Abstract
Oral administration is the most preferred route for drug administration in clinic. However, due to unsatisfactory physicochemical properties of drugs and various physiological barriers, the oral bioavailability of most poorly water-soluble and macromolecules drugs is low and the therapeutic effect is unsatisfactory. Ionic liquids (ILs), molten salts with unique properties, show amazing potential for oral delivery. In addition to being able to form active pharmaceutical ingredients based ILs (API-ILs) to overcome drug solubility and polymorphism issues, ILs have also been used to enhance the solubility of poorly soluble drugs, enhance drug stability in the gastrointestinal environment, improve drug permeability in intestinal mucus, and facilitate drug penetration across the intestinal epithelial barrier. Furthermore, ILs were attempted as formulation components to develop novel oral drug delivery systems. This review focus on the application progress of ILs in oral drug delivery and the mechanisms. The challenges and perspectives of the development of ILs-based oral delivery systems are also discussed.
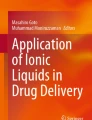
Graphical Abstract
This article reviews the latest advances of ionic liquids for oral drug delivery, focusing on the application and related mechanisms of ionic liquids in improving the drug physicochemical properties and enhancing drug delivery across physiological barriers.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
IINTRODUCTION
Oral administration is the most preferred route for drug administration in clinic, especially for long-term patients and out-patients. Moreover, in the past decade, oral drugs continue to dominate the market, accounting for more than 50% of FDA-approved drugs (1). However, after taking orally, drugs need to be absorbed into circulation from gastrointestinal (GI) tract firstly and then transported to the lesion site to exert therapeutic effect. Due to unsatisfactory physicochemical properties of drugs such as poor solubility and/or permeability, and various physiological barriers such as pH, enzyme barrier, and mucus and intestinal epithelial barriers, the oral bioavailability of most poorly water-soluble drugs and macromolecular drugs (> 1000 g/mol) is low and the therapeutic effect is unsatisfactory (2). Especially for protein and peptide drugs (PPDs), the oral bioavailability is usually less than 1% due to their large molecular weight, instability in digestive juice and poor membrane penetration (3). Therefore, oral formulations need to overcome these problems to achieve successful drug delivery (4, 5). A variety of strategies have been proposed to improve oral drug absorption (6), including lipid-based delivery systems, polymer nanoparticles (7,8,9,10), nano-drug crystals (11), polymer micelles (12, 13), liposomes (14) and self-emulsifying drug delivery systems (SEDDS) (15), etc. Despite great efforts, only a few of them have been successfully translated (16). Notably, oral PPDs are still blank in clinical practice except for the oral dosage form of sermaglutide approved by FDA in 2019 (17). However, the success of oral delivery of semaglutide is difficult to replicate since the enteric permeation enhancer used in this formulation, salcaprozate sodium, is not applicable to more PPDS (18). Novel materials or strategies still need to be explored to improve the oral bioavailability of drugs.
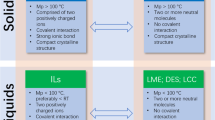
Fortunately, ionic liquids (ILs) have attracted extensive research interest as alternatives to traditional oral drug delivery systems (DDS) due to their excellent ability to enhance the solubility, stability and permeability of drugs. ILs are a class of organic salts that are usually liquid at temperatures below 100 °C. ILs that exist in the liquid state at room temperature are termed room-temperature ILs. The low melting point of ILs is achieved by the presence of bulky and asymmetric organic cations and organic/inorganic anions in the structure (19). Notably, ILs have many distinctive features such as excellent electrical conductivity, high thermal stability, extremely low volatility, reduced vapor pressure, amazing solubilizing ability and tunability. More importantly, the properties of ILs such as melting point, viscosity, electrical conductivity and even cytotoxicity are tunable, and can be tailored by selecting different ionic components (20). The properly designed ILs can have task-specific functionalities or impart specific biological activities that enable their use as a solubilizer of poorly soluble active pharmaceutical ingredients (API) (21), skin penetration enhancer (22), antibacterial agents (23), macromolecular stabilizer (24), and other biomedical field. Especially, ILs exhibit distinct properties that are not generally achievable with common delivery vehicles, and show promising application potential for oral drug delivery. ILs have both the ability to enhance the solubility and permeability of drugs, as well as improve drug stability in the gastrointestinal tract, and improve drug penetration through mucus and intestinal epithelial cells (25,26,27). Using ILs can overcome multiple barriers that are not conducive to drug absorption and improve oral bioavailability of drugs, while conventional formulations often only help to address one or two of these challenges associated with the oral route. Furthermore, in pharmaceutical formulations, ILs can perform multiple roles so that the use of ILs alone can replace several excipients and make formulations more effective and less costly. ILs have been attempted as formulation components to develop novel oral DDS, such as neat ILs-drug preparations (26), formation of API based ILs (API-ILs) (28), microemulsions and nanoemulsions (29), thermoresponsive gels (30), and polymers conjugation or combination formulation (31). ILs have gradually gained attention in applications for oral drug delivery.
This article reviewed the application progress of ILs in oral delivery of small molecular drugs and PPDs, focusing on underlying mechanisms of improving the drug physicochemical properties and enhancing drug delivery across physiological barriers (Fig. 1). And the current challenges and prospects are also discussed.
MECHANISMS OF ORAL DRUG DELIVERY OF ILs
ILs Enhance Drug Solubility and Stability
ILs have been widely used to increase the solubility of poorly soluble compounds, mainly by forming new interactions with solute molecules and destroying the original forces to promote solute integration (32). The multiple hydrogen bonds formed between the cations and anions of ILs and the drugs are an important mechanism for drug molecules to dissolve in ILs (33, 34). Dasari et al. (35) reported that lassbio-294, a cardiovascular drug with poor water solubility, could be successfully dissolved in imidazole ILs. Experiments and molecular dynamics simulations proved that the mechanism of drug dissolution was attributed to the formation of hydrogen bonds between anions [CH3COO-] of ILs and the drug. In another study, the increased solubility of glyburide in ILs composed of choline and tryptophan was found to be closely related to the formation of complex hydrogen bonds and π-π interactions between aromatic rings (36).
