Abstract
Nitric oxide (NO), which is produced from nitric oxide synthase, is an important cell signaling molecule that is crucial for many physiological functions such as neuronal death, neuronal survival, synaptic plasticity, and vascular homeostasis. This diffusible gaseous compound functions as an effector or second messenger in many intercellular communications and/or cell signaling pathways. Protein S-nitrosylation is a posttranslational modification that involves the covalent attachment of an NO group to the thiol side chain of select cysteine residues on target proteins. This process is thought to be very important for the regulation of cell death, cell survival, and gene expression in the central nervous system (CNS). However, there have been few reports on the role of protein S-nitrosylation in CNS disorders. Here, we briefly review specific examples of S-nitrosylation, with particular emphasis on its functions in neuronal cell death and survival. An understanding of the role and mechanisms underlying the effects of protein S-nitrosylation on neurodegenerative/neuroprotective events may reveal a novel therapeutic strategy for rescuing neurons in neurodegenerative diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nitric oxide (NO) is a gas that is freely permeable to the cellular plasma membrane; thus, it does not need a biological receptor to affect intracellular communication and/or signal transduction mechanisms. NO has dual effects: low levels of NO that are produced under physiological conditions stimulate many normal intracellular signaling pathways, whereas high levels lead to cellular injury [1]. Several neuronal models have demonstrated the neuroprotective actions of NO. For example, in dorsal root ganglia neurons, NO protects neurons after peripheral nerve injury [2]. In a cerebellar granule cell model, serum deprivation-induced cell death was rescued by NO donors [3]. Another neuronal cell model of trophic factor deprivation in spinal cord motor neurons demonstrated that NO exerted its neuroprotective effects by regulating the cyclic guanosine monophosphate (cGMP)-dependent signaling pathway [4]. NO activated the phosphatidylinositol 3-kinase (PI3K)/Akt survival signaling pathway and promoted cell survival in a 6-hydroxydopamine (6-OHDA)-induced apoptotic neuronal model of rat pheochromocytoma PC12 cells [5]. In a previous study, we proposed that NO-activated protein kinase activity is involved in neuritogenesis [6]. Furthermore, an NO donor and cGMP analog promoted neurite outgrowth in PC12h cells, whereas an NO synthase inhibitor, NO scavenger, and cGMP-dependent protein kinase inhibitor all inhibited neuritogenic action. These results suggest that neuritogenic actions are mediated by NO-dependent cGMP signaling [7, 8]. A similar result was reported for PC12 cells, in which cell differentiation was mediated by NO-cGMP-dependent angiotensin II binding to the angiotensin II receptor [9]. In hippocampal neurons, estradiol-stimulated dendritic branching was induced by the NO-cGMP pathway [10].
In contrast, excessive NO formation has emerged as an important mediator of neurotoxicity in a variety of disorders of the nervous system. When NO is present at higher than normal physiological levels, it can initiate a neurotoxic cascade such as glutamate signaling. A well-known mechanism for NO production involves activation of N-methyl-d-aspartate (NMDA)-type glutamate receptors. In the cascade, the glutamate neurotransmitter stimulates NMDA receptors, which stimulates calcium ion (Ca2+) influx into the cell via receptor-associated ion channels, in turn activating neuronal nitric oxide synthase (NOS) to produce NO. Treatment by NOS inhibitors or removal of arginine from the medium prevented NMDA neurotoxicity in a cortical neuron culture system [11]. A quencher of NO, hemoglobin prevents NMDA-induced neuronal damage [12]. NO is more harmful under pathological conditions that involve reactive oxygen species production, such as peroxynitrite. Dysfunction and structural dysregulation of neuronal network activity are fundamental causes of neurodegenerative disorders such as Alzheimer’s disease (AD), Parkinson’s disease (PD), Huntington’s disease, and amyotrophic lateral sclerosis (ALS). A marker of nitrosative stress, nitrotyrosine formation has been reported in patients with AD and PD [13–15]. In this review, we summarize the role of NO in regulating cell survival and cell death in the central nervous system (CNS).
Role of NOS Isoforms in the CNS
NO is an organic gas that is ubiquitously synthesized by NOS. In mammalian cells, NOS is subclassified into three types: neuronal NOS (nNOS or NOSI), inducible NOS (iNOS or NOSII), and endothelial NOS (eNOS or NOSIII). The functions of NO differ depending upon the cell type and enzyme isotype. nNOS is involved in neurotransmission by creating retrograde signaling between synapses. At the synapses, nNOS is coupled to the NMDA receptor via postsynaptic density-95 protein complexes [16]. Upon glutamate stimulation of the NMDA receptor, Ca2+ enters the cytoplasm through the ion channel, where in conjuction with calmodulin, it triggers nNOS activation and NO production [17]. Low levels of NO that are produced under physiological conditions stimulate many normal intracellular signaling pathways. In contrast, overstimulation of the NMDA receptor and subsequent Ca2+ influx induce pathological signaling, resulting in neural damage and death through production of toxic levels of NO [18]. A primary activator of nitrosative stress in AD is the release of excess Ca2+ into the cytosol following the overstimulation of NMDA receptors. nNOS mediates the long-term regulation of synaptic transmission in the CNS, the central regulation of blood pressure, smooth muscle relaxation, and vasodilation via peripheral nitrergic nerves. It is also implicated in neuronal cell death in cerebrovascular stroke [19]. The latter effect may be related to NO biosynthesis by nNOS that is dependent upon the tetrahydrobiopterin cofactor, the concentration of which is gradually decreased in the caudate nucleus of PD patients [20].
