Abstract
Any spinal cord injury carries the potential for persistent disability affecting motor, sensory and autonomic functions. To prevent this outcome, it is highly desirable to block a chain of deleterious reactions developing in the spinal areas immediately around the primary lesion. Thus, early timing of pharmacological neuroprotection should be one major strategy whose impact may be first studied with preclinical models. Using a simple in vitro model of the rat spinal cord it is possible to mimic pathological processes like excitotoxicity that damages neurons because of excessive glutamate receptor activation due to injury, or hypoxic/dysmetabolic insult that preferentially affects glia following vascular dysfunction. While ongoing research is exploring the various components of pathways leading to cell death, current treatment principally relies on the off-label use of riluzole (RLZ) or methylprednisolone sodium succinate (MPSS). The mechanism of action of these drugs is diverse as RLZ targets mainly neurons and MPSS targets glia. Even when applied after a transient excitotoxic stimulus, RLZ can provide effective prevention of secondary excitotoxic damage to premotoneurons, although not to motoneurons that remain very vulnerable. This observation indicates persistent inability to express locomotor activity despite pharmacological treatment conferring some histological protection. MPSS can protect glia from dysmetabolic insult, yet it remains poorly effective to prevent neuronal death. In summary, it appears that these pharmacological agents can produce delayed protection for certain cell types only, and that their combined administration does not provide additional benefit. The search should continue for better, mechanism-based neuroprotective agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinal cord injury (SCI) is one of the most prominent causes of chronic disability that affects a large number of people worldwide [1, 2] with devastating consequences such as physical, psychosocial and economic challenges not only for the patients who often have to live with a lifelong handicap, but also for their families and society at large. SCI is not restricted to adult people only, because children are frequently subjected to SCI that represents 1–2% of all pediatric fractures and is associated with high mortality rate [3]. Although some patients may show spontaneous (or partial) recovery after injury, most have permanent symptoms due to damage of the spinal cord that cannot currently be repaired with success. For many years, SCI was considered a disease that should not and cannot be treated, reflecting the long-lasting belief about the catastrophic nature of the injury and the lack of regenerative capacity of the spinal cord. More recently, strong efforts have been made to understand the pathophysiological changes underlying SCI [4], with the goal of developing and/or applying a specific strategy against neuronal damage. In the last few years the principle “Time Is Spine” has become important because it highlights the narrow time window between the initial cord injury and the secondary endogenous processes that largely amplify the anatomical/functional deficit: thus, there is a time-constrained opportunity to apply treatment (pharmacological and/or non-pharmacological) with the aim of arresting damage progression [4,5,6]. This is a critical issue since later attempts at repairing, rebuilding or replacing spinal networks are difficult. From this point of view, drugs such as riluzole (RLZ) and the synthetic corticosteroid methylprednisolone sodium succinate (MPSS) have been proposed as neuroprotective strategies to be administrated at the earliest stage (first few h) after SCI with the objective of containing and lessening the toxic environment generated in acute SCI, and to provide neuroprotection [6,7,8,9,10]. This goal has not been widely attained and their clinical use remains debatable. Thus, the purpose of the present review is to discuss how a preclinical in vitro animal model of SCI developed in our laboratory a few years ago may help to clarify the basic mechanisms of SCI and provide further information about future developments [11, 12]. Research with these preparations may pinpoint certain pathological processes targeted by RLZ or MPSS (or novel drugs to be devised in the future) and outline new translational approaches. Our review is meant to be a tribute to the research activity by Elias Michaelis who has been prominent in the field of studies of excitatory amino acid transmitters and characterized their receptors on synaptic membranes more than 30 years ago with long lasting implications for modern day Neuroscience [13].
Classification of SCI
The American Spinal Injury Association (ASIA) has established a standardized method for assessing neurologic status and classifying a spinal injury (International Standards for Neurological Classification of SCI) [6]. SCI can be categorized as complete with total functional loss below the lesion, or, more often, incomplete with a variable degree of sensory-motor deficit. The SCI etiology can be traumatic (traffic accidents, falls, violence, sports, work etc.) or non-traumatic (vertebral stenosis, spondylosis, tumors, cardiovascular disorders, pathological fractures due to osteoporosis, infective or iatrogenic diseases) [14, 15]. While the non-traumatic injuries usually are incomplete and develop more slowly than traumatic ones, the resulting symptoms can be equally severe with eventual paralysis and sensory deficit. After the initial damage, the SCI rapidly produces a pathological avalanche phenomenon that magnifies the disability and extends the spinal neurodegeneration [14,15,16]. Eventually SCI reduces function because of loss of voluntary movements and sensory perception, and enhancement of chronic pain and spasticity.
Pathobiology of SCI: Onset of Primary and Secondary Injury
The pathophysiology of SCI is largely determined by two critical phases divided into primary and secondary injury. The traumatic primary injury is considered as the epicenter of the lesion that triggers all pathological sequelae, and comprises cell death, local severance of axons, and damage to blood vessels with focal hemorrhage around the injury site. This phase starts at the time of the trauma and lasts about 2 h, and it is a decisive determinant of injury severity and future disability [17]. If the patient survives the primary phase that, in the case of major trauma, is frequently associated to multiple injuries with vascular collapse and respiratory depression, the secondary injury starts generating a cascade of events lasting hours/days/weeks or, perhaps, even months. These stages can be divided temporally into multiple, sequential stages: immediate, the early acute, subacute, intermediate and chronic phases [5, 17, 18]. Despite its heterogeneous etiology, the first phase of SCI is characterized by ongoing bleeding, peripheral inflammatory cell infiltration, acidosis and edema due to loss of vascular tone autoregulation and disruption of cerebrospinal fluid flow. Additional contributors to this pathology are mechanisms like an excitatory process mediated by excessive glutamate release, generation of free oxygen radicals and metabolic dysfunction [5, 17, 19], all phenomena that persist during the secondary phase. Elias Michaelis made important contributions to our understanding of the link between glutamate receptor function, oxidative stress and neurodegeneration [20]. Furthermore, Michaelis noted how not all cell death induced by glutamate is necessarily the result of activation of glutamate receptors as disruption of membrane transport of cysteine, for instance, may aggravate the energy deficit and mitochondrial dysfunction. In this scenario, astrocytes are also activated to produce scar-associated compounds, forming a glial scar with profound anatomo-pathological consequences for spinal network connections.
Ischemia and Metabolic Perturbation Underlying SCI
As indicated above, one of the first pathophysiological changes occurring at the time of spinal injury is decreased blood flow leading to rapid hypoxia and ischemia. Furthermore, vascular disruption, hemorrhage and metabolic dysfunction are generated around the ischemic area and make the deleterious effects stronger. The normal flow of cerebrospinal fluid is also depressed, thus contributing to tissue compression and lesion. At this stage, the microcirculation is damaged not only at the site of injury but also rostrally and caudally. A vicious cycle is, therefore, initiated whereby ischemia leads to hypoperfusion and subsequent reperfusion, resulting in overproduction of reactive oxygen/nitrogen species (ROS/RNS). The onset of oxidative stress then gives rise to oxidation of proteins, lipids and nucleic acids. This process has also been linked to altered Ca2+ homeostasis, mitochondrial dysfunction, pro-apoptotic signaling and glutamate-mediated excitotoxicity [17, 18]. The whole process reaches a peak with activation of cell death pathways around the injury epicenter.
One Hallmark of Traumatic SCI: Excitotoxicity
One important component of the early phases of SCI is excitotoxicity, namely a process of neurotoxicity caused by high levels of extracellular glutamate with subsequent overactivation of glutamatergic receptors at synaptic and extrasynaptic sites, leading to run-away depolarization of neurons (and glia) through a vast network [21,22,23]. Excitotoxicity has also been linked to the pathogenesis of neurodegenerative disorders like motor neuron disease (MND) which includes Amyotrophic Lateral Sclerosis (ALS or Lou Gehrig´s disease) because motoneurons are very vulnerable to glutamate excitotoxicity [24].
