Abstract
Epilepsy is characterized by the manifestation of spontaneous and recurrent seizures. The high prevalence of comorbidities associated with epilepsy, such as cognitive dysfunction, affects the patients quality of life. Adenosine signaling modulation might be an effective alternative to control seizures and epilepsy-associated comorbidities. This study aimed to verify the role of adenosine modulation on the seizure development and cognitive impairment induced by pentylenetetrazole (PTZ) in zebrafish. At first, animals were submitted to a training session in the inhibitory avoidance test and, after 10 min, they received an intraperitoneal injection of valproate, adenosine A1 receptor agonist cyclopentyladenosine (CPA), adenosine A1 receptor antagonist 8-cyclopentyl-1,3-dipropylxanthine (DPCPX), adenosine A2A receptor antagonist ZM 241385, adenosine deaminase inhibitor erythro-9-(2-hydroxy-3-nony1)-adenine hydrochloride (EHNA) or the nucleoside transporter inhibitor dipyridamole. Thirty min after the intraperitoneal injection, the animals were exposed to 7.5 mM PTZ for 10 min, where they were evaluated for latency to reach the seizure stages (I, II, and III). Finally, 24 h after the training session, the animals were submitted to the inhibitory avoidance test to verify their cognitive performance during the test session. Valproate, CPA, and EHNA showed antiseizure effects and prevented the memory impairment induced by PTZ exposure. DPCPX, ZM 241385, and dipyridamole pretreatments caused no changes in seizure development; however, these drugs prevented memory impairment without altering locomotion. Our results reinforce the antiseizure effects of adenosine signaling and support the idea that the involvement of adenosine in memory processes may be a target for preventive strategies against cognitive impairment associated with epilepsy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epilepsy is a chronic neurological disease characterized by the manifestation of spontaneous and recurrent seizures, affecting up to 70 million people worldwide [1, 2]. Epilepsy rarely occurs alone, and the presence of comorbidities is frequently reported [2, 3]. Cognitive dysfunction is a common comorbidity associated with epilepsy, including memory, attention, and processing difficulties [4]. Comorbidities affect the quality of a patient’s life, and the existence of these conditions must be relevant in the choice of epilepsy treatment [2, 5].
Conventional antiseizure drug treatments ensure in most of the cases effective seizure suppression; however, about 30–40% of patients are refractory to antiseizure drug treatments [6, 7]. Adenosine, a purine ribonucleoside, is a well-known endogenous modulator of neuronal excitability and several studies have shown the antiseizure action of this molecule [8,9,10,11,12,13]. Adenosine modulation might be an effective alternative to control seizures in patients resistant to conventional antiseizure drugs [13].
Adenosine can be produced by the dephosphorylation of nucleotides tri-, di-, and monophosphates (ATP, ADP, and AMP, respectively) or released through nucleoside transporters [14]. Ectonucleotidases are an enzyme cascade system that catalyzes the successive hydrolysis of adenine nucleotides [15]. ATP and ADP are hydrolyzed by the ectonucleoside triphosphate diphosphohydrolase (E-NTPDase) family members, whereas AMP is hydrolyzed by ecto-5′-nucleotidase, generating adenosine. Adenosine, through the action of adenosine deaminase, may be subsequently deaminated to inosine [16]. Adenosine may be released through concentrative or equilibrative nucleoside transporters [17].
Adenosine exerts its effects by acting through the G-protein-coupled receptors: A1, A2A, A2B, and A3 subtypes [18, 19]. During a seizure, extracellular adenosine levels increase and the antiseizure adenosine effects are mediated by adenosine A1 receptors, which cause presynaptic inhibition by reducing calcium influx and the excitability of the postsynaptic membrane by increasing potassium release [13, 20]. Moreover, activation of A1 receptors through selective receptor agonists effectively suppresses seizure activity, even in pharmaco-resistant epilepsy [10, 13, 14]. Although it has been suggested a neuroprotective and antiseizure action of adenosine A2A receptors [21, 22], studies have also demonstrated a proconvulsive and neurodegenerative role played by those receptors [23, 24]. The actions mediated by adenosine A2B receptors and adenosine A3 receptors in epilepsy are not completely characterized [13].
The involvement of adenosine receptors in cognitive processes has been demonstrated [25,26,27,28,29,30]. A study has shown that A1 receptors played a protective role against cognitive impairment by reducing neuron loss in a PTZ model in mice [29]. Furthermore, the A1 receptors agonist prevented scopolamine-induced working memory impairment in mice [31]. In zebrafish, different modulators of adenosine signaling prevented scopolamine-induced amnesia [26] and memory impairment induced by 3-Nitropropionic acid [30]. These data support the hypothesis that adenosine signaling may modulate memory processing. Therefore, adenosine signaling may be a target for the development of preventive strategies, not only for seizure control, but also for epilepsy-associated cognitive comorbidities.
Zebrafish is a promising model organism to study the mechanisms underlying epilepsy and the biological effects of brain function modulation [32, 33]. Previous studies have demonstrated the A1 and A2A receptors in zebrafish [34, 35]. Nucleoside Triphosphate Diphosphohydrolases (NTPDases), ecto-5′-nucleotidase, and adenosine deaminase activities were characterized in zebrafish brain membranes, along with the gene expression patterns of these enzymes [36,37,38,39].
Considering that adenosine signaling is controlled by nucleotide- and nucleoside-metabolizing enzymes and nucleoside transporters, the modulation of these mechanisms may be a target for new therapies for seizure control and epilepsy-associated comorbidities. Zebrafish is an effective model used in epilepsy research and the investigation of adenosine signaling in this species may contribute to elucidate the role of adenosine in epilepsy-related comorbidities. This study aimed to verify the effects of adenosine signaling on seizure development and cognitive impairment induced by PTZ in zebrafish.
