Abstract
The purpose of this study was to identify changes in presentation, treatment and outcomes of older patients with low-grade glioma (LGG) over the past 50 years. 94 adults aged 55 or older upon diagnosis of a WHO grade II LGG at Mayo Clinic between 1960 and 2011 were included and grouped by those diagnosed before (group I: 1960–1989) and after (group II: 1990–2011) the routine use of post-operative MRI. Median follow-up was 11.4 years. Pathologic diagnoses included astrocytoma in 55%, mixed oligoastrocytoma in 18% and oligodendroglioma in 27%. Gross total resection (GTR) was achieved in 10%, radical subtotal resection (rSTR) in 6%, subtotal resection (STR) in 20% and biopsy only in 64%. Post-operative radiotherapy (PORT) was given in 77%. More patients in the modern era received GTR/rSTR (20 vs. 7%), though the difference was not statistically significant. Median progression-free survival (PFS) was 3.0 years, with 5- and 10-year PFS rates of 31 and 10%, respectively. Median, 5- and 10-year overall survival (OS) was 4.1 years, 43 and 17%, respectively. PFS and OS did not improve in the modern era. Factors negatively associated with PFS on multivariate analysis included astrocytoma histology, contrast enhancement and STR/biopsy. Factors associated with poor OS on multivariate analysis included astrocytoma histology, deep location, contrast enhancement and STR/biopsy. Despite reports of improving outcomes for younger patients treated in the modern era, outcomes have not significantly improved for older patients. Further efforts to improve outcomes based on molecular genotyping are needed to determine a rational strategy for treatment intensification.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Low-grade gliomas (LGG) are defined as WHO grade I or II primary brain tumors often seen in younger patients [1]. Because of the uncommon nature of this disease, only a small number of prospective, randomized trials have been conducted [2, 3]. Consequently, prognostic factors and treatment recommendations are often based on retrospective reviews and expert opinion [4, 5].
Age has been established as an adverse prognostic factor by several studies [6–8]. While different age cutoffs have been proposed, our previous report of patients aged at least 55 years treated between 1960 and 1992 demonstrated poor outcomes in this cohort of patients [9]. Here, we expand our previous report with long-term follow-up in patients diagnosed between 1960 and 2011. The goal of this study was to evaluate changes in prognosis, treatment and outcomes in older adults with LGG over the past 50 years.
Materials and methods
This study was approved by the Mayo Clinic Institutional Review Board. Records from 852 adults diagnosed with a grade II glioma between 1960 and 2011 were reviewed. Of these, 94 were aged 55 of older and included in our analysis. While no modern, central pathologic review was performed, all diagnoses were confirmed by a Mayo Clinic neuropathologist. Patients were grouped by those who received a diagnosis before (group I: 1960–1989) and after (group II: 1990–2011) the routine use of postoperative MRI for adult LGGs at Mayo Clinic.
The extent of surgical resection was defined by postoperative imaging and operative reports if imaging was unavailable or not performed. Gross total resection (GTR) was defined as no evidence of remaining tumor after resection. Radical subtotal resection (rSTR) was defined as ≥90% of the tumor removed with some suspicion of residual tumor left behind. Subtotal resection (STR) was defined as <90% of tumor removed with an attempt at debulking. If no attempt was made to debulk the tumor, the procedure was classified as biopsy only (Bx).
Tumors were graded in accordance with WHO standards and recorded retrospectively from the original pathology reports. Grade I tumors were excluded from analysis. Grade II tumors included were diffuse and gemistocytic astrocytomas, oligodendrogliomas, and mixed oligoastrocytomas. Disease progression was determined by clinical assessment, imaging reports, pathology studies or the initiation of additional tumor-directed therapies. IDH status was not routinely reported. Nine patients had 1p/19q codeletion testing performed and six had a confirmed codeletion. Due to the limited number of patients with known 1p/19q codeletion status, it was not used as a prognostic factor in univariate or multivariate analyses.
Prognostic factors related to overall survival (OS) and progression-free survival (PFS) were determined using univariate and multivariate analyses. Factors tested were chosen based on their significance in previous studies [4–9]. ECOG performance status was retrospectively captured from review of medical records with enough detail to accurately perform a classification. PFS and OS curves were constructed using the Kaplan–Meier method and compared using the log-rank test. Multivariate analysis utilized the Cox proportional hazards model. Patients who died without documented recurrence were censored for recurrence at the time of death. All statistical significance tests were 2-tailed.
