Abstract
General population-based survival statistics for primary malignant brain or other central nervous system (CNS) tumors do not provide accurate estimations of prognosis for individuals who have survived for a significant period of time. For these persons, the use of conditional survival percentages provides more accurate information to estimate potential outcomes. Using information from the National Cancer Institute’s Surveillance, Epidemiology and End Results (SEER) program from 1995 to 2012, conditional survival percentages were calculated for 1 or 5 years of additional survival for all primary malignant brain and CNS tumors overall and by gender, race, ethnicity and age. Rates were calculated to include 1, 2, 3, 4, 5, 10 and 15 years post diagnosis. Conditional survival was also calculated in intervals from 1995–2004 to 2005–2012, to examine the potential effect that the introduction of new treatment protocols may have had on survival rates. The percentage of patients surviving one or five additional years varied by histology, age at diagnosis, gender, race and ethnicity. Younger persons (age <15 years at diagnosis) had higher conditional survival percentages for all histologies as compared to all histologies in older patients (age ≥15 years at diagnosis). The longer the amount of time post-diagnosis of a malignant brain or other CNS tumor, the higher the conditional survival. Younger persons at diagnosis had the highest conditional survival irrespective of histology. Use of conditional survival rates provides relevant additional information for patients and their families, as well as for clinicians and researchers, and helps with understanding prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary malignant brain and central nervous system (CNS) tumors are a rare cancer, only representing approximately 2 % of all cancers. Despite this, these tumors cause significant morbidity and mortality. Five-year relative survival rates following diagnosis of these tumors in patients under the age of 75 years encompass a broad range of survival from approximately 11–73 % [1]. Most reported cancer survival statistics are calculated from time of diagnosis, and provide an estimate of prognosis from 0 years of current survival. These statistics for relative survival calculated from time of diagnosis do not accurately describe the survival patterns for persons that have already survived for a period of time, because the probability of survival changes with increasing survival time.
Conditional survival is defined as the probability that a person will survive an additional number of years given that they have already survived a definitive amount of years after the time of diagnosis [2]. An important distinction to note is that relative survival rates describe the percent of persons surviving to a time point from the time of diagnosis, whereas conditional survival calculates survival to a time point after the patient has survived a certain number of years after their diagnosis. However, relative survival rates are used to calculate conditional survival rates in this paper as explained in the discussion. Use of conditional survival probabilities may provide more accurate estimations by offering survival estimates based on the outcomes of patients who have already survived for a period of time post-diagnosis.
Conditional survival probabilities have previously been reported for primary malignant brain and CNS tumors, but these analyses have often been limited to smaller time frames, specific treatment regimens, a select few histologies, or calculated conditional survival probabilities for primary malignant brain tumors overall. This study aims to examine a wide range of histologies over a 17-year time frame, by demographic factors that have previously been shown to affect survival in primary brain and CNS tumors, including age, sex, and race [1, 3–7]. In this study, conditional survival probabilities of surviving one or five additional years overall and by histology, gender, race and ethnicity were calculated for persons diagnosed with primary malignant brain and other CNS tumors from 1995 to 2012. Conditional survival probabilities were also calculated for the intervals from 1995–2004 to 2005–2012, to examine the potential effect that the introduction of new treatment protocols may have had on prognosis.
Methods
Data for this review were taken from the National Cancer Institute’s (NCI) Surveillance, Epidemiology and End Results (SEER) program. SEER includes data from 18 population-based cancer registries that are selected to be largely representative of the United States (US) population and covers approximately 28 % of the US population [8].
All analyses were done using SEER*Stat 8.2.1 [9]. Conditional survival percentages were generated for all primary malignant brain and CNS tumors using survival data collected between 1995 and 2012 [10]. Persons who were still alive at the end of December 2012 were censored. The percentages of persons surviving one additional year after a period of 1-, 2-, 3-, 4-, 5-, 10-, and 15-years after diagnosis were generated, along with their 95 % confidence intervals (95 % CI). The percentages of persons surviving five additional years after a period of 1, 2, 3 and 4 years after diagnosis were also generated, along with their 95 % CI. Significance of difference between two conditional survival probabilities was tested by whether the 95 % CIs overlapped for these two values. The cumulative observed survival (CP) was divided by the cumulative expected survival (CP*) within the same a–x interval, to obtain the cumulative relative survival (CR) [11]. The CR value is the value of conditional survival percentage generated by SEER*Stat that was used for each interval in this study. Malignant primary brain and other CNS tumors were defined as tumors with an International Classification of Disease, Oncology 3rd edition (ICD-O-3) site code of C70–C72, or C75.1–C75.3, and an ICD-O-3 behavior code of 3.