ILs Enhance Drug Stability
Low pH environment (pH = 1.5–3.5) in stomach often causes irreversible protein denaturation and provides an environment with the best active state of pepsin, which may degrading drugs (37). When considering oral delivery, the stability of macromolecular drugs is a priority. Oral preparations must be able to withstand the acidic environment and proteases in gastrointestinal tract. Amazingly, ILs are excellent storage stabilizers for macromolecular drugs, and they also have been proved to be able to protect the PPDs from gastric acid as well as digestive enzymes. The stability of a variety of protein drugs in ILs has been determined, such as insulin (26), monoclonal antibodies (38), stem bromelain (39, 40), and lysozyme (41), etc. With the changes of ILs anion and cation pair composition (39, 40) and ILs concentration (42), unique ILs solution structure (nanoheterogeneous) also changed, which were strongly correlated to the differences in the PPDs stability. In addition, ILs can form a tight shell around solvated protein, preventing its aggregation (43), and also promote the folding of the secondary structures, reducing the aggregation of PPDs (44). The interactions between ILs and macromolecular drugs are still unclear (32). Through molecular dynamics simulation, Palanisamy et al. explained the interaction mechanism between CAGE and insulin in different concentrations of CAGE aqueous solution (45). In their study, when the concentration was below 0.5 mol fraction, geranic acid mainly provided hydrogen bonds, gradually decreasing the water molecules around insulin, thereby reducing the conformational shift of insulin. There was no significant change in the secondary conformation of insulin. In the study of CAGE was used for oral insulin delivery, Banerjee et al. demonstrated that CAGE protects insulin from enzymatic degradation (26). In another study, CAGE has been proved to be able to inhibit the activity of dipeptidyl peptidase-4 which degrades glucagon-like peptide-1 (GLP-1), thereby improving the stability of GLP-1 (46).
ILs Enhance Drug Diffusion in Gastrointestinal Mucosa
The high-viscosity mucus layer of the GI tract effectively reduces the diffusion of drugs in the mucus and lower the retention time of drugs in GI tract, which is not conducive to the oral absorption (32). Mucin is the main functional component of the mucus layer and plays an important role in the mucus layer. Due to its brush-like structure, it effectively reduces the mobility of drugs and slows down the diffusion of drugs (47). Moreover, mucin fibers interact with the drug through van der Waals force, electrostatic force, and hydrophobic interaction to affect the drug structure (48). Peng et al. explored the interaction between choline based ILs and gastrointestinal mucus (49), found that choline based ILs can enhance the diffusion of macromolecular drugs in gastrointestinal mucus, and believed that choline plays an important role. By comparing the properties of the mucus layer, the possible explanation is that the positive charge of choline can effectively shield the negative charge of mucin glycoprotein in the mucus layer. Furthermore, ILs with higher conductivity have a greater impact on the viscosity of the mucus layer, because they are more conducive to the dissociation of anions and cations in the mucus layer, thereby dispersing the mucin polymer (49). In addition, compared with other mucus-modulating agents choline based ILs have no significant effect on native mucus gel structure, indicating their biocompatibility.
ILs Enhance Drug Intestinal Epithelium Transport
The intestinal epithelium is the last and most important barrier affecting drug absorption (48, 50). ILs can enhance intestinal epithelial transport of drugs by enhancing the fluidity of cell membranes, disrupting cell membrane integrity, or opening tight junctions between cells. Banerjee et al., found that hydrophilic IL CAGE enhanced insulin transepithelial transport, which was further verified by the CAGE concentration-dependent enhanced permeability of both paracellular permeability markers Lucifer yellow and fluorescein isothiocyanate (FITC)-dextran (26). In contrast, even at low concentrations, CAGE decreased the transcellular uptake of coumarin-6, which was a fluorescent marker for passive transcytosis. Therefore, CAGE can enhance insulin transport through paracellular route. In another research, Lim et al. found that 1-octyl-3-methylimidazolium cation (OMIM+) in amphiphilic ILs can insert into the cell membrane and coordinate with the negatively charged phospholipid group to form the structure of OMIM+-phosphate-OMIM+, which makes the fatty acid structure disordered, and the cell membrane is thinned by 0.6 nm (51). This enables ILs to facilitate the permeation of small molecules across membranes, such as a dramatic seven-fold increase in the permeability coefficient of cell membranes to ammonia. However, it is worth noting that the property of ILs to enhance drug permeability often brings about toxicity-related events. Rational design of ILs with high safety and high performance is one of the current research hotspots.
ORAL DELIVERY APPLICATION OF ACTIVE PHARMACEUTICAL INGREDIENTS BASED ILs (API-ILs)
Conversion to salt is usually an effective approach to overcome the unsatisfactory physicochemical properties of drugs. Approximately 50% of marketed drugs are supplied in salt form. However, the most significant problem of the solid form of drugs is crystal polymorphism. Using ILs technology, by pairing appropriate ions and fabricating API-ILs, the required drug properties can be finely tuned. API-ILs are novel molten salts that formed by the combination of the basic or acidic API and counterions, or two different APIs (52). At present, API-ILs have shown surprising effects to overcome the low solubility, insufficient stability, polymorphism and poor oral bioavailability of drugs. The hydrogen bonding and weak Coulomb force formed between cations and anions makes melting points of API-ILs lower, the lattice energies weaker, alleviating the polymorph formation, thus solving the problems of solubility, stability and bioavailability of API (34, 53). In addition, a wise choice of counterion with biological activity will enable API-ILs to have dual pharmacological activities and possibly produce a combination of compounds with synergistic effects (54). For example, compared with lidocaine hydrochloride, lidocaine docusate (an API-ILs) has a longer analgesic effect (54).
API-ILs Composed of Weakly Basic API and Counterions
Weakly basic API that are poorly water-soluble can be converted into API-ILs by pairing with lipophilic anions. In 2013, API-ILs was first reported for oral delivery by combining the cationic drug amitriptyline hydrochloride (AH) and the anionic surfactant sodium dodecyl sulfate (SDS) to prepare AH-SDS ILs (55). AH-SDS ILs can self-assemble into 342 nm-sized vesicles in water. The loading efficiency of AH in AH-SDS ILs was 57.7%. Compared with AH, AH-SDS ILs had a prolonged release profile and improved permeability in intestinal epithelium in vitro, and a smaller Cmax and a higher 72 h-post-dose concentration in vivo after oral administration in rabbits.
