Abstract
For high-risk low-grade gliomas (LGGs), adjuvant radiotherapy (RT) with procarbazine/lomustine/vincristine (PCV) chemotherapy increases overall survival (OS) over RT alone. However, in practice, temozolomide (TMZ) is often used instead of PCV. Using the National Cancer Data Base (NCDB), we provide the first investigation of practice patterns and outcomes of chemoradiotherapy with single-agent chemotherapy (SAC, analogous to TMZ) or multi-agent chemotherapy (MAC, analogous to PCV) for LGG. Patients with high-risk Grade II LGGs were queried in the NCDB. Inclusion was limited to patients treated with definitive RT and chemotherapy. Patients were divided into cohorts receiving SAC or MAC. Kaplan–Meier analysis compared overall survival (OS), and Cox proportional hazards models determined variables independently associated with OS. Of 1029 patients, 989 (96.1%) received SAC, while 40 (3.9%) received MAC. Patients treated more recently (2010–2012) were less likely to receive MAC (p = 0.029). No differences in median OS were observed between patients treated with MAC and SAC (45.3 vs. 59.2 months, p = 0.861). Independent predictors of worse OS included age >40, high Charlson–Deyo index, other governmental/unrecorded insurance status, biopsy only, astrocytoma histology, Western geographical region, and higher income. Substuting MAC with SAC had no impact on OS (p = 0.804). There is a significantly greater utilization of SAC compared to MAC in the US. There were no differences in OS between patients receiving SAC and MAC, nor did this factor impact OS on multivariate analysis, suggesting that the practice of substituting MAC with SAC for management of LGG may not adversely affect outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Low-grade gliomas (LGGs) comprise a heterogeneous group of neoplasms that, despite a rather uniform histology-based classification, exhibit substantial variations in biological behavior. LGGs comprise an estimated 5–15% of all primary brain tumors, equating to 2000–3000 cases per year in the United States [1].
The management of LGGs has recently been evaluated in a phase III trial demonstrating superiority of chemoradiotherapy (CRT) over radiotherapy (RT) alone, which has since become the treatment of choice for select LGG patients [2]. However, whereas chemotherapy (CT) delivered in the Radiation Therapy Oncology Group (RTOG) 9802 trial was PCV (procarbazine, lomustine, and vincristine), this regimen has known limitations regarding logistical aspects of administration as well as poor tolerance [3,4,5].
The arrival of temozolomide (TMZ) to the forefront of neuro-oncology was supported by initial data describing appropriate penetrability through the blood–brain barrier, ease of administration, and relatively good tolerance [6]. Owing to the results of randomized trials in glioblastoma, TMZ has now become the CT of choice in such cases [7, 8]. Prospective data also suggest similar efficacy of TMZ and PCV for high-grade gliomas in the primary [3], recurrent [9], and sequential [10, 11] settings.
As such, despite the use of multi-agent PCV CT in randomized trials of LGG, clinicians have often extrapolated the safety and efficacy of TMZ from the experience of high grade gliomas to LGGs [5, 12]. It has been shown that the vast majority of oncologists prefer TMZ for LGGs [13], and prospective data suggest high efficacy and tolerability of TMZ-based CRT [14]. Moreover, this has even extended to national guidelines, wherein both single-agent TMZ and multi-agent PCV are listed as equally appropriate options [15]. Furthermore, TMZ has been explored as single-agent therapy for various subsets of LGGs in lieu of RT in both the retrospective [16,17,18,19,20] and prospective [21,22,23] realms.
However, amidst the rising and widespread use of single-agent TMZ over multi-agent PCV for LGGs, there are virtually no comparative data between both regimens. Using the large volume afforded by the National Cancer Data Base (NCDB), we evaluated practice patterns and outcomes of patients with LGG undergoing CRT with either single-agent or multi-agent CT.