Excitotoxicity is a complex and multifactorial event triggering neuronal cell death [17, 18]. It is possible to discern various processes operating synergistically in this scenario: thus, rise in extracellular glutamate is due not only to its release from damaged cells (in which it is stored at high concentration) but also from strongly depolarized neurons. Glutamate, therefore, acts on ionotropic glutamate receptors to elicit intense Na+ and Ca2+ influx through NMDA, AMPA and KA (N-methyl-d-aspartic acid; alpha-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid; kainate) receptors with activation of intracellular deleterious pathways. Moreover, the large cell depolarization generates more firing of action potentials, further influx of Ca2+, and further release of glutamate to extensively recruit downstream neurons. This process is inadequately controlled by intrinsic inhibitory circuits. The Ca2+ overload is a primary actor (together with disruption of other ion homeostasis) to evoke upregulation of neuronal nitric oxide synthase (nNOS) and nitric oxide production, mitochondrial dysfunction, energy store collapse, ROS generation, release of lysosomal enzymes, and imbalance of superoxide dismutase (SOD-1) activity. An additional contribution to excitotoxicity may come from activation of the Ca2+ permeable membrane receptors TRPM2 and TRPM7 (TRPM, Transient receptor potential cation channel, subfamily M) [25] that are largely expressed in the spinal cord [26]. These receptors are stimulated by intracellular ROS and allow persistent Ca2+ influx with minimal channel inactivation to aggravate the metabolic dysfunction at cell level.
Energy failure can actually reverse the astroglial operation of excitatory amino acid transporters (EAAT) with further non-vesicular glutamate release [17, 27, 28]. Finally, glutamate released by damaged neurons can also activate NMDA and non-NMDA (AMPA/KA) receptors on oligodendrocytes with later damage to this type of cell and axonal demyelination [29]. It should also be noted that extracellular glutamate may also activate metabotropic glutamate receptors of various types to produce, via a negative feedback process, a degree of inhibition of excitotoxicity in vivo and in vitro [30,31,32]. This phenomenon has not been amply exploited to arrest acute SCI progression.
When the initial lesion has a non-traumatic origin, pathological processes emerge more gradually to elicit neuronal loss. The question then arises whether the cell death pathways are similar and affect the same cell types as trauma does.
The Role of Neuroinflammation During SCI
As mentioned before, secondary injury to the spinal cord causes death of local neurons and glia around the primary lesion, and encompasses an array of complex perturbations such as disruption of the blood-spinal cord barrier (BSB) that enables the influx of vasoactive peptides, cytokines and the infiltration of immune cells. These molecular events alter electrolyte homeostasis and contribute to hypoxia, excitotoxicity and neuroinflammatory responses which widen the extent of secondary injury. In the central nervous system (CNS) the spinal cord typically shows a prominent inflammatory response with greater vulnerability to secondary mechanisms [17,18,19, 33].
Neuroinflammation results from activation of several cell types, including microglia, endothelial cells, and infiltrating immune cells (polymorphonuclear leucocytes, macrophages and mast cells) together with a rapidly growing concentration of inflammatory cytokines (TNF-α, IL-1β and IL-6), proteases and other cytotoxic factors. Neutrophils are the first cell type recruited within a few hours, and their number peaks at 1–3 days after injury. Microglia is activated by day 1, and macrophages up to day 5 post injury [17,18,19].
Former studies have shown conflicting results on the role of anti-inflammatory or pro-inflammatory processes in the outcome of SCI [17, 19, 33]. On the one hand, secretion of high levels of TNF-α by macrophages, myeloid and other neuronal cells activates the macrophage/microglia program and increases release of ROS and RNS, thereby killing neurons and oligodendrocytes and exacerbating injury [34]. In support of this phenomenon it has been shown that intrathecal infusion of IL-1 antagonists up to 72 h after rat SCI decreases neuronal apoptosis [33, 34]. Furthermore, neutralization of TNF-α reduces apoptosis and promotes functional recovery [34]. On the other hand, TNF-α seems to be critical for remyelination by facilitating proliferation of oligodendrocytes [35].
At cellular level, depletion or inhibition of macrophages and neutrophils seems to be beneficial for recovery after SCI [36, 37], just like transplantation of the same cells or human central nervous system-derived neural stem cell (hCNS-SCns) to the injury site in the spinal cord [36,37,38]. Interaction between microglia and astrocytes mediates formation of the astroglia scar, a process thought to diminish the spread of inflammation and lesion volume [39]. Parts of the glia scar can protect the periphery of the injured area, and support tissue regeneration [40]. Nevertheless, the glial scar has been also suggested to inhibit axonal outgrowth, creating a physical barrier against axon regeneration following SCI [17, 33].
A novel molecular mechanism of neuroinflammation after SCI is reported to be orchestrated by newly formed endothelial cells located within the core of the injury, via expression of CD200 ligand (CD200L) and the CD200 receptor (CD200R) [33]. CD200L (OX2) is a well conserved type-1 membrane glycoprotein that contains two immunoglobulin superfamily domains. CD200L is widely expressed by a variety of lymphoid and non-lymphoid cells including endothelial, smooth muscle cells, neurons, astrocytes, and oligodendrocytes cells. CD200R contains cytoplasmic tyrosine residue domains (that modulate inflammatory response via interaction with CD200L) expressed in various cell types, including mouse macrophages, dendritic cells, and myeloid cells [41, 42].
Cohen and co-workers have reported that in physiological conditions CD200L is found only in endothelial cells of the mouse blood-cerebrospinal fluid barrier (BCSFB) and in the spinal cord meninges (blood-leptomeningeal barrier; BLMB), but not in the endothelium of the BSB. Following SCI, however, the newly proliferating endothelial cells located only at the epicenter of the lesion upregulate CD200L at different time points (days and weeks) after injury, a timeframe that seems critical for repair. The direct interaction between CD200L by the newly endothelial cells and the CD200R of microglia and macrophages at the site of lesion seems to be important to deliver an inhibitory signal to infiltrating macrophages and microglia [33, 41]. This mechanism is proposed to dampen neuroinflammation and to promote functional recovery after SCI [33, 41].
Notwithstanding these recent data, it is clear that certain processes of neuroinflammation remain poorly understood and their ultimate function in the outcome after lesion is complex, despite the fact that neuroinflammation is considered a key event to determine the severity of SCI. Indeed, its multifaceted characteristics have led to the proposal that it plays the role of a “double-edge sword” in SCI [17,18,19, 33, 34].
Experimental Excitotoxicity and Metabolic Perturbation Damage Different Cell Types
In view of the role of glutamate in acute SCI, it has been possible to set up experimental protocols to further investigate in vivo and/or in vitro the basic mechanisms of SCI and potential neuroprotection. One useful approach developed in our laboratory consists in applying KA that is a glutamate receptor agonist metabolically stable, not taken up via glutamate transporters, and 30- to 100-fold more potent than glutamate itself [43]. It is noteworthy that in vivo injection of KA into the rat lumbar spinal cord closely replicates the lesion induced by trauma to the same area [44]. Thus, our in vitro animal model with KA application seems to have heuristic value to explore the basic processes of SCI. In particular, we have shown that KA per se is sufficient to induce a severe excitotoxic insult yielding SCI models in vitro: (i) the rat isolated spinal cord preparation and, (ii) the rat organotypic spinal cord slice [11, 12, 45]. The in vitro preparation of the rat spinal cord offers the advantage of survival for up to 24 h with efficient synaptic transmission and locomotor network function monitored electrophysiologically from ventral roots that express the rhythmic, alternating oscillations underlying locomotion [46]. These patterns are generated by specialized networks referred to as central pattern generators (CPGs) located in the lower thoracic and lumbar regions of the spinal cord [47]. The organotypic slice is advantageous to study network changes over an extended period of time in a structure preserving the basic architecture of the spinal cord. In either preparation KA-evoked excitotoxicity concerns early neuronal damage rather than glia. Excitotoxicity is associated with death manifested by substantial pyknosis (nuclear chromatin condensation) which is the strongest in the dorsal grey matter followed by the ventral region [11, 12, 45, 46], because of the predominant distribution of AMPA and NMDA receptors [48] and higher neuronal density [49].