Currently, API-ILs are mostly used as formulation components to develop oral SEDDS to overcome the insufficient solubility of drug and enhance the stability of the formulation. It was reported that through the metathesis reaction, three weakly basic poorly water-soluble drugs, itraconazole (Itz), cinnarizine (Cin), and halofantrine, were converted into API-ILs by interacting with a series of lipophilic counterions (decylsulfate (DS), triflimide (Trim), docusate (Dos), oleate, niaproof). The resulted API-ILs can be highly soluble in SEDDS at a ratio of 1:1 w/w, and the solubility of Cin-DS and Itz-Dos in SEDDS was increased by about 7-fold and 50-fold compared with their free base form of SEDDS, respectively. The SEDDS containing Cin-Trim and Itz-Dos significantly increased plasma exposure of Cin (2-fold) and Itz (20-fold) compared with drug suspensions (56). API-ILs based on the weakly basic drug atazanavir (ATV) was reported using two lipophilic counterions to prepare the lipophilic salt of ATV-2-naphthalene sulfonic acid (ATV-2-NSA) and ATV-dioctyl sulfosuccinic (docusate) acid (ATV-Doc) (41). ATV-2-NSA and ATV-Doc could significantly improve the solubility of ATV in SEDDS, which was 5.7 and 3.7-fold that of ATV free base, respectively. Compared with ATV-Doc SEDDS and free AVT SEDDS, ATV-2-NSA SEDDS has better stability and no precipitation is observed within 30 h even at high concentrations (60 mg/mL). In addition, a rat PK study conducted at this concentration found that the exposure to ATV-2-NSA SEDDS was equivalent to that of ATV free-base solution, but with less variability. In another study, to address the low bioavailability of small molecule kinase inhibitors (smKI) erlotinib, gefitinib, ceritinib and cabozantinib, Williams et al. (57) prepared lipophilic salt-docusate ILs, which were co-administered with lipid-based formulations to improve the absorption of smKI. Compared with free base or commercially available salts, the solubility of API-ILs in the medium-chain SEDDS was significantly enhanced (> 100 mg/g, at least 5-fold that of the free base form). In vivo evaluation results showed that the absolute bioavailability of erlotinib docusate or cabotinib docusate based on SEDDS was significantly improved, approximately 1.5 and 1.8-fold that of free base or marketed salts. The weakly basic drugs and anion used to form API-ILs are shown in Fig. 2.
API-ILs Composed of Weakly Acidic API and Counterions
Similarly, as anionic component, weakly basic API can also be developed into API-ILs. Shadid et al. synthesized cholinium salt of sulfasalazine (Sulfa-ILs) with sulfasalazine and choline chlorided. The solubility of Sulfa-ILs in saline and phosphate buffer (pH 8.0) was about 4000 times and 10 times that of Sulfa in saline, respectively (58). Although Sulfa-ILs could partially precipitate in the simulated gastric fluid and show limited effect in increasing the solubility in simulated intestinal fluid, the oral absolute bioavailability of Sulfa-ILs in rats could be increased by about 2.5 times compared with the Sulfa-PM suspension (1:1 sulfa:choline mixture). Moshikur et al. developed a series of API-ILs based on the weakly acidic drug methotrexate (MTX). In this work, MTX was used as the anionic component and choline, tetramethylammonium, tetrabutylphosphine or proline ethyl ester (ProEt) as the cationic component (59). The experimental results showed that compared with MTX, IL[ProEt][MTX] exhibited better pharmacokinetic properties, its oral bioavailability was 4.6 times higher, and the accumulation of MTX in the lung, spleen, kidney and gastrointestinal tract was significantly reduced. In vivo antitumor studies further confirmed the improved efficacy of IL[ProEt][MTX] in inhibiting tumor growth. In another oral drug delivery study, weakly acidic and insoluble drugs tolfenamic acid (Tolf), meclofenamic acid, diclofenac and ibuprofen were respectively paired with counterions to form API-ILs to enhance drug dissolution in SEDDS. The prepared API-ILs had high solubility in SEDDS at ratio of 1:1 w/w. At high doses (100 mg/kg), the SEDDS preparation of Tolf ILs had a smoother, longer plasma exposure curve and decreased Cmax compared with free drugs (60). The weakly acidic drugs and cations used to form API-ILs are shown in Fig. 3.
API-ILs Composed of Weakly Basic API and Weakly Acidic API
Dual-active API-ILs synthesized from weakly acidic drugs and weakly basic drugs enables the co-delivery of these two drugs on the same platform. Clinically, diphenhydramine (DPH) is often used in combination with ibuprofen (IBU) or naproxen (NAP) for patients with sleep disorders with pain. Wang et al. (61) prepared proton ILs (DPH][IBU] PILs and [DPH][NAP] PILs) by pairing DPH with IBU or NAP to improve the poor solubility of IBU and NAP. The results showed that after formation of API-ILs, the solubility of IBU and NAP increased by about 7-fold and 9-fold, respectively. Subsequently, to further improve the problem of poor dissolution of PILs, [DPH][IBU] PILs and [DPH][NAP] PILs were dispersed into mesoporous silica, and the PILs-carrier composite showed improved dissolution and prolonged drug release and significantly improved bioavailability. The DPH and IBU or NAP used to form API-API are shown in Fig. 4.
DPH and IBU or NAP used to form API-API in oral DDS (61).
API-ILs, as a liquid salt, is an attractive way to overcome drugs polymorphism, poor solubility and poor absorption problems to improve drug therapeutic effect. Not only drugs in the cationic or anionic form can be made into API-ILs, but poorly ionizable or non-ionizable drugs can also be made into API-ILs by introducing ionizable functional groups to prepare prodrugs. In addition, there are thousands of counterions to choose from, and the judicious selection of counterions can produce synergistic effects with APIs, or enable API-ILs to have multiple pharmacological activities. Therefore, API-ILs has shown great potential in oral drug delivery. However, the application of API-ILs in oral DDS is still in its infancy, and more in-depth studies are required to fully understand and utilize API-ILs. In addition, the stability of API-ILs in the GI tract and its impact on the gut flora also deserve explore.
ILs BASED ORAL DDS FOR SMALL MOLECULE DRUGS
Poor solubility is the main challenge in the clinical application of BCS class II and BCS class IV drugs. According to statistics, 40% of marketed drugs and up to 70% of potential drug candidates exhibit extremely poor oral bioavailability due to water insolubility (62,63,64,65). ILs, known as "green solvent and super solvent", showed great application potential in dissolving drugs in place of volatile and toxic traditional solvents. The development of ILs-based oral DDS to overcome the solubility problem of BCS class II drugs was reported by Williams et al. for the first time (66). They prepared two kinds of ILs firstly, 1-hexyl-3-hexyloxy-carbonylpyridinium bis(trifluoromethylsulfonyl)imide ([hhcpy][NTf2]) and 1-hexyl-3-hexyloxy-carbonylpyridinium dicyanamide([hhcpy][N(CN)2]), and found that, compared with soybean oil, [hhcpy][NTf2] and [hhcpy][N(CN)2] could increase the solubility of danazol, itraconazole and fenofibrate by 5.5, 100, 1.7 times and 100, 500, 1.7 times, respectively. Then, in order to reduce the risk of drug precipitation caused by ILs miscible with water in vivo, they further studied another two1-methyl-3-octylpyridinum alkyl sulfate ILs ([C8mβpy][C10SO4] and [C8mβpy][C18SO4]). Finally, they prepared SEDDS with ILs instead of lipids to overcome the insufficient solubility of danazol in the formula. The result showed that the oral bioavailability of SEDSSC18SO4 in rats was 4.3 times that of danazol suspension, and was equivalent to SEDDSlipid. Notably, compared with that of SEDDSlipid, pharmacokinetic parameters of SEDDSC18SO4 including the plasma concentration and drug exposure time were much better. It was speculated that the related mechanism might be that ILs DDS enabled better interaction of danazol with endogenous bile salt micelles, resulting in markedly dispersed species that can be better absorbed.
