Abstract
Telomerase activation is critical in many cancers including central nervous system (CNS) tumors. Imetelstat is an oligonucleotide that binds to the template region of the RNA component of telomerase, inhibiting its enzymatic activity. We conducted an investigator-sponsored molecular biology (MB) and phase II study to estimate inhibition of tumor telomerase activity and sustained responses by imetelstat in children with recurrent CNS malignancies. In the MB study, patients with recurrent medulloblastoma, high-grade glioma (HGG) or ependymoma undergoing resection received one dose of imetelstat as a 2-h intravenous infusion at 285 mg/m2, 12–24 h before surgery. Telomerase activity was evaluated in fresh tumor from surgery. Post-surgery and in the phase II study, patients received imetelstat IV (days 1 and 8 q21-days) at 285 mg/m2. Imetelstat pharmacokinetic and pharmacodynamic studies were performed. Of two evaluable patients on the MB trial, intratumoral telomerase activity was inhibited by 95 % compared to baseline archival tissue in one patient and was inevaluable in one patient. Forty-two patients (40 evaluable for toxicity) were enrolled: 9 medulloblastomas, 18 HGG, 4 ependymomas, 9 diffuse intrinsic pontine gliomas. Most common grade 3/4 toxicities included thrombocytopenia (32.5 %), lymphopenia (17.5 %), neutropenia (12.5 %), ALT (7.5 %) and AST (5 %) elevation. Two patients died of intratumoral hemorrhage secondary to thrombocytopenia leading to premature study closure. No objective responses were observed. Telomerase inhibition was observed in peripheral blood mononuclear cells (PBMCs) for at least 8 days. Imetelstat demonstrated intratumoral and PBMC target inhibition; the regimen proved too toxic in children with recurrent CNS tumors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Telomeres are complexes consisting of tandem repeats of the TTAGGG DNA sequence with associated proteins and serve as protective caps for linear chromosomes. With each cell cycle, telomeres shorten until they reach a critical length that triggers cellular senescence or apoptosis [1]. This is counteracted by the activity of the telomerase enzyme. Human telomerase consists of at least two essential components, a protein catalytic subunit (hTERT) and an RNA template (hTERC) that contribute to the synthesis of telomeric repeats, thereby renovating telomeres.
Telomerase activation, a hallmark of the vast majority of cancers, is essential for maintaining an immortal phenotype by conferring unlimited replicative potential. While telomerase activity is undetectable in most normal tissues, it is increased in about 90 % of cancers [2, 3]. Telomerase activity has been detected in 10–100 % of anaplastic astrocytomas [3, 4], 26–100 % of glioblastoma [4] and 60–86 % of ependymomas [5, 6]. High hTERT expression occurs in up to 76 % of medulloblastoma/supratentorial primitive neuroectodermal tumors (PNET) [7] and 73 % of diffuse intrinsic pontine gliomas (DIPG) [8]. Telomerase activation is a negative prognosticator across CNS tumors [5, 8, 9] and may play a role in cancer stemness [5, 10, 11], making telomerase inhibition a rational therapeutic target even in the setting of cancer recurrence and therapy resistance.
Imetelstat (GRN163L, Geron Corporation), a covalently lipidated 13-mer-thiophosphoramidate oligonucleotide, targets hTERC and is a potent competitive inhibitor of the telomerase enzymatic activity [12]. It has demonstrated broad activity in vitro and in vivo in a variety of tumor types, including primary, stem-cell and metastatic compartments [5, 12, 13]. In single-agent early-phase adult clinical trials in variety of malignancies, imetelstat has shown the most impressive activity in myeloproliferative neoplasms [14, 15]. In a phase I pediatric solid tumor trial of imetelstat, the recommended phase II dose (RP2D) was determined as 285 mg/m2 on days 1 and 8 of a 21-day cycle with myelosuppression reported as the most common toxicity [16].
Here, we report a molecular biology (MB) and phase II study in children with recurrent CNS tumors. The primary objective of the MB study was to test the ability of imetelstat to inhibit telomerase activity assessed by telomere repeat amplification protocol (TRAP) intratumorally and in peripheral blood mononuclear cells (PBMCs) of children with recurrent medulloblastoma, high-grade glioma (HGG) or ependymoma undergoing surgical resection. The primary objective of the phase II study was to estimate the sustained objective response rates to imetelstat in children with recurrent CNS tumors.