To mimic a non-traumatic SCI in vitro it is possible to apply to the spinal cord a “pathological medium” that recapitulates hypoxic/hypoglycemic conditions occurring during a dysmetabolic lesion. This approach primarily damages the white matter (glial cells) and the long-fiber tracts that convey signals to and from brain neurons. Mature oligodendrocytes, that myelinate axons in the brain and spinal cord, support axon function and provide trophic support to neuronal somata [50], are very susceptible to cerebral ischemia, hypoxia and aglycemia caused by impaired cerebrovascular autoregulation [51]. For example, while mature myelin basic protein (MBP)-expressing oligodendrocytes are described as resistant to KA toxicity, hypoxia/ischemia applied to rat pups (postnatal day 7) produces selective white matter lesions and oligodendrocyte death [29, 52, 53]. In the isolated spinal cord model, loss of locomotor network activity induced by KA-excitotoxicity is a more severe deficit than the depression of rhythmicity observed after hypoxic–dysmetabolic insult that primarily targets interneurons and glia (oligodendrocytes and astrocytes) with lower damage to motoneurons [54,55,56].
An essential property of these in vitro animal models is that cell death develops slowly during a few hours after KA bath application (and washout). The predominant process is neither necrosis nor apoptosis, rather a special type of non-apoptotic cell death termed parthanatos [57]. This process is consequent to overactivation of DNA repairing enzymatic mechanisms with collateral hyperproduction of intracellular toxic polymers that are the actual cause of cell death. Since highly selective inhibitors of the parthanatos pathways are currently lacking, it is not surprising that pharmacological blockers currently available have limited efficacy on the in vitro SCI models [58, 59]. Studies with organotypic slices have shown that neuronal losses evoked by KA are completed after the first day following excitotoxicity [60] and that endogenous stem cells do not replace lost neurons [61].
Pharmacological Neuroprotection by RLZ or MPSS After Acute Experimental SCI
Many attempts have been made to preserve spinal gray and white matter affected by SCI [62]. In this section we will focus on two well-known neuroprotective drugs broadly studied and even tested in large-scale clinical trials, namely RLZ and MPSS. To gain insight into the mechanism of action by these drugs, we will largely discuss data from the experimental model of the rat isolated spinal cord that provides a unique possibility to study the timecourse and topography of the cellular and molecular changes during the first 24 h after lesion [12, 55]. Furthermore, with this model more than with in vivo preparations it is feasible to test different experimental paradigms to mimic the consequences of moderate or severe lesions, and to explore the effects of drugs and/or genetic manipulation.
The Use of RLZ as Neuroprotective Agent
Extracellular levels of glutamate increase considerably and transiently within 3 h after injury, with a second wave of release 2–3 days later [63]. Thus, neuronal rescue should be attempted as soon as possible [64]. For a long time, interventions as surgery, intensive care management and rehabilitation were considered as the principal treatments for SCI [5, 6]. Unfortunately, the effectiveness of these therapies is limited and depends on the type of injury and how fast they are applied. Other pharmacological neuroprotective therapies have also emerged to inhibit steps in the secondary pathway after SCI. The current neuroprotective therapies include 2-amino-6-(trifluoromethoxy)benzothiazole (RLZ or Rilutek®; Fig. 1a), which also has an antinociceptive and antispastic effect. This drug can be administrated orally, is approved by the U.S. Food and Drug Administration (FDA), and is considered as a safe and well-tolerated treatment for patients with ALS (National Institute for Clinical Excellence, http://www.nice.org.uk) [10, 65, 66]. Thus, RLZ has been shown to slow down symptom progression and to extend survival for a few months in patients with ALS, as well as to reduce the infarct volume, and to improve behavioral outcome after ischemic or traumatic brain injury [28, 66].
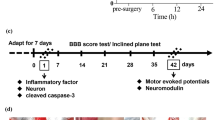
Chemical structure of Rilutek© or riluzole (RLZ), and its molecular weight (MW) (a). Lower schemes illustrate experimental protocols for SHAM or untreated spinal cords (b), and the potential neuroprotection by RLZ. Application of RLZ (5 µM) for 24 h (c) or 3 h (d) after KA (0.1 mM) for 1 h. Spinal cord were always washout (Wsh) after KA insult. In d the spinal cords were washed out with Krebs solution after RLZ application and kept in vitro for 24 h. The last strategy for neuroprotection (e) consisted in applying RLZ (5 µM) together KA (for 1 h) followed by Wsh, RLZ alone for further 3 h, Wsh and in vitro maintenance for the next 24 h (in Krebs solution). After each treatment, the spinal cords were fixed and processed for immunohistochemical analysis (b–e). Electrophysiological recording was carried out throughout each experimental protocol (not shown in the figure)
The rationale for using RLZ after SCI stems from the observations that neurons are exposed to a large influx of Na+ (via activated glutamate receptors and voltage gated Na+ channels) that promotes influx of Ca2+ (and Ca2+ release from intracellular organelles) to stimulate toxic cascades. Thus, it seemed appropriate to use channel blockers to avert secondary injury after SCI. In fact, Fehling´s group demonstrated with electrophysiological experiments that blocking Na+ channels with the local anesthetic QX-314 improved neurophysiological function in the isolated dorsal column of adult rats after acute spinal cord axonal injury [67]. RLZ is a Na+ channel blocker with preferential affinity for channels responsible for the persistent Na+ current supporting repeated spike discharges [68]. In addition, this drug also facilitates uptake of glutamate [69] to lower the extracellular concentration of this amino acid transmitter. Consequently, inhibition of neuronal excitability ensues [65, 70]. Although the RLZ mechanism of action is complex and largely depends on its plasma concentration, it remains the only current treatment for motoneuron disease as “anti-glutamatergic drug”. In a model of excitotoxicity applied to brainstem motoneurons, Cifra et al. have shown that RLZ counteracts the toxic effects caused by the glutamate uptake blocker threo-β-benzyloxyaspartate (TBOA) [69, 71]. Mazzone and Nistri have reported that, in the in vitro animal model of KA-mediated excitotoxicity of organotypic spinal cord cultures, RLZ blocks the early rise in extracellular glutamate (via Ca2+ dependent as well as independent mechanisms). Delayed administration of RLZ can decrease the number of dead neurons in central and dorsal regions, not in the ventral horn [72]. Based on its mechanism, it seems plausible that RLZ is a potential treatment to diminish neurological tissue destruction and to promote recovery in animal SCI [73].
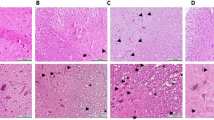
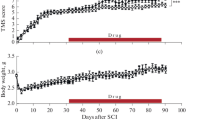
Delayed Neuroprotection by RLZ of Locomotor Networks and Neurons After Acute Injury In Vitro
In order to better mimic clinical settings with experimental models in vitro, investigating the question of how to reduce damage and increase cell survival during secondary injury requires the use of drugs to be administered after the lesion. Hence, our group has tested the effect of delayed application of RLZ on a model of KA-induced moderate excitotoxicity in the rat isolated spinal cord. The neurotoxic action of KA is routinely induced by a transient (1 h) application of this agent to replicate the condition of an acute injury when 1 h is often the shortest time for an acutely injured patient to be admitted to intensive care with life support and stabilization of critical parameters [38]. Figure 1b–e schematizes the protocols used for testing the effect of RLZ on KA-evoked excitotoxicity. In our model, KA-elicited damage is manifested within the first 2–3 h and reaches an apparent steady state 24 h later (Fig. 1b) [58, 74]. While RLZ per se is not neurotoxic, its application at 5 µM concentration (corresponding to the plasma therapeutic concentration) for 3 or 24 h after KA (0.05 or 0.1 mM) induces partial neuroprotection in the grey matter (Fig. 2a), although motoneurons remain vulnerable to KA (Fig. 2b). The functional outcome for locomotor network activity cannot be assessed 24 h later because RLZ evokes long lasting depression of network excitability (Fig. 2c, d) from which recovery is very slow [46]. Additionally, we have also explored two other protocols (Fig. 1d, e) based on former studies which had shown positive effects of pre or co-application of RLZ on chemically-evoked neuronal damage [75, 76]. Nevertheless, even with these protocols, no additional benefit in terms of histological or functional recovery has been observed [46]. In summary, even when the excitotoxic insult is moderate, RLZ is not fully effective to prevent experimental neuronal loss. Perhaps RLZ might confer functional benefit and neuroprotection at later times, a notion that can only be tested with a longer surviving preparation, a difficult goal to achieve with the spinal cord in vitro [46]. It has been suggested that a reasonable time window for clinical trials would be 12 h post-injury, although it should be borne in mind that the pathological changes of SCI peak approximately four times more rapidly in animals (for example, rats) than in humans [10].

