Abstract
Earthquakes result in overwhelming demand for medical resources at once, and affected areas requires reinforcement from neighbor cities. An effective allocation approach of medical rescue teams in early stage of disaster relief can improve rescue performance significantly. To find optimal allocation strategy, an integer nonlinear programming model is established, following utility principle. To construct the optimization model, stochastic transition probability of triage levels is introduced. Meanwhile, function from allocation scheme to fatalities of areas is established. Next, we design algorithm based on Lingo software to find solution of utility model. Finally, numerical experiments based on real data in 2008 Sichuan earthquake in China are used to compare utility approach with existing approaches in practice. The results of experiments indicate that: (1) to save more lives, a support team should preferentially be allocated to a worse and nearer affected area. When the worst area is not the nearest, the team also may be sent to an area with moderate severity and moderate distance. (2) Compared with severity strategy and distance strategy, utility strategy improves rescue efficiency significantly.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Natural disasters like earthquakes cause massive casualties at once. Local medical capabilities cannot meet overwhelming demand for medical treatment, so that reinforcement is required from neighbor cities. Shortly after disasters occur, medical personnel gather quickly and wait for assignment by emergency command center. Medical personnel from neighbor cities are very scarce and precious in initial stage of disaster response, so allocation strategy on these rescuers will significantly change total amount of fatalities.
In current disaster rescue practice, decision on destination of medical groups is made subjectively according to disaster data by decision makers. Basically, there are mainly two existing strategies to deal with reinforcement allocation. The first is called severity strategy, which proposes personnel assigned to harder-hit areas preferentially. The second is called distance strategy, which proposes personnel allocation gives priority to affected areas nearer to the save point. However, in case that the save point is nearer to the non-worst damaged affected area, these two strategies make conflicting decision, which lets decision makers confused. Therefore, a clear and effective approach is required for emergency command center.
A review of the literature for appropriate decision-making models shows that specific medical resource allocation problems have been discussed quite rarely.
In the literature on disaster management (Ajami and Fattahi 2009; Altay and Green 2006), activities are classified into the preparedness phase (period before the disaster), the response phase (period during and shortly after the disaster), and the recovery phase (period long time after the disaster). More specifically, the preparation phase addresses tasks related to planning, training, and establishment of necessary emergency services. Huseyin and Zelda (2010) propose a stochastic optimization approach to the storage and distribution problem of medical supplies to be used for disaster preparedness under a wide variety of possible disaster types and magnitudes. The approach can be used to suggest loading and routing of vehicles to transport medical supplies for disaster response, given the evaluation of up-to-date disaster field information. Horner and Downs (2010) study logistical planning to facilitate the distribution and transportation of relief goods to populations in need, to manage hurricane disasters. The study shows how a variant of the capacitated warehouse location model can be used to manage the flow of goods shipments to people in need. Pamela et al. (2010) apply OR methods to a real-world water distribution application in the field of disaster relief operations planning. The research provides solutions on where to place water tanks and which roads to use for the transport of drinking water in the phase of disaster response.
Additionally, primary aims during the response phase are reduction in casualties and economic losses according to disaster situations. Zhang et al. (2012) formulate the emergency resource allocation problem with constraints of multiple resources and possible secondary disasters. Optimal allocation of emergency resources is found by heuristic algorithm based on linear programming and network optimization. Hina et al. (2010) discuss a resource allocation approach to optimizing regional aid during public health emergencies. The result shows that optimal response involves delaying the distribution of resources from the central stockpile as much as possible. Fiedrich et al. (2000) argue that the main goal of the initial search-and-rescue period after strong earthquakes is to minimize the total number of fatalities. And they introduce a dynamic optimization model to calculate the resource performance and efficiency for different tasks related to emergency response.
Most literature above regards emergency resources general and non-characteristic. However, these works did not consider the difference between allocation of medical resource and general resource in the disaster response phase. Although several works focus on allocation of medical resources (Cao and Huang 2012; Felix et al. 2014), existing study still cannot suggest how to allocate medical teams after earthquakes. Total number of fatalities depends on allocation scheme of medical teams. However, existing models rarely explore the dependency mechanism from amount of medical resources to fatalities. To model the relationship, Carlos (2011) assumes lifetime expectancy of casualties to be Weibull-distributed, while Wilson et al. (2013) and Narjès et al. (2006) use Markov chain to represent the stochastic process of the health of a trapped casualty. Following their works, this paper accepts Markov chain in proposed model.
