The search for promising substances aimed at creating new chemotherapeutic drugs based on them is relevant in modern oncology. In this regard, new azoloazine derivatives, which are analogs of the well-known anticancer drug temozolomide, may be promising. The goal was to study the antitumor activity of 11 new azoloazine derivatives in vitro and in vivo. The MTT assay was used to assess the cytotoxic effect of the azoloazines on MCF-7 and CHO cells. BALB/c mice were orthotopically injected with 106 MCF-7 cells to simulate a xenogenic model of breast cancer. The test substances were administered at doses 1/2 IC50 once intraperitoneally 72 hours after tumor transplantation. The degree of differentiation and tumor extent in the tissue and the nature of metastasis were studied by analyzing histological sections of animals removed from the experiment. The volume of the primary tumor was measured. An evaluation of the cytotoxic activity of the new azoloazine derivatives showed that compounds 4, 6, and 9 were the most toxic to MCF-7 cells. Therefore, they were selected for cytotoxicity studies on normal cells (cultured CHO cells). Selected compounds 6 and 9 had low cytotoxicity against CHO cells, which was regarded as a positive aspect for their use as anticancer drugs. An in vivo experiment showed that administration of selected compounds 4, 6, and 9 led to more pronounced inhibition of tumor growth than the use of epirubicin alone. Histological analysis also revealed that compounds 4, 6, and 9 exhibited antitumor activity. The antitumor effects of the new azoloazine derivatives obtained in in vitro and in vivo experiments proved their high activity as potential chemotherapeutic agents and their prospects for further studies aimed at creating new antitumor drugs based on them.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Breast cancer (BC) is the most common oncological disease among the female population of Russia and most developed countries. Its incidence and mortality from it are on the rise. About one million new cases of BC are reported each year. According to statistics, BC currently afflicts all age groups, reaching an average of 2.2%; for the 35-54 age group, 7.7% [1].
Currently, the search for new antiblastoma drugs that could be prescribed by oncologists for BC patients is still urgent [2].
Chemical compounds of the azoloazine class, which are isosteres of purine bases, could be interesting derivatives [3]. Researchers at Ural Federal University named after the First Russian President B. N. Yeltsin (Yeltsin URU) synthesized series of imidazo[5,1-c][1,2,4]triazines [10] and imidazo-[5,1-d][1,2,3,5]tetrazin-4-ones that had stable chemical structures and were interesting for assessing their possible use as potential antitumor agents [4].
The goal of the present work was to study the antitumor activity of 11 new azoloazine derivatives in experiments in vitro and in vivo.
Experimental Part
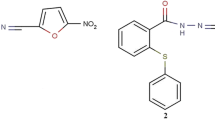
The potential antitumor properties of 11 new azoloazine derivatives were assessed. These were 3-n-propyl-4-oxoimidazo[5,1-d][1,2,3,5]tetrazine-8-carboxylic acid ethyl ester (1), 3-cyclohexyl-4-oxoimidazo[5,1-d][1,2,3,5]tetrazine-8-carboxylic acid ethyl ester (2), 3-n-propyl-4-oxoimidazo-[5,1-d][1,2,3,5]tetrazine-8-N-piperidinylcarboxamide (3), 3-cyclohexyl-4-oxoimidazo[5,1-d][1,2,3,5]tetrazine-8-N-pi-peridinylcarboxamide (4), 5-(p-tolyl)-8-ethoxycarbonylamino pyrazolo[5,1-d][1,2,3,5]thiotriazine (5), 4-aminoimidazo[5,1-c][1,2,4]triazine-3,8-dicarboxylic acid diethyl ester (6), 4-amino-8-ethoxycarbonylimidazo[5,1-c][1,2,4]triazine-3-N-cyclohexylcarboxamide (7), 4-amino-8-ethoxycarbonylimidazo[5,1-c][1,2,4]triazine-3-N-benzylcarboxamide (8), 4-amino-8-ethoxycarbonylimidazo[5,1-c][1,2,4]triazine-3-N-(p-tolyl)carboxamide (9), 3-(3′-phenyl-4′-methoxycar-bonylisoxazolyl)-7-phenylpyrazolo[5,1-c][1,2,4]triazine (10), and 3-(3′-phenyl-4′-methoxycarbonylisoxazolyl)-7-(p-tolyl)-pyrazolo[5,1-c][1,2,4]triazine (11) [4]. The preparation methods, chemical structures, and purities of the tested compounds were published earlier [4]. The compounds were supplied by researchers at Yeltsin UFU for testing of their cytotoxic and antitumor properties.
