Abstract
Formulation of nanocrystals is a distinctive approach which can effectively improve the delivery of poorly water-soluble drugs, thus enticing the development of the nanocrystals technology. The characteristics of nanocrystals resulted in an exceptional drug delivery conductance, including saturation solubility, dissolution velocity, adhesiveness, and affinity. Nanocrystals were treated as versatile pharmaceuticals that could be delivered through almost all routes of administration. In the current review, oral, pulmonary, and intravenous routes of administration were presented. Also, the targeting of drug nanocrystals, as well as issues of efficacy and safety, were also discussed. Several methods were applied for nanocrystals production including top-down production strategy (media milling, high-pressure homogenization), bottom-up production strategy (antisolvent precipitation, supercritical fluid process, and precipitation by removal of solvent), and the combination approaches. Moreover, this review also described the evaluation and characterization of the drug nanocrystals and summarized the current commercial pharmaceutical products utilizing nanocrystals technology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With the development of high-throughput screening and combinatorial chemistry in drug development programs, the prospect of synthetic new drugs (SND) and promotion of the quality can be anticipated (Chin et al. 2014). However, the molecules in the drug development process are eliminated about 40 %/year, statistically, because of their poor water solubility and bioavailability (Tran and Nguyen 2011). Currently, a number of methods are being used to promote the delivery of such compounds, including cyclodextrin complexations, solid dispersions, nanosizing and lipid-based drug delivery systems (e.g., liposome and microemulsion).
However, these strategies are limited to the usage of drugs with certain properties regarding their molecular size, conformation (e.g., molecules need to be incorporated into the ring structure of cyclodextrin), or chemistry (e.g., solubility difference in certain organic media) (Lemke et al. 2010). Furthermore, the usage of cosolvents or surfactants is also possible, but often leads to increased side effects, for example, HP-β-cyclodextrin brings about the nephrotoxicity of itraconazole in Sporanox® and Cremophor enhances the toxicity of Taxol (Shi et al. 2014), as well as other disadvantages like organic solvent residues.
To overcome these obstacles, formulation of the drugs as nanocrystals was proposed. Drug nanocrystals are submicron colloidal dispersion systems of pure drug nanoparticles stabilized by surfactants, polymers or a mixture of both (Zhang et al. 2011). By this means, the nanocrystals particles possess a 100 % drug loading in contrast to the traditional nanoparticles which consist of either a lipid polymeric matrix such as liposomes, nanoemulsions and lipid nanoparticles or polymeric nanoparticles (Muller et al. 2011).
The high drug loading capacity makes the nanocrystals quite efficient in transporting the drug to/into the cells, achieving a sufficiently high therapeutic concentration for a pharmacological effect. Presuming that the pure drug particles, less than 1000 nm size, were suspended in an aqueous medium, they were referred to as drug nanosuspensions, and if the drug particles are partially or integrally crystalline, they were referred to as drug nanocrystals (Donoso et al. 2012). The degree of crystallinity could vary widely, which mainly depends on the adsorption process.
The particles of drug nanocrystals were maintained with the characteristics of decreased particle diameter and increased surface area, leading to an enhanced dissolution rate. A common consensus that the enhancement of bioavailability of drugs may reduce subject-to-subject variability was largely attributed to increasing the dissolution rate. As a result, nanonization has been treated as the ultimate universal formulation strategy for drugs with low solubility and high permeability (Biopharmaceutics Classification System II) (Cheng et al. 2004). With the development of nanotechnology, nanocrystals have progressed to a wide application, which can not only regulate the poor water solubility issues during in vivo drug delivery but also offer solutions for potential drug compounds eliminated by conventional methods.