The rest of the paper is organized as follows. Section 2 illustrates the allocation problem in a mathematical manner. Sections 3 and 4 detail the mathematical model and algorithm for the medical team allocation problem. Experimental results and conclusion are given in Sects. 5 and 6, respectively.
2 Problem statement
We consider a severe earthquake. After the earthquake occurs at time zero, m hard-hit areas \(A_{i} \left( {1 \le i \le m} \right)\) require medical support. A medical team is considered as one basic unit of casualty treatment in this paper. Shortly after disaster occurs, at time \(t = t_{0} (t_{0} > 0)\), medical support teams in n save points \(S_{j} \left( {1 \le j \le n} \right)\) are ready and waiting for allocation by emergency command center. We define an n-dimensional vector \(s \equiv \left\{ {s_{j} ; 1 \le j \le n} \right\}\), where s j represents the amount of medical support teams waiting for assignment in each save point S j . Besides support medical teams from neighbor cities, local medical teams in affected areas have been working on disaster relief since time zero. The m-dimensional vector \(r^{0} \equiv \left\{ {r_{i}^{0} ; 1 \le i \le m} \right\}\) symbols number of local medical teams in every affected areas at time t = t 0. Patients are classified into J categories \(\left\{ {L_{k} ;1 \le k \le J} \right\}\), and the categories are sorted in a descending order by urgency; i.e., L 1-type casualties are with severe wounds, while L J -type casualties suffer minor injuries. Matrix C m × J symbols number and structure of casualties in all areas; e.g., \(C_{ik} \left( {1 \le i \le m,1 \le k \le J} \right)\) represents number of L k -type casualties who are waiting for treatment in A i .
As soon as destination from emergency command center is known, a medical rescue team from a save point spends a period of time traveling to its assigned affected area. Let matrix T m × n be the time distance from save points to affected areas, where T ij is the time a medical team spends in traveling from point S j to area A i . A support team cannot rescue any patient, until it reaches the affected area. This paper is considering the problem of medical rescue in early stage after disaster, so arrival time of considered support teams should be much earlier than golden rescue time line 72 h, so we have \(T_{ij} < < 72\). And let \(t = t_{0}^{{\prime }}\) be the planned next decision epoch when a new allocation scheme will be made after enough new support teams get ready in save points.
Based on information above, at current decision epoch time \(t = t_{0}\), decision makers have to determine allocation scheme \(X_{m \times n}\) of teams, where X ij is number of teams assigned from point S j to area A i , with total number of saved lives in all affected areas maximization during interval \(\left[ {t_{0} ,t_{0}^{{\prime }} } \right]\) as objective.
3 Saving function of areas
Since not all patients receiving treatment will ultimately survive, we introduce saving function to reflect the probability of casualties that may survive from disaster. Combining saving function of individual casualties, we can establish saving function of areas, which is a mapping from allocation scheme of medical rescue teams to number of survivors in areas.
3.1 Saving function of casualties
Wilson et al. (2013), Narjès et al. (2006) and Chu et al. (2015) employ stochastic Markov chain to model transition of triage levels as shown in Fig. 1. According to the chain model, health states of casualties in all J categories may deteriorate in various probabilities every hour. In Fig. 1, category ‘D’ represents the state of death. Without operative intervention, L 1-type casualties may die in probability of P 1D, and keep in L 1 category in probability of P 11 in 1 h, where \(P_{{ 1 {\text{D}}}} + P_{11} = 1\). Similarly, for other less urgent categories, a casualty in category k(1 < k ≤ J) is possible to deteriorate into category k − 1 in probability of P k,k−1 and remain in category k in probability of P k,k , where \(P_{k,k - 1} + P_{k,k - 1} = 1\). Note that all the state transition is unidirectional without intervention, from optimistic to pessimistic.