iNOS, which is upregulated by acute inflammatory stimuli, is strongly implicated in the pathogenesis of neurodegenerative diseases. Pathological levels of NO via iNOS induction in activated glial cells lead to various neurodegenerative diseases. NO is further oxidized to nitrite peroxynitrite and free radicals to highly interact with thiols and the ion-sulfur center of various enzymes [21], resulting in apoptosis, neurotoxicity, neuronal degeneration, and numerous CNS disorders. Activation of iNOS requires gene transcription, and its induction can be influenced by endotoxin and cytokines such as lipopolysaccharides, interleukin (IL)-1β, IL-2, interferon-γ (IFN-γ), and tumor necrosis factor (TNF). Although the endogenous factors that induce iNOS expression in the aging brain are unknown, TNF levels in the cerebrospinal fluid and peripheral circulation, as well as IL-1β and IFN-γ levels in monocytes are increased by aging [22]. iNOS expression was induced in the hippocampal dentate gyrus of an ischemia brain model [23]. In addition, alterations in NO release were observed from neutrophils obtained from PD patients and the increased expression of iNOS was reported in 6-OHDA- and lipopolysaccharide-induced models of PD [13]. iNOS induction in astroglial cells rather than microglial cells is involved in its pathological status in AD [14] and PD [15]. Co-culture of iNOS-expressing astrocytes and neurons immediately caused damage to the neuronal respiratory chain and loss of ATP [24].
The major function of eNOS is regulation of vascular smooth muscle relaxation via a cGMP-mediated signal transduction pathway. eNOS is mostly expressed in endothelial cells, although it has also been found in cardiac monocytes, platelets, and certain neurons of the brain. Ca2+-activated calmodulin is important for the regulation of eNOS activity. eNOS produces NO in a pulsatile manner, with eNOS activity increasing when intracellular Ca2+ levels rise. It has been reported that eNOS is induced under inflammatory conditions [25]. eNOS is involved in neuronal functions such as long-term potentiation in the hippocampus and NMDA-stimulated gamma-aminobutyric acid release in various regions of the brain [26].
Protein S-Nitrosylation
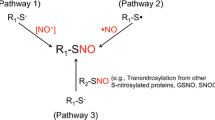
Because NO is a free gas, it can easily penetrate the biological membrane. The superoxide radical shows high affinity for NO. The reaction between NO and the superoxide anion induces the production of peroxynitrite [27], which is a highly reactive molecule that can cause extensive damage to proteins, lipids, and DNA. NO interacts with thiols, which are organosulfur compounds that contain a carbon-bonded sulfhydryl (–C–SH or R–SH) group. Several actions of NO, including neurotransmission and vasodilation, are mediated by the activation of soluble guanylate cyclase and subsequent elevation of cGMP levels [28], whereas other actions are mediated by S-nitrosylation of the free cysteine group of proteins [28]. Since Jaffery and Snyder [29] discovered the “biotin-switch assay” (Fig. 1) for protein S-nitrosylation, more than 1000 proteins have been identified as S-nitrosylation target proteins (Table 1). S-nitrosylation can mediate neuroprotective or neurotoxic effects, depending upon the action of the targets [30].
Schematic of S-nitrosylated protein detection using the “biotin-switch assay”. Step 1 Free thiols are blocked by a methylthiolation reagent. Step 2 Reduction of S-nitrosylation bonds to thiols with reductant. Step 3 Newly reformed cysteines react with biotin-conjugated thiol-modifying reagent. Step 4 Target biotinylated proteins are collected by avidin-coupled reagents
Targets of S-Nitrosylation in Modulating Cell Function and Mediating Protection in the CNS
NMDA receptors mediate Ca2+ entry into the cell to regulate physiological processes such as synaptic plasticity and memory, but overstimulation by glutamate or other agonists can cause neuronal cell death. S-nitrosylation of the redox modulatory site of the NMDA receptor resulted in downregulation of NMDA receptor activity [18]. Thus, under excitotoxic conditions, S-nitrosylation of NMDA receptors can provide neuroprotective effects. The autonomous activity of Ca2+/calmodulin-dependent protein kinase II α (CaMKIIα) mediates excitotoxic neuronal cell death during ischemia [31]. NO-induced S-nitrosylation of CaMKIIα also directly generates autonomous activity [32], which may be involved in excitotoxic neuronal cell death. Type 1 ryanodine receptor (RyR1) is the Ca2+-induced Ca2+ release channel in the endoplasmic reticulum (ER) [33]. During epileptic seizures, S-nitrosylation of RyR1 causes Ca2+ release from the ER via the RyR1, causing seizure-dependent neuronal cell death [34].