ILs composed of amphiphilic ions showed excellent ability to improve drug solubility and great potential for oral delivery. Amphiphilic ions of these ILs have a synergistic effect on improving drug solubility. The hydrophobic part, can accumulate around the solute, and there is no counterion that strongly interacts with water, limiting the degree of solute-hydrotrope aggregation. Choline, an important component of cell membrane with low toxicity and high biodegradability, is a hydrophilic cation which can be paired with hydrophobic molecules to synthesize third-generation ILs with excellent dissolving ability (34). Sintra et al. reported that both cholinium vanillate and cholinium gallate based ILs were able to increase the solubility of ibuprofen by up to 500-fold, while cholinium salicylate based ILs could enhance ibuprofen’s solubility by up to 6000-fold, and all these three choline based ILs could increase naproxen’s solubility by up to 600-fold when compared with pure water (67).
Moreover, ILs formed by anions with different charge numbers showed a certain difference in solubilization ability. Based on choline and phosphate, Agostinho et al. (68) prepared five monoanionic and five dianionic ILs and found that dianionic ILs had a stronger solubilizing effect than monoanionic ILs. The solubility of ibuprofen and piroxicam could be increased by 300-fold and 480-fold with 0.25 mol% dianionic ILs, respectively, while 0.3 mol% monoanionic ILs could only increase the solubility by tenfold. In another study, Shi et al. (69) found that the ILs based choline and geranate (CAGE, a composition with choline: geranic acid stoichiometry of 1:2) markedly increased the solubilityand oral bioavailability of sorafenib (SRF). The results showed that the apparent solubility of SRF tosylate in CAGE was 100 million times higher than that in water. Notably, the solubility of SRF in 10% CAGE was still 221-fold that of water. Following oral administration of SRF-CAGE in rats, the peak plasma concentration and elimination half-life of SRF were increased by 2.2-fold and 2-fold, respectively, and the average absorption time was prolonged by 1.6-fold compared with SRF suspension formulation. After 80 times dilution of SRF-CAGE with water or PBS (pH 7.4), nanocomplexes were formed, which may be the mechanism by which of CAGE promote SRF oral absorption (Fig. 5). In further experiments, Shi et al.(70)demonstrated that CAGE could significantly enhance the anti-tumor effect of SRF on 4T1 cells and Caco2 cells by increasing apoptosis and blocking cell cycle progression.
ILs can improve drug permeability by enhancing transmembrane capacity, which is important for oral delivery of BCS class IV and III drugs. Eleni et al. used ILs (1-Butyl-3-methylimidazolium hexafluorophosphate, 1-Butyl-3- methylimidazolium tetrafluoroborate and 1-Hexyl-3-methylimidazolium chloride (HMIMCl)) in combination with a lipid-based formulation (self-nano-emulsifying drug delivery systems (SNEDDS), ILs:SNEDDS = 3:7) to improve the oral bioavailability of BCS IV drug amphotericin B (AmpB) (71). The results showed that ILs not only significantly improved the solubility of AmpB, but also increased the transport of AmpB across Caco-2 cell monolayer. The AmpB transport amount in the SNEDDS:HMIMCl group was more than three times that of the SNEDDS group. In another study, Shi et al. proved that CAGE enhanced SRF penetration and crossing over multicellular structures and the efficacy of SRF on these cells (70).
ILs BASED VARIOUS ORAL DELIVERY SYSTEMS FOR PROTEIN AND PEPTIDE DRUGS
Direct Dispersion and Oral Delivery of Insulin by Neat ILs
Initially, neat ILs were used for transdermal delivery of proteins. Banerjee et al. (22) firstly demonstrated the effectiveness of the topical transdermal application of CAGE by simply mixing neat choline-geranate (CAGE) and various proteins (bovine serum albumin, ovalbumin and insulin), demonstrating that CAGE could stabilize macromolecular drugs and assist macromolecular drugs to cross the skin barrier. Then they further successfully delivered insulin orally using CAGE (26), even though the intestinal epithelial barrier environment was more complicated than that of the skin (72, 73). As shown in Fig. 6, CAGE significantly enhanced the oral bioavailability of insulin, resulting in a 40% decline of blood glucose levels in rats, due to its excellent ability to protect protein from proteolytic enzymes and promote insulin penetrate through the mucus membrane by opening tight connections. Besides, Insulin-CAGE was stable for 2 months at RT and at least 4 months at 4 °C as assessed through secondary structure and in vivo bioactivity evaluation. CAGE provides a stable environment for protein, probably due to modifications of water structure around the protein and interactions with charged residues on the protein surface (74, 75). Consisting only of insulin and an ionic liquid, Insulin-CAGE is a simple and robust formulation that can be effortlessly prepared in a single-step process, and requires no structural modification of insulin and no additional excipients to enhance efficacy (26). Thus, it precludes the generation of an immune response to modified protein or the loss of active ingredients during preparation. Taken together, neat ILs appear to play a great role in the oral delivery of proteins.
Neat ILs for Oral Delivery of Insulin (26) a The structures of CAGE. b Circular dichroism spectra of insulin isolated from CAGE at different months. c Blood glucose lowering efficacy of various formulations compared with initial levels. d Blood glucose changes after normalizing for fasting effect related blood glucose changes. Reproduced with the permission from Ref. 26. Copyright © 2018 National Academy of Sciences.
Ionic Liquid Gel for Oral Delivery of Insulin
ILs can also be added to different prescriptions to meet different delivery needs. As shown in Fig. 7, to address the issue of poor liquid localization in the GI environments, Peng et al. prepared ionic liquid gel patches for oral delivery of insulin (49, 76). They demonstrated that the “ionogel” CAGE-patches were a novel and simple approach which could encapsulate ILs and drugs in a gel. Due to their adjustable properties, ILs could be easily mixed into PVA aqueous solutions and dried or subjected to repeat freeze and thaw cycles to obtain ionic liquid gel patches. Due to the slow-release characteristics of the gel, about 40% of the loaded insulin was released within 5 h, and CAGE had a similar release behavior, suggesting that ILs are compatible in different systems. This novel IL gel approach allows localized and controlled release of ILs and drugs in the GI tract for enhanced oral delivery.
