Abstract
Background The role of olanzapine in the treatment of chemotherapy-induced nausea and vomiting (CINV) in addition to the antiemetic therapeutic combination with aprepitant, setrons, and corticosteroids has not been well defined. Objective To investigate the effectiveness of the addition of olanzapine to a standard triplet therapy for the prevention of CINV in patients who experienced CINV during their first chemotherapy course, despite receiving a well-managed prevention protocol. Setting One comprehensive cancer centre in France. Method In a retrospective study with comparator, patients with a high risk of emesis were assigned to two groups during two different 6-month periods, before and after the introduction of olanzapine in clinical practice, respectively. In the olanzapine group, the antiemetic protocol for the second course of chemotherapy was reinforced by the addition of olanzapine at 5 mg/day from day 1 to 5 in contrast with the control group. Main outcome measure The proportion of patients who experienced neither nausea nor emesis during the delayed phase (24–120 h). Results The 25 patients in each group exhibited comparable characteristics and emetic chemotherapy level. During the first course, no significant difference was observed. During the second course, nausea and vomiting were ameliorated in 12 patients in the olanzapine group and 4 patients in the control group (p < 0.05). Nausea (12 vs. 4, p < 0.05) and vomiting (18 vs. 11, p < 0.05) also significantly improved. In the OLZ group, no adverse event was linked to olanzapine use. Conclusion The addition of olanzapine was observed to effectively restore CINV prevention in patients who did not respond to standard antiemetic therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impacts on practice
-
Olanzapine is effective for the secondary prophylaxis of delayed chemo-induced nausea and vomiting.
-
Giving 5mg/day olanzapine is feasible and should be considered for further prospective studies.
-
The sequential use of olanzapine is very well tolerated.
Introduction
Chemotherapy-induced nausea and vomiting (CINV) are adverse reactions with strongly deleterious effects on patient quality of life [1,2,3]. When severe CINV occurs, it may affect the physiological state of an already fragile patient and result in anorexia, malnutrition, or dehydration. The occurrence of CINV can ultimately affect the type of treatment that a patient with cancer can receive. Furthermore, the adverse reactions may result in additional hospitalisation or medical consultation, which can have a significant medico-economic impact [3, 4].
The development of effective therapeutic strategies for the prevention of CINV over the past three decades has led to a significant improvement in patient tolerance of antineoplastic agents. These strategies include consensus guidelines to prevent CINV established by organisations, such as the American Society of Clinical Oncology (ASCO), the Multinational Association for Supportive Care in Cancer (MASCC), the European Society of Medical Oncology (ESMO), and the National Comprehensive Cancer Network (NCCN) [5,6,7,8]. In particular, for highly emetogenic chemotherapy, the current standard treatment to prevent CINV combines three pharmacological classes: neurokinin-1 receptor antagonist (NK1RA), 5-hydroxytryptamine-3 receptor antagonist (5-HT3RA), and corticosteroids. However, in a phase III trial conducted by de Wit et al. only 62% of patients who received this triplet therapy with cisplatin-based chemotherapy experienced complete response (CR), which was defined as no emesis or use of rescue therapy like metoclopramide [9]. Finally, when patients experience CINV despite the application of the standard treatment, particularly in the early courses of chemotherapy, they could develop anxiety and anticipatory nausea and vomiting [10]. In the case of breakthrough CINV, antiemetic rescue therapy and secondary prophylaxis are based on rescue therapy, but the recommendations are not consensual.
Olanzapine is an atypical antipsychotic drug that targets five types of receptors: dopaminergic (D1, D2, and D4), serotonergic (5-HT2A, 5-HT2C, 5-HT3, and 5-HT6), adrenergic (alpha1), histaminergic (H1), and muscarinic (M1, M2, M3, and M4) [11]. In particular, antagonism of receptors D2, 5-HT2C, 5-HT3, M1, and H1, which are involved in CINV genesis, provides a partial explanation for their antiemetic properties [12, 13]. Since the first phase I trial [14], numerous studies have attempted to evaluate the contribution of olanzapine in the prevention and treatment of CINV.