Materials and Methods
Animals
A total of 336 adult zebrafish (Danio rerio) of the wild-type AB strain (5–7 months old, ~ 50:50 male: female ratio) were used in the experiments. Animals were obtained from our breeding colony and kept in automated recirculating systems (Zebtec, Tecniplast, Italy) with reverse-osmosis-filtered water and conditions recommended for the species [40, 41]. Temperature (28℃ ± 2℃), pH (7.0–7.5), conductivity (300–700 μS), ammonia (< 0.02 mg/L), hardness (80–300 mg/L), nitrite (< 1 mg/L), nitrate (< 50 mg/L), and chloride (0 mg/L) were monitored. Fish were maintained under a 14 h light:10 h dark photoperiod cycle and fed with commercial flakes (TetraMin Tropical Flake Fish®) three times a day. All protocols were approved by the Institutional Animal Care Committee from Pontifícia Universidade Católica do Rio Grande do Sul, Brazil (CEUA- PUCRS, protocol number 9427). This study was registered in the Sistema Nacional de Gestão do Patrimônio Genético e Conhecimento Tradicional Associado-SISGEN (Protocol No. A3B073D).
Experimental Design
This study investigated the effects of drugs that can modulate adenosine signaling on memory consolidation impairment caused by PTZ-induced seizures in zebrafish. The experimental design is seen in Fig. 1.
Schematic representation of the experimental procedures. On day 1, animals were submitted to a training session in the inhibitory avoidance test. After 10 min, they received an intraperitoneal injection of the chosen drug. 30 min later, the animals were exposed to 7.5 mM PTZ for 10 min. On day 2, the animals were submitted to the inhibitory avoidance test to verify their cognitive performance during the test session and then had their locomotor behavior assessed
At first, zebrafish were randomly assigned to the experimental groups and submitted to a training session in the inhibitory avoidance test. After 10 min, they received an intraperitoneal injection of the chosen drug. After 30 min, the animals were exposed to 7.5 mM PTZ for 10 min, where they were assessed for latency to reach the seizure stages (I, II, and III). Finally, 24 h after the training session, the animals were submitted to the inhibitory avoidance test to verify their cognitive performance during the test session, and then had their locomotor behavior evaluated.
The animals were randomly separated (8 fish per tank) in a 2-L aquarium with aerated and unchlorinated water, 24 h before the beginning of the tests. The experiments were performed between 9 a.m. and 11 a.m., and they were conducted in duplicate. No experimental procedure was carried out in the maintenance area of fish to avoid any type of behavioral stress. The animals were fed twice a day at 12 p.m. and 5 p.m. Animals were not fed before the experiment.
Drug Pretreatments
Valproate (Sigma-Aldrich, St Louis, MO), cyclopentyladenosine (CPA; Sigma-Aldrich, St Louis, MO), erythro-9-(2-hydroxy-3-nony1)-adenine hydrochloride (EHNA; Sigma-Aldrich, St Louis, MO), 4-(2-[7-amino-2-{2-fury1}{1,2,4}triazolo-{2,3-a}{1,3,5}triazin-5-yl-amino]ethyl) phenol (ZM 241385; Tocris Cookson, USA); dipyridamole (Sigma-Aldrich, St Louis, MO), and 8-cyclopentyl-1,3-dipropylxanthine (DPCPX; Tocris Cookson, USA) were used in the study. Saline was used as a vehicle for valproate, CPA, and EHNA, and 3% DMSO was used as a vehicle for DPCPX, ZM 241385, and dipyridamole according to previous studies [26, 42].The doses tested are: 100 mg/kg valproate, 2 mg/kg CPA, 75 mg/kg EHNA, 2 mg/kg ZM 241385, 20 mg/kg dipyridamole, and 15 mg/kg DPCPX were administered via intraperitoneal in a volume of 10 μl using a 3/10-mL U-100 BD Ultra-FineM Short Insulin Syringe 8 mm (5/16 inch) × 31G Short Needle (Becton Dickinson and Company, New Jersey, USA). The doses for each drug tested were chosen based on previous studies conducted in our laboratory [42]. Before vehicle or drug administration, fish were anesthetized by immersion in a 100 mg/L tricaine solution (ethyl 3-aminobenzoate methanesulfonate salt; Sigma-Aldrich, St Louis, MO) until the animal demonstrated a lack of motor coordination and decreased respiration rate. After the injection, the animals were placed in a separate tank for 30 min before PTZ (pentylenetetrazole; Sigma-Aldrich, St Louis, MO) exposure.
PTZ-Induced Seizures
Seizures induced by PTZ are characterized by progressive behavioral changes in zebrafish, which are identified in three stages: (i) increased swimming activity (stage I); (ii) fast and circle swimming (stage II); and (iii) loss of posture and immobility for 1–3 s (stage III). The animals were individually exposed to 500 ml of 7.5 mM PTZ solution in a glass tank (15 cm × 15 cm × 6 cm; L × H × W) for 10 min. The behavior was recorded on video and the latency to the first episode of seizure activity in each stage was identified as previously described [43].
Behavioral Analysis
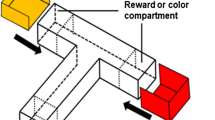
Inhibitory Avoidance
Memory was assessed through the inhibitory avoidance test as described in the literature [44]. The behavioral apparatus comprises an aquarium (18 cm × 7 cm × 9 cm; L × H × W) with a mobile guillotine-type partition (9 cm × 7 cm; L × H), which separates the aquarium into two compartments of the same size, one dark (8 lux) and the other light (130 lux). The dark and light compartments are covered by opaque plastic self-adhesive films in black and white colors, respectively, covering the external walls, bottom, and corresponding sides of the movable partition. The aquarium water level was 3 cm high, and the partition was raised 2 cm above the bottom of the aquarium to allow the free movement of the animals from one compartment to the other. Two electrodes were placed in the dark compartment and, when these electrodes were activated, they produced an electric shock of 3 ± 0.2 V. The animals were trained and tested individually in the inhibitory avoidance apparatus.