Figures c, d are reprinted from Sámano et al. [46]. A study of the potential neuroprotective effect of riluzole on locomotor networks of the neonatal rat spinal cord in vitro damaged by excitotoxicity. Copyright (2012), with permission from Elsevier
RLZ administration followed by KA insult partially neuroprotects neurons in gray matter. a Histograms of pyknosis occurrence in different spinal cord regions. Inset shows spinal cord half section with regions [dorsal, central, lateral and ventral white matter (LWM, VWM)] used for cell counting based on DAPI-staining. Significant tests are for 0.1 mM KA versus SHAM, and KA 0.1 mM/RLZ 5 µM versus KA 0.1 mM (*P < 0.01, **P < 0.001, ***P < 0.05). Scale bar = 100 µm. On the right, representative micrographs of cell nuclei stained with DAPI in the dorsal horn of SHAM (top), KA (0.1 mM; middle) or KA (0.1 mM) followed by RLZ 5 (5 µM; bottom). Major pyknosis is observed in the dorsal region after KA (0.1 mM) application (middle), which is modestly reduced after treatment with 24 h RLZ (5 µM; black arrows in bottom micrograph). Scale bar = 50 µm. b Histograms showing number of SMI-32 positive motoneurons in ventral horn 24 h in SHAM, RLZ per se, KA (0.1 mM) alone or treated with RLZ (5 µM) after washout of KA (0.1 mM). Statistical difference is only observed when comparing KA 0.1 mM alone versus SHAM (*P < 0.01, n = 6). Right panels depict representative micrographs of SMI-32 positive motoneurons in ventral region for SHAM (left), KA 0.1 mM (right) and KA 0.1 mM/RLZ 5 µM (bottom). Scale bar = 100 µm. c Alternating oscillations typical of fictive locomotion induced by bath-applied NMDA (4 µΜ) and 5-HT (10 µM) are observed in control (CTR, left), and are absent after 24 h RLZ (5 µM) application (right). d Example of cumulative depolarization and oscillatory activity induced electrically by train of stimuli applied to dorsal root (DR) in control (left) and its block after 24 h RLZ 5 µM (right).
While Michaelis has delineated the concept of selective vulnerability of certain brain neurons [77], the molecular mechanisms making RLZ particularly ineffective on motoneurons [46, 72] remain elusive. The dorsal horn region is better protected by RLZ despite its higher number of neurons and larger density of glutamate receptors [45, 46]. Perhaps excitotoxicity in the ventral horn develops with distinctive (though unclear) mechanisms insensitive to RLZ. Furthermore, even when RLZ inhibits KA-evoked glutamate release [72], this drug might be unable to block the direct depolarization of neurons by KA, a phenomenon likely to be intense for motoneurons that are located in superficial laminae and readily suffer from excessive depolarization [78].
Clinical trials with RLZ have been conducted in phase I/IIa for patients with SCI between 2010 and 2011 [10], and have shown that RLZ induces some neurological improvement and has a well-defined safety profile in patients with relatively few (and not serious) adverse effects. However, there is still the need to extend these clinical data. In fact, the international multi-center clinical trial named “Riluzole in Acute Spinal Cord Injury Study” (RISCIS) is currently at phase II/III with the aim of continuing the evaluation of the efficacy and safety of RLZ in patients with acute SCI. The study started in August 2013 and the estimated study completion date is December 2018 (https://clinicaltrials.gov/ct2/show/results/NCT01597518) [79, 80].
Use of MPSS as Neuroprotective Compound
The current scenario of new cases of SCI is gradually changing as trauma is no more the principal cause. Thus, the non-traumatic cases of SCI have increased, including those due to spinal cord ischemia (without fractures) which usually are incomplete. In comparison to traumatic SCI, there is relatively little research on non-traumatic SCI epidemiology. While this condition was thought to be rare in children, it is now recognized as a cause of paediatric paraplegia [81]. Hence, the proposal of studying neonatal spinal cord preparations is not too remote from what occurs in clinical conditions. Nowadays a significant proportion of individuals admitted to rehabilitation are patients with non-traumatic SCI [14, 15]. For a long time, steroid therapy based on methylprednisolone sodium succinate (MPSS) (Fig. 3a) has been applied as the “first approach protector” against ALS and acute SCI [82, 83]. Curiously, even though MPSS has been widely used clinically because its potent anti-inflammatory, antioxidant and anti-lipoperoxidation properties, it has not yet received FDA approval [84, 85]. The rationale for using MPSS in acute SCI was based on the destructive processes affecting the white matter as consequence of ischemia and lipoperoxidation [86]. In fact, experimental studies of laboratory animals have shown beneficial actions by MPSS after acute SCI, especially for white matter oligodendrocytes and with early delivery of this drug [87,88,89]. Due to promising initial reports from experimental studies, multicenter clinical trials, referred to as National Acute Spinal Cord Injury Study Trials (NASCIS I, II and III) were developed as summarized in large scale reviews [90, 91]. After the publication of these trials, the use of MPSS generated significant controversy because the moderate neurological improvement was often coupled to important side effects such as serious infective disease [92]. To date, the clinical and scientific communities remain divided over the use of this drug as the main treatment: nevertheless, MPSS is still used and, at times, considered as “standard of care” for acute SCI [86].

Figures d, e are reprinted from Sámano et al. [56]. A study of methylprednisolone neuroprotection against acute injury to the rat spinal cord in vitro. Copyright (2016), with permission from Elsevier. (Color figure online)
Chemical structure of SOLU-MEDROL© (Pfizer) or Methylprednisolone Sodium Succinate (MPSS) and its molecular weight (MW). b Percentage of pyknosis in the regions shown in the spinal cord half section (dorsal, central, ventral, white matter, lateral and ventral white matter (WM, LWM, VWM)) in SHAM, MPSS (10 µM) alone, pathological medium (PM) or MPSS (10 µM) after PM. Scale bar = 100 µm. MPSS per se is not toxic, while there is significant increase in pyknotic nuclei of white matter in samples exposed to PM alone versus SHAM preparations (*P < 0.05 and **P < 0.01). For those samples treated with PM followed by 24 h MPSS, significant decrease in pyknosis is found in WM zones versus PM alone (***P < 0.001). On the right, the white arrows show in the micrographs representative examples of spinal cord preparations in the region VWM (SHAM, top panel, with minimal pyknosis), treated with PM showing abundant pyknosis in VWM (middle panel), and with PM/MPSS (10 µM) showing lower pyknosis in the same area (bottom panel). c Examples of confocal images of GFAP positive fibers (green) together with DAPI staining (red pseudocolor to improve contrast) in a section of VWM in SHAM, PM (alone for 1 h), or 24 h MPSS after PM application. White arrows show in SHAM large GFAP signal and few pyknotic nuclei, while in PM samples there is large loss of GFAP-positive fibers with abundant pyknosis, whereas PM/MPSS 10 µM treatment induces some recovery of immunofluorescence intensity to GFAP-stained fibers although pyknosis remains abundant. Scale bar = 100 µm. The plot represents the intensity of fluorescence from GFAP positive fibers for each condition (expressed as arbitrary units, AU). Data are significantly different in WM areas between PM versus SHAM and PM/MPSS 10 µM versus PM alone (***P < 0.001, **P < 0.01). d Representative records of cumulative depolarization of SHAM, PM, and PM/MPSS 10 µM treated preparations. e No significant improvement was found by MPSS (10 µM) administration for 24 h.