Drug nanocrystals could be prepared not only by breaking down larger micron-sized particles with milling but also building up desirable particles from the molecular state-like precipitation. In either scenario, free energy is necessitated to form a new surface area (Gramdorf et al. 2008). It is attributed to the theory that when located on a free surface, the attraction forces in water molecules are decreased compared to the previous state. This system prefers to reduce the amplification on the surface area through either agglomerating small particles, regardless of their formation mechanism, or dissolving incipient crystalline nuclei, in the case of precipitation. This phenomenon could be resisted by adding the surface active agents to the system. The addition of these surfactants, concurrent to the formation of a new surface, brings about immediate and efficient protection than if added at a later stage. Based on their complementary properties, surfactants are divided into two categories: nonionic polymers, which provide a steric repulsion effect, i.e., compression, and charged/active ionic agents, which offer an electrostatic repulsion effect among the particles (Morgenthal et al. 2014). A confederative application of polymers and ionic surfactants complementing each other assures both steric and electrostatic repulsion mechanisms. In addition to the property of the bulk particles, the stability of colloids is primarily determined by the adjunction of surfactants, which leads to the potential repulsive effect. However, it does not imply a modest effect of drugs on the stability of suspensions, which usually affects the nature of the surface together with the surfactant.
Special properties of nanocrystals
Saturation solubility
Commonly, when the temperature and the compounds of the dissolution medium are maintained in the initial state, the saturation solubility (C s) of the drugs is constant (Mauludin et al. 2009a), which is suitable for the particles of the micrometer range or above. A similar principle C s is also closely related to the particle size below 1–2 μm (Zhu 2013). Based on the theory that C s increases with decreasing particle size below 1000 nm, drug nanocrystals possess the property of increased saturation solubility. Two equations can clarify the underlying mechanism.
wherein C s = the saturation solubility; σ = the interfacial tension of substance; V = the molar volume of the particles; C α = the solubility of the solid substance consisting of large particles; R = the gas constant; T = the absolute temperature; ρ = the density of the solid substance; and r = the radius of particles.
Ostwald–Freundlich Eq. (1) evidently shows that the saturation solubility of drugs is inversely proportional to the radius of the particles. Although this mechanism does not correspond with larger particles, it is applicable for materials with a mean particle size of less than 1–2 μm, for example, the typical particle size of nanocrystals is about 600 nm (Thorat and Dalvi 2012).
wherein P r = the dissolution pressure of one particle with the radius (r); γ = the surface tension between particles; M r = the molecular weight of particle; P ∞ = the dissolution pressure of a theoretically infinitely large particle; r = the radius of the particle; R = the gas constant; T = the absolute temperature; and ρ = the density of the particle.
Based on Kelvin Eq. (2), the vapor pressure of lipid droplets converting into a gas phase will increase accompanied by the spread of curvature of the surface, which means that the particle size is reduced. Since the vapor pressure of each liquid is an augmentation of various components, the increase or decrease in vapor pressure will be regulated by the available compound-specific substance. The situation of molecules from a liquid droplet converting into a gas phase, such as an aerosol, can be used as a reference for the transfer of nanocrystals molecules from a solid to a liquid dispersion medium. Thus, the Kelvin equation is also applicable to explain the relation between the dissolution pressure and the curvature of the solid particles in a liquid, wherein the dissolution pressure is equivalent to the vapor pressure. At saturation solubility state, the recrystallizing molecules and dissolving molecules are in equilibrium. The dissolution pressure can be increased along with the expanded curvature (decreasing particle size) (Kratz and Warnecke 2012). Moreover, the curvature is especially immense when the particle size is in the nanometer range. Therefore, the equilibrium is shifted toward dissolution, thereby increasing the saturation solubility.
Dissolution velocity
Prior to absorption of drugs, the active pharmaceutical ingredient (API) should be released from the pharmaceutical dosage, for example, the active ingredients of oral formulations must be solubilized in the gastrointestinal fluid. The dissolution velocity played a major role in the dissolution kinetics of the suspension of poorly soluble drugs. Ordinarily, both the diffusion layer thickness and the molecular diffusion distance were reduced along with the diminished particle size (Liu et al. 2011). The mechanism can be explained by two related equations:
wherein dm/dt = the dissolution velocity; D = the diffusion coefficient of the solution; S = the surface area of drugs; V = the volume of dissolution medium; h = the thickness of the diffusion layer adjacent to the surface of dissolution; C s = the saturated solubility of drugs; and C t = the concentration of the drug solution.
