Abstract
Background
Children initially diagnosed with isolated GH deficiency (IGHD) have a variable rate to progress to combined pituitary hormone deficiency (CPHD) during follow-up.
Objective
To evaluate the development of CPHD in a group of childhood-onset IGHD followed at a single tertiary center over a long period of time.
Patients and methods
We retrospectively analyzed data from 83 patients initially diagnosed as IGHD with a mean follow-up of 15.2 years. The Kaplan–Meier method and Cox regression analysis was used to estimate the temporal progression and to identify risk factors to development of CPHD over time.
Results
From 83 patients initially with IGHD, 37 (45 %) developed CPHD after a median time of follow up of 5.4 years (range from 1.2 to 21 years). LH and FSH deficiencies were the most common pituitary hormone (38 %) deficiencies developed followed by TSH (31 %), ACTH (12 %) and ADH deficiency (5 %). ADH deficiency (3.1 ± 1 years from GHD diagnosis) presented earlier and ACTH deficiency (9.3 ± 3.5 years) presented later during follow up compared to LH/FSH (8.3 ± 4 years) and TSH (7.5 ± 5.6 years) deficiencies. In a Cox regression model, pituitary stalk abnormalities was the strongest risk factor for the development of CPHD (hazard ratio of 3.28; p = 0.002).
Conclusion
Our study indicated a high frequency of development of CPHD in patients initially diagnosed as IGHD at childhood. Half of our patients with IGHD developed the second hormone deficiency after 5 years of diagnosis, reinforcing the need for lifelong monitoring of pituitary function in these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Childhood onset GH deficiency (GHD) may be isolated (IGHD) or combined with other pituitary hormone deficiencies (CPHD). The diagnosis is mainly based on clinical and auxological parameters as well as failure to respond to GH stimulation tests [1]. The initial evaluation of patients with GHD usually comprehends magnetic resonance imaging (MRI) to evaluate the anatomic integrity of hypothalamic-pituitary region and laboratory evaluation to assess the global pituitary function. Although this first evaluation is useful to classify patients as IGHD or CPHD at diagnosis, it does not rule out the development of additional pituitary hormone deficiencies during follow-up.
This is a major concern as it can cause clinical outcomes, ranging from decrease in general well-being to life-threatening conditions [2, 3]. Patients with CPHD at the diagnosis are usually monitored for the development of additional pituitary hormone deficiencies throughout life. Although most patients initially diagnosed as IGHD remain only with GH deficiency, a considerable number of patients with IGHD evolve to CPHD [4–8].
Some studies have attempted to define the frequency and predictors for the progression of IGHD to CPHD [4–12]. However, most of these studies evaluated a small number of patients with IGHD (n < 26) [5, 9–12], followed by a relatively short-term period (mean of ≤4 years) [5–8] or included only patients with pituitary MRI abnormalities [5, 10–12]. This heterogeneity among studies may explain the wide variability in the rate of development of CPHD in a patient first diagnosed as IGHD (median of 16 %, range from 2 to 94 %) [4–10, 12]. These studies suggested that specific pituitary MRI findings (ectopic posterior pituitary and pituitary stalk abnormalities) [4, 6, 7] and the presence of some genetic defects (such as autosomal dominat GH1 mutations) [7, 13] are variables that increase the probability of developing additional hormonal deficiencies.
The aim of this study was to evaluate the frequency and temporal progression of development of CPHD in a large cohort of childhood-onset IGHD followed at a single tertiary center over a long period of time (average 15 years) and search for prognostic factors related to development of CPHD.
Patients and methods
Patients
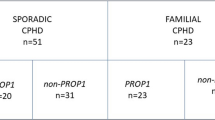
Approval by the Hospital Ethics Committee and written informed consent from patients or parents/guardians were obtained for the study. A retrospective analysis of findings on clinical, endocrine function and MRI was performed in 245 patients followed between 1979 and 2013 at our GHD outpatient clinic. Patients with central nervous system tumors or previous radiation therapy were not included. Patients who presented as CPHD (n = 108, 73M/35F) or unknown hormonal status (n = 27) at baseline were excluded. Patients who developed additional pituitary deficiency during the first year of follow up were considered CPHD at diagnosis (n = 7). Among patients with IGHD at diagnosis (n = 112), 16 were excluded because of short follow-up (≤4 years) and 13 due to lack of data in medical records. Thus, 83 patients (44M/39F) with first diagnosis of IGHD with long-term follow-up (mean of 15.2 years, range from 4.5 to 33.8 years) were selected for the present study.
