Abstract
Epilepsy, a prevalent neurological disease characterized by spontaneous recurrent seizures (SRS), is often refractory to treatment with anti-seizure drugs (ASDs), so that more effective ASDs are urgently needed. For this purpose, it would be important to develop, validate, and implement new animal models of pharmacoresistant epilepsy into drug discovery. Several chronic animal models with difficult-to-treat SRS do exist; however, most of these models are not suited for drug screening, because drug testing on SRS necessitates laborious video-EEG seizure monitoring. More recently, it was proposed that, instead of monitoring SRS, chemical or electrical induction of acute seizures in epileptic rodents may be used as a surrogate for testing the efficacy of novel ASDs against refractory SRS. Indeed, several ASDs were shown to lose their efficacy on acute seizures, when such seizures were induced by pentylenetetrazole (PTZ) in epileptic rather than nonepileptic rats, whereas this was not observed when using the maximal electroshock seizure test. Subsequent studies confirmed the loss of anti-seizure efficacy of valproate against PTZ-induced seizures in epileptic mice, but several other ASDs were more potent against PTZ in epileptic than nonepileptic mice. This was also observed when using the 6-Hz model of partial seizures in epileptic mice, in which the potency of levetiracetam, in particular, was markedly increased compared to nonepileptic animals. Overall, these observations suggest that performing acute seizure tests in epileptic rodents provides valuable information on the pharmacological profile of ASDs, in particular those with mechanisms inherent to disease-induced brain alterations. However, it appears that further work is needed to define optimal approaches for acute seizure induction and generation of epileptic/drug refractory animals that would permit reliable screening of new ASDs with improved potential to provide seizure control in patients with pharmacoresistant epilepsy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Anticonvulsant Screening Program (ASP) of the U.S. National Institute of Neurological Disorders and Stroke (NINDS) focuses on the identification of promising new drug treatments for epilepsy [1–5]. The program provides opportunities for researchers from academia and industry in the U.S. and abroad to submit compounds for screening in a battery of well-established rodent seizure models. Since the inception of the ASP in 1975, these tests are performed at a contract facility based at the Department of Pharmacology at the University of Utah in Salt Lake City. Under the leadership of H. Steve White, who directed the program in Utah from 2001 to 2015, and his predecessors, the efforts of the ASP have contributed to the successful development of several new anti-seizure drugs (ASDs) for the treatment of refractory partial epilepsy [6]. The availability of these new ASDs significantly improved the therapeutic options for many patients, but overall did not change the remission rates for new-onset epilepsy nor the magnitude of ASD-resistant epilepsy [7]. Initially, the ASP was primarily based on drug testing in three rodent models, the maximal electroshock seizure (MES) test, the s.c. pentylenetetrazole (PTZ) test, and the rotarod neurotoxicity test, using normal (nonepileptic) mice and rats [1–3].
The MES and s.c. PTZ tests both belong to the disappointingly small group of validated animal models of seizures in that they have identified novel treatments that were subsequently found effective in patients [8]. In the traditional MES test, a suprathreshold 60- or 50-Hz electrical stimulus (50 mA in mice and 150 mA in rats) is applied via corneal electrodes for 0.2 s [2]. The endpoint in the MES test is tonic hindlimb extension, and the test is thought to be a predictive model for generalized tonic-clonic seizures. In addition, it was proposed that the MES test may also identify ASDs with efficacy against partial seizures [1, 2], but the lack of anti-MES activity of several ASDs (e.g., levetiracetam, tiagabine, vigabatrin) that subsequently were shown to suppress partial seizures in epilepsy patients strongly argues against this idea [9]. In the s.c. PTZ (metrazol) seizure test, PTZ is administered at a dose (~85 mg/kg) that induces clonic seizures in ~100 % of normal (nonepileptic) mice [2]. This test was thought to be useful to identify drugs that block generalized nonconvulsive (absence, myoclonic) seizures [3]. Later, the s.c. PTZ test has been abandoned as an initial screen [5], because it did not correctly predict the effect of several novel ASDs, including lamotrigine and levetiracetam, to suppress absence seizures and resulted in false positive data (e.g., tiagabine, vigabatrin) for other ASDs.
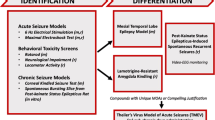
When carried out in normal (nonepileptic) mice or rats, both the MES and PTZ tests are obviously not suited to predict efficacy of novel compounds against pharmacoresistant partial seizures [7]. Therefore, prompted by Steve White, additional animal models of partial seizures, such as the mouse 6-Hz test of ASD-resistant partial seizures, mouse corneal kindling, and the lamotrigine-resistant kindled rat model of partial seizures were added to the ASP [5, 10]. The ASP (which was recently renamed as “Epilepsy Therapy Screening Program” [ETSP]) and others now routinely employ the 6-Hz test for screening due to the relative insensitivity of this test to several major ASDs, such as phenytoin and lamotrigine [5]. However, more recent analyses of numerous drug data obtained by this model have indicated that it is not strictly suited for discovering more effective ASDs for patients with as yet pharmacoresistant partial seizures but rather may be more useful for differentiation of novel compounds [8]. Thus, in view of the fact that approximately 30 % of patients have epilepsy that remains refractory to current ASDs [5, 7], there is an urgent need for simple models of pharmacoresistant seizures that are suitable for screening large numbers of compounds for discovery of more effective drugs.
Traditionally, the MES, PTZ and 6-Hz seizure models have been performed in normal healthy (naive) rodents that do not exhibit any of the brain alterations that are found in chronic epilepsy and are likely involved in the mechanisms leading to intractable seizures [7, 9]. In a landmark paper, Blanco et al. [11] suggested in 2009 that the acute induction of MES and PTZ seizures in epileptic rats might yield a distinct screening profile for ASDs, potentially identifying ASDs with new pharmacologic profiles. This idea stimulated other groups to compare ASD efficacy in acute seizure models in epileptic vs. nonepileptic mice to further explore the suggestion of Blanco et al. [11]. In this review, the data from these studies will be critically appraised with the purpose of discussing if this provides a new paradigm for screening of new treatments for pharmacoresistant epilepsy.
Acute Induction of MES and PTZ Seizures in Pilocarpine-Induced Epileptic Rats
The pilocarpine model, in which spontaneous recurrent seizures (SRS) develop following induction of a prolonged status epilepticus (SE), is one of the most widely used models of temporal lobe epilepsy (TLE), a common and severe form of epilepsy which is often difficult-to-treat with ASDs [12–14]. SRSs in this model respond only to high, partially toxic doses of ASDs [15] and many of the rats are pharmacoresistant at tolerable doses of ASDs [16, 17]. In this respect, it is important to consider that pharmacoresistance in animal models has been minimally defined as persistent seizure activity that does not respond to monotherapy at tolerable doses with at least two current ASDs [18]. Thus, an anti-seizure effect of a drug at a toxic dose, as with several ASDs in the study of Leite and Cavalheiro [15], is without relevance in terms of prediction of clinical efficacy. Resistance to ASDs has also been reported for another post-SE model of TLE, in which SE is induced by sustained electrical stimulation of the basolateral amygdala [19, 20]. In this model, ASD responders and nonresponders have been compared in the search for mechanisms of pharmacoresistance [9]. A variety of possible mechanisms were discovered in nonresponders, including severe hippocampal damage, overexpression of the brain efflux transporter P-glycoprotein, and alterations in ASD targets such as the GABAA receptor [9].
