Abstract
Glioblastoma (GBM) is the most common primary malignant brain tumor. Microvascular proliferation is one of the characteristic pathologic features of GBM. Mitochondrial dysfunction plays an important role in the pathogenesis of GBM. In this study, microvascular proliferation from GBM and normal brain blood vessels were laser microdissected and total RNA was isolated from these microvasculatures. The difference of mRNA expression profiles among GBM microvasculature, normal brain blood vessels and GBM tumor cells was evaluated by mitochondria and metabolism PCR gene arrays. It was found that the mRNA levels of ATP5A1 and ATP5B in GBM tumor cells as well as microvascular proliferation were significantly higher compared with normal brain blood vessels. Immunohistochemical stains with anti-ATP5A1 antibody or anti-ATP5B antibody were performed on tissue microarray, which demonstrated strongly positive expression of ATP5A1 and ATP5B in GBM tumor cells and GBM microvascular proliferation while normal blood vessels were negative. By analyzing The Cancer Genome Atlas data sets for GBM and other cancers, genomic DNA alterations (mutation, amplification or deletion) were less likely the reason for the high expression of ATP5A1 and ATP5B in GBM. Our miRNA microarray data showed that miRNAs that target ATP5A1 or ATP5B were down-regulated, which might be the most likely reason for the high expression of ATP5A1 and ATP5B in GBM tumor cells and microvascular proliferation. These findings help us better understand the pathogenesis of GBM, and agents against ATP5A1 and/or ATP5B might effectively kill both tumor cells and microvascular proliferation in GBM. MiRNAs, such as Let-7f, miR-16, miR-23, miR-100 and miR-101, that target ATP5A1 or ATP5B, might be potential therapeutic agents for GBM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma (GBM) (WHO grade IV) is the most common and highly malignant primary brain tumor. GBM comprises 50–60 % of all gliomas. The median survival time for GBM patients is about 15 months despite aggressive multimodality therapy. Pseudopalisading necrosis and microvascular proliferation are characteristic pathologic features for GBM that distinguish GBM from lower grade astrocytomas [1]. During last few decades, almost all chemotherapeutic agents are only targeted on GBM tumor cells but not on tumor microenvironments. Targeted anti-angiogenic therapy with Avastin, a monoclonal antibody against vascular endothelial growth factor, induces temporary tumor remission on MRI, but does not significantly prolong the overall survival time [2]. In combined therapy with temozolomide and anti-angiogenic agent for gliomas, it is found that Avastin can restore the blood–brain barrier in the GBM microvasculature which reduces the permeability of temozolomide [3]. Thorough investigation of the nature of endothelial cells in microvascular proliferation is essential to develop more effective targeted therapy.
Mitochondria are essential cellular organelles in normal cells and neoplastic cells, which are involved in numerous complicated physiological processes such as energy generation, cell proliferation and apoptosis [4]. Each of the oxidative phosphorylation enzymes in mitochondria, Complexes I–V, is a multi-subunit enzyme coded by mtDNA and/or nDNA [5]. Although GBM, like other cancer cells, favor abnormal energy production via aerobic glycolysis [6, 7], it becomes more and more evident that mitochondrial dysfunction plays an important role in the pathogenesis of GBM [8–10].
In this study, we investigated the difference of mRNA expression profiles among GBM microvasculature, normal brain blood vessels and GBM tumor cells using Human Mitochondrial Energy Metabolism PCR Arrays. The mRNA array results were validated by immunohistochemistry on tissue microarray. We also explored the reason that cause the high expression of ATP5A1 and ATP5B in GBM microvasculature and tumor cells by genomic DNA analysis using The Cancer Genome Atlas data and microRNA (miRNA) analysis.
Materials and methods
Laser-capture microdissection
IRB approval for this study was obtained from the North Shore and Long Island Jewish Health System Institutional Review Board. All formalin-fixed, paraffin-embedded (FFPE) tissue specimens used in this study were collected as part of standard clinical care and were considered to be leftover and unnecessary for patient treatment. To obtain microvascular proliferation in GBM (7 cases) and normal blood vessels in normal brain (4 cases), laser-capture microdissection (LCM) (Leica LMD7000) was performed on FFPE samples. Five μm sections of human tissue were cut at room temperature and transferred to PEN-membrane, 4.0 µm slides (Leica) for LCM. About 10,000 cells were laser microdissected from microvascular proliferation in GBM and normal blood vessels in normal brain.
