Abstract
Purpose
The controversial practice of methylprednisolone (MP) application in acute spinal cord injury (ASCI) is gradually decreasing. This is a survey study designed to assess the current use of MP in ASCI in Poland.
Methods
The questionnaire comprised of five questions was distributed among 251 spinal surgeons, members of the Polish Society of Spinal Surgery. One hundred and ten (43.8 %) responded, and data from 108 were included in the study.
Results
Majority of respondents (73.1 %) declared the use of MP in ASCI. Most of them (41.7 %) adhered to the NASCIS II protocol, and 24.1 % rather used the NASCIS III protocol. Predominant rationale for the use of steroids was fear of litigation (36.7 %), 30.4 % declared it is as an institutional standard, nearly one-third believed in the effectiveness of drug in improving neurological outcomes. The subgroup analyses revealed no statistically significant interaction for specialty, age, personal involvement in care and institutional case volume.
Conclusions
As opposed to the literature data from similar studies performed in other countries, the rate of use of MP in ASCI remains high.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinal cord injury (SCI) remains a devastating condition often affecting young, otherwise healthy individuals. In Poland, the annual incidence of SCI is approximately 14.5 per 1 million population [1]. Intensive research over the years has led to a comprehensive understanding of its mechanisms; however, these advances have not translated into improved neurological outcomes. Though many new methods of treatment have been proposed to manage acute spinal cord injury (ASCI) over the last few decades, only one treatment regimen based on the high-dose methylprednisolone (MP) was widely introduced into clinical practice.
The publications of results from NASICIS II and III trials in early 90s [2, 3] resulted in international recognition of this therapy as a standard for the treatment of ASCI, but soon it became a subject of much controversy and criticism. Many reports pointed to numerous flaws of NASCIS series trials such as improper randomization, inadequate assessment of outcomes, incomplete reporting of results and, most of all, drawing conclusions from the post hoc analysis [4]. However, despite heavy critique from many authors, MP remained in use even if the rationale has changed over time. A survey study in 2006 by Eck et al. [5] revealed that majority of respondents used MP out of fear of litigation. With the increasing evidence of serious side effects far exceeding the potential benefits, MP use in ASCI started to decrease worldwide [6, 7]. In the second iteration of guidelines for the management of ASCI by the AANS/CNS Joint Section on Disorders of the Spine and Peripheral Nerves published in 2013, there is a level I recommendation against the use of MP in ASCI [8]. Within a few months, similar recommendations were issued by the Polish Society of Spinal Surgery (PSoSS), a nonprofit medical association comprising of about 300 members, mostly, spine surgeons [9].
PSoSS is the largest organization in this field in Poland and is affiliated with the EuroSpine, the Spine Society of Europe. This survey study was designed to assess the current status of MP use in SCI in Poland among practicing spinal surgeons associated with the PSoSS. In particular, it aimed to determine which is the prevalent protocol and what is the rationale for this therapy.
Methods
The questionnaire comprised of five questions. The questions were pertained to the specialty, use of steroids in SCI including the protocol favored, rationale for its use, volume/number of SCI cases in his/her institution and the extent of personal involvement in SCI patient care (Table 1). The questionnaire was similar to the one designed by Eck et al. [5]. The demographic section of the form included only one question about the age of the respondent (≤45 or >45 years old). A self-validating web form was provided for data acquisition, allowing only clean and correct data, without missing values. The survey questionnaire was distributed to all the 251 spinal surgeons, members of the PSoSS, between March and May 2013. The results were presented as descriptive statistics. The Pearson’s Chi-square test was used to assess the significance of differences among defined subgroups.
Results
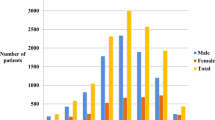
Out of 251 members of the PSoSS, 110 (43.8 %) responded. Data from two respondents were excluded, as they were practicing outside Poland. Thus, the final number of participating surgeons was 108. The resulting data are shown in Table 2. There were 44 orthopedic surgeons (nine in training) and 64 neurosurgeons (12 in training). Seventy of them were aged 45 years or less, and 38 were more than 45 years old at the time of application. Nearly three quarters (73.1 %) of all the respondents declared the use of steroids, and majority (41.7 %) of them followed the NASCIS II protocol. Twenty-six (24.1 %) surgeons adhered to the NASCIS III protocol, four used steroids regardless of the timing of administration, and four used steroids other than MP. The differences among specialties were statistically not significant (p = 0.90). Likewise, the use of steroids was independent of other factors, such as the age, and the annual volume of SCI patients treated in respondents’ institution. In terms of rationale for treatment, the replies were almost equally distributed among the three available options. Nearly 33 % of respondents claim that their primary motivation for the use of steroids was their belief in the effectiveness of drug in improving the neurological outcomes. Institutional standard is a rationale in 30.4 %, but a majority (36.7 %) of the respondents used steroids for medicolegal reasons. Orthopedic surgeons believe that clinical benefit is seen in 40.6 % in MP users compared to 27.7 % in nonusers. Thirty-four percent of neurosurgeons claimed that they used the MP therapy as an institutional standard. A quarter of orthopedic surgeons marked this option. The differences in rationales for treatment among specialties were not statistically significant (p = 0.46).