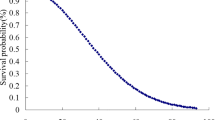
According to the model in Fig. 1, the earlier a casualty gets treatment, the more possible he survives in disaster. In fact, about 98 % will survive if casualties are treated within 20 min after earthquake, while survival probability declines to 63 % if treated in 1 h (Hu et al. 2010). For a casualty in category k(1 < k ≤ J), his probability of death can be calculated in an iterative manner as follows:
where τ is treated time of the casualty. \(p^{D} \left( {\tau ,k} \right)\) is the estimated probability of a L k casualty may die in the disaster, if he is treated at time τ. Obviously, the probability p S of his survival can be formulated as:
In particular, in practical disaster relief, the critical mortality rate is proposed to measure performance of treatment system by Armstrong et al. (2008) and Frykberg (2004). This measure considers only immediate casualties and delayed casualties who may die of the disaster. In the two-category scenario, J = 2, there are L 1 and L 2 casualties waiting for treatment. By formulation (1) and (2), we can calculate survival probability with respect to treated time.
3.2 Saving function of various areas
A rescue team assigned to worse area or less damaged area may lead to different rescue results. Hence, given limited rescue resource, decision scheme has an influence on performance of rescue. We call the relationship from decision to rescue performance as saving function of areas.
By scale of casualty and local medical ability on sites, we divide affected areas into three categories: worst hit area, worse hit area, and lightly hit area. Exactly two quantitative measures, \(\alpha\) and \(\beta\), are introduced to identify this type of affected area. Based on formulation (3), \(\alpha\) and \(\beta\) are determined by the following formulation (4) and formulation (5), respectively.
\(\alpha\) is expected life span of immediate casualties, while \(\beta\) is expected life span of delayed casualties. Then, average declining rate of survival probability are \(\alpha^{ - 1}\) and \(\beta^{ - 1}\), respectively, for immediate casualties and delayed casualties. With respect to these two measures and decision scheme, each type of areas follows distinctive saving function, respectively, described as below.
3.2.1 Worst hit area
Areas in this category are hit most seriously and extremely lack medical resources. Using measures \(\alpha\) and \(\beta\), worst hit area is quantitatively defined as follows.
Definition 1 (Worst hit area)
An area is a worst hit area, in case those immediate casualties cannot all be treated within \(\alpha\) hours, nor delayed injured casualties can all be treated within \(\beta\) hours, only relying on local medical resource and small quantity of support.
Based on analysis above, expected amount of immediate casualties saved by local medical personnel in worst hit area \(A_{i}\) can be calculated and represented as:
where Y symbols number of saved casualties, whose superscript 0 indicates local medical resource, subscript i indicates affected area \(A_{i}\), and subscript 1 indicates immediate casualties. And \(\varPsi_{1}\) is mean process time of immediate casualties.
As discussed, life span of immediate casualties may exceed \(\alpha\) hours in a low probability, without any intervention. In other words, an immediate casualty is possible to survive only if treated before time \(t = \alpha\). Therefore, saving calculation of support teams is little different with local teams; due to travel time, it is possible for a support team to arrive the assigned area after time \(t = \alpha\), when no immediate casualty is waiting for first aid treatment. Hence, relying on distance, all teams from \(S_{j}\) to \(A_{i}\) can save number of immediate casualties:
where of \(Y_{i1}^{j}\), superscript j indicates rescue teams from \(S_{j}\), subscript i indicates affected area \(A_{i}\), and subscript 1 indicates immediate casualties. And \(X_{ij}\) is number of rescue teams assigned from \(S_{j}\) to \(A_{i}\) by decision scheme.
First aid treatment on delayed casualties is executed after immediate casualties treatment is complete in area \(A_{i}\). Amount of delayed casualties saved by local medical personnel in \(A_{i}\) can be calculated and represented as:
where \(\varPsi_{2}\) is mean process time of delayed casualties.
If a support team from \(S_{j}\) arrives before time \(t = \alpha\), it can start first aid treatment for delayed casualties at \(t = \alpha\) right after first aid for immediate casualties is complete. Otherwise, the treatment starts at \(t = t_{0} + T_{ij}\) as soon as the team arrives at area \(A_{i}\). Hence, each team from \(S_{j}\) to \(A_{i}\) can save number of delayed casualties:
Combining formulation (6)–(9), saving function of worst hit area \(A_{i}\) during time interval \(\left[ {t_{0} ,t_{0}^{{\prime }} } \right]\) is formulated as:
3.2.2 Worse hit area
Areas in this category suffer relative slight disaster compared to worst hit areas. However, external support is still required to achieve better rescue result. We also use quantitative measures \(\alpha\) and \(\beta\) to define this type of affected areas.
Definition 2 (Worse hit area)
An area is a worse hit area, in case those immediate casualties can all be treated within \(\alpha\) hours, but delayed casualties cannot all be treated before the next decision time \(t = t_{0}^{{\prime }}\), relying on local medical personnel and small quantity of support.
