-English languages.
Data analysis
Pearson χ2 test, continuity correction χ2 test, or Fisher’s exact test was used to evaluate the statistical significance with a 2 × 2 table. The significant difference of R × C cross tables was assessed by Wilcoxon rank test, Kruskal–Wallis test, or Spearman rank correlation. The data were analyzed using GraphPad Prism 7 (GraphPad Software, La Jolla, California, USA).
Results
The presentation of six cases of EAPA
Six patients with ectopic ACTH-secreting pituitary adenomas in our hospital were identified with EAPA; four of them were females, and the other two were males (F/M ratio 4: 2). All of them presented with typical manifestations of Cushing’s syndrome, including weight gain, central obesity, supraclavicular fatty pads, a round face and facial plethora, etc. The interval between the onset of symptoms and diagnosis ranged from 2 to 7 years. A routine workup and an endocrinological evaluation were performed for each patient. The main test results are shown in Table 1.
All six patients showed impaired rhythms of cortisol secretion, elevated plasma ACTH levels (normal range 0–46 pg/ml) and increased 24 h UFC levels (normal range 12.3–103.5 µg/24 h). Low-dose DST demonstrated no suppression in all six patients, which indicated a confirmed diagnosis of Cushing’s syndrome. Five of these patients showed suppressed results during high-dose DST, but the other one (case 2) showed no suppression with high-dose DST.
Negative findings of tumors on adrenal CT scans for these six patients helped to exclude adrenal adenomas. Octreotide imaging was performed in all patients to ensure that there were no ectopic neuroendocrine tumors that could secrete ACTH. Finally, all patients received pituitary dynamic-enhanced MRI (Fig. 1a–f), but only one (case 3) showed a false positive result suggestive of an intrasellar mass. The adenomas were located in the suprasellar region in four patients (cases 1–4) and in the cavernous sinus in the other two patients (cases 5 and 6). Thus, MRI succeeded in initially indicating the correct locations for five patients (83.3%).
There were four patients (cases 2–5) who received IPSS, and three of them (cases 2–4) had positive central: peripheral results (C: P > 2), which indicated pituitary tumors. One patient (case 5) had a C: P ratio less than 2: 1 (1.2: 1), and an arteriovenous malformation was found, which could influence the results of IPSS.
The tumors were finally removed with transsphenoidal surgery (cases 2, 5, and 6) or craniotomy (cases 1, 3, and 4), and the diagnosis of EAPA was confirmed via postoperative pathological examination. Interestingly, case 3 underwent endoscopic transsphenoidal pituitary exploration, but no lesion was found. Then, a repeated MRI (Fig. 1c) showed pituitary stalk thickening, and a craniotomy was carried out for removing the tumor successfully. Additionally, case 6 also experienced intrasellar surgery failure, and the lesion in the left cavernous sinus was not resected completely (Fig. 1f); however, radiotherapy was performed, which were successful for shrinking the tumor.
Cases 2 and 3 experienced long-term remission (serum morning cortisol < 5 µg/dl) after two surgeries, and case 4 maintained partial remission (serum morning cortisol 5–10 µg/dl) after craniotomy during the 2-month follow-up. Three patients received radiotherapy after surgery because of incomplete remission or residual tumors; one of them experienced partial remission (case 1), but the other two underwent bilateral adrenalectomy (case 5) and medical therapy (case 6).
Coronal contrast-enhanced MRI of cases 1 (a), 2 (b) and 3 (c) and 4 (d) showing the suprasellar mass (arrows). Case 3 underwent MRI after failed pituitary exploration, and the MRI shows pituitary stalk thickening (c). The MRI of cases 5 (e) and 6 (f) showing lesions (arrows) in the cavernous sinus, in which f shows a picture after a failed pituitary surgery
Literature review
Demographics
A total of 54 out of 58 patients with a confirmed diagnosis of EAPA were analyzed because the individual information of 4 patients was not available in the literature [13]. Of 54 patients, 42 (77.8%) were females, and 12 (22.2%) were males. The age ranged from 11 to 76 years, the mean age was 38 years, and the median age was 37.5 years, based on the available data (Fig. 2). The mean age of females was 37 years and that of males was 40 years.