During the training session, the fish were placed in the clear area of the aquarium with the partition closed and, after 1 min of acclimatization, the partition was raised, allowing the animals to transition to the dark side through the opening. After the animal crosses to the dark side, the partition was closed, and the animal received a pulsed electric shock administered for 5 s. The animals were then removed and placed in their respective aquariums. After 24 h, the test session was performed, where the fish were submitted to the same protocol; however, they did not receive the shock. The cognitive performance was evaluated through the latency to enter the dark area and this parameter was used as an index of memory retention.
Locomotor Activity
The locomotor activity was performed as described previously [45, 46]. Fish were placed individually in a glass tank (30 cm × 15 cm × 10 cm; L × H × W) filled with 2 L of non-chlorinated water and recorded on video for 7 min, where the first minute recorded was to habituate the fish. The videos were analyzed using EthoVision XT® tracking software (version 11.5, Noldus, Wageningen, Netherlands) at a rate of 30 positions per second. The distance traveled (m) parameter was chosen to verify locomotor alterations.
Statistical Analysis
The normality of data and homogeneity of variances were analyzed by the Shapiro-Wilk test and Bartlett's tests, respectively. Data were expressed as mean ± standard error of the mean (SEM). Nonparametric data of latencies to enter the dark area in training and test sessions were analyzed by the Mann-Whitney U test. Parametric data from seizure latency were analyzed by unpaired Student's t-test followed by Dunnett's post-hoc test. Parametric data from the locomotor test were evaluated by two-way ANOVA, followed by the Student-Newman-Keuls multiple comparison test (effects of water and PTZ). The level of significance was set at p < 0.05, and GraphPad Prism 8 (La Jolla, CA, USA) software was used for statistical analysis.
Results
Effects of Adenosine Signaling Modulation on PTZ-Induced Seizures
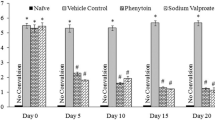
Fig. 2 shows the latency to the first behavioral manifestation of each seizure stage (I, II, and III). All animals showed progressive behavioral alterations and reached all seizure stages.
Effect of A 100 mg/kg valproate (VPA), B 2 mg/kg CPA, C 15 mg/kg DPCPX, D 2 mg/kg ZM 241385 (ZM), E 75 mg/kg EHNA or F 20 mg/kg dipyridamole (DIP) on the latency to the first behavioral manifestation of each stage of PTZ-induced seizures (I, II and III). *p < 0.05, **p < 0.01, ***p < 0.001 indicate differences between the groups compared by the unpaired Student's t-test. All data were expressed as mean ± SEM (n = 11–20 per group)
To investigate seizure development and zebrafish response to a classic antiseizure drug, we investigated the effects of valproate on PTZ-induced seizures (Fig. 2A). Valproate pretreatment increased the latency to reach stages I, II, and III (p = 0.0173; p = 0.0076; p = 0.0127, respectively) when compared to control group. The animals exposed to PTZ without valproate treatment (saline group) reached stages I, II, and III at 134.7 ± 31.99, 387.3 ± 36.58, and 406.3 ± 37.49 s, respectively, whereas animals pretreated with valproate reached stages I, II, and III at 274.1 ± 45.95, 510.7 ± 23.98, and 522.9 ± 24.14 s, respectively.
To verify the role of adenosine on PTZ-induced seizures, we evaluated different drugs that modulate adenosine signaling. CPA, the selective A1 receptors agonist, provided significant protection against PTZ-induced seizures at stages II and III (p = 0.0028 and p = 0.0374, respectively) (Fig. 2B). Stage II was observed at 224.6 ± 19.70 s (saline group) and 334.5 ± 27.83 s (CPA group). The latency to reach stage III was 303.7 ± 29.20 s in the saline group and 397.9 ± 32.12 s in the CPA group. CPA did not cause changes in the latency to reach stage I (p = 0.4468) when compared to the control group. Stage I was observed at 77.53 ± 10.66 s (saline group) and 90.29 ± 12.87 s (CPA group). The selective A1 receptors antagonist, DPCPX, was not able to change behavior seizures responses at stages I, II, and III (p = 0.7401; p = 0.4697; p = 0.3790, respectively), when compared to the control group (Fig. 2C). The latencies to reach stages I, II, and III were observed at 128 ± 11.45, 256.3 ± 24.42 and 261.3 ± 24.30 s, respectively (DMSO group), and 134.6 ± 16.13, 280.9 ± 21.73 and 291.2 ± 23 s, respectively (DPCPX group). Similarly, ZM 241385, the A2A receptors antagonist, did not cause changes at seizure stages I, II, and III (p = 0.1895; p = 0.1481; p = 0.2873, respectively), when compared to the control group (Fig. 2D). DMSO group reached stages I, II, and III at 91.73 ± 23.86, 212.4 ± 33.01, and 278.7 ± 45.91 s, respectively. ZM 241385 group reached stages I, II, and III at 57.27 ± 8.60, 284.6 ± 34.70, and 351.3 ± 48.20 s, respectively.
The animals pretreated with EHNA, an adenosine deaminase inhibitor, took longer to reach stages I, II, and III (p = 0.0192, p = 0.0006, and p = 0.0085, respectively), when compared to the control group (Fig. 2E). For the saline group, stages I, II, and III were observed at 77.53 ± 10.66, 224.6 ± 19.70, and 319.3 ± 31.72 s, respectively; for the EHNA group, stages I, II, and III were observed at 149.3 ± 27.27, 380.2 ± 37.16, and 458.6 ± 38.63 s, respectively. Finally, the adenosine reuptake inhibition by the nonspecific nucleoside transport inhibitor, dipyridamole, did not cause changes at seizure stages I, II, and III (p = 0.8823; p = 0.4910; p = 0.8654, respectively) (Fig. 2F). In the vehicle (DMSO) group, the animals exposed to PTZ reached stages I, II, and III at 107.7 ± 26.99, 198.8 ± 33.07, and 278.7 ± 45.91 s, respectively. Animals pretreated with dipyridamole plus PTZ reached stages I, II, and III at 102.5 ± 21.49, 239.3 ± 47.44, and 290.3 ± 49.54 s, respectively. Descriptive data of the drugs’ effects on the latency to the first behavioral manifestation of each stage of PTZ-induced seizures (I, II, and III) and digital tracking maps of the total distance traveled are in Table S1 and Figure S1 (Supplementary Information), respectively.