Total RNA isolation
Total RNA was extracted from the microdissected samples and the GBM tissue sections after microvascular proliferation microdissection using miRNeasy FFPE Kit (Qiagen) as per the manufacturer’s instructions. RNA was quantified using a Nanodrop 1000 spectrophotometer v3.3 (Thermo Scientific).
Mitochondrial energy metabolism plus PCR Arrays
cDNA synthesis was performed with 160 ng RNA in a final volume of 10 μl using First-Strand cDNA synthesis kit (Qiagen), following the manufacturer’s instructions. cDNA was preamplified using RT2 PreAMP cDNA Synthesis Kit (Qiagen), and Human Mitochondrial Energy Metabolism Plus Primer Mix (Qiagen) as primers. Preamplified cDNA was applied to Human Mitochondrial Energy Metabolism Plus 384-well format RT2 Profiler PCR Arrays (Qiagen). qPCR was performed as per the manufacturer’s instructions using RT2 SYBR® Green qPCR Mastermix (Qiagen) on a LightCycler® 480 Instrument II (Roche), and Ct values were obtained by performing data analysis using LightCycler®480 Software (Roche). ΔΔCt-based fold-change and statistical significance analysis was performed using the Integrated Web-based Software Package for the PCR Array System at the GeneGlobe Data Analysis Center on the Qiagen website.
Construction of glioma tissue microarray
Glioma samples were obtained from patients who had undergone surgery at our institution from 2004 through 2015. The formalin-fixed paraffin-embedded archival tissue blocks were retrieved and matching hematoxylin and eosin stained slides were screened for representative tumor regions by a neuropathologist. For GBM cases, areas with microvascular proliferation were selected. The tissue microarrays (TMA) were constructed from selected gliomas using a microarrayer (Beecher Instruments) as described previously [11]. The TMA included 42 GBM, 10 low-grade astrocytomas, 8 oligodendrogliomas and 6 normal brain tissues. Each specimen was sampled in duplicate from representative areas of either one or two donor blocks using a 1.5-mm punch.
Immunohistochemistry
A standard indirect immunoperoxidase procedure (Pierce™ Peroxidase IHC Detection Kit, Thermo Scientific Pierce) was followed as per the manufacturer’s instructions. Antigen retrieval was performed. Antibodies against ATP5A1 (Rabbit monocolonal anti-ATP5A1 antibody, ABCAM) (1:50 dilution) or ATP5B (Rabbit monocolonal anti-ATPB antibody, ABCAM) (1:100 dilution) were overlaid on tissue microarray sections and incubated overnight at 4 °C. Slides were incubated with HRP-conjugated goat anti-Rabbit secondary antibody (1:500 dilution) at room temperature for 30 min. The Metal Enhanced DAB Substrate Working Solution (Thermo Scientific) was added to the tissue and incubated until the desired staining was achieved. Immunohistochemical stains for ATP5A1 or ATPB were blindedly evaluated by a neuropathologist and placed into one of two categories: positive or negative. Negative was defined as very weak-to-absent staining, or less than 25 % strongly reacting tumor cells. Positive was defined as strong reaction in ≥25 % of tumor cells.
Genomic DNA mutation and amplification analysis using The Cancer Genome Atlas (TCGA) data
In order to see whether the high expression of ATP5A1 or ATP5B in gliobastoma was due to gene mutation or amplification, we went to Memorial Sloan-Kettering Cancer Center cBioPortal for Cancer Genomics web site (http://www.cbioportal.org/index.do). We searched the genetic alterations for both ATP5A1 and ATP5B genes in 14 TCGA databases including two GBM databases [12, 13].
