Abstract
Introduction
Pseudoprogression (PsP) is a diagnostic dilemma in glioblastoma (GBM) after chemoradiotherapy (CRT). Magnetic resonance imaging (MRI) features may fail to distinguish PsP from early true progression (eTP), however clinical findings may aid in their distinction.
Methods
Sixty-seven patients received CRT for GBM between 2003 and 2016, and had pre- and post-treatment imaging suitable for retrospective evaluation using RANO criteria. Patients with signs of progression within the first 12-weeks post-radiation (P-12) were selected. Lesions that improved or stabilized were defined as PsP, and lesions that progressed were defined as eTP.
Results
The median follow up for all patients was 17.6 months. Signs of progression developed in 35/67 (52.2%) patients within P-12. Of these, 20/35 (57.1%) were subsequently defined as eTP and 15/35 (42.9%) as PsP. MRI demonstrated increased contrast enhancement in 84.2% of eTP and 100% of PsP, and elevated CBV in 73.7% for eTP and 93.3% for PsP. A decrease in FLAIR was not seen in eTP patients, but was seen in 26.7% PsP patients. Patients with eTP were significantly more likely to require increased steroid doses or suffer clinical decline than PsP patients (OR 4.89, 95% CI 1.003–19.27; p = 0.046). KPS declined in 25% with eTP and none of the PsP patients.
Conclusions
MRI imaging did not differentiate eTP from PsP, however, KPS decline or need for increased steroids was significantly more common in eTP versus PsP. Investigation and standardization of clinical assessments in response criteria may help address the diagnostic dilemma of pseudoprogression after frontline treatment for GBM.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Glioblastoma (GBM) is the most common high-grade primary central nervous system (CNS) tumor, and is associated with a very poor prognosis. Over a decade ago, radiation therapy (RT) with concurrent and adjuvant temozolomide (TMZ) was established as the standard of care post-operatively for GBM. However, the addition of TMZ to radiation therapy created a clinical quandary, as it was found to increase the rate of pseudoprogression (PsP), a phenomenon that when seen on post-radiation imaging can suggest progression of disease. However, in contrast to true progression, PsP lesions stabilize or resolve without specific treatment [1, 2].
Rates of PsP vary in the literature from 3 to 30%, with rates being highly dependent on the study definition of PsP and the diagnostic modalities used [3,4,5,6,7]. Pathologic confirmation remains the gold standard for diagnosis of recurrent or residual disease in GBM, however, response assessment criteria have been established as a means of non-invasively identifying progression of disease in daily clinical decision making. Most studies in the PsP literature have focused on new or progressive areas of contrast enhancement as the defining sign of progression, and do not apply modern clinical and radiographic response assessment criteria which include T2-weighted MRI images, steroid dose, and KPS decline, in the assessment of response. The current recommendations for response assessment from the Response Assessment in Neuro-Oncology (RANO) group incorporate both radiographic changes and clinical signs to define progressive disease [8].
Systematic assessment of response criteria in PsP is clinically significant issue, as the erroneous diagnosis of disease progression may result in an inappropriate change in management when, in fact, there has been a positive tumor response. Thus, the failure to recognize PsP may lead to cessation of effective treatment strategies. Conversely, the misclassification of truly progressive disease may delay the implementation of alternative therapy. In our series, we highlight the radiographic and clinical characteristics of patients with eTP and PsP in the RANO era, additionally providing a timeline comparing PsP and early true progression with corresponding clinical outcomes.
Methods
Patient selection criteria
Patients with histologically confirmed World Health Organization (WHO) grade IV GBM treated on a National Cancer Institute (NCI) institutional review board (IRB) approved protocol between 2003 and 2016 were retrospectively reviewed. Informed consent was obtained from all individual participants included in this IRB approved study. Inclusion criteria consisted of age 18 years or older, post-operative baseline MRI scan less than 48 h after surgery, adjuvant radiation therapy received at our institution, completion of entire adjuvant course of radiotherapy, and continued clinical and radiographic follow-up until the time of progression. Patients were excluded from the analysis if they were treated with bevacizumab or a new systemic agent within the first 12-weeks post-radiation therapy. Tumor volume was calculated using Eclipse (Varian, Stanford, CA) contouring software, and lesions were separated into volumetric quartiles for comparison. O6-methylguanine-DNA methyltransferase (MGMT) promoter methylation analysis was performed by the NCI Molecular Diagnostics Laboratory of the Laboratory of Pathology.