Ionic Liquid Aqueous Solution for Oral Delivery of Monoclonal Antibody
Encouraged by the ability of CAGE in the stabilization and successful oral delivery of insulin, Angsantikul et al. attempted to dissolve therapeutic monoclonal antibodies in ILs aqueous solution for oral delivery. As shown in Fig. 8, they prepared choline-glycolate (CGLY) and assessed the effects of CGLY on antibody stability, in vitro transport, and in vivo uptake (38). Compared with insulin (5.8kda), antihuman TNF-α mouse IgG1(150kda) had a larger molecular weight and a more complicated structure, presenting greater challenges to successful oral administration. Firstly, they screened different concentrations and types of CGLY for their ability to bind monoclonal antibodies and found that the excess glycolic acid in the prescription was detrimental to maintaining antibody integrity, resulting in a formulation of CGLY (2:1). Under the premise of ensuring the structural activity of the antibody, the plasma IgG level in CGLY-IgG group was five-fold higher than that of control group 5 h after administration. Mechanism studies had shown that CGLY could enhance the permeation of IgG through intestinal mucus and epithelium.
Ionic liquid aqueous solution for oral delivery of IgG (38) a Chemical structures of choline and glycolic acid. CGLY variants (choline:glycolic acid molar ratios of 2:1, 1:1, and 1:2) were prepared by salt metathesis of choline bicarbonate and glycolic acid. b Retained antigen binding capability of antihuman TNF-α mouse IgG1 antibody (clone MAb11) isolated from CGLY variants at a concentration range between 20 and 90%v/v. c Fluorescence quantification of FITC-IgG per unit area on villi. d In vivo plasma antihuman TNF-α IgG concentration after intrajejunal injection of the IgG in CGLY2:1 or saline, quantified by ELISA. Reproduced with the permission from Ref. 38. Copyright © 2020 John Wiley and Sons.
Ionic Liquid Functionalized Silica Nanoparticles for Oral Delivery of Insulin
Chemical modification is a commonly used method for drug delivery, which can improve performance and endow the carrier the functions suitable for oral delivery (77).Therefore, Mahkam et al. modified the imidazole group on SiO for oral delivery of insulin (78). At pH 1.0, which was the pH of gastric acid, the Si–O group was protonated. Therefore, the positive charge of the imidazole group made the insulin molecules electrostatically attracted, increasing the drug load of insulin. At neutral pH, the pH of the gut, Si–O was deprotonated and carried a large amount of negative charge, repelling the insulin molecule and allowing insulin release. It provides a new way to improve the solubility of macromolecular drugs.
In summary, ILs were attempted as formulation components to develop various novel oral drug delivery systems for macromolecules. The liquid form of ILs facilitates their smooth addition, and its unique ionic and hydrogen bonds make it dissolve well in different formulations. However, at present, there are only few studies on the application of ILs in oral delivery macromolecular drugs, and most of which are studies on oral delivery of insulin molecules. Research on other macromolecular drugs needs to be expanded urgently. We believe that the application potential of ILs for oral delivery of macromolecules remains to be explored.
CHALLENGES
Although exciting study results were elucidated, many challenges remain in the application of ILs for the development of oral DDS. Firstly, the study of ILs based oral DDS lacks systematic and still in its initial stage. Current studies mainly focus on observing the effects of ILs on drug solubility, permeability and oral bioavailability, lacking evaluation of therapeutic efficacy and in vivo safety. Secondly, although ILs is considered a green solvent with low vitality and low toxicity compared with traditional solvents, its safety remains challenged in biomedical applications especially for systemic administration. The cytotoxicity and microbial toxicity of the first- and second-generation ILs make their development in drug delivery a challenge. The development of third-generation ILs with better biocompatibility has greatly improved the safety of ILs, but long-term toxicity studies are still needed. Thirdly, ILs have been reported to have the ability to enhance the penetration of drugs through gastrointestinal barriers, including mucus and epithelial barriers, which may be related to the cations of ILs, but the specific mechanism remains unclear. Correctly understanding the mechanism will help researchers better understand ILs and design ILs more rationally. Fourthly, the ionizable ions of ILs face different pH changes in the GI tract, which will lead to ILs instability and drug precipitation. Therefore, improving the stability of ILs in the GI tract and reducing the risk of drug precipitation are also urgent problems to overcome in the application of ILs for oral administration. Finally, the lack of a recognized regulatory system for the application of ILs in oral DDS is also a major constraint on ILs development (52). However, with the further development of ILs, regulatory loopholes will gradually be overcome. MRX-7EAT, an API-ILs patch, is currently the only ILs preparation that has entered clinical trials for transdermal delivery but terminated due to unsatisfactory treatment effects. The successful transformation of ILs preparation into clinical practice still faces great challenges. The great potential of ILs in improving the efficiency of oral drug delivery and therapeutic effect means that ILs is a promising vector and worth exploring.
PERSPECTIVES
Overall, ILs have unprecedented advantages in improving the oral absorption of drugs, and are very promising carriers for oral delivery, which will definitely attract more researchers to conduct in-depth studies. With the development of application research of ILs in oral delivery, the deeper mechanisms will be elucidated, and the structure–activity relationship between ILs and their safety and delivery efficacy will be expounded, which will be conducive to the design of safer and more efficient ILs. Furthermore, clinical studies on tailored biocompatible ILs are expected to begin in the near future to facilitate successful market translation of IL-based DDS.
Abbreviations
- AmpB:
-
Amphotericin B
- API:
-
Active pharmaceutical ingredients
- ATV:
-
Atazanavir
- ATV-2-NSA:
-
Atazanavir-2-naphthalene sulfonic acid
- ATV-Doc:
-
Atazanavir-dioctyl sulfosuccinic (docusate) acid
- CAGE:
-
ILs based choline and geranic acid
- CGLY:
-
Choline-glycolate
- Cin:
-
Cinnarizine
- DDS:
-
Drug delivery systems
- Dos:
-
Docusate
- DPH:
-
Diphenhydramine
- DS:
-
Decylsulfate
- FITC:
-
Fluorescein isothiocyanate
- GI:
-
Gastrointestinal
- GLP-1:
-
Glucagon-like peptide-1
- HMIMCl:
-
1-Hexyl-3-methylimidazolium chloride
- [hhcpy] [N(CN) 2]:
-
1-Hexyl-3-hexyloxy-carbonylpyridinium dicyanamide
- [hhcpy] [NTf 2]:
-
1-Hexyl-3-hexyloxy-carbonylpyridinium bis(trifluoromethylsulfonyl)imide
- IBU:
-
Ibuprofen
- ILs:
-
Ionic liquids
- Itz:
-
Itraconazole
- NAP:
-
Naproxen
- PILs:
-
Proton ionic liquids
- PPDs:
-
Protein peptide drugs
- SEDDS:
-
Self-emulsifying drug delivery systems
- SmKI:
-
Small molecule kinase inhibitors
- SNEDDS:
-
Self-nano-emulsifying drug delivery systems
- SRF:
-
Sorafenib
- Tolf:
-
Tolfenamic acid
- Trim:
-
Triflimide
References
Brown TD, Whitehead KA, Mitragotri S. Materials for oral delivery of proteins and peptides. Nature Reviews Materials. 2019;5.