Human Cancer Pathway Finder 384HC microRNA arrays
For GBM samples, 500 ng total RNA were converted to cNDA using miScript II RT Kit (Qiagen) with its HiSpec Buffer. For blood vessels, 100 ng total RNA were converted to cDNA using HiSpec Buffer, then the cDNA was preamplified using miScript PreAMP PCR Kit (Qiagen) and miScript PreAMP Premer Mixes for Human Cancer Pathway Finder 384HC (MBHS-3102Z, Qiagen). Real-Time PCR was done with miScript SYBR® Green PCR Kit (Qiagen) and miScript miRNA PCR Array for Human Cancer Pathway Finder 384HC (Qiagen) on a LightCycler® 480 Instrument II. Ct values were obtained by performing data analysis using LightCycler®480 Software. ΔΔCt-based fold-change and statistical significance analysis were performed using the Integrated Web-based Software Package for the PCR Array System at the GeneGlobe Data Analysis Center on the Qiagen website. A list of miRNAs that target ATP5A1 or ATP5B was generated by searching from miRTarBase (http://mirtarbase.mbc.nctu.edu.tw/), the experimentally validated microRNA-target interactions database [14], and then the expression levels of these miRNA from our miRNA array data were evaluated.
Result
High mRNA levels of ATP5A1 and ATP5B in tumor cells and microvascaular proliferation in GBM
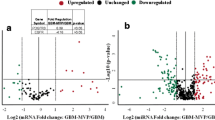
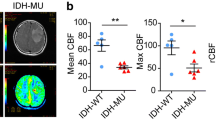
Total RNA was extracted from brain blood vessels, GBM microvascular proliferation and GBM tissue sections after microvascular proliferation microdissection. Total RNA was used for Human Mitochondrial Energy Metabolism Plus RT2 Profiler PCR Array, which profiled the expression of 84 key genes involved in mitochondrial respiration, including genes encoding components of the electron transport chain and oxidative phosphorylation complexes. After data analysis, the volcano plots of the signal intensities between GBM microvasculature and normal brain blood vessels, and between GBM and normal brain blood vessels were generated (Fig. 1a, b). The mRNA levels of ATP5A1 (Fold change = 14.35, p < 0.01) and ATP5B (Fold change = 10.56, p < 0.01) were significantly higher in GBM microvasculature than normal brain blood vessels. The mRNA levels of ATP5A1 (Fold change = 22.45, p < 0.01) and ATP5B (Fold change = 11.17, p < 0.01) were also significantly higher in GBM than normal brain blood vessels. NDUFS6 was also statistically significantly up-regulated in both GBM tumor cells and microvascular proliferation compared to normal blood vessels (Fold change >3.00, p < 0.05). ATP5H, ATP5I, ATP5J, COX6B1, COX7A2L, COX7B, NDUFA3, NDUFAB1, NDUFB5, NDUFS4, SDHA, UQCRC2 and HSPA1A were statistically significantly down-regulated in both GBM tumor cells and microvascular proliferation compared to normal blood vessels (Fold change <−3.00, p < 0.05).
The volcano plots of PCR mRNA arrays and microRNA arrays. a The volcano plot of the signal intensities between GBM microvascular proliferation and normal brain blood vessels in the Human Mitochondrial Energy Metabolism plus PCR mRNA arrays. b The volcano plot of the signal intensities between GBM and normal brain blood vessels in the Human Mitochondrial Energy Metabolism plus PCR mRNA arrays. c The volcano plot of the signal intensities between GBM microvascular proliferation and normal brain blood vessels in Human Cancer Pathway Finder 384HC MicroRNA arrays. d The volcano plot of the signal intensities between GBM and normal brain blood vessels in Human Cancer Pathway Finder 384HC MicroRNA arrays. Statistical significance and fold-changes are displayed on the y- and x-axes, respectively. Red dots and green dots represent outliers beyond the ±3 fold changes for mRNA arrays. Yellow dots and blue dots represent outliers beyond the ±2 fold changes for microRNA arrays
High expression of ATP5A1 and ATP5B proteins in tumor cells and endothelial cells of microvascaular proliferation in GBM
Immunohistochemical stains by anti-ATP5A1 and anti-ATP5B antibodies were performed on tissue microarrays. It was found that 39 out of 42 GBM cases were positive for ATP5A1 with strong and diffuse cytoplasmic staining, and 41 out of 42 GBM cases were positive for ATP5B with strong and diffuse cytoplasmic staining (Fig. 2). Endothelial cells of microvascular proliferation in all GBM cases were strongly positive for ATP5A1 and ATP5B while normal brain blood vessels were negative for both ATP5A1 and ATP5B (Fig. 3). In low-grade astrocytoma cases, 6 out of 10 cases were positive for ATP5A1, and 9 out of 10 cases were positive for ATP5B. In low-grade oligodendroglioma cases, 4 out of 8 cases were positive for ATP5A1, and 5 out of 8 cases were positive for ATP5B (Fig. 3).