The inherent problem of the pilocarpine and most other post-SE models of TLE is that SRS occur infrequently and with considerable inter-individual variation, so that prolonged continuous (24/7) video-EEG monitoring is needed for determining drug efficacies [9]. Thus, such models are not suited for drug screening. Blanco et al. [11] had the original idea that using acute seizure tests such as the MES and PTZ tests in pilocarpine-induced epileptic rats might yield a distinct screening profile for ASDs, because the brain alterations underlying epilepsy may also affect the pharmacological responsiveness of induced acute seizures in such rats. The strategy that they used is illustrated in Fig. 1a. SE was induced by pilocarpine in groups of adult male Wistar rats and suppressed after 90 min by thiopental to reduce mortality. Sham (saline) controls received all treatments except for pilocarpine. 30 days after SE, maximal electroshock (60-Hz, 100 mA for 0.25 s via transauricular electrodes) and PTZ (50 mg/kg s.c.) were used to induce acute seizures. As shown in Fig. 1b, the three ASDs used in this study (valproate, 400 mg/kg p.o.; phenobarbital, 40 mg/kg p.o., and phenytoin, 50 mg/kg p.o.) significantly suppressed tonic MES without any difference between sham controls and epileptic rats. In contrast, a marked difference between sham control and epileptic rats was found in the PTZ seizure test (Fig. 1c) in that the three ASDs suppressed clonic seizures in controls but not in epileptic rats. Thus, clonic PTZ seizures became resistant to these three ASDs when induced on an epileptic background, so that the PTZ model became a surrogate model for ASD-resistant seizures in epileptic rats. Interestingly, when pilocarpine-treated rats without successful SE induction were used as a third (nonepileptic) group, a significantly reduced anti-seizure effect of valproate and phenytoin (but not phenobarbital) was observed in comparison to sham control animals, indicating that the brain alterations induced by pilocarpine affected the efficacy of ASDs even in the absence of SE or SRS [11]. An additional observation was that animals of the SE and non-SE pilocarpine groups pretreated with vehicle (i.e., saline) alone exhibited significantly more severe seizure types after PTZ injection than sham controls [11].
Effect of the anti-seizure drugs (ASDs) valproate (VPA), phenobarbital (PB) and phenytoin (PHT) on acute seizures in nonepileptic (sham control) vs. epileptic rats as reported by Blanco et al. [11]. a Illustrates the experimental protocol used. Epilepsy was induced by pilocarpine-mediated status epilepticus (SE); for acute seizures either the maximal electroshock seizure (MES) or the s.c. pentylenetetrazole (PTZ) seizure test were used 30 days after SE induced by pilocarpine. In rats with SE, spontaneous seizures were verified by video monitoring over 1 week. b Shows the effect of fixed doses of the three ASDs (doses indicated in mg/kg p.o. in brackets below the columns) on the incidence of MES in groups of rats. Significant differences to saline-treated rats are indicated by asterisks (P < 0.05); “0” indicates that tonic seizures were completely suppressed in all rats. No difference in ASD efficacy between nonepileptic sham controls and epileptic rats was observed, but all ASDs significantly suppressed MES. c Shows the effect of fixed doses of the three ASDs on the incidence of clonic PTZ seizures in groups of rats. Significant differences to saline-treated rats are indicated by asterisks (P < 0.05); “0” indicates that clonic seizures were completely suppressed in all rats. The anti-seizure effect of the 3 ASDs observed in nonepileptic sham controls was completely lost in epileptic rats, resulting in a significant difference between sham controls and epileptic rats, which is indicated by the hatch sign (P < 0.05)
The difference between MES and PTZ reported by Blanco et al. [11] shows that the lower efficacy of ASDs in epileptic animals is not necessarily universal but can be dependent on the model, which at first sight seems to detract from the value of the observation. Furthermore, the observation in both SE and non-SE pilocarpine animals may suggest that pharmacokinetic factors (such as overexpression of drug efflux transporters at the blood–brain barrier) may be involved, which was not studied.
One unexpected finding of the study of Blanco et al. [11] was that phenytoin suppressed clonic PTZ seizures in naive rats. Phenytoin and other ASDs that act via modulation of voltage-dependent sodium channels are typically not effective in the PTZ model [21]. For instance, in the ASP, oral administration of phenytoin was found to suppress MES in rats with a median effective dose (ED50) of 30 mg/kg, whereas phenytoin was not effective in the s.c. PTZ seizure test [3]. Thus, it is difficult to understand how phenytoin could suppress PTZ-induced seizures in the study of Blanco et al. [11]. Furthermore, the predictive value of ASD effects in the PTZ model is generally considered quite limited [9], so that it would be advantageous if the findings of Blanco et al. [11] could be translated to more relevant acute seizure tests, such as the 6-Hz test. It is also interesting to note that the current intensity (100 mA) used in the rat MES test and the PTZ dose (50 mg/kg s.c.) used in the PTZ seizure test were lower than commonly used in these tests [22], which may have affected ASD efficacy, particularly because dose-response relationships were not explored. Moreover, the study of Blanco et al. [11] was limited to three old ASDs (phenobarbital, phenytoin, valproate), so that it was important to evaluate whether the resistance of PTZ seizures to ASDs in epileptic rodents extends to other, more recent ASDs.
Acute Induction of MES and PTZ Seizures in Epileptic Mice of the Pilocarpine Model
The interesting findings of Blanco et al. [11] prompted several subsequent studies that explored whether these findings could be translated to mice, which are typically used for screening in drug discovery programs [5]. In one of these studies [23], we used timed i.v. infusion of PTZ for determining the PTZ seizure threshold rather than injecting one fixed dose of PTZ as in the study of Blanco et al. [11]. The protocol of our mouse study is shown in Fig. 2a. Mice were made epileptic by pilocarpine-induced SE and then used for determining the effects of 5 ASDs (phenobarbital, valproate, lamotrigine, diazepam, and levetiracetam) on the PTZ seizure threshold, starting 6 weeks after SE. Sham controls were used for comparison. As shown in Fig. 2b, in contrast to the study of Blanco et al. [11] in rats, phenobarbital was not less effective against PTZ seizures in epileptic vs. control mice, but even tended to be more effective in one of the two experiments performed with phenobarbital in mice. The same was observed for diazepam, levetiracetam, and lamotrigine (Fig. 2b). However, as in the experiments of Blanco et al. [11] in rats, valproate proved to be less effective in epileptic vs. nonepileptic mice (Fig. 2b). This was observed at i.p. doses of 200 and 300 mg/kg, whereas the difference was lost at 400 mg/kg. In some of the experiments in epileptic mice, seizure threshold was lower and seizure severity at threshold was higher than in sham controls [23] as previously reported [24]. Overall, the mouse experiments illustrated in Fig. 2 indicate that induction of acute seizures with PTZ in epileptic mice of the pilocarpine model does not provide an effective and valuable surrogate method to screen drugs for anti-seizure efficacy in a model of difficult-to-treat chronic epilepsy as previously suggested from experiments with this approach in rats [11]. Among the 5 ASDs examined in the mouse experiments, only valproate was less effective at increasing PTZ seizure threshold in epileptic vs. nonepileptic mice and this difference in efficacy was restricted to a dose range of 200–300 mg/kg. Although the approach of Blanco et al. [11] reported for the pilocarpine model in rats is interesting, it obviously does not translate to the pilocarpine model in mice, possibly indicating inter-species differences in this model. Furthermore, it is not known whether the observations of Blanco et al. [11] with phenobarbital, phenytoin and valproate would extend to other ASDs with their approach. In any event, it would be important to prove whether the findings reported by Blanco et al. [11] can be replicated by another laboratory.