In a phase II trial, Abe et al. evaluated the addition of 5 mg olanzapine to triplet therapy (aprepitant, palonosetron, and dexamethasone) administered each day for 5 days to adult patients with gynaecological cancer who were also administered cisplatin (≥ 50 mg/m2). A CR rate (no vomiting and no rescue therapy) for delayed CINV of 95% was observed [15]. In a large phase III study focused on the first course of chemotherapy, the systematic addition of olanzapine (10 mg on days 1–4) to triplet antiemetic therapy (aprepitant or fosaprepitant; palonosetron, ondansetron, or granisetron; and dexamethasone) ameliorated delayed nausea, as well as the delayed CR rate (no vomiting and no rescue therapy) in adult patients [16]. Since this trial, the ASCO and NCCN published recommendations for the systematic addition of olanzapine to standard triplet therapy (10 mg on days 1–4 or 2–4) [7, 8]. In another phase III trial, Navari et al. evaluated olanzapine as a rescue treatment for CINV in adult patients who had received prior prophylaxis with palonosetron, fosaprepitant, and dexamethasone; they observed that, for the management of breakthrough CINV, 10 mg olanzapine once daily for 3 days was superior to 10 mg metoclopramide three times daily for 3 days [17]. Regardless of whether olanzapine was administered as a monotherapy or in combination, at the dosage of 5 or 10 mg for 4 or 5 days, all published clinical trials of olanzapine with CR rate (no vomiting, no rescue therapy) in delayed CINV as primary endpoint report notably good tolerance with no grade 3 nor 4 toxicity [18,19,20,21,22,23].
Aim of the study
In this study, we evaluated the impact of the addition of olanzapine during the second course of chemotherapy in adult patients receiving highly emetic chemotherapy who did not respond to the standard antiemetic therapy (aprepitant, ondansetron, and methylprednisolone) during the first course. The primary objective was to evaluate the occurrence of nausea and vomiting in the delayed phase (composite endpoints: CINV). Furthermore, the occurrence of all degrees of nausea (CIN), the occurrence of vomiting (CIV), and the tolerance of the treatment were all independently evaluated.
Ethics approval
This study was approved by the Scientific Commission of Clinical Trials of Gustave Roussy Cancer Campus, Villejuif.
Method
Study design
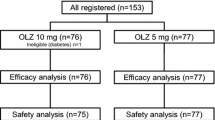
This study evaluated the addition of olanzapine (ZYPREXA® 5 mg) to a standard antiemetic therapy for the control of nausea and vomiting in patients who had experienced nausea or/and emesis in the delayed phase, despite standard therapy during the previous chemotherapy course. The study was retrospective and open, and compared olanzapine plus the standard triplet therapy with the standard triplet therapy alone. In this study, a course of chemotherapy has the same definition as a cycle of chemotherapy: a single administration of a chemotherapy regimen.
The study population was composed of adult patients for whom CINV prevention failed during their first course of chemotherapy, despite standard therapy, and who had never received olanzapine. All patients were treated with standard triplet therapy [a 5-HTRA (ondansetron on day 1, 8 mg intravenous 30 min prior to chemotherapy), NK1RAs (aprepitant 125 mg orally on day 1, 1 h prior to chemotherapy, and aprepitant 80 mg in the morning on days 2–3), and a corticosteroid (methylprednisolone 60 mg intravenous on day 1, 30 min prior to chemotherapy, and 64 mg orally in the morning on days 2–4)]. One group (the OLZ group) received 5 mg of olanzapine per day in addition to the standard treatment from day 1 to day 5 of chemotherapy. The second group (the Comparator group) received only standard treatment (without any breakthrough therapy). Both groups of patients received at least two courses of chemotherapy. The frequency and severity of CINV were compared between the two groups during the first and second courses of chemotherapy. Failure to prevent CINV during the delayed phase (i.e. between 24 and 120 h after the course of chemotherapy) was defined as grade 2 or higher for nausea and grade 1 or higher for vomiting in accordance with the National Cancer Institute’s Common Terminology Criteria for Adverse Events (NCI-CTCAE) v.4.03.
