Abstract
“Neurodegenerative disorder” is an umbrella term for a group of fatal progressive neurological illnesses characterized by neuronal loss and inflammation. Interleukin-6 (IL-6), a pleiotropic cytokine, significantly affects the activities of nerve cells and plays a pivotal role in neuroinflammation. Furthermore, as high levels of IL-6 have been frequently observed in association with several neurodegenerative disorders, it may potentially be used as a biomarker for the progression and prognosis of these diseases. This review summarizes the production and function of IL-6 as well as its downstream signaling pathways. Moreover, we make a comprehensive review on the roles of IL-6 in neurodegenerative disorders and its potential clinical application.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inclusive of Alzheimer’s disease (AD), Parkinson’s disease (PD), amyotrophic lateral sclerosis (ALS), Huntington's disease (HD), and multiple sclerosis (MS), neurodegenerative disorders comprise a heterogeneous group of neurological disorders that induce progressive, irreversible loss of neurons in the central nervous system (CNS) [1]. The brain damage induced by neurodegenerative disorders often leads to a series of dysregulated motor and nonmotor manifestations, culminating in death within years or decades. Furthermore, as aging is a major risk factor for such disorders, older adults constitute the vast majority of patients with neurodegenerative disorders [2]. As the global population ages, the prevalence of neurodegenerative diseases surges. Aside from straining medical resources and public finances, the rising incidence of neurodegenerative disease will severely diminish the quality of life of millions of patients and their caregivers.
Neuroinflammation (i.e., an inflammatory response within the CNS) contributes significantly to the pathogenesis of neurodegenerative disorders [1]. In response to neuronal damage, the sustained activation of innate immune cells in the CNS produces excessive amounts of proinflammation cytokines and induces chronic inflammation, which can compromise synaptic function, energy homeostasis, and protein aggregation, and exacerbate neurodegeneration [3]. Though the close ties between neuroinflammation and neurodegeneration have been established, the specific mechanisms underlying the complicated regulatory networks remain elusive and require further investigation.
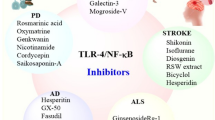
As a well-characterized proinflammatory component in the CNS, interleukin-6 (IL-6) primarily exerts a negative influence on neurons and plays a pathogenic role in neurodegenerative disorders [4]. This review summarizes the literature on the role IL-6 plays in common neurodegenerative disorders and presents an overview of the drugs that either decrease the expression of IL-6 or block IL-6 signaling to halt or slow disease progression (Table 1).
IL-6 Production and its Mode of Action
IL-6 is encoded by the IL-6 gene, which is mapped to chromosome 7p21 in human [5]. Mature IL-6 is a single-chain glycoprotein with 184 amino acids that exhibits a typical structure with four long, well-arranged helices and an extra mini-helix [6]. IL-6 is synthesized and secreted by a variety of cell types, such as T cells, B cells, monocytes, fibroblasts, and endothelial cells. Adipocytes and skeletal muscle can also produce IL-6 under healthy conditions [7, 8]. A large-scale meta-analysis involving a population of 12,421 revealed that the average plasma IL-6 concentration in healthy individuals is quite low, ranging from 4.631 to 5.740 pg/ml, and the lowest value was 0 pg/ml [9]. The basal IL-6 level was significantly higher in older adults than in younger people, demonstrating that the expression of IL-6 is age-related. This finding was confirmed in studies of disease-free wild-type mice [9,10,11]. The age-dependency in IL-6 expression is consistent with the higher susceptibility of older adults to inflammatory diseases.
When confronted with stimuli such as lipopolysaccharides, interleukin-1 beta (IL-1β), angiotensin III, kojic acid etc., the producing cells promptly synthesize redundant IL-6 [12,13,14,15,16]. Moreover, the secretion of IL-6 increases dramatically in progressive stages of inflammatory diseases and cancers. For instance, in pediatric sepsis patients infected with G-bacteria, the level of IL-6 could rise to 1000–1200 pg/ml [17]. Meanwhile, considerably higher IL-6 values have been observed in patients with prostate cancer [18].
The expression of IL-6 can be linked to genetic polymorphisms—especially those in promoter region, such as rs1800795 G/C and rs1800796 G/C. A study reported that the rs1800795 (C) allele produces more IL-6 than the (G) allele [19], while other studies showed the inconsistent results [20, 21]. Concerning rs1800796, available evidence suggests that IL-6 in individuals with rs1800796CC or rs1800796CG are higher than in those with GG genotypes [22]. As the influence of polymorphisms on IL-6 may depend on demographic, ethnic, or racial factors, differences between samples and limitations on their sizes may account for the inconsistency in the literature, large-scale, multi-center, and multi-ethnic research is necessary to resolve the controversies.
IL-6 functions mainly through binding to IL-6 receptor (IL-6R), which appears in the forms of membrane-bound IL-6R (mIL-6R) and soluble IL-6R (sIL-6R). The former is an 80-kDa membrane-bound protein limitedly expressed on the surface of hepatocytes and leukocytes, while the latter is primarily generated by the unbinding of mIL-6R or resulting from the alternative splicing of mRNA [23, 24]. These receptors both show special high affinity for IL-6, however, subsequent signal transduction requires essential assistance of transducer glycoprotein 130 (gp130), which is a 130-kDa transmembrane protein, ubiquitously expressed on the surface of almost every type of cells (except mature granulocytes) and is responsible for transducing intracellular signals through homodimerization [25, 26]. Upon binding IL-6, a transmembrane hexameric complex encompassing 2 IL-6, 2 IL-6R and 2 gp130 assembles and initiate downstream signalings [27]. There are two types of functional hexamers: the IL-6/mIL-6R/gp130 complex is formed only on a few cells that express mIL-6R, while the IL-6/sIL-6R/gp130 complex is formed on cells that lack mIL-6R. IL-6 engages with three distinct signaling pathways to regulate its biological effects: classical signaling, trans-signaling, and cluster signaling. Ultimately inducing anti-inflammatory effects, classical IL-6 signaling occurs when complex IL-6/mIL-6R/gp130 appears on the surface of selected cells. By contrast, trans-signaling results in pro-inflammatory potency. This pathway can be triggered when complex IL-6/sIL-6R/gp130 is present: i.e., on most cells devoid of mIL-6R. Also known as trans-presentation progress, cluster signaling involves the presentation of the pre-formed IL-6–IL-6R complex from dendritic cells to T cells expressing gp130 in a trans manner, leading to subsequent gp130 dimerization in the receiving cells [28]. Regardless of the signaling pathway activated, the dimerization by gp130 constitutes a start switch capable of triggering intracellular signals, including the Janus kinase (JAK)/signal transducer and activator of transcription (STAT), phosphatidylinositol 3-kinase/Akt, and mitogen-activated protein kinase pathways.
Normal Biological Functions of IL-6 in the Central Nervous System
IL-6 in the CNS is either synthesized and secreted by neurons and glial cells or transported from the outside of the CNS (Fig. 1A) [29,30,31,32,33,34]. IL-6 levels in the CNS are low under normal physiological conditions but increase sharply under psychological stress, pathological conditions (e.g., AD, PD, and MS), or stimulation with tumor necrosis factor-alpha [35,36,37,38,39,40].
Pathogenic role of IL-6 in neurodegenerative diseases. In the CNS, IL-6 promotes neuroinflammation and may thus promote the pathogenesis of neurodegenerative disorders. A There are two main sources of IL-6 in the CNS: mainly produced by T cells, B cells, and monocytes, circulating IL-6 can cross the blood–brain barrier and reach the CNS; otherwise, IL-6 is secreted by neurons and glial cells. B While IL-6 exerts both beneficial and detrimental effects in the CNS, its detrimental effects—especially its promotion of neuroinflammation—commonly dominate during illness. C IL-6 participates in the pathogenesis of prevalent neurodegenerative disorders, including AD, PD, ALS, HD, and MS. These diseases have different pathological features: e.g., ALS is characterized by the aggregation of TDP-43, while HD is principally associated with the mutation of HTT. Although the exact mechanism is unclear, the expression of IL-6 generally increases with the severity of these diseases. BBB blood–brain barrier, NSC neural stem cell, AD Alzheimer’s disease, Aβ amyloid-beta, NFTs neurofibrillary tangles, PD Parkinson’s disease, ALS amyotrophic lateral sclerosis, TDP-43 TAR DNA-binding protein 43, HD Huntington’s disease, HTT huntingtin protein, MS multiple sclerosis, CNS central nervous system
Effects of IL-6 on Neurogenesis
IL-6 plays a significant role in mammalian neurogenesis, the process whereby neurons and glial cells mature from neural stem cells (NSCs) in specialized niches of the brain [41]. Neurogenesis is a multistage program consisting of proliferation, differentiation, migration, survival, and integration. Proliferation of NSCs is negatively affected by IL-6 [42,43,44], though the underlying mechanism remains unclear. IL‐6 is also a critical regulator of NSC differentiation through inhibiting differentiation of NSCs into neurons while boosting their differentiation into glial cells via the JAK2/STAT3 signaling pathway in dose-dependent manner [43, 45]. In addition, NSCs preconditioned with IL-6 can be reprogrammed and assume new characteristics of tolerance to oxidative stress and angiogenesis induced by STAT3, thus reducing ischemic injury in stroke mice [46].