The MCF-7 breast adenocarcinoma cell line, which is universal and widely used in BC research [5], was selected as the cell culture tumor model in experiments in vitro. CHO, cell culture of epithelium from Chinese hamster ovary, was used to assess the safety of the new pharmacological agents [6].
MCF-7 and CHO cells were thawed, rinsed, and cultivated to a concentration of 104 cells in DMEM medium (100 μL) in a CO2 incubator at 37°C and 5% CO2. The cytotoxic activity of the cells was studied by cultivation with the tested compounds at final concentrations of 0.25, 1.0, 2.5, 5.0, and 10.0 μM. The negative controls were untreated cells; the positive controls, cells treated with epirubicin at analogous concentrations of the tested compounds (0.25, 1.0, 2.5, 5.0, and 10.0 μM). Epirubicin (ZAO Lens, Russia, lyophilizate for preparation of solutions) was selected as the reference drug because it is included in many chemotherapeutic protocols for treating patients with early and progressive/metastatic BC, according to recommendations of the Association of Oncologists of Russia. Plates were incubated for 1 h at 37°C. Cells were separated from the surface using trypsin/EDTA solution (0.25%) and centrifuged. The precipitate was resuspended in Hank’s solution.
The viability of cells in culture was determined using the MTT assay. Cell survival was calculated using the formula:
where ODtest is the average optical density in wells of the test group; ODmed, average optical density in wells with medium; ODc, average optical density in wells with controls.
The concentration of a tested compound at which the maximum suppression of viability vs. the control occurred (Cc/Cmax) was determined.
The concentration of a compound that caused 50% death of cells (IC50) was calculated graphically from a dose-dependent curve using Origin software (OriginLab Corp.). Six parallel observations were made for all compounds at each studied concentration and for the control.
The experiment in vivo was conducted on BALB/c female mice in compliance with bioethical standards given in Rules for Working with Experimental Animals and Directive 2010/63/EU of the European Parliament and the Council of the European Union on Protection of Animals Used for Scientific Purposes.
Xenogenic BC was modeled by three preliminary administrations to the animals of azathioprine at a dose of 1 mg/kg. MCF-7 cells (106) were orthotopically injected in the basal region of the nipple in the initial step [7].
The following experimental groups were included in the experiment:
-
1.
Control, animals injected once intraperitoneally (i.p.) with normal saline (0.2 mL) 72 h after injection of tumor cells.
-
2.
Epirubicin, animals injected once i.p. with epirubicin at a dose 1/2 of IC50 in normal saline (0.2 mL) 72 h after injection of tumor cells.
-
3.
Compound 4, animals injected once i.p. with compound 4 at a dose 1/2 of IC50 in normal saline (0.2 mL) 72 h before injection of tumor cells.
-
4.
Compound 6, animals injected once i.p. with compound 6 at a dose 1/2 of IC50 in normal saline (0.2 mL) 72 h before injection of tumor cells.
-
5.
Compound 9, animals injected once i.p. with compound 9 at a dose 1/2 of IC50 in normal saline (0.2 mL) 72 h before injection of tumor cells.
The animals were housed in a partial barrier system under standard conditions in plastic cages with six animals and access ad libitum to water and feed.
The animals were euthanized on the 15th day. The parts where the tumor cells were injected and the analogous parts from the opposite side were excised. The overall volume of the primary tumor (mm3) was calculated using the equation:
where a is the length of the tumor; b, width of the tumor; and c, height of the tumor.
Tumor growth inhibition (TGI, %) was calculated using the equation:
where A is the average tumor volume in the control group; B, average tumor volume in the test group.
Histological specimens were prepared using a Microm STP 420 tissue processor (Microm, Germany), a Leica EG 1160 embedding station (Leica, Germany), a Leica RM 2255 rotary microtome (Leica, Germany), a Dako CoverStainer (Dako, Denmark), and a Dako Link 48 Immunohistochemistry Autostainer (Dako, Denmark). The immunohistochemistry of animal tumor tissue was evaluated using cytokeratin 8/18 marker (DakoCytomation, Denmark) [8].