MPSS Preferentially Protects Glial Cells of the White Matter After Acute Spinal Injury
Our reports with the in vitro SCI preparation have shown that a pathological medium (PM; containing free radicals and hypoxic/aglycemic conditions) preferentially damages white matter and slows down fictive locomotion [11, 46, 54,55,56]. These results have led us to explore whether any neuroprotection by MPSS might be dependent on the type of SCI and be differentially effective on white or gray matter. Our experimental protocols have employed moderate excitotoxicity (through KA application) or PM damage (mimicking the dysmetabolic perturbations occurring after a vascular dysfunction) [46, 64]. Thus, we have found that MPSS per se (6–10 µM for 24 h: concentration based on published clinical guidelines [93]) has no toxic effects on spinal cord preparations. Starting 1 h after PM, continuous application of MPSS is associated with significantly lower number of pyknotic nuclei, and a larger number of surviving astrocytes and oligodendrocytes in the ventrolateral region of the white matter, despite a substantial number of dead cells (Fig. 3b, c). Although dorsal root stimulus trains can still elicit cumulative depolarization of premotoneurons and motoneurons, this response remains virtually free from alternating oscillations expressed by lumbar locomotor networks (Fig. 3d, e). It is noteworthy that both concentrations of MPSS (6 or 10 µM; 24 h) are equi-effective, suggesting that the full effect had been attained. After KA (0.1 mM; 1 h), MPSS (6 or 10 µM) application does not stop gray matter pyknosis and does not allow recovery in locomotor network function. In particular, motoneurons, which are highly vulnerable to KA, cannot be rescued with 24 h MPSS treatment [46, 56].
These data accord with previous in vivo and in vitro studies of the rat SCI indicating that MPSS can reduce loss of glia even though the functional gain remains questionable [87,88,89]. Nonetheless, many issues remain unanswered, for example: (i) are glial cells within the gray or white matter differentially sensitive to lesion? (ii) what are the mechanisms underlying the action of MPSS against acute SCI? and (iii) what factors are important to direct the action of MPSS to white matter glial cells rather than gray matter neurons? It is of interest that prospective studies of longterm neurological recovery after SCI have shown no systematic improvement in motor scores of acute SCI patients after a MPSS bolus [94] although conscious patients with acute SCI at hospital admission favor administration of MPPS even for allegedly minor neurological improvement [95].
Conclusions and Future Directions
Different approaches have been probed in a large range of experimental models in vitro and in vivo to generate new pharmacological strategies potentially transferable from bench to bedside. Although early therapeutic interventions to avoid chronicity and to promote repair and/or recovery after SCI have been widely explored, less focus has been directed to find out pharmacological treatments preferential to neurons or glial cells. Figure 4 summarizes current information concerning the molecular targets involved in the effects of RLZ (a–d) or MPSS (e–l).
Schematic diagram summarizing the main mechanisms exerted by RLZ or MPSS against noxious processes (glutamate excitotoxicity, hypoxia, ischemia, etc) when spinal cord tissue reacts to the primary injury. Since secondary injury is an important target for drug therapy, multiple, beneficial effects (a–d) could be induced by low micromolar concentrations of RLZ (5 µM) treatment, particularly to neurons of the spinal gray. RLZ may increase neuronal and glial (astrocytic) glutamate uptake (a), as well as block presynaptic release of glutamate from hyperactive synapses, thus reducing further excessive release of glutamate (b). These processes contribute to limit glutamate binding to its different ionotropic (NMDAr, AMPAr and KAINATEr) and metabotropic receptors (mGluR). Persistent activation of ionotropic receptors overloads neuron with Ca2+, triggering in turn excitotoxic cell death pathways. Since RLZ can block persistent Na+ currents (c), it diminishes the long-lasting firing of action potentials by neurons, dampens neuronal excitability and cell death in certain areas (d). MPSS induces glial cell-selective protection (astrocytes and oligodendrocytes) in the white matter. In astrocytes MPSS can limit ROS production (e), membrane lipoperoxidation (f), and apoptotic cell death (g) after injury. In oligodendrocytes (OLs) MPSS reverses apoptotic processes via activation of glucocorticoid receptors (GR) (h). Down-regulation of bcl-xL (an important anti-apoptotic regulator, and splicing isoform of bcl-x gene) (i), activation of caspase-3 (j) and DNA laddering can all be attenuated by MPSS in OLs [87]. The anti-apoptotic effects of MPSS can be also exerted through binding of GR to STAT5 (a transcription factor from the family of signal transducers and activators of STAT), which in turn modulates bcl-x gene expression (k) [88]. MPSS can also protects OLs against excitotoxicity via interaction with HIF-1α/Epo (hypoxic inducing factor 1α/neuroprotective cytokine erythropoietin) (l) [89]. The red crosses represent noxious effects counteracted by RLZ in neurons or by MPSS in glial cells (astrocytes and oligodendrocytes)
These results lead us to ask what is the best choice of clinically-available drugs, namely RLZ or MPSS? The answer may probably depend on the type, circumstances and severity of the lesion. It might be even worth considering the possibility of combining these drugs to attack different pathophysiological aspects and to provide improved neuroprotection to the spinal tissue. However, it is also essential to evaluate the potential side effects exerted by these compounds, and their synergy. Although we did not test the effects of combination of RLZ and MPSS on our in vitro acute SCI preparation, another report indicates no additional benefit or dramatic neuroprotection in gray and/or white matter [96].
To date, most pharmacological strategies have been based on the concept of blocking the effects of glutamate on network excitability. In principle, however, it should be feasible to dampen excitation by enhancing intrinsic inhibitory mechanisms. In this sense, recent results showing depression of neuronal excitability and neuroprotection by facilitating the operation of leak K+ currents with volatile anesthetics [97] or GABA-mediated synaptic inhibition with i.v. anesthetics like propofol [98] are encouraging.