Conditional survival probabilities were generated overall, as well as by histology, gender, age, ethnicity and race. Histologic groups were defined using the Central Brain Tumor Registry of the United States (CBTRUS) schema [1, 12]. Ethnicity was defined as Hispanic or non-Hispanic–Latino, while race was defined as White, Black and a combined group of American Indian/Alaska Natives (AIAN) and Asian Pacific Islander (API) [13]. Age at diagnosis was grouped into three groups: children (age 0–14 years), adolescents and young adults (AYA, age 15–39 years), and older adults (age 40+ years).
In 2005, the Stupp protocol which included concurrent radiation and chemotherapy with temozolomide became standard of care in glioblastoma. This protocol provided major improvements in newly diagnosed glioblastoma median survival [14], which could have possibly had an effect on conditional survival. To account for this major change of treatment, in addition to the main analysis from 1995 to 2012, an additional analysis was also performed including two separate groups from 1995–2004 to 2005–2012. Histologies included in the separate analysis include glioblastoma, anaplastic astrocytoma, and oligodendroglioma, since these include high grade gliomas that were may have been treated using the Stupp protocol. Age at diagnosis was divided into two groups: young adults (AYA, age 15–39) and older adults (age 40+ years). Children (age 0–14 years) were not included because of the low number of children with gliomas. By comparing these two groups to the period of conditional survival from 1995 to 2012, possible differences in conditional survival from the Stupp protocol can be identified.
Results
Overall conditional survival probabilities after 1 year of survival by histology are presented in Table 1. The probability of surviving one additional year increased with increasing years post-diagnosis. The probability of surviving one additional year was 44.1 % (95 % CI 43.7–44.5 %) for 1-year survivors, 90.5 % (95 % CI 90.0–90.9 %) for 5-year survivors and 94.4 % (95 % CI 93.8–95.0 %) for 10-year survivors. Significant increases in probability of surviving one additional year were seen in patients with most histologic types, with the exception of oligodendroglioma, neuronal and mixed neuronal-glial tumors, and other neoplasms related to the meninges for which the probability of surviving one additional year remained relatively unchanged with increased current survival. After surviving 2 years after diagnosis, the probability of surviving an additional year was greater than 50 % in all histologies with the exception of glioblastoma in which the probability of survival was 23.8 % (95 % CI 22.9–24.6 %).
Overall conditional survival of an additional 5 years for 1-, 2-, 3- and 4-years post-diagnosis are presented in Table 2 by histology. The percentage of surviving five additional years for all tumors was 34.4 % (95 % CI 34.0–34.7 %) for 1-year survivors, 59.2 % (95 % CI 58.6–59.7 %) for 2-year survivors, 77.9 % (95 % CI 77.4–78.4 %) for 3-year survivors, and 88.2 % (95 % CI 87.7–88.7 %) for 4-year survivors. All histologies demonstrated increased 5-year predicted survival with an increasing period of current survival. After surviving 2 years, the 5-year conditional survival was greater than 50 % for all histologies except for anaplastic astrocytoma and glioblastoma, where the probability of survival was 45.0 % (95 % CI 42.7–47.3 %) and 13.6 % (95 % CI 12.9–14.4 %) respectively.
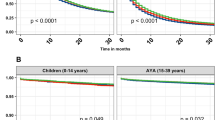
One year of conditional survival was estimated for glioblastoma, anaplastic astrocytoma, and oligodendroglioma from 1995 to 2004 as well as from 2005 to 2012 for ages 15–39 and 40+ for 1, 2, 3, 4, 5, 10 and 15 years past diagnosis. Among glioblastoma and anaplastic astrocytoma, the first year after diagnosis was found to have a significantly higher conditional survival in 2005–2012 versus 1995–2004 in both age groups (Fig. 1a–d). Two years past diagnosis in glioblastoma patients aged 40+ also had significantly higher conditional survival in 2005–2012 versus 1995–2004 (Fig. 1b). Oligodendroglioma seemed to have a slight favor towards increased conditional survival for 2005–2012, but none of the findings were statistically significant (Fig. 1e, f).