Experimental data were statistically processed using the Statistica 10.0 program (Dell, USA). Results were given as Me(Q1; Q3) considering the lack of a normal distribution in sets according to the Shapiro-Wilk criterion. Intragroup comparative analysis used the Kruskal-Wallis criterion (nonparametric ANOVA version) followed by multiple comparisons according to Bonferroni-Dunn. Comparisons among groups used the Mann-Whitney criterion. Differences were considered significant for confidence probability p < 0.05.
Results and Discussion
The search for new types of BC therapy is critical because long-term growth inhibition of it is still not guaranteed although significant progress has been made in treating it [9]. The use of targeted therapy is hindered because BC is heterogeneous [8]. The standard treatment protocols with broadspectrum chemotherapeutic drugs are inadequate and the drugs themselves are rather toxic [10]. These circumstances are the main drivers of the search for promising drugs to create new chemotherapeutic agents based on them [2].
The present work focused on studies of new azoloazine derivatives. Azoloazines are known to possess anti-inflammatory, antioxidant [11], antibacterial, and antifungal activity [12]. Also, their antitumor activity has been reported [13].
The first stage involved screening of 11 new azoloazine derivatives that were synthesized in the Department of Organic Synthesis Technology, Yeltsin UFU, to determine their cytotoxicity against MCF-7 human tumor cells.
An experiment in vitro showed that addition of epirubicin to MCF-7 culture produced a pronounced cytotoxic effect only at the maximum concentration (10 μM) (Fig. 1). The maximum suppression Cc/Cmax was 1.72/0.82 = 2.10. The IC50 value was 9.37 μm.
Only some of the tested compounds demonstrated higher cytotoxic activity than epirubicin. For example, cultivation of MCF-7 with the 11 new azoloazine derivatives showed that compounds 1, 4, 6, 8, and 9 exhibited dose-dependent cytotoxic activity (Fig. 1). The maximum suppression Cc/Cmax for these compounds were 1.64/0.66 = 2.48 (for concentration 10.0 M) (1); 2.13/0.29 = 7.34 (for concentration 10.0 μM) (4); 2.13/0.53 = 4.02 (for concentration 10.0 μM) (6); 1.83/0.83 = 2.20 (for concentration 10.0 μM) (8); and 1.83/0.60 = 3.05 (for concentration 5.0 μM) (9) (Fig. 2). Compounds 4, 6, and 9 had the greatest cytotoxic activity. The calculated concentrations for 50% inhibition (IC50) of these compounds were 0.86, 2.98, and 5.05 μM, respectively.
It is noteworthy that compound 1 had moderate inhibitory activity on the growth of the tumor cells; compound 8, low activity (Fig. 1). Addition of compounds 5 and 7 to the medium led to moderate non-dose-dependent cytotoxic activity (Fig. 1). The maximum suppressions Cc/Cmax were 2.13/0.75 = 2.84 (for concentration 10.0 μM) and 1.84/0.70 = 2.62 (for concentration 5.0 μM), respectively (Fig. 2). Compounds 2, 3, 10, and 11 did not affect the growth of MCF-7 cells in vitro (Fig. 1).
The tested compounds were divided into three groups according to cytotoxic activity against the tumor cells based on the results of the studies, i.e., compounds with no or extremely low cytotoxic effects (2, 3, 10, 11); compounds with moderate cytotoxic effects (1, 5, 7, 8); and compounds with high cytotoxic activity over the whole range of studied concentrations (4, 6, 9) (Fig. 2).
Epirubicin had a maximum suppression of Cc/Cmax 1.55/0.78 = 1.99 (for concentration 5 μM) against CHO cells. The calculated IC 50 value was 8.74 μM. According to the MTT assay, compound 4 significantly reduced the viability of CHO cells over the whole range of concentrations (Fig. 3). The maximum suppression Cc/Cmax was 1.55/0.59 = 2.63 (for concentration 5.0 μM); IC50, 7.18 μM. Compound 6 exhibited moderate cytotoxic effects over the whole range of studied concentrations (Fig. 3). The maximum suppression Cc/Cmax was 1.55/0.89 = 1.74 (for concentration 10.0 μM). The calculated IC50 value in the studied concentration range was not achieved, i.e., was >10 μM. Compound 9 showed a minimal effect against CHO cells (Fig. 3). The maximum suppression Cc/Cmax was 1.55/1.28 = 1.21 (for concentration 10.0 μM); IC50, beyond the limits of the concentration range.