Patient selection and treatment
For both groups, the patients were eligible for inclusion in the study if they were older than 18 years and CINV had not been prevented during the delayed phase of their first course of chemotherapy, despite standard and rescue treatments (metoclopramide 10 mg t.i.d.). All patients enrolled between November 2011 and April 2012 were assigned to the comparative group and all patients enrolled between November 2013 and April 2014 were assigned to the OLZ group.
Data collection and analysis
The data were collected from the patient’s electronic medical records and from intravenous chemotherapy prescription software Win Simbad® (Gustave Roussy Cancer Campus, Villejuif, France). A standardised data collection system was validated by a pharmacist and an oncologist. All relevant demographical data (age, sex, weight, and height) and medical records (type and location of the tumour, stage, performance status, renal, hepatic function, and blood glucose) were collected. The emetogenic potential of the chemotherapy was determined in accordance with previous recommendations [5,6,7,8].
The occurrence and grade of nausea and vomiting during the first and second courses of chemotherapy were assessed during the delayed phase (between 24 and 120 h from the end of each chemotherapy course). The effectiveness of the antiemetic prevention was evaluated based on the absence of nausea and/or vomiting. The percentage of patients who jointly experienced no nausea and no vomiting (CINV), no vomiting (CIV), or no nausea (CIN) was compared within each group after the first and second courses, and between the two groups.
The statistical tests used were the Chi square test and Fisher’s exact test for comparison between the groups, McNemar’s test for intragroup comparison (first course versus second course) and Student’s t test for quantitative demographic data. All statistical analysis was computed by using R® (The R Project for Statistical Computing v.3.2.2). The significance level for the first alpha type was 0.05.
Results
Patients and treatment characteristics
The study comprised 50 patients, with 25 patients per group. The average age of the study participants was 50.3 ± 12.9 years in the OLZ group and 56.0 ± 9.2 years in the Comparator group. Both groups were statistically comparable with respect to age, sex, body mass index, renal and hepatic function, and performance status (Table 1). The most frequent oncological localisations were lung cancer (OLZ: 48%; Comparator: 56%) and sarcoma (OLZ: 24%; Comparator: 8%). In the OLZ group, 72% of patients presented with metastatic disease; in the Comparator group, this was 64%. A comparable majority of patients had received highly emetogenic chemotherapy (cisplatin ≥ 70 mg/m2) in both groups (OLZ: 92%; Comparator: 96%), whereas the three other chemotherapy regimens were composed of anthracycline and cyclophosphamide (similar to a highly emetogenic therapy). In total, 36% of all patients had previously received a high-emetic-risk regimen containing cisplatin (OLZ: 25%; Comparator: 16%). For all patients, the chemotherapy regimen was not modified between the first and the second course.
Evaluation of antiemetic activity of olanzapine
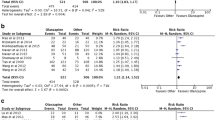
The results for the control of CINV and vomiting at the end of the second course are shown in Fig. 1. Although none of the patients in the OLZ group reported a delay in CINV during their first course, these symptoms significantly improved after they were treated with olanzapine, with 48% of them reporting no delay in CINV during their second course (p = 0.0015). The control of CIV (p = 0.0042) and CIN (p = 0.0033) also significantly improved in the OLZ group from course 1 to course 2. In contrast, patients in the control group reported no improvement in the control of CINV between the two courses for CINV, CIV, and CIN. When both groups were compared during second course, patients in the OLZ group experienced significantly better control of CINV (48% vs. 4%; p < 0.034), CIV (p < 0.045), and CIN (p < 0.034) than patients in the Comparator group.