All patients underwent surgical resection followed by involved field external beam radiation with concurrent daily TMZ at 75 mg/m2/day. Adjuvant TMZ was then prescribed at 150–200 mg/m2/day for 5 of every 28 days for 6–12 cycles or until disease progression or treatment related toxicity developed.
True progression and pseudoprogression categorization
Multiparametric MRI scans were performed prior to RT initiation, at approximately 4-weeks following RT completion, and every 8–12 weeks thereafter. Cases were reviewed by a neuroradiologist (J.B.) and response assessment was per RANO criteria [8]. Decline in KPS score was defined as a decline of greater than or equal to 20 points. Within the initial 12-weeks post-radiation therapy, patients were assessed for signs of progression (Table 1) adopted from RANO criteria. Patients with stable disease (SD) or partial response (PR) were considered non-progressive disease (non-PD), patients who had radiographic and/or clinical signs of progression were considered to have preliminary progressive disease (PPD). After the initial 12-weeks post-radiation, PPD lesions that had improved or stabilized were documented as pseudoprogression (PsP) and lesions that continued to progress were considered early true progression (eTP).
Magnetic resonance imaging
MRI was performed at 1.5 or 3.0 T (Philips Acheiva) using an 8-channel head coil with a standard protocol using two doses of a gadolinium based contrast agent (GBCA) for dynamic imaging according to the following schedule: (1) Pre-contrast: Sagittal SE T1w, 3D SWI. Axial SE T1, FSE T2, EPI diffusion tensor (15 direction B = 0, 1000). (2) For dynamic contrast enhanced (DCE) MRI Dynamic 1: Dynamic contrast enhanced (DCE) MRI using T1 FFE. (3) Post-contrast 1: Axial SE T1 (follows first dose). (4) Dynamic 2: Dynamic susceptibility contrast (DSC) using T2* EPI (5) Post-contrast 2: Sagittal 3D isotropic T1-FFE and 3D FLAIR. Each dynamic study was associated with bolus injection of 0.1 mmol/kg ProHance (unless contraindicated due to prior adverse reaction in which case another agent was substituted). For DCE, injection was 0.3 mL/s. For DSC, injection rate was typically 5 mL/s, but could be reduced based on status of I.V. access.
Perfusion maps of CBV, CBF and mTT were computed by the estimation of an arterial input function and deconvolution. The preinjection for the DCE MRI component of the imaging minimizes leakage effects on DSC estimates, therefore, no leakage correction was performed.
Statistical analysis
Tumor progression was documented based on KPS decline or MRI-documented progression of disease. The date of death was determined based on clinic notes or using the internet-based Social Security Death Index. Progression-free survival and overall survival were measured from the date of diagnosis to the date of progression, death, or last follow-up. Time to-event distributions were estimated using the Kaplan–Meier method and compared with the log-rank test. Cox regression was used for univariate and multivariate analysis. Association between categorical variables were tested by the Chi square test and mean difference of continuous variables between subgroups of patients were compared by the t-test. All p-values correspond to two-sided tests, with a p-value < 0.05 considered statistically significant.
Results
Patient characteristics
Sixty-seven patients were treated with RT/TMZ at the NCI in Bethesda, Maryland between 2003 and 2016 and met inclusion criteria for this study. Patient demographics and baseline characteristics are presented in Table 2. All patients received 59.4–60 Gy in 30–33 fractions with concurrent TMZ, except 3 patients who did not complete concurrent TMZ and 1 patient who received 50 Gy in 24 fractions. 6 of the 67 patients did not initiate adjuvant TMZ, 3 due to early progression of disease and 3 due to residual toxicity from concurrent TMZ. The mean age of all patients was 55.7 years and 70% were male.
Time to progression and overall survival
At a median follow-up of 17.6 months, overall PFS was 9.0 months (95% CI 7.5–10.4), and OS was 20.7 months (95% CI 17.3–27.0) for the entire cohort. MGMT promotor status was available in 33 patients, with 13/33 (39.4%) being MGMT methylation positive (Table 2). OS was significantly improved in MGMT methylated tumors with a median OS of 37.0 months versus 15.3 months for unmethylated tumors (p = 0.001). In patients with known recurrence (n = 55), patterns of recurrence were primarily local (within the 90% isodose line). Tumor recurrence was non-local (outside of the 90% isodose line) in only two cases, and in both cases the recurrence was outside the time limit for defining PsP (˃ 10 months post-radiation therapy).