Effects of Adenosine Signaling Modulation on Memory Consolidation Impairment Induced by PTZ
Figure 3 shows the effects of PTZ-induced seizures on the cognition of animals pretreated and submitted to the inhibitory avoidance task. Interestingly, the Mann–Whitney U test revealed that the classic antiseizure drug and all adenosine signaling modulators prevented the memory impairment induced by PTZ.
Effect of A 100 mg/kg valproate (VPA), B 2 mg/kg CPA, C 15 mg/kg DPCPX, D 2 mg/kg ZM 241385 (ZM), E 75 mg/kg EHNA or F 20 mg/kg dipyridamole (DIP) on the latency to enter in the dark area during the training and test session on inhibitory avoidance test. **p < 0.01, ***p < 0.001, ****p < 0.0001 indicate differences between training and test session of each group compared by Mann–Whitney U test t. All data were expressed as mean ± SEM (n = 12–20 per group)
Pretreatment of valproate (p = < 0.0001; Fig. 3A), CPA (p = 0.0004; Fig. 3B), DPCPX (p = 0.0001; Fig. 3C), ZM 241385 (p = 0.0019; Fig. 3D), EHNA (p = < 0.0001; Fig. 3E) or dipyridamole (p = 0.0001; Fig. 3F), followed by water treatment, showed a significant increase in the latency to enter the dark compartment in the test session. Their respective vehicle-groups (p = < 0.0001, Fig. 3A; p = < 0.0001, Fig. 3B; p = 0.0005, Fig. 3C; p = < 0.0001, Fig. 3D; p = < 0.0001, Fig. 3E; p = < 0.0001, Fig. 3F, respectively), followed by water treatment, also demonstrated retention of memory during the test session. However, vehicle-exposed animals subsequently treated with PTZ did not exhibit memory retention during the test session performed 24 h after training (Fig. 3A–F). Interestingly, treatment with valproate (p = < 0.0001; Fig. 3A), CPA (p = 0.0002; Fig. 3B), DPCPX (p = 0.0009; Fig. 3C), ZM 241385 (p = 0.0004; Fig. 3D), EHNA (p = < 0.0001; Fig. 3E) or dipyridamole (p = 0.0009; Fig. 3F) prevented the memory consolidation impairment induced by PTZ. Descriptive data of the drugs’ effects on the latency to enter the dark area during the training and test session on inhibitory avoidance test are in Table S2 (Supplementary Information).
Effects of Adenosine Signaling Modulation on Locomotor Activity
Figure 4 shows the effects of PTZ-induced seizures on the locomotor behavior of animals pretreated and submitted to the inhibitory avoidance task.
The two-way ANOVA showed no significant water x PTZ interaction for the pretreatment of valproate [F(1,66) = 1.331, p = 0.2527; Fig. 4A], CPA [F(1,53) = 1.667, p = 0.2023; Fig. 4B), DPCPX [F(1,55) = 0.1675, p = 0.6840; Fig. 4C), ZM 241385 [F(1,43) = 0.01183, p = 0.9139; Fig. 4D), EHNA [F (1,46) = 0.0070, p = 0.9338; Fig. 4E), and dipyridamole [F(1,41) = 1.615, p = 2109; Fig. 4F) on locomotor activity. Descriptive data of the drugs’ effects on zebrafish distance traveled are in Table S3 (Supplementary Information).
Discussion
Adenosine plays a protective role by interacting with adenosine receptors when its extracellular concentration is increased [47]. Several data have shown the crucial role of adenosine as a modulator of neurotransmission and a neuroprotective agent against excitotoxic neuronal injury [47, 48]. Our results reinforce the role of adenosine receptors in seizure control and its effects on memory formation.
Previous studies have demonstrated that antiseizure drugs can interfere with the purinergic system [49,50,51]. In our results, we observed that the animals pretreated with valproate took longer to reach all seizure stages, demonstrating its anticonvulsant activity. A study using zebrafish showed that antiseizure drug pretreatments suppressed the increase of adenosine deamination induced by seizures, which coincided with a longer period for the animals to reach seizure stage III [49]. In addition, valproate treatment suppressed the increase of adenosine deaminase activity induced by PTZ-kindling in mice brain tissue [52].
Furthermore, our results showed that zebrafish pretreated with CPA, the A1 receptors agonist, took longer to reach II and III seizure stages. On the other hand, the pretreatment with DPCPX, the A1 receptors antagonist, caused no changes in the animal’s behavior during the seizure stages. The same was observed when zebrafish were pretreated with ZM 241385, the selective A2A receptors antagonist. These results corroborate with the studies suggesting that the deregulation of A1 receptor signaling is intrinsically linked to the pathophysiology of epilepsy [12, 13, 53].
Adenosine is released from the cytoplasm by nucleoside transporters, or through ATP degradation into adenosine by ectonucleotidases, pathways that represent an important source of extracellular adenosine [14, 20]. Adenosine deaminase catalyzes the irreversible deamination of adenosine to inosine, and the inhibition of its activity modulates acute seizures in zebrafish [12, 42]. When pretreated with EHNA, an adenosine deaminase inhibitor, animals showed longer latency to reach II and III seizure stages. These data suggest that modulation of adenosine levels by adenosine deaminase activity has a key role in seizure control in zebrafish.