Effects of IL-6 on Neurons
IL-6 interacts with neurons in a seemingly contradictory manner. On one hand, IL-6 can induce serious injury in cortical pyramidal neurons. Using oxygen consumption rate as an evaluation criterion, cortical neurons exposed to IL-6 had a saliently higher oxygen consumption rate relative to untreated neurons, indirectly implying impaired mitochondrial respiration in the exposed neurons [47]. On the other hand, IL-6 can act as a neuroprotective agent by preserving anterior horn neurons from irreversible virus-induced injury and enhancing the survival of sympathetic neurons [31, 48]. These data demonstrate that effects of IL-6 on neurons may depend on the distribution of brain regions and pathological types.
Effects of IL-6 on Glial Cells
Microglia are the dominant immune cells of the CNS. Exposing microglia to IL-6 potentiates their secretion of inflammatory cytokines, like IL-1β, IL-6 itself, and TNF-α, and promotes their proliferation and repopulation [49,50,51]. Increased concentrations of IL-1β can induce the production of IL-6 in astrocytes, creating a positive feedback loop between astrocytes and microglia that may result in a hyper-inflammatory state—especially in patients with neuroinflammatory diseases.
Besides activating the pro-inflammatory phenotype, IL-6 plays a neuroprotective role in microglia. In acute IL-6 exposure, microglia-like cells will upregulate chemokine secretion and thus recruit additional immune cells to remove necrotic cellular debris at lesion sites [51]. Chronic IL-6 exposure induces microglial proliferation and a desensitized phenotype [52, 53]. Hence, IL-6 not only promotes neuroinflammation and causes neurological impairment, but also repairs brain injury by stimulating the proliferation and regeneration of microglia.
In astrocytes, IL-6 also plays dual functions. It alleviates mitochondrial damage and suppressing astrocyte apoptosis, while it can also recruit T cells to the CNS by enhancing astrocytic CCL20 expression with the aid of sIL-6R and IL-17 [54,55,56,57]. More importantly, the conjunction of IL-6 and sIL-6R can promote the expression of neurotrophins in astrocytes in a dose- and region-dependent manner [58]. The dual effect of IL-6 in microglia and astrocytes underscores its clinical potential in the treatment of neurodegenerative disorders.
Effects of IL-6 on Synapse Formation
As key process in the development of the brain, synapse formation is also regulated by IL-6 [59,60,61]. To determine the correlation between early prenatal inflammation and abnormal neurodevelopment, female mice were injected with IL-6 during pregnancy. The transient elevation of prenatal IL-6 enhanced glutamatergic synaptogenesis and undermined hippocampal connectivity in the offspring [62]. An excessive number of excitatory contacts in the offspring will induce an E/I imbalance: a hallmark of neurodevelopmental defects that cause the development of neurodegenerative disorders in the long term.
Significantly, regardless of the capacity of IL-6 to positively or negatively regulate neural cells, its proinflammatory activities play a dominant role under pathological conditions by bolstering the inflammatory environment and inducing neuroinflammation (Fig. 1B).
The Role of IL-6 in Neurodegenerative Disorders
With the growth of the geriatric population and the attendant rise in the prevalence of neurodegenerative disorders, these diseases are attracting increasing attention from the global research community. The following section reviews the pathological features of several common neurodegenerative disorders (Fig. 1C) and how IL-6 contributes to these diseases.
IL-6 and Alzheimer’s Disease
AD is an age-related neurodegenerative disease characterized by progressive cognitive decline and memory impairment. Furthermore, it is listed as one of the leading causes of death in the elderly population, particularly of those aged ≥ 65 years [63,64,65]. Based on a newly developed prediction model, current number of patients with AD has reached 69 million—a greater figure than the previously estimated 50 million [66], which will continue to increase with the aging population. In consequence, the global economic burden of treating patients with AD will become increasingly heavier and exert an extraordinary influence on society and individuals [64].
Amyloid cascade, tau protein, neuroinflammation, metal ions, and oxidative stress have all been suggested to participate in the pathogenesis of AD and a wealth of evidence has suggested that IL-6 is closely related to these processes. For example, AD is characterized by the appearance and proliferation of beta-amyloid and phosphorylated tau, and the formation of these abnormal proteins can trigger IL-6 production [65, 67]. Elevated IL-6 has proved to promote not only the accumulation of amyloid beta plaques by activating BACE1 and NF-κB [68], but also the generation of neurofibrillary tangles by regulating the CDK5/p35 pathway [69], thus contributing to a vicious circle that leads to exacerbating pathology. Additionally, IL-6 participates in the blood–brain barrier dysfunction, an early pathological hallmark characterized by barrier leakage [70]. By activating the NADPH oxidase pathway, IL-6 downregulate the expression of tight junction proteins in brain endothelial cells, leading to an increase of paracellular permeability. Furthermore, with stimulation of IL-6, CD4+ T cells can be induced to differentiate into Th17 cells, which contribute to beta-amyloid accumulation and neuronal damage through direct cytotoxic effects of IL-17A [71]. Although heterogeneity in study populations has inevitably yielded controversial findings, most of current literature supports the notion that the levels of IL-6 in the serum, CSF, and stool samples are significantly higher in patients with AD than in controls [67, 72,73,74,75,76,77]. Elevated IL-6 correlates inversely with hypothalamic/hippocampal volumes and Mini-Mental State Examination scores, and significantly increases the risk of cognitive decline in AD patients [67, 76, 78]. Based on the marked increase in IL-6 of the AD patients, some researchers have suggested that IL-6 may hold the potential to be a useful marker in AD [79,80,81]. Thereinto, a case–control study has evaluated the diagnostic significance of IL-6 in serum ([AUC] = 0.930), which demonstrated that IL-6 was a promising biomarker to distinguish AD patients from the normal controls [80]. However, further studies are required to find more relevant and stable biomarkers, and to confirm their exact clinical utility in a larger cohort of patients in the future.
Whether IL-6 gene polymorphism contributes to the risk of AD remains unclear. In a study of Chinese Han subjects, participants homozygous for the G allele of rs1800796 were found to have a lower risk of developing late-onset AD [82]. The findings of a Brazilian case–control study contested this conclusion [83]. The ethnic differences between the study populations and their limited sample sizes may account for the contradictory results. While the literature features a similar discrepancy concerning rs1800795, most reports agree that the C allele in CC homozygotes has a negative association with the risk of AD [19, 84, 85]. Hence, whether a genetic polymorphism of IL-6 regulates the risk of AD remains uncertain. Larger, more standardized investigations are needed to settle this question.
Accompanying the discovery regarding the deleterious role of IL-6 in AD, multiple IL-6 production inhibitors have been developed in recent years aim at lowering IL-6 levels to alleviate neuroinflammation in AD [67]. Among them, sulforaphene, verbascoside, sterubin, and xanthoxylin hybrids have shown promising results for the treatment of AD [86,87,88,89]. Meanwhile, tocilizumab, a humanized antibody to IL-6 receptor, has thus far been shown to protect against cognitive deficits in AD models [90]. In addition, the neurodegeneration and cognitive impairment of AD mouse models has been almost completely abolished, when IL-6 trans-signaling was blocked specifically (by crossing them with GFAP-sgp130Fc mice) [91]. The results indicate that blocking IL-6 production or signal transduction does indeed alleviate the burden of AD, suggesting that this may be a new potential therapeutic target at early stages of the disease.
While these agents or methods have shown achieved exciting results in cell cultures or animal models, much time and effort remain before they can undergo testing in clinical trials or be used in clinical application.
IL-6 and Parkinson’s Disease
PD is the second most common neurodegenerative disease. While it is currently estimated to affect 7 million people worldwide, its prevalence is expected to double in the next 30 years [92], as old age is the most important independent risk factor of this disease [93].
Aside from presenting with motor manifestations such as bradykinesia and resting tremor or rigidity, patients with PD also exhibit depression, anxiety, and cognitive decline. These symptoms may result from a selective loss of dopaminergic neurons and the formation of α-synuclein-containing Lewy bodies [94,95,96,97,98,99]. Though specific mechanism underlying the development of such symptoms remains unclear, there is a general consensus that neuroinflammation is involved in the pathogenesis of neurodegeneration consequent of PD [97, 100,101,102].
Among the inflammatory molecules, IL-6, which reflects the neuroinflammatory pathogenesis of the disease, has attracted considerable research interest [103,104,105,106]. On one hand, pathological α-synuclein induces the secretion of IL-6 by microglia; on the other hand, overexpressed IL-6 can trigger toxic neuronal iron accumulation by activating the cellular iron sequestration response, leading to dopaminergic cell death and exacerbating neurodegeneration [107,108,109]. Besides, Th17 cells stimulated by IL-6 can induce dopaminergic neuronal apoptosis via a direct contact or secretion of IL-17A [110, 111].