Effect of the anti-seizure drugs (ASDs) phenobarbital (PB), diazepam (DZP), levetiracetam (LEV), lamotrigine (LTG) and valproate (VPA) on acute seizures in nonepileptic (sham control) vs. epileptic mice as reported by Töllner et al. [23]. a Illustrates the experimental protocol used. Epilepsy was induced by pilocarpine-mediated status epilepticus (SE). For induction of acute seizures, the threshold to myoclonic seizures induced by timed i.v. infusion of pentylenetetrazole (PTZ) was determined, starting 6 weeks after SE induced by pilocarpine. b Shows the effect of fixed doses of the 5 ASDs (doses indicated in mg/kg i.p. in brackets below the columns) on the threshold for PTZ seizures in percent above control threshold. The experiments with PB and VPA were performed twice in separate groups of mice. Significant differences to saline-treated mice are indicated by asterisks (P < 0.05). Significant differences between sham control and epileptic mice are indicated by the hatch sign (P < 0.05). A reduced anti-seizure effect in epileptic mice was only observed for VPA and was restricted to 200 and 300 mg/kg of this ASD
In another study, we used the MES threshold (MEST) as an acute seizure model in epileptic and nonepileptic mice [25]. The experimental protocol was similar to that illustrated in Fig. 2a. As reported previously [24], the control MEST did not differ between nonepileptic and epileptic mice. Phenobarbital (10 mg/kg i.p.) induced a similar MEST increase in both groups of mice (Fig. 3a), which would confirm the study of Blanco et al. [11] with the MES test in rats. In our study, we were interested to evaluate whether the brain alterations induced in the pilocarpine model increase the efficacy of drugs such as bumetanide that act by inhibiting the chloride influx transporter NKCC1 (SLC12A2), the principal transport mechanism responsible for Cl− uptake and for the depolarizing GABAA receptor responses of immature neurons and hippocampal neurons in adult patients with pharmacoresistant TLE [26]. In the adult brain, neuronal NKCC1 expression is low, but expression significantly increases after pilocarpine-induced SE in mice [27]. Bumetanide has been reported to increase the anti-seizure efficacy of phenobarbital in chronic models of neonatal and adult seizures [28, 29], so we hypothesized that this may translate to an increased effect of the bumetanide/phenobarbital combination on MEST in epileptic mice [25]. Bumetanide only poorly penetrates into the brain [30], so we also evaluated the effects of a lipophilic prodrug of bumetanide, BUM5 (the N,N-dimethylaminoethylester of bumetanide), which has been shown to lead to significantly higher bumetanide brain levels than the parent drug [29]. As shown in Fig. 3a, the effect of phenobarbital on MEST was not potentiated by bumetanide in either nonepileptic or epileptic mice, whereas BUM5 caused a marked potentiation in epileptic animals, which was not observed in sham controls. BUM5 alone was not effective (not illustrated). When the experiment with BUM5 and phenobarbital was repeated in another group of epileptic mice 14 weeks after SE, the effect became even more marked (Fig. 3a).
Effect of phenobarbital (PB) or combinations of PB and either bumetanide (BUM) or its prodrug BUM5 on acute seizures in nonepileptic (sham control) vs. epileptic mice as reported by Erker et al. [25] (a) or from unpublished experiments of K. Töllner, F. Twele and W. Löscher (b). The experimental protocol was similar to that illustrated in Fig. 2a. a Shows the effect of fixed doses of PB alone or in combination with BUM or BUM5 (i.v. doses indicated in mg/kg in brackets below the columns) on the threshold for maximal electroshock seizures (MES) in percent above control threshold. Significant differences to saline-treated mice are indicated by asterisks (P < 0.05). Differences between sham control and epileptic mice are indicated by the hatch sign (P < 0.05). The experiment with PB and BUM5 was repeated once in mice 14 weeks after SE. BUM5, but not BUM, significantly increased the anti-seizure efficacy of PB and this was only observed in epileptic mice. b Shows the effect of fixed doses of PB alone or in combination with BUM or BUM5 on the threshold for pentylenetetrazole (PTZ) seizures (determined by timed i.v. infusion of PTZ) in percent above control threshold. Significant differences to saline-treated mice are indicated by asterisks (P < 0.05). Neither BUM nor BUM5 potentiated PB in epileptic or nonepileptic mice in this acute seizure model, demonstrating a marked difference to the experiments with MES threshold illustrated in (a)
This prompted us to also determine the effect of these combinations on the PTZ seizure threshold in epileptic vs. nonepileptic mice (Fig. 3b). In contrast to the observations with MEST, combining BUM5 with phenobarbital did not potentiate the effect of phenobarbital on PTZ seizure threshold in epileptic mice (Fig. 3b). Epileptic mice exhibited a tendency for more marked drug effects, but the differences from naive animals were not statistically significant.
These data demonstrate that the pharmacology of drugs may strikingly change in epileptic rodents, but that the direction of the changes depends on the mechanism of action of the compounds being tested. Thus, the translational value of drug effects against acute seizures in epileptic rodents may be significantly higher than respective effects in nonepileptic mice or rats, particularly for drugs with mechanisms inherent to disease-induced brain alterations. However, this hypothesis needs to be further explored.
Similar findings were previously reported for drug adverse effects. Again depending on the mechanism of action of a given drug, the adverse effect potential in epileptic or kindled rodents was more predictive for specific adverse effects in patients with pharmacoresistant epilepsy than adverse effects determined in nonepileptic animals [31–35].
Acute Induction of 6-Hz Seizures in Epileptic Mice of the Pilocarpine Model
The 6-Hz test in mice was first described more than 60 years ago by Toman [36] and designated as the “psychomotor seizure test”. In this test, electrical stimulation with low-frequency (6-Hz) rectangular pulses of 0.2-msec duration delivered through corneal electrodes for 3 s induces seizures that are reminiscent of “psychomotor seizures” (i.e., complex-partial seizures) occurring in human partial epilepsy such as TLE. Brown et al. [37] reported that 6-Hz seizures are resistant to phenytoin, which was considered to be inconsistent with the clinical efficacy of phenytoin in the treatment of psychomotor seizures, so the 6-Hz test was subsequently abandoned. 50 years later, the group of Steve White [38] re-evaluated the utility of the 6-Hz model as a potential screen for therapy-resistant epilepsy. While the test did not discriminate between clinical classes of ASDs when used at the convulsant current inducing seizures in 97 % of the mice (CC97; 22 mA), increasing the current intensity by 50 % (i.e., 32 mA) decreased the sensitivity of the 6-Hz seizures to phenytoin and lamotrigine. At a current intensity of 2 × CC97 (i.e. 44 mA), only two ASDs, levetiracetam and valproate, displayed complete protection against 6-Hz seizures in nonepileptic CF-1 mice, although the efficacy of these drugs was markedly reduced when compared to lower stimulation intensities [38]. Based on these observations, Barton et al. [38] suggested that 6-Hz stimulation may provide a useful model of therapy-resistant limbic seizures. However, as noted above, more recent studies have cast doubt on the value of the 6-Hz test as a model of drug-refractory partial seizures. Several clinically established and investigational ASDs, including phenobarbital, retigabine, brivaracetam, and carisbamate, potently suppress 6-Hz seizures induced by 44 mA, but there is no clinical evidence that these drugs possess superior efficacy in patients with drug-refractory partial seizures [9]. The high-current (i.e., 44 mA) 6-Hz model seems to be predominantly resistant to sodium channel modulators such as phenytoin and lamotrigine, whereas drugs with other mechanisms, particularly GABAergic compounds, remain quite effective. Thus, this test is probably not a model of drug-refractory seizures, but may help to discriminate drugs on the basis of mechanism of action during development. In this respect, it is important to note that the strain of mice also strongly influences the treatment response in this model [39].
Based on the observations of Blanco et al. [11] with the MES and PTZ seizure tests in epileptic rats, we evaluated whether performing the 6-Hz test in epileptic mice renders this test more resistant to ASDs [24]. The protocol that we used was similar to that illustrated in Fig. 2a except that the 6-Hz experiments were started 5 months after a pilocarpine-induced SE, i.e., at a time where all mice had progressed to chronic epilepsy with SRS. As in all other experiments in epileptic mice by our group discussed here, female NMRI mice were used. Compared to sham controls, the sensitivity of mice to induction of seizures by 6-Hz stimulation was significantly increased in epileptic mice [24]. However, unexpectedly, the anti-seizure efficacy of phenobarbital in the 6-Hz test was not significantly altered in epileptic mice, irrespective of whether 32 or 44 mA was used for seizure induction (Fig. 4a). Furthermore, we observed a striking increase in the anti-seizure efficacy of levetiracetam in the 6-Hz test in epileptic animals, in that the ED50 decreased from 17.6 mg/kg in controls to 1.5 mg/kg in epileptic mice, i.e., a 12-fold increase in efficacy (Fig. 4a).