Regulation of adenosine levels by the action of nucleoside transporters is another important mechanism that may be crucial in controlling seizures. Here, the nucleoside transporter inhibition by dipyridamole has no protective effects on seizure development in zebrafish. Animals pretreated with dipyridamole showed no changes in latency to reach the seizure stages. This result opposes the previous report that observed the protective effect of dipyridamole on seizure development in zebrafish [42]. Although our study did not demonstrate the protective effect of dipyridamole, the modulation of adenosine levels through the activity of ectonucleotidases and nucleoside transporters are important mechanisms for the control of epilepsy as well as potential targets for pharmacological therapies [17].
Adenosine has been reported as a neuromodulator, with an important role in synaptic plasticity and memory processing, and its depletion can disrupt memory formation [54,55,56]. Previous studies using adult zebrafish showed the memory impairment induced by the convulsant PTZ to reproduce cognitive dysfunctions as epilepsy-related comorbidities [57, 58]. Therefore, to verify the zebrafish’s cognitive performance on the inhibitory avoidance task, we choose the memory consolidation phase due to the robust response without altering animal locomotion [58]. As demonstrated in previous studies, our data showed that animals pretreated with vehicles (saline or DMSO), followed by PTZ exposure, did not show memory retention when tested on the inhibitory avoidance task [58], characterizing a PTZ-induced seizures memory impairment.
Our work demonstrated that the valproate and all the adenosine modulators pretreatments prevented the memory consolidation impairment induced by PTZ, without altering locomotor activity. Studies have already demonstrated that valproate had the ability to recover learning and memory in rodent models of neurodegeneration [59, 60] and also contributed to memory consolidation and retrieval in mice [61]. We also observed that the A1 receptors agonist (CPA) and the adenosine deaminase inhibitor (EHNA) promoted anticonvulsant effects and prevented memory impairment. In addition to the anticonvulsant effects, the activation of A1 receptors by adenosine may modulate long-term potentiation, long-term depression, and depotentiation, which are crucial processes for learning and memory in different brain areas [53, 55]. A study showed a reduced performance of A1 receptors knockout mice after memory impairment induced by PTZ-kindling on the Morris water maze test [29]. Moreover, epileptic A1 receptors knockout mice exhibited reduced neuronal cell survival and increased activation of caspase-3 in the hippocampus [29]. Also, our findings have shown that the A1 receptor antagonist (DPCPX), the selective A2A receptor antagonist (ZM 241385), and the nonspecific nucleoside transporter inhibitor (dipyridamole) pretreatments caused no changes in seizure development; however, they prevented memory impairment induced by PTZ. Other studies have described the beneficial effects of A1 and A2A receptor antagonism on mechanisms of learning and memory [30, 62, 63]. Interestingly, similar effects promoted by adenosine receptor agonists and antagonists in the prevention of memory impairment induced by PTZ were observed in our study, which could lead us to the hypothesis that these compounds may act through different mechanisms, i.e., as a neuroprotector on cognition pathways and/or as an anticonvulsant. Some compounds, such as A1 and A2A receptor antagonists, could modulate directly cognitive functions, exerting a neuroprotective role, and preventing the memory impairment induced by PTZ-seizures. On the other hand, some adenosinergic compounds, such as A1 receptor agonists, have anticonvulsant effects able to reduce seizure development, which could avoid the occurrence of memory deficits induced by PTZ. Previous studies demonstrated significant improvement in scopolamine-induced memory impairment using A1 and A2A receptor antagonists in adult zebrafish and mice [26, 64]. Wiprich et al. [30] have also demonstrated that the A1 receptor agonist CPA, the A1 receptor antagonist DPCPX, the A2A receptor antagonist ZM 241385, and the nonselective antagonist of A2A and A1 receptors caffeine reversed 3-NPA-induced memory impairment in adult zebrafish during the inhibitory avoidance task. These findings corroborate our results, suggesting that the modulation of adenosine receptors could influence different mechanisms and pathways, resulting in the prevention of memory impairment induced by a neurological disorder. Although the adenosine receptors were already identified in zebrafish through molecular studies [34, 35], the affinities of adenosine receptors by their agonists and antagonists have not been reported. Therefore, we chose to test doses already evaluated in zebrafish in other models of neurological disorders, in which it was performed dose–response curves [42]. It is also relevant to mention that there is a gap of knowledge on the pharmacokinetics and pharmacodynamics of these drugs in zebrafish, which could influence the effects observed by the adenosine agonists and antagonists in seizure control and/or memory processing. Therefore, the paradoxical effects of both agonists and antagonists of adenosine receptors and their effects on different pathways need to be further investigated in zebrafish.
An argument for the mechanisms related to the interaction between seizures and memory is that seizures directly injure neural networks that are essential for the memory formation processes. PTZ-induced seizures caused alterations in oxidant-antioxidant balance, γ-aminobutyric acid (GABA) concentration, and neuronal cells in mice brain [65]. Adenosine is recognized as a crucial molecule in the homeostasis of the nervous system cells. It is released upon conditions of metabolic stress and many of the known effects of this molecule are neuroprotective properties [66]. Adenosine may decrease excitatory amino acid release, limit calcium influx, hyperpolarize the neuronal membrane, restrain the activation of N-methyl-D-aspartate (NMDA) receptors, inhibit free radical formation, and exert modulatory effects in neuronal cells [20, 67,68,69].
Changes in the distance traveled parameter were not observed in the classical antiseizure drug and all the adenosine modulators pretreatments. Importantly, the locomotor behavior was not altered 24 h after the exposure period, demonstrating that the animals’ performance on inhibitory avoidance task is not associated with locomotor changes but with a learning response [58].