Patients and methods
Patient eligibility
Common eligibility criteria for the MB and phase II study included patients aged ≥12 months to ≤21 years with measurable recurrent or refractory medulloblastoma/PNET (stratum A), HGG (stratum B), or ependymoma (stratum C). Patients with DIPG (stratum D) were only eligible for the phase II trial. Histologic verification of malignancy was required except in DIPG patients. Patients with imaging evidence of CNS hemorrhage, including punctate areas on baseline magnetic resonance imaging (MRI) obtained within 14 days prior to study enrollment, were ineligible. For the MB study, eligible patients included those for whom surgical resection was indicated and who were amenable to receiving one dose of imetelstat 12–24 h before surgery. Other eligibility criteria for both MB and phase II studies included: Lansky or Karnofsky performance score ≥50; recovery from acute toxicities of all prior therapy; ≥3 months since craniospinal radiation therapy (RT), ≥2 weeks since local palliative RT; ≥3 months since autologous stem cell transplantation; adequate bone marrow function (hemoglobin ≥8.0 g/dL, absolute neutrophil count ≥1000/mL, platelets ≥100,000/mL transfusion-independent defined as no platelet transfusions within a 7-day period prior to enrollment); adequate renal function (age-adjusted normal serum creatinine or glomerular filtration ≥70 mL/min/1.73 m2); adequate liver function (total bilirubin <2.0 mg/dL, ALT (SGPT) ≤3× institutional upper limit of normal [IULN], AST (SGOT) ≤3× IULN, alkaline phosphatase <2.5× IULN, albumin ≥2 g/dL); adequate coagulation (PTT <1.2× IULN). Patients were excluded if pregnant or lactating, had a known bleeding diathesis, were on systemic anticoagulants or had an uncontrolled concurrent illness. Informed consent and assent were obtained according to institutional guidelines. Institutional review boards of participating institutions maintained protocol approval throughout the study. After a patient with medulloblastoma died on study due to intratumoral bleeding associated with thrombocytopenia, the study was put on clinical hold by the food and drug administration (FDA), amended and reopened to exclude patients with medulloblastoma/PNET and to redefine transfusion independence for platelets as no transfusion requirement within 4 weeks prior to enrollment. Post-amendment changes for safety are outlined in the “Dose modifications” and “Study evaluations” sections.
Drug administration
Imetelstat sodium was supplied by Geron Corporation as a sterile lyophilized powder. It was reconstituted with 0.9 % sodium chloride to achieve a final drug concentration of 1 mg/ml for injection. On the phase II study, imetelstat was administered once on days 1 and 8 of every 21-day course as a 2-h infusion intravenously at 285 mg/m2. In the absence of disease progression or unacceptable toxicity, patients could receive up to 34 courses (2 years). On the MB study, imetelstat was administered once, 12–24 h prior to the anticipated time of surgery. Imetelstat was recommenced 14–21 days after surgery and then administered according to the phase II study schedule.
Dose modifications
Toxicity was graded according to the Common Terminology Criteria for Adverse Events (CTCAE) version 4.0. Hematologic dose-limiting toxicity (DLT) was defined as: grade 4 thrombocytopenia or neutropenia; grade 3 thrombocytopenia requiring a platelet transfusion on >2 occasions within a 14-day period; myelosuppression leading to >7 days delay between treatment courses; ≥grade 3 PTT prolongation. Non-hematologic DLT was defined as any grade 3 or 4 non-hematological toxicity excluding: grade 3 nausea and vomiting controlled with antiemetics, grade 3 transaminase elevation that returned to eligibility criteria within 7 days of drug interruption and did not recur upon re-challenge, grade 3 fever or infection, grade 3 electrolyte imbalance responsive to oral supplementation; any non-hematologic toxicity that caused ≥7 days delay between courses or led to omission of the day 8 dose. After a patient with medulloblastoma died from an intratumoral hemorrhage related to thrombocytopenia, the protocol was amended to require the omission of day 8 imetelstat in patients with a platelet count ≤75,000/mm3 and dose reduction for subsequent courses.