Effect of anti-seizure drugs (ASDs) on acute 6-Hz partial seizures in nonepileptic (sham control) vs. epileptic mice as reported by Bankstahl et al. [24] (a) and Leclercq and Kaminski [40] (b). The experimental protocol was similar to that illustrated in Fig. 2a except that experiments started 5 months after pilocarpine-induced SE in (a), 2 weeks in (b), and 8 weeks in (c). Anti-seizure ED50s (median effective doses in mg/kg i.p.) were determined in the 6-Hz test in either epileptic or nonepileptic mice by dose-effect experiments for phenobarbital (PB), levetiracetam (LEV), phenytoin (PHT), carbamazepine (CBZ), diazepam (DZP) and perampanel (PRP). If no ED50 could be determined, the highest dose tested is shown. Significant differences in ED50s between epileptic and nonepileptic mice is indicated by the hatch sign (P < 0.05). Of the ASDs tested, LEV exhibited the most marked difference in anti-seizure potency between epileptic and nonepileptic mice, demonstrating that epilepsy strikingly increased the potency of LEV
In a subsequent study by Leclercq and Kaminski [40] in male NMRI mice, the 6-Hz test (with 44 mA) was performed either 2 or 8 weeks after pilocarpine-induced SE, i.e., earlier than in our study in which experiments were started 5 months after SE. As shown in Fig. 4b, c, Leclercq and Kaminski [40] confirmed our finding that the anti-seizure efficacy of levetiracetam in the 6-Hz test is increased in epileptic mice. At 2 weeks post-SE, a 22-fold increase in efficacy of levetiracetam was found in post-SE vs. sham control mice (Fig. 4b), while the difference was less marked after 8 weeks (Fig. 4c). In addition to levetiracetam, the anti-seizure efficacy of diazepam in the 6-Hz test was also increased in epileptic mice. In contrast, the efficacy of carbamazepine and phenytoin was lower in epileptic than nonepileptic mice, while the efficacy of perampanel (PRL) did not change (Fig. 4b, c). Thus, again the mechanism of action of a given drug determined whether pre-existing epilepsy enhanced, decreased or did not alter its anti-seizure efficacy in the acute seizure test. Both groups that independently found the striking increase in efficacy of levetiracetam in the 6-Hz model in epileptic mice suggested that this increased efficacy is most likely due to an altered expression or functionality of its main molecular target, the synaptic vesicle protein 2A (SV2A) [24, 40].
Interestingly, in the experiments of Leclercq and Kaminski [40], naive mice exhibited a higher sensitivity to anti-seizure effects of ASDs in the 6-Hz test than sham controls, which was particularly striking for levetiracetam (ED50 59 mg/kg in naive vs. 403 mg/kg in sham treated mice). The authors attributed this difference to the fact that naive mice were group-housed whereas sham controls (and pilocarpine mice) were single-housed, which is known to be associated with enhanced stress and anxiety, both of which have been reported to influence seizure susceptibility and ASD efficacy [14, 41–43].
Is Acute Seizure Induction in Rats or Mice Made Epileptic by Pilocarpine a Viable Approach for Drug Screening?
So far, the reviewed studies all used the pilocarpine model in rodents and seizure induction by MES, PTZ (or their threshold variants), or 6-Hz stimulation. Several findings were inconsistent among studies. The most striking outcome was the increased efficacy of levetiracetam (SV2A) and BUM5 (NKCC1) combined with phenobarbital, indicating that the targets for these drugs are altered in epileptic rodents. However, one may argue that it is hard to see how this supports acute testing in pilocarpine animals as a reliable screening approach for identification of ASDs with superior efficacy against drug refractory epilepsy. Thus, additional studies on this approach are needed. Some important aspects that need to be explored are discussed in the following.
-
1.
While the pilocarpine model per se is possibly not a model of drug refractory epilepsy—besides the finding that some animals are drug refractory—it may induce brain alterations of potential pathophysiological relevance in epilepsy patients, enabling it to reveal new and novel mechanisms of action (e.g., NKCC1 and SV2A) of relevance for treatment of chronic epilepsy. This needs to be further explored.
-
2.
All available studies used the pilocarpine model. What happens if SE is induced by other means, such as for instance intrahippocampal injection of kainate that seems to induce a more drug refractory condition [44–46]? Would that enable acute testing in these animals to identify ASDs with potential for drug resistant epilepsy? This important question needs to be evaluated.
-
3.
It is not yet clear which seizure test (MES, PTZ, 6-Hz or other) is best suited to use for acute testing in epileptic animals.
-
4.
In most of the experimental studies there was no attempt to determine whether the difference in anti-seizure or adverse effects of drugs between epileptic and nonepileptic rodents reflected a purely pharmacodynamic phenomenon, e.g., due to alterations in drug targets, or whether pharmacokinetic factors also contributed to the different responsiveness to ASDs, e.g., due to seizure-induced impairment of blood–brain barrier integrity or overexpression of efflux transporters such as P-glycoprotein.
-
5.
Alternative, non-chemical approaches to induction of epilepsy need to be explored such as kindling or use of mutant rodents with genetic forms of epilepsy.
Is Assessment of Seizure Threshold Critical in Studies Comparing Differences in Response to Anti-seizure Drugs Between Naïve and Epileptic Animals After Acute Seizure Challenge?
At least in part, the differences between the findings of Blanco et al. [11] and our studies could be due to the fact that fixed, supramaximal (supra-threshold) convulsive stimuli were used in the MES and PTZ models in the experiments of Blanco et al. [11], whereas we determined ASD effects on seizure thresholds [23, 25]. In seizure threshold models, such as the timed i.v. PTZ infusion test or the MEST test, the effect of a drug on seizure threshold of an individual animal (or group of animals) is determined instead of using a fixed electrical or chemical seizure stimulus that ignores individual differences of animals in terms of seizure susceptibility [22]. As a consequence, seizure threshold tests are much more sensitive to identify anti-seizure drug activity (or differences in anti-seizure drug activity between naïve and epileptic animals) than tests with fixed convulsive stimuli [22]. By comparing drug effects in threshold and (supra) maximal models it can be differentiated if anti-seizure activity of a compound results from the elevation of seizure threshold or from other mechanisms, such as reduction of seizure spread. In addition, determination of seizure thresholds is useful to assess altered seizure susceptibility as a consequence of epileptogenesis in models such as the pilocarpine model [8]. Furthermore, threshold tests allow detection of proconvulsant effects of a given drug [22]. Thus we recommend using seizure threshold models in studies comparing differences in response to ASDs between naïve and epileptic animals after acute seizure challenge.
Translation of Findings with Acute Seizure Induction in Epileptic Rodents to Non-human Primates
Recently, Mello and colleagues tried to translate their findings with PTZ in pilocarpine rats [11] to a non-human primate model [47]. In adult marmosets, SE was induced by pilocarpine as previously described [48]. 3 months after SE, acute seizures were induced by PTZ (40 mg/kg i.p.). The effects of phenobarbital (40 mg/kg p.o.), valproate (400 mg/kg p.o.), and carbamazepine (150 mg/kg p.o.) on PTZ seizures were compared in epileptic and nonepileptic marmosets. While phenobarbital exhibited the same anti-seizure efficacy in both groups, which would be consistent with our findings in pilocarpine mice (Fig. 2b) [23], the effects of valproate and carbamazepine were less pronounced in epileptic than nonepileptic animals [47]. The authors proposed that induction of PTZ seizures in marmosets made chronically epileptic by pilocarpine-induced SE might constitute a novel approach for investigating new ASDs, and that this approach in a non-human primate model might have a higher translational value than rodent models. Given the fact that only three old ASDs were studied, this proposal appears a bit premature. Furthermore, as with phenytoin in the rat study of Blanco et al. [11], it is surprising that carbamazepine exerted any anti-seizure effect on seizures induced by PTZ in marmosets. Clonic PTZ seizures are generally not sensitive to suppression by ASDs such as phenytoin and carbamazepine that act by modulating voltage-dependent sodium channels [3, 8, 49], and it would be astonishing if this was different in marmosets. Furthermore, the dose (150 mg/kg) of carbamazepine chosen for these experiments is huge and presumably associated with adverse effects that could conceal the expression of seizures. Nevertheless, the approach of using epileptic marmosets as a model for acute seizure testing is of great interest and could offer an advantage in the preclinical evaluation of new ASDs.