Characteristics of EAPAs in different locations
Data were available for the tumor locations of all 58 patients. The most frequent location for EAPAs was the cavernous sinus (20 cases, 34.5%) [3, 7, 10, 13,14,15,16,17,18,19], followed by the sphenoid sinus (18 cases, 31.0%) [4, 7, 9, 10, 20,21,22,23,24,25,26,27,28,29,30,31,32,33] and the suprasellar region (12 cases, 20.7%) [8, 11, 34,35,36,37]. Locations such as the interpeduncular cistern [38], superior orbital fissure [39], clivus [39], nasal cavity [40, 41], ethmoid sinus [7, 40], maxillary sinus [40, 42], and parasellar region (not in the cavernous sinus) [10, 43] have also been reported. Patients were mainly reported from North America, Europe and East Asia (Japan, South Korea and China), probably because only literature in English was included. The tumor location and regional distribution information for all reported cases is shown in Fig. 3.
Patients with the most frequent locations, including the cavernous sinus, sphenoid sinus and suprasellar region, were analyzed to compare their clinical features (Table 2). Sex information was available for all patients whose adenomas were located in the sphenoid sinus and suprasellar region, but 90.0% (18/20) of cases were located in the cavernous sinus. No statistically significant sex difference was found among the three locations.
The positive rates of the imaging findings of adenomas in the sphenoid sinus, cavernous sinus and suprasellar region were 72.2% (13/18), 35.0% (7/20), 91.7% (11/12), respectively, with statistically significant differences (p = 0.0032). There were no false positive imaging manifestations for adenomas located in the sphenoid sinus, but 3 (15.0%) manifestations were observed for the cavernous sinus, and 1 (8.3%) manifestation was observed for the suprasellar region.
The tumor size data were available for 26 patients, of whom 11 (42.3%) had macroadenomas (diameter < 1 cm) and 15 (57.7%) had microadenomas (diameter ≥ 1 cm). No significant differences were found among the different groups (p = 0.4270).
There were 37 patients whose data of low-dose DST were described, included our patients, but nonsuppressed results occurred only in one case [14]. High-dose DST results were available in 11 (61.1%), 16 (80%) and 7 (58.3%) patients whose tumors were located in the sphenoid sinus, cavernous sinus and suprasellar region, respectively. The results showed that high-dose DST was suppressed in 54.5% of patients in the sphenoid sinus group. The suppressed rate for the cavernous sinus group was 56.2% and for the suprasellar group was 71.4%. There was no statistically significant difference among these groups (p = 0.7460).
Data on IPSS detection were available in 24 (41.4%) patients for the three most common locations: 6 (33.3%) in the sphenoid sinus group, 14 (70.0%) in the cavernous sinus group and 4 (33.3%) in the suprasellar group. The number of patients whose ratio of central-to-peripheral ACTH gradient (C: P) was > 2 for the sphenoid sinus was 5 (83.3%), for the cavernous sinus was 11 (78.6%), and for the suprasellar region was 4 (100%). No significant difference was found among the groups (p = 0.5979). In total, 24 patients received the IPSS test, of whom 20 (83.3%) had a C: P ratio > 2. Notably, there were three patients [3, 14, 17] who received cavernous sinus sampling showing a C: P ratio > 2, in whom one patient [14] with a tumor in the cavernous sinus had a negative IPSS test.
Thirty (51.7%) patients underwent surgery. The patients with suprasellar tumors were much more likely to receive craniotomy (77.8%) (p = 0.0002) than patients in the other two groups.
The outcomes showed that the total remission rate was 68.4% (39/57). The remission rate was 94.1% (16/17) for patients whose tumors were located in the sphenoid sinus, 60.0% (9/15) for the cavernous sinus and 75.0% (9/12) for the suprasellar region. Although a relatively higher rate was observed in the sphenoid sinus group than in the other groups, no statistically significant differences were found among the different groups in terms of the remission rates (p = 0.0696).
Risk factors
Sex, negative image detection rate, tumor size, high-dose DST and IPSS results, surgical approach and tumor location were used to analyze the risk factors associated with outcomes. Sex differences were associated with EAPA prognosis, and the available data showed that male patients predicted a higher rate (100.0%) of remission than female patients (68.4%). Although there was no significant difference among the groups of different locations, tumors in the cavernous sinus predicted a relatively lower remission rate (60.0%) than tumors in other locations. However, none of the other factors were significantly related to remission (Table 3). Multivariate logistic regression analysis was not performed because of the small sample size, and no obvious association factors were found.