Clinical evaluation
All patients were followed during growth period 3 or 4 times a year and later twice a year to assess hormonal function and clinical status. Evaluations were performed at the same period of the day and included measurements of height (measured with a stadiometer), weight (measured with a digital scale) and pubertal status. Body mass index (BMI) was calculated as weight (kg) divided by height (m) squared. Height and body mass index (BMI) were expressed as SDS [14]. Target height was calculated [(father’s height + mother’s height + 13 cm for boys or −13 cm for girls)/2] and expressed as SDS. Height deficit was calculated by reducing height SDS at diagnosis from target height SDS. Delivery data were collected and include type of delivery, fetal presentation at birth and perinatal insults.
Hormonal assays
GHD was considered when peak GH after clonidine and hypoglycemia stimulation tests was <5 µg/liter measured by immunoradiometric assay (IRMA) or ≤3.2 µg/liter measured by fluorimetric assay (FIA) in two different occasions [15]. TSH deficiency was defined by low free T4 or total T4 concomitant with low or normal TSH. Absence of thyroid antibodies and normal thyroid ultrasound were obtained when basal TSH levels were slightly elevated to exclude primary hypothyroidism diagnosis. LH and FSH deficiencies were defined by absence of pubertal signs or arrested pubertal development concurrent with low testosterone or estradiol and low or inappropriately normal LH and FSH levels. ACTH deficiency was defined by basal cortisol below 3.6 µg/dl (100 nmol/liter) or cortisol peak after hypoglycemia below 18 µg/dl (497 nmol/liter). Antidiuretic hormone (ADH) deficiency was diagnosed in patients who had low urinary density and/or osmolarity associated with urinary volume above 50 ml/kg in 24 h.
GH was measured before and 60, 90, and 120 min after clonidine stimulation (0.1 mg/m2, po). Glucose, cortisol, GH, TSH, PRL, LH, and FSH were measured in basal state and 15, 30, 45, 60, and 90 min after a combined stimulation test (0.1 U/kg insulin, 200 µg TRH, and 100 µg GnRH, iv). T3, T4, free T4, dehydroepiandrosterone sulfate, estradiol (in girls), and testosterone (in boys) levels were measured at baseline. GH, LH, FSH and prolactin were measured by IRMA until 1992 and then, by FIA. The level of cortisol was measured by radioimmunoassay (RIA) until 1995 and then, by FIA. The level of TSH, total T4 and free T4 were measured by RIA until 1998 and then, by fluorimetric assay (FIA).
Hypothalamic-pituitary MRI
MRI scans were performed in a 1.5 Tesla unit (Signa, GE, Milwaukee, WI, USA) using T1-weighted sagittal and coronal scans with TR: 350 ms and TE: 20 ms. All images were analyzed by the same neuroradiologist (C.C.L.) [16]. The coronal images were obtained using 3.0-mm slice thickness with 10 % gap before and after administration of 0.1 mmol/liter of a paramagnetic contrast (gadolinium). As new MRI techniques have emerged, updated pituitary images were requested to homogeneously evaluate the pituitary anatomy of patients followed for a long period of time. We considered a normal pituitary stalk when we identified a normal diameter from the level of the optic chiasm to its insertion on the pituitary gland. Optic nerves and midline structures were examined.
Statistical analysis
Results were expressed as mean ± SD. Differences between patients who remained IGHD and patients who developed CPHD were tested by t test or Kruskal–Wallis and Chi square or Fisher exact test, as appropriate. Time to progression of additional pituitary hormone deficiency was demonstrated by the Kaplan–Meier curve. Risk for CPHD development was evaluated by univariate analysis (log-rank test) and by multivariate analysis (Cox proportional hazards regression models). A p value <0.05 was considered statistically significant. All statistical calculations were carried out using SPSS (version 18.0.0 SPSS Inc., Chicago, IL).