Similar to AD, the serum and CSF concentrations of IL-6 are markedly higher in patients with PD than healthy controls. This finding reinforces the clinical evidence that the onset of PD is accompanied by an enhanced inflammatory response [38, 112]. Furthermore, a positive correlation was identified between IL-6 level and disease severity whereas those with advanced motor or nonmotor symptoms and fatigue suffer even higher level of IL-6 [113,114,115,116]. Finally, elevated levels of IL-6 may be an independent predictor of increased mortality risk in PD patients [117], and statistical evidence from a Mendelian randomization study concluded that increased concentrations of IL-6 were associated with earlier onset of PD [118]. Given these evidence, abnormally high levels of IL-6 may be used as a potential biomarker for early diagnosis, progressive detection, and prognostic evaluation of PD.
IL-6 not only affects the initiation and progression of neurodegenerative processes in PD, but may also contribute to the treatment of the disorder. The treatment of PD mainly includes both pharmacologic and nonpharmacologic therapies. Levodopa remains the most commonly prescribed medication [95, 119]. With an improved understanding of the pluripotent roles of IL-6 in the pathogenesis of PD, IL-6 inhibitors may become a promising treatment alternative. For instance, the neurotrophic and anti-inflammatory drug, echinacoside, has been demonstrated both in vivo and in vitro to protect dopaminergic neurons by inhibiting the IL-6/JAK2/STAT3 pathway in PD models [120]. Future investigations should thoroughly investigate the role of IL-6 in the pathogenesis of PD to gain greater insight into its clinical potential in preventing and treating PD, as well as improving the affected patients’ quality of life.
IL-6 and Amyotrophic Lateral Sclerosis
ALS is the third-most common adult-onset neurodegenerative disease. With a mean onset age of 60 years, ALS is mainly characterized by the cytoplasmic aggregation of TAR DNA-binding protein 43 and the progressive loss of motor neurons in the brain and spinal cord that eventually causes death within 2–5 years of onset [121, 122].
Accumulating evidence implicates involvement of IL-6 associated neuroinflammation in ALS. Relatively high concentrations of IL-6 in serum, CSF, and astrocytes were observed in patients with ALS, indicating an increased inflammatory response [123,124,125,126]. Furthermore, an association between higher levels of IL-6 and shorter lifespans was observed in the transgenic SOD1G93A mouse model of ALS [127, 128]. One possible reason for this phenomenon is that IL-6 upregulates the activity of pro-inflammatory endothelial cells through the trans-signaling pathway, thus causing barrier damage and accelerating motor neuron death [129].
A deeper understanding of the IL-6-mediated inflammatory response and its role in ALS may inform the use of IL-6 as a diagnostic and prognostic biomarker, as well as provide clues for an endothelial-IL-6-targeting therapy in the future. Though any such therapy has yet to emerge, the development of other intervention strategies that target IL-6 is already underway. The first IL-6 receptor antagonist tocilizumab has been safely used to normalize inflammation in ALS patients [130,131,132]. Furthermore, demonstrating its potential as a neuroprotective agent, the tetanus toxin C-terminal fragment helped to reduce the levels of IL-6 levels in SOD1G93A mice [133]. However, studies of anti-IL-6 drugs and their potential in treating ALS are limited in number and scope. Further research is needed to develop novel, more effective therapies.
IL-6 and Huntington’s Disease
HD is an autosomal dominant neurodegenerative disorder caused by an aberrant CAG repeat expansion in the HTT gene that compromises cognition, motor ability, and behavior [134, 135]. Though symptoms can manifest at any time during a patient’s life, they most commonly begin to present in middle age and remain until death.
Similar to other neurodegenerative diseases, patients with HD and animal models of the disorder exhibit increased plasma levels of IL-6 [136,137,138,139]. A combination of plasma IL-6, IL-10, and IL-5 has been shown to discriminate well between premanifest HD and controls (AUC = 0.81) [140]. Mutant huntingtin appears to cause the production of abnormal monocytes, which release excess IL-6 by upregulating the NF-ĸB signaling pathway and contribute to neurotoxicity [140, 141].Furthermore, IL-6 is detected in elevated concentrations in the saliva and CSF of patients with HD [137, 142]. Higher salivary levels of IL-6 were found to be correlated with higher Total Motor Scores [137], an indicator of disease severity. Hence, salivary IL-6 features potential as a non-invasive biomarker for HD symptom severity. Moreover, in the BACHD murine model of HD, changes in the concentration of IL-6 varied between peripheral organs; higher levels were found in the kidney and heart, and lower concentrations in the spleen [143].
A growing number of supportive and symptomatic management strategies may improve the treatment of HD. Despite the precise molecular mechanisms underlying the elevated expression of IL-6 in patients with HD remaining unknown, the most noteworthy of emerging treatment modalities are those that aim to reduce IL-6 levels. For example, cilostazol’s anti-inflammatory and neuroprotective properties may help to alleviate HD symptoms by acting on the IL-6/JAK2/STAT3 signaling pathways [144]. However, recent evidence also suggests that IL-6 deficiency exacerbates dysregulated behavioral phenotypes in HD model mice by affecting genes associated with synaptic function [145]. The inconsistency between these two findings may be explained by the neuroprotective effect of IL-6: i.e., lowering concentrations IL-6 to excess may be harmful, but maintaining IL-6 at a moderate level may improve outcomes for patients with HD. Future research should explore this supposition and determine the optimal level of IL-6 in patients with HD.
IL-6 and Multiple Sclerosis
As chronic and incurable inflammatory demyelinating disease of the CNS, MS is the most common non-traumatic disabling ailment among young adults between the ages of 20 and 40 years [146]. Despite the relatively early onset of MS, aging is the most relevant factor for its clinical consequences and outcomes, as older patients are more likely to suffer permanent disability after developing MS [147, 148]. According to the data from the Multiple Sclerosis International Federation’s third edition of the Atlas of MS, the prevalence of MS has risen from 2.2 million to 2.8 million since 2013 [149].
Patients with MS exhibit elevated serum and CSF concentrations of IL-6. The levels of IL-6 are especially high in patients with abdominal obesity because abdominal fat accumulation contributes directly to the overproduction of proinflammatory cytokines [150, 151]. Similarly, increased level of IL-6 receptors on CD4+ T cells were detected in MS patients [152]. Though the precise role of IL-6 signaling in MS pathogenesis has not been fully understood, it is possible that IL-6 promotes the differentiation of CD4+ T cells towards Th17 cells by binding with IL-6R, ultimately causing the demyelination of axons [153]. Alternatively, IL-6 may compromise synaptic plasticity directly, an innate method for the CNS to compensate for MS-induced damage, which in turn exacerbate disease progression [154]. Finally, the rs1818879 polymorphism of IL-6 may influence the subclinical neuroinflammatory activities in MS [155]. These hypotheses could explain the positive correlation between IL-6 values and disease severity [156].
Conclusions and perspectives
This review proposes that IL-6, a core inflammatory cytokine, plays a major role in different neurodegenerative disorders. Currently, it is generally accepted that the expression of IL-6 in peripheral blood, CSF, or other body fluids is abnormally high in patients with neurodegenerative diseases. Furthermore, the degree of elevation tends to correlate positively with the severity of the disease.
Although the specific mechanisms in each of these diseases vary, increased IL-6 induces neuroinflammation, which promotes abnormal protein aggregation, damages functioning neurons, impairs synaptic function, and ultimately exacerbates neurodegeneration. Notably, Th17 cells, which differentiate from CD4+ T cells in response to IL-6 stimulation, have been reported to be associated with the pathogenesis of several neurodegenerative diseases, including AD, PD and MS. Th17 cells and their cytokines can induce the aggregation of misfolded proteins and cause neuronal death, through direct cytotoxic effects or the recruitment of immune cells. Although the exact mechanisms of their function remain to be elucidated, existing data suggest that Th17 cells and Th17-related signaling pathways may be potentially effective therapeutic targets.
Currently, the clinical diagnosis of degenerative diseases is made mostly based on clinical symptoms, which may only appear in advanced stages of the disease, thus precluding therapeutic intervention in early stages. There is a need for seeking markers to reveal early pathogenic events, as well as monitor disease progression and treatment response. Indeed, one of the aims of this review is to analyze the potential of IL-6 as a biomarker for diagnosis, progression and prognosis in neurodegenerative diseases. Based on existing research, the diagnostic ability of IL-6 in AD and HD groups has been preliminarily demonstrated [80, 140]. Regrettably, due to the complexity of the nervous system and the ambiguous pathogenesis of various degenerative diseases, convincing evidence of IL-6 being an effective biomarker in other neurodegenerative diseases is still insufficient. To further confirm the role of IL-6 in neurodegenerative disorders, more in-depth studies are needed.