ATP5A1 and ATP5B immunohistochemical stains in glioblastomas. a, b Hematoxylin and eosin stain (H&E stain) shows GBM with hypercellularity, nuclear pleomorphism and microvascular proliferation (400×). c ATP5A1 immunohistochemical stain demonstrates that GBM tumor cells and microvascular proliferation are strongly and diffusely positive for ATP5A1 (400×). d ATP5B immunohistochemical stain reveals that GBM tumor cells and microvascular proliferation are strongly and diffusely positive for ATP5B (400×)
ATP5A1 and ATP5B immunohistochemical stains in low grade gliomas and normal brain blood vessels. a Hematoxylin and eosin stain (H&E stain) shows a low-grade astrocytoma with mildly cellularity, and hyperchromatic and irregular nuclei (400×). b H&E stain demonstrates a low-grade oligodendroglioma with mildly cellularity, round and uniform nuclei and perinuclear halos (400×). c ATP5A1 immunohistochemical stain shows that astrocytoma tumor cells are strongly and diffusely positive for ATP5A1 (400×). d ATP5A1 immunohistochemical stain demonstrates that oligodendroglioma tumor cells are negative for ATP5A1 (400×). e ATP5B immunohistochemical stain reveals that astrocytoma tumor cells are strongly and diffusely positive for ATP5B (400×). f ATP5B immunohistochemical stain demonstrates that oligodendroglioma tumor cells are negative for ATP5B (400×). g ATP5A1 immunohistochemical stain shows that normal brain blood vessels are negative for ATP5A1. 400×. h ATP5B immunohistochemical stain demonstrates that normal brain blood vessels are negative for ATP5B (400×)
Genomic DNA mutation or amplification less likely was the reason for the high expression of ATP5A1 and ATP5B in GBM
We searched the genetic alterations for both ATP5A1 and ATP5B genes in 14 TCGA data sets including two GBM databases from The Memorial Sloan-Kettering Cancer Center cBioPortal for Cancer Genomics web site [12, 13]. Ten out of 14 data sets showed genetics alteration for ATP5A1 gene (Fig. 4a). ATP5A1 mutation occurred in a small percentage of breast invasive carcinoma, GBM, renal clear cell carcinoma, stomach adenocarcinoma, bladder urothelial carcinoma, lung adenocarcinoma, lung squamous cell carcinoma (SCC), uterine endometrioid carcinoma and colorectal adenocarcinoma (0.2–2.4 %) (Fig. 4a). ATP5A1 gene was amplified in a small percentage of breast invasive carcinoma, colorectal adenocarcinoma, endometrioid carcinoma, urothelial carcinoma, lung SCC and ovarian serous carcinoma (0.2–1.9 %) (Fig. 4a). One out of 281 GBM cases (0.4 %) had ATP5A1 A282S mutation with low ATP5A1 mRNA expression in the data sets. Twelve out of 14 data sets demonstrated genetics alteration for ATP5B gene (Fig. 4b). ATP5B mutation was noted in a small percentage of breast invasive carcinoma, GBM, lung adenocarcinoma, renal clear cell carcinoma, lung SCC, endometrioid carcinoma, colorectal adenocarcinoma, urothelial carcinoma and stomach adenocarcinoma (0.2–1.7 %) (Fig. 4b). There was ATP5B gene amplification in a small percentage of breast invasive carcinoma, papillary thyroid carcinoma, stomach adenocarcinoma, GBM (1/91 in TCGA 2008, 4/281 in TCGA 2013), ovarian serous carcinoma and lung adenocarcinoma (0.2–3.5 %) (Fig. 4b). One out of 281 GBM cases (0.4 %) had ATP5B S386L mutation and exhibited average ATP5B mRNA expression in the data sets. Those GBM cases with ATP5B gene amplification in the data sets did show a moderate to marked increase in ATP5B mRNA expression. Since very small percentage of GBM cases in these large data sets had ATP5A1 and ATP5B mutation or amplification, and no case had deletion of these two genes, genomic DNA alterations less likely were the reason for the high expression of ATP5A1 and ATP5B in GBM.