Given i, \(t_{0}\), and \(T_{ij} \left( {j = 1, \ldots ,n} \right)\), sort \(T_{ij}\) in ascending order, and we obtain an ascending sequence:
For a decision matrix \(X\), end time of immediate casualties treatment \(t_{1}\) can be calculated. Then, insert \(t_{1}\) into sequence (11), and a new sequence (12) is achieved.
Teams from first h save points in sequence (12) are able to work on immediate casualties treatment in \(A_{i}\), and total saved by them can be calculated as formula (13):
where \(Y_{i1}^{*}\) symbols total number of immediate casualties saved by all external rescue teams in \(A_{i}\).
Similar to worst hit area, number of immediate casualties in worse hit area saved by local teams is:
At time \(\left( {t = t_{1} } \right)\), first aid treatment of immediate casualties is complete. After that, all teams turn to work on delayed casualties until next decision epoch \(t = t_{0}^{{\prime }}\).
During interval \(\left[ {t_{1} ,t_{0}^{{\prime }} } \right]\), local teams save number of delayed casualties:
Teams from \(S_{j}\) may arrive \(A_{i}\) after \(t = t_{1}\). In that case, start time on delayed casualties treatment is \(\hbox{max} \left\{ {t_{1} ,t_{0} + T_{ij} } \right\}\). Then, number of delayed casualties saved by teams from \(S_{j}\) is:
Combining formulations (13)–(16), saving function of worse hit area \(A_{i}\) during \(\left[ {t_{0} ,t_{0}^{{\prime }} } \right]\) is formulated as:
3.2.3 Lightly hit areas
We define lightly hit area as an area performs no significant difference in rescue results whether support medical teams are dispatched to the area or not. Obviously, in early stage of disaster, scarce support resource should be assigned to worst hit areas and worse hit areas preferentially.
3.2.4 Saving function of areas
Based on the above analysis, this paper only discusses problem of personnel allocation to worst hit areas and worse hit areas. With same support, a worst hit area and a worse hit area may follow different saving function:
4 Utility approach
4.1 Principle of allocation
Decision makers allocate scarce and limited medical rescue teams among a volume of areas full of injured patients. This makes a distributive justice problem that addresses how benefits should be distributed within a population. John and Kenneth (2007) examine three principles of distributive justice: the principle of utility, the difference principle, and the principle of equal chances, analyzing how each might be used in medical system.
-
The principle of utility
This principle, also called the greatest happiness principle, is the cornerstone of utilitarianism. It judges allocation schemes insofar as they produce the greatest net benefit among all related affected areas. The principle offers compelling moral justification for the practice of medical relief, although causes problems such as scope of concern, calculation of consequences, and unequal outcomes.
-
The difference principle
This principle permits unequal distribution of medical resource as long as such inequalities provide the best outcome for the least well-off.
-
The principle of equal chances
This principle claims that each person should be given an equal chance to survive in his hypothetical situation. It proposes to treat as many casualties as possible, even if not everyone regrettably can be saved.
Based on analysis by John and Kenneth (2007), we eventually employ the principle of utility in decision-making model of rescue team allocation in the following subsection. So, the strategy implied by the model is called utility strategy.
4.2 An integer nonlinear mathematical programming
The principle of utility is one of the most widely accepted principles in many medicine scheduling systems (Iserson and Moskop 2007). Core proposal of the principle is to achieve greatest overall benefit, which appears as total number of saved maximization in this study.
Following the principle of utility, we establish a decision support model as shown below. Objective of the model is to find a solution \(X_{m \times n}\) which leads to as many as possible lives saved.
Objective function (18) maximizes total expected number of saved casualties; constraint (19) indicates that sum of rescue teams sent from each save point is no more than number of teams gathered in the point; constraint (20) indicates that the proposed model is an integer mathematical programming, and number of medical teams is a nonnegative integer; constraint (21) in early stage of earthquake response, affected areas are in huge lack of medical resources. Until next decision-making epoch, a lot of casualties are still waiting for treatment. Even after early support teams arrive, medical resources in areas still cannot meet demand.