Acute Seizure Induction as a Pharmacological Tool in Other Chronic Models of Epilepsy
Kainate Model
Two interesting studies from Czuczwar et al. [50, 51] examined whether hippocampal lesions induced by intracerebroventricular injection of kainate (0.1 or 0.2 µg) in mice alter the anti-seizure effects of several ASDs in the MES and PTZ seizure models. When drugs were tested 5 days after kainate injection, the anti-seizure effects of diazepam and phenobarbital were significantly reduced in both seizure tests in kainate-lesioned mice when compared to naive mice [50, 51]. In contrast, such difference was not observed with trimethadione, valproate, carbamazepine, phenytoin, and acetazolamide. The authors suggested that the mechanisms of action of diazepam and phenobarbital are partially dependent on the intact functions of the hippocampal formation [50, 51], which would be consistent with the target and network hypotheses of pharmacoresistant epilepsy [35]. The studies of Czuczwar et al. [50, 51] in the early 1980s are conceptually similar to the study of Blanco et al. [11] and are, to my knowledge, the first to demonstrate that the efficacy of several ASDs in MES/PTZ models is altered in a chronic model of epilepsy, although ASD testing was performed during the latent period before epilepsy develops in the kainate model.
Kindling
Probably the oldest use of acute seizure induction for drug testing in a chronic model of epilepsy is the amygdala kindling model of TLE in rats. The term “kindling” refers to a phenomenon in which periodic focal administration of initially subconvulsive electrical stimulations to a brain structure (such as amygdala or hippocampus) eventually results in intense limbic (partial) and secondarily generalized convulsive seizures [52]. Once established, this enhanced sensitivity to electrical stimulation is permanent and the rats are termed “fully kindled”. In the intracranial EEG, kindling is characterized by electrographic seizures or “afterdischarges” localized initially to the stimulated structure, but becoming longer and more widespread during subsequent stimulations [53]. Furthermore, the afterdischarge threshold (ADT) significantly declines during kindling acquisition, illustrating the enhanced susceptibility to stimulation. Numerous neurochemical, neurophysiological and molecular studies have shown similarities between alterations occurring in the kindled brain and brains from patients with TLE [53], although kindling possibly reflects only one component of the complex epileptogenic mechanisms that lead to SRS.
The anti-seizure efficacy of ASDs in fully kindled rats can be determined either by using a fixed suprathreshold current (e.g. 400 or 500 µA) stimulation of the amygdala after drug treatment or by determining the drug’s effect on the ADT [53, 54]. Löscher et al. [55] were the first to report that anticonvulsant efficacy of various ASDs is significantly lower in fully kindled rats compared to the MES test in naive rats, so that amygdala kindling was proposed as a model of pharmacoresistant TLE. There was, however, one exception. In 1993, Löscher and Hönack [56] reported that levetiracetam is ineffective at suppressing seizures in the traditional MES (using stimuli of 150 mA in rats and 50 mA in mice) and s.c. PTZ (80 mg/kg s.c. in mice and 90 mg/kg s.c. in rats) seizure tests in naive rats and mice, but has potent anti-seizure activity in amygdala kindled rats. As shown in Fig. 5, only a moderate anti-seizure effect of levetiracetam was seen in naive rats when determining the effect of levetiracetam on the threshold for MES, but a much more pronounced effect was observed when determining the thresholds for focal (ADT) or secondarily generalized seizures (GST) in amygdala kindled rats. This finding led to a paradigm shift in ASD development, because novel drugs that were ineffective in both MES and PTZ tests should, in theory, never have been pursued as an ASD candidate [57]. Subsequent studies showed that levetiracetam induces potent and complete seizure suppression in all animals possessing a chronic epileptic condition, including kindled mice and rats and rodents with different types of genetic epilepsies [58]. Levetiracetam thereby contrasted with all other ASDs known at the time by possessing a more selective action in epileptic animals. This observation challenged decades of conventional wisdom in ASD discovery and resulted in a revision of the screening models employed both by the NINDS-sponsored ASP program and the pharmaceutical industry [57]. The more recent findings with levetiracetam in the 6-Hz model in epileptic mice described above are thus in line with these earlier observations with this drug in epileptic or kindled rodents. Amygdala kindling is one of the few validated animal models of seizures, because it helped to identify the unique profile of levetiracetam, which subsequently translated to clinical efficacy in patients with TLE [57]. Furthermore, the efficacy of all modern ASDs against difficult-to-treat partial seizures was correctly predicted by this model [9, 59].
Effect of levetiracetam (LEV) on the threshold for maximal electroshock seizures (MEST) in naive rats vs. the threshold for EEG afterdischarges (ADT) and secondarily generalized seizures (GST) in amygdala kindled rats. LEV was administered 1 h before threshold induction; doses of LEV are indicated below the columns. Significant difference to vehicle control threshold is indicated by asterisk (P < 0.05), whereas significant difference between the effect of LEV on seizure thresholds in kindled vs. naive rats is indicated by the hash sign (P < 0.05). Data are from Löscher and Hönack [56] and unpublished experiments of H. Potschka and W. Löscher; “n.t.” indicates “not tested”. Note the huge differences in anti-seizure efficacy of LEV between kindled and naive rats. Even at the highest dose (108 mg/kg i.p.), the effect of LEV on MEST in naive rats was far below the effect on ADT and GST seen at 54 mg/kg LEV in fully kindled rats, demonstrating that kindling strikingly increased the anti-seizure efficacy of LEV. The opposite effect (lower effect in kindled vs. MES in naive rats) was obtained for several other anti-seizure drugs [55], indicating that the enhanced effect of LEV in kindled rats was a specific phenomenon for this drug, most likely as a result of altered expression or functionality of its target SV2A. It would, of course, be interesting to evaluate whether kindling also changes the anti-seizure efficacy of LEV on MEST by comparing its effect on MEST in kindled vs. nonkindled rats
However, the traditional kindling model with once daily electrical stimulation via a depth electrode is technically demanding and laborious and thus not suited for screening but rather for further differentiation of compounds that have been discovered by simpler models [9]. Corneal kindling in mice is an alternative and may be suited as a model of difficult-to-treat seizures, particularly if 6-Hz stimuli are used [60–64]. Indeed, corneal kindling would be another example of using acute induction of seizures in animals with chronic brain alterations, but the predictive value of this model for treatment of pharmacoresistant partial seizures is not sufficiently known as yet.
Genetic Animal Models of Reflex Epilepsy
Acute seizure induction in genetic models of epilepsy is another example of how chronic epilepsy models can be used for screening. There are various models of “reflex epilepsy” in which seizures can be induced by specific sensory stimuli such as auditory stimulation in audiogenic seizure-susceptible mice (e.g., DBA/2) and rats, different sensory stimuli in gerbils with reflex seizures, and intermittent light stimulation in photosensitive baboons (Papio papio) [9, 65–70]. In particular, audiogenic seizure-susceptible DBA/2 mice are widely used in drug screening. They respond to various categories of ASDs, are often more sensitive to anti-seizure effects of investigational compounds than the traditional MES test, and are thus a sensitive tool to discover anti-seizure efficacy of novel compounds [66, 71]. Interestingly, DBA/2 mice exhibit a decreased MEST and an increased susceptibility to various chemoconvulsants [72, 73], which may be involved in their enhanced susceptibility to ASDs. However, the broad susceptibility of audiogenic seizures in DBA/2 mice to ASDs is also a major disadvantage of this model, because a drug effect against audiogenic seizures in DBA/2 mice is not predictive for efficacy against any specific type of seizures or difficult-to-treat forms of seizures in patients [9, 70]. It would be interesting to evaluate if the effects of ASDs in the MES and PTZ tests in DBA/2 mice differ from those in normal (nonepileptic) mice.