Devadasu VR, Deb PK, Maheshwari R, Sharma P, Tekade RK. Physicochemical, Pharmaceutical, and Biological Considerations in GIT Absorption of Drugs - ScienceDirect. Dosage Form Design Considerations. 2018:149–178.
Zhu Q, Chen Z, Paul PK, Lu Y, Wu W, Qi J. Oral delivery of proteins and peptides: Challenges, status quo and future perspectives. Acta Pharm Sin B. 2021;11(8):2416–48.
Buckley ST, Baekdal TA, Vegge A, Maarbjerg SJ, Pyke C, Ahnfelt-Ronne J, Madsen KG, Scheele SG, Alanentalo T, Kirk RK, Pedersen BL, Skyggebjerg RB, Benie AJ, Strauss HM, Wahlund PO, Bjerregaard S, Farkas E, Fekete C, Sondergaard FL, Borregaard J, Hartoft-Nielsen ML, Knudsen LB. Transcellular stomach absorption of a derivatized glucagon-like peptide-1 receptor agonist. Sci Transl Med. 2018;10(467).
Niu ZG, Samaridou E, Jaumain E, Coene J, Ullio G, Shrestha N, Garcia J, Duran-Lobato M, Tovar S, Santander-Orteg MJ, Lozano MV, Arroyo-Jimenez MM, Ramos-Membrive R, Penuelas I, Mabondzo A, Preat V, Teixido M, Giralt E, Alonso MJ. PEG-PGA enveloped octaarginine-peptide nanocomplexes: An oral peptide delivery strategy. J Control Release. 2018;276:125–39.
Sun M, Hu H, Sun L, Fan Z. The application of biomacromolecules to improve oral absorption by enhanced intestinal permeability: A mini-review. Chin Chem Lett. 2020;31(7):1729–36.
Zhou S, Deng H, Zhang Y, Wu P, He B, Dai W, Zhang H, Zhang Q, Zhao R, Wang X. Thiolated Nanoparticles Overcome the Mucus Barrier and Epithelial Barrier for Oral Delivery of Insulin. Mol Pharm. 2020;17(1):239–50.
Wang XQ, Zhang Q. pH-sensitive polymeric nanoparticles to improve oral bioavailability of peptide/protein drugs and poorly water-soluble drugs. Eur J Pharm Biopharm. 2012;82(2):219–29.
Zhang Y, Ding S, Li J, Peng X, Li J, Chang J, Gao W, He B. In vivo formation of Cu (DDC) 2 complex induced by nanomedicine for mesothelioma chemotherapy. Chin Chem Lett. 2020;31(12):3168–72.
He M, Yu L, Yang Y, Zou B, Ma W, Yu M, Lu J, Xiong G, Yu Z, Li A. Delivery of triptolide with reduction-sensitive polymer nanoparticles for liver cancer therapy on patient-derived xenografts models. Chin Chem Lett. 2020;31(12):3178–82.
Chen Z, Wu W, Lu Y. What is the future for nanocrystal-based drug-delivery systems? Ther Deliv. 2020;11(4):225–9.
Chen T, Tu L, Wang G, Qi N, Wu W, Zhang W, Feng J. Multi-functional chitosan polymeric micelles as oral paclitaxel delivery systems for enhanced bioavailability and anti-tumor efficacy. Int J Pharm. 2020;578:119105.
Hu Q, Bai L, Zhu Z, Su Z, Bai P, Tang M, Dou C, Yan J, Tong R, Zhang W. β-Elemene-loaded polymeric micelles intensify anti-carcinoma efficacy and alleviate side effects. Chin Chem Lett. 2020;31(3):915–8.
He H, Lu Y, Qi J, Zhu Q, Chen Z, Wu W. Adapting liposomes for oral drug delivery. Acta Pharm Sin B. 2019;9(1):36–48.
Abou Assi R, I MA, Seok Ming T, Siok Yee C, H AW, Asif SM, Darwis Y. Liquid and Solid Self-Emulsifying Drug Delivery Systems (SEDDs) as Carriers for the Oral Delivery of Azithromycin: Optimization, In Vitro Characterization and Stability Assessment. Pharmaceutics. 2020;12(11).
Ghadi R, Dand N. BCS class IV drugs: Highly notorious candidates for formulation development. J Control Release. 2017;248:71–95.
Moroz E, Matoori S, Leroux J-C. Oral delivery of macromolecular drugs: Where we are after almost 100 years of attempts. Adv Drug Deliv Rev. 2016;101:108–21.
Twarog C, Fattah S, Heade J, Maher S, Fattal E, Brayden DJ. Intestinal Permeation Enhancers for Oral Delivery of Macromolecules: A Comparison between Salcaprozate Sodium (SNAC) and Sodium Caprate (C10). Pharmaceutics. 2019;11(2):78.
Seddon RDRKR. Ionic Liquids—Solvents of the Future? science. 2003.
Egorova KS, Gordeev EG, Ananikov VP. Biological Activity of Ionic Liquids and Their Application in Pharmaceutics and Medicine. Chem Rev. 2017;117(10):7132–89.
Li X, Ma N, Zhang L, Ling G, Zhang P. Applications of choline-based ionic liquids in drug delivery. Int J Pharm. 2022;612:121366.
Banerjee A, Ibsen K, Iwao Y, Zakrewsky M, Mitragotri S. Transdermal Protein Delivery Using Choline and Geranate (CAGE) Deep Eutectic Solvent. Adv Healthcare Mater. 2017;6(15):1601411.
Messali M, Moussa Z, Alzahrani AY, El-Naggar MY, ElDouhaibi AS, Judeh ZMA, Hammouti B. Synthesis, characterization and the antimicrobial activity of new eco-friendly ionic liquids. Chemosphere. 2013;91(11):1627–34.
Ishikawa Y, Takekiyo T, Yoshimura Y. Recovery and cryopreservation of insulin amyloid using ionic liquids. J Mol Liq. 2018;272:1019–24.
Guncheva M, Idakieva K, Todinova S, Yancheva D, Paunova-Krasteva T, Ossowicz P, Janus E. Structural, Thermal, and Storage Stability of Rapana Thomasiana Hemocyanin in the Presence of Cholinium-Amino Acid-Based Ionic Liquids. Molecules. 2021;26(6).