Results
Of the 852 adults diagnosed with LGG in our database, 94 were aged 55 or older. Median follow-up was 11.4 years overall, not reached in group I and 10.8 years in group II (p = 0.001). Patient characteristics are summarized in Table 1. The median age at diagnosis was 63.7 years. Most of the patients were male (59%). Overall, most patients presented with seizures (65%) or sensorimotor symptoms (53%). Fewer patients presented with headaches in the modern era (8 vs. 39%, p = 0.0003).
Gross total resection (GTR) was achieved in 9.6%, radical subtotal resection (rSTR) in 6.4%, subtotal resection (STR) in 20.2% and biopsy only in 63.8%. More patients in the modern era received GTR/rSTR (19.7 vs. 7.1%), though the difference was not statistically significant (p = 0.11). ECOG performance status was not associated with extent of resection (p = 0.13). Pathologic diagnoses included astrocytoma in 55%, mixed oligoastrocytoma in 18% and oligodendroglioma in 27%. Significantly fewer patients were diagnosed with pure astrocytomas in the modern group (71 vs. 49%), which corresponded to an increase in mixed oligoastrocytoma diagnoses (4 vs. 36%). Fewer patients in the modern group received RT alone (64 vs. 75%), which corresponded to a significant increase in the use of chemoradiotherapy (14 vs. 0%). Chemotherapy included temozolomide (TMZ) in nine patients and BCNU in two patients.
More patients with oligodendroglial tumors underwent GTR (24%) compared with pure astrocytomas (10%; p = 0.06). There was no correlation with tumor size (p = 0.50) or location (p = 0.93) and frequency of GTR/rSTR. Similarly, there was no correlation between symptoms at diagnosis and frequency of GTR/rSTR (all p > 0.05). PORT was predominantly delivered in patients undergoing STR or biopsy (84%) compared with patients undergoing GTR/rSTR (33%; p < 0.0001). No relationship between performance status (p = 0.24), tumor size (p = 0.89) or histology (p = 0.13) and delivery of PORT was seen.
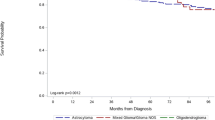
Median progression-free survival (PFS) was 3.0 years. At 5 and 10 years, PFS was 31 and 10%, respectively. Median PFS was similar between group I (2.1 years) and group II (3.3 years; p = 0.49). Kaplan–Meier curves for PFS are shown in Fig. 1. Factors associated with PFS on univariate analysis (Table 2) included ECOG performance status 0–1 (RR 0.44, 95% CI 0.24–0.81, p = 0.01), sensory/motor symptoms (RR 1.89, 95% CI 1.2–3.0, p = 0.01), astrocytoma histology (RR 2.41, 95% CI 1.5–3.9, p = 0.0002) contrast enhancement (RR 2.38, 95% CI 1.3–4.3, p = 0.01) and GTR/rSTR (RR 0.48, 95% CI 0.21–0.93, p = 0.03). Kaplan–Meier curves depicting PFS based on histology and extent of resection are shown in Fig. 2. On multivariate analysis (Table 3), astrocytoma histology (RR 2.40, 95% CI 1.42–4.09, p = 0.001), contrast enhancement (RR 2.93, 95% CI 1.46–5.80, p = 0.003) and GTR/rSTR (RR 0.35, 95% CI 0.14–0.79, p = 0.01) remained statistically significantly associated with PFS.
Demonstrates changes in OS (a) and PFS (b) in years based on histology. The blue lines indicate astrocytic histology compared with ologoastrocytoma or oligodendroglioma in red. In addition, this figure shows OS (c) and PFS (d) in years based on extent of resection. The blue lines indicate GTR/rSTR compared with STR/Bx in red
Median, 5- and 10-year overall survival (OS) was 4.1 years, 43 and 17%, respectively. Median OS was similar between group I (2.8 years) and group II (4.7 years; p = 0.49). Kaplan–Meier curves for OS are shown in Fig. 1. Factors associated with OS on univariate analysis (Table 2) included ECOG performance status 0–1 (RR 0.38, 95% CI 0.21–0.69, p = 0.002), astrocytoma histology (RR 2.29, 95% CI 1.4–3.8, p = 0.001), deep location (RR 1.76, 95% CI 1.0–2.9, p = 0.04), contrast enhancement (RR 2.98, 95% CI 1.6–5.5, p = 0.001), GTR/rSTR (RR 0.30, 95% CI 0.1–0.7, p = 0.002) and PORT (RR 1.9, 95% CI 1.1–3.6, p = 0.03). Kaplan–Meier curves depicting OS based on histology and extent of resection are shown in Fig. 2. On multivariate analysis for OS (Table 3), astrocytoma histology (RR 2.76, 95% 1.60–4.88, p = 0.0003), deep location (RR 1.97, 95% CI 1.05–3.64, p = 0.04), contrast enhancement (RR 3.98, 95% CI 1.92–8.09, p = 0.0003) and GTR/rSTR (RR 0.22; 95% CI 0.07–0.56, p = 0.001) remained statistically significant.