In contrast, the genetically epilepsy-prone rat (GEPR) model, which is composed of two independently derived inbred strains that exhibit a characteristic convulsive pattern in response to a standardized sound stimulus (the moderately epileptic GEPR-3 and the more severely epileptic GEPR-9), can be used to differentiate drugs by their effects on specific seizure types [65, 70, 74]. Furthermore, reflex seizures and epilepsies represent an ancient human model to understand basic mechanisms of epilepsy [75] and the same may be true for animal models of reflex epilepsies. Indeed, the GEPR has recently been proposed as a model of epileptogenesis [70].
Other Types of Genetic Animal Models of Epilepsy
Another strategy of using genetic animal models of epilepsy for drug testing would be induction of acute seizures by electrical or chemical means in genetic models with SRS. For instance, the Genetic Absence Epilepsy Rats from Strasbourg (GAERS), an inbred strain of Wistar rats with spontaneous absence-like spike-wave discharges, which are widely used for testing novel compounds for efficacy against absence seizures [76], show an increased susceptibility to seizure induction by PTZ [77], but are resistant to propagation of seizures induced by amygdala stimulation [78]. Seizure thresholds are often decreased in epileptic rodents [79], but this is rarely used for testing drugs. A recent example comes from Steve White’s group in mouse models of human KCNQ2 and KCNQ3 mutations that cause benign familial neonatal convulsions [80]. Although the heterozygous mice did not appear to have spontaneous seizures, they exhibited decreased electroconvulsive seizure thresholds when stimulated with 6-Hz or 60-Hz currents and enhanced susceptibility to corneally kindled seizures [80]. Thus, induction of such seizures would allow drug testing in these mutant mice. Another example are mutant zebrafish models, in which seizures can be induced by exposure to standard convulsant manipulations (e.g., PTZ, pilocarpine, 4-aminopyridine, heat) to allow drug testing for anti-seizure activity [81, 82].
The recent acceleration in gene discoveries from epileptic encephalopathies and recapitulation of identified mutations in rodents or zebrafish facilitates characterization of the ensuing phenotypes and drug screening in these animals [81–83]. This is a powerful tool with which to approach pharmacoresistance in rare epilepsy syndromes with a well-defined and causal gene mutation responsible for the condition. This will not solve the major part of drug resistant epilepsy but holds the promise to provide an effective contribution to optimal diagnosis and treatment for a number of rare epilepsies, paving the way for precision medicine in epilepsy.
Conclusions
The intriguing idea of Blanco et al. [11] to obtain novel screening models for drug testing by inducing acute seizures in epileptic rather than naive rodents has initiated several subsequent studies that evaluated this idea in mice. These studies did not generally confirm the findings of Blanco et al. [11] that ASDs lose their anti-seizure efficacy in acute seizure tests in epileptic animals but rather showed that the anti-seizure efficacy may decrease, increase or not change at all, depending on the mechanism of action of a drug tested by this novel strategy. As demonstrated with levetiracetam, the altered pharmacological sensitivity of acute seizure tests in epileptic or kindled animals may be more predictive for clinical activity than data from testing in naive mice or rats. This important finding corroborates previous data showing that the predictability of adverse effect testing in epileptic or kindled rodents is much higher than testing in naive animals, simply because the chronic brain alterations associated with epilepsy may have a profound effect on the pharmacodynamic and toxicodynamic activities of drugs [35]. Thus, although drug testing by using acute seizure induction in epileptic rodents does not seem to provide a novel screening strategy for discovering drugs with improved efficacy against pharmacoresistant seizures, it may offer an excellent platform for drugs with mechanisms inherent to disease-induced brain alterations. Based on the initial findings of Blanco et al. [11] using the rat pilocarpine model, further experiments are required to evaluate species differences and whether rats or mice are better suited to use in acute seizure tests in epileptic animals as an approach for finding more effective treatments for pharmacoresistant epilepsy. In addition, as discussed above, further studies are required to explore which model(s) should be used for generating epileptic/pharmacoresistant animals and which acute seizure tests to use in such model(s). The ASP/ETSP is uniquely placed to undertake such work.
Abbreviations
- AED:
-
Antiepileptic drug
- ASD:
-
Anti-seizure drug
- ASP:
-
Anticonvulsant Screening Program
- BUM5:
-
N,N-dimethylaminoethylester of bumetanide
- CC:
-
Convulsant current
- ED50 :
-
Median effective dose
- EEG:
-
Electroencephalogram
- ETSP:
-
Epilepsy Therapy Screening Program
- GAERS:
-
Genetic absence epilepsy rats from strasbourg
- GEPR:
-
Genetically epilepsy-prone rat
- MES:
-
Maximal electroshock seizure
- MEST:
-
MES threshold
- NINDS:
-
National Institute of Neurological Disorders and Stroke
- NKCC:
-
N-K-2Cl cotransporter
- PTZ:
-
Pentylenetetrazole
- SE:
-
Status epilepticus
- SRS:
-
Spontaneous recurrent seizures
- SV2A:
-
Synaptic vesicle protein 2A
- TLE:
-
Temporal lobe epilepsy
References
Krall RL, Penry JK, Kupferberg HJ, Swinyard EA (1978) Antiepileptic drug development: I. History and a program for progress. Epilepsia 19:393–408
Krall RL, Penry JK, White BG, Kupferberg HJ, Swinyard EA (1978) Antiepileptic drug development: II. Anticonvulsant drug screening. Epilepsia 19:409–428
Gladding GD, Kupferberg HJ, Swinyard EA (1985) Antiepileptic drug development program. In: Frey H-H, Janz D (eds) Antiepileptic drugs. Springer, Berlin, pp 341–350
White HS, Wolf HH, Woodhead JH, Kupferberg HJ (1998) The National Institutes of Health Anticonvulsant Drug Development Program: screening for efficacy. Adv Neurol 76:29–39
Wilcox KS, Dixon-Salazar T, Sills GJ, Ben Menachem E, White HS, Porter RJ, Dichter MA, Moshe SL, Noebels JL, Privitera MD, Rogawski MA (2013) Issues related to development of new antiseizure treatments. Epilepsia 54(Suppl 4):24–34
French JA, White HS, Klitgaard H, Holmes GL, Privitera MD, Cole AJ, Quay E, Wiebe S, Schmidt D, Porter RJ, Arzimanoglou A, Trinka E, Perucca E (2013) Development of new treatment approaches for epilepsy: unmet needs and opportunities. Epilepsia 54(Suppl 4):3–12
Löscher W, Schmidt D (2011) Modern antiepileptic drug development has failed to deliver: ways out of the current dilemma. Epilepsia 52:657–678
Löscher W (2016) Fit for purpose application of currently existing animal models in the discovery of novel epilepsy therapies. Epilepsy Res. doi:10.1016/j.eplepsyres.2016.05.016
Löscher W (2011) Critical review of current animal models of seizures and epilepsy used in the discovery and development of new antiepileptic drugs. Seizure 20:359–368
White HS, Smith-Yockman M, Srivastava A, Wilcox KS (2006) Therapeutic assays for the identification and characterization of antiepileptic and antiepileptogenic drugs. In: Pitkänen A, Schwartzkroin PA, Moshé SL (eds) Models of seizures and epilepsy. Elsevier, Amsterdam, pp 539–549
Blanco MM, Dos SJ Jr, Perez-Mendes P, Kohek SR, Cavarsan CF, Hummel M, Albuquerque C, Mello LE (2009) Assessment of seizure susceptibility in pilocarpine epileptic and nonepileptic Wistar rats and of seizure reinduction with pentylenetetrazole and electroshock models. Epilepsia 50:824–831
Leite JP, Garcia-Cairasco N, Cavalheiro EA (2002) New insights from the use of pilocarpine and kainate models. Epilepsy Res 50:93–103