Banerjee A, Ibsen K, Brown T, Chen RW, Agatemor C, Mitragotri S. Ionic liquids for oral insulin delivery. P Natl Acad Sci USA. 2018;115(28):7296–301.
Caparica R, Julio A, Fernandes F, Araujo MEM, Costa JG, de Almeida TS. Upgrading the Topical Delivery of Poorly Soluble Drugs Using Ionic Liquids as a Versatile Tool. Int J Mol Sci. 2021;22(9).
Cojocaru OA, Bica K, Gurau G, Narita A, McCrary PD, Shamshina JL, Barber PS, Rogers RD. Prodrug ionic liquids: functionalizing neutral active pharmaceutical ingredients to take advantage of the ionic liquid form. MedChemComm. 2013;4(3):559–63.
Pyne A, Kuchlyan J, Maiti C, Dhara D, Sarkar N. Cholesterol Based Surface Active Ionic Liquid That Can Form Microemulsions and Spontaneous Vesicles. Langmuir. 2017;33(23):5891–9.
Ziolkowski B, Diamond D. Thermoresponsive poly(ionic liquid) hydrogels. Chem Commun. 2013;49(87):10308–10.
Noshadi I, Walker BW, Portillo-Lara R, Sani ES, Gomes N, Aziziyan MR, Annabi N. Engineering Biodegradable and Biocompatible Bio-ionic Liquid Conjugated Hydrogels with Tunable Conductivity and Mechanical Properties. Sci Rep-Uk. 2017;7.
Curreri AM, Mitragotri S, Tanner EEL. Recent Advances in Ionic Liquids in Biomedicine. Adv Sci (Weinh). 2021;8(17):e2004819.
Moniruzzaman M, Tahara Y, Tamura M, Kamiya N, Goto M. Ionic liquid-assisted transdermal delivery of sparingly soluble drugs. Chem Commun (Camb). 2010;46(9):1452–4.
Moshikur RM, Chowdhury MR, Moniruzzaman M, Goto M. Biocompatible ionic liquids and their applications in pharmaceutics. Green Chemistry.
Dasari S, Mallik BS. Solubility and solvation free energy of a cardiovascular drug, LASSBio-294, in ionic liquids: A computational study. J Mol Liq. 2020;301.
Alawi MA, Hamdan II, Sallam AA, Heshmeh NA. Solubility enhancement of glibenclamide in choline–tryptophan ionic liquid: Preparation, characterization and mechanism of solubilization. J Mol Liq. 2015;212:629–34.
Woodley JF. Enzymatic Barriers for Gi Peptide and Protein Delivery. Crit Rev Ther Drug. 1994;11(2–3):61–95.
Angsantikul P, Peng KV, Curreri AM, Chua Y, Chen KVZ, Ehondor J, Mitragotri S. Ionic Liquids and Deep Eutectic Solvents for Enhanced Delivery of Antibodies in the Gastrointestinal Tract. Adv Funct Mater. 2020.
Kumar PK, Jha I, Venkatesu P, Bahadur I, Ebenso EE. A comparative study of the stability of stem bromelain based on the variation of anions of imidazolium-based ionic liquids. J Mol Liq. 2017;246:178–86.
Buchfink R, Tischer A, Patil G, Rudolph R, Lange C. Ionic liquids as refolding additives: Variation of the anion. J Biotechnol. 2010;150(1):64–72.
Morgen M, Saxena A, Chen XQ, Miller W, Nkansah R, Goodwin A, Cape J, Haskell R, Su C, Gudmundsson O, Hageman M, Kumar A, Chowan GS, Rao A, Holenarsipur VK. Lipophilic salts of poorly soluble compounds to enable high-dose lipidic SEDDS formulations in drug discovery. Eur J Pharm Biopharm. 2017;117:212–23.
Takekiyo T, Yamazaki K, Yamaguchi E, Abe H, Yoshimura Y. High Ionic Liquid Concentration-Induced Structural Change of Protein in Aqueous Solution: A Case Study of Lysozyme. J Phys Chem B. 2012;116(36):11092–7.
Constatinescu D, Herrmann C, Weingartner H. Patterns of protein unfolding and protein aggregation in ionic liquids. Phys Chem Chem Phys. 2010;12(8):1756–63.
Attri P, Venkatesu P, Kumar A. Activity and stability of alpha-chymotrypsin in biocompatible ionic liquids: enzyme refolding by triethyl ammonium acetate. Phys Chem Chem Phys. 2011;13(7):2788–96.
Palanisamy K, Prakash M. Molecular Mechanism Behind the Stabilization of Insulin by Choline and Geranate (CAGE) Ionic Liquids - Computational Insights on Oral Insulin Drug Formulation. Phys Chem Chem Phys. 2021.
Agatemor C, Brown TD, Gao Y, Ohmori N, Ibsen KN, Mitragotri S. Choline-Geranate Deep Eutectic Solvent Improves Stability and Half-Life of Glucagon-Like Peptide-1. Advanced Therapeutics. 2021;4(3):2000180.
Zhang X, Cheng HB, Dong W, Zhang MX, Liu QY, Wang XH, Guan J, Wu HY, Mao SR. Design and intestinal mucus penetration mechanism of core-shell nanocomplex. J Control Release. 2018;272:29–38.
Capaldo CT, Powell DN, Kalman D. Layered defense: how mucus and tight junctions seal the intestinal barrier. J Mol Med. 2017;95(9):927–34.
Peng K, Gao YS, Angsantikul P, LaBarbiera A, Goetz M, Curreri AM, Rodrigues D, Tanner EEL, Mitragotri S. Modulation of Gastrointestinal Mucus Properties with Ionic Liquids for Drug Delivery. Advanced Healthcare Materials. 2021;10(13).
Cheng H, Leblond CP. Origin, differentiation and renewal of the four main epithelial cell types in the mouse small intestine. V. Unitarian Theory of the origin of the four epithelial cell types. Am J Anat. 1974;141(4):537–561.
Lim GS, Jaenicke S, Klahn M. How the spontaneous insertion of amphiphilic imidazolium-based cations changes biological membranes: a molecular simulation study. Phys Chem Chem Phys. 2015;17(43):29171–83.
Shamshina JL, Barber PS, Rogers RD. Ionic liquids in drug delivery. Expert Opin Drug Deliv. 2013;10(10):1367–81.
Lee AY, Erdemir D, Myerson AS. Crystal polymorphism in chemical process development. Annu Rev Chem Biomol Eng. 2011;2:259–80.
Hough WL, Smiglak M, Rodríguez H, Swatloski RP, Spear SK, Daly DT, Pernak J, Grisel JE, Carliss RD, Soutullo M. The third evolution of ionic liquids: active pharmaceutical ingredients. New J Chem. 2007;31(8):1429–36.