Cross-cancer alteration summary for ATP5A1 and ATP5B1. a Cross-cancer alteration summary for ATP5A1 in The Cancer Genome Atlas (TCGA) data at cBioPortal for Cancer Genomics. b Cross-cancer alteration summary for ATP5B in The Cancer Genome Atlas (TCGA) data at cBioPortal for Cancer Genomics. AML-Acute myeloid leukemia, Bladder- Bladder urothelial carcinoma, Colorectal- Colorectal adenocarcinoma, chRCC- Chromophobe renal cell carcinoma, ccRCC- Clear cell renal cell carcinoma, Lung adeno-Lung adenocarcinoma, Ovarian-Ovarian serous carcinoma, Thyroid–Thyroid papillary carcinoma, Stomach–Stomach-adenocarcinoma, Uterine–Uterine endometrioid carcinoma
Multiple miRNAs targeting ATP5A1 or ATP5B in tumor cells and microvascular proliferation in GBM were significantly decreased
In order to evaluate miRNAs that target ATP5A1 or ATP5B, total RNA from the same specimens used for mRNA array was used for Human Cancer Pathway Finder 384HC MicroRNA Array analysis, which profiled the expression of 372 miRNAs differentially expressed in tumors versus normal tissue. After data analysis, the volcano plots of the signal intensities of different miRNAs between GBM microvasculature and normal brain blood vessels, and between GBM and normal brain blood vessels were generated (Fig. 1c, d). A list of miRNAs that target ATP5A1 or ATP5B was produced by searching from miRTarBase [14], and then the expression levels of these miRNA from our Human Cancer Pathway Finder 384HC MicroRNA array data were evaluated. Five miRNAs (miR-16-5p, miR-23a-3p, miR-23b-3p, miR-26a-5p and miR-100-5p) targeting ATP5A1 mRNA were significantly down-regulated in GBM microvascular proliferation (ranging from −2.38 to −32.51) and GBM tumor cells (ranging from −2.85 to −25.69) compared to normal brain blood vessels (p < 0.01) (Table 1). Six miRNAs (let-7f-5p, miR-24-3p, miR-101-3p, miR-125b-5p, miR-193b-3p and miR-331-3p) that target ATP5B mRNA were significantly down-regulated in GBM microvascular proliferation (ranging from −2.93 to −40.63) compared to normal blood vessels in brain (p < 0.01); 6 miRNAs (let-7f-5p, miR-24-3p, miR-125b-5p, miR-320a, miR-423-5p and miR-744-5p) that target ATP5B mRNA were significantly down-regulated in GBM tumor cells (ranging from −1.63 to −7.07) compared to normal brain blood vessels (p < 0.01 or p < 0.05) (Table 1).
Discussion
Glioblasotma (GBM) and other cancers are primarily considered as a disease of energy metabolism [15]. More and more researchers are becoming interested in functional processes linked to mitochondrial regulation in GBM [16]. By mitochondrial proteomics assay, Deighton, RF et al. [10] find 117 mitochondrial proteins are increased in GBM, which are associated with oxidative damage, such as catalase, superoxide dismutase 2, peroxiredoxin 1 and peroxiredoxin 4. There is a decrease in many proteins (especially respiratory chain proteins, including 23 complex-I proteins) involved in energy metabolism. Mitochondrial ATP synthase consists of 5 different subunits (alpha, beta, gamma, delta, and epsilon). ATP5A1 and ATP5B genes encode the 553 amino acid α-subunit and the 529 amino acid β-subunit respectively. Using RT-PCR, ATP5B gene expressions are found significantly higher in colorectal cancer tissues [17]. In in vitro study, the deficiency of D-(+)-glucose can induce the expression of ATP5A1 in human MDA-MB-231 breast cancer cells [18]. So far, there is no publication regarding the expression of ATP5A1 and ATP5B in glioma. Our study shows that there is a statistically significant increase in the expression of ATP5A1 or ATP5B in GBM tumor cells and GBM microvascular proliferation at mRNA and protein levels compared to normal brain blood vessels. The elevation of ATP5A1 and ATP5B in GBM is most likely due to an attempt to meet the high demand for ATP in this highly proliferative tumor. Since ATP5A1 and ATP5B proteins are highly expressed in more than half of low-grade gliomas, they cannot be used as markers to separate high-grade gliomas from low-grade gliomas.