Discussion
In this study, we assessed outcomes for a large series of older adults diagnosed with LGG over the past five decades. In contrast to our prior study of all adults diagnosed with LGG with a median survival of 8.0 years, outcomes were poor in the older adults selected for this study [10]. While many conventional prognostic factors remained significant in our analysis, the benefit of adjuvant therapy was not seen. In addition, no significant improvement in outcomes was seen over time despite the use of modern treatment techniques. This ultimately raises questions about the optimal treatment paradigm for this population of patients.
In this series, achieving GTR/rSTR was the only treatment-related prognostic factor that remained significant on multivariate analysis. This is consistent with prior retrospective studies [7, 11]. In a modern series by Claus et al., patients who underwent STR had an increase in the risk of disease recurrence of 1.4 times, and a 4.9 times increase in the risk of death compared with GTR [12]. In a study of high-grade gliomas in eloquent areas of the brain, resecting at least 90% of the tumor resulted in significantly improved 5-year OS of 93% compared with 41% in patients with less than 70% of the tumor resected [13]. Ultimately, a major driving factor in the poor outcomes reported here may very well be that only a minority of patients in the present study underwent GTR/rSTR.
In our prior study of all LGG patients, those treated with modern techniques had longer survival [5]. In the present study, no such improvement was seen. While more patients in the modern era received GTR/rSTR, only a small proportion of our population underwent GTR/rSTR. As the frequency of STR decreased, the rate of biopsy alone significantly increased. It is possible that modern imaging allowed surgeons to better assess extent of disease and more accurately estimate functional deficits after resection, which in turn could have persuaded surgeons away from incomplete and highly morbid resections. Compared with our prior publication of all adults with LGG, the rate of GTR was lower in this series (10 vs. 25%; p < 0.0001). While there was no significant difference in the frequency of deep tumors (p = 0.35), older adults were more likely to have sensorimotor symptoms (p < 0.001), which could have limited enthusiasm for extensive resections in eloquent areas of the brain. Taken together, our data suggests the strategy of maximal safe resection utilized in younger patients may be important in the optimal treatment of older adults as well.
In our cohort, the majority of patients undergoing STR or biopsy received adjuvant radiotherapy whereas a smaller proportion received adjuvant radiotherapy after GTR/rSTR. The effect of adjuvant radiotherapy in the general LGG population was evaluated in a large, randomized, prospective trial in EORTC 22845. The trial randomized patients to receive 54 Gy of radiotherapy immediately after surgery or at the time of progression. Early radiotherapy significantly improved seizure control and PFS, but not OS [14]. Because the present study was not randomized, it is possible that confounding variables have overshadowed the impact of radiotherapy. Specifically, the patients selected to receive adjuvant radiotherapy tended to have less extensive resections and may have fared worse without adjuvant therapy.
The changing histologic classifications over time reported here are not unique to our study [15]. Histologic classification of low-grade glioma can be quite complex and is subject to significant interobserver variability [16]. There exists a growing body of literature establishing the prognostic significance of molecular classifiers in gliomas [17, 18]. In the seminal paper by Eckel-Passow and colleagues, patients were retrospectively classified based on the presence or absence of TERT mutation, IDH mutation and 1p/19q codeletions [18]. They found that tumors with solely TERT mutations were more often seen in older patients and that survival of grade II and III gliomas with solely TERT mutations was dismal. In a study by The Cancer Genome Atlas Research Network (TCGA), grade II and III gliomas were classified based on a comprehensive, integrative analysis of 293 tissue specimens using advanced molecular platforms [17]. They ultimately found that prognosis was more accurately predicted by IDH, 1p/19q and TP53 status than by histologic classification, and that tumors with wild type IDH had genomic aberrations and clinical outcomes similar to glioblastoma. Prospective data using molecular classifiers to guide treatment decisions are beginning to emerge. The German Glioma Network (GGN) reported a small, prospective cohort of patients classified by IDH, 1p/19q and TERT mutation status, confirming a higher proportion of IDH wild type classification in older patients, along with worse survival for this group [19]. In EORTC 22033–26033, patients with high-risk low-grade gliomas were randomized to receive either conformal radiotherapy or dose-dense temozolomide [20]. Although there was no significant difference in PFS overall, patients with IDH mutations and intact 1p/19q had better PFS when treated with radiotherapy. In the TCGA, EORTC and GGN studies, patients with wild type IDH were more often older than those with IDH mutations, again confirming the molecular underpinnings of the bleak prognosis and unique clinical challenge of treating older adults with LGG.
