Abstract
The present study evaluated usefulness of the positron emission tomography with 11C-methionine for prediction of the clinical course and treatment decision-making in adult patients with newly diagnosed non-enhancing brain lesions mimicking low-grade gliomas. Retrospective analysis was done in 163 cases. In overall, 131 tumors underwent surgical resection, which in 34 cases was done after initial period of observation. Among the latter 5 patients were operated on after significant clinical deterioration. In overall, 3 resected neoplasms corresponded to WHO histopathological grade I, 87 to grade II, 39 to grade III, and 2 to grade IV. In all 163 cases the tumor/normal brain uptake ratio (T/N ratio) of 11C-methionine ranged from 0.68 to 8.02 (mean 2.21 ± 1.16, median 1.81). Mean T/N ratios of non-operated lesions, low-grade and high-grade tumors were 1.60 ± 0.85, 2.27 ± 1.22, and 2.54 ± 1.09, respectively (P < 0.0001), but overlap between 3 groups was prominent. In patients who had clinical deterioration during the period of observation T/N ratios of the lesion varied from 1.49 to 3.38 (mean 2.23 ± 0.70, median 2.15). Comparison of the deterioration-free survival of patients with T/N ratios of the lesion above and below 1.90 revealed statistically significant difference (P < 0.0001). In conclusion, “wait-and-scan” strategy with delay of surgical treatment does not seem reasonable option if T/N ratio of 11C-methionine in the non-enhancing glioma-like brain lesion constitutes ≥1.90, since it may be associated with significant risk of tumor progression and clinical deterioration during follow-up.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Choice of the optimal treatment strategy in patients with suspected low-grade gliomas is difficult. Early surgery in such cases may reduce potential risks of malignant progression of the tumor and improve overall survival, but, on the other hand, may result in additional neurological morbidity, especially if the neoplasm is located in eloquent brain areas. Moreover, some lesions may be non-neoplastic and do not require resection. The objective of the present study was evaluation of usefulness of the positron emission tomography with 11C-methionine (MET-PET) for prediction of the clinical course and treatment decision-making in adult patients with newly diagnosed non-enhancing glioma-like brain lesions.
Materials and methods
Routine use of MET-PET for preoperative examination of patients with suspected intracranial gliomas was started by our group from 2004. During 5 subsequent years 297 consecutive examinations were done and their results were collected in constantly maintained computer database. For the purpose of this study 134 cases were excluded due to at least one of the following reasons: age of the patient less than 15 years (10 cases), residual or recurrent tumor (45 cases), presence of contrast enhancement of the lesion on T1-weighted MRI (64 cases), necessity of emergent surgery prompted by poor general condition (6 cases), and absence of the surgical treatment or additional MRI investigations within 3 months after PET examination (9 cases). The residual cohort of 163 patients represented the clinical basis of the present retrospective analysis, which was approved by the Ethics Committee of the Tokyo Women’s Medical University (#3533; August 10, 2015).
Clinical data
The study group included 98 men and 65 women. Their age varied from 16 to 72 years (mean 41 ± 13 years, median 38 years). The Karnofsky Performance Scale (KPS) score was 100 in 110 patients, 90—in 50, and 80—in 3. According to MRI examinations performed with different models of 1.5 Tesla MR scanners all lesions had hypointense signal on T1-weighted, and hyperintense signal on T2-weighted and FLAIR images. No one mass exhibited contrast enhancement after intravenous administration of the double dose (0.2 mmol/kg) of the gadolinium-based contrast media gadoteridol (ProHance®; Eisai Co., Tokyo, Japan) or gadopentetate dimeglumine (Magnevist®; Nihon Shering, Osaka, Japan).
Positron emission tomography with 11C-methionine
Applied technique of MET-PET was reported previously and published elsewhere [1–3]. Shortly, Advance NXi Imaging System (GE Yokokawa Medical Systems, Tokyo, Japan), which provides 35 transaxial images at 4.25 mm intervals, was used. The in-plane spatial resolution (full width at half maximum) was 4.8 mm, and standard 2D scan mode was utilized. Before emission scan was acquired, a 3-min transmission scan was obtained to correct photon attenuation with a ring source containing 68Ge. A dose of 7.0 MBq/kg of 11C-methionine was injected intravenously. The emission scan was acquired during 30 min, starting 5 min after radioisotope administration. The images were reconstructed with the ordered-subsets expectation maximization algorithm.