Antiemetic activity of olanzapine in delayed phase for nausea and vomiting (NV), nausea (N) and vomiting (V). On the dotted line appears the statistical difference between the proportion of patients who meet endpoints at intercure 2 when compared with the proportion of patients who meet endpoints at intercure 1 inside each group (Comparator and Olanzapine). On full line appears the proportion of patients who meet endpoints at intercure 2 between Comparator and Olanzapine group. Non-significant statistically differences are not represented
Treatment safety
The known adverse effects of olanzapine were not reported in the patients’ electronic health records. Clinically, no significant weight gain was observed in patients treated with olanzapine. For the measurement on day 1 of each course, the weight loss (mean ± standard deviation) from course 1 to course 2 was − 0.80 ± 3.11 kg for the OLZ group and − 1.28 ± 3.59 kg for the Comparator group. The relative weight loss from course 1 to course 3 was − 1.84 ± 3.52 kg for the OLZ group and − 1.68 ± 3.42 kg for the Comparator group. Biologically, no significant variations in transaminase enzymes or bilirubin were observed. Glycaemia was not detected.
Discussion
Our study illustrates that the addition of 5 mg olanzapine between day 1 to day 5 significantly reinforced protection against CINV during the delayed phase compared with the standard antiemetic therapy. The main objective of the study, to reduce delayed CINV, was achieved, as well as the secondary objectives. Finally, we discovered a significant benefit from the addition of olanzapine to the standard triplet therapy after failure to prevent delayed CINV during the first course of chemotherapy.
In the three comparative studies in which olanzapine was added to a standard antiemetic protocol, the drug significantly improved the symptoms of nausea and vomiting during the delayed phase. In a study of adult patients by Tan et al. the CR was 78.6% in the treatment group and 56.5% in the control group. Nausea improved in 69.9% patients in the treatment group and 30.4% in the control group [24]. It should be noted that because of the unavailability of aprepitant in China, the protocol used in this study for the prevention of nausea and vomiting did not include an NK1RA [25]. Mizukami et al. also reported the effectiveness of olanzapine in addition to standard prophylaxis in adult patients in the delayed phase, showing an improvement in total control (no vomiting, no use of rescue medication, and maximum nausea of 5 mm on a 100 mm VAS). The TC was 64% in the treated group and 23% in the control group. In this trial, the choice of the setron was made by the clinician [26]. Finally, a large study by Navari et al. in adult patients showed a significant improvement for patients who received olanzapine in the delayed phase with respect to the control of nausea (42% in the treated group versus 25% in the control group, p = 0.002) and the CR rate (67% in the treated group versus 52% in the control group, p = 0.007) [16]. In this study, the standard therapy was a choice of conventional triplet therapy with aprepitant (or fosaprepitant), a setron with either a short half-life (ondansetron or granisetron) or a long half-life (palonosetron), and dexamethasone at the appropriate dose.
Our study evaluated the addition of olanzapine for delayed CINV prevention during the second course of chemotherapy only for patients who experienced CINV during their first course. Olanzapine was administered daily at 5 mg from day 1, similar to previous studies [15, 26]. Although several studies investigated 10 mg daily, recent investigations have highlighted the non-inferiority between 5 and 10 mg in terms of effectiveness, with 5 mg resulting in less drowsiness [27].
As proposed by Hernandez-Torres et al. we selected a composite endpoint that represented the absence of both nausea and vomiting to better understand the effect of olanzapine on the control of CINV [28]. For similar reasons, Navari et al. also recently adopted the absence of nausea as a main objective, because they now consider this criterion more appropriate than CR [16].