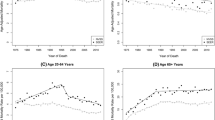
Conditional survival probabilities were also estimated by gender, age, ethnicity and race for glioblastoma (Fig. 2a–d) and malignant meningioma (Fig. 3a–d). Among malignant meningioma, females exhibited higher survival rates at all timepoints (Fig. 3a). Conditional survival percentages were consistently higher in younger patients for glioblastoma (Fig. 2b) and malignant meningioma (Fig. 3b). AIAN/API had significantly higher conditional survival than Whites and Blacks in glioblastoma for first year post-diagnosis, but there was no significant difference with increasing times of current survival (Fig. 2d).
Discussion
In addition to commonly reported overall or relative survival estimates, conditional survival rates provide an important measure of population-level cancer survival, as well as a potentially more accurate prediction of prognosis for longer term survivors in the United States. Overall survival statistics are strongly influenced by persons that survive a short period of time after their diagnosis. This effect can be particularly significant in cancers with low 1-year overall survival, such as glioblastoma and anaplastic astrocytoma, where 1-year overall survival is 36.5 and 61.3 %, respectively [1]. Our results show generally that the longer a person survives after diagnosis, the higher the probability that they will survive at least one or five additional year(s) (Tables 1, 2).
There have been several previous analyses that generated conditional survival probabilities for patients with brain and CNS tumors. Many of these have focused solely on glioblastoma, or other high grade gliomas [2, 15], and have found increasing conditional probability of survival with increasing years of current survival as well as a significant effect of histology, lower WHO grade, lower age, site and treatment regimen on conditional survival. A previous analysis estimated conditional survival probabilities for malignant or non-malignant primary brain tumors and found improved conditional survival estimates histology, malignancy and lower age at diagnosis. This analysis also found that conditional survival probability was greatest after 2 years of survival, as compared to this analysis which found increasing survival estimates with each year of increased current survival [16]. Another analysis found that older patients (65 years old or greater) diagnosed with a glioblastoma had decreased conditional probability of 5-year survival upon survival of 2 years than younger patients, and that the proportion of persons surviving five additional years after 2 years of current survival was significantly higher than those having already survived only 1 year [17]. These studies have shown that overall, patients who have survived at least 2 years post-diagnosis have a higher conditional probability of survival than patients still in the first 2 years of their diagnosis [2, 15–17]. Despite these pertinent findings, these studies only examined conditional survival based on age, treatment and histology whereas this current study also investigated gender, ethnicity and race.
In this study, glioblastoma conditional survival was reviewed from 1995 to 2012, then examined from 1995–2004 to 2005–2012 from ages 15 to 39 and 40+. These two time periods were chosen because of the possible effect that the Stupp protocol may have had on conditional survival. The probability of an additional year of survival after 2 years post-diagnosis with glioblastoma reported in our study overall was 23.80 % as seen in Table 1. In Fig. 1, 1 year of conditional survival after 2 years post-diagnosis from 1995 to 2004 was 43.1 and 15.8 % in ages 15–39 and 40+, respectively. Also, in Fig. 1, 1 year of conditional survival after 2 years post-diagnosis from 2005 to 2012 was 46.4 and 24.1 % in ages 15–39 and 40+, respectively. These findings are lower than Porter et al.’s published percentage of 56.0 % (95 % CI 48.1–63.1 %) [16], except for ages 15–39 from 2005 to 2012 where there is overlap between the confidence intervals of the two values (Fig. 1a). While both studies used the SEER cancer registries, Porter et al. used data from 5 SEER registries and from a different timeframe, 1985–2005, while this current study contained data from 18 SEER registries from 1995 to 2012. With the advent of the Stupp protocol of concurrent radiation and chemotherapy with temozolomide pointing to slight improvements in median survival for glioblastoma, the relative survival for glioblastoma has also shown improvement and also contributed to the differences in conditional probability between the two studies. Two year relative conditional survival for glioblastoma in the dataset used for this analysis is 15.2 %, as compared to 30.9 % in Porter, et al. [16]. The analyses in the current study also had lower rates of survival for glioblastoma as compared to those found in McNamara et al. [18]. These differences indicate that the survival cohort used to generate the statistics in these two analyses is likely quite different.