Tracer accumulation in the region of interest (ROI) was analyzed as the standardized uptake value (SUV), which is the radioisotope activity concentration in the ROI at a fixed time point divided by the injected dose normalized to the patient’s weight. The tumor/normal brain uptake ratios (T/N ratios) of 11C-methionine were calculated by dividing the maximum SUV of the lesion by the mean SUV of the contralateral normal frontal cortex. The lesion maximum SUV was used instead of the mean SUV to minimize the effect of heterogeneity of radioisotope accumulation. In all cases co-registration of PET and MRI was undertaken [4] with an image analysis software package (Dr. View; AJS, Tokyo, Japan). If increased accumulation of 11C-methionine was absent or not clear, ROI selection was done with a reference to MRI.
Treatment and follow-up
Ninety-eight patients were scheduled for elective surgery (early surgery group) within 3 months after MET-PET. In other 65 cases “wait-and-scan” strategy was chosen initially (initial observation group), which was caused either by desire of the patient and his or her family to delay or avoid surgical treatment, or by suspicion of the attending neurosurgeon that the lesion might be non-neoplastic. The patients in the latter group were advised to perform evaluation in outpatient clinic and MRI examinations (plain and contrast-enhanced T1-weighted, T2-weighted, and FLAIR images) each 3 months.
Statistics
Non-parametric statistical tests, namely Chi square test, Mann–Whitney test, and Kruskal–Wallis test, were used for groups’ comparisons as appropriate. Survival analysis was done according to Kaplan–Meier method from the day of PET investigation and cases were censored at the time of elective surgery or at last follow-up examination. Comparison of survival curves was performed with log-rank test. The level of significance was determined at P < 0.05.
Results
In all 163 patients the maximal T/N ratio on MET-PET of non-enhancing glioma-like brain lesions ranged from 0.68 to 8.02 (mean 2.21 ± 1.16, median 1.81). In overall, T/N ratio was significantly higher in early surgery group (Table 1).
Early surgery group
One patient initially scheduled for early surgery rejected it later on, but desired to undergo empirical radiochemotherapy. In 97 other patients in this group tumor removal was done within the interval from 7 days to 2.9 months (mean 1.4 ± 0.8 months, median 1.3 months) after MET-PET. According to MRI no one lesion changed its size or enhancement characteristics during the period preceding the intervention, and no one patient experienced clinical deterioration.
Initial observation group
Eventually, 34 out of 65 patients initially scheduled for observation underwent surgical resection of the lesion. It was done within the interval from 3.1 to 84.7 months (mean 13.2 ± 17.0 months, median 5.4 months) after MET-PET. In 29 cases delayed surgery was performed owed to the absence of the lesion regression and strong suspicion on the tumor presence, but without evidence of significant changes of the mass volume or contrast enhancement pattern. In other 5 patients surgery was done owed to significant deterioration of the clinical condition caused by either rapid progression of the neoplasm (3 cases) or intratumoral hemorrhage (2 cases).
Other 31 patients initially scheduled for observation were followed without surgery from 2.8 to 98.3 months (mean 44.6 ± 32.0 months, median 48.1 months) after MET-PET. According to MRI 24 of these lesions did not changed size or enhancement characteristics, whereas 7 demonstrated volume regression.
11C-methionine uptake and histopathological characteristics of the lesion
In all 131 patients, who underwent lesion resection, surgery was done within the interval from 7 days to 84.7 months (mean 4.5 ± 10 months, median 1.8 months) after MET-PET. Histopathological investigation according to current WHO criteria [5] revealed 1 dysembryoplastic neuroepithelial tumor, 1 gangliocytoma, 1 non-classified glioneuronal tumor, 16 diffuse astrocytomas, 28 oligoastrocytomas, 43 oligodendrogliomas, 13 anaplastic astrocytomas, 14 anaplastic oligoastrocytomas, 12 anaplastic oligodendrogliomas, and 2 glioblastomas. In overall, 3 neoplasms corresponded to WHO histopathological grade I, 87 to grade II, 39 to grade III, and 2 to grade IV. There was no statistically significant difference in proportions of low- and high-grade tumors among patients in early surgery and initial observation groups (P = 0.2543).