Mitogen-activated protein kinase kinase 4 (MKK4) is activated via phosphorylation and regulates cell proliferation, differentiation, survival, and migration in response to cellular stress [35]. In the ischemia/reperfusion brain, MKK4 is S-nitrosylated by endogenous NO. Inhibition of S-nitrosylation and activation of MKK4 results in decreases in NMDA receptor-mediated neuronal degeneration and apoptosis [36]. The Src homology 2 domain-containing phosphatase (SHP-2) increases neural progenitor cells and neuronal survival through activation of extracellular signal-regulated kinase 1/2 (ERK1/2) [37]. Excitotoxic injuries induce S-nitrosylation of SHP-2, resulting in increased susceptibility to NMDA receptor-mediated excitotoxicity by inhibition of ERK1/2 activation [38]. Cyclooxygenase (COX)-2 is involved in NMDA receptor-mediated neurotoxicity via the generation of prostaglandins. This neurotoxicity is due to activation of COX-2 by S-nitrosylation after selective binding of nNOS to COX-2 [39]. Peroxiredoxin 2 (Prx 2) is one of the antioxidant enzymes that are abundantly present in mammalian neurons. S-nitrosylation of this enzyme interrupts the normal redox cycle via inhibition of peroxidase activity, resulting in the accumulation of cellular peroxides and neuronal cell death [40]. In addition to Prx2, Prx1 is also nitrosylated by NO/S-nitrosylation donors [41], promoting disulfide formation on Prx1 catalytic cysteines and disrupting the oligomeric structure of Prx1, ultimately leading to loss of peroxidase activity [41].
FLICE inhibitory protein (FLIP) and Bcl-2 are key apoptosis regulatory proteins. FLIP inhibits mitochondrial-mediated apoptosis through the inhibition of caspase-8 and Fas-associated death domain binding. S-nitrosylation of FLIP and Bcl-2 suppresses their ubiquitination and proteasomal degradation, subsequently enhancing antiapoptotic activity through their stabilization [42, 43]. Proliferating cell nuclear antigen (PCNA) interacts with caspase-9 and partially blocks its activation. S-nitrosylation of PCNA did not inhibit caspase-9 activation and apoptosis in rotenone-treated SH-SY5Y neuroblastoma cells [44]. X-linked inhibitor of apoptosis (XIAP) can inhibit pro-caspase activity via ubiquitination and degradation, thereby suppressing caspase-mediated apoptosis and promoting cell survival. Under cerebral ischemia–reperfusion condition, S-nitrosylation of XIAP occurs via the thioredoxin system [45]. S-nitrosylation of XIAP inhibits its E3 ubiquitin ligase activity, and induces apoptosis [46]. DJ-1 (PARK7) acts as a neuroprotective protein via modulation of multiple cellular survival signaling pathways including the phosphatase and tensin homolog (PTEN)/PI3K/Akt cascade [47]. PTEN and Akt are nitrosylated and regulate Akt-mediated cell survival signaling [48]. Under low concentrations of NO, S-nitrosylation of PTEN leads to inhibition of its phosphatase activity and consequent Akt phosphorylation/activation, resulting in cell survival, proliferation, and growth. S-nitrosylated DJ-1 can be a source of NO group for PTEN [49]. Thus, transferring NO from DJ-1 to PTEN, results in enhanced neuroprotection. In contrast, high NO levels lead to S-nitrosylated Akt and inhibition of this neuroprotective pathway [48].
Glyceraldehyde-3-phosphate dehydrogenase (GAPDH) is generally characterized as a housekeeping glycolytic enzyme. GAPDH undergoes S-nitrosylation, which facilitates its binding to seven in absentia homolog 1 (SIAH1), an E3 ubiquitin ligase, resulting in nuclear translocation [50]. The nuclear GAPDH/SIAH1 complex augments p300/CBP-mediated acetylation of nuclear proteins, including p53, which regulates cell death [51]. GAPDH’s competitor of SIAH protein enhances life (GOSPEL) is a novel GAPDH-binding protein expressed in the cytosol [52]. It competes with SIAH1 for binding to GAPDH upon S-nitrosylation, preventing nuclear translocation of GAPDH and resulting in neuroprotection [53]. B23/nucleophosmin is a nucleolar chaperone that plays a role in cellular stress responses [54]. It binds to both SIAH1 and GAPDH, disrupting the SIAH1-GAPDH complex in the nucleus in response to nitrosative stress. S-nitrosylation of B23 enhances B23-SIAH1 binding and mediates its neuroprotective actions [55]. In addition, S-nitrosylated GAPDH may be an NO donor to B23 by transnitrosylation [55].
Protein disulfide isomerase (PDI) is an ER chaperone that is induced during ER stress, and is responsible for the formation of disulfide bonds in proteins [56]. S-nitrosylation of PDI inhibits its enzymatic and chaperone activities. The accumulation of misfolded and polyubiquitinated proteins results in persistent ER stress [57]. The three major ER stress-sensing proteins are protein kinase R-like ER kinase (PERK), inositol-requiring enzyme 1 (IRE1), and activating transcription factor 6 (ATF6). S-nitrosylation of IRE1α attenuates its ribonuclease activity, and S-nitrosylation of PERK activates its kinase activity and downstream phosphorylation/inactivation of eIF2α. These S-nitrosylated proteins disrupt unfolded protein response signals and leads to ER stress-mediated cell death [58].