The current study included a large population-based sample (N = 33,204 glioblastomas) and the majority (58 %) of patients included in the previous analysis received concurrent chemotherapy and radiation, which has been shown to contribute to improved survival [18]. This may account for the overlap seen from 1995 to 2012 in ages 15–39 years (Fig. 1a), where the standard of care changed with the introduction of the Stupp protocol, and both samples may have had similar treatment. However, the age intervals are much different and must be considered when comparing the two. Still, it appears that the introduction of adjuvant temozolomide and concurrent radiation contributed to a slight improvement in conditional survival, especially in the first 2 years post diagnosis.
While investigating the relationship between the conditional survival probabilities of patients diagnosed with glioblastoma and various demographic variables, distinct trends were observed. The conditional survival data for glioblastoma patients showed that as subjects’ age increased, conditional survival decreased (Fig. 2), which corresponds to the previous findings of Davis et al. and Porter et al. [16, 17]. The oldest age group had the lowest conditional survival percentages significantly for 1-, 2-, 3-, 4-, and 5-years after diagnosis (Fig. 2). Older people may not be offered certain treatment options such as clinical trials or aggressive treatment options, or may even decline aggressive treatment options. Bauchet et al. recognized in elderly glioblastoma patients that radiation therapy provided significant improvements in their outcomes but transportation to a hospital for daily treatment could be difficult, especially if the patient is frail [19]. Advanced age is a demographic factor that significantly decreased conditional survival in the first 5 years after diagnosis.
The present study also found that conditional survival rates for glioblastoma were higher among Hispanics significantly in the first 2 years of survival (Fig. 2c), and is similar to previous findings [1, 20, 21]. This may be related to the Hispanic Paradox: despite low socioeconomic status and decreasing quality and access of healthcare, Hispanics demonstrate similar health patterns and mortality rates as Whites across many diseases. Although the cause of the Hispanic Paradox is unknown, research has increasingly shown that Hispanics have higher health outcomes despite their lower socioeconomic status [20]. Hispanic ethnicity slightly favors increased conditional survival in the first 2 years after diagnosis.
Females with a glioblastoma demonstrated higher conditional survival than males with the same diagnosis (Fig. 2a), which is consistent with some previous reports. This is similar to the findings of Sant et al., where 5 year relative survival of malignant CNS tumors was significantly favored for women (21.7 vs. 18.5 %) [22]. Another study found that younger females may be predictive of longer survival in glioblastomas [23]. While both findings use relative survival, and not conditional survival, a slight increase in relative survival for females over 5 years might be responsible for increased conditional survival relative to men, since more females are living longer. Overall, conditional survival rates for glioblastoma demonstrated significant trends across age, ethnicity and gender.
The conditional survival of malignant meningioma patients was then examined with respect to each demographic variable. There was no definitive relationship or trend between conditional survival among meningioma patients and ethnicity. However, similar to gender related findings associated with glioblastoma, malignant meningioma patients demonstrated higher conditional survival rates in women than in men. This reflects findings from Perry et al.’s study that aggressive meningiomas were more common in males than in females [24]. When studying malignant meningioma incidence trends in relation to age and gender, Ksherrty et al. observed higher incidence rates in middle-age females (age 35–64 years) but lower incidence rates in elderly females (age >64 years) compared to males in the same age groups with similar diagnoses [25]. The increased incidence of meningioma in middle-age females may be attributable to higher levels of estrogen and progesterone than in males of the same age which may increase the risk of development of meningiomas.
Strengths and limitations
The SEER datasets comprise the largest population-based dataset in the US that allows for survival calculations based on active patient follow up. This analysis represents the most up to date conditional survival analysis of brain tumors, and also presents data on a wide range of brain tumor histologies. Additionally, quality improvement in the SEER dataset is a high caliber decentralized process that includes SEER staff as well as independent contractors following a quality improvement cycle [26]. Due to the high quality active follow-up conducted by SEER registries, the survival information presented in this report is assumed to be highly accurate. The populations represented by the SEER registry system are constructed to be representative of the US population.