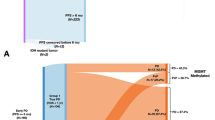
Pseudoprogression, early true progression, and non-progressive disease
Imaging changes concerning for progression (Table 1) developed in 35/67 (52.2%) patients within 12-weeks after radiation. Most patients (28/35) were diagnosed as PPD in the first post-radiation MRI at the 4-week time point (median of 3.4 weeks for eTP and 3.8 weeks for PsP), and only 7/35 were diagnosed between 5 and 12 weeks. With additional follow-up, it was determined that 20/35 (57.1%) patients fulfilled criteria for eTP and 15/35 (42.9%) fulfilled criteria for PsP (Table 1).
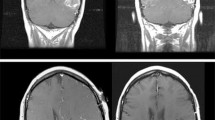
Rates of increased contrast enhancement on MRI was similar between patients with eTP (84.2%) and PsP (100%) at 4-weeks post-chemoradiation. FLAIR volume was increased, decreased, and stable in 46.7, 26.7, and 26.7% in patients with PsP respectively. This was compared to FLAIR increased in 73.7%, stable in 26.3% of patients with eTP, with none having decreased FLAIR (Table 3). Progression of contrast enhancement or FLAIR volume did not distinguish between PsP and eTP, but of note, FLAIR signal decreased in 26.7% of PsP patients, which was not observed in any of the eTP cases.
Though not a component of the RANO criteria, perfusion imaging was also assessed. Perfusion imaging of regions of interest demonstrated elevated relative cerebral blood volume (rCBV) in 73.7% of eTP and 93.3% of PsP patients (Table 3). When initially assessed by radiologists at the time of imaging, elevated perfusion was interpreted as potential residual high-grade disease in all cases. On retrospective review, increased perfusion did not differentiate eTP and PsP.
Though no statistically significant differences on imaging were noted, there was a significant difference between patients with PsP and eTP in their need for increased steroids or the documentation of a clinical decline (OR 4.89, 95% CI 1.003–19.27; p = 0.046). For example, in response to worsening neurological symptoms, 9/20 (45%) eTP and 3/15 (20%) PsP required increased steroids after assessment by their oncologist. KPS declined in 5/20 (25%) eTP at a mean of 6 weeks, but no KPS declines were seen in the patients with PsP.
As expected, OS was significantly worse in patients with eTP (p = 0.032) with a median OS of 13.2 months (95% CI 11.1–20.1) versus 23.6 months (95% CI 16.5–65.3+) for patients with PsP (Fig. 1). Additionally, patients with eTP had a significantly shorter median OS of 13.2 months compared with the non-PD group (p < 0.001). However, there was no statistically significant benefit for PsP compared with non-PD at median OS of 23.6 and 27.6 months, respectively (p = 0.617). On univariate analysis, age ≥ 50, male gender, larger, and MGMT unmethylated tumors, and eTP were a detriment to PFS and OS (Table 4). On multivariate analysis age ≥ 50, tumor size, MGMT non-methylated, and eTP were significantly detrimental to OS (Table 4). Unmethylated MGMT status was an independent risk factor for survival (p = 0.003), and predictive of eTP (p = 0.005).
Kaplan–Meier analysis of progression free survival (PFS) and overall survival (OS) for patients with early true progression (eTP), pseudoprogression (PsP), and non-progressive disease (non-PD) The median PFS for eTP was 4.95 months (95% CI 4.0–5.4), for PsP was 10.1 months (95% CI 9.0–65.3 months), and non-PD was 11.2 months (95% CI 9.2–15.1). The median OS for eTP was 13.2 months (95% CI 11.1–20.1), for PsP was 23.6 months (95% CI 16.5–65.3+), and for non-PD was 27.6 months (95% CI 22.5–37.0)
Discussion
Pseudoprogression continues to be a diagnostic dilemma, and in this retrospective study we attempt to delineate the clinical trajectory of PsP patients in daily practice using RANO criteria. The rate of PsP in our cohort was 22.4%, which falls within the published range of 3–30%, however, ours is one of few studies that have holistically applied current RANO criteria to define progression [3, 4, 9,10,11]. A limitation of previous reports on progression and pseudoprogression in the literature is the variability of definitions of progression used, as most studies have primarily focused specifically on changes in contrast enhancement [3, 4, 6,7,8, 12].