NO suppresses the deacetylase activity of histone deacetylase 6 (HDAC6) by S-nitrosylation in vitro and increases acetylated α-tubulin, a major substrate for HDAC6. HDAC6 plays a crucial role in promoting aggresome formation of misfolded/ubiquitinated proteins, which are pathological features common to neurodegenerative diseases. The accumulation of misfolded proteins and subsequent cell death may be partly dependent on HDAC6 inactivation via S-nitrosylation [59].
Parkin is an E3 ubiquitin ligase involved in the ubiquitination of proteins that are important in the survival of dopamine neurons in PD. Downregulated E3 ligase activity impairs ubiquitination and degradation of substrate proteins, potentially contributing to Lewy body formation and neuronal cell injury or death. S-nitrosylation inhibits the ubiquitin E3 ligase activity of parkin and its protective functions [60].
Autophagy is a major degradation process for misfolded proteins or damaged organelles. c-Jun N-terminal kinase (JNK) and IκB kinase β (IKKβ) are involved in the regulation of autophagic processes [61, 62]. S-nitrosylation of JNK1 or IKKβ inhibits autophagosome formation due to inhibition of their kinase activities [63]. Insulin-degrading enzyme (IDE), a 110 kDa metalloendopeptidase, cleaves multiple short polypeptides including β-amyloid (Aβ) [64]. S-nitrosylation results in the complete inactivation and oligomerization of IDE, which may contribute to AD pathophysiology by decreasing Aβ degradation [65].
Antioxidative Effects of NO Through Keap1 S-Nitrosylation Signaling in the CNS
Because of their accessibility for experimental manipulations and relatively simple structure, the retina represent “approachable parts of the brain” that have long served as an important model system for studying the mechanisms of cell survival or death in the CNS. Retinal ganglion cells (RGCs), the projection neurons of the retina, integrate information from photoreceptors via several types of interneurons, although some RGCs are also intrinsically photosensitive. While a growing number of S-nitrosylaion proteins reportedly contribute to pathogenesis of brain diseases, there have been few studies on their role in retinal diseases. We investigated the role of protein S-nitrosylation by NO in RGC survival after optic nerve injury [66, 67]. Many reagents such as glyceryl trinitrate, sodium nitroprusside, and S-nitrosothiols have been reported as NO donors [68]. Recently, NO donor drugs have been designed as NO-releasing compounds such as nipradilol (Nip), which has been registered as an antiglaucoma drug. The protective actions of Nip have been shown in various neuronal cells [69] including RGCs [70]. Mizuno et al. [71] demonstrated that Nip shows protective effects through NO-dependent mechanisms; however, the detailed mechanisms underlying these protective effects are not fully understood. Some lines of evidence have indicated that NO can attenuate RGC death [72] through a NO/cGMP-dependent pathway [73]. Moreover, Tomita et al. [74] reported that the beneficial effects of Nip on RGC death was not completely negated by inhibiting protein kinase G. Furthermore, Naito [75] reported that Nip attenuates hydrogen peroxide-induced lipid peroxidation. To determine if the neuroprotective actions of Nip are mediated by antioxidative processes via a NO/cGMP- or NO/S-nitrosylation-dependent mechanism, we examined the possible role of the Kelch-like ECH-associated protein 1 (Keap1). The Keap1 and NF-E2-related factor 2 (Nrf2) pathways regulate the expression of cytoprotective genes in response to oxidative stress or electrophilic stress [76]. Keap1 is a redox-sensor system protein that allows the activation of Nrf2 by modification including oxidation, alkylation, and S-nitrosylation [77]. Once activated, Nrf2 translocates to the nucleus from the cytosol, and binds to the antioxidant responsive element of target genes, driving the expression of antioxidative heme oxygenase-1 (HO-1) (Fig. 2). The Keap1 sensor protein contains 27 cysteine residues. Interestingly, NO activates the Keap1/Nrf2 pathway by S-nitrosylation of Keap1 in colon carcinoma cells [78]. Two reactive cysteines of Keap1, Cys 273 and Cys 288, have been identified as key sites of Nrf2 translocation activity [79].
NO/S-Nitrosyation-Dependent Antioxidative Protein Induction by Nip
NO can be directly involved in the modulation of HO-1 expression. NO-releasing agents can markedly increase HO-1 mRNA and protein expression in a variety of tissues including neuronal cells [80]. The protective effects of Nip are dependent upon newly synthesized antioxidative proteins, such as HO-1. A previous study by our group showed that after 4 h of Nip treatment, HO-1 mRNA and protein expression increased in RGC-5, a retinal neural cell line [81]. HO-1 is an antioxidative protein that degrades intracellular heme to free iron, carbon monoxide, and biliverdin, which is then converted to bilirubin. Bilirubin acts as a strong endogenous reactive oxygen species scavenger and attenuates the final production of lipid peroxidation, 4-hydroxy-2-nonenal. These results indicate that the protective effect of Nip is dependent upon NO-induced HO-1 induction. In addition, a previous study showed that Nip promotes translocation of Nrf2 into the nucleus, which was inhibited by NO scavengers and an S-nitrosylation inhibitor (dithiothreitol). Translocated Nrf2 was bound to the E1 enhancer of HO-1 promoter as an antioxidative responsive element [66]. These results indicate that the Nip-mediated translocation of Nrf2 to the nucleus is dependent upon NO/S-nitrosylation.