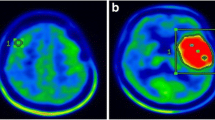
Mean T/N ratios of non-operated lesions, low-grade and high-grade tumors were 1.60 ± 0.85, 2.27 ± 1.22, and 2.54 ± 1.09, respectively. This difference was statistically significant (P < 0.0001), but overlap between 3 groups was prominent (Fig. 1). Comparison of T/N ratios in astrocytic, oligoastrocytic, and oligodendroglial gliomas consistently revealed lower radioisotope uptake in astrocytomas, but the differences reached statistical significance only in subgroup of anaplastic (WHO histopathological grade III) tumors (Table 2).
11C-methionine uptake and clinical course
As marked above, 5 patients in the initial observation group demonstrated significant deterioration of their clinical condition during follow-up. It manifested from 6 to 37.6 months (mean 27.6 ± 13.3 months, median 35.2 months) after MET-PET and prompted urgent lesion resection. In these cases T/N ratios varied from 1.49 to 3.38 (mean 2.23 ± 0.70, median 2.15). To define the optimal cut-off level for prediction of the clinical deterioration during follow-up, comparative survival analysis was done with calculation of the hazard ratios (HR) within the interval of T/N ratios from 1.40 to 3.40 with an increment of 0.10. The greatest HR (25.54) corresponded to cut-off of T/N ratio at 1.90. Comparison of the deterioration-free survival of patients with T/N ratios of the lesion above and below this cut-off level (Fig. 2) revealed statistically significant difference (P < 0.0001). Actuarial deterioration-free survival proportions of patients with T/N ratios of the lesion ≥1.90 (N = 80) at 1, 2, and 3 years after MET-PET were 0.89 ± 0.12, 0.71 ± 0.19, and 0.27 ± 0.23, respectively. In contrast, deterioration was noted in only one patient with T/N ratio < 1.90 (N = 83), and it had happened at 3.1 years after MET-PET.
On the other hand, in 7 other patients in the initial observation group regression of the lesion was noted within the interval from 5.8 to 87.9 months (mean 40.1 ± 36.3 months, median 18.1 months) after MET PET. In these cases T/N ratios varied from 0.90 to 1.80 (mean 1.38 ± 0.36, median 1.31). To define the optimal cut-off level for prediction of the lesion regression during follow-up, comparative survival analysis was done with calculations of HR within the interval of T/N ratios from 0.90 to 1.80 with an increment of 0.10. The greatest HR (2.93) corresponded to cut-off of T/N ratio at 1.00. However, comparison of lesion regressions in subgroups with T/N ratio above and below this cut-off level (Fig. 3) did not reveal statistically significant difference (P = 0.2846). Actuarial proportions of non-regressed lesions in cases with T/N ratios ≥1.00 (N = 152) at 1, 2, and 3 years after MET-PET were 0.98 ± 0.03, 0.91 ± 0.05, and 0.91 ± 0.06, respectively. In contrast, in cases with T/N ratio <1.00 (N = 11) actuarial proportions of non-regressed lesions at 1, 2, and 3 years after MET-PET were 0.75 ± 0.22, 0.75 ± 0.38, and 0.75 ± 0.38, respectively.