Using modern criteria, radiologic features alone continue to be unable to differentiate eTP from PsP. Similar rates of increasing contrast enhancement were seen between groups, as has been previously documented [3, 6, 9, 13]. While inconsistently applied as a sign of progression in previous publications, T2-weighted and FLAIR imaging changes were also not significantly different between groups. This data supports the updated response evaluation criteria specifically for clinical trials in GBM, which suggest that the prognostic value of T2 or FLAIR change is not well established as the distinction between edema and non-enhancing tumor complicates interpretation [14].
Physiologic MRI techniques, such as perfusion imaging, have been increasingly utilized in the past decade, however, limitations in differentiating PsP or pseudoresponse have prevented their application in clinical response assessment [8, 14, 15]. Initial associations with perfusion imaging were promising as they proposed a relationship between elevated perfusion and active tumor, suggesting that rCBV may be a predictor of poor outcome in high grade glioma [16, 17]. In our cohort, both eTP and PsP patients when differentiated using RANO criteria had similar rates of increased rCBV, and elevated perfusion alone was not predictive of outcomes. The dilemma of elevated perfusion in PsP supports ongoing efforts to quantify specific metrics to differentiate PsP from true progression, such as setting thresholds for rCBV, percentage signal intensity recovery, and relative peak height. However, our data also highlights the need for standardized acquisition and consensus values for these techniques, that they might be most useful in daily patient management for application in standardized assessment criteria [14, 18,19,20].
In our cohort, PPD was diagnosed by radiologists most often at the time of first post-radiation MRI (usually the 3–4-week time point) which is a clinically significant timepoint in that it sets the baseline for adjuvant systemic therapy, and this did not differ between PsP and eTP groups. This is important to note, as the majority of potential PsP patients are captured early within the 12-week window as described by the RANO guidelines for diagnosis of pseudoprogression [8]. However, PsP has been documented up to 6 months post-radiation [12, 21], and a limitation of retrospective analyses is the exclusion of a small number of patients who have a response to therapy and experience continued pseuodprogression past 12-weeks. In our cohort, patients with continued signs of progression past 12 weeks went on to additional therapies, thus confounding analysis of any late responses to treatment.
Within current RANO clinical response assessment criteria, clinical status is acknowledged as an important variable in the definition of progression. Related to this, documentation of steroid dose adjustments is necessary when interpreting changes on imaging. The initiation or modification of steroid dose adds a layer of complexity to response assessment in that, changes in steroid dose not only have radiographic effects, but usually originate from a change in clinical status and/or neurologic symptoms. In our series, we found that the use of steroids was a potentially more sensitive indicator differentiating eTP from PsP due to its role as a surrogate gauge of decline in clinical status and/or symptoms. Patients who required increase in their steroids post-radiation were more than twice as likely to be experiencing eTP. While clinical symptom quantification may be promising for response assessment, one of the limitations of including clinical assessment directly into response criteria is that the exact definition of change in neurologic symptoms is currently imprecise. Our data supports efforts to standardize and quantify these criteria in the neuro-oncology literature not only for the benefit of clinical trials, but for wholistic response assessment [14, 15, 22]. Additionally, none of the PsP patients experienced a decline in their KPS, as defined by RANO, in conjunction with their radiographic signs of progression, while this was seen in 25% of eTP patients; underscoring the importance of clinical assessment in response evaluation for high grade gliomas. Clinical symptoms and their trajectory in the RANO era have been examined in one other retrospective publication by Balana et al. [11], therefore, these findings would benefit from investigation and validation in prospective clinical trials, preferably with patient reported outcomes analysis, as the rates of clinical and neurologic decline in the setting of pseudoprogression using current response criteria are poorly understood.
As previously reported in GBM, older age and larger tumor size were associated with poorer survival on univariate and multivariate analysis [14, 23, 24]. MGMT methylation has known prognostic significance in GBM, and rates of MGMT methylation were significantly lower in patients with eTP in our patient cohort. Since 2008 a relationship between MGMT promoter methylation status and PsP has been postulated [6, 25]. In their cohort of 103 patients, Brandes et al. noted a significant increase in MGMT promoter methylation in patients with PsP [3]. Recently, associations between molecular and pathologic features, such as IDH-1 and p53 mutations, tumor proliferation index, and percent viable tumor at resection have also been correlated with PsP and outcome at recurrence [3, 6, 7, 26,27,28,29]. Continued investigation of molecular subtypes of disease, and risk factors for pseudoprogression, may help predict the likelihood that imaging changes are more likely true progression or PsP. However, to date tumor markers do not reliably predict the underlying cause of imaging changes.