Thus, a comparison of the cytotoxicity of the azoloazine derivatives showed that these compounds exhibited various activities against BC cells despite the similar structures and physicochemical properties. Studies of the cytotoxic activities of the new azoloazine derivatives showed that compounds 4, 6, and 9 possessed pronounced advantages over the other compounds. However, the actual mechanisms, proof of their differences, and a comparison of their molecular structures require separate studies. Namely these compounds were selected for further research to reveal their possible antitumor properties.
The second stage of the research focused on checking the hypothesis about the possible antitumor activity of 4, 6, and 9 for a xenogenic BC model in vivo in mice.
A study of the antitumor activity in an experiment in vivo showed that administration of epirubicin to animals with tumors led to moderate growth inhibition of the primary tumor (24.5%). Administration of 4, 6, and 9 had more pronounced antitumor effects. For example, administration to mice with BC of 4 at a dose 1/2 of IC50 inhibited tumor growth by 60.8%; of 6, 32.7%; of 9, 38.8% (Table 1).
The experimental results indicated that all tested compounds had antitumor activity. It is noteworthy that the tested compounds had more pronounced activity against the primary tumor than epirubicin.
Histological studies revealed changes in the transplantation area and adjoining adipose tissue and lymph nodes. Also, individual transformed cells and their accumulations as small clusters or trabecula were observed in all experimental groups at the site of tumor cell transplantation on day 15 after injection (Fig. 4a). In separate instances, cells formed chains situated around unaltered channels like targets or owl’s eyes. The lumen was either filled with cells or partially free with a mucoid secretion for intraductal invasion. Several tumor cells were necrotized and surrounded by a lymphohistocytic infiltrate (Fig. 4a and 4b).
Basal region of mouse breast nipple 15 d after transplantation of MCF-7 cells: single tumor cells and small clusters, clearly expressed reactive changes in lymphatic tissue (a); edge infiltration of tissue near lymph node gate. Hematoxylin and eosin stains. 200× magnification (b). Immunohistochemical images of human cytokeratin 8/10 in mice with BC (c, d): animal with untreated tumor (c); animal with tumor treated with compound 4 (d).
Immunohistochemical studies revealed a specific protein, human cytokeratin 8/18 in the tumor tissue of control mice. Administration of the tested compounds reduced the expression of this protein (Fig. 4c and 4d).
The histological pattern demonstrated a decrease and decomposition of part of the tumor structures in the mouse tissues. However, the remaining cells were very atypical, demonstrated a tendency for mitosis and invasion, and formed fresh accumulations in breast tissue adjoining adipose tissue and lymph nodes. Judging from the decrease in the tumor-specific protein human cytokeratin 8/18 in the animal tumor tissues, the immunohistochemical studies also proved the pronounced antitumor effect of the new azoloazine derivatives.
Therefore, the tested compounds could be placed in the following order based on the results of the in vivo studies: 4 > 9 > 6 > epirubicin. Thus, 4 was the most active antitumor compound. This conclusion should be treated as preliminary because only one model (xenogenic transplantation in mice) and one cell line (MCF-7) was used in the work to evaluate the antitumor activity. Thus, the results demonstrated promise for further research on the new azoloazine derivatives (4, 6, 9), which could inhibit the development of tumors in other experimental models of grafted tumors.
A possible mechanism for the antitumor activity of the studied compounds could be their ability to induce apoptosis of tumor cells by DNA damage due to methylation of N7 and O6 of guanine and N3 of adenine. Thymidine instead of cytosine would be incorporated into DNA because of the damage [14]. For example, Dwyer, et al. showed that pyrazolopyridine derivatives could block the activity of serine/threonine kinases Pim-1 and Pim-2, which are excessively expressed with oncological diseases such as leukemia and lymphoma [15].
Toxicity for nontumor cells is one of the main limitations on the broad use of all known cytostatic drugs [16].