Curia G, Longo D, Biagini G, Jones RS, Avoli M (2008) The pilocarpine model of temporal lobe epilepsy. J Neurosci Methods 172:143–157
Levesque M, Avoli M, Bernard C (2016) Animal models of temporal lobe epilepsy following systemic chemoconvulsant administration. J Neurosci Methods 260:45–52
Leite JP, Cavalheiro EA (1995) Effects of conventional antiepileptic drugs in a model of spontaneous recurrent seizures in rats. Epilepsy Res 20:93–104
Glien M, Brandt C, Potschka H, Löscher W (2002) Effects of the novel antiepileptic drug levetiracetam on spontaneous recurrent seizures in the rat pilocarpine model of temporal lobe epilepsy. Epilepsia 43:350–357
Bankstahl M, Bankstahl JP, Löscher W (2012) Inter-individual variation in the anticonvulsant effect of phenobarbital in the pilocarpine rat model of temporal lobe epilepsy. Exp Neurol 234:70–84
Stables JP, Bertram E, Dudek FE, Holmes G, Mathern G, Pitkänen A, White HS (2003) Therapy discovery for pharmacoresistant epilepsy and for disease-modifying therapeutics: summary of the NIH/NINDS/AES models II workshop. Epilepsia 44:1472–1478
Brandt C, Volk HA, Löscher W (2004) Striking differences in individual anticonvulsant response to phenobarbital in rats with spontaneous seizures after status epilepticus. Epilepsia 45:1488–1497
Bethmann K, Brandt C, Löscher W (2007) Resistance to phenobarbital extends to phenytoin in a rat model of temporal lobe epilepsy. Epilepsia 48:816–826
White HS (1997) Clinical significance of animal seizure models and mechanism of action studies of potential antiepileptic drugs. Epilepsia 38:S9–S17
Löscher W, Schmidt D (1988) Which animal models should be used in the search for new antiepileptic drugs? A proposal based on experimental and clinical considerations. Epilepsy Res 2:145–181
Töllner K, Twele F, Löscher W (2016) Evaluation of the pentylenetetrazole seizure threshold test in epileptic mice as surrogate model for drug testing against pharmacoresistant seizures. Epilepsy Behav 57:95–104
Bankstahl M, Bankstahl JP, Löscher W (2013) Pilocarpine-induced epilepsy in mice alters seizure thresholds and the efficacy of antiepileptic drugs in the 6-Hertz psychomotor seizure model. Epilepsy Res 107:205–216
Erker T, Brandt C, Töllner K, Schreppel P, Twele F, Schidlitzki A, Löscher W (2016) The bumetanide prodrug BUM5, but not bumetanide, potentiates the anti-seizure effect of phenobarbital in adult epileptic mice. Epilepsia 57:698–705
Kaila K, Price TJ, Payne JA, Puskarjov M, Voipio J (2014) Cation-chloride cotransporters in neuronal development, plasticity and disease. Nat Rev Neurosci 15:637–654
Li X, Zhou J, Chen Z, Chen S, Zhu F, Zhou L (2008) Long-term expressional changes of Na+ -K+ -Cl- co-transporter 1 (NKCC1) and K+ -Cl- co-transporter 2 (KCC2) in CA1 region of hippocampus following lithium-pilocarpine induced status epilepticus (PISE). Brain Res 1221:141–146
Cleary RT, Sun H, Huynh T, Manning SM, Li Y, Rotenberg A, Talos DM, Kahle KT, Jackson M, Rakhade SN, Berry G, Jensen FE (2013) Bumetanide enhances phenobarbital efficacy in a rat model of hypoxic neonatal seizures. PLoS One 8:e57148
Töllner K, Brandt C, Töpfer M, Brunhofer G, Erker T, Gabriel M, Feit PW, Lindfors J, Kaila K, Löscher W (2014) A novel prodrug-based strategy to increase effects of bumetanide in epilepsy. Ann Neurol 75:550–562
Brandt C, Nozadze M, Heuchert N, Rattka M, Löscher W (2010) Disease-modifying effects of phenobarbital and the NKCC1 inhibitor bumetanide in the pilocarpine model of temporal lobe epilepsy. J Neurosci 30:8602–8612
Löscher W, Hönack D (1991) Responses to NMDA receptor antagonists altered by epileptogenesis. Trends Pharmacol Sci 12:52
Hönack D, Löscher W (1995) Kindling increases the sensitivity of rats to adverse effects of certain antiepileptic drugs. Epilepsia 36:763–771
Löscher W, Schmidt D (1994) Strategies in antiepileptic drug development: is rational drug design superior to random screening and structural variation? Epilepsy Res 17:95–134
Klitgaard H, Matagne A, Lamberty Y (2002) Use of epileptic animals for adverse effect testing. Epilepsy Res 50:55–65
Löscher W, Klitgaard H, Twyman RE, Schmidt D (2013) New avenues for antiepileptic drug discovery and development. Nat Rev Drug Discov 12:757–776
Toman JEP (1951) Neuropharmacologic Considerations in Psychic Seizures. Neurology 1:444–460
Brown WC, Schiffman DO, Swinyard EA, Goodman LS (1953) Comparative assay of antiepileptic drugs by “pychomotor” seizure test and minimal electroshock threshold test. J Pharmacol Exp Ther 107:273–283
Barton ME, Klein BD, Wolf HH, White HS (2001) Pharmacological characterization of the 6 Hz psychomotor seizure model of partial epilepsy. Epilepsy Res 47:217–228
Leclercq K, Kaminski RM (2015) Genetic background of mice strongly influences treatment resistance in the 6 Hz seizure model. Epilepsia 56:310–318
Leclercq K, Kaminski RM (2015) Status epilepticus induction has prolonged effects on the efficacy of antiepileptic drugs in the 6-Hz seizure model. Epilepsy Behav 49:55–60
Deutsch SI, Mastropaolo J, Riggs RL, Rosse RB (1997) The antiseizure efficacies of MK-801, phencyclidine, ketamine, and memantine are altered selectively by stress. Pharmacol Biochem Behav 58:709–712
Reddy DS, Rogawski MA (2002) Stress-induced deoxycorticosterone-derived neurosteroids modulate GABA(A) receptor function and seizure susceptibility. J Neurosci 22:3795–3805
Joels M (2009) Stress, the hippocampus, and epilepsy. Epilepsia 50:586–597
Riban V, Bouilleret V, Pham L, Fritschy JM, Marescaux C, Depaulis A (2002) Evolution of hippocampal epileptic activity during the development of hippocampal sclerosis in a mouse model of temporal lobe epilepsy. Neuroscience 112:101–111
Klein S, Bankstahl M, Löscher W (2015) Inter-individual variation in the effect of antiepileptic drugs in the intrahippocampal kainate model of mesial temporal lobe epilepsy in mice. Neuropharmacology 90:53–62
Duveau V, Pouyatos B, Bressand K, Bouyssieres C, Chabrol T, Roche Y, Depaulis A, Roucard C (2016) Differential effects of antiepileptic drugs on focal seizures in the intrahippocampal kainate mouse model of mesial temporal lobe epilepsy. CNS Neurosci Ther 22:497–506
Pontes JCC, Lima TZ, Queiroz CM, Cinini SM, Blanco MM, Mello LE (2016) Seizures triggered by pentylenetetrazol in marmosets made chronically epileptic with pilocarpine show greater refractoriness to treatment. Epilepsy Res 126:16-25
Perez-Mendes P, Blanco MM, Calcagnotto ME, Cinini SM, Bachiega J, Papoti D, Covolan L, Tannus A, Mello LE (2011) Modeling epileptogenesis and temporal lobe epilepsy in a non-human primate. Epilepsy Res 96:45–57
Smith M, Wilcox KS, White HS (2007) Discovery of antiepileptic drugs. Neurother 4:12–17
Czuczwar SJ, Turski L, Turski W, Kleinrok Z (1981) Effects of some antiepileptic drugs in pentetrazol-induced convulsions in mice lesioned with kainic acid. Epilepsia 22:407–414
Czuczwar SJ, Turski L, Kleinrok Z (1982) Anticonvulsant action of phenobarbital, diazepam, carbamazepine, and diphenylhydantoin in the electroshock test in mice after lesion of hippocampal pyramidal cells with intracerebroventricular kainic acid. Epilepsia 23:377–382
Goddard GV, McIntyre DC, Leech CK (1969) A permanent change in brain function resulting from daily electrical stimulation. Exp Neurol 25:295–330
Sato M, Racine RJ, McIntyre DC (1990) Kindling: basic mechanisms and clinical validity. Electroenceph Clin Neurophysiol 76:459–472
Löscher W (1997) Animal models of intractable epilepsy. Prog Neurobiol 53:239–258
Löscher W, Jäckel R, Czuczwar SJ (1986) Is amygdala kindling in rats a model for drug-resistant partial epilepsy? Exp Neurol 93:211–226
Löscher W, Hönack D (1993) Profile of ucb L059, a novel anticonvulsant drug, in models of partial and generalized epilepsy in mice and rats. Eur J Pharmacol 232:147–158
Klitgaard, H., and Verdru, P. 2007. Levetiracetam: the first SV2A ligand for the treatment of epilepsy. Expert Opin Drug Discov 2:1537–1545.