Materials and methods
This study analyzed the NCDB, which is a joint project of the Commission on Cancer (CoC) of the American College of Surgeons and the American Cancer Society. The NCDB consists of de-identified information regarding tumor characteristics, patient demographics, and patient survival for approximately 70% of the US population [24]. The NCDB contains information not included in the surveillance, epidemiology, and end results database, including details regarding use of systemic therapy. The data used in the study were derived from a de-identified NCDB file. The American College of Surgeons and the CoC have not verified and are neither responsible for the analytic or statistical methodology employed nor the conclusions drawn from these data by the investigators. As all patient information in the NCDB database is de-identified, this study was exempt from institutional review board evaluation.
The NCDB was queried to identify patients diagnosed with LGG between 2004 and 2012. In order to be included in the present study, patients were required to meet the “high risk” criteria as laid out in RTOG 9802, which is to have been diagnosed with a supratentorial World Health Organization (WHO) Grade 2 Astrocytoma (International Classification of Disease for Oncology [ICD-O-3] codes 9383, 9384, 9400, 9401, 9410, 9411, 9412, 9420, 9421, 9424, or 9425), Oligodendroglioma (ICD-O-3 cods 9450, 9451, 9460, or 9505), or mixed Oligoastrocytoma (ICD-O-3 code 9382) with age ≥40 or sub-total resection (2). Additional inclusion criteria included histological diagnostic confirmation of disease, receipt of concurrent or adjuvant chemotherapy, receipt of definitive radiation therapy (RT), and known vital status. Definitive RT referred to an external beam dose of ≥45 Gy. Concurrent or adjuvant chemotherapy was defined as chemotherapy that was initiated within 100 days of commencing RT, as we wanted to exclude patients who received chemotherapy in the salvage setting. The patients were divided into two groups based on the number of chemotherapy agents used: single-agent chemotherapy (SAC) or multi-agent chemotherapy (MAC). Though the NCDB does not record names of chemotherapy drugs used, SAC most likely indicates use of TMZ, whereas MAC most likely indicates PCV. These are the only two regimens suggested by national guidelines in the primary setting [15]. Patients were excluded in the settings of palliation, incomplete RT and/or chemotherapy treatment details, and unknown follow-up time. Information collected on each patient broadly included demographic data, comorbidity information, clinicopathologic tumor parameters, and treatment facility characteristics. An Academic Comprehensive Cancer Program was one that provides postgraduate medical education in at least four program areas and reports more than 500 newly diagnosed cancer cases each year. All other facility types, including Comprehensive Community Cancer Programs, Community Cancer Programs, and Integrated Network Cancer Programs were classified as non-academic. The patient’s county was categorized as metropolitan (population greater than 50,000 people), urban (population between 2500 and 49,999 people), or rural (population less than 2,500 people) using a classification scheme created by the United States Department of Agriculture Economic Research Service [25]. Patient comorbidity was recorded by the Charlson–Deyo comorbidity index and was recorded as 0, 1, or 2, with an increasing number indicating greater burden of comorbid conditions.
The primary endpoint was OS, defined as the interval between the date of diagnosis and the date of death or last contact, between patients treated with either SAC or MAC. Endpoints such as local control and cancer specific survival are not recorded in the NCDB. Fisher’s exact or χ2 test analyzed categorical proportions between groups in the non-parametric and parametric settings, respectively. Multivariable logistic regression modeling was utilized to determine characteristics that were predictive for receipt of MAC. Multivariate analyses as part of Cox proportional hazards modeling were additionally used to identify variables associated with OS. The Kaplan–Meier method was used for survival analysis, and comparisons between groups receiving treatment with SAC versus those receiving treatment with MAC were performed with the log-rank test. In order to ensure adequate follow-up time, only patients diagnosed between 2004 and 2007 were included in the survival analysis. Utilization of MAC and SAC over time was plotted using a line graph. All statistical tests were two-sided, with a threshold of p ≤ 0.05 for statistical significance, and were done using STATA (version 14, College Station, TX).
Results
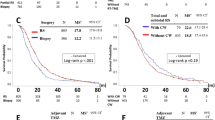
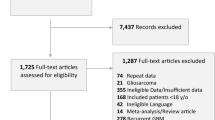
A complete flow diagram of patient selection is illustrated in Fig. 1. The most notable finding therein was that of the 1029 total patients, a great majority (n = 989, 96.1%) received SAC, whereas just 3.9% (n = 40) received MAC. When examining rates of MAC delivery from 2004 to 2012, there were yearly fluctuations; the final 3 years of the study period were arguably the most consistent in terms of lower rates of MAC utilization (Fig. 2).