Finally, the relationship between PsP and overall survival is not yet clear, as data on statistically significant improvement is variable, and robust molecular data is only now emerging [4, 6, 26, 28]. While there is widespread agreement on the inferior prognosis of eTP, there is significant controversy surrounding the prognosis of PsP in relation to non-PD. Some investigators have found that patients with PsP have significantly improved overall survival [3, 6, 13], while other groups have not [10, 18, 30,31,32] reflecting the heterogeneity and limitations of the available data and the lack of a combination of robust models that incorporate both biological behavior and imaging features, including other modalities such as physiologic imaging. In our study using RANO groupings, patients with eTP had a significantly shorter median OS of 13.2 months compared with the PsP and non-PD groups with no statistically significant benefit for PsP compared with non-PD at median OS of 23.6 and 27.6 months, respectively which is comparable with previous literature that incorporate other response assessment methods. Further prospective analysis, and studies with larger patient numbers using modern response assessment, may be able to provide more insight into the radiologic biomarkers, molecular risk grouping, and prognostic significance of pseudoprogression in this common CNS disease.
Conclusion
PsP is a diagnostic dilemma in the management of patients with malignant primary brain tumors. To date, conventional MRI studies including perfusion imaging do not reliably differentiate pseudoprogression from true progression. However, there are important differences in clinical findings. In our cohort, worsening of KPS or the need for increased steroids within the first 12-weeks post-radiation therapy was significantly increased in eTP versus PsP. This was often preceded by clinical neurologic worsening. Assessment of these findings and of the clinical course of PsP require prospective validation, and the implementation of standardized assessment of neurologic function would greatly facilitate the widespread use of this metric as an aid in decision making regarding PsP. In the future, tumor molecular analyses as well as novel imaging technologies may help differentiate true progression from pseudoprogression. However, awareness of the frequent occurrence of pseudoprogression is critically important so patients do not have effective treatment halted, or alternative therapies initiated and erroneously considered effective as the PsP spontaneously improves.
References
Chamberlain MC et al (2007) Early necrosis following concurrent Temodar and radiotherapy in patients with glioblastoma. J Neurooncol 82(1):81–83
Fink J, Born D, Chamberlain MC (2011) Pseudoprogression: relevance with respect to treatment of high-grade gliomas. Curr Treat Options Oncol 12(3):240–252
Brandes AA et al (2008) MGMT promoter methylation status can predict the incidence and outcome of pseudoprogression after concomitant radiochemotherapy in newly diagnosed glioblastoma patients. J Clin Oncol 26(13):2192–2197
Linhares P et al (2013) Early pseudoprogression following chemoradiotherapy in glioblastoma patients: the value of RANO evaluation. J Oncol 2013:690585
Young RJ et al (2013) MRI perfusion in determining pseudoprogression in patients with glioblastoma. Clin Imaging 37(1):41–49
Li H et al (2016) IDH mutation and MGMT promoter methylation are associated with the pseudoprogression and improved prognosis of glioblastoma multiforme patients who have undergone concurrent and adjuvant temozolomide-based chemoradiotherapy. Clin Neurol Neurosurg 151:31–36
Pouleau HB et al (2012) High levels of cellular proliferation predict pseudoprogression in glioblastoma patients. Int J Oncol 40(4):923–928
Wen PY et al (2010) Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group. J Clin Oncol 28(11):1963–1972
Gerstner ER et al (2009) Effect of adding temozolomide to radiation therapy on the incidence of pseudo-progression. J Neurooncol 94(1):97–101
Kong DS et al (2011) Diagnostic dilemma of pseudoprogression in the treatment of newly diagnosed glioblastomas: the role of assessing relative cerebral blood flow volume and oxygen-6-methylguanine-DNA methyltransferase promoter methylation status. AJNR Am J Neuroradiol 32(2):382–387