Klitgaard H (2001) Levetiracetam: the preclinical profile of a new class of antiepileptic drugs? Epilepsia 42(Suppl 4):13–18
Löscher W (2002) Animal models of epilepsy for the development of antiepileptogenic and disease-modifying drugs. A comparison of the pharmacology of kindling and post-status epilepticus models of temporal lobe epilepsy. Epilepsy Res 50:105–123
White HS, Wolf HH, Swinyard EA, Skeen GA, Sofia RD (1992) A neuropharmacological evaluation of felbamate as a novel anticonvulsant. Epilepsia 33:564–572
Matagne A, Klitgaard H (1998) Validation of corneally kindled mice: a sensitive screening model for partial epilepsy in man. Epilepsy Res 31:59–71
Potschka H, Löscher W (1999) Corneal kindling in mice: behavioral and pharmacological differences to conventional kindling. Epilepsy Res 37:109–120
Rowley NM, White HS (2010) Comparative anticonvulsant efficacy in the corneal kindled mouse model of partial epilepsy: correlation with other seizure and epilepsy models. Epilepsy Res 92:163–169
Leclercq K, Matagne A, Kaminski RM (2014) Low potency and limited efficacy of antiepileptic drugs in the mouse 6 Hz corneal kindling model. Epilepsy Res 108:675–683
Jobe PC, Mishra PK, Ludvig N, Dailey JW (1991) Scope and contribution of genetic models to an understanding of the epilepsies. Crit Rev Neurobiol 6:183–220
Löscher W (1984) Genetic animal models of epilepsy as a unique resource for the evaluation of anticonvulsant drugs. A review. Methods Find Exp Clin Pharmacol 6:531–547
Löscher W, Meldrum BS (1984) Evaluation of anticonvulsant drugs in genetic animal models of epilepsy. Fed Proc 43:276–284
Naquet RG, Valin A (1998) Experimental models of reflex epilepsy. Adv Neurol 75:15–28
Seyfried TN, Todorova MT, Poderycki MJ (1999) Experimental models of multifactorial epilepsies: the EL mouse and mice susceptible to audiogenic seizures. Adv Neurol 79:279–290
De Sarro G, Russo E, Citraro R, Meldrum BS (2015) Genetically epilepsy-prone rats (GEPRs) and DBA/2 mice: two animal models of audiogenic reflex epilepsy for the evaluation of new generation AEDs. Epilepsy Behav. doi:10.1016/j.yebeh.2015.06.030
Chapman AG, Croucher MJ, Meldrum BS (1984) Evaluation of anticonvulsant drugs in DBA/2 mice with sound-induced seizures. Arzneimittelforschung 34:1261–1270
Ferraro TN, Golden GT, Snyder R, Laibinis M, Smith GG, Buono RJ, Berrettini WH (1998) Genetic influences on electrical seizure threshold. Brain Res 813:207–210
Chaix Y, Ferraro TN, Lapouble E, Martin B (2007) Chemoconvulsant-induced seizure susceptibility: toward a common genetic basis? Epilepsia 48(Suppl 5):48–52
Dailey JW, Jobe PC (1985) Anticonvulsant drugs and the genetically epilepsy-prone rat. Fed Proc 44:2640–2644
Striano S, Coppola A, del Gaudio L, Striano P (2012) Reflex seizures and reflex epilepsies: old models for understanding mechanisms of epileptogenesis. Epilepsy Res 100:1–11
Depaulis A, David O, Charpier S (2016) The genetic absence epilepsy rat from Strasbourg as a model to decipher the neuronal and network mechanisms of generalized idiopathic epilepsies. J Neurosci Methods 260:159–174
Brailowsky S, Montiel T, Boehrer A, Marescaux C, Vergnes M (1999) Susceptibility to focal and generalized seizures in Wistar rats with genetic absence-like epilepsy. Neuroscience 93:1173–1177
Eskazan E, Onat FY, Aker R, Oner G (2002) Resistance to propagation of amygdaloid kindling seizures in rats with genetic absence epilepsy. Epilepsia 43:1115–1119
Frankel WN (2009) Genetics of complex neurological disease: challenges and opportunities for modeling epilepsy in mice and rats. Trends Genet 25:361–367
Otto JF, Singh NA, Dahle EJ, Leppert MF, Pappas CM, Pruess TH, Wilcox KS, White HS (2009) Electroconvulsive seizure thresholds and kindling acquisition rates are altered in mouse models of human KCNQ2 and KCNQ3 mutations for benign familial neonatal convulsions. Epilepsia 50:1752–1759
Baraban SC, Löscher W (2014) What new modeling approaches will help us identify promising drug treatments? Adv Exp Med Biol 813:283–294
Grone BP, Baraban SC (2015) Animal models in epilepsy research: legacies and new directions. Nat Neurosci 18:339–343
Bialer, M., White, H.S (2010) Key factors in the discovery and development of new antiepileptic drugs. Nat Rev Drug Discov 9:68–82
Acknowledgments
The author thanks Michael A. Rogawski, Henrik Klitgaard, Graeme Sills, Stanislaw Jerzy Czuczwar, Luiz E. Mello, Kathrin Töllner, Claudia Brandt, Marion Bankstahl, and Manuela Gernert for excellent comments on previous versions of the manuscript and Kathrin Töllner for contributing unpublished data from PTZ seizure threshold experiments in epileptic and naive mice. The author’s own studies were supported by grants from the Deutsche Forschungsgemeinschaft (Bonn, Germany) and funding from the European Union’s Seventh Framework Programme (FP7/2007–2013) under Grant Agreement no 602102 (EPITARGET).
Author information
Authors and Affiliations
Corresponding author
Additional information
This review is dedicated to my colleague and friend Dr. H. Steve White to acknowledge his outstanding contributions in anti-seizure drug discovery and development of novel models of drug-resistant seizures.
Rights and permissions
About this article
Cite this article
Löscher, W. The Search for New Screening Models of Pharmacoresistant Epilepsy: Is Induction of Acute Seizures in Epileptic Rodents a Suitable Approach?. Neurochem Res 42, 1926–1938 (2017). https://doi.org/10.1007/s11064-016-2025-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-016-2025-7