Discussion
After publication of the results of NASCIS II trial [8], MP instantaneously became an unofficial standard of treatment. The lack of viable treatment options targeted to abate secondary injury, together with a tremendous pressure from the society, propelled the acceptance of this new standard of care. This hasty validation of a new treatment did not go unnoticed by the professional community. Soon, articles criticizing the NASCIS series were published. Although these studies were well prepared and executed, the conclusions were drawn up upon the retrospective analysis of data, as the primary data failed to show significant differences in motor outcomes between the treatment groups. Thus, these trials cannot be classified as level I, but rather level III. Other authors point to numerous other flaws, such as improper randomization [4], lack of compelling data and failure to include functional outcomes important to the patients [10]. Overall, these studies do not provide sufficiently strong evidences to justify the use of MP in ASCI. Furthermore, the NASCIS studies were not followed by other trials of adequate size and quality supporting the use of MP. On the contrary, there is mounting clinical evidence that MP in high doses has a potential for major complications, such as sepsis, pneumonia, urinary tract infection, gastrointestinal ulcer/bleeding and pulmonary embolism [11–13]. Corticosteroid Randomization after Significant Head injury (CRASH) was a large international trial designed to assess the safety and efficacy of the corticosteroids for the treatment of traumatic brain injury [14]. Initially planned to enroll 20,000 patients, it was terminated halfway through when the interim analysis revealed significantly increased mortality in the MP treated group. Although this study did not address the SCI patients directly, it further heated up the debate on the safety of MP administration as the protocol of MP administration was similar to that of NASCIS III study.
In 2013, an important set of guidelines were published by the AANS/CNS Joint Section on Disorders of the Spine and Peripheral Nerves [6]. For the first time, level I recommendation was made against the use of MP in ASCI. The authors stated that there are sufficient Class I, Class II and Class III evidences and that high-dose steroids are associated with harmful side effects including death.
As a result of prolonged international dispute, a steady decline in the use of MP in ASCI is observed. Other articles similar to this have also shown this trend in several countries across the globe. A Canadian study in 2008 by Hurlbert and Hamilton [7] compared the survey data from 2001 to 2006 and showed a complete reversal of practice. The number of respondents using MP dropped from 76 % in 2001 to 24 % in 2006. In another survey in 2012 of neurosurgeons practicing in the United Kingdom from [15], only 21 % recommended the use of glucocorticoids in an incomplete SCI (16 % patients). Felleiter et al. [6] retrospectively analyzed the changes in adherence to MP therapy in ASCI between the two study periods, 2001–2003 and 2008–2010, in Switzerland’s largest center dealing with SCI. The rate of patients treated with MP dropped from 96 % in 2001–2003 to 23 % in 2008–2010. Interestingly, the pooled data showed a better rate of neurological improvement in MP users (32 vs 28 %), although the differences were statistically not significant. A national study on current practice of MP administration in ASCI in Germany [16] revealed that 55 % of surveyed departments still use MP. It is noteworthy that respondents from 14 departments (9.7 %), 11 of them from academic institutions, declared that they used an obsolete protocol from the NASCIS I trial.
There are certain limitations in this study. The most important one was its reliance on self-report data on respondents’ typical practice not the facts from medical records. Thus, the exact prevalence of MP use is not known. However, the intention of this study was to analyze current opinions in response to the publication of new recommendations. Another limitation comes from the lack of precise information on incidence of SCI in Poland in recent years, and it would allow to estimate to what extent the results are representative at the national level.
Our results show that despite available clinical evidence, the rate of practitioners using MP in Poland remains even higher (73.1 %) than in previously published studies. Moreover, more than one-third of respondents choose to use MP because of the fear of litigation. This is rather a subcultural belief without evidence backing. Such “defensive medicine” practices are very popular in Poland as formal recommendations are rarely formulated by responsible agencies often leading to actions contrary to patients’ best interest. Noteworthy is a greater percentage of more experienced surgeon refusing the MP treatment, albeit not statistically significant. The plausible explanation is that it is likely a consequence of greater confidence and hence lower fear of litigation related to more frequent exposure to SCI patients. We hope that the formulation of new relevant standards supported with subsequent information will help surgeons reject the harmful practice of MP application in ASCI.