Study evaluations
Pretreatment evaluations included history, physical examination, performance status, complete blood count (CBC), electrolytes, renal and liver function tests, coagulation profile and pregnancy test for female patients of childbearing age. For the MB study, during the surgical course, CBCs were obtained within 12 h prior to surgery, daily for 7 days post-operatively and twice weekly for the rest of the post-operative course. PTT was drawn Q6 h after the pre-surgery imetelstat dose until surgery was performed.
Following a patient death due to treatment-related thrombocytopenia, additional safety measures were implemented. For both MB and phase II studies, CBCs were obtained twice weekly and in the 24 h prior to the day 1 and day 8 imetelstat doses in each cycle. Platelets were kept ≥50,000/mm3 throughout treatment and a transfusion-independent platelet count of >75,000/mm3 was required on day 8 prior to drug administration. Electrolytes, renal and liver function tests and coagulation profiles were obtained within 24 h of day 1 and day 8 imetelstat doses in course 1 and prior to each course, thereafter. Disease evaluations were obtained at baseline, post-surgery (for patients on the MB arm) and after every third cycle, thereafter.
Response criteria
Tumor response was defined as follows: complete response: complete MRI disappearance of tumor with stable or decreasing corticosteroid dose maintained for ≥6 weeks; partial response, ≥50 % reduction in bi-dimensional tumor measurements with stable or decreasing corticosteroids dose, maintained for ≥6 weeks; progressive disease, worsening neurologic status or >25 % increase in the bi-dimensional measurements, new lesions, or increasing corticosteroid dose; stable disease (SD): response not meeting criteria for other categories, with stable neurologic examination and corticosteroid dose.
Pharmacokinetic studies
Pharmacokinetic studies were performed in consenting patients in the phase II study. Serial blood samples (2 mL) were obtained on course 1 day 1, before imetelstat administration, at the end of infusion (EOI), 4 (±1) and 24 (±2) h post-infusion. Plasma concentrations of imetelstat were measured by a validated hybridization-ELISA assay by Charles River Laboratories, Inc. (Wilmington, Massachusetts, USA) as previously described [16]. Imetelstat concentration–time data were summarized using descriptive statistics. For each pharmacokinetic study, the peak serum imetelstat concentration (Cmax) and time to Cmax (Tmax) were determined from the plasma concentration–time profile.
Telomerase activity in PBMCs and tumor
PBMCs were isolated from patients’ whole blood by density gradient centrifugation using Ficoll-Paque PLUS (GE Healthcare LifeSciences) according to the manufacturer’s instructions. PBMCs were collected before treatment, 6–8 h, and 24 (±2) h after the first imetelstat dose; prior to the day 8 dose; and before the day 1 dose in cycles 2 and 3. In the MB study, PBMCs were collected before treatment, at the time of surgery, and 72 (±6) h after the first imetelstat dose. Fresh flash-frozen tumor samples from archival tissue and time of surgery (20–50 mg) were collected. Tumor tissue was placed in ice-cold lysis buffer and mechanically homogenized using gentle MACS (Miltenyi, Cologne, Germany) program protein_01, centrifuged for 5 min at 330×g at 4 °C to pool the foamed sample. Samples were incubated in ice for 30 min and centrifuged for 20 min at 14,000×g at 4 °C. Supernatant was transferred to a sterile RNAse/DNAse-free tube and stored at −80 °C until assay was performed. PBMC and tumor extracts were analyzed for telomerase activity using the TRAPeze Telomerase Detection Kit (Millipore). Cell extracts were prepared according to protocols provided by the manufacturer. 400 ng (fresh tissue) and 800 ng (PBMCs) of total protein were assayed for telomerase activity.
Statistical considerations
For the MB study, to detect a decrease in telomerase activity rate from 80 % (if imetelstat inactive) to 30 % (if imetelstat active), 6 patients with detected telomerase on archival tissue were needed to achieve an attained power of 93 % with α of 3.3 %. Based on these criteria, if 4 or more of these 6 (67 %) subjects’ tissues demonstrated 50 % reduction in telomerase activity after surgical resection, this was to be considered promising evidence for biological activity. There was no reason to expect that the ability of imetelstat to inhibit telomerase activity was related to histology. Thus, the statistical analysis and inference for the MB study was planned as an overall comparison among subjects whose archival tumors demonstrated telomerase activity regardless of histology.