In light of the recently published long-term results from RTOG 9802 and 0424, it is possible that our lack of benefit seen with adjuvant chemotherapy is driven by the small number of patients who received chemotherapy. In RTOG 9802, LGG patients older than 40 years of age or those with a subtotal resection were randomized to receive adjuvant radiotherapy alone or adjuvant radiotherapy followed by six cycles of procarbazine, lomustine and vincristine (PCV). The addition of chemotherapy significantly improved median OS to 13.3 years compared with 7.8 years without chemotherapy, with the greatest benefit seen in patients with oligodendroglial tumors [21]. Our cohort of patients would have qualified for inclusion in the trial, so it is likely that our limited proportion of patients receiving chemotherapy (12% overall; none receiving PCV) limited our ability to detect a benefit to its use. However, given that our group predominantly had astrocytic tumors that would be expected to benefit the least from PCV, the more favorable toxicity profile of TMZ may have been attractive. Moreover, many patients in our group would have qualified for RTOG 0424, the phase II trial of TMZ-based chemoradiotherapy with encouraging 3-year OS of 73% [22]. While RTOG 9802 and 0424 support the use of chemotherapy in high-risk patients with LGG, the optimal regimen for older patients remains to be determined. Further efforts to individualize care based on molecular genotyping will be important to determine a rational strategy for treatment intensification in this subgroup.
This study has several important limitations, many of which are related to its retrospective nature. First, because treatment decisions are often made in the context of all available clinical information, adjuvant therapies were delivered based on the presence of adverse prognostic factors. Thus, it is difficult to draw conclusions from these data regarding the benefit of adjuvant therapy, as the group receiving adjuvant treatment was not balanced with respect to the group observed postoperatively. Second, genetic testing was not routinely performed for the majority of patients and consequently IDH1, 1p/19q, TERT and TP53 classifications are not known. Third, a neurosurgeon’s impression of the extent of tumor resected tends to be unreliable, although our prior study revealed a high degree of concordance between the surgeon’s impression and postoperative imaging at our institution [4, 5, 23]. However, the early cohort presented here did not have postoperative MRI and consequently the true extent of resection may have been overestimated. Additionally, there remains the possibility of under-sampling the tumor in patients with incomplete resections or solely biopsies, leading to a diagnosis of grade II glioma when components of grade III or IV disease could be present. Furthermore, no central pathologic review was performed. This has the potential to influence the results, as it is well established that significant interobserver variation exists in the pathologic classification of gliomas [16]. Lastly, our study has no long-term quality of life (QOL), patient reported outcomes (PRO) or toxicity data. A longitudinal assessment of QOL and PRO would be particularly useful to determine whether or not adjuvant therapy results in any meaningful improvement in these domains, particularly in light of the improved seizure control with radiotherapy reported in EORTC 22845 [14].
Conclusion
In summary, this is a large retrospective series of adults aged 55 years or older with a newly-diagnosed WHO grade II glioma at a single institution between 1960 and 2011. While the frequency of GTR/rSTR increased slightly with time, fewer surgeons are attempting STR and more proceed with biopsy alone in the modern era. Despite advances in modern surgery, radiotherapy and chemotherapy, outcomes remain poor and have not substantially improved with time. In fact, the natural history reported here bears striking similarity to anaplastic tumors. As we enter the molecular era of glioma classification, improved treatment strategies are needed for older adults with aggressive low-grade gliomas.