Abbreviations
- ALS:
-
Amyotrophic lateral sclerosis
- AMPA:
-
Alpha-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid
- ASIA:
-
American Spinal Injury Association
- AU:
-
Arbitrary units
- bcl-xL :
-
Anti-apoptotic regulator, and splicing isoform of bcl-x gene
- BCSFB:
-
Blood-cerebrospinal fluid barrier
- BLMB:
-
Blood-leptomeningeal barrier
- BSB:
-
Blood-spinal barrier
- CD200L:
-
CD200 ligand
- CD200R:
-
CD200 receptor
- CNS:
-
Central nervous system
- CPG:
-
Central pattern generators
- SCI:
-
Spinal cord injury
- DAPI:
-
4′,6-Diamidino-2-phenylindole
- EAAT:
-
Excitatory amino acid transporters
- EPO:
-
Cytokine erythropoietin
- FDA:
-
Food and Drug Administration
- GFAP:
-
Glial fibrillary acidic protein
- GR:
-
Glucocorticoid receptor
- HIF1α:
-
Hypoxic inducing factor 1α
- hCNS-SCns:
-
Human central nervous system-derived neural stem cell
- i.v.:
-
Intravenous
- IL:
-
Interleukin
- KA:
-
Kainate
- LWM:
-
Lateral white matter
- MBP:
-
Mature myelin basic protein
- MPSS:
-
Methylprednisolone sodium succinate
- NASCIS:
-
National Acute Spinal Cord Injury Study Trials
- NMDA:
-
N-methyl-d-aspartic acid
- nNOS:
-
Neuronal nitric oxide synthase
- OLs:
-
Oligodendrocytes
- PM:
-
Pathological medium
- RISCIS:
-
Riluzole in Acute Spinal Cord Injury Study
- RLZ:
-
Riluzole or rilutek
- RNS:
-
Reactive nitrogen species
- ROS:
-
Reactive oxygen species
- SMI-32:
-
Neurofilament H non-phosphorylated antibody
- SOD-1:
-
Superoxide dismutase
- STAT5:
-
Activator transcription factor STAT
- TBOA:
-
Threo-β-benzyloxyaspartate
- TNF-α:
-
Tumor necrosis factor alpha
- TRPM:
-
Transient receptor potential cation channel, subfamily M
- VWM:
-
Ventral white matter
- WM:
-
White matter
- Wsh:
-
Washout
- 5-HT:
-
5-Hydroxytryptamine
References
Furlan JC, Sakakibara BM, Miller WC, Krassioukov AV (2013) Global incidence and prevalence of traumatic spinal cord injury. Can J Neurol Sci 40:456–464
Singh A, Tetreault L, Kalsi-Ryan S, Nouri A, Fehlings MG (2014) Global prevalence and incidence of traumatic spinal cord injury. Clin Epidemiol 6:309–331. https://doi.org/10.2147/CLEP.S68889
Leonard M, Sproule J, McCormack D (2007) Paediatric spinal trauma and associated injuries. Injury 38:188–193
Cristante AF, Barros Filho TE, Marcon RM, Letaif OB, Rocha ID (2002) Therapeutic approaches for spinal cord injury. Clinics 67:1219–1224
Ahuja CS, Martin AR, Fehlings M (2016) Recent advances in managing a spinal cord injury secondary to trauma. F1000Research 5:1–13. https://doi.org/10.12688/f1000research.7586.1
Ahuja CS, Nori S, Tetreault L, Wilson J, Kwon B, Harrop J, Choi D, Fehlings MG (2017) Traumatic spinal cord injury-repair and regeneration. Neurosurgery 1:S9–S22. https://doi.org/10.1093/neuros/nyw080
Rabchevsky AG, Fugaccia I, Sullivan PG, Blades DA, Scheff SW (2002) Efficacy of methylprednisolone therapy for the injured rat spinal cord. J Neurosci Res 1:7–18
Hawryluk GW, Rowland J, Kwon BK, Fehlings MG (2008) Protection and repair of the injured spinal cord: a review of completed, ongoing, and planned clinical trials for acute spinal cord injury. Neurosurg Focus 25:E14. https://doi.org/10.3171/FOC.2008.25.11.E14
Wilson JR, Fehlings MG (2014) Riluzole for acute traumatic spinal cord injury: a promising neuroprotective treatment strategy. World Neurosurg 81:825–829. https://doi.org/10.1016/j.wneu.2013.01.001
Nagoshi N, Nakashima H, Fehlings MG (2015) Riluzole as a neuroprotective drug for spinal cord injury: from bench to bedside. Molecules 20:7775–7789. https://doi.org/10.3390/molecules20057775
Taccola G, Margaryan G, Mladinic M, Nistri A (2008) Kainate and metabolic perturbation mimicking spinal injury differentially contribute to early damage of locomotor networks in the in vitro neonatal rat spinal cord. Neuroscience 155:538–555. https://doi.org/10.1016/j.neuroscience.2008.06.008
Kuzhandaivel A, Nistri A, Mazzone GL, Mladinic M (2011) Molecular mechanisms underlying cell death in spinal networks in relation to locomotor activity after acute injury in vitro. Front Cell Neurosci 5:1–17. https://doi.org/10.3389/fncel.2011.00009
Chang HH, Michaelis EK, Roy S (1984) Functional characteristics of L-glutamate. N-methyl-D-aspartate and kainate receptors in isolated brain synaptic membranes. Neurochem Res 9:903–915
Rossignol S, Schwab M, Schwartz M, Fehlings MG (2007) Spinal cord injury: time to move? J Neurosci 27:11782–11792
van den Berg ME, Castellote JM, Mahillo-Fernandez I, de Pedro-Cuesta J (2010) Incidence of spinal cord injury worldwide: a systematic review. Neuroepidemiology 34:184–192. https://doi.org/10.1159/000279335
Courtine G, van den Brand R, Musienko P (2011) Spinal cord injury: time to move. Lancet 4:1896–1998. https://doi.org/10.1016/S0140-6736(11)60711-3
Rowland JW, Hawryluk GW, Kwon B, Fehlings MG (2008) Current status of acute spinal cord injury pathophysiology and emerging therapies: promise on the horizon. Neurosurg Focus 25:1–17. https://doi.org/10.3171/FOC.2008.25.11.E2
Ufuk T, Ganesh S, Sigurd B (2005) Spine cord injury: an update. Semin Spine Surg 17:73–83
Dumont RJ, Okonkwo DO, Verma S, Hurlbert RJ, Boulos PT. Ellegala DB, Dumont AS (2001) Acute spinal cord injury, part I: pathophysiologic mechanisms. Clin Neuropharmacol 24:254–264
Michaelis EK (1998) Molecular biology of glutamate receptors in the central nervous system and their role in excitotoxicity, oxidative stress and aging. Prog Neurobiol 54:369–415
Park E, Velumian AA, Fehlings MG (2004) The role of excitotoxicity in secondary mechanisms of spinal cord injury: a review with an emphasis on the implications for white matter degeneration. J Neurotrauma 21:754–774
Szydlowska K, Tymianski M (2010) Calcium, ischemia and excitotoxicity. Cell Calcium 47:122–129. https://doi.org/10.1016/j.ceca.2010.01.003
Choi DW (1992) Excitotoxic cell death. J Neurobiol 23:1261–1276
King AE, Woodhouse A, Kirkcaldie MT, Vickers JC (2016) Excitotoxicity in ALS: overstimulation, or overreaction? Exp Neurol 1:162–171. https://doi.org/10.1016/j.expneurol.2015.09.019
Aarts MM, Tymianski M (2005) TRPMs and neuronal cell death. Pflügers Arch 451:243–249
Bianchetti E, Mladinic M, Nistri A (2013) Mechanisms underlying cell death in ischemia-like damage to the rat spinal cord in vitro. Cell Death Dis 4:e707. https://doi.org/10.1038/cddis.2013.237
Lewerenz J, Maher P (2015) Chronic glutamate toxicity in neurodegenerative diseases—what is the evidence? Front Neurosci 16:1–20. https://doi.org/10.3389/fnins.2015.00469
Lau A, Tymianski M (2010) Glutamate receptors, neurotoxicity and neurodegeneration. Pflugers Arch 460:525–542
Fern R, Moller T (2000) Rapid ischemic cell death in immature oligodendrocytes: a fatal glutamate release feedback loop. J Neurosci 20:34–42
Buisson A, Choi DW (1995) The inhibitory mGluR agonist, S-4-carboxy-3-hydroxy-phenylglycine selectively attenuates NMDA neurotoxicity and oxygen-glucose deprivation-induced neuronal death. Neuropharmacology 34:1081–1087
Colwell CS, Altemus KL, Levine MS (1996) Metabotropic glutamate receptor activation selectively limits excitotoxic damage in the intact neostriatum. Brain Res 726:223–226
Pizzi M, Consolandi O, Memo M, Spano PF (1996) Activation of multiple metabotropic glutamate receptor subtypes prevents NMDA-induced excitotoxicity in rat hippocampal slices. Eur J Neurosci 8:1516–1521