However, with respect to psychiatric indications, clear associations between olanzapine and weight gain [29,30,31], akathisia, various cardiovascular disorders, and urinary incontinence have been reported; these outcomes have not been observed in our study. These results confirmed the distinct tolerance profile of olanzapine in short-term treatment compared with continuous treatment [18,19,20,21,22,23]. In two different prospective studies, the first with 44 patients and the second with 241 patients, no significant differences in drowsiness between the olanzapine and comparison groups were observed [26, 32]. A randomized controlled study published by Navari et al. showed a significant rate of undesired fatigue in patients administered olanzapine on Day 2 compared with that at baseline; however, the attending clinician did not attribute the two grade 3 and three grade 4 adverse events observed in patients administered olanzapine to the drug [16]. In terms of biological disorders, because the manufacturer of olanzapine states that iatrogenic hyperglycaemia appears after 3 months of continuous treatment, the risk of hyperglycaemia was assumed to be low. A side effect of obesity has not yet been reported when olanzapine is used as an antiemetic [18,19,20,21,22,23].
The recent antiemetic recommendations from ASCO have included the addition of olanzapine [8] after the high-quality study by Navari et al. which confirmed the value of olanzapine as a systematic addition to the triple standard therapy for highly emetogenic chemotherapy [16]. From our perspective, the systematic addition of olanzapine to the standard prevention therapy raised several questions. Firstly, the standard triplet therapy has led to a significant reduction in the occurrence of CINV. The addition of another drug to this therapy is excessive polypharmacy, which is already a concern for patients [33]. Another area for improvement was the actual application of these recommendations. In a cohort of 1295 patients, Gilmore et al. showed that only 57.3% of antiemetic therapies prescribed conformed to current recommendations. Patients who were prescribed the recommended therapy experienced significantly less CINV than other patients (p < 0.001) during the overall time period [34]. Finally, and paradoxically, recent investigations observed a trend of the overuse of antiemetics with unnecessary associated costs [35]. As shown in our study, olanzapine can be used to reinforce the standard treatment after failure. This clinical practice appears to be more reasonable than the systematic addition of olanzapine and may help improve the efficiency of these antiemetic treatments.
Our study has some limitations, because it was a retrospective study with a small sample size, and patients were selected without randomization.
Conclusion
Our study showed that the addition of olanzapine to a standard prevention protocol in patients who lack CINV control can significantly improve the prevention of CINV with a highly acceptable risk-to-benefit ratio. Although the role of olanzapine in the prevention of CINV is currently under discussion, our study supported this original strategy for antiemetic treatment. Large-scale prospective and comparative studies could help to confirm our observations.
References
Bloechl-Daum B, Deuson RR, Mavros P, Hansen M, Herrstedt J. Delayed nausea and vomiting continue to reduce patients’ quality of life after highly and moderately emetogenic chemotherapy despite antiemetic treatment. J Clin Oncol. 2006;24(27):4472–8.
Fernández-Ortega P, Caloto MT, Chirveches E, Marquilles R, Francisco JS, Quesada A, et al. Chemotherapy-induced nausea and vomiting in clinical practice: impact on patients’ quality of life. Support Care Cancer. 2012;20(12):3141–8.
Sommariva S, Pongiglione B, Tarricone R. Impact of chemotherapy-induced nausea and vomiting on health-related quality of life and resource utilization: a systematic review. Crit Rev Oncol Hematol. 2016;99:13–36.
Carlotto A, Hogsett VL, Maiorini EM, Razulis JG, Sonis ST. The economic burden of toxicities associated with cancer treatment: review of the literature and analysis of nausea and vomiting, diarrhoea, oral mucositis and fatigue. Pharmacoeconomics. 2013;31(9):753–66.
Navari RM, Aapro M. Antiemetic prophylaxis for chemotherapy-induced nausea and vomiting. N Engl J Med. 2016;374(14):1356–67.
Roila F, Molassiotis A, Herrstedt J, Aapro M, Gralla RJ, Bruera E, et al. 2016 MASCC and ESMO guideline update for the prevention of chemotherapy- and radiotherapy-induced nausea and vomiting and of nausea and vomiting in advanced cancer patients. Ann Oncol. 2016;27(suppl. 5):v119–33.