At present, there are no treatments that can cure neurodegenerative disorders or reverse the physical and mental damage they induce. While some drugs approved by the Food and Drug Administration, such as levodopa, donepezil, riluzole, are used in clinical practice, they only relieve symptoms without improving the outcomes of the diseases [95, 157, 158]. Due to the limited application and efficacy of these medicines, finding new therapeutic targets and developing effective treatment plans remains a priority in the decades to come, and IL-6 shows promise as a candidate for the focus of future investigations. Some novel inhibitors of IL-6 have been shown to be useful in attenuating the development of neurodegenerative disorders in animal models and may proceed to human trials. Development of safe and effective anti-IL-6 therapy will benefit patients suffering from neurodegenerative disorders.
Availability of Data and Materials
Not applicable.
Abbreviations
- IL-6:
-
Interleukin-6
- AD:
-
Alzheimer’s disease
- PD:
-
Parkinson’s disease
- ALS:
-
Amyotrophic lateral sclerosis
- HD:
-
Huntington’s disease
- MS:
-
Multiple sclerosis
- CNS:
-
Central nervous system
- IL-1β:
-
Interleukin-1 beta
- IL-6R:
-
IL-6 receptor
- mIL-6R:
-
Membrane-bound IL-6R
- sIL-6R:
-
Soluble IL-6R
- gp130:
-
Glycoprotein 130
- JAK:
-
Janus kinase
- STAT:
-
Signal transducer and activator of transcription
- NSCs:
-
Neural stem cells
- CSF:
-
Cerebrospinal fluid
References
Wilson DM 3rd, Cookson MR, Van Den Bosch L, Zetterberg H, Holtzman DM, Dewachter I (2023) Hallmarks of neurodegenerative diseases. Cell 186:693–714
Hou Y, Dan X, Babbar M, Wei Y, Hasselbalch SG, Croteau DL, Bohr VA (2019) Ageing as a risk factor for neurodegenerative disease. Nat Rev Neurol 15:565–581
Stephenson J, Nutma E, van der Valk P, Amor S (2018) Inflammation in CNS neurodegenerative diseases. Immunology 154:204–219
Erta M, Quintana A, Hidalgo J (2012) Interleukin-6, a major cytokine in the central nervous system. Int J Biol Sci 8:1254–1266
Hirano TYK, Harada H (1986) Complementary DNA for a novel human interleukin (BSF-2) that induces B lymphocytes to produce immunoglobulin. Nature 324:73–76
Somers W, Stahl M, Seehra JS (1997) 1.9 A crystal structure of interleukin 6: implications for a novel mode of receptor dimerization and signaling. EMBO J 16:989–997
Luan D, Dadpey B, Zaid J, Bridge-Comer PE, DeLuca JH, Xia W, Castle J, Reilly SM (2023) Adipocyte-secreted IL-6 sensitizes macrophages to IL-4 signaling. Diabetes 72:367–374
Nara H, Watanabe R (2021) Anti-inflammatory effect of muscle-derived interleukin-6 and its involvement in lipid metabolism. Int J Mol Sci 22(18):9889
Said EA, Al-Reesi I, Al-Shizawi N, Jaju S, Al-Balushi MS, Koh CY, Al-Jabri AA, Jeyaseelan L (2021) Defining IL-6 levels in healthy individuals: a meta-analysis. J Med Virol 93:3915–3924
Wei J, Xu H, Davies JL, Hemmings GP (1992) Increase of plasma IL-6 concentration with age in healthy subjects. Life Sci 51:1953–1956
Tyrrell DJ, Blin MG, Song J, Wood SC, Zhang M, Beard DA, Goldstein DR (2020) Age-associated mitochondrial dysfunction accelerates atherogenesis. Circ Res 126:298–314
Alanazi AZ, Clark MA (2019) Angiotensin III induces JAK2/STAT3 leading to IL-6 production in rat vascular smooth muscle cells. Int J Mol Sci 20(22):5551
Liu JF, Chi MC, Lin CY, Lee CW, Chang TM, Han CK, Huang YL, Fong YC, Chen HT, Tang CH (2021) PM2.5 facilitates IL-6 production in human osteoarthritis synovial fibroblasts via ASK1 activation. J Cell Physiol 236:2205–2213
Russell FD, Visagie JC, Noll JL (2022) Secretion of IL-6 by fibroblasts exposed to Australian honeys involves lipopolysaccharide and is independent of floral source. Sci Rep 12:16628
Choi H, Kim K, Han J, Choi H, Jin SH, Lee EK, Shin DW, Lee TR, Lee AY, Noh M (2012) Kojic acid-induced IL-6 production in human keratinocytes plays a role in its anti-melanogenic activity in skin. J Dermatol Sci 66:207–215
Gerosa RC, Boettcher S, Kovtonyuk LV, Hausmann A, Hardt WD, Hidalgo J, Nombela-Arrieta C, Manz MG (2021) CXCL12-abundant reticular cells are the major source of IL-6 upon LPS stimulation and thereby regulate hematopoiesis. Blood Adv 5:5002–5015
Zhang Y, Li B, Ning B (2022) Evaluating IL-6 and IL-10 as rapid diagnostic tools for Gram-negative bacteria and as disease severity predictors in pediatric sepsis patients in the intensive care unit. Front Immunol 13:1043968
Merz C, von Massenhausen A, Queisser A, Vogel W, Andren O, Kirfel J, Duensing S, Perner S, Nowak M (2016) IL-6 overexpression in ERG-positive prostate cancer is mediated by prostaglandin receptor EP2. Am J Pathol 186:974–984
Licastro F, Grimaldi LM, Bonafe M, Martina C, Olivieri F, Cavallone L, Giovanietti S, Masliah E, Franceschi C (2003) Interleukin-6 gene alleles affect the risk of Alzheimer’s disease and levels of the cytokine in blood and brain. Neurobiol Aging 24:921–926
Pereira DS, Garcia DM, Narciso FM, Santos ML, Dias JM, Queiroz BZ, Souza ER, Nobrega OT, Pereira LS (2011) Effects of 174 G/C polymorphism in the promoter region of the interleukin-6 gene on plasma IL-6 levels and muscle strength in elderly women. Braz J Med Biol Res 44:123–129
Walston J, Arking DE, Fallin D, Li T, Beamer B, Xue Q, Ferrucci L, Fried LP, Chakravarti A (2005) IL-6 gene variation is not associated with increased serum levels of IL-6, muscle, weakness, or frailty in older women. Exp Gerontol 40:344–352
Zhang G, Zhou B, Wang W, Zhang M, Zhao Y, Wang Z, Yang L, Zhai J, Feng CG, Wang J, Chen X (2012) A functional single-nucleotide polymorphism in the promoter of the gene encoding interleukin 6 is associated with susceptibility to tuberculosis. J Infect Dis 205:1697–1704
Riethmueller S, Somasundaram P, Ehlers JC, Hung CW, Flynn CM, Lokau J, Agthe M, Dusterhoft S, Zhu Y, Grotzinger J, Lorenzen I, Koudelka T, Yamamoto K, Pickhinke U, Wichert R, Becker-Pauly C, Radisch M, Albrecht A, Hessefort M, Stahnke D, Unverzagt C, Rose-John S, Tholey A, Garbers C (2017) Proteolytic origin of the soluble human IL-6R in vivo and a decisive role of N-glycosylation. PLoS Biol 15:e2000080
Lust JA, Donovan KA, Kline MP, Greipp PR, Kyle RA, Maihle NJ (1992) Isolation of an mRNA encoding a soluble form of the human interleukin-6 receptor. Cytokine 4:96–100
Wilkinson AN, Gartlan KH, Kelly G, Samson LD, Olver SD, Avery J, Zomerdijk N, Tey SK, Lee JS, Vuckovic S, Hill GR (2018) Granulocytes are unresponsive to IL-6 due to an absence of gp130. J Immunol 200:3547–3555
Hibi M, Murakami M, Saito M, Hirano T, Taga T, Kishimoto T (1990) Molecular cloning and expression of an IL-6 signal transducer, gp130. Cell 63:1149–1157
Boulanger MJ, Chow DC, Brevnova EE, Garcia KC (2003) Hexameric structure and assembly of the interleukin-6/IL-6 alpha-receptor/gp130 complex. Science 300:2101–2104
Heink S, Yogev N, Garbers C, Herwerth M, Aly L, Gasperi C, Husterer V, Croxford AL, Moller-Hackbarth K, Bartsch HS, Sotlar K, Krebs S, Regen T, Blum H, Hemmer B, Misgeld T, Wunderlich TF, Hidalgo J, Oukka M, Rose-John S, Schmidt-Supprian M, Waisman A, Korn T (2017) Trans-presentation of IL-6 by dendritic cells is required for the priming of pathogenic T(H)17 cells. Nat Immunol 18:74–85