Conclusion
To our knowledge, this is the first time that the role of adenosine modulation is evaluated in a memory consolidation impairment promoted by PTZ-induced seizures in zebrafish. Our results reinforce the anticonvulsant effects of adenosine signaling, and the data presented here suggest that the modulation of adenosine levels via adenosine metabolism or by the inhibition of nucleoside transporters can prevent memory consolidation impairment induced by PTZ. These findings support the idea that the involvement of adenosine in memory processes may be a target for preventive strategies against cognitive impairment.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Scheffer IE, Berkovic S, Capovilla G et al (2017) ILAE classification of the epilepsies: position paper of the ILAE Commission for Classification and Terminology. Epilepsia 58:512–521. https://doi.org/10.1111/epi.13709
Thijs RD, Surges R, O’Brien TJ, Sander JW (2019) Epilepsy in adults. The Lancet 393:689–701. https://doi.org/10.1016/S0140-6736(18)32596-0
Fisher RS, Acevedo C, Arzimanoglou A et al (2014) ILAE official report: a practical clinical definition of epilepsy. Epilepsia 55:475–482. https://doi.org/10.1111/epi.12550
Baxendale S, Thompson P (2016) The new approach to epilepsy classification: cognition and behavior in adult epilepsy syndromes. Epilepsy Behav 64:253–256. https://doi.org/10.1016/j.yebeh.2016.09.003
Kanner AM (2016) Management of psychiatric and neurological comorbidities in epilepsy. Nat Rev Neurol 12:106–116. https://doi.org/10.1038/nrneurol.2015.243
White HS, Smith MD, Wilcox KS (2007) Mechanisms of action of antiepileptic drugs. In: International review of neurobiology. Elsevier, New York, pp 85–110
Kwan P, Sills GJ, Brodie MJ (2001) The mechanisms of action of commonly used antiepileptic drugs. Pharmacol Ther 90:21–34. https://doi.org/10.1016/S0163-7258(01)00122-X
Ault B, Wang CM (1986) Adenosine inhibits epileptiform activity arising in hippocampal area CA3. Br J Pharmacol 87:695–703. https://doi.org/10.1111/j.1476-5381.1986.tb14587.x
Boison D (2012) Adenosine dysfunction in epilepsy. Glia 60:1234–1243. https://doi.org/10.1002/glia.22285
Boison D (2005) Adenosine and epilepsy: from therapeutic rationale to new therapeutic strategies. Neuroscientist 11:25–36. https://doi.org/10.1177/1073858404269112
Dragunow M, Goddard GV, Laverty R (1985) Is adenosine an endogenous anticonvulsant? Epilepsia 26:480–487. https://doi.org/10.1111/j.1528-1157.1985.tb05684.x
Weltha L, Reemmer J, Boison D (2019) The role of adenosine in epilepsy. Brain Res Bull 151:46–54. https://doi.org/10.1016/j.brainresbull.2018.11.008
Beamer E, Kuchukulla M, Boison D, Engel T (2021) ATP and adenosine—two players in the control of seizures and epilepsy development. Progr Neurobiol 204:102105. https://doi.org/10.1016/j.pneurobio.2021.102105
Borea PA, Gessi S, Merighi S et al (2018) Pharmacology of adenosine receptors: the state of the art. Physiol Rev 98:1591–1625. https://doi.org/10.1152/physrev.00049.2017
Zimmermann H, Zebisch M, Sträter N (2012) Cellular function and molecular structure of ecto-nucleotidases. Purinergic Signal 8:437–502. https://doi.org/10.1007/s11302-012-9309-4
Ipata PL, Camici M, Micheli V, Tozzi MG (2011) Metabolic network of nucleosides in the brain. CTMC 11:909–922. https://doi.org/10.2174/156802611795347555
Bonan CD (2012) Ectonucleotidases and nucleotide/nucleoside transporters as pharmacological targets for neurological disorders. CNSNDDT 11:739–750. https://doi.org/10.2174/187152712803581092
Burnstock G (2007) Purine and pyrimidine receptors. Cell Mol Life Sci 64:1471–1483. https://doi.org/10.1007/s00018-007-6497-0
Layland J, Carrick D, Lee M et al (2014) Adenosine. JACC Cardiovasc Interv 7:581–591. https://doi.org/10.1016/j.jcin.2014.02.009
Fredholm BB, Chen J-F, Cunha RA et al (2005) Adenosine and brain function. In: International review of neurobiology. Elsevier, New York, pp 191–270
Vianna EPM, Ferreira AT, Dona F et al (2005) Modulation of seizures and synaptic plasticity by adenosinergic receptors in an experimental model of temporal lobe epilepsy induced by pilocarpine in rats. Epilepsia 46:166–173. https://doi.org/10.1111/j.1528-1167.2005.01027.x
Masino SA, Kawamura M, Ruskin DN (2014) Adenosine receptors and epilepsy. In: International review of neurobiology. Elsevier, New York, pp 233–255
Stockwell J, Jakova E, Cayabyab F (2017) Adenosine A1 and A2A receptors in the brain: current research and their role in neurodegeneration. Molecules 22:676. https://doi.org/10.3390/molecules22040676
Gupta YK, Malhotra J (1997) Adenosinergic system as an endogenous anticonvulsant mechanism. Indian J Physiol Pharmacol 41:329–343
Cognato GP, Agostinho PM, Hockemeyer J et al (2010) Caffeine and an adenosine A 2A receptor antagonist prevent memory impairment and synaptotoxicity in adult rats triggered by a convulsive episode in early life. J Neurochem 112:453–462. https://doi.org/10.1111/j.1471-4159.2009.06465.x
Bortolotto JW, de Melo GM, de Cognato G et al (2015) Modulation of adenosine signaling prevents scopolamine-induced cognitive impairment in zebrafish. Neurobiol Learn Mem 118:113–119. https://doi.org/10.1016/j.nlm.2014.11.016