For the phase II trial, a Simon’s phase II minimax design with the identical parameters was used to investigate the sustained objective response rate (sORR) separately in each stratum. Imetelstat activity would be considered disappointing if the true, unknown sORR was ≤5 % and the design would have 90 % power to detect a true, unknown sORR of 0.25 with α = 10 %. With these parameters, the design would reject imetelstat at the first stage if none of the first 13 subjects experienced a sOR. Otherwise, the trial would continue to accrue a total of 20 evaluable subjects. Imetelstat would be considered active if at least 3 of 20 subjects experience a sOR. The response evaluation period was set as nine courses (27 weeks).
Results
Patient characteristics
Three patients, one each with medulloblastoma, HGG and ependymoma were enrolled on the MB study. The patient with ependymoma was inevaluable as he did not receive drug because of the FDA Clinical Hold. No peri-operative complications were observed among patients treated in the MB study. Both evaluable patients received three courses of therapy. Forty patients, 39 eligible, were enrolled on the phase II study. One patient with medulloblastoma was ineligible. The median number of courses was 1 (range: 1–3) in the phase II study. Table 1 summarizes the characteristics of the eligible patients on the MB and phase II studies.
Toxicity
All patients who received at least one dose of imetelstat were evaluable for toxicity. The most common grade 3/4 toxicities included thrombocytopenia (32.5 %), lymphopenia (17.5 %), neutropenia (12.5 %), ALT (7.5 %) and AST (5 %) elevation. Two patients died of intratumoral hemorrhage secondary to thrombocytopenia leading to premature study closure. Tables 2 and 3 summarize the number of adverse events (AE) >grade 2, attributed to therapy and observed in >10 % of evaluable patients in at least one stratum for the MB and phase II studies, respectively.
Responses
No objective responses were reported on this study. The study was placed on Clinical Hold by the FDA after the first treatment-related death (intratumoral hemorrhage secondary to thrombocytopenia in a medulloblastoma patient) and 15 patients were taken off study. Upon study resumption, none of the patients on the phase II arm remained on treatment long enough to be evaluable for SD because of the premature closure of the study following the second patient death.
Pharmacokinetics
Imetelstat plasma pharmacokinetic studies were performed in 10 patients on the phase II study. All patients received imetelstat 285 mg/m2 as a 2-hour infusion. The median age and body surface area (BSA) were 12.7 years (range: 2.3–19.3 years) and 1.58 m2 (range: 0.56–1.72 m2). The actual infusion start/stop times were not recorded and nominal times were assumed for collection of blood samples. Therefore, the Tmax occurred at 2 h for all patients as this was assumed to be the EOI time. The median maximum concentration (Cmax) was 97.5 µg/mL (range: 84–173 µg/mL).
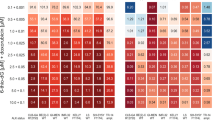
Telomerase inhibition in PBMCs
Baseline and/or post-treatment PBMC samples were submitted from 13 patients at various time points. If telomerase activity could not be assessed at baseline, the sample was considered inevaluable for assessment of telomerase activity following imetelstat treatment. Samples from six patients were consequently considered evaluable and were analyzed. Telomerase inhibition was observed in PBMCs of five out of six patients and was sustained for at least 8 days in all samples. Telomerase activity returned to baseline by day 21 post-imetelstat administration. Inhibition of telomerase activity at different time points in PBMCs and quantification of telomerase inhibition in one representative patient with HGG on the phase II study are shown in Fig. 1.
a Patient received imetelstat on days 1 and 8 in each 21-day cycle at 285 mg/m2. Total protein extracts were assayed for telomerase activity during course 1, day 1 pre-IMT (C1D1-pre); course 1, day 1 post-IMT (C1D1-post); course 1, day 2 (C1D2); course 1, day 8 (C1D8); course 2, day 1 pre-IMT (C2D1) and course 3, day 1 pre-IMT (C3D1). Telomerase activity was evaluated by TRAP assay using 800 ng of total protein extracted from PBMCs. Lanes labeled (−ve) and (+ve) depict the negative (protein extraction buffer) and the positive controls (30 ng of total protein extract from HeLa cells) of the assay, respectively. b Quantification of telomerase activity in a. The telomerase products (6-bp ladder) and the 36-bp internal control (PCR internal control) bands were quantified using a Storm phosphoimager. Relative telomerase activity was calculated as the intensity ratio of the TRAP ladder (telomerase products) to that of the PCR internal control. The percentage of inhibition was calculated by dividing the intensity ratio of sample post-IMT with the intensity ratio of the sample pre-IMT at different timepoints: course 1, day 1 pre-IMT (C1D1-pre); course 1, day 1 post-IMT (C1D1-post); course 1, day 2 (C1D2); course 1, day 8 (C1D8); course 2, day 1 pre-IMT (C2D1) and course 3, day 1 pre-IMT (C3D1). Note sustained inhibition of telomerase activity until C1D8 and recovery of telomerase activity by C2D1
Telomerase inhibition in tumor
Of two evaluable patients on the MB trial, intratumoral telomerase activity was inhibited by 95 % compared to baseline archival tissue in one patient with HGG (Fig. 2). This patient’s tumor was removed 26.5 h after imetelstat infusion. Telomerase activity post-imetelstat was not assessed in the second patient with medulloblastoma due to tumor hemorrhage at resection making the TRAP assay uninterpretable.