Conclusions
In this review, we briefly summarized the role of NO as a neurotoxicant and as a neuroprotector in CNS disorders. We focused on protein S-nitrosylation, which plays an important role in both neuroprotective and neurotoxic effects and is involved in the pathogenesis of a number of neurodegenerative disorders such as AD and PD. Because there have been few reports on protein S-nitrosylation in CNS disorders, elucidating the specific targets of S-nitrosylation and understanding their regulatory mechanisms could lead to the development of therapeutic strategies and targets for the treatment of neurodegenerative diseases.
References
Hara MR, Snyder SH (2007) Cell signaling and neuronal death. Annu Rev Pharmacol Toxicol 47:117–141
Thippeswamy T, Jain RK, Mumtaz N, Morris R (2001) Inhibition of neuronal nitric oxide synthase results in neurodegenerative changes in the axotomised dorsal root ganglion neurons: evidence for a neuroprotective role of nitric oxide in vivo. Neurosci Res 40:37–44
Ciani E, Guidi S, Della Valle G, Perini G, Bartesaghi R, Contestabile A (2002) Nitric oxide protects neuroblastoma cells from apoptosis induced by serum deprivation through cAMP-response element-binding protein (CREB) activation. J Biol Chem 277:49896–49902
Estevez AG, Spear N, Thompson JA, Cornwell TL, Radi R, Barbeito L, Beckman JS (1998) Nitric oxide-dependent production of cGMP supports the survival of rat embryonic motor neurons cultured with brain-derived neurotrophic factor. J Neurosci 18:3708–3714
Ha KS, Kim KM, Kwon YG, Bai SK, Nam WD, Yoo YM, Kim PK, Chung HT, Billiar TR, Kim YM (2003) Nitric oxide prevents 6-hydroxydopamine-induced apoptosis in PC12 cells through cGMP-dependent PI3 kinase/Akt activation. FASEB J 17:1036–1047
Koriyama Y, Yasuda R, Homma K, Mawatari K, Nagashima M, Sugitani K, Matsukawa T, Kato S (2009) Nitric oxide-cGMP signaling regulates axonal elongation during optic nerve regeneration in the goldfish in vitro and in vivo. J Neurochem 110:890–901
Yamazaki M, Chiba K, Mohri T, Hatanaka H (2001) Activation of the mitogen-activated protein kinase cascade through nitric oxide synthesis as a mechanism of neuritogenic effect of genipin in PC12h cells. J Neurochem 79:45–54
Yamazaki M, Chiba K, Mohri T, Hatanaka H (2004) Cyclic GMP-dependent neurite outgrowth by genipin and nerve growth factor in PC12h cells. Eur J Pharmacol 488:35–43
Zhao Y, Biermann T, Luther C, Unger T, Culman J, Gohlke P (2003) Contribution of bradykinin and nitric oxide to AT2 receptor-mediated differentiation in PC12 W cells. J Neurochem 85:759–767
Audesirk T, Cabell L, Kern M, Audesirk G (2003) Enhancement of dendritic branching in cultured hippocampal neurons by 17β-estradiol is mediated by nitric oxide. Int J Dev Neurosci 21:225–233
Catania MV, Giuffrida R, Seminara G, Barbagallo G, Aronica E, Gorter JA, Dell’Albani P, Ravagna A, Calabrese V, Giuffrida-Stella AM (2003) Upregulation of neuronal nitric oxide synthase in in vitro stellate astrocytes and in vivo reactive astrocytes after electrically induced status epilepticus. Neurochem Res 28:607–615
Stewart VC, Heslegrave AJ, Brown GC, Clark JB, Heales SJ (2002) Nitric oxide-dependent damage to neuronal mitochondria involves the NMDA receptor. Eur J Neurosci 15:458–464
Gatto EM, Riobo NA, Carreras MC, Chernavsky A, Rubio A, Satz ML, Poderoso JJ (2000) Overexpression of neutrophil neuronal nitric oxide synthase in Parkinson’s disease. Nitric Oxide 4:534–539
Wallace MN, Geddes JG, Farquhar DA, Masson MR (1997) Nitric oxide synthase in reactive astrocytes adjacent to β-amyloid plaques. Exp Neurol 144:266–272
Hunot S, Boissiere F, Faucheux B, Brugg B, Mouatt-Prigent A, Agid Y, Hirsch EC (1996) Nitric oxide synthase and neuronal vulnerability in Parkinson’s disease. Neuroscience 72:355–363
Sattler R, Xiong Z, Lu WY, Hafner M, MacDonald JF, Tymianski M (1999) Specific coupling of NMDA receptor activation to nitric oxide neurotoxicity by PSD-95 protein. Science 284:1845–1848
Bredt DS, Hwang PM, Glatt CE, Lowenstein C, Reed RR, Snyder SH (1991) Cloned and expressed nitric oxide synthase structurally resembles cytochrome P-450 reductase. Nature 351:714–718