Haab Lutte A, Huppes Majolo J, Reali Nazario L, Da Silva RS (2018) Early exposure to ethanol is able to affect the memory of adult zebrafish: possible role of adenosine. Neurotoxicology 69:17–22. https://doi.org/10.1016/j.neuro.2018.08.012
Nazario LR, Antonioli R, Capiotti KM et al (2015) Caffeine protects against memory loss induced by high and non-anxiolytic dose of cannabidiol in adult zebrafish (Danio rerio). Pharmacol Biochem Behav 135:210–216. https://doi.org/10.1016/j.pbb.2015.06.008
Zhou Q, Zhu S, Guo Y et al (2018) Adenosine A1 receptors play an important protective role against cognitive impairment and long-term potentiation inhibition in a pentylenetetrazol mouse model of epilepsy. Mol Neurobiol 55:3316–3327. https://doi.org/10.1007/s12035-017-0571-x
Wiprich MT, Altenhofen S, Gusso D et al (2022) Modulation of adenosine signaling reverses 3-nitropropionic acid-induced bradykinesia and memory impairment in adult zebrafish. Progr Neuro-Psychopharmacol Biol Psychiatry 119:110602. https://doi.org/10.1016/j.pnpbp.2022.110602
Hooper N, Fraser C, Stone TW (1996) Effects of purine analogues on spontaneous alternation in mice. Psychopharmacology 123:250–257. https://doi.org/10.1007/BF02246579
Gawel K, Langlois M, Martins T et al (2020) Seizing the moment: zebrafish epilepsy models. Neurosci Biobehav Rev 116:1–20. https://doi.org/10.1016/j.neubiorev.2020.06.010
Yaksi E, Jamali A, Diaz Verdugo C, Jurisch-Yaksi N (2021) Past, present and future of zebrafish in epilepsy research. FEBS J 288:7243–7255. https://doi.org/10.1111/febs.15694
Capiotti KM, Menezes FP, Nazario LR et al (2011) Early exposure to caffeine affects gene expression of adenosine receptors, DARPP-32 and BDNF without affecting sensibility and morphology of developing zebrafish (Danio rerio). Neurotoxicol Teratol 33:680–685. https://doi.org/10.1016/j.ntt.2011.08.010
Boehmler W, Petko J, Woll M et al (2009) Identification of zebrafish A2 adenosine receptors and expression in developing embryos. Gene Expr Patterns 9:144–151. https://doi.org/10.1016/j.gep.2008.11.006
Rico EP, Senger MR, da Fauth M, G, et al (2003) ATP and ADP hydrolysis in brain membranes of zebrafish (Danio rerio). Life Sci 73:2071–2082. https://doi.org/10.1016/S0024-3205(03)00596-4
Senger MR, Rico EP, Dias RD et al (2004) Ecto-5′-nucleotidase activity in brain membranes of zebrafish (Danio rerio). Comput Biochem Physiol B 139:203–207. https://doi.org/10.1016/j.cbpc.2004.07.011
Rosemberg DB, Rico EP, Guidoti MR et al (2007) Adenosine deaminase-related genes: molecular identification, tissue expression pattern and truncated alternative splice isoform in adult zebrafish (Danio rerio). Life Sci 81:1526–1534. https://doi.org/10.1016/j.lfs.2007.09.019
Rosemberg DB, Rico EP, Senger MR et al (2008) Kinetic characterization of adenosine deaminase activity in zebrafish (Danio rerio) brain. Comput Biochem Physiol B 151:96–101. https://doi.org/10.1016/j.cbpb.2008.06.001
Westerfield M (2007) The zebrafish book. A guide for the laboratory use of zebrafish (Danio rerio), 5th edn. University of Oregon Press, Eugene
Westerfield M (2000) The zebrafish book. A guide for the laboratory use of zebrafish (Danio rerio), 4th edn. University of Oregon Press, Eugene
Siebel AM, Menezes FP, Capiotti KM et al (2015) Role of adenosine signaling on pentylenetetrazole-induced seizures in zebrafish. Zebrafish 12:127–136. https://doi.org/10.1089/zeb.2014.1004
Baraban SC, Taylor MR, Castro PA, Baier H (2005) Pentylenetetrazole induced changes in zebrafish behavior, neural activity and c-fos expression. Neuroscience 131:759–768. https://doi.org/10.1016/j.neuroscience.2004.11.031
Blank M, Guerim LD, Cordeiro RF, Vianna MRM (2009) A one-trial inhibitory avoidance task to zebrafish: rapid acquisition of an NMDA-dependent long-term memory. Neurobiol Learn Mem 92:529–534. https://doi.org/10.1016/j.nlm.2009.07.001
Altenhofen S, Wiprich MT, Nery LR et al (2017) Manganese(II) chloride alters behavioral and neurochemical parameters in larvae and adult zebrafish. Aquat Toxicol 182:172–183. https://doi.org/10.1016/j.aquatox.2016.11.013
Gusso D, Altenhofen S, Fritsch PM et al (2021) Oxytetracycline induces anxiety-like behavior in adult zebrafish. Toxicol Appl Pharmacol 426:115616. https://doi.org/10.1016/j.taap.2021.115616
Stone TW (2005) Adenosine, neurodegeneration and neuroprotection. Neurol Res 27:161–168. https://doi.org/10.1179/016164105X21896
Varani K, Vincenzi F, Merighi S et al (2017) Biochemical and pharmacological role of A1 adenosine receptors and their modulation as novel therapeutic strategy. In: Atassi MZ (ed) Protein reviews. Springer, Singapore, pp 193–232
Siebel AM, Piato AL, Schaefer IC et al (2013) Antiepileptic drugs prevent changes in adenosine deamination during acute seizure episodes in adult zebrafish. Pharmacol Biochem Behav 104:20–26. https://doi.org/10.1016/j.pbb.2012.12.021
de Cognato GP, Bruno AN, da Silva RS, et al (2007) Antiepileptic drugs prevent changes induced by pilocarpine model of epilepsy in brain ecto-nucleotidases. Neurochem Res 32:1046–1055. https://doi.org/10.1007/s11064-006-9272-y
Siebel AM, Piato AL, Capiotti KM et al (2011) PTZ-induced seizures inhibit adenosine deamination in adult zebrafish brain membranes. Brain Res Bull 86:385–389. https://doi.org/10.1016/j.brainresbull.2011.08.017