Balana C et al (2017) Pseudoprogression as an adverse event of glioblastoma therapy. Cancer Med 6(12):2858–2866
Radbruch A et al (2015) Pseudoprogression in patients with glioblastoma: clinical relevance despite low incidence. Neuro Oncol 17(1):151–159
Gunjur A et al (2011) Early post-treatment pseudo-progression amongst glioblastoma multiforme patients treated with radiotherapy and temozolomide: a retrospective analysis. J Med Imaging Radiat Oncol 55(6):603–610
Ellingson BM, Wen PY, Cloughesy TF (2017) Modified Criteria for radiographic response assessment in glioblastoma clinical trials. Neurotherapeutics 14(2):307–320
Nowosielski M, Wen PY (2018) Imaging criteria in neuro-oncology. Semin Neurol 38(1):24–31
Di Stefano AL et al (2014) Facing contrast-enhancing gliomas: perfusion MRI in grade III and grade IV gliomas according to tumor area. Biomed Res Int 2014: 154350
Law M et al (2008) Gliomas: predicting time to progression or survival with cerebral blood volume measurements at dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging. Radiology 247(2):490–498
Thomas AA et al (2015) Dynamic contrast enhanced T1 MRI perfusion differentiates pseudoprogression from recurrent glioblastoma. J Neurooncol 125(1):183–190
Gahramanov S et al (2013) Pseudoprogression of glioblastoma after chemo- and radiation therapy: diagnosis by using dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging with ferumoxytol versus gadoteridol and correlation with survival. Radiology 266(3):842–852
Gahramanov S et al (2014) Diagnosis of pseudoprogression using MRI perfusion in patients with glioblastoma multiforme may predict improved survival. CNS Oncol 3(6):389–400
Nasseri M et al (2014) Evaluation of pseudoprogression in patients with glioblastoma multiforme using dynamic magnetic resonance imaging with ferumoxytol calls RANO criteria into question. Neuro Oncol 16(8):1146–1154
Nayak L et al (2014) The Neurologic Assessment in Neuro-Oncology (NANO) Scale: a tool to assess neurologic function for integration in the Radiologic Assessment in Neuro-Oncology (RANO) Criteria. Neurology 82(10 Supplement):S22.005
Lamborn KR, Chang SM, Prados MD (2004) Prognostic factors for survival of patients with glioblastoma: recursive partitioning analysis. Neuro Oncol 6(3):227–235
Ho J et al (2013) Chemoirradiation for glioblastoma multiforme: The National Cancer Institute experience. PLoS ONE 8(8):e70745
Yoon RG et al (2017) Different diagnostic values of imaging parameters to predict pseudoprogression in glioblastoma subgroups stratified by MGMT promoter methylation. Eur Radiol 27(1):255–266
Motegi H et al (2013) IDH1 mutation as a potential novel biomarker for distinguishing pseudoprogression from true progression in patients with glioblastoma treated with temozolomide and radiotherapy. Brain Tumor Pathol 30(2):67–72
Gzell C et al (2016) Proliferation index predicts survival after second craniotomy within 6 months of adjuvant radiotherapy for high-grade glioma. Clin Oncol (R Coll Radiol) 28(3):215–222
Kang HC et al (2011) Pseudoprogression in patients with malignant gliomas treated with concurrent temozolomide and radiotherapy: potential role of p53. J Neurooncol 102(1):157–162
Romano A et al (2013) Apparent diffusion coefficient obtained by magnetic resonance imaging as a prognostic marker in glioblastomas: correlation with MGMT promoter methylation status. Eur Radiol 23(2):513–520
Sanghera P et al (2010) Pseudoprogression following chemoradiotherapy for glioblastoma multiforme. Can J Neurol Sci 37(1):36–42
Roldan GB et al (2009) Population-based study of pseudoprogression after chemoradiotherapy in GBM. Can J Neurol Sci 36(5):617–622
Young RJ et al (2011) Potential utility of conventional MRI signs in diagnosing pseudoprogression in glioblastoma. Neurology 76(22):1918–1924
Funding
This research was funded by the intramural research program at the National Cancer Institute (Grant Number ZID BC 010990).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Rowe, L.S., Butman, J.A., Mackey, M. et al. Differentiating pseudoprogression from true progression: analysis of radiographic, biologic, and clinical clues in GBM. J Neurooncol 139, 145–152 (2018). https://doi.org/10.1007/s11060-018-2855-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-018-2855-z