Table 1 displays that there were no statistical differences in several clinical and treatment characteristics of patients receiving SAC and MAC, including age, comorbidity score, and socioeconomic parameters. Multivariable logistic regression was performed to address independent predictors of MAC receipt (Supplementary Table 1). Patients treated in more recent years (2010–2012) were less likely to receive MAC (p = 0.029). Moreover, non-private health insurance (Medicare, Medicaid, and uninsured) independently predicted for MAC administration (p < 0.05 for each).
Figure 3 illustrates Kaplan–Meier survival analysis of patients receiving MAC- or SAC-based CRT, which did not show statistical differences (p = 0.861). Median OS in the respective groups were 45.3 and 59.2 months.
Multivariate Cox proportional hazards modeling identified predictors of worse OS in the patient population, which included age >40, Charlson–Deyo comorbidity score of 2, other governmental/unrecorded insurance status, biopsy only, astrocytoma histology, and lower income (Table 2). Of note, use of MAC versus SAC was not associated with OS (hazard ratio 1.198, 95% CI 0.618–2.320, p = 0.804).
Discussion
Owing to the sheer lack of studies examining practice patterns and outcomes of MAC versus SAC in the setting of multimodal treatment for LGG, reporting of such data is essential. To our knowledge, this is the first such investigation; despite the obvious dearth of patients receiving MAC, there are several reflections to be gleaned. First, despite the deficiency of comparative data, there is a strikingly high rate of SAC utilization in the United States, likely a result of strong clinician preference, as seen in other reports [13]. Second, there were no differences in OS between patients receiving SAC and MAC, nor did this factor impact OS on multivariate analysis, suggesting that substitution of MAC with SAC for management of LGG may be reasonable. Third, the most important factors independently predicting for SAC administration were more recent treatment years (2010–2012) and private health insurance.
Although notably limited by the sample size comparisons, similar OS between groups echoes data suggesting equivalence between TMZ and PCV in high-grade gliomas in various clinical circumstances [3, 9,10,11]. Collectively, the amount evidence that is possible in such retrospective investigations suggests that substituting TMZ for PCV is safe and efficacious without proof of a compromise in OS, although direct recommendations to use TMZ over PCV cannot be made with this analysis. Though the ALLIANCE-N0577-CODEL will provide answers regarding the efficacy of TMZ compared to PCV [26], it will be many years before this study will provide meaningful conclusions, and in the current setting, providing retrospective data is important. However, it is predictably questioned whether these data would affect the already high rate of SAC delivery (especially in recent years), as exemplified by this report.
Additionally, a foremost goal of oncology is to discern socioeconomic disparities in delivery of cancer care. In this investigation, the independent correlation between non-private insurance status and an increased tendency to receive MAC cannot be overlooked. Because TMZ can be substantially less toxic than PCV, together with the novel findings of similar OS as observed herein, there are health policy implications of this association. Specific causes of non-private insurance associating with MAC is unknown but potentially relates to substandard insurance coverage of TMZ in certain regions. If true, the lack of comparative data between TMZ and PCV—in terms of both outcomes and toxicities—could be highly imperative to providing greater coverage for TMZ by various payers. In turn, more universal coverage of TMZ, owing to greater available data supporting equivalent efficacy and reduced toxicities, could reduce clinical adverse effects in a broader and socioeconomically diverse patient population.
The management of LGGs continues to be in flux based on the rise of molecular profiling of these neoplasms, and as such, the conclusions made in this and other studies of LGGs may need to be revised based on further genomic findings [27]. For instance, emerging data suggest that LGGs with wild-type IDH expression may experience similar OS as glioblastomas with IDH mutations [27], and that LGGs can be divided into high-, intermediate- and low-risk prognostic groups based on their IDH mutation, 1p/19q codeletion, and TERT mutation statuses [28]. Though it is too premature to assume changes in management based on these genomic signatures at this time, retrospective analyses of completed trials yields noteworthy data. For instance, in an analysis of the EORTC 22033 study, examining the subset of LGGs harboring IDH mutations and non-codeletions revealed that RT produced higher OS when comparing to TMZ [21]. This example highlights the fact that it could be likely that various molecular subgroups of LGGs may indeed require diverse interventions, leading to the necessity of major revisions regarding current management options.