It is very common that gene mutation and/or amplification of genomic DNA can cause the high expression of certain oncogenes in several different cancer cells including GBM. However, 14 TCGA data sets including two GBM databases from The Memorial Sloan-Kettering Cancer Center cBioPortal for Cancer Genomics web site show that only very small percentage of cases have ATP5A1 mutation (0.2–2.4 %), APT5A1 amplification (0.2–1.9 %), ATP5B mutation (0.2–1.7 %) or APT5B amplification (0.2–3.5 %) (Fig. 4a, b) [12, 13]. In the data sets, 1 out of 281 GBM cases (0.4 %) has ATP5A1 A282S mutation with decreased ATP5A1 mRNA expression. One out of 281 GBM cases (0.4 %) has ATP5B S386L mutation with average ATP5B mRNA expression demonstrated in the data sets. Five out of 372 GBM cases with ATP5B gene amplification do show a moderate to marked increase in ATP5B mRNA expression demonstrated in the data sets. Based on the results from these large data sets for GBM and other cancers, genomic DNA alterations (mutation, amplification or deletion) are less likely the reason for the high expression of ATP5A1 and ATP5B in almost all cases of GBM as shown in the present study.
It is well known that miRNAs can function as potential oncogenes or tumor suppressor genes during the initiation and progression of cancer [19]. It is recently found that miR-7-5p is down-regulated in GBM microvasculature and inhibits vascular endothelial cell proliferation by targeting RAF1 [20]. Human Cancer Pathway Finder 384HC MicroRNA Array analysis for evaluating these miRNAs targeting ATP5A1 or ATP5B is performed. The expression level of miR-16-5p, miR-23a-3p, miR-23b-3p, miR-26a-5p and miR-100-5p that target ATP5A1 mRNA are significantly decreased in GBM microvascular proliferation and GBM tumor cells compared to normal brain blood vessels (p < 0.01) (Table 1). The expression levels of let-7f-5p, miR-24-3p, hsa-miR-101-3p, hsa-miR-125b-5p, miR-193b-3p and miR-331-3p that target ATP5B mRNA are significantly reduced in GBM microvascular proliferation compared to normal brain blood vessels (p < 0.01); let-7f-5p, miR-24-3p, miR-125b-5p, miR-320a, miR-423-5p and miR-744-5p that target ATP5B mRNA are also significantly down-regulated in GBM tumor cells compared to normal blood vessels in brain (p < 0.01 or p < 0.05) (Table 1). The findings indicate that the down-regulation of these miRNAs that target ATP5A1 or ATP5B is the most likely reason for the high expression of ATP5A1 and ATP5B in almost all cases of GBM tumor cells and microvascular proliferation as shown in the present study. Some of these miRNAs are found to be involved in the proliferation, invasion, or other aspects of glioma. By targeting periostin, let-7f inhibits glioma cell proliferation and migration [21]. MiR-16 significantly inhibits the growth of U87MG glioma in vivo probably by slowing down the cell proliferation and suppressing angiogenesis [22]. MiR-16 inhibits glioma cell growth and invasion by suppressing epithelial-mesenchymal transition-related gene (vimentin, beta-catenin and E-cadherin), BCL2, and the nuclear factor-kappaB1/MMP9 signaling pathway in human glioma [23, 24]. MiR-23b significantly inhibits the proliferation and invasion of glioma cells by targeting Pyk2, HIF-1α, β-catenin, MMP2, MMP9, VEGF and ZEB1 [25, 26]. The up-regulation of miR-100 reduces GBM tumorigenicity by inhibiting silencing mediator of retinoid or thyroid hormone receptor-2 gene [27]. The high expression of miR-100 in M059K cells and other cancer cells decreases ATM expression and sensitizes cancer cells to ionizing radiation [28]. The mRNA translation-related gene cytoplasmic polyadenylation element-binding protein 1, overexpressed in glioma cells and tissues, is directly targeted and inhibited by miR-101 [29]. MiR-320 inhibits glioma cell proliferation and metastasis via targeting E2F1 [30]. It is confirmed by previous publications that let-7f -5p, miR-101, miR-320a, miR-423-5p and miR-744-5p can directly bind to ATP5B 3′UTR; miR-16-5p, miR-23a-3p, miR-23b-3p, miR-26a-5p and miR-100-5 can directly bind to ATP5A1 3′UTR [31, 32]. It is very clear that let-7f, miR-16, miR-23, miR-100, miR-101 and miR-320a act as tumor suppressors in glioma by negatively regulating different genes in the published literature while they can target either ATP5A1 or ATP5B.