Results
Patients’ characteristics
Clinical characteristics of 83 consecutive patients with IGHD at diagnosis are shown in Table 1. The cohort was characterized by a slight preponderance of boys over girls. The vast majority of patients were prepubertal at baseline with severe GHD, as shown by the median of highest GH level obtained in two different stimulation tests being 1.2 µg/L (range 0.1–3.8 µg/L) and the presence of severe short stature. A history of vaginal breech birth was reported in 13 % of cases, most of these patients reported perinatal insult. The patients had a high frequency of consanguinity (27 %). A genetic etiology was found in 15 patients (18 %): 6 with GH1 mutations (5 inherited by recessive and one by dominant mode), 5 with GHRHR mutations, two with HESX1 mutations, one with PROP1 deletion and one with GLI2 mutation. These mutations were described in previous studies [16–20].
Normal pituitary MRI was found in 19 % of our patients. Association between ectopic posterior pituitary, stalk defects and hypoplastic anterior pituitary was the most frequent finding at pituitary MRI, observed in 43 % of patients (Fig. 1). The minority of these patients (19 %) had reported perinatal insult and/or vaginal breech birth. Only 5 patients of this cohort presented other central nervous system malformations (two with septo-optic dysplasia, one with sphenoidal meningocele, one with dysgenesis of corpus callosum and one with sphenoidal meningocele and dysgenesis of corpus callosum).
Development of combined pituitary hormone deficiency
From 83 patients initially with IGHD, 37 [mean of 44.6 %, 95 % confidence interval (CI) of 33.9 to −55.3 %] developed CPHD after a median time of follow up of 5.4 years (3.3 and 9.1 years at 25th and 75th percentiles, respectively; Fig. 2a). The most common additional pituitary deficiencies were LH/FSH, followed by TSH, ACTH and ADH (Table 1). This frequency was similar between genders. Fifteen patients developed only one additional pituitary deficiency besides GHD (LH/FSH = 9, TSH = 5 and ADH = 1), 12 had two additional deficiencies (LH/FSH + TSH = 10, TSH + ACTH = 1 and LH/FSH + ADH = 1), 9 patients had three additional deficiencies (LH/FSH + TSH + ACTH = 8 and LH/FSH + TSH + ADH = 1) and 1 had four additional deficiencies.
Patients that developed CPHD have a female predominance (p = 0.024) and had a higher frequency of induced puberty (51 vs. 4.7 %, p < 0.001) than patients that remained IGHD. Both groups of patients had similar occurrence of perinatal insults, consanguinity history and clinical characteristics at diagnosis (Table 1).
Normal pituitary MRI was more frequent in patients that remained IGHD (p = 0.01), whereas stalk abnormalities (p = 0.002) and anterior pituitary hypoplasia (p = 0.037) was more frequently observed in patients who developed CPHD (Fig. 1). Among patients with normal MRI (n = 16), only 2 developed CPHD, one of them had a heterozygous autosomal dominant GH1 splice site mutation (c.291 + 1G > T) known to evolve with other pituitary hormone deficiencies [13]. Four patients had mutations in genes previously associated to CPHD (HESX1 two patients, PROP1 and GLI2 one patient each) and all developed CPHD, except the patient with a heterozygous GLI2 mutation [19]. None of the 10 patients with mutations in genes associated with permanent IGHD (5 with GH1 mutations inherited by recessive mode and 5 with GHRHR mutations) developed CPHD after a median of 15 years of follow-up.
Time to event analysis
The temporal progression of new pituitary hormone deficiencies development is illustrated by the Kaplan–Meier curve (Fig. 2b). TSH and LH/FSH deficiencies developed 7.5 ± 5.6 and 8.3 ± 4.0 from GHD diagnosis, respectively. ADH deficiency developed earlier (3.1 ± 1.0 years from GHD diagnosis, p = 0.0001) and ACTH deficiency developed later (9.3 ± 3.5 years, p < 0.002) than TSH and LH/FSH deficiencies. All these deficiencies occurred in a wide distribution throughout the follow-up, ranging from 1.2 up to 21.2 years, except ADH deficiency, which occurred between 2.3 and 4.2 years from GHD diagnosis.