Discussion
Low-grade gliomas in adults are typically presenting as non-enhancing mass lesions located within the cerebral hemispheres. Despite slow growth, more than 50 % of these tumors may eventually undergo malignant transformation, which usually occurs in 5–7 years after the initial diagnosis [6, 7]. Additionally, the clinical course of more than 10 % of such neoplasms may be complicated by intratumoral hemorrhage [8]. Therefore, establishment of the correct diagnosis and timely treatment of patients with low-grade gliomas seems very important for improvement of their prognosis. Nevertheless, non-negligible proportion of non-enhancing brain lesions may result from ischemia, demyelination, inflammation, trauma, and dysplasia and do not require any intervention [9–12]. For differentiation of the neoplastic and non-neoplastic pathology, it is rather usual to observe the patient until the evident growth of the lesion or appearance of symptoms. It is particularly common practice in cases of lesions with unequivocal radiological findings, located within eloquent cortical areas or deep brain structures. However, in cases of tumors such “wait-and-scan” strategy may result in time loss, non-reasonable delay of surgery, and attainment of resection under less optimal conditions [13]. It emphasizes the role of advanced neuroimaging technologies for establishment of the correct preoperative diagnosis and prediction of prognosis.
At present MET-PET tracer is widely considered as effective technique for clinical evaluation of gliomas [14]. It had been used for discrimination between the tumor and non-neoplastic lesions [15, 16], non-invasive preoperative typing and grading of the neoplasm [17–20], precise delineation of its borders [21–23], prediction of prognosis [17, 18, 24, 25], detection of malignant transformation [26], and differentiation of recurrence from treatment-induced changes [16, 27–29]. Multiple reports noted usefulness of MET-PET for detection of gliomas with the range of sensitivity between 70 and 100 %, however recommended cut-off values of T/N ratios ranged widely (from 1.3 to 1.9) [14, 19, 28, 29]. Previously in our practice cut-off value of 2.0 was applied for discrimination of high- and low-uptake lesions and provided 87 % sensitivity for identification of glioma presence [1]. It is evident, however, that setting of the cut-off value at a lower level may increase sensitivity of the tumor diagnosis, but decrease its specificity with the greater risk for unnecessary interventions in cases of non-surgical diseases. In the series of Kawai et al. [11] various non-neoplastic intracranial pathology, including intracerebral hemorrhages, cerebral infarctions, brain abscesses, multiple sclerosis, Behçet disease, etc. demonstrated mild-to-moderate uptake of 11C-methionine, whereas a single case of hypertrophic pachymeningitis even exhibited a strong uptake. Harada et al. [12] reported a case of cerebral venous infarction mimicking glioma on MET-PET with T/N ratio of 1.69.
As was demonstrated herein MET-PET may also provide additional clues for appropriate decision-making in patients with non-enhancing glioma-like brain lesions. Clinical deterioration during the course of observation was significantly more frequent in cases with T/N ratios ≥1.90, and no one such lesion underwent spontaneous regression. In contrast, no one patient with T/N ratio < 1.90 demonstrated clinical impairment within 3 years after radiological diagnosis, and 11 % of the lesions showed volume reduction. Greater risk of deterioration of high-uptake lesions may be related to their greater proliferative activity and vascularization. Several studies demonstrated correlation of 11C-methionine uptake with MIB-1 index [2, 16] and microvessel density in gliomas [30, 31]. Ullrich et al. [26] reported association between accumulation rate of the radioisotope and immunohistochemical expression of the vascular endothelial growth factor (VEGF), which is considered as major promoter of neovascularization in gliomas corresponding to intratumoral hemorrhages and malignant transformation [32–34]. Others demonstrated that 11C-methionine uptake also correlates with tumor cell density [35], MGMT promoter methylation [36], and 1p/19q co-deletion [3].
Based on the presented results intracranial glioma-like brain lesions demonstrating high radioisotope uptake on MET-PET (T/N ratios ≥ 1.90) should preferably undergo early surgical resection (within 3 months after radiological diagnosis) for avoidance of the possible deterioration and improvement of prognosis. In the same time more or less prolonged observation of the low-uptake masses (T/N ratios < 1.90) with regular MRI scans may be associated with minimal risk of clinical impairment. It may permit to distinguish non-neoplastic, tumor-mimicking diseases and to avoid unnecessary surgery in some cases. Definitely, stereotactic biopsy may be applied in the latter cohort instead of “wait-and-scan” strategy, but in many occasions it may leave some diagnostic uncertainty owed to histopathological heterogeneity of gliomas [37]. In such cases, MET-PET may be effectively used either for selection of the optimal target for tissue sampling [38], or as additional prognostic marker to support tissue diagnosis [14, 17, 24, 25].