Additionally, conditional survival for an interval of 17 years has not been done in the detail of demographics that this study has presented. Observing factors such as gender, age, ethnicity and race within conditional survival allows a greater understanding of CNS tumor behavior over time. Comparing conditional survival for glioblastoma and malignant meningioma in their respective four-panel figures allows for sex, age, race, and ethnicity to be easily and effectively compared to one another. The examined time period from 1995 to 2012 represents the most recent and accurate information available on primary brain and CNS tumor behavior. Furthermore, to account for possible differences in treatment beginning in 2005, the analysis among different time intervals from 1995–2004 to 2005–2012 was performed. This helped elucidate differences that may exist between the two timeframes and perhaps allow for a more accurate representation of conditional survival in recent years. Using one and 5 years of conditional survival in Tables 1 and 2 allows for a consistent comparison of short term and long term conditional survival among all histology sites within the same dataset.
The established SEER dataset and the presentation of conditional survival are strong points to consider in this study. The SEER database is a high quality dataset with a long period of case ascertainment, active follow up, and a relatively large sample size for this rare disease. Use of these data comes with several limitations. First, the study data are retrospective, and each cohort of period survival is made up of persons diagnosed with and treated for their brain and CNS tumor at many different years in the overall period. For example, the 2-year survivors could include both a person diagnosed in 1995 who had survived to 1997, as well as a person diagnosed in 2009 who had survived to 2011. Both of these persons are factored into the survival probability of a 2-year survivor living an additional year. This means that the results of this analysis might not accurately represent the survival probabilities of a person diagnosed today. Our time-period analysis suggests that there have not been significant gains in survival between the two periods we examined, and as a result we believe the effect of this to be small.
It is important to note with increasing age, there is increased probability of dying from any cause during a period of years [27]. Our study accounted for this by using relative survival in the calculations of conditional survival. Relative survival is a measure of observed survival that is adjusted for death due to all other factors in the population based on age-based life tables. In some cases relative survival may be an accurate measure of population-level survival patterns than observed survival because relative survival accounts for other factors that affect subsets of the population, whereas observed survival does not. In this study, older patients may not receive the same level of treatment as younger patients, and may be excluded from some therapeutic trials. Additionally, females in general have a decreased probability of dying from any cause at any age as compared to males [27]. Using relative survival helped account for these certain factors within the US, and thus the results of conditional survival could be compared to other countries that share similar factors. For example, results could be compared to more developed countries that also have a large elderly population since those patients will likely share an increased risk of dying. Accounting for these factors in the SEER database and in this study is not feasible, but important to note when examining the decreased conditional survival in older patients and in females.
Relative survival is calculated using life tables that are based on survival patterns in the US during the time covered by this analysis. As a result these adjustments may not affect survival patterns in other countries, or at other points in time. It must be emphasized that the results found in this study are not generalizable to survival analysis of brain tumors in countries other than the US where survival patterns may vary. Relative survival adjustments have the largest impact when survival after diagnosis is long, which is not the case with brain tumors overall. As a result, relative survival calculations within some groups may not differ significantly from overall survival. Still, the use of relative survival rates in the calculation of conditional survival in this study we believe allows for a clearer understanding of brain tumor behavior in the US.
There have also been changes to definitions of tumor histologies over the period used in this analysis, during which there have been three revisions of the WHO classification of tumors of the central nervous system (1997, 2000, and 2007). Modifications to this classification scheme have had dramatic effects on diagnostic criteria for several of the tumors used in this analysis, and may affect which tumors are included within each histology category over time. Our time period analysis suggests that this does not have a significant effect on conditional survival probabilities for a selected group of tumors, and we believe that the overall effect of this should be minimal. The current structure of the SEER registry system does not allow for central pathology review, and as a result these results reflect diagnoses made within each patient’s individual clinical care.