Gadient RA, Otten U (1994) Identification of interleukin-6 (IL-6)-expressing neurons in the cerebellum and hippocampus of normal adult rats. Neurosci Lett 182:243–246
Gadient RA, Otten U (1994) Expression of interleukin-6 (IL-6) and interleukin-6 receptor (IL-6R) mRNAs in rat brain during postnatal development. Brain Res 637:10–14
Marz P, Cheng JG, Gadient RA, Patterson PH, Stoyan T, Otten U, Rose-John S (1998) Sympathetic neurons can produce and respond to interleukin 6. Proc Natl Acad Sci U S A 95:3251–3256
Sallmann S, Juttler E, Prinz S, Petersen N, Knopf U, Weiser T, Schwaninger M (2000) Induction of interleukin-6 by depolarization of neurons. J Neurosci 20:8637–8642
Van Wagoner NJ, Oh JW, Repovic P, Benveniste EN (1999) Interleukin-6 (IL-6) production by astrocytes: autocrine regulation by IL-6 and the soluble IL-6 receptor. J Neurosci 19:5236–5244
Banks WA, Kastin AJ, Gutierrez EG (1994) Penetration of interleukin-6 across the murine blood-brain barrier. Neurosci Lett 179:53–56
Liu H, Wu X, Luo J, Wang X, Guo H, Feng D, Zhao L, Bai H, Song M, Liu X, Guo W, Li X, Yue L, Wang B, Qu Y (2019) Pterostilbene Attenuates Astrocytic Inflammation and Neuronal Oxidative Injury After Ischemia-Reperfusion by Inhibiting NF-kappaB Phosphorylation. Front Immunol 10:2408
Jankord R, Zhang R, Flak JN, Solomon MB, Albertz J, Herman JP (2010) Stress activation of IL-6 neurons in the hypothalamus. Am J Physiol Regul Integr Comp Physiol 299:R343-351
Swardfager W, Lanctot K, Rothenburg L, Wong A, Cappell J, Herrmann N (2010) A meta-analysis of cytokines in Alzheimer’s disease. Biol Psychiatry 68:930–941
Qin XY, Zhang SP, Cao C, Loh YP, Cheng Y (2016) Aberrations in peripheral inflammatory cytokine levels in Parkinson disease: a systematic review and meta-analysis. JAMA Neurol 73:1316–1324
Zhang H, Wu J, Shen FF, Yuan YS, Li X, Ji P, Zhu L, Sun L, Ding J, Niu Q, Zhang KZ (2020) Activated Schwann cells and increased inflammatory cytokines IL-1beta, IL-6, and TNF-alpha in patients’ sural nerve are lack of tight relationship with specific sensory disturbances in Parkinson’s disease. CNS Neurosci Ther 26:518–526
Stampanoni Bassi M, Iezzi E, Drulovic J, Pekmezovic T, Gilio L, Furlan R, Finardi A, Marfia GA, Sica F, Centonze D, Buttari F (2020) IL-6 in the cerebrospinal fluid signals disease activity in multiple sclerosis. Front Cell Neurosci 14:120
Sun GJ, Zhou Y, Stadel RP, Moss J, Yong JH, Ito S, Kawasaki NK, Phan AT, Oh JH, Modak N, Reed RR, Toni N, Song H, Ming GL (2015) Tangential migration of neuronal precursors of glutamatergic neurons in the adult mammalian brain. Proc Natl Acad Sci U S A 112:9484–9489
Monje ML, Toda H, Palmer TD (2003) Inflammatory blockade restores adult hippocampal neurogenesis. Science 302:1760–1765
Kong X, Gong Z, Zhang L, Sun X, Ou Z, Xu B, Huang J, Long D, He X, Lin X, Li Q, Xu L, Xuan A (2019) JAK2/STAT3 signaling mediates IL-6-inhibited neurogenesis of neural stem cells through DNA demethylation/methylation. Brain Behav Immun 79:159–173
Storer MA, Gallagher D, Fatt MP, Simonetta JV, Kaplan DR, Miller FD (2018) Interleukin-6 regulates adult neural stem cell numbers during normal and abnormal post-natal development. Stem Cell Reports 10:1464–1480
Taga T, Fukuda S (2005) Role of IL-6 in the neural stem cell differentiation. Clin Rev Allergy Immunol 28:249–256
Sakata H, Narasimhan P, Niizuma K, Maier CM, Wakai T, Chan PH (2012) Interleukin 6-preconditioned neural stem cells reduce ischaemic injury in stroke mice. Brain 135:3298–3310
Kathuria A, Lopez-Lengowski K, Roffman JL, Karmacharya R (2022) Distinct effects of interleukin-6 and interferon-gamma on differentiating human cortical neurons. Brain Behav Immun 103:97–108
Pavelko KD, Howe CL, Drescher KM, Gamez JD, Johnson AJ, Wei T, Ransohoff RM, Rodriguez M (2003) Interleukin-6 protects anterior horn neurons from lethal virus-induced injury. J Neurosci 23:481–492
West PK, Viengkhou B, Campbell IL, Hofer MJ (2019) Microglia responses to interleukin-6 and type I interferons in neuroinflammatory disease. Glia 67:1821–1841
Willis EF, MacDonald KPA, Nguyen QH, Garrido AL, Gillespie ER, Harley SBR, Bartlett PF, Schroder WA, Yates AG, Anthony DC, Rose-John S, Ruitenberg MJ, Vukovic J (2020) Repopulating microglia promote brain repair in an IL-6-dependent manner. Cell 180(833–846):e816
Couch ACM, Solomon S, Duarte RRR, Marrocu A, Sun Y, Sichlinger L, Matuleviciute R, Polit LD, Hanger B, Brown A, Kordasti S, Srivastava DP, Vernon AC (2023) Acute IL-6 exposure triggers canonical IL6Ra signaling in hiPSC microglia, but not neural progenitor cells. Brain Behav Immun 110:43–59
Recasens M, Almolda B, Perez-Clausell J, Campbell IL, Gonzalez B, Castellano B (2021) Chronic exposure to IL-6 induces a desensitized phenotype of the microglia. J Neuroinflammation 18:31
West PK, McCorkindale AN, Guennewig B, Ashhurst TM, Viengkhou B, Hayashida E, Jung SR, Butovsky O, Campbell IL, Hofer MJ (2022) The cytokines interleukin-6 and interferon-alpha induce distinct microglia phenotypes. J Neuroinflammation 19:96
Chen XL, Wang Y, Peng WW, Zheng YJ, Zhang TN, Wang PJ, Huang JD, Zeng QY (2018) Effects of interleukin-6 and IL-6/AMPK signaling pathway on mitochondrial biogenesis and astrocytes viability under experimental septic condition. Int Immunopharmacol 59:287–294
Gu Y, He M, Zhou X, Liu J, Hou N, Bin T, Zhang Y, Li T, Chen J (2016) Endogenous IL-6 of mesenchymal stem cell improves behavioral outcome of hypoxic-ischemic brain damage neonatal rats by supressing apoptosis in astrocyte. Sci Rep 6:18587
Meares GP, Ma X, Qin H, Benveniste EN (2012) Regulation of CCL20 expression in astrocytes by IL-6 and IL-17. Glia 60:771–781
Levison SW, Jiang FJ, Stoltzfus OK, Ducceschi MH (2000) IL-6-type cytokines enhance epidermal growth factor-stimulated astrocyte proliferation. Glia 32:328–337
Marz P, Heese K, Dimitriades-Schmutz B, Rose-John S, Otten U (1999) Role of interleukin-6 and soluble IL-6 receptor in region-specific induction of astrocytic differentiation and neurotrophin expression. Glia 26:191–200
Faust TE, Schafer DP (2021) IL-6 boosts synaptogenesis STAT! Immunity 54:2444–2446
Gruol DL (2015) IL-6 regulation of synaptic function in the CNS. Neuropharmacology 96:42–54
Rudolph MD, Graham AM, Feczko E, Miranda-Dominguez O, Rasmussen JM, Nardos R, Entringer S, Wadhwa PD, Buss C, Fair DA (2018) Maternal IL-6 during pregnancy can be estimated from newborn brain connectivity and predicts future working memory in offspring. Nat Neurosci 21:765–772
Mirabella F, Desiato G, Mancinelli S, Fossati G, Rasile M, Morini R, Markicevic M, Grimm C, Amegandjin C, Termanini A, Peano C, Kunderfranco P, di Cristo G, Zerbi V, Menna E, Lodato S, Matteoli M, Pozzi D (2021) Prenatal interleukin 6 elevation increases glutamatergic synapse density and disrupts hippocampal connectivity in offspring. Immunity 54:2611-2631 e2618
Lane CA, Hardy J, Schott JM (2018) Alzheimer’s disease. Eur J Neurol 25:59–70
Joseph G, Bryan J, Tricia J, Jessica R, Kezia S, Sarah T, Jennifer W (2023) 2023 Alzheimer’s disease facts and figures. Alzheimers Dement 19:1598–1695