In tumor inhibition of telomerase activity post-imetelstat (IMT) treatment in one patient with HGG enrolled on the MB study. a Patient received the first dose of imetelstat 26.5 h before surgery. Total protein extracts were assayed for telomerase activity. Telomerase activity was evaluated by TRAP assay using 400 ng of total protein extracted from fresh flash-frozen tumor tissue samples collected from archival tissue (lane 1, pre-IMT) and second surgery (lane 2, post-IMT). Lanes 3 and 4 are the negative (protein extraction buffer) and the positive controls (30 ng of total protein extract from HeLa cells) of the assay, respectively. PCR internal control and telomerase products are indicated with a black arrow. b Quantification of telomerase activity in a. The telomerase products (6-bp ladder) and the 36-bp internal control (PCR internal control) bands were quantified using a Storm phosphoimager. Relative telomerase activity was calculated as the intensity ratio of the TRAP ladder (telomerase products) to that of the PCR internal control. The percentage of inhibition was calculated by dividing the intensity ratio of sample post-IMT with the intensity ratio of the sample pre-IMT. The assay was repeated three times. The calculated telomerase activity inhibition is ~95 % relative to telomerase activity in the tissue collected at the time of the first surgery (lane 1). The values shown are the mean ± SD of three independent experiments
Discussion
Imetelstat toxicities reported in this investigator-sponsored study are similar to previous adult and pediatric studies which included thrombocytopenia, lymphopenia and neutropenia [16, 17]. Despite stringent eligibility criteria and careful monitoring of hematologic parameters in this CNS-specific trial, two patients died of intratumoral hemorrhage secondary to thrombocytopenia leading to premature closure of the study. Following the first patient death on study, an exhaustive analysis of the toxicity data from patients on protocol revealed that median time for platelet nadir was 13 days (range: 6–21 days) post day 1 of imetelstat, putting patients at risk for cumulative myelosuppression by the time the day 8 dose was given. Although additional safety measures and closer monitoring of hematologic parameters were introduced, these modifications did not mitigate the risk of severe thrombocytopenia causing intratumoral bleeding and made the schedule of drug administration intolerable in the recurrent CNS tumor patient population. This is in contrast with the tolerability of imetelstat demonstrated in non-CNS patients in the pediatric phase I trial despite commonly-reported thrombocytopenia [16], where no hemorrhage was reported. Interestingly, however, in a pilot trial in adults with myelofibrosis, one patient who received an equivalent dose of weekly imetelstat also died from intracranial hemorrhage caused by drug associated myelosupression [14].
This study represents the first pharmacokinetic report of imetelstat in pediatric patients with recurrent brain tumors. The Cmax in patients from this study receiving 285 mg/m2 is 97.5 µg/mL and is nearly identical to 96.7 µg/mL previously reported by our phase I study in pediatric patients with refractory or recurrent solid tumors [16]. Due to the small number of evaluable samples and the premature closure of the study, further discussion of imetelstat pharmacokinetics or pharmacodynamics (PD) from this study is limited.