Lipton SA, Choi YB, Pan ZH, Lei SZ, Chen HS, Sucher NJ, Loscalzo J, Singel DJ, Stamler JS (1993) A redox-based mechanism for the neuroprotective and neurodestructive effects of nitric oxide and related nitroso-compounds. Nature 364:626–632
Forstermann U, Sessa WC (2012) Nitric oxide synthases: regulation and function. Eur Heart J 33:829–837
Kuiper MA, Visser JJ, Bergmans PL, Scheltens P, Wolters EC (1994) Decreased cerebrospinal fluid nitrate levels in Parkinson’s disease, Alzheimer’s disease and multiple system atrophy patients. J Neurol Sci 121:46–49
Chiou GC (2001) Review: effects of nitric oxide on eye diseases and their treatment. J Ocul Pharmacol Ther 17:189–198
Cannon JG (1995) Cytokines in aging and muscle homeostasis. J Gerontol A 50:120–123
Zhu DY, Liu SH, Sun HS, Lu YM (2003) Expression of inducible nitric oxide synthase after focal cerebral ischemia stimulates neurogenesis in the adult rodent dentate gyrus. J Neurosci 23:223–229
Stewart VC, Land JM, Clark JB, Heales SJ (1998) Pretreatment of astrocytes with interferon-α/β prevents neuronal mitochondrial respiratory chain damage. J Neurochem 70:432–434
Borsani E, Giovannozzi S, Cocchi MA, Boninsegna R, Rezzani R, Rodella LF (2013) Endothelial nitric oxide synthase in dorsal root ganglia during chronic inflammatory nociception. Cells Tissues Org 197:159–168
Garthwaite J (2008) Concepts of neural nitric oxide-mediated transmission. Eur J Neurosci 27:2783–2802
Beckman JS, Beckman TW, Chen J, Marshall PA, Freeman BA (1990) Apparent hydroxyl radical production by peroxynitrite: implications for endothelial injury from nitric oxide and superoxide. Proc Natl Acad Sci USA 87:1620–1624
Schmidt HH, Lohmann SM, Walter U (1993) The nitric oxide and cGMP signal transduction system: regulation and mechanism of action. Biochim Biophys Acta 1178:153–175
Jaffrey SR, Erdjument-Bromage H, Ferris CD, Tempst P, Snyder SH (2001) Protein S-nitrosylation: a physiological signal for neuronal nitric oxide. Nat Cell Biol 3:193–197
Nakamura T, Lipton SA (2011) Redox modulation by S-nitrosylation contributes to protein misfolding, mitochondrial dynamics, and neuronal synaptic damage in neurodegenerative diseases. Cell Death Differ 18:1478–1486
Coultrap SJ, Vest RS, Ashpole NM, Hudmon A, Bayer KU (2011) CaMKII in cerebral ischemia. Acta Pharmacol Sin 32:861–872
Coultrap SJ, Bayer KU (2014) Nitric oxide induces Ca2+-independent activity of the Ca2+/calmodulin-dependent protein kinase II (CaMKII). J Biol Chem 289:19458–19465
Eu JP, Sun J, Xu L, Stamler JS, Meissner G (2000) The skeletal muscle calcium release channel: coupled O2 sensor and NO signaling functions. Cell 102:499–509
Mikami Y, Kanemaru K, Okubo Y, Nakaune T, Suzuki J, Shibata K, Sugiyama H, Koyama R, Murayama T, Ito A, Yamazawa T, Ikegaya Y, Sakurai T, Saito N, Kakizawa S, Iino M (2016) Nitric oxide-induced activation of the type 1 ryanodine receptor is critical for epileptic seizure-induced neuronal cell death. EBioMedicine 11:253–261
Kundumani-Sridharan V, Subramani J, Das KC (2015) Thioredoxin activates MKK4-NFκB pathway in a redox-dependent manner to control manganese superoxide dismutase gene expression in endothelial cells. J Biol Chem 290:17505–17519
Wei XW, Hao LY, Qi SH (2016) Inhibition on the S-nitrosylation of MKK4 can protect hippocampal CA1 neurons in rat cerebral ischemia/reperfusion. Brain Res Bull 124:123–128
Shi ZQ, Yu DH, Park M, Marshall M, Feng GS (2000) Molecular mechanism for the Shp-2 tyrosine phosphatase function in promoting growth factor stimulation of Erk activity. Mol Cell Biol 20:1526–1536
Shi ZQ, Sunico CR, McKercher SR, Cui J, Feng GS, Nakamura T, Lipton SA (2013) S-nitrosylated SHP-2 contributes to NMDA receptor-mediated excitotoxicity in acute ischemic stroke. Proc Natl Acad Sci USA 110:3137–3142
Tian J, Kim SF, Hester L, Snyder SH (2008) S-nitrosylation/activation of COX-2 mediates NMDA neurotoxicity. Proc Natl Acad Sci USA 105:10537–10540
Fang J, Nakamura T, Cho DH, Gu Z, Lipton SA (2007) S-nitrosylation of peroxiredoxin 2 promotes oxidative stress-induced neuronal cell death in Parkinson’s disease. Proc Natl Acad Sci USA 104:18742–18747
Engelman R, Weisman-Shomer P, Ziv T, Xu J, Arner ES, Benhar M (2013) Multilevel regulation of 2-Cys peroxiredoxin reaction cycle by S-nitrosylation. J Biol Chem 288:11312–11324