4.3 Solving the programming
The programming model above, following the principle of utility, is nonlinear with integer variables. Optimization modelling software Lingo provides great solution for nonlinear integer programming. Although time performance of Lingo is questioned when scale of problem gets extremely huge, Lingo has many advantages, including easy to program. Additionally, scale of medical rescue teams allocation problem is limited. Therefore, Lingo 11.0 is selected to find optimal \(X_{m \times n}\), and corresponding pseudocode is given in Algorithm 1.
5 Numerical experiments
5.1 Experimental parameters
We collect data of 2008 Sichuan earthquake in China through the literature. And some data are quite important for proposed approach.
According to Lei et al. (2008), from May 12, 2008, to June 30, 2008, Mianyang City, one of the worst hit areas, received and cured 21628 casualties, 846 of which, 3.61 %, died. Based on this, approximately, we can think a casualty will eventually survive if he is still alive after first aid treatment. Additionally, Jiang et al. (2008) analyze data of 2283 emergency patients in 2008 Sichuan earthquake. They found that median treatment duration of immediate casualties is 34 min and median treatment duration of delayed casualties is 61.50 min. Hence, values of parameters \(\varPsi_{1}\), \(\varPsi_{2}\) are determined, \(\varPsi_{1} = 0.57\) and \(\varPsi_{2} = 1.025\) hours.
First surge of death comes in several seconds to minutes after earthquake; second surge comes in several minutes to hours; and third surge comes in several hours to weeks (Jian and Ma 2010). For medical rescue, first three days are golden 72 h. Hence, based on the literature (Jiang et al. 2008; Jian and Ma 2010; Feng et al. 2009), let \(\alpha = 4\) hours, \(\beta = 72\) hours.
Let current decision epoch be \(t_{0} = 0.2\) and next decision epoch be \(t_{0}^{'} = 5\); the objective of approaches is to determine how to allocate support teams at \(t = 0.2\), realizing expected number of saved casualties maximization from time \(t = 0.2\) to time \(t = 5\).
5.2 Simulation experiment: potential earthquakes in Sichuan
We present a simulation experiment to demonstrate our approach to responding to an earthquake in Sichuan Province of China. It is based on statistics and the literature on 2008 Sichuan earthquake (Lei et al. 2008; Jiang et al. 2008; Jian and Ma 2010; Feng et al. 2009). Although our approach supports affected areas and save points from everywhere, for the sake of convenience we restrict areas and points all in Sichuan Province in this simulation experiment.
In recent years, the Sichuan area is frequently attacked by earthquakes. The province consists of 21 prefecture-level divisions: 18 prefecture-level cities and 3 autonomous prefectures as marked in Fig. 2. The time a rescue team travels from one division to another is estimated via Yahoo Maps. For example, as shown in Fig. 3, Yahoo Maps evaluates that driving from Chengdu to Leshan takes 1 h and 29 min. And so forth, distance matrix \(T_{21 \times 21}\) is obtained among 21 divisions of Sichuan.
To generate problem instance, we follow the steps below.
Step 1 Randomly determine m number of affected areas requiring support and n number of save points. However, an area cannot request and send out support teams simultaneously. In other words, sum of m and n is no more than 21, and the other \(21 - m - n\) divisions neither request nor send out support teams.
Step 2 Set number of local medical teams in affected areas and number of rescue teams in save points. The number of local medical teams is approximated by 1.2 % multiplied by amount of licensed doctors in the area, which are listed in Table 1, while the number of teams in the save points is approximated by 0.2 % multiplied by amount of licensed doctors. The values of 1.2 and 0.2 % are determined based on discussions with several emergency management coordinators of a large medical center in Dalian, China. Delphi method is adopted in the process of parameter determination.
Step 3 Generate casualties data of affected areas. First, m affected areas follow Bernoulli distribution with parameter \(p = \frac{10}{39}\), where p is the probability that the area is a worst hit area, and 1 − p is the probability that the area is a worse hit area. Besides, value of p is determined because 10 worst hit areas and 29 worse hit areas exist in real 2008 Sichuan earthquake. Then, number of casualties in an area is casualty ratio multiplied by population of the area. Casualty ratio is obtained fitting on real ratio of 2008 Sichuan earthquake in Table 2. For worst hit areas, casualty ratio follows normal distribution \(N\left( {0.1182,0.08516} \right)\), and for worse hit areas, casualty ratio follows normal distribution \(N\left( {0.0146,0.01532} \right)\).
Finally, if an area is marked as worst hit area, ratio of immediate casualties is uniformly distributed in interval [20, 30 %], while the random ratio uniformly distributes in [10, 20 %] for worse hit areas.