The two most obvious limitations of this work are the aforementioned limited sample size of patients receiving MAC, as well as the central assumption when making a parallel between MAC and PCV as well as SAC and TMZ. It is possible that some patients receiving multi-agent chemotherapy as recorded in the NCDB received only PC, and Vincristine was dropped in order to offer patients a less toxic treatment. As mentioned before, TMZ and PCV are the two default chemotherapeutic regimens of choice for primary LGGs [15], and the lack of named CT agents is a limitation of any NCDB study. Nevertheless, it does not take away from the necessity for other corroborative work to reinforce the hypotheses-generating conclusions presented herein. Additionally, the retrospective methodology and potential for selection bias does not substitute for prospective data. Second, precise reasons for specific CT regimen utilization in each patient are difficult to discern, which is a concern of any retrospective study. There were no differences in Charlson Deyo indices, but this is not known to be synonymous with performance status. Third, the NCDB also does not provide further important details, such as Karnofsky performance status in a majority of patients, radiotherapy field design/volumes/techniques, and CT dose/cycles received. Importantly, it also does not record subsequent courses of therapy in cases of recurrence (e.g., retreatment with CT, RT and/or targeted agents). Specific molecular/genomic signatures of LGGs are also not captured by the NCDB. Lastly, the NCDB offers no data on recurrence and other survival parameters; most importantly, progression-free survival and cancer-specific mortality are also not included. This information is essential to make a determination on the value of CT regimen in this patient population.
Conclusions
The large majority of patients with LGGs receiving CRT receive SAC, with just 4% receiving MAC. Non-private health insurance (Medicaid, Medicare, and no insurance) independently predicted for receipt of MAC, and more recent treatment years (2010–2012) of receiving SAC. There were no observed differences in OS in patients receiving SAC and MAC, and chemotherapy regimen did not independently predict for OS, suggesting that the practice of substituting MAC with SAC for management of LGG may not adversely affect outcome.
References
Pouratian N, Schiff D (2010) Management of low-grade glioma. Curr Neurol Neurosci Rep 10:224–231
Buckner JC, Shaw EG, Pugh SL et al (2016) Radiation plus procarbazine, CCNU, and vincristine in low-grade glioma. N Engl J Med 374:1344–1355
Brandes AA, Nicolardi L, Tosoni A et al (2006) Survival following adjuvant PCV or temozolomide for anaplastic astrocytoma. Neuro Oncol 8:253–260
Rinne ML, Wen PY (2015) Treating anaplastic oligodendrogliomas and WHO grade 2 gliomas: PCV or temozlomide? The case for temozolomide. Oncology 29:265–275
van den Bent MJ (2015) Chemotherapy for low-grade glioma: when, for whom, which regimen? Curr Opin Neurol 28:633–638
O’Reilly SM, Newlands ES, Glaser MG et al (1993) Temozolomide: a new oral cytotoxic chemotherapeutic agent with promising activity against primary brain tumors. Eur J Cancer 29A:940–942
Stupp R, Mason WP, van den Bent MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996
Stupp R, Hegi ME, Mason WP et al (2009) Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomized phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 10:459–466
Brada M, Stenning S, Gabe R et al (2010) Temozolomide versus procarbazine, lomustine, and vincristine in recurrent high-grade glioma. J Clin Oncol 28:4601–4608
Wick W, Hartmann C, Engel C et al (2009) NOA-04 randomized phase III trial of sequential radiochemotherapy of anaplastic glioma with procarbazine, lomustine, and vincristine or temozolomide. J Clin Oncol 27:5874–5880