Hansson O, Edelmayer RM, Boxer AL, Carrillo MC, Mielke MM, Rabinovici GD, Salloway S, Sperling R, Zetterberg H, Teunissen CE (2022) The Alzheimer’s Association appropriate use recommendations for blood biomarkers in Alzheimer’s disease. Alzheimers Dement 18:2669–2686
Gustavsson A, Norton N, Fast T, Frolich L, Georges J, Holzapfel D, Kirabali T, Krolak-Salmon P, Rossini PM, Ferretti MT, Lanman L, Chadha AS, van der Flier WM (2023) Global estimates on the number of persons across the Alzheimer’s disease continuum. Alzheimers Dement 19:658–670
Lyra ESNM, Goncalves RA, Pascoal TA, Lima-Filho RAS, Resende EPF, Vieira ELM, Teixeira AL, de Souza LC, Peny JA, Fortuna JTS, Furigo IC, Hashiguchi D, Miya-Coreixas VS, Clarke JR, Abisambra JF, Longo BM, Donato J Jr, Fraser PE, Rosa-Neto P, Caramelli P, Ferreira ST, De Felice FG (2021) Pro-inflammatory interleukin-6 signaling links cognitive impairments and peripheral metabolic alterations in Alzheimer’s disease. Transl Psychiatry 11:251
Calsolaro V, Edison P (2016) Neuroinflammation in Alzheimer’s disease: current evidence and future directions. Alzheimers Dement 12:719–732
Quintanilla RA, Orellana DI, Gonzalez-Billault C, Maccioni RB (2004) Interleukin-6 induces Alzheimer-type phosphorylation of tau protein by deregulating the cdk5/p35 pathway. Exp Cell Res 295:245–257
Rochfort KD, Collins LE, Murphy RP, Cummins PM (2014) Downregulation of blood-brain barrier phenotype by proinflammatory cytokines involves NADPH oxidase-dependent ROS generation: consequences for interendothelial adherens and tight junctions. PLoS ONE 9:e101815
Zenaro E, Pietronigro E, Della Bianca V, Piacentino G, Marongiu L, Budui S, Turano E, Rossi B, Angiari S, Dusi S, Montresor A, Carlucci T, Nani S, Tosadori G, Calciano L, Catalucci D, Berton G, Bonetti B, Constantin G (2015) Neutrophils promote Alzheimer’s disease-like pathology and cognitive decline via LFA-1 integrin. Nat Med 21:880–886
Shen XN, Niu LD, Wang YJ, Cao XP, Liu Q, Tan L, Zhang C, Yu JT (2019) Inflammatory markers in Alzheimer’s disease and mild cognitive impairment: a meta-analysis and systematic review of 170 studies. J Neurol Neurosurg Psychiatry 90:590–598
Kaur D, Sharma V, Deshmukh R (2019) Activation of microglia and astrocytes: a roadway to neuroinflammation and Alzheimer’s disease. Inflammopharmacology 27:663–677
Gulmammadli N, Konukoglu D, Merve Kurtulus E, Tezen D, Ibrahim Erbay M, Bozluolcay M (2022) Serum sirtuin-1, HMGB1-TLR4, NF-KB and IL-6 levels in Alzheimer’s: the relation between neuroinflammatory pathway and severity of dementia. Curr Alzheimer Res. 19:841–848
Wang SS, Li XH, Liu P, Li J, Liu L (2022) The relationship between Alzheimer’s disease and intestinal microflora structure and inflammatory factors. Front Aging Neurosci 14:972982
Brosseron F, Maass A, Kleineidam L, Ravichandran KA, Kolbe CC, Wolfsgruber S, Santarelli F, Hasler LM, McManus R, Ising C, Roske S, Peters O, Cosma NC, Schneider LS, Wang X, Priller J, Spruth EJ, Altenstein S, Schneider A, Fliessbach K, Wiltfang J, Schott BH, Buerger K, Janowitz D, Dichgans M, Perneczky R, Rauchmann BS, Teipel S, Kilimann I, Gorss D, Laske C, Munk MH, Duzel E, Yakupow R, Dobisch L, Metzger CD, Glanz W, Ewers M, Dechent P, Haynes JD, Scheffler K, Roy N, Rostamzadeh A, Spottke A, Ramirez A, Mengel D, Synofzik M, Jucker M, Latz E, Jessen F, Wagner M, Heneka MT, group Ds, (2023) Serum IL-6, sAXL, and YKL-40 as systemic correlates of reduced brain structure and function in Alzheimer’s disease: results from the DELCODE study. Alzheimers Res Ther 15:13
Lopez-Rodriguez AB, Hennessy E, Murray CL, Nazmi A, Delaney HJ, Healy D, Fagan SG, Rooney M, Stewart E, Lewis A, de Barra N, Scarry P, Riggs-Miller L, Boche D, Cunningham MO, Cunningham C (2021) Acute systemic inflammation exacerbates neuroinflammation in Alzheimer’s disease: IL-1beta drives amplified responses in primed astrocytes and neuronal network dysfunction. Alzheimers Dement 17:1735–1755
Leonardo S, Fregni F (2023) Association of inflammation and cognition in the elderly: a systematic review and meta-analysis. Front Aging Neurosci 15:1069439
Anuradha U, Kumar A, Singh RK (2022) The clinical correlation of proinflammatory and anti-inflammatory biomarkers with Alzheimer disease: a meta-analysis. Neurol Sci 43:285–298
Wang J, Zhou F, Xiong CE, Wang GP, Chen LW, Zhang YT, Qi SG, Wang ZH, Mei C, Xu YJ, Zhan JB, Cheng J (2023) Serum sirtuin1: a potential blood biomarker for early diagnosis of Alzheimer’s disease. Aging (Albany NY) 15:9464–9478
Lai KSP, Liu CS, Rau A, Lanctot KL, Kohler CA, Pakosh M, Carvalho AF, Herrmann N (2017) Peripheral inflammatory markers in Alzheimer’s disease: a systematic review and meta-analysis of 175 studies. J Neurol Neurosurg Psychiatry 88:876–882
Zhao J, Liu P, Hua L, Yang X, Zeng Z, Li X, Wang S, Liu Y, Liu Y, Wang Y (2020) Haplotype analysis on association between variants of interleukin 6 (IL-6) and late-onset Alzheimer’s disease in a Chinese Han population. Exp Gerontol 131:110813
Rasmussen L, Delabio R, Horiguchi L, Mizumoto I, Terazaki CR, Mazzotti D, Bertolucci PH, Pinhel MA, Souza D, Krieger H, Kawamata C, Minett T, Smith MC, Payao SL (2013) Association between interleukin 6 gene haplotype and Alzheimer’s disease: a Brazilian case-control study. J Alzheimers Dis 36:733–738
Faltraco F, Burger K, Zill P, Teipel SJ, Moller HJ, Hampel H, Bondy B, Ackenheil M (2003) Interleukin-6-174 G/C promoter gene polymorphism C allele reduces Alzheimer’s disease risk. J Am Geriatr Soc 51:578–579
Sawkulycz X, Bradburn S, Robinson A, Payton A, Pendleton N, Murgatroyd C (2020) Regulation of interleukin 6 by a polymorphic CpG within the frontal cortex in Alzheimer’s disease. Neurobiol Aging 92:75–81
Yang W, Liu Y, Xu QQ, Xian YF, Lin ZX (2020) Sulforaphene ameliorates neuroinflammation and hyperphosphorylated tau protein via regulating the PI3K/Akt/GSK-3beta pathway in experimental models of Alzheimer’s disease. Oxid Med Cell Longev 2020:4754195
Kaur S, Bansal Y (2022) Design, molecular docking, synthesis and evaluation of xanthoxylin hybrids as dual inhibitors of IL-6 and acetylcholinesterase for Alzheimer’s disease. Bioorg Chem 121:105670
Chen S, Liu H, Wang S, Jiang H, Gao L, Wang L, Teng L, Wang C, Wang D (2022) The neuroprotection of verbascoside in Alzheimer’s disease mediated through mitigation of neuroinflammation via blocking NF-kappaB-p65 signaling. Nutrients 14(1):1417
Kazmi I, Al-Abbasi FA, Afzal M, Shahid Nadeem M, Altayb HN (2023) Sterubin protects against chemically-induced Alzheimer’s disease by reducing biomarkers of inflammation- IL-6/ IL-beta/ TNF-alpha and oxidative stress- SOD/MDA in rats. Saudi J Biol Sci 30:103560
Elcioglu HK, Aslan E, Ahmad S, Alan S, Salva E, Elcioglu OH, Kabasakal L (2016) Tocilizumab’s effect on cognitive deficits induced by intracerebroventricular administration of streptozotocin in Alzheimer’s model. Mol Cell Biochem 420:21–28
Escrig A, Canal C, Sanchis P, Fernandez-Gayol O, Montilla A, Comes G, Molinero A, Giralt M, Gimenez-Llort L, Becker-Pauly C, Rose-John S, Hidalgo J (2019) IL-6 trans-signaling in the brain influences the behavioral and physio-pathological phenotype of the Tg2576 and 3xTgAD mouse models of Alzheimer’s disease. Brain Behav Immun 82:145–159