Discussion
Pituitary adenomas represent the most common lesion that presents in the sellar area, and they account for 10–25% of intracranial tumors [12]; however, ectopic pituitary adenomas (EPAs) are an extremely rare entity [44, 45]. Generally, EPA is defined as adenoma located outside the sella turcica, and there is no connection with the normal intrasellar pituitary gland [46]. There have been several hypotheses regarding the origin and pathogenesis of EPAs, but the exact mechanism remains unclear [47]. One of the broadly accepted considerations is that ectopic adenomas originate from the neoplastic proliferation of embryonic pituitary residues along the path of migration of Rathke’s pouch [47, 48]. The anatomic distribution of EPAs has been reported, including the suprasellar region, sphenoid sinus, clivus, cavernous sinus, nasal cavity, superior orbital fissure, temporal lobe, third ventricle and so on [44, 49]. However, the most common locations of EPAs are the suprasellar region and sphenoid sinus, which together account for more than half of all EPAs, followed by the clivus and the cavernous sinus [49, 50]. There are various hormone-secreting types of EPAs. Based on the reported cases, ACTH-secreting adenomas are the most common, followed by prolactinomas, nonfunctioning pituitary adenomas and growth hormone-secreting adenomas [50].
As one of the largest endocrine and pituitary centers in China, in our hospital, a large number of patients with Cushing’s syndrome are admitted every year, but the composition of EAPAs is still extremely low, with only 6 cases identified in 19 years. In addition, only 58 cases could be found that met the inclusion criteria. Therefore, EAPA is an extremely rare disease. Although Cushing’s syndrome can be due to a variety of etiologies, ACTH-secreting pituitary adenomas (Cushing’s disease, CD) accounted for approximately 65–70% of cases [12]. The female-to-male ratio of CD is 3–8:1. However, as a rare source of CD, the demographic data of EAPAs also suggest a similar female predominance with a ratio of 3.5: 1 [51, 52]. Although patients with an age range of 11–76 years can be affected, the majority of patients are in their 3rd decade of life.
As the most common form of Cushing’s syndrome, CD continues to be a difficult challenge in terms of both the diagnosis and management [53]. Therefore, the identification and treatment of EAPAs are incredibly difficult because of the lack of experience and clinical evidence [2]. Due to the similarity of clinical symptoms, signs and laboratory tests to intrasellar pituitary corticotrophin adenomas, it is sometimes difficult to identify the source of EAPAs, especially when imaging demonstrates false positive results indicating an intrasellar lesion, which ultimately leads to unnecessary pituitary exploration [7, 41, 44].
Both EAPA and intrasellar pituitary corticotrophin adenoma patients can present with elevated 24 h UFC and blunting of the diurnal rhythm of cortisol secretion [7, 33, 54]. Additional biochemical testing and imaging examinations are essential to identify the cause after the establishment of a diagnosis of Cushing syndrome. High-dose DST has been widely used to distinguish CD from ectopic ACTH-producing neuroendocrine tumors [55]. We obtained high-dose DST results for a total of 38 patients with EAPAs, and 63.2% (24/38) showed suppression, which means that high-dose DST for EAPAs had similar values to those for intrasellar pituitary corticotrophin adenomas. However, the nonsuppression rate of 36.8% for EAPAs indicates that high-dose DST is not an ideal method for distinguishing EAPAs from ectopic tumors.
Bilateral inferior petrosal sinus sampling (IPSS) is considered to be the most accurate test for identifying of CD [56], especially when small sellar masses are difficult to detect from imaging tests [49]. In general, the presence of a central to peripheral ACTH gradient (2:1 or higher before CRH or desmopressin and 3:1 or higher after CRH or desmopressin) can predict a pituitary source for ACTH-dependent Cushing’s syndrome with high sensitivity (approximately 94%) and specificity [54, 57]. Although only limited data were collected before CRH or desmopressin, the occurrence rate for a C: P ratio > 2 in the EAPAs was 81.5% (22/27). The relatively lower positive rate of IPSS for EAPAs may be due to the incomplete data, as only a few patients underwent CRH or desmopressin tests. Therefore, the positive rate could have been higher if CRH or desmopressin tests had been performed in all patients. Additionally, the use of IPSS for EAPAs is the same as that for intrasellar pituitary corticotrophin adenomas, which also helps to distinguish EAPAs from ectopic neuroendocrine neoplasms. It is worth noting that there were three patients with intracavernous pituitary adenomas who presented with positive results from cavernous sinus sampling (CSS) [3, 14]. However, the study of Kathryn et al. [50] showed that CSS is as safe as IPSS for distinguishing patients with CD from those with ectopic ACTH syndrome. Thus, CSS is not adequate for identifying an intracavernous source of CD but can be a substitute for IPSS.