Azad N, Vallyathan V, Wang L, Tantishaiyakul V, Stehlik C, Leonard SS, Rojanasakul Y (2006) S-nitrosylation of Bcl-2 inhibits its ubiquitin-proteasomal degradation. A novel antiapoptotic mechanism that suppresses apoptosis. J Biol Chem 281:34124–34134
Chanvorachote P, Nimmannit U, Wang L, Stehlik C, Lu B, Azad N, Rojanasakul Y (2005) Nitric oxide negatively regulates Fas CD95-induced apoptosis through inhibition of ubiquitin-proteasome-mediated degradation of FLICE inhibitory protein. J Biol Chem 280:42044–42050
Yin L, Xie Y, Yin S, Lv X, Zhang J, Gu Z, Sun H, Liu S (2015) The S-nitrosylation status of PCNA localized in cytosol impacts the apoptotic pathway in a Parkinson’s disease paradigm. PLoS ONE 10:e0117546
Zhang D, Zhao N, Ma B, Wang Y, Zhang G, Yan X, Hu S, Xu T (2016) Procaspase-9 induces its cleavage by transnitrosylating XIAP via the Thioredoxin system during cerebral ischemia-reperfusion in rats. Sci Rep 6:24203
Nakamura T, Wang L, Wong CC, Scott FL, Eckelman BP, Han X, Tzitzilonis C, Meng F, Gu Z, Holland EA, Clemente AT, Okamoto S, Salvesen GS, Riek R, Yates JR 3rd, Lipton SA (2010) Transnitrosylation of XIAP regulates caspase-dependent neuronal cell death. Mol Cell 39:184–195
Aleyasin H, Rousseaux MW, Marcogliese PC, Hewitt SJ, Irrcher I, Joselin AP, Parsanejad M, Kim RH, Rizzu P, Callaghan SM, Slack RS, Mak TW, Park DS (2010) DJ-1 protects the nigrostriatal axis from the neurotoxin MPTP by modulation of the AKT pathway. Proc Natl Acad Sci USA 107:3186–3191
Numajiri N, Takasawa K, Nishiya T, Tanaka H, Ohno K, Hayakawa W, Asada M, Matsuda H, Azumi K, Kamata H, Nakamura T, Hara H, Minami M, Lipton SA, Uehara T (2011) On-off system for PI3-kinase-Akt signaling through S-nitrosylation of phosphatase with sequence homology to tensin (PTEN). Proc Natl Acad Sci USA 108:10349–10354
Choi MS, Nakamura T, Cho SJ, Han X, Holland EA, Qu J, Petsko GA, Yates JR 3rd, Liddington RC, Lipton SA (2014) Transnitrosylation from DJ-1 to PTEN attenuates neuronal cell death in parkinson’s disease models. J Neurosci 34:15123–15131
Hara MR, Agrawal N, Kim SF, Cascio MB, Fujimuro M, Ozeki Y, Takahashi M, Cheah JH, Tankou SK, Hester LD, Ferris CD, Hayward SD, Snyder SH, Sawa A (2005) S-nitrosylated GAPDH initiates apoptotic cell death by nuclear translocation following Siah1 binding. Nat Cell Biol 7:665–674
Hara MR, Cascio MB, Sawa A (2006) GAPDH as a sensor of NO stress. Biochim Biophys Acta 1762:502–509
Tristan C, Shahani N, Sedlak TW, Sawa A (2011) The diverse functions of GAPDH: views from different subcellular compartments. Cell Signal 23:317–323
Sen N, Hara MR, Ahmad AS, Cascio MB, Kamiya A, Ehmsen JT, Agrawal N, Hester L, Dore S, Snyder SH, Sawa A (2009) GOSPEL: a neuroprotective protein that binds to GAPDH upon S-nitrosylation. Neuron 63:81–91
Colombo E, Alcalay M, Pelicci PG (2011) Nucleophosmin and its complex network: a possible therapeutic target in hematological diseases. Oncogene 30:2595–2609
Lee SB, Kim CK, Lee KH, Ahn JY (2012) S-nitrosylation of B23/nucleophosmin by GAPDH protects cells from the SIAH1-GAPDH death cascade. J Cell Biol 199:65–76
Perri ER, Thomas CJ, Parakh S, Spencer DM, Atkin JD (2015) The Unfolded Protein Response and the Role of Protein Disulfide Isomerase in Neurodegeneration. Front Cell Dev Biol 3:80
Uehara T, Nakamura T, Yao D, Shi ZQ, Gu Z, Ma Y, Masliah E, Nomura Y, Lipton SA (2006) S-nitrosylated protein-disulphide isomerase links protein misfolding to neurodegeneration. Nature 441:513–517
Nakato R, Ohkubo Y, Konishi A, Shibata M, Kaneko Y, Iwawaki T, Nakamura T, Lipton SA, Uehara T (2015) Regulation of the unfolded protein response via S-nitrosylation of sensors of endoplasmic reticulum stress. Sci Rep 5:14812
Okuda K, Ito A, Uehara T (2015) Regulation of histone deacetylase 6 activity via S-nitrosylation. Biol Pharm Bull 38:1434–1437
Chung KK, Thomas B, Li X, Pletnikova O, Troncoso JC, Marsh L, Dawson VL, Dawson TM (2004) S-nitrosylation of parkin regulates ubiquitination and compromises parkin’s protective function. Science 304:1328–1331
Criollo A, Senovilla L, Authier H, Maiuri MC, Morselli E, Vitale I, Kepp O, Tasdemir E, Galluzzi L, Shen S, Tailler M, Delahaye N, Tesniere A, De Stefano D, Younes AB, Harper F, Pierron G, Lavandero S, Zitvogel L, Israel A, Baud V, Kroemer G (2010) The IKK complex contributes to the induction of autophagy. EMBO J 29:619–631