Wick W, Roth P, Hartmann C et al (2016) Long-term analysis of the NOA-04 randomized phase III trial of sequential radiochemotherapy of anaplastic glioma with PCV or temozolomide. Neuro Oncol 18:1529–1537
Ziu M, Kalkanis SN, Gilbert M et al (2015) The role of initial chemotherapy for the treatment of adults with diffuse low grade glioma: a systematic review and evidence-based clinical practice guidelines. J Neurooncol 125:585–607
Field KM, Rosenthal MA, Khasraw M et al (2016) Evolving management of low grade glioma: no consensus amongst treating clinicians. J Clin Neurosci 23:81–87
Fisher BJ, Hu C, Macdonald DR et al (2015) Phase 2 study of temozolomide-based chemoradiation therapy for high-risk low-grade gliomas: preliminary results of radiation therapy oncology group 0424. Int J Radiat Oncol Biol Phys 91:497–504
National Comprehensive Cancer Network (2016) Central nervous system cancers. Version 1. https://www.nccn.org/professionals/physician_gls/pdf/cns.pdf. Accessed 9 Dec 2016
van den Bent MJ, Chinot O, Boogerd W et al (2003) Second-line chemotherapy with temozolomide in recurrent oligodendroglioma after PCV (procarbazine, lomustine and vincristine) chemotherapy: EORTC Brain Tumor Group phase II study 26972. Ann Oncol 14:599–602
Pace A, Vidiri A, Galie E et al (2003) Temozolomide chemotherapy for progressive low-grade glioma: clinical benefits and radiological response. Ann Oncol 14:1722–1726
Hoang-Xuan K, Capelle L, Kujas M et al (2004) Temozolomide as initial treatment for adults with low-grade oligodendrogliomas or oligoastrocytomas and correlation with chromosome 1p deletions. J Clin Oncol 22:3133–3138
Kaloshi G, Benouaich-Amiel A, Diakite F et al (2007) Temozolomide for low-grade gliomas: predictive impact of 1p/19q loss on response and outcome. Neurology 68:1831–1836
Wahl M, Phillips JJ, Molinaro AM et al (2016) Chemotherapy for adult low-grade gliomas: clinical outcomes by molecular subtype in a phase II study of adjuvant temozolomide. Neuro Oncol 19:242–251
Baumert BG, Hegi ME, van den Bent et al (2016) Temozolomide chemotherapy versus radiotherapy in high-risk low-grade glioma (EORTC 22033-26033): a randomized, open-label, phase 3 intergroup study. Lancet Oncol 17:1521–1532
Kesari S, Schiff D, Drappatz J et al (2009) Phase II study of protracted daily temozolomide for low-grade gliomas in adults. Clin Cancer Res 15:330–337
Quinn J, Reardon D, Friedman A et al (2003) Phase II trial of temozolomide in patients with progressive low-grade glioma. J Clin Oncol 21:646–651
Bilimoria K, Stewart A, Winchester D, Ko C (2008) The National Cancer Data Base: a powerful initiative to improve cancer care in the United States. Ann Surg Oncol 15:683–690
United States Department of Agriculture (2016) Rural-urban continuum codes. https://www.ers.usda.gov/data-products/rural-urban-continuum-codes. Accessed 16 Dec 2016
National Cancer Institute (2016) Radiation therapy or radiation therapy and temozolomide in treating patients with newly diagnosed anaplastic glioma or low grade glioma. https://www.cancer.gov/about-cancer/treatment/clinical-trials/search/view?cdrid=640442. Accessed 12 Dec 2016
Verma V, Mehta MP (2016) Clinical ramifications of “genomic staging” of low-grade gliomas. J Neurooncol 129:195–199
Eckel-Passow JE, Lachance DH, Molinaro AM et al (2015) Glioma groups based on 1p/19q, IDH, and TERT promoter mutations in tumors. N Engl J Med 372:2499–2508
Funding
There was no research support for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflicts of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Haque, W., Verma, V., Butler, E.B. et al. Patterns of care and outcomes of multi-agent versus single-agent chemotherapy as part of multimodal management of low grade glioma. J Neurooncol 133, 369–375 (2017). https://doi.org/10.1007/s11060-017-2443-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-017-2443-7