Given that the incidence of ectopic tumors from other anatomical sites is much higher than that of EAPAs, octreotide imaging or radiological examinations of the trunk are still important for detecting underlying tumors [58]. High-resolution pituitary MRI is essential for localizing a pituitary source for ACTH-dependent Cushing’s syndrome [49, 53]. However, only 60–70% of pituitary corticotrophin adenomas are detectable on MRI [54, 58], and the rate of identification depends on the experience of the radiologists or neurosurgeons to some extent. The rate of negative imaging examinations (including MRI and CT) for EAPAs was 58.9% (33/56). In contrast, the relatively low invisibility rate made it hard to pinpoint the source of excess ACTH initially. A total of 8.9% (5/56) of patients had false positive imaging manifestations suggestive of an intrasellar source, which led to the failed pituitary exploration. Therefore, the potential for EAPAs should be considered even with positive findings on pituitary MRI since false positive results may appear. However, the invisibility rates of the imaging findings varied with different locations, and EAPAs in the suprasellar region were much easier to identify; however, in the cavernous sinus, EAPAs were most difficult to identify, leading to neglect.
Due to the negative results of the correlation analysis between the tumor locations and the preoperative examinations (including DST and IPSS), a localization diagnosis without the use of MRI or PET/CT before surgery might be difficult. Thus, there are no specific biochemical tests or ideal tools to diagnose EAPAs, but imaging examinations are the key test for localizing the tumor. It is worth noting that there was a patient whose tumor was detected by PET/CT [40]. EAPAs are derived from pituitary tissue, which can express the somatostatin receptor (SSTR) and can be detected by Ga-68-DOTANOC-PET/CT [59]. Thus, PET/CT may be a potential diagnostic tool for the localization of an ectopic source of pituitary adenoma [7, 31, 40], but more studies should be carried out.
According to the published literature, the most common location for EAPAs is the sphenoid sinus [29], which is not consistent with what we found. The most common location in this study was the cavernous sinus, which may be due to the improvement in advanced technologies, especially imaging examinations, and the fact that more doctors are focusing on this rare disease. Although we sought to determine the difference between EAPA and intrasellar pituitary corticotrophin adenoma from this retrospective study, there was no ideal way to distinguish between them. Therefore, except for ectopic Cushing syndrome, EAPA should be considered when Cushing’s disease is suspected but when no lesion is found in the pituitary MRI.
The goals of treatment for Cushing’s disease include normalization of cortisol secretion, tumor resection, control of comorbidities and improvement of quality of life [60]. As a source of CD, for EAPAs, curative surgery should be the first choice of treatment, similar to the treatment principles for intrasellar pituitary corticotrophin adenomas [54, 60]. Furthermore, the second-line treatment is radiotherapy, followed by medical therapy and bilateral adrenalectomy, theoretically [54]. As the first-line therapy, transsphenoidal surgery (TSS) is an ideal way to reach up to 70–90% remission for patients with CD [61]. Several factors, including tumor size, location, preoperative tumor visualization and intra-operative tumor visualization, are considered to be associated with remission in CD [62, 63]. Although no significant factors were found to predict remission of EAPAs due to the limitations of sample size and incomplete data, the low invisibility rate in the imaging examinations for tumors in the cavernous sinus may be related to the low remission rate. Thus, it is believed that only an accurate diagnosis can lead to effective tumor resection, and unnecessary surgery, such as bilateral adrenalectomy and hypophysectomy, should be avoided [7]. Since lateral surgical extension towards the cavernous sinus is limited during microscopic transsphenoidal surgery [18], an endoscopic method is recommended, especially for tumors located in the cavernous sinus. Furthermore, a predominance for craniotomy was shown retrospectively for suprasellar masses, but a trans-tuberculum sella approach should be considered in this situation because it can provide a direct view of the supra-diaphragmatic space and can preserve the normal pituitary gland [64].
Given that the sample size was relatively small and that the follow-up periods were inconsistent, the real remission rate was difficult to evaluate. Although there was no statistically significant difference in remission among the tumors in different locations; the low rate of tumor visualization for the location of the cavernous sinus indicates great difficult for identifying and removing the tumor. In addition, the invasion of the internal carotid artery often leads to difficult cavernous exploration and failed surgery [18]. This hypothesis was verified by the outcome of a lower remission rate for cavernous adenomas, indicating the importance of the accurate diagnosis of EAPAs and their location.