Imetelstat treatment led to inhibition of telomerase activity in both PBMCs and tumor. To our knowledge, this is the first published report of intratumoral telomerase inhibition following imetelstat administration in brain malignancies. Similar to findings from the phase I pediatric study, telomerase activity was inhibited in PBMCs for up to 8 days post-imetelstat administration. Telomerase inhibition in PBMCs was not further assessed until the start of a new cycle, at which time telomerase activity was fully restored. Toxicities associated with this drug, particularly thrombocytopenia, prevented more frequent dosing in our patient population at risk for CNS bleed. It is known that minimal telomerase acitivity and short-term telomerase expression are sufficient to restore the shortest telomeres and maintain cell viability [18, 19]. Thus, the inability to administer imetelstat more frequently than on days 1 and 8 of a 21-day course to accomplish more sustained telomerase inhibition may partially explain the lack of objective responses in this study. We postulate that continued tumor cell proliferation occurred in patients’ tumors in this trial due to telomere length recovery, precluding cell growth arrest or cell death. As previously suggested by preclinical data using orthotopic HGG mice xenografts [10, 13], this study presents clinical evidence, albeit in one patient, that imetelstat crosses the blood–brain barrier in pediatric patients with recurrent CNS tumors based on its ability to inhibit telomerase activity by >95 % intratumorally 26.5 h after imetelstat infusion.
In summary, imetelstat achieved intratumoral and PBMC target inhibition at 285 mg/m2. While the regimen proved too toxic in children with recurrent or refractory CNS tumors, telomerase and telomeres remain relevant therapeutic targets in this patient population given the role played by telomerase reactivation in oncogenesis. Preclinical studies of a telomere-targeted strategy consisting of the incorporation of 6-thio-deoxyguanosine [20], a telomerase substrate analog, into telomeres are currently being tested pre-clinically and appear to be promising.
References
Blackburn EH (1991) Structure and function of telomeres. Nature 350(6319):569–573. doi:10.1038/350569a0
Kim NW, Piatyszek MA, Prowse KR, Harley CB, West MD, Ho PL, Coviello GM, Wright WE, Weinrich SL, Shay JW (1994) Specific association of human telomerase activity with immortal cells and cancer. Science 266(5193):2011–2015
Shay JW, Bacchetti S (1997) A survey of telomerase activity in human cancer. Eur J Cancer 33(5):787–791. doi:10.1016/S0959-8049(97)00062-2
Komata T, Kanzawa T, Kondo Y, Kondo S (2002) Telomerase as a therapeutic target for malignant gliomas. Oncogene 21(4):656–663. doi:10.1038/sj.onc.1205072
Barszczyk M, Buczkowicz P, Castelo-Branco P, Mack SC, Ramaswamy V, Mangerel J, Agnihotri S, Remke M, Golbourn B, Pajovic S, Elizabeth C, Yu M, Luu B, Morrison A, Adamski J, Nethery-Brokx K, Li XN, Van Meter T, Dirks PB, Rutka JT, Taylor MD, Tabori U, Hawkins C (2014) Telomerase inhibition abolishes the tumorigenicity of pediatric ependymoma tumor-initiating cells. Acta Neuropathol (Berl) 128(6):863–877. doi:10.1007/s00401-014-1327-6
Ridley L, Rahman R, Brundler MA, Ellison D, Lowe J, Robson K, Prebble E, Luckett I, Gilbertson RJ, Parkes S, Rand V, Coyle B, Grundy RG, Children’s C Leukaemia group biological studies C (2008) Multifactorial analysis of predictors of outcome in pediatric intracranial ependymoma. Neuro-Oncol 10(5):675–689. doi:10.1215/15228517-2008-036
Didiano D, Shalaby T, Lang D, Grotzer MA (2004) Telomere maintenance in childhood primitive neuroectodermal brain tumors. Neuro-Oncol 6(1):1–8. doi:10.1215/S1152851703000176
Dorris K, Sobo M, Onar-Thomas A, Panditharatna E, Stevenson CB, Gardner SL, Dewire MD, Pierson CR, Olshefski R, Rempel SA, Goldman S, Miles L, Fouladi M, Drissi R (2014) Prognostic significance of telomere maintenance mechanisms in pediatric high-grade gliomas. J Neurooncol 117(1):67–76. doi:10.1007/s11060-014-1374-9