Rust R, Kaiser J (2017) Insights into the dual role of inflammation after spinal cord injury. J Neurosci 37:4658–4660. https://doi.org/10.1523/JNEUROSCI.0498-17.2017
Mietto BS, Mostacada K, Martinez AM (2015) Neurotrauma and inflammation: CNS and PNS responses. Mediat Inflamm 2015:251204. https://doi.org/10.1155/2015/251204
Arnett HA, Mason J, Marino M, Suzuki K, Matsushima GK, Ting JP (2001) TNF alpha promotes proliferation of oligodendrocyte progenitors and remyelination. Nat Neurosci 4:1116–1122
Fehlings MG, Nguyen DH (2010) Immunoglobulin G: a potential treatment to attenuate neuroinflammation following spinal cord injury. J Clin Immunol 1:S109–S112. https://doi.org/10.1007/s10875-010-9404-7
David S, Kroner A (2011) Repertoire of microglial and macrophage responses after spinal cord injury. Nat Rev Neurosci 12:388–399. https://doi.org/10.1038/nrn3053
Piltti KM1, Salazar DL, Uchida N, Cummings BJ, Anderson AJ (2013) Safety of epicenter versus intact parenchyma as a transplantation site for human neural stem cells for spinal cord injury therapy. Stem Cells Transl Med 2:204–216. https://doi.org/10.5966/sctm.2012-0110
Saghazadeh A, Rezaei N (2017) The role of timing in the treatment of spinal cord injury. Biomed Pharmacother 92:128–139. https://doi.org/10.1016/j.biopha.2017.05.048
Anderson MA, Burda JE, Ren Y, Ao Y, O’Shea TM, Kawaguchi R, Coppola G, Khakh BS, Deming TJ, Sofroniew MV (2016) Astrocyte scar formation aids central nervous system axon regeneration. Nature 532:195–200. https://doi.org/10.1038/nature17623
Cohen M, Ben-Yehuda H, Porat Z, Raposo C, Gordon S, Schwartz M (2017) Newly formed endothelial cells regulate myeloid cell activity following spinal cord injury via expression of CD200 ligand. J Neurosci 25:972–985. https://doi.org/10.1523/JNEUROSCI.2199-16.2016
Wright GJ, Jones M, Puklavec MJ, Brown MH, Barclay AN (2001) The unusual distribution of the neuronal/lymphoid cell surface CD200 (OX2) glycoprotein is conserved in humans. 102(2):173–179
Constanti A, Nistri A (1976) A comparative study of the effects of glutamate and kainate on the lobster muscle fibre and the frog spinal cord. Br J Pharmacol 57:359–368
Magnuson DS, Trinder TC, Zhang YP, Burke D, Morassutti DJ, Shields CB (1999) Comparing deficits following excitotoxic and contusion injuries in the thoracic and lumbar spinal cord of the adult rat. Exp Neurol 156:191–204
Mazzone GL, Margaryan G, Kuzhandaivel A, Nasrabady SE, Mladinic M, Nistri A (2010) Kainate-induced delayed onset of excitotoxicity with functional loss unrelated to the extent of neuronal damage in the in vitro spinal cord. Neuroscience 168:451–462. https://doi.org/10.1016/j.neuroscience.2010.03.055
Sámano C, Nasrabady SE, Nistri A (2012) A study of the potential neuroprotective effect of riluzole on locomotor networks of the neonatal rat spinal cord in vitro damaged by excitotoxicity. Neuroscience 222:356–365. https://doi.org/10.1016/j.neuroscience.2012.06.064
Kiehn O, Kjaerulff O (1998) Distribution of central pattern generators for rhythmic motor outputs in the spinal cord of limbed vertebrates. Ann N Y Acad Sci 860:110–129
Tolle TR, Berthele A, Zieglgansberger W, Seeburg PH, Wisden W (1993) The differential expression of 16 NMDA and non-NMDA receptor subunits in the rat spinal cord and in periaqueductal gray. J Neurosci 13:5009–5028
Cifra A, Mazzone GL, Nani F, Nistri A, Mladinic M (2012) Postnatal developmental profile of neurons and glia in motor nuclei of the brainstem and spinal cord, and its comparison with organotypic slice cultures. Dev Neurobiol 72:1140–1160. https://doi.org/10.1002/dneu.20991
McTigue DM, Tripathi RB (2008) The life, death, and replacement of oligodendrocytes in the adult CNS. J Neurochem 107:1–19. https://doi.org/10.1111/j.1471-4159.2008.05570.x
Volpe JJ (1997) Brain injury in the premature infant: from pathogenesis to prevention. Brain Dev 19:519–534
Rosenberg PA, Dai W, Gan XD, Ali S, Fu J, Back SA, Sanchez RM, Segal MM, Follett PL, Jensen FE, Volpe JJ (2003) Mature myelin basic protein-expressing oligodendrocytes are insensitive to kainate toxicity. J Neurosci Res 71:237–245
Follett PL, Rosenberg PA, Volpe JJ, Jensen FE (2000) NBQX attenuates excitotoxic injury in developing white matter. J Neurosci 15:9235–9241
Margaryan G, Mladinic M, Mattioli C, Nistri A (2009) Extracellular magnesium enhances the damage to locomotor networks produced by metabolic perturbation mimicking spinal injury in the neonatal rat spinal cord in vitro. Neuroscience 163:669–682. https://doi.org/10.1016/j.neuroscience.2009.07.005
Kuzhandaivel A, Margaryan G, Nistri A, Mladinic M (2010) Extensive glial apoptosis develops early after hypoxic-dysmetabolic insult to the neonatal rat spinal cord in vitro. Neuroscience 169:325–338. https://doi.org/10.1016/j.neuroscience.2010.05.011
Sámano C, Kaur J, Nistri A (2016) A study of methylprednisolone neuroprotection against acute injury to the rat spinal cord in vitro. Neuroscience 315:136–149. https://doi.org/10.1016/j.neuroscience.2015.12.003
Eliasson MJ, Sampei K, Mandir AS, Hurn PD, Traystman RJ, Bao J, Pieper A, Wang ZQ, Dawson TM, Snyder SH, Dawson VL (1997) Poly(ADP-ribose) polymerase gene disruption renders mice resistant to cerebral ischemia. Nat Med 3:1089–1095
Nasrabady SE, Kuzhandaivel A, Nistri A (2011) Studies of locomotor network neuroprotection by the selective poly(ADP-ribose) polymerase-1 inhibitor PJ-34 against excitotoxic injury to the rat spinal cord in vitro. Eur J Neurosci 33:2216–2227. https://doi.org/10.1111/j.1460-9568.2011.07714.x
Nasrabady SE, Kuzhandaivel A, Akrami A, Bianchetti E, Milanese M, Bonanno G, Nistri A (2012) Unusual increase in lumbar network excitability of the rat spinal cord evoked by the PARP-1 inhibitor PJ-34 through inhibition of glutamate uptake. Neuropharmacology 63:415–426. https://doi.org/10.1016/j.neuropharm.2012.04.014
Mazzone GL, Mladinic M, Nistri A (2013) Excitotoxic cell death induces delayed proliferation of endogenous neuroprogenitor cells in organotypic slice cultures of the rat spinal cord. Cell Death Dis. https://doi.org/10.1038/cddis.2013.431
Mladinic M, Bianchetti E, Dekanic A, Mazzone GL, Nistri A (2014) ATF3 is a novel nuclear marker for migrating ependymal stem cells in the rat spinal cord. Stem Cell Res 12:815–827. https://doi.org/10.1016/j.scr.2014.03.006
Cox A, Varma A, Banik N (2015) Recent advances in the pharmacologic treatment of spinal cord injury. Metab Brain Dis 30:473–482. https://doi.org/10.1007/s11011-014-9547-y
Mazzone GL, Nistri A (2011) Electrochemical detection of endogenous glutamate release from rat spinal cord organotypic slices as a real-time method to monitor excitotoxicity. J Neurosci Methods 15:128–132. https://doi.org/10.1016/j.jneumeth.2011.01.033
Doble A (1999) The role of excitotoxicity in neurodegenerative disease: implications for therapy. Pharmacol Ther 81:163–221
Guidance on the use of Riluzole (Rilutek) for the treatment of Motor Neurone Disease. Technology appraisal guidance Published: 23 January 2001 http://www.nice.org.uk/guidance/ta20
Bellingham MC (2011) A review of the neural mechanisms of action and clinical efficiency of riluzole in treating amyotrophic lateral sclerosis: what have we learned in the last decade? CNS Neurosci Ther 17:4–31. https://doi.org/10.1111/j.1755-5949.2009.00116.x