Berger MJ, Ettinger DS, Aston J, Barbour S, Bergsbaken J, Bierman PJ, et al. Antiemesis, Version 2.2017. Featured updates to the NCCN guidelines. J Natl Compr Canc Netw. 2017;15:883–93.
Hesketh PJ, Kris MG, Basch E, Bohlke K, Barbour SY, Clark-Snow RA, et al. Antiemetics: American society of clinical oncology clinical practice guideline update. J Clin Oncol. 2017;35(28):3240–61.
de Wit R, Herrstedt J, Rapoport B, Carides AD, Carides G, Elmer M, et al. Addition of the oral NK1 antagonist aprepitant to standard antiemetics provides protection against nausea and vomiting during multiple cycles of cisplatin-based chemotherapy. J Clin Oncol. 2003;21(22):4105–11.
Roscoe JA, Bushunow P, Morrow GR, Hickok JT, Kuebler PJ, Jacobs A, et al. Patient expectation is a strong predictor of severe nausea after chemotherapy: a University of Rochester Community Clinical Oncology Program study of patients with breast carcinoma. Cancer. 2004;101(11):2701–8.
Bymaster FP, Calligaro DO, Falcone JF, Marsh RD, Moore NA, Tye NC, et al. Radioreceptor binding profile of the atypical antipsychotic olanzapine. Neuropsychopharmacology. 1996;14(2):87–96.
Pirl WF, Roth AJ. Remission of chemotherapy-induced emesis with concurrent olanzapine treatment: a case report. Psychooncology. 2000;9(1):84–7.
Passik SD, Kirsh KL, Theobald DE, Dickerson P, Trowbridge R, Gray D, et al. A retrospective chart review of the use of olanzapine for the prevention of delayed emesis in cancer patients. J Pain Symptom Manag. 2003;25(5):485–8.
Passik SD, Navari RM, Jung S-H, Nagy C, Vinson J, Kirsh KL, et al. A phase I trial of olanzapine (Zyprexa) for the prevention of delayed emesis in cancer patients: a Hoosier Oncology Group study. Cancer Invest. 2004;22(3):383–8.
Abe M, Hirashima Y, Kasamatsu Y, Kado N, Komeda S, Kuji S, et al. Efficacy and safety of olanzapine combined with aprepitant, palonosetron, and dexamethasone for preventing nausea and vomiting induced by cisplatin-based chemotherapy in gynecological cancer: KCOG-G1301 phase II trial. Support Care Cancer. 2016;24(2):675–82.
Navari RM, Qin R, Ruddy KJ, Liu H, Powell SF, Bajaj M, et al. Olanzapine for the prevention of chemotherapy-induced nausea and vomiting. N Engl J Med. 2016;375(2):134–42.
Navari RM, Nagy CK, Gray SE. The use of olanzapine versus metoclopramide for the treatment of breakthrough chemotherapy-induced nausea and vomiting in patients receiving highly emetogenic chemotherapy. Support Care Cancer. 2013;21(6):1655–63.
Hocking CM, Kichenadasse G. Olanzapine for chemotherapy-induced nausea and vomiting: a systematic review. Support Care Cancer. 2014;22(4):1143–51.
Fonte C, Fatigoni S, Roila F. A review of olanzapine as an antiemetic in chemotherapy-induced nausea and vomiting and in palliative care patients. Crit Rev Oncol Hematol. 2015;95(2):214–21.
Chelkeba L, Gidey K, Mamo A, Matso T, Yohannes B, Melaku T. Olanzapine for chemotherapy-induced nausea and vomiting: systematic review and meta-analysis. Pharm Pract. 2017;15(1):877.
Chiu L, Chow R, Popovic M, Navari RM, Shumway NM, Chiu N, et al. Efficacy of olanzapine for the prophylaxis and rescure of chemotherapy-induced nausea and vomiting (CINV): a systematic review and meta-analysis. Support Care Cancer. 2016;24(5):2381–92.