In the univariate analysis, the risk of CPHD development was significantly greater for patients with vaginal breech birth, ectopic posterior pituitary, pituitary stalk abnormalities and hypoplastic anterior pituitary (Table 2). In a Cox regression model, the presence of pituitary stalk abnormalities was the strongest risk factor for the development of CPHD in our cohort of IGHD children, with a calculated risk increased of 3.28 fold (p = 0.002, Fig. 3). The addition of history of vaginal breech birth to the model was associated with a small increase in the hazard ratio (from 3.28 to 3.37, p = 0.009; Table 2).
Discussion
The establishment of risk to develop additional pituitary deficiencies in patients initially diagnosed as IGHD has a practical implication for clinical endocrinologists. In the present study, we described the temporal frequency of development of CPHD in a cohort of childhood-onset IGHD followed for an average of 15 years at a single tertiary center. We showed a high prevalence (45 %) of development of CPHD in our cohort and half of these patients developed the second hormone pituitary deficiency after 5.4 years of GHD diagnosis (Fig. 2a). Several studies exhibited a low frequency of CPHD development (range from 2 to 9 %) [4, 6–8]. The discrepancy between the present study and previous ones can be partially explained by the relatively short period of patients follow up in these studies (less than 5 years). Additionally, all patients included in our study were followed in a single center and were routinely assessed by laboratory and clinical evaluation; both factors increase our sensitivity to detect patients that developed new pituitary hormone deficiency. In contrast, the two large multicenter studies identified hormone deficiency based on case report forms filled out by innumerous investigators, probably using different diagnosis criteria, which may interfere in the rate of detection of new deficiencies [7, 8]. The progression of techniques employed in hormone assays and MRI throughout time and their impact on time of diagnosis of patients are limitations of this study, but these changes are inherent to long term follow-up studies.
LH/FSH deficiencies were the most common pituitary hormone deficiency described in our cohort, followed by TSH, ACTH and ADH deficiencies (Table 1). Although most studies described TSH deficiency as the commonest deficiency [5, 7, 8], these studies had a short follow up and many patients have not reached pubertal age, therefore, the diagnosis of LH/FSH deficiencies might have been underestimated. Corroborating with this supposition, when we analyzed our data using only the first 5 years of follow up, we observed that TSH deficiency was the most common pituitary hormone deficiency (data not shown).
Only one previous study evaluated the temporal progression of additional pituitary hormone deficiencies in patients with idiopathic IGHD [8]. In this study, the median time to development of LH/FSH, ACTH and TSH deficiencies (1.9–3.3 years) was much lower than in our study (6.4–9.4 years), probably because of the shorter follow up. Nevertheless, median time to develop ADH deficiency (2.4 years) [8] was similar to our data (2.9 years), confirming that development of ADH deficiency when present, occurs early during follow up (Fig. 2b). ACTH deficiency occurred later during follow up in our study, as previously demonstrated [21].
Pituitary stalk abnormality was the strongest predictor for development of CPHD in patients initially diagnosed as IGHD in our study (Fig. 3a). Most longitudinal studies exhibited ectopic posterior pituitary and/or pituitary stalk abnormalities as predictors of CPHD development [4–6]. The ectopic bright signal of posterior pituitary is easier recognizable than the pituitary stalk, which requires contrast agent for an optimal visualization [22]. In our study all MRI were reviewed by a single neuroradiologist, which improved the identification of pituitary stalk abnormalities. Among the 44 patients with pituitary stalk abnormalities (37 of them also had ectopic posterior pituitary), and 27 developed a second hormone deficiency (Fig. 1). Conversely, only 2 of 16 patients with normal MRI developed an additional hormonal deficiency, including a patient with an autosomal dominant GH1 mutation, associated to development of CPHD [13].
In our cohort, 15 patients (18 %) had an identified genetic etiology, 5 of these patients had mutations known to cause CPHD and 80 % developed CPHD; and 10 patients had mutations known to cause IGHD and 100 % remained IGHD. In a previous study, patients with known genetic defects had more severe GHD phenotype and were more frequently diagnosed as CPHD [7]. At the present time, only a small portion of patients with GHD have an identified molecular diagnosis. These defects should be divided in two groups according to the potential to cause IGHD or CPHD. It is possible that in the near future, with the identification and characterization of novel genes associated with GHD, we will be able to better predict the evolution of patients initially diagnosed as IGHD based on combined information of MRI and genetic analysis.