There are several limitations in our study. Due to the retrospective nature, selection bias was unavoidable. Because of the limited data and information obtained from previous studies, the real results, including the preoperative diagnostic tests, imaging findings and outcomes, could not be accurately and comprehensively estimated. The small sample size and the susceptibility to publication bias may underestimate the incidence of EAPAs and even draw inaccurate results.
Conclusion
As one of causes of Cushing’s disease, EAPAs are a rare disease. Because of the biochemical similarity between EAPA and intrasellar pituitary corticotrophin adenoma, it is difficult to distinguish them by the use of common tests only, including IPSS. Given the severity of the disease, for patients with negative intrasellar findings, a careful review of imaging examinations should be considered due to the possibility of this uncommon situation. PET/CT may be a potential tool for pinpointing the lesion, but more studies should be carried out. Once the disease is highly suspected, tumor resection should be performed as the first choice of treatment by an experienced surgeon. For patients with residual tumors or recurrence, radiation or medical therapy should be considered as alternative treatments, especially when tumors are located in the cavernous sinus when complete resection is difficult, in order to achieve biochemical remission and decrease mortality.
Abbreviations
- ACTH:
-
Adrenocorticotrophic hormone
- EAPA:
-
Ectopic ACTH-secreting pituitary adenoma
- CD:
-
Cushing’s disease
- DST:
-
Dexamethasone suppression test
- MRI:
-
Magnetic resonance imaging
- CT:
-
Computed tomography
- IPSS:
-
Inferior petrosal sinus sampling
- UFC:
-
Urine free cortisol
- C:P:
-
The ratio of the central-to-peripheral ACTH gradient
- TSS:
-
Transsphenoidal surgery
- CSS:
-
Cavernous sinus sampling
References
Lacroix A et al (2015) Cushing's syndrome. Lancet 386(9996):913–927
Prague JK, May S, Whitelaw BC (2013) Cushing's syndrome. BMJ 346:f945
Wilson CB, Mindermann T, Tyrrell JB (1995) Extrasellar, intracavernous sinus adrenocorticotropin-releasing adenoma causing Cushing's disease. J Clin Endocrinol Metab 80(6):1774–1777
Johnston PC et al (2014) Ectopic ACTH-secreting pituitary adenomas within the sphenoid sinus. Endocrine 47(3):717–724
Pivonello R et al (2017) Cushing's disease: the burden of illness. Endocrine 56(1):10–18
Valassi E et al (2011) The European Registry on Cushing's syndrome: 2-year experience. Baseline demographic and clinical characteristics. Eur J Endocrinol 165(3):383–392
Knappe UJ et al (2017) Ectopic adrenocorticotropic hormone-secreting pituitary adenomas: an underestimated entity. Neurosurgery 80(4):525–533
Dyer EH et al (1994) Functioning ectopic supradiaphragmatic pituitary adenomas. Neurosurgery 34(3):529–532 (discussion 532)
Esteban F et al (1997) Ectopic pituitary adenoma in the sphenoid causing Nelson's syndrome. J Laryngol Otol 111(6):565–567
Pluta RM et al (1999) Extrapituitary parasellar microadenoma in Cushing's disease. J Clin Endocrinol Metab 84(8):2912–2923
Hou L et al (2002) Suprasellar adrenocorticotropic hormone-secreting ectopic pituitary adenoma: case report and literature review. Neurosurgery 50(3):618–625
Molitch ME (2017) Diagnosis and treatment of pituitary adenomas: a review. Jama 317(5):516–524
Ohnishi T et al (2000) Intracavernous sinus ectopic adrenocorticotropin-secreting tumours causing therapeutic failure in transsphenoidal surgery for Cushing's disease. Acta Neurochir (Wien) 142(8):855–864
Sanno N et al (1999) Ectopic corticotroph adenoma in the cavernous sinus: case report. Neurosurgery 45(4):914–917
Hamon M et al (2003) Case report: cushing disease caused by an ectopic intracavernous pituitary microadenoma: case report and review of the literature. J Comput Assist Tomogr 27(3):424–426