Using the SEER database presents several limitations for studying survival in malignant brain tumors. Information on extent of resection of CNS tumors is limited and the variables used to record these data have changed over time, and as a result are difficult to incorporate into these models. Quantifying extent of resection and estimating conditional survival may be a part of future research, since there is a relationship between the extent of resection and prognosis of glioblastomas [28, 29]. There is no chemotherapy information for brain and CNS tumors recorded in SEER, and as a result we are not able to consider these treatment patterns in these models. Finally, many genetic and molecular biomarkers that are prognostic in some malignant brain and CNS tumors (such as 1p/19q deletion status and MGMT methylation status) have only been required data elements since 2010, and are not part of the public release SEER data set. IDH1/2 mutation status has emerged as one of the most significant predictors of glioma treatment response and prognosis, but is not currently collected by cancer registrars within the SEER program. The use of genetic and molecular markers in estimating conditional survival is a potential area of future research, since these biomarkers may help further classify tumor behavior more effectively than the WHO Grade. Using extent of resection, chemotherapy treatment details, and extent of resection in estimating conditional survival may help to further our understanding of CNS tumors and may contribute to improved prognosis.
For histologies with poor overall survival, the number of patients who survived beyond one or 2 years may be relatively small. The decline in sample size may have diminished the reliability of these estimates. In an attempt to limit this affect, we have suppressed any survival statistic calculated from a base population of 50 or less. There have also been several reorganizations to the SEER data system during the study time period that potentially could impact the results and generalizability of this analysis [30]. Still, these limitations were addressed as much as possible in order to provide the most accurate information available.
Conclusion
Conditional survival statistics provide a valuable resource for accurate and relevant estimates of survival for brain tumor patients who have already survived beyond a certain period. Availability of these statistics aid in understanding the demographic factors underlying improved survival. They provide a barometer for gauging long term survival that is useful to researchers, clinicians, patients and families and may result in developing new research questions aimed in improving patient care and in expanding support programs.
References
Ostrom QT, Gittleman H, Liao P, Rouse C, Chen Y, Dowling J, Wolinsky Y, Kruchko C, Barnholtz-Sloan J (2014) CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2007–2011. Neuro Oncol 16:iv1–iv63
Polley MY, Lamborn KR, Chang SM, Butowski N, Clarke JL, Prados M (2011) Conditional probability of survival in patients with newly diagnosed glioblastoma. J Clin Oncol 29:4175–4180
Johnson DR, Ma DJ, Buckner JC, Hammack JE (2012) Conditional probability of long-term survival in glioblastoma. Cancer 118:5608–5613
Pan I-W, Ferguson SD, Lam S (2015) Patient and treatment factors associated with survival among adult glioblastoma patients: a USA population-based study from 2000–2010. J Clin Neurosci 22:1575–1581
Najari BB, Rink M, Li PS, Karakiewicz PI, Scherr DS, Shabsigh R, Meryn S, Schlegel PN, Shariat SF (2013) Sex disparities in cancer mortality: the risks of being a man in the United States. J Urol 189:1470–1474
Trinh VT, Davies JM, Berger MS (2015) Surgery for primary supratentorial brain tumors in the United States, 2000–2009: effect of provider and hospital caseload on complication rates. J Neurosurg 122:280–296
Curry WT, Carter BS, Barker FG (2010) Racial, ethnic, and socioeconomic disparities in patient outcomes after craniotomy for tumor in adult patients in the United States, 1988–2004. Neurosurgery 66:427–438
Overview of the Seer Program. In: National Cancer Institute. http://seer.cancer.gov/about/overview.html. Accessed 7 Oct 2015
SEER*Stat Software. In: National Cancer Institute. http://seer.cancer.gov/seerstat/. Accessed 7 Oct 2015