Tolosa E, Garrido A, Scholz SW, Poewe W (2021) Challenges in the diagnosis of Parkinson’s disease. Lancet Neurol 20:385–397
Rodriguez M, Rodriguez-Sabate C, Morales I, Sanchez A, Sabate M (2015) Parkinson’s disease as a result of aging. Aging Cell 14:293–308
Reich SG, Savitt JM (2019) Parkinson’s disease. Med Clin North Am 103:337–350
Armstrong MJ, Okun MS (2020) Diagnosis and treatment of parkinson disease: a review. JAMA 323:548–560
Cacabelos R (2017) Parkinson’s disease: from pathogenesis to pharmacogenomics. Int J Mol Sci 18(3):551
Schapira AH, Jenner P (2011) Etiology and pathogenesis of Parkinson’s disease. Mov Disord 26:1049–1055
Wakabayashi K, Tanji K, Odagiri S, Miki Y, Mori F, Takahashi H (2013) The Lewy body in Parkinson’s disease and related neurodegenerative disorders. Mol Neurobiol 47:495–508
Cong S, Xiang C, Zhang S, Zhang T, Wang H, Cong S (2022) Prevalence and clinical aspects of depression in Parkinson’s disease: a systematic review and meta-analysis of 129 studies. Neurosci Biobehav Rev 141:104749
Liu TW, Chen CM, Chang KH (2022) Biomarker of neuroinflammation in Parkinson’s disease. Int J Mol Sci 23(8):4148
Marogianni C, Sokratous M, Dardiotis E, Hadjigeorgiou GM, Bogdanos D, Xiromerisiou G (2020) Neurodegeneration and inflammation-an interesting interplay in Parkinson’s disease. Int J Mol Sci 21(22):8421
Lee SYH, Yates NJ, Tye SJ (2022) Inflammatory mechanisms in parkinson’s disease: from pathogenesis to targeted therapies. Neuroscientist 28:485–506
Rabenstein M, Besong Agbo D, Wolf E, Dams J, Nicolai M, Roeder A, Bacher M, Dodel RC, Noelker C (2019) Effect of naturally occurring alpha-synuclein-antibodies on toxic alpha-synuclein-fragments. Neurosci Lett 704:181–188
Nash Y, Schmukler E, Trudler D, Pinkas-Kramarski R, Frenkel D (2017) DJ-1 deficiency impairs autophagy and reduces alpha-synuclein phagocytosis by microglia. J Neurochem 143:584–594
Dohgu S, Takata F, Matsumoto J, Kimura I, Yamauchi A, Kataoka Y (2019) Monomeric alpha-synuclein induces blood-brain barrier dysfunction through activated brain pericytes releasing inflammatory mediators in vitro. Microvasc Res 124:61–66
Du T, Wu Z, Luo H, Lu S, Ma K (2019) Injection of alpha-syn-98 aggregates into the brain triggers alpha-synuclein pathology and an inflammatory response. Front Mol Neurosci 12:189
Li XZ, Bai LM, Yang YP, Luo WF, Hu WD, Chen JP, Mao CJ, Liu CF (2009) Effects of IL-6 secreted from astrocytes on the survival of dopaminergic neurons in lipopolysaccharide-induced inflammation. Neurosci Res 65:252–258
Ma J, Gao J, Niu M, Zhang X, Wang J, Xie A (2020) P2X4R overexpression upregulates interleukin-6 and exacerbates 6-OHDA-induced dopaminergic degeneration in a rat model of PD. Front Aging Neurosci 12:580068
Sterling JK, Kam TI, Guttha S, Park H, Baumann B, Mehrabani-Tabari AA, Schultz H, Anderson B, Alnemri A, Chou SC, Troncoso JC, Dawson VL, Dawson TM, Dunaief JL (2022) Interleukin-6 triggers toxic neuronal iron sequestration in response to pathological alpha-synuclein. Cell Rep 38:110358
Sommer A, Marxreiter F, Krach F, Fadler T, Grosch J, Maroni M, Graef D, Eberhardt E, Riemenschneider MJ, Yeo GW, Kohl Z, Xiang W, Gage FH, Winkler J, Prots I, Winner B (2018) Th17 lymphocytes induce neuronal cell death in a human iPSC-based model of Parkinson’s disease. Cell Stem Cell 23(123–131):e126
Gate D, Tapp E, Leventhal O, Shahid M, Nonninger TJ, Yang AC, Strempfl K, Unger MS, Fehlmann T, Oh H, Channappa D, Henderson VW, Keller A, Aigner L, Galasko DR, Davis MM, Poston KL, Wyss-Coray T (2021) CD4(+) T cells contribute to neurodegeneration in Lewy body dementia. Science 374:868–874
Chen X, Hu Y, Cao Z, Liu Q, Cheng Y (2018) Cerebrospinal fluid inflammatory cytokine aberrations in alzheimer’s disease, parkinson’s disease and amyotrophic lateral sclerosis: a systematic review and meta-analysis. Front Immunol 9:2122
Hofmann KW, Schuh AF, Saute J, Townsend R, Fricke D, Leke R, Souza DO, Portela LV, Chaves ML, Rieder CR (2009) Interleukin-6 serum levels in patients with Parkinson’s disease. Neurochem Res 34:1401–1404
Pereira JR, Santos LVD, Santos RMS, Campos ALF, Pimenta AL, de Oliveira MS, Bacheti GG, Rocha NP, Teixeira AL, Christo PP, Scalzo PL (2016) IL-6 serum levels are elevated in Parkinson’s disease patients with fatigue compared to patients without fatigue. J Neurol Sci 370:153–156
Green HF, Khosousi S, Svenningsson P (2019) Plasma IL-6 and IL-17A correlate with severity of motor and non-motor symptoms in Parkinson’s disease. J Parkinsons Dis 9:705–709
Kim R, Kim HJ, Shin JH, Lee CY, Jeon SH, Jeon B (2022) Serum inflammatory markers and progression of nonmotor symptoms in early Parkinson’s disease. Mov Disord 37:1535–1541
Dufek M, Rektorova I, Thon V, Lokaj J, Rektor I (2015) Interleukin-6 May contribute to mortality in parkinson’s disease patients: a 4-year prospective study. Parkinsons Dis 2015:898192
Bottigliengo D, Foco L, Seibler P, Klein C, Konig IR, Del Greco MF (2022) A Mendelian randomization study investigating the causal role of inflammation on Parkinson’s disease. Brain 145:3444–3453
Vijiaratnam N, Simuni T, Bandmann O, Morris HR, Foltynie T (2021) Progress towards therapies for disease modification in Parkinson’s disease. Lancet Neurol 20:559–572
Yang X, Yv Q, Ye F, Chen S, He Z, Li W, Dong F (2022) Echinacoside protects dopaminergic neurons through regulating IL-6/JAK2/STAT3 pathway in Parkinson’s disease model. Front Pharmacol 13:848813
Feldman EL, Goutman SA, Petri S, Mazzini L, Savelieff MG, Shaw PJ, Sobue G (2022) Amyotrophic lateral sclerosis. Lancet 400:1363–1380
Wijesekera LC, Leigh PN (2009) Amyotrophic lateral sclerosis. Orphanet J Rare Dis 4:3
Hu Y, Cao C, Qin XY, Yu Y, Yuan J, Zhao Y, Cheng Y (2017) Increased peripheral blood inflammatory cytokine levels in amyotrophic lateral sclerosis: a meta-analysis study. Sci Rep 7:9094
Ono S, Hu J, Shimizu N, Imai T, Nakagawa H (2001) Increased interleukin-6 of skin and serum in amyotrophic lateral sclerosis. J Neurol Sci 187:27–34
Moreau C, Devos D, Brunaud-Danel V, Defebvre L, Perez T, Destee A, Tonnel AB, Lassalle P, Just N (2005) Elevated IL-6 and TNF-alpha levels in patients with ALS: inflammation or hypoxia? Neurology 65:1958–1960
Chen Y, Xia K, Chen L, Fan D (2019) Increased interleukin-6 levels in the astrocyte-derived exosomes of sporadic amyotrophic lateral sclerosis patients. Front Neurosci 13:574
Lu CH, Allen K, Oei F, Leoni E, Kuhle J, Tree T, Fratta P, Sharma N, Sidle K, Howard R, Orrell R, Fish M, Greensmith L, Pearce N, Gallo V, Malaspina A (2016) Systemic inflammatory response and neuromuscular involvement in amyotrophic lateral sclerosis. Neurol Neuroimmunol Neuroinflamm 3:e244
Moreno-Martinez L, de la Torre M, Toivonen JM, Zaragoza P, Garcia-Redondo A, Calvo AC, Osta R (2019) Circulating Cytokines could not be good prognostic biomarkers in a mouse model of amyotrophic lateral sclerosis. Front Immunol 10:801
Garbuzova-Davis S, Ehrhart J, Sanberg PR, Borlongan CV (2018) Potential role of humoral IL-6 cytokine in mediating pro-inflammatory endothelial cell response in amyotrophic lateral sclerosis. Int J Mol Sci 19(2):423