The main limitation of the present study is its retrospective nature and small number of events of interest. It is not possible to define clearly how the patients were selected for early or delayed surgical procedures. Moreover, since histopathological diagnosis of glioma was established in all operated cases, the preoperative neuroradiological findings should be rather convincing. Other used diagnostic modalities, such as diffusion-weighted imaging and proton magnetic resonance spectroscopy, were not analyzed. It should be also noted, that PET is costly technique, mainly available only in the large academic centers, which may preclude widespread application of the proposed diagnostic algorithm.
Conclusion
According to results of the present retrospective study MET-PET may be useful for prediction of the clinical course in adult patients with newly diagnosed non-enhancing glioma-like brain lesions, which may be helpful for treatment decision-making. “Wait-and-scan” strategy with delay of surgical treatment does not seem reasonable option if tumor/normal brain uptake ratio of 11C-methionine in the mass constitutes ≥1.90, since it may be associated with significant risk of tumor progression and clinical deterioration during follow-up and with negligible probability of spontaneous lesion regression. Nevertheless, validation of the suggested MET-PET-based diagnostic algorithm should be done in further prospective studies.
References
Kato T, Shinoda J, Nakayama N, Miwa K, Okumura A, Yano H, Yoshimura S, Maruyama T, Muragaki Y, Iwama T (2008) Metabolic assessment of gliomas using 11C-methionine, [18F] fluorodeoxyglucose, and 11C-choline positron-emission tomography. AJNR Am J Neuroradiol 29:1176–1182
Kato T, Shinoda J, Oka N, Miwa K, Nakayama N, Yano H, Maruyama T, Muragaki Y, Iwama T (2008) Analysis of 11C-methionine uptake in low-grade gliomas and correlation with proliferative activity. AJNR Am J Neuroradiol 29:1867–1871
Saito T, Maruyama T, Muragaki Y, Tanaka M, Nitta M, Shinoda J, Aki T, Iseki H, Kurisu K, Okada Y (2013) 11C-methionine uptake correlates with combined 1p and 19q loss of heterozygosity in oligodendroglial tumors. AJNR Am J Neuroradiol 34:85–91
Kapouleas I, Alavi A, Alves WM, Gur RE, Weiss DW (1991) Registration of three-dimensional MR and PET images of the human brain without markers. Radiology 181:731–739
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK (eds) (2007) WHO classification of tumours of the central nervous system, 4th edn. IARC Press, Lyon
Recht L, Lew R, Smith T (1992) Suspected low-grade glioma: is deferring treatment safe? Ann Neurol 31:431–436
Agulnik M, Mason W (2006) The changing management of low-grade astrocytomas and oligodendrogliomas. Hematol Oncol Clin N Am 20:1249–1266
Kondziolka D, Bernstein M, Resch L, Tator CH, Fleming JF, Vanderlinden RG, Schutz H (1987) Significance of hemorrhage into brain tumors: clinicopathological study. J Neurosurg 67:852–857
Koh M, Goh K, Chen C, Howe H (2002) Cerebral infarct mimicking glioma in Sjogren’s syndrome. Hong Kong Med J 8:292–294
Mandrioli J, Ficarra G, Callari G, Sola P, Merelli E (2004) Monofocal acute large demyelinating lesion mimicking brain glioma. Neurol Sci 25(Suppl 4):S386–S388
Kawai N, Okauchi M, Miyake K, Sasakawa Y, Yamamoto Y, Nishiyama Y, Tamiya T (2010) 11C-methionine positron emission tomography in nontumorous brain lesions. No Shinkei Geka 38:985–995 (in Japanese)
Harada Y, Hirata K, Kobayashi H, Usui R, Shiga T, Terae S, Shirato H, Tamaki N (2012) A pitfall of C-11 methionine PET: cerebral venous infarction mimicked a glioma. Clin Nucl Med 37:110–111