5.3 Strategy comparison
Different allocation strategies cause different rescue results. This section calculates evaluated number of saved casualties between current decision epoch and the next decision epoch under three strategies: utility strategy, severity strategy, and distance strategy.
In order to evaluate the improvement resulting from utility strategy when compared to other strategies, totally 190 problem instances are generated, varying m from 2 to 20. For each given m, number of save points n varies from 1 to \(21 - m\). Moreover, for each problem instance, performance of each of the three strategies is averaged over 100 simulation replications. Each replication is assembled with random number of worst/worse hit areas and casualties.
Results in Fig. 4 show how the performance of strategies varies over different values of m. For each replication, performance of distance strategy is normalized to 1, while performance of severity strategy and utility strategy are, respectively, ratio of expected number of survivor by corresponding strategy to the number by distance strategy. Each performance is averaged over \(2100 - 100m\) replications. The results confirm that proposed utility strategy has advantage over existing distance strategy and severity strategy.
5.4 Detailed solution comparison
In order to gain a better understanding of the reason why utility strategy is advantageous over the others, we investigate a 4 × 3 problem instance (\(m = 4,n = 3\)), including 4 affected areas and 3 save points. Let \(A_{i} \left( {i = 1,2,3,4} \right)\) be affected areas ordered by severity, where \(A_{1}\) and \(A_{2}\) are worst hit areas, \(A_{3}\) and \(A_{4}\) are worse hit areas. Related casualty matrix \(C_{4 \times 2}\) is shown below.
In the scenario, \(A_{1}\) is the hardest hit area with immediate casualty ratio around 30 %, while \(A_{4}\) is the lightest hit area with immediate casualty ratio 10 %. Let \(r^{0} = \left( {25,25,25,25} \right)\) and \(t_{0} = 0.2\), then at time \(t = 0.2\), there are 25 local medical groups in each area. Number vector of support teams in save points is \(s = \left( {10,10,10} \right)\). The duration a team travels from save points to affected areas is as follows:
By using Lingo program explained above, experiment data are analyzed and processed; finally, we got optimal support team allocation decision matrix:
According to the optimal solution, we find: (1) teams in save point \(S_{1}\) is assigned to the worst hit area \(A_{1}\) but not the nearest \(A_{4}\); (2) teams in save point \(S_{2}\) is assigned to the nearest area \(A_{2}\), although \(A_{1}\) is a worse hit area; (3) teams in save point \(S_{3}\) is assigned to neither the nearest \(A_{4}\) nor the worst \(A_{1}\), but \(A_{3}\) with moderate severity and moderate time distance.
Based on the utility approach and findings above, we get first conclusion in the paper.
Conclusion 1 To save more survivors, a support team should be assigned to affected areas that are worse or nearer to the save point. In case that the area with worst severity is not the nearest one, it is possible that optimal scheme assigns the team to an area with both moderate severity and moderate distance.
-
1.
Severity strategy
The severity strategy takes severity of areas affected by disaster as determinant factor. Support teams are always sent to the worst damaged area in initial stage. In the problem instance, no matter from perspective of number of casualties or ratio of casualties to local medical ability, affected area \(A_{1}\) is the worst damaged area. Following severity-first rule, all support from three save points is assigned to \(A_{1}\), and allocation solution is:
Corresponding saved number under severity strategy is 447.7.
-
2.
Distance strategy
Since road traffic may be blocked or interrupted after disaster, distance in length cannot reflect travel time of support teams exactly. So, time is directly used to measure distance from save points to affected areas and takes hour as unit. Following distance-first rule, as shown below, \(S_{1}\) is assigned to support \(A_{4}\), \(S_{2}\) is assigned to support \(A_{2}\), and \(S_{3}\) is assigned to support \(A_{4}\).
Corresponding saved number under distance strategy is 453.2.
-
3.
Utility strategy
Different from severity strategy and distance strategy, utility approach gives an allocation solution as formula (22). Saved number according to (22) is 456.4. The number is 1.94 % more than severity strategy and 0.71 % more than distance strategy. Here, we get the second conclusion:
Conclusion 2 Existing rescue teams assignment strategies, including severity strategy and distance strategy, in early stage of disaster relief, usually lead to non-optimal result. Utility approach can find better allocation plan than existing approaches.