Agrawal S, Fehlings M (1997) The effect of the sodium channel blocker QX-314 on recovery after acute spinal cord axonal injury. J Neurotrauma 14:81–88
Urbani A, Belluzzi O (2000) Riluzole inhibits the persistent sodium current in mammalian CNS neurons. Eur J Neurosci 12:3567–3574
Cifra A, Mazzone GL, Nistri A (2013) Riluzole: what it does to spinal and brainstem neurons and how it does it. Neuroscientist 19:137–144. https://doi.org/10.1177/1073858412444932
Lamanauskas N, Nistri A (2008) Riluzole blocks persistent Na+ and Ca2+ currents and modulates release of glutamate via presynaptic NMDA receptors on neonatal rat hypoglossal motoneurons in vitro. Eur J Neurosci 27:2501–2514. https://doi.org/10.1111/j.1460-9568.2008.06211.x
Cifra A, Nani F, Nistri A (2011) Respiratory motoneurons and pathological conditions: lessons from hypoglossal motoneurons challenged by excitotoxic or oxidative stress. Respir Physiol Neurobiol 179:89–96. https://doi.org/10.1016/j.resp.2011.03.017
Mazzone GL, Nistri A (2011) Delayed neuroprotection by riluzole against excitotoxic damage evoked by kainate on rat organotypic spinal cord cultures. Neuroscience 190:318–327. https://doi.org/10.1016/j.neuroscience.2011.06.013
Wilson JR, Fehlings MG (2014) Riluzole for acute traumatic spinal cord injury: a promising neuroprotective treatment strategy. World Neurosurg 8:825–829. https://doi.org/10.1016/j.wneu.2013.01.001
Kuzhandaivel A, Nistri A, Mladinic M (2010) Kainate-mediated excitotoxicity induces neuronal death in the rat spinal cord in vitro via a PARP-1 dependent cell death pathway (Parthanatos). Cell Mol Neurobiol 30:1001–1012. https://doi.org/10.1007/s10571-010-9531-y
Chang G, Guo Y, Jia Y, Duan W, Li B, Yu J, Li C (2010) Protective effect of combination of sulforaphane and riluzole on glutamate-mediated excitotoxicity. Biol Pharm Bull 33:1477–1483
Verhave PS, Jongsma MJ, Van Den Berg RM, Vanwersch RA, Smit AB, Philippens IH (2012) Neuroprotective effects of riluzole in early phase Parkinson’s disease on clinically relevant parameters in the marmoset MPTP model. Neuropharmacology 62:1700–1707. https://doi.org/10.1016/j.neuropharm.2011.11.016
Wang X, Michaelis EK (2010) Selective neuronal vulnerability to oxidative stress in the brain. Front Aging Neurosci. https://doi.org/10.3389/fnagi.2010.00012
Gou-Fabregas M, Garcera A, Mincheva S, Perez-Garcia MJ, Comella JX, Soler RM (2009) Specific vulnerability of mouse spinal cord motoneurons to membrane depolarization. J Neurochem 110:1842–1854. https://doi.org/10.1111/j.1471-4159.2009.06278.x
Fehlings MG, Kopjar B, Grossman RG (2016) 329 Efficacy and safety of Riluzole in acute spinal cord injury: rationale and design of AOSpine phase III multicenter double-blinded randomized controlled trial (RISCIS). Neurosurgery. https://doi.org/10.1227/01.neu.0000489818.21218.72
Grossman RG, Fehlings MG, Frankowski RF, Burau KD, Chow DS, Tator C, Teng A, Toups EG, Harrop JS, Aarabi B, Shaffrey CI, Johnson MM, Harkema SJ, Boakye M, Guest JD, Wilson JR (2014) A prospective, multicenter, phase I matched-comparison group trial of safety, pharmacokinetics, and preliminary efficacy of riluzole in patients with traumatic spinal cord injury. J Neurotrauma 31:239–255. https://doi.org/10.1089/neu.2013.2969
Nance JR, Golomb MR (2007) Ischemic spinal cord infarction in children without vertebral fracture. Pediatr Neurol 36:209–216
Bracken MB, Shepard MJ, Collins WF et al (1990) A randomized, controlled trial of methylprednisolone or naloxone in the treatment of acute spinal cord injury. Results of the second National Acute Spinal Cord Injury Study. N Engl J Med 322:1405–1411
Bracken MB, Shepard MJ, Collins WF et al (1992) Methylprednisolone or naloxone treatment after acute spinal cord injury: I-year follow-up data. Results of the second National Acute Spinal Cord Injury Study, 1992. J Neurosurg 76:23–31
Cheung V, Hoshide R, Bansal V, Kasper E, Chen CC (2015) Methylprednisolone in the management of spinal cord injuries: lessons from randomized, controlled trials. Surg Neurol Int 6:142. https://doi.org/10.4103/2152-7806.163452
Hall ED (2011) Antioxidant therapies for acute spinal cord injury. Neurotherapeutics 8:152–167. https://doi.org/10.1007/s13311-011-0026-4
Miekisiak G, Kloc W, Janusz W, Kaczmarczyk J, Latka D, Zarzycki D (2014) Current use of methylprednisolone for acute spinal cord injury in Poland: survey study. Eur J Orthop Surg Traumatol 24:S269–S273. https://doi.org/10.1007/s00590-014-1422-3
Lee JM, Yan P, Xiao Q, Chen S, Lee KY, Hsu CY, Xu J (2008) Methylprednisolone protects oligodendrocytes but not neurons after spinal cord injury. J Neurosci 28:3141–3149. https://doi.org/10.1523/JNEUROSCI.5547-07.2008
Xu J, Chen S, Chen H, Xiao Q, Hsu CY, Michael D, Bao J (2009) STAT5 mediates antiapoptotic effects of methylprednisolone on oligodendrocytes. J Neurosci 29:2022–2026. https://doi.org/10.1523/JNEUROSCI.2621-08.2009
Sun YY, Wang CY, Hsu MF, Juan SH, Chang CY, Chou CM, Yang LY, Hung KS, Xu J, Lee YH, Hsu CY (2010) Glucocorticoid protection of oligodendrocytes against excitotoxin involving hypoxia-inducible factor-1alpha in a cell-type-specific manner. J Neurosci 30:9621–9630. https://doi.org/10.1523/JNEUROSCI.2295-10.2010
Bracken MB (2012) Steroids for acute spinal cord injury. Cochrane Database Syst Rev 18:1–51. https://doi.org/10.1002/14651858.CD001046.pub2
Harrop JS (2014) Spinal cord injury: debating the efficacy of methylprednisolone. Neurosurgery 61:30–31. https://doi.org/10.1227/NEU.0000000000000391
Fehlings MG, Wilson JR, Cho N (2014) Methylprednisolone for the treatment of acute spinal cord injury: counterpoint. Neurosurgery 1:36–42. https://doi.org/10.1227/NEU.0000000000000412
Sauerland S, Nagelschmidt M, Mallmann P, Neugebauer EA (2000) Risks and benefits of preoperative high dose methylprednisolone in surgical patients: a systematic review. Drug Saf 23:449–461
Ito Y, Sugimoto Y, Tomioka M, Kai N, Tanaka M (2009) Does high dose methylprednisolone sodium succinate really improve neurological status in patient with acute cervical cord injury?: a prospective study about neurological recovery and early complications. Spine 34:2121–2124. https://doi.org/10.1097/BRS.0b013e3181b613c7
Bowers CA, Kundu B, Rosenbluth J, Hawryluk GW (2016) Patients with spinal cord injuries favor administration of methylprednisolone. PLoS ONE. https://doi.org/10.1371/journal.pone.0145991
Mu X, Azbill RD, Springer JE (2000) Riluzole and methylprednisolone combined treatment improves functional recovery in traumatic spinal cord injury. J Neurotrauma 17:773–780
Shabbir A, Bianchetti E, Nistri A (2015) The volatile anesthetic methoxyflurane protects motoneurons against excitotoxicity in an in vitro model of rat spinal cord injury. Neuroscience 285:269–280. https://doi.org/10.1016/j.neuroscience.2014.11.023
Kaur J, Flores Gutiérrez J, Nistri A (2016) Neuroprotective effect of propofol against excitotoxic injury to locomotor networks of the rat spinal cord in vitro. Eur J Neurosci 44:2418–2430. https://doi.org/10.1111/ejn.13353
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sámano, C., Nistri, A. Mechanism of Neuroprotection Against Experimental Spinal Cord Injury by Riluzole or Methylprednisolone. Neurochem Res 44, 200–213 (2019). https://doi.org/10.1007/s11064-017-2459-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-017-2459-6