Surveillance Epidemiology and End Results (SEER) Program. SEER*Stat Database: incidence— SEER 18 Regs research data + Hurricane Katrina impacted Louisiana cases, Nov 2013 Sub (1973–2011 varying)—linked to county attributes—Total U.S., 1969–2012 count
Algorithms for special intervals/conditional survival. In: National Cancer Institute. http://seer.cancer.gov/seerstat/WebHelp/Algorithms_for_Special_Intervals_Conditional_Survival.htm. Accessed 9 Oct 2015
Kleihues P, Cavenee W (2000) Tumours of the nervous system: World Health Organization classification of tumours. IARC Press, Lyon
NAACCR Race and Ethnicity Work Group NAACCR guideline for enhancing Hispanic/Latino identification: revised NAACCR Hispanic/Latino identification algorithm [NHIA v2.2.1]
Stupp R, Mason WP, van den Bent MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996
Tsao-Wei DD, Hu J, Groshen SG, Chamberlain MC (2012) Conditional survival of high-grade glioma in Los Angeles County during the year 1990–2000. J Neurooncol 110:145–152
Porter KR, McCarthy BJ, Berbaum ML, Davis FG (2011) Conditional survival of all primary brain tumor patients by age, behavior, and histology. Neuroepidemiology 36:230–239
Davis FG, McCarthy BJ, Freels S, Kupelian V, Bondy ML (1999) The conditional probability of survival of patients with primary malignant brain tumors: surveillance, epidemiology, and end results (SEER) data. Cancer 85:485–491
McNamara MG, Lwin Z, Jiang H, Chung C, Millar B-A, Sahgal A, Laperriere N, Mason WP (2014) Conditional probability of survival and post-progression survival in patients with glioblastoma in the temozolomide treatment era. J Neurooncol 117:153–160
Bauchet L, Zouaoui S, Darlix A, Menjot de Champfleur N, Ferreira E, Fabbro M, Kerr C, Taillandier L (2014) Assessment and treatment relevance in elderly glioblastoma patients. Neuro Oncol 16:1459–1468
Franzini L, Ribble JC, Keddie AM (2001) Understanding the Hispanic paradox. Ethn Dis 11:496–518
Jemal A, Clegg LX, Ward E, Ries LAG, Wu X, Jamison PM, Wingo PA, Howe HL, Anderson RN, Edwards BK (2004) Annual report to the nation on the status of cancer, 1975–2001, with a special feature regarding survival. Cancer 101:3–27
Sant M, Minicozzi P, Lagorio S, Børge Johannesen T, Marcos-Gragera R, Francisci S (2012) Survival of European patients with central nervous system tumors. Int J Cancer 131:173–185
Shinojima N, Kochi M, Hamada J et al (2004) The influence of sex and the presence of giant cells on postoperative long-term survival in adult patients with supratentorial glioblastoma multiforme. J Neurosurg 101:219–226
Perry A, Stafford SL, Scheithauer BW, Suman VJ, Lohse CM (1997) Meningioma grading: an analysis of histologic parameters. Am J Surg Pathol 21:1455–1465
Kshettry VR, Ostrom QT, Kruchko C, Al-Mefty O, Barnett GH, Barnholtz-Sloan JS (2015) Descriptive epidemiology of World Health Organization grades II and III intracranial meningiomas in the United States. Neuro Oncol 17:1166–1173
Process—SEER quality improvement. In: National Cancer Institute. http://seer.cancer.gov/qi/process.html. Accessed 17 Oct 2015
Arias E (2015) National Vital Statistics Reports. 64:1–63
Dea N, Fournier-Gosselin M-P, Mathieu D, Goffaux P, Fortin D (2012) Does extent of resection impact survival in patients bearing glioblastoma? Can J Neurol Sci 39:632–637
Ringel F, Pape H, Sabel M et al (2016) Clinical benefit from resection of recurrent glioblastomas: results of a multicenter study including 503 patients with recurrent glioblastomas undergoing surgical resection. Neuro Oncol 18:96–104
Number of Persons by race and Hispanic ethnicity for SEER participants (2010 census data). In: National Cancer Institute. http://seer.cancer.gov/registries/data.html. Accessed 20 Jul 2015
Acknowledgments
Funding for CBTRUS was provided by the Centers for Disease Control and Prevention (CDC) under Agreement 5U58DP00381, The Sontag Foundation, Genentech, Novocure, Celldex Therapeutics, AbbVie, along with the Musella Foundation, Elekta, the Zelda Dorin Tetenbaum Memorial Fund, as well as private and in kind donations. Contents are solely the responsibility of the authors and do not necessarily represent the official views of the CDC.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Farah, P., Blanda, R., Kromer, C. et al. Conditional survival after diagnosis with malignant brain and central nervous system tumor in the United States, 1995–2012. J Neurooncol 128, 419–429 (2016). https://doi.org/10.1007/s11060-016-2127-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-016-2127-8