References
Louis DN, Ohgaki H, Wiestler OD et al (2007) The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 114:97–109
Shaw EG, Wang M, Coons SW et al (2012) Randomized trial of radiation therapy plus procarbazine, lomustine, and vincristine chemotherapy for supratentorial adult low-grade glioma: initial results of RTOG 9802. J Clin Oncol 30:3065–3070
Karim AB, Maat B, Hatlevoll R et al (1996) A randomized trial on dose-response in radiation therapy of low-grade cerebral glioma: European Organization for Research and Treatment of Cancer (EORTC) Study 22844. Int J Radiat Oncol Biol Phys 36:549–556
Youland RS, Brown PD, Giannini C, Parney IF, Uhm JH, Laack NN (2013) Adult low-grade glioma: 19-year experience at a single institution. Am J Clin Oncol 36:612–619
Youland RS, Schomas DA, Brown PD et al (2013) Changes in presentation, treatment, and outcomes of adult low-grade gliomas over the past 50 years. Neuro Oncol 15:1102–1110
Bauman G, Lote K, Larson D et al (1999) Pretreatment factors predict overall survival for patients with low-grade glioma: a recursive partitioning analysis. Int J Radiat Oncol Biol Phys 45:923–929
Pignatti F, van den Bent M, Curran D et al (2002) Prognostic factors for survival in adult patients with cerebral low-grade glioma. J Clin Oncol 20:2076–2084
Leighton C, Fisher B, Bauman G et al (1997) Supratentorial low-grade glioma in adults: an analysis of prognostic factors and timing of radiation. J Clin Oncol 15:1294–1301
Schomas DA, Laack NN, Brown PD (2009) Low-grade gliomas in older patients: long-term follow-up from Mayo Clinic. Cancer 115:3969–3978
Youland RS, Khwaja SS, Schomas DA, Keating GF, Wetjen NM, Laack NN (2013) Prognostic factors and survival patterns in pediatric low-grade gliomas over 4 decades. J Pediatr Hematol Oncol 35:197–205
Janny P, Cure H, Mohr M et al (1994) Low grade supratentorial astrocytomas. Management and prognostic factors. Cancer 73:1937–1945
Claus EB, Horlacher A, Hsu L et al (2005) Survival rates in patients with low-grade glioma after intraoperative magnetic resonance image guidance. Cancer 103:1227–1233
Ius T, Isola M, Budai R et al (2012) Low-grade glioma surgery in eloquent areas: volumetric analysis of extent of resection and its impact on overall survival. A single-institution experience in 190 patients: clinical article. J Neurosurg 117:1039–1052
van den Bent MJ, Afra D, de Witte O et al (2005) Long-term efficacy of early versus delayed radiotherapy for low-grade astrocytoma and oligodendroglioma in adults: the EORTC 22845 randomised trial. Lancet 366:985–990
Claus EB, Black PM (2006) Survival rates and patterns of care for patients diagnosed with supratentorial low-grade gliomas: data from the SEER program, 1973–2001. Cancer 106:1358–1363
Coons SW, Johnson PC, Scheithauer BW, Yates AJ, Pearl DK (1997) Improving diagnostic accuracy and interobserver concordance in the classification and grading of primary gliomas. Cancer 79:1381–1393
Brat DJ, Verhaak RG, Aldape KD et al (2015) Comprehensive, integrative genomic analysis of diffuse lower-Grade gliomas. N Engl J Med 372:2481–2498
Eckel-Passow JE, Lachance DH, Molinaro AM et al (2015) Glioma groups based on 1p/19q, IDH, and TERT promoter mutations in tumors. N Engl J Med 372:2499–2508
Weller M, Weber RG, Willscher E et al (2015) Molecular classification of diffuse cerebral WHO grade II/III gliomas using genome- and transcriptome-wide profiling improves stratification of prognostically distinct patient groups. Acta Neuropathol 129:679–693
Baumert BG, Hegi ME, van den Bent MJ et al (2016) Temozolomide chemotherapy versus radiotherapy in high-risk low-grade glioma (EORTC 22033–26033): a randomised, open-label, phase 3 intergroup study. Lancet Oncol 17:1521–1532
Buckner JC, Shaw EG, Pugh SL et al (2016) Radiation plus procarbazine, CCNU, and vincristine in low-grade glioma. N Engl J Med 374:1344–1355
Fisher BJ, Hu C, Macdonald DR et al (2015) Phase 2 study of temozolomide-based chemoradiation therapy for high-risk low-grade gliomas: preliminary results of Radiation Therapy Oncology Group 0424. Int J Radiat Oncol Biol Phys 91:497–504
Shaw EG, Berkey B, Coons SW et al (2008) Recurrence following neurosurgeon-determined gross-total resection of adult supratentorial low-grade glioma: results of a prospective clinical trial. J Neurosurg 109:835–841
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Youland, R.S., Schomas, D.A., Brown, P.D. et al. Patterns of care and treatment outcomes in older adults with low grade glioma: a 50-year experience. J Neurooncol 133, 339–346 (2017). https://doi.org/10.1007/s11060-017-2439-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-017-2439-3