Citreoviridin, an ATP synthase inhibitor, can suppress the proliferation and growth of breast and lung cancers. [33, 34] Mitochondria-targeting rosamines can inhibit Complex II and ATP synthase activities of the mitochondrial oxidative phosphorylation pathway in 4T1 murine breast cancer [35]. Because both tumor cells and microvascular proliferation in GBM have substantial expression of ATP5A1 and ATP5B, agents against ATP5A1 and/or ATP5B at RNA and protein levels might effectively destroy both tumor cells and microvascular proliferation in GBM. MiRNAs targeting ATP5A1 or ATP5B, especially Let-7f, miR-16, miR-23, miR-100 and miR-101, might be potential therapeutic agents for GBM.
References
Kleihues P, Burger P, Aldape K et al (2007) Glioblastoma. In: Louis DN, Ohgaki H, Wiestler OD, Cavenee WK (eds) WHO classification of tumours of the cenral nervous system. IARC Press, Lyon, pp 33–49
Norden AD, Young GS, Setayesh K et al (2008) Bevacizumab for recurrent malignant gliomas: efficacy, toxicity, and patterns of recurrence. Neurology 70:779–787
Wesseling P, Claes A, Maass C (2007) Combined temozolomide (TMZ) and anti-angiogenic therapy of gliomas: a capricious cocktail? In: Twelfth annual meeting of the society for neuro-oncology
Benard G, Rossignol R (2008) Ultrastructure of the mitochondrion and its bearing on function and bioenergetics. Antioxid Redox Signal 10:1313–1342
DiMauro S, Schon EA, Carelli V, Hirano M (2013) The clinical maze of mitochondrial neurology. Nat Rev Neurol 9:429–444
Furnari FB, Fenton T, Bachoo RM et al (2007) Malignant astrocytic glioma: genetics, biology, and paths to treatment. Genes Dev 21:2683–2710
Ziegler DS, Kung AL, Kieran MW (2008) Anti-apoptosis mechanisms in malignant gliomas. J Clin Oncol 26:493–500
Ordys BB, Launay S, Deighton RF, McCulloch J, Whittle IR (2010) The role of mitochondria in glioma pathophysiology. Mol Neurobiol 42:64–75
Griguer CE, Oliva CR (2011) Bioenergetics pathways and therapeutic resistance in gliomas: emerging role of mitochondria. Curr Pharm Des 17:2421–2427
Deighton RF, Le BT, Martin SF et al (2014) Interactions among mitochondrial proteins altered in glioblastoma. J Neurooncol 118:247–256
Kononen J, Bubendorf L, Kallioniemi A et al (1998) Tissue microarrays for high-throughput molecular profiling of tumor specimens. Nat Med 4:844–847
Cerami E, Gao J, Dogrusoz U et al (2012) The cBio cancer genomics portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov 2:401–404
Gao J, Aksoy BA, Dogrusoz U et al (2013) Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci Signal 6:l1
Hsu SD, Tseng YT, Shrestha S et al (2014) miRTarBase update 2014: an information resource for experimentally validated miRNA-target interactions. Nucleic Acids Res 42:D78–D85
Seyfried TN, Shelton LM (2010) Cancer as a metabolic disease. Nutr Metab (Lond) 7:7
Nagy A, Eder K, Selak MA, Kalman B (2015) Mitochondrial energy metabolism and apoptosis regulation in glioblastoma. Brain Res 1595:127–142
Geyik E, Igci YZ, Pala E et al (2014) Investigation of the association between ATP2B4 and ATP5B genes with colorectal cancer. Gene 540:178–182
Eto I (2011) Upstream molecular signaling pathways of p27(Kip1) expression in human breast cancer cells in vitro: differential effects of 4-hydroxytamoxifen and deficiency of either D-(+)-glucose or L-leucine. Cancer Cell Int 11:31
Ahmed FE (2007) Role of miRNA in carcinogenesis and biomarker selection: a methodological view. Expert Rev Mol Diagn 7:569–603