Borsello T, Croquelois K, Hornung JP, Clarke PG (2003) N-methyl-d-aspartate-triggered neuronal death in organotypic hippocampal cultures is endocytic, autophagic and mediated by the c-Jun N-terminal kinase pathway. Eur J Neurosci 18:473–485
Sarkar S, Korolchuk VI, Renna M, Imarisio S, Fleming A, Williams A, Garcia-Arencibia M, Rose C, Luo S, Underwood BR, Kroemer G, O’Kane CJ, Rubinsztein DC (2011) Complex inhibitory effects of nitric oxide on autophagy. Mol Cell 43:19–32
Kurochkin IV, Goto S (1994) Alzheimer’s β-amyloid peptide specifically interacts with and is degraded by insulin degrading enzyme. FEBS Lett 345:33–37
Ralat LA, Ren M, Schilling AB, Tang WJ (2009) Protective role of Cys-178 against the inactivation and oligomerization of human insulin-degrading enzyme by oxidation and nitrosylation. J Biol Chem 284:34005–34018
Koriyama Y, Chiba K, Yamazaki M, Suzuki H, Muramoto K, Kato S (2010) Long-acting genipin derivative protects retinal ganglion cells from oxidative stress models in vitro and in vivo through the Nrf2/antioxidant response element signaling pathway. J Neurochem 115:79–91
Koriyama Y, Kamiya M, Takadera T, Arai K, Sugitani K, Ogai K, Kato S (2012) Protective action of nipradilol mediated through S-nitrosylation of Keap1 and HO-1 induction in retinal ganglion cells. Neurochem Int 61:1242–1253
Miller MR, Megson IL (2007) Recent developments in nitric oxide donor drugs. Br J Pharmacol 151:305–321
Taguchi R, Shirakawa H, Yamaguchi T, Kume T, Katsuki H, Akaike A (2006) Nitric oxide-mediated effect of nipradilol, an α- and β-adrenergic blocker, on glutamate neurotoxicity in rat cortical cultures. Eur J Pharmacol 535:86–94
Nakazawa T, Tomita H, Yamaguchi K, Sato Y, Shimura M, Kuwahara S, Tamai M (2002) Neuroprotective effect of nipradilol on axotomized rat retinal ganglion cells. Curr Eye Res 24:114–122
Mizuno K, Koide T, Yoshimura M, Araie M (2001) Neuroprotective effect and intraocular penetration of nipradilol, a β-blocker with nitric oxide donative action. Invest Ophthalmol Vis Sci 42:688–694
Imai N, Tsuyama Y, Murayama K, Adachi-Usami E (1997) Protective effect of nitric oxide on ischemic retina. Nippon Ganka Gakkai Zasshi 101:639–643
Ando A, Yamazaki Y, Kaneko S, Miyake M, Nambu R, Taomoto M, Unezaki S, Okuda-Ashitaka E, Okumura T, Ito S, Matsumura M (2005) Cytoprotection by nipradilol, an anti-glaucomatous agent, via down-regulation of apoptosis related gene expression and activation of NF-kappaB. Exp Eye Res 80:501–507
Tomita H, Nakazawa T, Sugano E, Abe T, Tamai M (2002) Nipradilol inhibits apoptosis by preventing the activation of caspase-3 via S-nitrosylation and the cGMP-dependent pathway. Eur J Pharmacol 452:263–268
Naito A, Aniya Y, Sakanashi M (1994) Antioxidative action of the nitrovasodilator nicorandil: inhibition of oxidative activation of liver microsomal glutathione S-transferase and lipid peroxidation. Jpn J Pharmacol 65:209–213
Baird L, Dinkova-Kostova AT (2011) The cytoprotective role of the Keap1-Nrf2 pathway. Arch Toxicol 85:241–272
Himori N, Yamamoto K, Maruyama K, Ryu M, Taguchi K, Yamamoto M, Nakazawa T (2013) Critical role of Nrf2 in oxidative stress-induced retinal ganglion cell death. J Neurochem 127:669–680
Li CQ, Kim MY, Godoy LC, Thiantanawat A, Trudel LJ, Wogan GN (2009) Nitric oxide activation of Keap1/Nrf2 signaling in human colon carcinoma cells. Proc Natl Acad Sci USA 106:14547–14551
Buckley BJ, Li S, Whorton AR (2008) Keap1 modification and nuclear accumulation in response to S-nitrosocysteine. Free Radic Biol Med 44:692–698
Calabrese V, Boyd-Kimball D, Scapagnini G, Butterfield DA (2004) Nitric oxide and cellular stress response in brain aging and neurodegenerative disorders: the role of vitagenes. In Vivo 18:245–267
Maines MD (1988) Heme oxygenase: function, multiplicity, regulatory mechanisms, and clinical applications. FASEB J 2:2557–2568
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Koriyama, Y., Furukawa, A. S-Nitrosylation Regulates Cell Survival and Death in the Central Nervous System. Neurochem Res 43, 50–58 (2018). https://doi.org/10.1007/s11064-017-2303-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-017-2303-z