6 Conclusions
This article has aimed at developing a decision-making approach to medical personnel support allocation in first stage of disaster relief. Proposed utility approach suggests emergency command center how to assign support teams. As seen from the experimental test results, utility approach can save more survivors significantly, compared to existing strategies.
For further studies, we are going to combine utility approach with GIS and emergency management system. With geography, casualty, and local medical ability data provided by information system, decision could be made more automatically and efficiently, which is meaningful in practice.
References
Ajami S, Fattahi M (2009) The role of earthquake information management systems (EIMSs) in reducing destruction: a comparative study of Japan, Turkey and Iran. Disaster Prev Manag 18:150–161
Altay N, Green WG (2006) OR/MS research in disaster operations management. Eur J Oper Res 175:475–493
Armstrong JH, Frykberg ER, Burris D (2008) Toward a national standard in primary mass casualty triage. Disaster Med Public Health Prep 2(s1):8–10
Cao H, Huang S (2012) Principles of scarce medical resource allocation in natural disaster relief: a simulation approach. Med Decis Making 32:470–475
Carlos C (2011) Effective patient prioritization in mass casualty incidents using hyper heuristics and the pilot method. OR Spectrum 33:699–720
Chu X, Zhong QY, Khokhar SG (2015) Triage scheduling optimization for mass casualty and disaster response. Asia Pacif J Oper Res. doi:10.1142/S0217595915500414
Felix W, Guido S, Stefan F et al (2014) Emergency response in natural disaster management: allocation and scheduling of rescue units. Eur J Oper Res 235:697–708
Feng L, Wang LM, Chen L et al (2009) Method of triage and remedy for earthquake casualties. Mod Med Health 25:323–325 (in Chinese)
Fiedrich F, Gehbauer F, Rickers U (2000) Optimized resource allocation for emergency response after earthquake disasters. Saf Sci 35:41–57
Frykberg ER (2004) Principles of mass casualty management following terrorist disasters. Ann Surg 239:319–321
Hina A, Raghu TS, Vinze A (2010) Resource allocation for demand surge mitigation during disaster response. Decis Support Syst 50:304–315
Horner MW, Downs JA (2010) Optimizing hurricane disaster relief goods distribution: model development and application with respect to planning strategies. Disasters 34:821–844
Hu WJ, Zhao WH, Li YF et al (2010) Analysis of emergency medical staging in Wenchuan earthquake casualty treatment. Pract J Clin Med 7:20–24 (in Chinese)
Huseyin OM, Zelda BZ (2010) Stochastic optimization of medical supply location and distribution in disaster management. Int J Prod Econ 126:76–84
Iserson KV, Moskop JC (2007) Triage in medicine, part I: concept, history, and types. Ann Emerg Med 49:275–281
Jian HS, Ma JF (2010) Significance of casualty time curve in medical rescue of Wenchuan earthquake. J Traum Surg 12:535–537 (in Chinese)
Jiang YW, Zhang JC, Zhong Y et al (2008) Summary of triage after Wenchuan earthquake in 2 weeks. Chin J Evid Based Med 8:722–725 (in Chinese)
John CM, Kenneth VI (2007) Triage in medicine, part II: underlying values and principles. Ann Emerg Med 49(3):282–287
Lei BL, Zhou Y, Zhu Y et al (2008) The emergency response of medical rescue in the worst-hit Mianyang areas after Wenchuan earthquake. Chin J Evid Based Med 8:581–587 (in Chinese)
Narjès BS, Tarek BM, Julie D et al (2006) Assessing large scale emergency rescue plans: an agent based approach. Int J Intell Control Syst 11:260–271
Pamela CN, Karl FD, Richard FH (2010) Water distribution in disaster relief. Int J Phys Distrib Logist Manag 40:693–708
Wilson DT, Hawe GI, Coates G et al (2013) A multi-objective combinatorial model of casualty processing in major incident response. Eur J Oper Res 230:643–655
Zhang JH, Li J, Liu ZP (2012) Multiple-resource and multiple-depot emergency response problem considering secondary disasters. Expert Syst Appl 39:11066–11071
Acknowledgments
This research was sponsored by National Science Foundation of China (No. 91024029).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chu, X., Zhong, Q. Post-earthquake allocation approach of medical rescue teams. Nat Hazards 79, 1809–1824 (2015). https://doi.org/10.1007/s11069-015-1928-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11069-015-1928-y