In conclusion, our study indicated that a high proportion of patients initially diagnosed as IGHD developed additional pituitary hormone deficiency. Our results reinforce the need for lifelong monitoring of pituitary function in IGHD patients, since a second pituitary hormone deficiency can develop up to 21 years after GHD diagnosis.
References
Growth Hormone Research Society (2000) Consensus guidelines for the diagnosis and treatment of growth hormone (GH) deficiency in childhood and adolescence: summary statement of the GH Research Society. GH Research Society. J Clin Endocrinol Metab 85(11):3990–3993. doi:10.1210/jcem.85.11.6984
Schneider HJ, Aimaretti G, Kreitschmann-Andermahr I, Stalla GK, Ghigo E (2007) Hypopituitarism. Lancet 369(9571):1461–1470. doi:10.1016/S0140-6736(07)60673-4
Shulman DI, Palmert MR, Kemp SF (2007) Adrenal insufficiency: still a cause of morbidity and death in childhood. Pediatrics 119(2):e484–e494. doi:10.1542/peds.2006-1612
Bozzola M, Mengarda F, Sartirana P, Tato L, Chaussain JL (2000) Long-term follow-up evaluation of magnetic resonance imaging in the prognosis of permanent GH deficiency. Eur J Endocrinol 143(4):493–496. doi:10.1530/eje.0.1430493
di Iorgi N, Secco A, Napoli F, Tinelli C, Calcagno A, Fratangeli N, Ambrosini L, Rossi A, Lorini R, Maghnie M (2007) Deterioration of growth hormone (GH) response and anterior pituitary function in young adults with childhood-onset GH deficiency and ectopic posterior pituitary: a two-year prospective follow-up study. J Clin Endocrinol Metab 92(10):3875–3884. doi:10.1210/jc.2007-1081
Jagtap VS, Acharya SV, Sarathi V, Lila AR, Budyal SR, Kasaliwal R, Sankhe SS, Bandgar TR, Menon PS, Shah NS (2012) Ectopic posterior pituitary and stalk abnormality predicts severity and coexisting hormone deficiencies in patients with congenital growth hormone deficiency. Pituitary 15(2):243–250. doi:10.1007/s11102-011-0321-4
Deal C, Hasselmann C, Pfaffle RW, Zimmermann AG, Quigley CA, Child CJ, Shavrikova EP, Cutler GB Jr, Blum WF (2013) Associations between pituitary imaging abnormalities and clinical and biochemical phenotypes in children with congenital growth hormone deficiency: data from an international observational study. Horm Res Paediatr 79(5):283–292. doi:10.1159/000350829
Blum WF, Deal C, Zimmermann AG, Shavrikova EP, Child CJ, Quigley CA, Drop SL, Cutler GB Jr, Rosenfeld RG (2014) Development of additional pituitary hormone deficiencies in pediatric patients originally diagnosed with idiopathic isolated GH deficiency. Eur J Endocrinol 170(1):13–21. doi:10.1530/EJE-13-0643
Lange M, Feldt-Rasmussen U, Svendsen OL, Kastrup KW, Juul A, Muller J (2003) High risk of adrenal insufficiency in adults previously treated for idiopathic childhood onset growth hormone deficiency. J Clin Endocrinol Metab 88(12):5784–5789. doi:10.1210/jc.2003-030529
Leger J, Danner S, Simon D, Garel C, Czernichow P (2005) Do all patients with childhood-onset growth hormone deficiency (GHD) and ectopic neurohypophysis have persistent GHD in adulthood? J Clin Endocrinol Metab 90(2):650–656. doi:10.1210/jc.2004-1274
Tauber M, Chevrel J, Diene G, Moulin P, Jouret B, Oliver I, Pienkowski C, Sevely A (2005) Long-term evolution of endocrine disorders and effect of GH therapy in 35 patients with pituitary stalk interruption syndrome. Horm Res 64(6):266–273. doi:10.1159/000089425
Fernandez-Rodriguez E, Quinteiro C, Barreiro J, Marazuela M, Pereiro I, Peino R, Cabezas-Agricola JM, Dominguez F, Casanueva FF, Bernabeu I (2011) Pituitary stalk dysgenesis-induced hypopituitarism in adult patients: prevalence, evolution of hormone dysfunction and genetic analysis. Neuroendocrinology 93(3):181–188. doi:10.1159/000324087