The experimental results showed that 4 had the greatest antitumor activity, which proved its promise as a potential new molecule for designing antitumor drugs based on it for BC patients. It also possessed cytotoxicity for nontumor CHO cells. Therefore, this compound could be dangerous for normal cells and tissues. However, this assumption requires further verification.
Conflict of interest
We declare no conflict of interest.
Financing
The research was performed in the framework of a state task.
Information on results from a check of the study protocol by the ethics committee
The experimental study design was approved after review by the Local Ethics Committee of Volgograd State Medical University, Ministry of Health of Russia (Protocol No. 2021/049 of May 27, 2021).
Acknowledgments
We thank Corresponding Member Prof. Dr. V. V. Udut, Deputy Director for Science and Therapy, Head of the Laboratory of Physiology and Molecular and Clinical Pharmacology, Goldberg Research Institute of Pharmacology and Regenerative Medicine, Tomsk National Research Medical Center, Russian Academy of Sciences, for support and assistance with discussing the research results. We thank Corresponding Member Prof. Dr. N. V. Cherdyntseva, Deputy Director for Science and Therapy, Research Institute of Oncology, Tomsk National Research Medical Center, Russian Academy of Sciences, Head of the Laboratory of Molecular Oncology and Cancer Immunology, for the supplied materials and their structuring for subsequent analysis.
References
A. F. Rositch., K. Unger-Saldana, R. J. DeBoer, et al., Cancer, 26(10), 2394 – 2404 (2020).
M. Longacre, N. A. Snyder, G. Housman, et al., Int. J. Mol. Sci., 17(5), 759 (2016).
K. V. Savateev, E. N. Ulomskii, I. I. Butorin, et al., Usp. Khim., 87(7), 636 – 669 (2018).
E. V. Sadchikova, Izv. Akad. Nauk, Ser. Khim., 7, 1867 – 1872 (2016).
B. C. Baguley and E. Leung, in: Breast Cancer - Carcinogenesis, Cell Growth and Signalling Pathways, M. Gunduz and E. Gunduz (eds.), InTech, Rijeka (2011), pp. 245 – 256.
J. Y. Kim, Y.-G. Kim., and G. M. Lee, Appl. Microbiol. Biotechnol., 93(3), 917 – 930 (2012).
R. Alexandrova, D. Dinev, I. Gavrilova-Valcheva, et al., Merit Res. J. Med. Med. Sci., 7(2), 73 – 79 (2019).
G. A. Frank, Breast Cancer. Practical Guide for Physicians [in Russian], G. A. Frank, L. E. Zavalishina, and K. M. Pozharisskii (eds.), RMAPO, Moscow (2014).
M. Akram, M. Iqbal, M. Daniyal, et al., Biol. Res., 50(1), e33 (2017).
S. J. Done Preface, Breast Cancer — Recent Advances in Biology, Imaging and Therapeutics, Rijeka, InTech, IX (2011).
V. Horishny, L. Mandzyuk, R. Lytvyn, et al., Russ. J. Org. Chem., 56(4), 588 – 595 (2020).
Z. Ahani, M. Nikbin, M. F. Maghsoodlou, et al., J. Iran Chem. Soc., 15, 2423 – 2430 (2018).
V. Horishny, F. Chaban, and V. Matiychuk, Russ. J. Org. Chem., 56(3), 454 – 457 (2020).
G. Ramis, E. Thomas-Moya, S. F. de Mattos, et al., PLoS One, 7, e38770 (2012).
M. P. Dwyer, K. Keertikar, K. Paruch, et al., Bioorg. Med. Chem. Lett., 22(23), 6178 – 6182 (2013).
A. P. Men’shenina, T. I. Moiseenko, E. V. Verenikina, et al., Sovrem. Probl. Nauki Obraz., No. 3 (187) (2019).
Author information
Authors and Affiliations
Corresponding author
Additional information
Translated from Khimiko-Farmatsevticheskii Zhurnal, Vol. 58, No. 3, pp. 3 – 10, March, 2024.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Al-Humairi, A.H. Experimental In Vitro and In Vivo Studies of the Antitumor Activity of New Azoloazine Derivatives for the Treatment of Breast Cancer. Pharm Chem J 58, 399–406 (2024). https://doi.org/10.1007/s11094-024-03158-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11094-024-03158-2