Conclusions
This study concurs with previously published studies, that despite overwhelming evidence against the use of steroids in ASCI, this potentially harmful practice remains common. An informative campaign should be implemented to promote adherence to current standards, as the fear of litigation and lack of feasible options make the application of MP difficult to eradicate.
References
Pietraszkiewicz F, Tysiewicz-Dudek M (2010) Epidemiology of spinal injuries in Lubuskie Province. Ortop Traumatol Rehabil 12(5):435
Bracken MB, Shepard MJ, Collins WF, Holford TR, Young W, Baskin DS, Eisenberg HM, Flamm E, Leo-Summers L, Maroon J (1990) A randomized, controlled trial of methylprednisolone or naloxone in the treatment of acute spinal-cord injury: results of the Second National Acute Spinal Cord Injury Study. N Engl J Med 322(20):1405–1411
Bracken MB, Shepard MJ, Holford TR, Leo-Summers L, Aldrich EF, Fazl M, Fehlings M, Herr DL, Hitchon PW, Marshall LF (1997) Administration of methylprednisolone for 24 or 48 hours or tirilazad mesylate for 48 hours in the treatment of acute spinal cord injury results of the third national acute spinal cord injury randomized controlled trial. JAMA 277(20):1597–1604
Coleman WP, Benzel E, Cahill DW, Ducker T, Geisler F, Green B, Gropper MR, Goffin J, Madsen PW III, Maiman DJ (2000) A critical appraisal of the reporting of the National Acute Spinal Cord Injury Studies (II and III) of methylprednisolone in acute spinal cord injury. J Spinal Disord Tech 13(3):185–199
Eck JC, Nachtigall D, Humphreys SC, Hodges SD (2006) Questionnaire survey of spine surgeons on the use of methylprednisolone for acute spinal cord injury. Spine 31(9):E250–E253
Felleiter P, Müller N, Schumann F, Felix O, Lierz P (2012) Changes in the use of the methylprednisolone protocol for traumatic spinal cord injury in Switzerland. Spine 37(11):953–956
Hurlbert RJ, Hamilton MG (2008) Methylprednisolone for acute spinal cord injury: 5-year practice reversal. Can J Neurol Sci 35(1):41–45
Hurlbert RJ, Hadley MN, Walters BC, Aarabi B, Dhall SS, Gelb DE, Rozzelle CJ, Ryken TC, Theodore N (2013) Pharmacological therapy for acute spinal cord injury. Neurosurgery 72:93–105
Miekisiak G, Kloc W, Janusz W, Kaczmarczyk J, Latka D, Zarzycki D (2013) The use of methylprednisolone in the acute phase of spinal cord injury. The official position of the Polish Society of Spinal Surgery. J Spine Surg 5(1):11–24
Hurlbert RJ (2000) Methylprednisolone for acute spinal cord injury: an inappropriate standard of care. J Neurosurg Spine 93(1):1–7
Ito Y, Sugimoto Y, Tomioka M, Kai N, Tanaka M (2009) Does high dose methylprednisolone sodium succinate really improve neurological status in patient with acute cervical cord injury?: a prospective study about neurological recovery and early complications. Spine 34(20):2121–2124
Chikuda H, Yasunaga H, Takeshita K, Horiguchi H, Kawaguchi H, Ohe K, Fushimi K, Tanaka S (2013) Mortality and morbidity after high-dose methylprednisolone treatment in patients with acute cervical spinal cord injury: a propensity-matched analysis using a nationwide administrative database. Emerg Med J. doi:10.1136/emermed-2012-202058
Matsumoto T, Tamaki T, Kawakami M, Yoshida M, Ando M, Yamada H (2001) Early complications of high-dose methylprednisolone sodium succinate treatment in the follow-up of acute cervical spinal cord injury. Spine 26(4):426–430
Roberts I, Yates D, Sandercock P, Farrell B, Wasserberg J, Lomas G, Cottingham R, Svoboda P, Brayley N, Mazairac G (2004) Effect of intravenous corticosteroids on death within 14 days in 10008 adults with clinically significant head injury (MRC CRASH trial): randomised placebo-controlled trial. Lancet 364(9442):1321–1328
Werndle MC, Zoumprouli A, Sedgwick P, Papadopoulos MC (2012) Variability in the treatment of acute spinal cord injury in the United Kingdom: results of a national survey. J Neurotrauma 29(5):880–888
Druschel C, Schaser K-D, Schwab JM (2013) Current practice of methylprednisolone administration for acute spinal cord injury in Germany: a national survey. Spine 38(11):E669–E677
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miekisiak, G., Kloc, W., Janusz, W. et al. Current use of methylprednisolone for acute spinal cord injury in Poland: survey study. Eur J Orthop Surg Traumatol 24 (Suppl 1), 269–273 (2014). https://doi.org/10.1007/s00590-014-1422-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-014-1422-3