Ilhan A, Gurel A, Armutcu F et al (2005) Antiepileptogenic and antioxidant effects of oil against pentylenetetrazol-induced kindling in mice. Neuropharmacology 49:456–464. https://doi.org/10.1016/j.neuropharm.2005.04.004
Tescarollo FC, Rombo DM, DeLiberto LK et al (2020) Role of adenosine in epilepsy and seizures. J Caff Adenosine Res 10:45–60. https://doi.org/10.1089/caff.2019.0022
Dias RB, Rombo DM, Ribeiro JA et al (2013) Adenosine: setting the stage for plasticity. Trends Neurosci 36:248–257. https://doi.org/10.1016/j.tins.2012.12.003
Ribeiro JA, Sebastião AM, de Mendonça A (2002) Adenosine receptors in the nervous system: pathophysiological implications. Prog Neurobiol 68:377–392. https://doi.org/10.1016/S0301-0082(02)00155-7
de Mendonça A, Costenla AR, Ribeiro JA (2002) Persistence of the neuromodulatory effects of adenosine on synaptic transmission after long-term potentiation and long-term depression. Brain Res 932:56–60. https://doi.org/10.1016/S0006-8993(02)02281-3
Canzian J, Müller TE, Franscescon F et al (2019) Modeling psychiatric comorbid symptoms of epileptic seizures in zebrafish. J Psychiatr Res 119:14–22. https://doi.org/10.1016/j.jpsychires.2019.09.007
Bertoncello KT, Zanandrea R, Bonan CD (2022) Pentylenetetrazole-induced seizures cause impairment of memory acquisition and consolidation in zebrafish (Danio rerio). Behav Brain Res 432:113974. https://doi.org/10.1016/j.bbr.2022.113974
Nalivaeva NN, Belyaev ND, Lewis DI et al (2012) Effect of sodium valproate administration on brain neprilysin expression and memory in rats. J Mol Neurosci 46:569–577. https://doi.org/10.1007/s12031-011-9644-x
Yao Z-G, Liang L, Liu Y et al (2014) Valproate improves memory deficits in an Alzheimer’s disease mouse model: investigation of possible mechanisms of action. Cell Mol Neurobiol 34:805–812. https://doi.org/10.1007/s10571-013-0012-y
Fischer A, Sananbenesi F, Wang X et al (2007) Recovery of learning and memory is associated with chromatin remodelling. Nature 447:178–182. https://doi.org/10.1038/nature05772
Zhao Z-A, Zhao Y, Ning Y-L et al (2017) Adenosine A2A receptor inactivation alleviates early-onset cognitive dysfunction after traumatic brain injury involving an inhibition of tau hyperphosphorylation. Transl Psychiatry 7:e1123–e1123. https://doi.org/10.1038/tp.2017.98
Prediger RDS, Fernandes D, Takahashi RN (2005) Blockade of adenosine A2A receptors reverses short-term social memory impairments in spontaneously hypertensive rats. Behav Brain Res 159:197–205. https://doi.org/10.1016/j.bbr.2004.10.017
Pagnussat N, Almeida AS, Marques DM et al (2015) Adenosine A 2 A receptors are necessary and sufficient to trigger memory impairment in adult mice: A 2 A receptor controls memory. Br J Pharmacol 172:3831–3845. https://doi.org/10.1111/bph.13180
Taiwe GS, Ndieudieu Kouamou AL, Dabole B et al (2021) Protective effects of anthocleista djalonensis extracts against pentylenetetrazole-induced epileptic seizures and neuronal cell loss: role of antioxidant defense system. Evid Based Complement Altern Med 2021:1–18. https://doi.org/10.1155/2021/5523705
de Mendonça A, Sebastião AM, Ribeiro JA (2000) Adenosine: does it have a neuroprotective role after all? Brain Res Rev 33:258–274. https://doi.org/10.1016/S0165-0173(00)00033-3
Fredholm BB (1997) Adenosine and neuroprotection. Int Rev Neurobiol 40:259–280
Schubert P, Rudolphi KA, Fredholm BB, Nakamura Y (1994) Modulation of nerve and glial function by adenosine–role in the development of ischemic damage. Int J Biochem 26:1227–1236. https://doi.org/10.1016/0020-711x(94)90092-2
Van Wylen DGL, Park TS, Rubio R, Berne RM (1986) Increases in cerebral interstitial fluid adenosine concentration during hypoxia, local potassium infusion, and ischemia. J Cereb Blood Flow Metab 6:522–528. https://doi.org/10.1038/jcbfm.1986.97
Acknowledgements
This study was funded in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brasil (CAPES)—finance code 001, Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) (Proc. 420695/2018-4), Fundação de Amparo à Pesquisa do Estado do Rio Grande do Sul (Proc. 17/2551-0000977-0), and Instituto Nacional de Ciências e Tecnologia para Doenças Cerebrais, Excitotoxicidade e Neuroproteção. K.T.B. is recipient of a fellowship from CAPES. C.D.B. (Proc. 304450/2019-7) is recipient of CNPq research productivity grants.
Funding
Funding was provided by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (001), Conselho Nacional de Desenvolvimento Científico e Tecnológico (420695/2018-4), Fundação de Amparo à Pesquisa do Estado do Rio Grande do Sul (17/2551-0000977-0).
Author information
Authors and Affiliations
Contributions
KTB: Conceptualization, investigation, methodology, writing—original draft, data curation. CDB: Conceptualization, supervision, funding acquisition, writing—review and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bertoncello, K.T., Bonan, C.D. The Effect of Adenosine Signaling on Memory Impairment Induced by Pentylenetetrazole in Zebrafish. Neurochem Res 48, 1889–1899 (2023). https://doi.org/10.1007/s11064-023-03867-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-023-03867-2