Sanai N, Chang S, Berger MS (2011) Low-grade gliomas in adults. J Neurosurg 115:948–965
Glaudemans AWJM, Enting RH, Heesters MAAM, Dierckx RAJO, van Rheenen RWJ, Walenkamp AME, Slart RHJA (2013) Value of 11C-methionine PET in imaging brain tumors and metastases. Eur J Nucl Med Mol Imaging 40:615–635
Herholz K, Hölzer T, Bauer B, Schröder R, Voges J, Ernestus R, Mendoza G, Weber-Luxenburger G, Lottgen J, Thiel A, Wienhard K, Heiss WD (1998) 11C-methionine PET for differential diagnosis of low-grade gliomas. Neurology 50:1316–1322
Chung J, Kim Y, Kim S, Lee Y, Paek S, Yeo J, Jeong JM, Lee DS, Jung HW, Lee MC (2002) Usefulness of 11C-methionine PET in the evaluation of brain lesions that are hypo- or isometabolic on 18F-FDG PET. Eur J Nucl Med Mol Imaging 29:176–182
Nariai T, Tanaka Y, Wakimoto H, Aoyagi M, Tamaki M, Ishiwata K, Senda M, Ishii K, Hirakawa K, Ohno K (2005) Usefulness of L-[methyl-11C] methionine-positron emission tomography as a biological monitoring tool in the treatment of glioma. J Neurosurg 103:498–507
Ceyssens S, Van Laere K, de Groot T, Goffin J, Bormans G, Mortelmans L (2006) [11C]methionine PET, histopathology, and survival in primary brain tumors and recurrence. AJNR Am J Neuroradiol 27:1432–1437
Galldiks N, Kracht LW, Dunkl V, Ullrich RT, Vollmar S, Jacobs AH, Fink GR, Schroeter M (2011) Imaging of non- or very subtle contrast-enhancing malignant gliomas with [11C]-methionine positron emission tomography. Mol Imaging 10:453–459
Shinozaki N, Uchino Y, Yoshikawa K, Matsutani T, Hasegawa A, Saeki N, Iwadate Y (2011) Discrimination between low-grade oligodendrogliomas and diffuse astrocytoma with the aid of 11C-methionine positron emission tomography. J Neurosurg 114:1640–1647
Braun V, Dempf S, Weller R, Reske S, Schachenmayr W, Richter H (2002) Cranial neuronavigation with direct integration of 11C methionine positron emission tomography (PET) data—results of a pilot study in 32 surgical cases. Acta Neurochir (Wien) 144:777–782
Kracht L, Miletic H, Busch S, Jacobs A, Voges J, Hoevels M, Klein JC, Herholz K, Heiss WD (2004) Delineation of brain tumor extent with [11C]l-methionine positron emission tomography: local comparison with stereotactic histopathology. Clin Cancer Res 10:7163–7170
Miwa K, Shinoda J, Yano H, Okumura A, Iwama T, Nakashima T, Sakai N (2004) Discrepancy between lesion distributions on methionine PET and MR images in patients with glioblastoma multiforme: insight from a PET and MR fusion image study. J Neurol Neurosurg Psychiatry 75:1457–1462
De Witte O, Goldberg I, Wikler D, Rorive S, Damhaut P, Monclus M, Salmon I, Brotchi J, Goldman S (2001) Positron emission tomography with injection of methionine as a prognostic factor in glioma. J Neurosurg 95:746–750
Smits A, Westerberg E, Ribom D (2008) Adding 11C-methionine PET to the EORTC prognostic factors in grade 2 gliomas. Eur J Nucl Med Mol Imaging 35:65–71
Ullrich RT, Kracht L, Brunn A, Herholz K, Frommolt P, Miletic H, Deckert M, Heiss WD, Jacobs AH (2009) Methyl-L-11C-methionine PET as a diagnostic marker for malignant progression in patients with glioma. J Nucl Med 50:1962–1968
Terakawa Y, Tsuyuguchi N, Iwai Y, Yamanaka K, Higashiyama S, Takami T, Ohata K (2008) Diagnostic accuracy of 11C-methionine PET for differentiation of recurrent brain tumors from radiation necrosis after radiotherapy. J Nucl Med 49:694–699