Zhang L, Liu J, Tian T, Gao Y, Ji X, Li Z, Luan Y. Pharmaceutically active ionic liquid self-assembled vesicles for the application as an efficient drug delivery system. ChemPhysChem. 2013;14(15):3454–7.
Sahbaz Y, Williams HD, Nguyen TH, Saunders J, Ford L, Charman SA, Scammells PJ, Porter CJ. Transformation of poorly water-soluble drugs into lipophilic ionic liquids enhances oral drug exposure from lipid based formulations. Mol Pharm. 2015;12(6):1980–91.
Williams HD, Ford L, Han S, Tangso KJ, Lim S, Shackleford DM, Vodak DT, Benameur H, Pouton CW, Scammells PJ, Porter CJH. Enhancing the Oral Absorption of Kinase Inhibitors Using Lipophilic Salts and Lipid-Based Formulations. Mol Pharm. 2018;15(12):5678–96.
Shadid M, Gurau G, Shamshina J, Chuang B-C, Hailu S, Guan E, Chowdhury S, Wu J-T, Rizvi SA, Griffin R. Sulfasalazine in ionic liquid form with improved solubility and exposure. MedChemComm. 2015;6(10):1837–41.
Moshikur RM, Ali MK, Wakabayashi R, Moniruzzaman M, Goto M. Methotrexate-based ionic liquid as a potent anticancer drug for oral delivery: In vivo pharmacokinetics, biodistribution, and antitumor efficacy. Int J Pharm. 2021;608:121129.
Sahbaz Y, Nguyen TH, Ford L, McEvoy CL, Williams HD, Scammells PJ, Porter CJH. Ionic Liquid Forms of Weakly Acidic Drugs in Oral Lipid Formulations: Preparation, Characterization, in Vitro Digestion, and in Vivo Absorption Studies. Mol Pharm. 2017;14(11):3669–83.
Wang C, Chopade SA, Guo Y, Early JT, Tang B, Wang E, Hillmyer MA, Lodge TP, Sun CC. Preparation, Characterization, and Formulation Development of Drug-Drug Protic Ionic Liquids of Diphenhydramine with Ibuprofen and Naproxen. Mol Pharm. 2018;15(9):4190–201.
Lipinski CA. Poor aqueous solubility - An industry wide problem in drug discovery. American Pharmaceutical Review. 2002;5(3):82–5.
Cooper ER. Nanoparticles: A personal experience for formulating poorly water soluble drugs. J Control Release. 2010;141(3):300–2.
Liu R. Water Insoluble Drug Formulation, Second Edition. Crc Press. 2008(4A):2038.
Rodriguez-Aller M, Guillarme D, Veuthey JL, Gurny R. Strategies for formulating and delivering poorly water-soluble drugs. Journal of Drug Delivery Science & Technology. 2015;30:342–51.
Williams HD, Sahbaz Y, Ford L, Nguyen TH, Scammells PJ, Porter CJ. Ionic liquids provide unique opportunities for oral drug delivery: structure optimization and in vivo evidence of utility. Chem Commun (Camb). 2014;50(14):1688–90.
Sintra TE, Abranches DO, Benfica J, Soares BP, Ventura SPM, Coutinho JAP. Cholinium-based ionic liquids as bioinspired hydrotropes to tackle solubility challenges in drug formulation. Eur J Pharm Biopharm. 2021;164:86–92.
Agostinho DAS, Jesus AR, Silva ABP, Esperanca J, Paiva A, Duarte ARC, Reis PM. Improvement of New Dianionic Ionic Liquids vs Monoanionic in Solubility of Poorly Water-Soluble Drugs. J Pharm Sci. 2021;110(6):2489–500.
Shi Y, Zhao Z, Gao Y, Pan DC, Salinas AK, Tanner EEL, Guo J, Mitragotri S. Oral delivery of sorafenib through spontaneous formation of ionic liquid nanocomplexes. J Control Release. 2020;322:602–9.
Shi Y, Zhao Z, Peng K, Gao Y, Wu D, Kim J, Mitragotri S. Enhancement of Anticancer Efficacy and Tumor Penetration of Sorafenib by Ionic Liquids. Adv Healthc Mater. 2021;10(2):e2001455.
Kontogiannidou E, Meikopoulos T, Gika H, Panteris E, Vizirianakis IS, Mullertz A, Fatouros DG. In Vitro Evaluation of Self-Nano-Emulsifying Drug Delivery Systems (SNEDDS) Containing Room Temperature Ionic Liquids (RTILs) for the Oral Delivery of Amphotericin B. Pharmaceutics. 2020;12(8).
Goldberg M, Gomez-Orellana I. Challenges for the oral delivery of macromolecules. Nat Rev Drug Discovery. 2003;2(4):289–95.
Parry DM, Yaffe P, Duerksen DR. Detecting clinically significant change in serial measurements of intestinal permeability. Clin Chem. 2005;51:A42–3.
Weaver KD, Vrikkis RM, Van Vorst MP, Trullinger J, Vijayaraghavan R, Foureau DM, McKillop IH, MacFarlane DR, Krueger JK, Elliott GD. Structure and function of proteins in hydrated choline dihydrogen phosphate ionic liquid. Phys Chem Chem Phys. 2012;14(2):790–801.
Bisht M, Mondal D, Pereira MM, Freire MG, Venkatesu P, Coutinho JAP. Long-term protein packaging in cholinium-based ionic liquids: improved catalytic activity and enhanced stability of cytochrome c against multiple stresses. Green Chem. 2017;19(20):4900–11.
Peng K, Shi Y, Labarbiera A, Mitragotri S. Mucoadhesive Ionic Liquid Gel Patches for Oral Delivery. ACS Biomaterials Science & Engineering. 2020.
Gupta A, Kushwaha SS, Mishra A. A Review on Recent Technologies and Patents on Silica Nanoparticles for Cancer Treatment and Diagnosis. Recent Pat Drug Deliv Formul. 2020;14(2):126–44.
Mahkam M, Hosseinzadeh F, Galehassadi M. Preparation of Ionic Liquid Functionalized Silica Nanoparticles for Oral Drug Delivery. Journal of Biomaterials and Nanobiotechnology. 2012;03(03):391–5.
Author information
Authors and Affiliations
Contributions
Yujie Shi, Linxia Jiang, Yi Sun, An Lu and Xiangyu Wang were responsible for original draft and visualization. Yujie Shi revised the manuscript. All of the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflicting interests in connection with this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jiang, L., Sun, Y., Lu, A. et al. Ionic Liquids: Promising Approach for Oral Drug Delivery. Pharm Res 39, 2353–2365 (2022). https://doi.org/10.1007/s11095-022-03260-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-022-03260-8