DeRemer DL, Clemmons AB, Orr J, Clark SM, Gandhi AS. Emerging role of olanzapine for prevention and treatment of chemotherapy-induced nausea and vomiting. Pharmacotherapy. 2016;36(2):218–29.
Yoodee J, Permsuwan U, Nimworapan M. Efficacy and safety of olanzapine for the prevention of chemotherapy-inducec nausea and vomiting: a systematic review and meta-analysis. Crit Rev Oncol Hematol. 2017;112:113–25.
Tan L, Liu J, Liu X, Chen J, Yan Z, Yang H, et al. Clinical research of Olanzapine for prevention of chemotherapy-induced nausea and vomiting. J Exp Clin Cancer Res. 2009;28:131.
Liu J, Tan L, Zhang H, Li H, Liu X, Yan Z, et al. QoL evaluation of olanzapine for chemotherapy-induced nausea and vomiting comparing with 5-HT3 receptor antagonist. Eur J Cancer Care. 2015;24(3):436–43.
Mizukami N, Yamauchi M, Koike K, Watanabe A, Ichihara K, Masumori N, et al. Olanzapine for the prevention of chemotherapy-induced nausea and vomiting in patients receiving highly or moderately emetogenic chemotherapy: a randomized, double-blind, placebo-controlled study. J Pain Symptom Manag. 2014;47(3):542–50.
Yanai T, Iwasa S, Hashimoto H, Ohyanagi F, Takigushi T, Takedas K, et al. A double-blind randomized phase II dose-finding study of olanzapine 10 mg or 5 mg for the prophylaxis of emesis induced by highly emetogenic cisplatin-based chemotherapy. Int J Clin Oncol. 2018;23(2):382–8.
Hernandez Torres C, Mazzarello S, Ng T, Dranitsaris G, Hutton B, Smith S, et al. Defining optimal control of chemotherapy-induced nausea and vomiting-based on patients’ experience. Support Care Cancer. 2015;23(11):3341–59.
Hale AS. Olanzapine. Br J Hosp Med. 1997;58(9):442–5.
Allison DB, Casey DE. Antipsychotic-induced weight gain: a review of the literature. J Clin Psychiatry. 2001;62(Suppl 7):22–31.
Fountaine RJ, Taylor AE, Mancuso JP, Greenway FL, Byerley LO, Smith SR, et al. Increased food intake and energy expenditure following administration of olanzapine to healthy men. Obesity. 2010;18(8):1646–51.
Navari RM, Gray SE, Kerr AC. Olanzapine versus aprepitant for the prevention of chemotherapy-induced nausea and vomiting: a randomized phase III trial. J Support Oncol. 2011;9(5):188–95.
Nightingale G, Hajjar E, Swartz K, Andrel-Sendecki J, Chapman A. Evaluation of a pharmacist-led medication assessment used to identify prevalence of and associations with polypharmacy and potentially inappropriate medication use among ambulatory senior adults with cancer. J Clin Oncol. 2015;33(13):1453–9.
Gilmore JW, Peacock NW, Gu A, Szabo S, Rammage M, Sharpe J, et al. Antiemetic guideline consistency and incidence of chemotherapy-induced nausea and vomiting in US community oncology practice: INSPIRE study. J Oncol Pract. 2014;10(1):68–74.
Encinosa W, Dadidoff AJ. Changes in antiemetic overuse to choosing wisely recommendations. JAMA Oncol. 2016;3(3):320–6.
Acknowledgements
Mr. Vincent Blazy for the help in software data extraction.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Slimano, F., Netzer, F., Borget, I. et al. Olanzapine as antiemetic drug in oncology: a retrospective study in non-responders to standard antiemetic therapy. Int J Clin Pharm 40, 1265–1271 (2018). https://doi.org/10.1007/s11096-018-0649-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-018-0649-1