Mullis PE, Robinson IC, Salemi S, Eble A, Besson A, Vuissoz JM, Deladoey J, Simon D, Czernichow P, Binder G (2005) Isolated autosomal dominant growth hormone deficiency: an evolving pituitary deficit? A multicenter follow-up study. J Clin Endocrinol Metab 90(4):2089–2096. doi:10.1210/jc.2004-1280
Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, Mei Z, Curtin LR, Roche AF, Johnson CL (2000) CDC growth charts: United States. Adv Data (314):1–27. http://www.ncbi.nlm.nih.gov/pubmed/11183293
Silva EG, Slhessarenko N, Arnhold IJ, Batista MC, Estefan V, Osorio MG, Marui S, Mendonca BB (2003) GH values after clonidine stimulation measured by immunofluorometric assay in normal prepubertal children and GH-deficient patients. Horm Res 59(5):229–233. doi:10.1159/000070222
Osorio MG, Marui S, Jorge AA, Latronico AC, Lo LS, Leite CC, Estefan V, Mendonca BB, Arnhold IJ (2002) Pituitary magnetic resonance imaging and function in patients with growth hormone deficiency with and without mutations in GHRH-R, GH-1, or PROP-1 genes. J Clin Endocrinol Metab 87(11):5076–5084
Carvalho LR, Woods KS, Mendonca BB, Marcal N, Zamparini AL, Stifani S, Brickman JM, Arnhold IJ, Dattani MT (2003) A homozygous mutation in HESX1 is associated with evolving hypopituitarism due to impaired repressor-corepressor interaction. J Clin Invest 112(8):1192–1201. doi:10.1172/JCI18589
Rocha MG, Marchisotti FG, Osorio MG, Marui S, Carvalho LR, Jorge AA, Mendonca BB, Arnhold IJ (2008) High prevalence of pituitary magnetic resonance abnormalities and gene mutations in a cohort of Brazilian children with growth hormone deficiency and response to treatment. J Pediatr Endocrinol Metab 21(7):673–680
Franca MM, Jorge AA, Carvalho LR, Costalonga EF, Vasques GA, Leite CC, Mendonca BB, Arnhold IJ (2010) Novel heterozygous nonsense GLI2 mutations in patients with hypopituitarism and ectopic posterior pituitary lobe without holoprosencephaly. J Clin Endocrinol Metab 95(11):E384–E391. doi:10.1210/jc.2010-1050
Marui S, Trarbach EB, Boguszewski MC, Franca MM, Jorge AA, Inoue H, Nishi MY, de Lacerda Filho L, Aguiar-Oliveira MH, Mendonca BB, Arnhold IJ (2012) GH-releasing hormone receptor gene: a novel splice-disrupting mutation and study of founder effects. Horm Res Paediatr 78(3):165–172. doi:10.1159/000342760
Makino S, Kawasaki D, Irimoto H, Tanimoto M (2002) Late onset of adrenocortical failure in GH deficiency with invisible pituitary stalk: a case report of a 48-year-old Japanese man and review of the literature. Endocr J 49(2):231–240
Garel C, Leger J (2007) Contribution of magnetic resonance imaging in non-tumoral hypopituitarism in children. Horm Res 67(4):194–202. doi:10.1159/000097755
Acknowledgments
This work was supported by grants from Sao Paulo Research Foundation (FAPESP) (2013/03236-5) and from The National Council for Scientific and Technological Development (CNPq) (307922/2013-8 to I.J.P.A.; 305743/2011-2 to B.B.M.; 304678/2012-0 to A.A.L.J).
Conflict of interest
The authors declare there is no conflict of interest that could be perceived as influencing the impartiality of the research reported.
Author information
Authors and Affiliations
Corresponding author
Additional information
Luciani R. S. Carvalho and Alexander A. L. Jorge have contributed equally to this article.
Rights and permissions
About this article
Cite this article
Otto, A.P., França, M.M., Correa, F.A. et al. Frequent development of combined pituitary hormone deficiency in patients initially diagnosed as isolated growth hormone deficiency: a long term follow-up of patients from a single center. Pituitary 18, 561–567 (2015). https://doi.org/10.1007/s11102-014-0610-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-014-0610-9