Kim LJ et al (2003) Ectopic intracavernous sinus adrenocorticotropic hormone-secreting microadenoma: could this be a common cause of failed transsphenoidal surgery in Cushing disease? Case report. J Neurosurg 98(6):1312–1317
Koizumi M et al (2011) Successful treatment of Cushing's disease caused by ectopic intracavernous microadenoma. Pituitary 14(3):295–298
Balasa AF et al (2017) Ectopic intracavernous corticotroph microadenoma: case report of an extremely rare pathology. Rom J Morphol Embryol 58(4):1447–1451
Koutourousiou M, Winstead WI (2017) Endoscopic endonasal surgery for remission of cushing disease caused by ectopic intracavernous macroadenoma: case report and literature review. World Neurosurg 98:870
Kammer H, George R (1981) Cushing's disease in a patient with an ectopic pituitary adenoma. Jama 246(23):2722–2724
Burch WM et al (1985) Cushing's disease caused by an ectopic pituitary adenoma within the sphenoid sinus. N Engl J Med 312(9):587–588
Lloyd RV et al (1986) Ectopic pituitary adenomas with normal anterior pituitary glands. Am J Surg Pathol 10(8):546–552
Schteingart DE et al (1987) Cushing's syndrome caused by an ectopic pituitary adenoma. Neurosurgery 21(2):223–227
Slonim SM et al (1993) MRI appearances of an ectopic pituitary adenoma: case report and review of the literature. Neuroradiology 35(7):546–548
Morita H et al (1994) Cushing’s syndrome caused by an ectopic pituitary adenoma of the sphenoid sinus.&nbsp;Adrenal crisis after partial resections of the adenoma. Endocr Pathol 5(2):123–130
Coire CI et al (1997) Cushing's syndrome from an ectopic pituitary adenoma with peliosis: a histological, immunohistochemical, and ultrastructural study and review of the literature. Endocr Pathol 8(1):65–74
Bethge H et al (1999) Cushing's syndrome due to an ectopic ACTH-secreting pituitary tumour mimicking occult paraneoplastic ectopic ACTH production. Clin Endocrinol (Oxf) 51(6):809–814
Al-Gahtany M et al (2003) Juxtaposition of an ectopic corticotroph adenoma of the sphenoid sinus with orthotopic intrasellar corticotroph hyperplasia in a patient with Cushing disease. Case report. J Neurosurg 98(4):891–896
Suzuki J et al (2004) An aberrant ACTH-producing ectopic pituitary adenoma in the sphenoid sinus. Endocr J 51(1):97–103
Zerikly RK et al (2009) Cyclic Cushing syndrome due to an ectopic pituitary adenoma. Nat Clin Pract Endocrinol Metab 5(3):174–179
Willhauck MJ et al (2012) An unusual case of ectopic ACTH syndrome. Exp Clin Endocrinol Diabetes 120(2):63–67
Flitsch J et al (2015) A pitfall in diagnosing Cushing's disease: ectopic ACTH-producing pituitary adenoma in the sphenoid sinus. Pituitary 18(2):279–282
Seltzer J et al (2015) Ectopic ACTH-secreting pituitary adenoma of the sphenoid sinus: case report of endoscopic endonasal resection and systematic review of the literature. Neurosurg Focus 38(2):E10
Matsumura A et al (1990) Suprasellar ectopic pituitary adenoma: case report and review of the literature. Neurosurgery 26(4):681–685
Tal A (1993) Cushing's disease caused by ectopic pituitary adenoma within the pituitary stalk. South Med J 86(2):249–250
Murakami N et al (1998) Supra- and extrasellar pituitary microadenoma as a cause of Cushing's disease. Endocr J 45(5):631–636
Jung S et al (2000) Supradiaphragmatic ectopic adrenocorticotropic hormone-secreting adenoma. Pathol Int 50(11):901–904
Takahata T et al (1995) Ectopic pituitary adenoma occurring in the interpeduncular cistern. Case report. J Neurosurg 83(6):1092–1094
H O-S, E.D.J (1975) Pituitary adenomas of adolescents. J Neurosurg 43(4):437–439
Veit JA et al (2013) Detection of paranasal ectopic adrenocorticotropic hormone-secreting pituitary adenoma by Ga-68-DOTANOC positron-emission tomography-computed tomography. Laryngoscope 123(5):1132–1135
Gurazada K et al (2014) Nasally located ectopic ACTH-secreting pituitary adenoma (EAPA) causing Nelson's syndrome: diagnostic challenges. Pituitary 17(5):423–429