Mizwicki MT, Fiala M, Magpantay L, Aziz N, Sayre J, Liu G, Siani A, Chan D, Martinez-Maza O, Chattopadhyay M, La Cava A (2012) Tocilizumab attenuates inflammation in ALS patients through inhibition of IL6 receptor signaling. Am J Neurodegener Dis 1:305–315
Fiala M, Mizwicki MT, Weitzman R, Magpantay L, Nishimoto N (2013) Tocilizumab infusion therapy normalizes inflammation in sporadic ALS patients. Am J Neurodegener Dis 2:129–139
Milligan C, Atassi N, Babu S, Barohn RJ, Caress JB, Cudkowicz ME, Evora A, Hawkins GA, Wosiski-Kuhn M, Macklin EA, Shefner JM, Simmons Z, Bowser RP, Ladha SS (2021) Tocilizumab is safe and tolerable and reduces C-reactive protein concentrations in the plasma and cerebrospinal fluid of ALS patients. Muscle Nerve 64:309–320
Moreno-Martinez L, de la Torre M, Munoz MJ, Zaragoza P, Aguilera J, Calvo AC, Osta R (2020) Neuroprotective fragment C of tetanus toxin modulates IL-6 in an ALS mouse model. Toxins (Basel) 12(5):330
Walker FO (2007) Huntington’s disease. Lancet 369:218–228
McColgan P, Tabrizi SJ (2018) Huntington’s disease: a clinical review. Eur J Neurol 25:24–34
Saba J, Couselo FL, Bruno J, Carniglia L, Durand D, Lasaga M, Caruso C (2022) Neuroinflammation in Huntington’s disease: a starring role for astrocyte and microglia. Curr Neuropharmacol 20:1116–1143
Corey-Bloom J, Fischer RS, Kim A, Snell C, Parkin GM, Granger DA, Granger SW, Thomas EA (2020) Levels of interleukin-6 in saliva, but not plasma, correlate with clinical metrics in Huntington’s disease patients and healthy control subjects. Int J Mol Sci 21(17):6363
Yang HM, Yang S, Huang SS, Tang BS, Guo JF (2017) Microglial activation in the pathogenesis of Huntington’s disease. Front Aging Neurosci 9:193
Chang KH, Wu YR, Chen YC, Chen CM (2015) Plasma inflammatory biomarkers for Huntington’s disease patients and mouse model. Brain Behav Immun 44:121–127
Bjorkqvist M, Wild EJ, Thiele J, Silvestroni A, Andre R, Lahiri N, Raibon E, Lee RV, Benn CL, Soulet D, Magnusson A, Woodman B, Landles C, Pouladi MA, Hayden MR, Khalili-Shirazi A, Lowdell MW, Brundin P, Bates GP, Leavitt BR, Moller T, Tabrizi SJ (2008) A novel pathogenic pathway of immune activation detectable before clinical onset in Huntington’s disease. J Exp Med 205:1869–1877
Jang M, Lee SE, Cho IH (2018) Adeno-associated viral vector serotype DJ-mediated overexpression of N171–82Q-mutant Huntingtin in the striatum of juvenile mice is a new model for Huntington’s disease. Front Cell Neurosci 12:157
Rodrigues FB, Byrne LM, McColgan P, Robertson N, Tabrizi SJ, Zetterberg H, Wild EJ (2016) Cerebrospinal fluid inflammatory biomarkers reflect clinical severity in Huntington’s disease. PLoS ONE 11:e0163479
Valadao PAC, Oliveira BDS, Joviano-Santos JV, Vieira ELM, Rocha NP, Teixeira AL, Guatimosim C, de Miranda AS (2019) Inflammatory changes in peripheral organs in the BACHD murine model of Huntington’s disease. Life Sci 232:116653
El-Abhar H, Abd El Fattah MA, Wadie W, El-Tanbouly DM (2018) Cilostazol disrupts TLR-4, Akt/GSK-3beta/CREB, and IL-6/JAK-2/STAT-3/SOCS-3 crosstalk in a rat model of Huntington’s disease. PLoS ONE 13:e0203837
Wertz MH, Pineda SS, Lee H, Kulicke R, Kellis M, Heiman M (2020) Interleukin-6 deficiency exacerbates Huntington’s disease model phenotypes. Mol Neurodegener 15:29
Benedict RHB, Amato MP, DeLuca J, Geurts JJG (2020) Cognitive impairment in multiple sclerosis: clinical management, MRI, and therapeutic avenues. Lancet Neurol 19:860–871
Giovannoni G, Hawkes CH, Lechner-Scott J, Levy M, Waubant E (2020) Ageing and multiple sclerosis. Mult Scler Relat Disord 38:101953
Graves JS, Krysko KM, Hua LH, Absinta M, Franklin RJM, Segal BM (2023) Ageing and multiple sclerosis. Lancet Neurol 22:66–77
Walton C, King R, Rechtman L, Kaye W, Leray E, Marrie RA, Robertson N, La Rocca N, Uitdehaag B, van der Mei I, Wallin M, Helme A, Angood Napier C, Rijke N, Baneke P (2020) Rising prevalence of multiple sclerosis worldwide: insights from the Atlas of MS, third edition. Mult Scler. 26:1816–1821
Stelmasiak Z, Koziol-Montewka M, Dobosz B, Rejdak K, Bartosik-Psujek H, Mitosek-Szewczyk K, Belniak-Legiec E (2000) Interleukin-6 concentration in serum and cerebrospinal fluid in multiple sclerosis patients. Med Sci Monit 6:1104–1108
Drehmer E, Platero JL, Carrera-Julia S, Moreno ML, Tvarijonaviciute A, Navarro MA, Lopez-Rodriguez MM, Orti JER (2020) The relation between eating habits and abdominal fat, anthropometry, PON1 and IL-6 levels in patients with multiple sclerosis. Nutrients 12(3):744
Bongioanni P, Mosti S, Romano MR, Lombardo F, Moscato G, Meucci G (2000) Increased T-lymphocyte interleukin-6 binding in patients with multiple sclerosis. Eur J Neurol 7:291–297
Serada S, Fujimoto M, Mihara M, Koike N, Ohsugi Y, Nomura S, Yoshida H, Nishikawa T, Terabe F, Ohkawara T, Takahashi T, Ripley B, Kimura A, Kishimoto T, Naka T (2008) IL-6 blockade inhibits the induction of myelin antigen-specific Th17 cells and Th1 cells in experimental autoimmune encephalomyelitis. Proc Natl Acad Sci U S A 105:9041–9046
Stampanoni Bassi M, Iezzi E, Mori F, Simonelli I, Gilio L, Buttari F, Sica F, De Paolis N, Mandolesi G, Musella A, De Vito F, Dolcetti E, Bruno A, Furlan R, Finardi A, Marfia GA, Centonze D, Rizzo FR (2019) Interleukin-6 disrupts synaptic plasticity and impairs tissue damage compensation in multiple sclerosis. Neurorehabil Neural Repair 33:825–835
Bruno A, Dolcetti E, Azzolini F, Moscatelli A, Gambardella S, Ferese R, Rizzo FR, Gilio L, Iezzi E, Galifi G, Borrelli A, Buttari F, Furlan R, Finardi A, De Vito F, Musella A, Guadalupi L, Mandolesi G, Centonze D, Stampanoni Bassi M (2022) Interleukin 6 SNP rs1818879 regulates radiological and inflammatory activity in multiple sclerosis. Genes (Basel) 13(5):897
Platero JL, Cuerda-Ballester M, Ibanez V, Sancho D, Lopez-Rodriguez MM, Drehmer E, Orti JER (2020) The Impact of Coconut Oil and Epigallocatechin Gallate on the Levels of IL-6, Anxiety and Disability in Multiple Sclerosis Patients. Nutrients 12(2):305
Marucci G, Buccioni M, Ben DD, Lambertucci C, Volpini R, Amenta F (2021) Efficacy of acetylcholinesterase inhibitors in Alzheimer’s disease. Neuropharmacology 190:108352
Jaiswal MK (2019) Riluzole and edaravone: a tale of two amyotrophic lateral sclerosis drugs. Med Res Rev 39:733–748
Acknowledgements
The authors thank Chenguang Zhang and Wenting Hou for critically reviewing the manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (No. 82003809), Beijing Natural Science Foundation (No. 7222157) and Beijing Hospital Nova Project (BJ-2020-087).
Author information
Authors and Affiliations
Contributions
CS and CZ: designed the study, and drafted the manuscript, CZ: participated in the revision of the manuscript.
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declared that no potential conflicts of interest exist.
Ethical Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Written informed consent for publication was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shan, C., Zhang, C. & Zhang, C. The Role of IL-6 in Neurodegenerative Disorders. Neurochem Res 49, 834–846 (2024). https://doi.org/10.1007/s11064-023-04085-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-023-04085-6