Liu Z, Liu Y, Li L et al (2014) MiR-7-5p is frequently downregulated in glioblastoma microvasculature and inhibits vascular endothelial cell proliferation by targeting RAF1. Tumour Biol 35:10177–10184
Yan S, Han X, Xue H et al (2015) Let-7f inhibits glioma cell proliferation, migration, and invasion by targeting periostin. J Cell Biochem 116:1680–1692
Zhang N, Zhou H, Yu L, Lin J, Sheng H, Wang M (2014) The influence of miR-16 on proliferation and angiogenesis of U87MG in vivo. Zhonghua Yi Xue Za Zhi 94:2618–2621
Wang Q, Li X, Zhu Y, Yang P (2014) MicroRNA-16 suppresses epithelial-mesenchymal transition related gene expression in human glioma. Mol Med Rep 10:3310–3314
Yang TQ, Lu XJ, Wu TF et al (2014) MicroRNA-16 inhibits glioma cell growth and invasion through suppression of BCL2 and the nuclear factor-kappaB1/MMP9 signaling pathway. Cancer Sci 105:265–271
Loftus JC, Ross JT, Paquette KM et al (2012) miRNA expression profiling in migrating glioblastoma cells: regulation of cell migration and invasion by miR-23b via targeting of Pyk2. PLoS One 7:e39818
Chen L, Zhang K, Shi Z et al (2014) A lentivirus-mediated miR-23b sponge diminishes the malignant phenotype of glioma cells in vitro and in vivo. Oncol Rep 31:1573–1580
Alrfaei BM, Vemuganti R, Kuo JS (2013) microRNA-100 targets SMRT/NCOR2, reduces proliferation, and improves survival in glioblastoma animal models. PLoS One 8:e80865
Ng WL, Yan D, Zhang X, Mo YY, Wang Y (2010) Over-expression of miR-100 is responsible for the low-expression of ATM in the human glioma cell line: M059J. DNA Repair (Amst) 9:1170–1175
Xiaoping L, Zhibin Y, Wenjuan L et al (2013) CPEB1, a histone-modified hypomethylated gene, is regulated by miR-101 and involved in cell senescence in glioma. Cell Death Dis 4:e675
Sun JY, Xiao WZ, Wang F et al (2015) MicroRNA-320 inhibits cell proliferation in glioma by targeting E2F1. Mol Med Rep 12:2355–2359
Zheng SQ, Li YX, Zhang Y, Li X, Tang H (2011) MiR-101 regulates HSV-1 replication by targeting ATP5B. Antiviral Res 89:219–226
Helwak A, Kudla G, Dudnakova T, Tollervey D (2013) Mapping the human miRNA interactome by CLASH reveals frequent noncanonical binding. Cell 153:654–665
Chang HY, Huang TC, Chen NN, Huang HC, Juan HF (2014) Combination therapy targeting ectopic ATP synthase and 26S proteasome induces ER stress in breast cancer cells. Cell Death Dis 5:e1540
Wu YH, Hu CW, Chien CW, Chen YJ, Huang HC, Juan HF (2013) Quantitative proteomic analysis of human lung tumor xenografts treated with the ectopic ATP synthase inhibitor citreoviridin. PLoS One 8:e70642
Lim SH, Wu L, Kiew LV, Chung LY, Burgess K, Lee HB (2014) Rosamines targeting the cancer oxidative phosphorylation pathway. PLoS One 9:e82934
Acknowledgments
We give special thanks to Dr. Betty Diamond, who provided the lab space and equipments. We also appreciate help and support from all her lab members. We are thankful for Mr. Daniel Loen and Ms. Jill Wishinsky for managing the Grant. Dept. of Pathology and Lab. Medicine: We thank Dr. James Crawford for his support and encouragement, Ms. Claudine Alexis for ordering all our materials, and people in histology laboratory for technical support.
Funding
This work was supported by North Shore-LIJ Cancer Institute.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest.
Rights and permissions
About this article
Cite this article
Xu, G., Li, J.Y. ATP5A1 and ATP5B are highly expressed in glioblastoma tumor cells and endothelial cells of microvascular proliferation. J Neurooncol 126, 405–413 (2016). https://doi.org/10.1007/s11060-015-1984-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-015-1984-x