Kim CH, Cheong JH, Bak KH, Kim JM, Oh SJ (2006) Prognostic implication of telomerase activity in patients with brain tumors. J Korean Med Sci 21(1):126–130
Marian CO, Cho SK, McEllin BM, Maher EA, Hatanpaa KJ, Madden CJ, Mickey BE, Wright WE, Shay JW, Bachoo RM (2010) The telomerase antagonist, imetelstat, efficiently targets glioblastoma tumor-initiating cells leading to decreased proliferation and tumor growth. Clin Cancer Res 16(1):154–163. doi:10.1158/1078-0432.CCR-09-2850
Terali K, Yilmazer A (2016) New surprises from an old favourite: the emergence of telomerase as a key player in the regulation of cancer stemness. Biochimie 121:170–178. doi:10.1016/j.biochi.2015.12.001
Gryaznov SM, Jackson S, Dikmen G, Harley C, Herbert BS, Wright WE, Shay JW (2007) Oligonucleotide conjugate GRN163L targeting human telomerase as potential anticancer and antimetastatic agent. Nucleosides Nucleotides Nucleic Acids 26(10–12):1577–1579. doi:10.1080/15257770701547271
Ferrandon S, Malleval C, El Hamdani B, Battiston-Montagne P, Bolbos R, Langlois JB, Manas P, Gryaznov SM, Alphonse G, Honnorat J, Rodriguez-Lafrasse C, Poncet D (2015) Telomerase inhibition improves tumor response to radiotherapy in a murine orthotopic model of human glioblastoma. Mol Cancer 14:134. doi:10.1186/s12943-015-0376-3
Tefferi A, Lasho TL, Begna KH, Patnaik MM, Zblewski DL, Finke CM, Laborde RR, Wassie E, Schimek L, Hanson CA, Gangat N, Wang X, Pardanani A (2015) A pilot study of the telomerase inhibitor imetelstat for myelofibrosis. N Engl J Med 373(10):908–919. doi:10.1056/NEJMoa1310523
Baerlocher GM, Oppliger Leibundgut E, Ottmann OG, Spitzer G, Odenike O, McDevitt MA, Roth A, Daskalakis M, Burington B, Stuart M, Snyder DS (2015) Telomerase inhibitor imetelstat in patients with essential thrombocythemia. N Engl J Med 373(10):920–928. doi:10.1056/NEJMoa1503479
Thompson PA, Drissi R, Muscal JA, Panditharatna E, Fouladi M, Ingle AM, Ahern CH, Reid JM, Lin T, Weigel BJ, Blaney SM (2013) A phase I trial of imetelstat in children with refractory or recurrent solid tumors: a children’s oncology group phase I consortium study (ADVL1112). Clin Cancer Res 19(23):6578–6584. doi:10.1158/1078-0432.CCR-13-1117
Roth A, Harley CB, Baerlocher GM (2010) Imetelstat (GRN163L)–telomerase-based cancer therapy. Recent Results Cancer Res 184:221–234. doi:10.1007/978-3-642-01222-8_16
Ouellette MM, Liao M, Herbert BS, Johnson M, Holt SE, Liss HS, Shay JW, Wright WE (2000) Subsenescent telomere lengths in fibroblasts immortalized by limiting amounts of telomerase. J Biol Chem 275(14):10072–10076
Steinert S, Shay JW, Wright WE (2000) Transient expression of human telomerase extends the life span of normal human fibroblasts. Biochem Biophys Res Commun 273(3):1095–1098. doi:10.1006/bbrc.2000.3080
Mender I, Gryaznov S, Dikmen ZG, Wright WE, Shay JW (2015) Induction of telomere dysfunction mediated by the telomerase substrate precursor 6-thio-2′-deoxyguanosine. Cancer Discov 5(1):82–95. doi:10.1158/2159-8290.CD-14-0609
Acknowledgements
We acknowledge the outstanding clinical research support of Christopher Smith and Emily Carps and the regulatory support of Dr. Renee Doughman. This work was supported in part by Cincinnati Children’s Basic Science Research and the Clinical Translational, Outcomes and Health Services Redesign grant (R.D.), National Institute of Health Grant U01 CA81457 for the Pediatric Brain Tumor Consortium (M.F. and J.B.) and American Lebanese Syrian Associated Charities.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Salloum, R., Hummel, T.R., Kumar, S.S. et al. A molecular biology and phase II study of imetelstat (GRN163L) in children with recurrent or refractory central nervous system malignancies: a pediatric brain tumor consortium study. J Neurooncol 129, 443–451 (2016). https://doi.org/10.1007/s11060-016-2189-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-016-2189-7