Tripathi M, Sharma R, Varshney R, Jaimini A, Jain J, Souza MM, Bal J, Pandey S, Kumar N, Mishra AK, Mondal A (2012) Comparison of F-18 FDG and C-11 methionine PET/CT for the evaluation of recurrent primary brain tumors. Clin Nucl Med 37:158–163
Nihashi T, Dahabreh IJ, Terasawa T (2013) Diagnostic accuracy of PET for recurrent glioma diagnosis: a meta-analysis. AJNR Am J Neuroradiol 34:944–950
Kracht LW, Friese M, Herholz K, Schroeder R, Bauer B, Jacobs A, Heiss WD (2003) Methyl-[11C]-l-methionine uptake as measured by positron emission tomography correlates to microvessel density in patients with glioma. Eur J Nucl Med Mol Imaging 30:868–873
Viel T, Boehm-Sturm P, Rapic S, Monfared P, Neumaier B, Hoehn M, Jacobs AH (2013) Non-invasive imaging of glioma vessel size and densities in correlation with tumour cell proliferation by small animal PET and MRI. Eur J Nucl Med Mol Imaging 40:1595–1606
Cheng S, Nagane M, Huang H, Cavenee W (1997) Intracerebral tumor-associated hemorrhage caused by overexpression of the vascular endothelial growth factor isoforms VEGF121 and VEGF165 but not VEGF189. Proc Natl Acad Sci USA 94:12081–12087
Abdulrauf S, Edvardsen K, Ho K, Yang X, Rock J, Rosenblum M (1998) Vascular endothelial growth factor expression and vascular density as prognostic markers of survival in patients with low-grade astrocytoma. J Neurosurg 88:513–520
Schmidt N, Westphal M, Hagel C, Ergün S, Stavrou D, Rosen E, Lamszus K (1999) Levels of vascular endothelial growth factor, hepatocyte growth factor/scatter factor and basic fibroblast growth factor in human gliomas and their relation to angiogenesis. Int J Cancer 84:10–18
Okita Y, Kinoshita M, Goto T, Kagawa N, Kishima H, Shimosegawa E, Hatazawa J, Hashimoto N, Yoshimine T (2010) 11C-methionine uptake correlates with tumor cell density rather than with microvessel density in glioma: a stereotactic image-histology comparison. Neuroimage 49:2977–2982
Okita Y, Nonaka M, Shofuda T, Kanematsu D, Yoshioka E, Kodama Y, Mano M, Nakajima S, Kanemura Y (2014) 11C-methinine uptake correlates with MGMT promoter methylation in nonenhancing gliomas. Clin Neurol Neurosurg 125:212–216
Muragaki Y, Chernov M, Maruyama T, Ochiai T, Taira T, Kubo O, Nakamura R, Iseki H, Hori T, Takakura K (2008) Low-grade glioma on stereotactic biopsy: how often is the diagnosis accurate? Minim Invasive Neurosurg 51:275–279
Massager N, David P, Goldman S, Pirotte B, Wikler D, Salmon I, Nagy N, Brotchi J, Levivier M (2000) Combined magnetic resonance imaging- and positron emission tomography-guided stereotactic biopsy in brainstem mass lesions: diagnostic yield in a series of 30 patients. J Neurosurg 93:951–957
Acknowledgments
The authors are thankful to Drs. Tatsuki Aki, Soko Ikuta, Takayuki Kato, Osami Kubo, Kazuhiro Miwa, Noriyuki Nakayama, Naoki Oka, Shunsuke Takenaka, Shingo Yonezawa, and Mikhail Chernov for their help during the study and manuscript preparation.
Grant support
This study was supported by grants from the Japan National Cancer Research and Development Fund and Core Research for Evolutional Science and Technology (CREST), Japan Science and Technology Agency.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This study contains no conflict of interests.
Rights and permissions
About this article
Cite this article
Watanabe, A., Muragaki, Y., Maruyama, T. et al. Usefulness of 11C-methionine positron emission tomography for treatment-decision making in cases of non-enhancing glioma-like brain lesions. J Neurooncol 126, 577–583 (2016). https://doi.org/10.1007/s11060-015-2004-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-015-2004-x