Sindoni A et al (2018) Ectopic adrenocorticotropic hormone-secreting pituitary adenoma localized by 18F-Choline PET/CT. Clin Nucl Med 43(1):e25–e26
Bonner RA, Mukai K, Oppenheimer JH (1979) Two unusual variants of Nelson's syndrome. J Clin Endocrinol Metab 49(1):23–29
Zhou HJ et al (2017) 'Ectopic' suprasellar type IIa PRL-secreting pituitary adenoma. Pituitary 20(4):477–484
Thompson LD, Seethala RR, Muller S (2012) Ectopic sphenoid sinus pituitary adenoma (ESSPA) with normal anterior pituitary gland: a clinicopathologic and immunophenotypic study of 32 cases with a comprehensive review of the english literature. Head Neck Pathol 6(1):75–100
Ba T et al (2017) Ectopic pituitary adenomas presenting as sphenoid or clival lesions: case series and management recommendations. J Neurol Surg B 78(2):120–124
Wang Q et al (2016) Ectopic suprasellar thyrotropin-secreting pituitary adenoma: case report and literature review. World Neurosurg 95:617.e13–617.e18
Aegly A et al (2019) Ectopic pituitary adenomas: common presentations of a rare entity. Pituitary 22(4):339–343
Guerrero CA et al (2007) Ectopic suprasellar growth hormone-secreting pituitary adenoma: case report. Neurosurg 61(4):E879 (discussion E879)
Mitsuya K et al (2004) Ectopic growth hormone-releasing adenoma in the cavernous sinus–case report. Neurol Med Chir (Tokyo) 44(7):380–385
Boscaro M et al (2001) Cushing's syndrome. Lancet 357(9258):783–791
Newell-Price J et al (1998) The diagnosis and differential diagnosis of Cushing's syndrome and pseudo-Cushing's states. Endocr Rev 19(5):647–672
Kennedy L, Recinos PF (2017) Cushing disease: are we making progress? J Clin Endocrinol Metab 102(7):2133–2135
Tritos NA, Biller BM (2014) Cushing's disease. Handb Clin Neurol 124:221–234
Nieman LK et al (1986) The ovine corticotropin-releasing hormone stimulation test and the dexamethasone suppression test in the differential diagnosis of Cushing's syndrome. Ann Intern Med 105(6):862–867
Oldfield EH et al (1985) Preoperative lateralization of ACTH-secreting pituitary microadenomas by bilateral and simultaneous inferior petrosal venous sinus sampling. N Engl J Med 312(2):100–103
Bonelli FS et al (2000) Adrenocorticotropic hormone-dependent Cushing's syndrome: sensitivity and specificity of inferior petrosal sinus sampling. AJNR Am J Neuroradiol 21(4):690–696
Findling JW, Raff H (2006) Cushing's Syndrome: important issues in diagnosis and management. J Clin Endocrinol Metab 91(10):3746–3753
Kuyumcu S et al (2013) Physiological and tumoral uptake of (68)Ga-DOTATATE: standardized uptake values and challenges in interpretation. Ann Nucl Med 27(6):538–545
Biller BM et al (2008) Treatment of adrenocorticotropin-dependent Cushing's syndrome: a consensus statement. J Clin Endocrinol Metab 93(7):2454–2462
Swearingen B, Barker FG, and Zervas NT (1999) The management of pituitary adenomas: the MGH experience. Clin Neurosurg 45:48–56
Hammer GD et al (2004) Transsphenoidal microsurgery for Cushing's disease: initial outcome and long-term results. J Clin Endocrinol Metab 89(12):6348–6357
Rollin GA et al (2004) Dynamics of serum cortisol levels after transsphenoidal surgery in a cohort of patients with Cushing's disease. J Clin Endocrinol Metab 89(3):1131–1139
Kinoshita Y et al (2012) Supra-diaphragmatic pituitary adenoma removed through the trans-tuberculum sellae approach. Case report. Neurol Med Chir (Tokyo) 52(2):91–95
Funding
This study was funded by the CAMS Innovation Fund for Medical Science (CAMS-2016-I2M-1-002) and The National Key Research and Development Program of China (No. 2016YFC0901501).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhu, J., Lu, L., Yao, Y. et al. Long-term follow-up for ectopic ACTH-secreting pituitary adenoma in a single tertiary medical center and a literature review. Pituitary 23, 149–159 (2020). https://doi.org/10.1007/s11102-019-01017-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-019-01017-y