The particles size reduction leads to an increased surface area (S), and according to Noyes–Whitney Eq. (3), an increased dissolution velocity (dm/dt) will appear. Taking into account that the dissolution velocity is the rate-limiting step, micronized processing could be a suitable way to effectively improve the bioavailability of poorly soluble drugs. Furthermore, when the micronization drugs are converted to nanonization, the dissolution velocity will substantially increase with the further expansion of the particle surface.
The diffusion distance is a critical factor in dissolution velocity. As a part of the hydrodynamic boundary layer, the diffusional distance is also strongly dependent on the particle size, and the mechanism can be shown by Prandtl Eq. (4):
wherein h H = the hydrodynamic boundary layer thickness; k = constant; L = the length of the particle surface in the direction of flow; and V = the relative velocity of the flowing liquid surrounding the particle.
Based on Eqs. (3) and (4), the particle size reduction leads to a decreased diffusion distance and consequently an increased dissolution velocity, thus designating it as a favorable method to increase the dissolution velocity of a water-insoluble drug by transforming the drug powder into nanocrystals.
Adhesiveness
The dominant barrier to cellular absorption and transmission mainly exists in the epithelial cells of mammalian tissues and organs, such as the brain, cornea, lungs, and gastrointestinal tract (Rasenack et al. 2003). The intestinal epithelial cells play a major role in the drug delivery process, altering the efficacy of oral formulations. These cells form tight junctions similar to other epidermal cells, thereby limiting the paracellular flux of active pharmaceutical ingredients. In order to successfully permeate the epithelial cells via transcellular diffusion and be effectively absorbed in the gastrointestinal tract (GIT), it is necessary to possess optimum physicochemical properties for dosage forms.
Surface properties play an important role throughout development of nanocrystals, for example during preparation, in the coating of beads for wet milling to maximize attrition and minimize erosion. Stabilization occurs when the interaction(s) between nanocrystals and excipient(s) are optimized which is a function of surface chemistry and has been shown to be anisotropic for crystalline pharmaceutical powders (Wang et al. 2012). It has been shown that increased adhesion may lead to improved oral absorption. Surface functionalization can alter and further enhance properties of nanocrystals depending on the needs for release profile and targeted drug delivery (Fig. 1).
Surface functionalization of nanocrystals (Wang et al. 2012)
The mononuclear phagocyte system (MPS) as ‘‘radar system’’ of the body normally detects the nanocrystals as foreign particles to the body (Muller et al. 2011). It is very fast and efficient for the MPS cells to removal foreign particles from the blood stream by phagocytosis. This process triggers and initiates phagocytosis or internalization of the nanocrystals. The pH-dependent solubility profiles of the phagocytized nanocrystal drug particles may allow these drugs to be dissolved after the pH was subjected to the progressively decreasing in phagolysosomes. Depending on their lipophilicity and pH-solubility curves, suitable drugs can pass through the phagolysosomal membrane. Consequently, the drugs provide sustained drug release where they first enter the cytoplasm and are then excluded by diffusing down drugs concentration gradients.
The study on the intracellular delivery showed that the drugs increase in adhesiveness to the surface as the particle size decreases (Lee et al. 2005). For example, compared to coarse powders, there is a distinct enhancement in the adhesiveness of ultrafine particles. The high adhesiveness of small drug nanoparticles could be exploited for improving different delivery approaches of poorly water-soluble drugs, such as oral, local, and dermal. The adhesive property could be further enhanced by modifying the surface of drug nanocrystals with polymers, such as chitosan, carbopol, and polyethylene glycol. (Keck and Muller 2006). After surface modification, drug nanocrystals could not only achieve increased mucoadhesiveness of nanoparticles for oral application but also improve site-specific targeting with selective surfactant/polymer after intravenous (IV) injection, such as targeting to the bone marrow and brain. Moreover, this kind of innovative technology can be arranged in groups with traditional dosage forms-like tablets or capsules (Sosnik et al. 2014).
Affinity
Compared to the conventional drug formulations, nanocrystals are advantageous due to less usage of cosolvents, excipients, and solubilizing agents, which often cause a series of side effects comprising of hypersensitivity reactions, incompatibility with main ingredients, and limiting the dissolution rate of the active ingredient in formulations (Keck 2010). Targeted delivery to tissue or organ lesions rather than to healthy sites can further reduce the side effects of drug delivery.
In the case of cancer therapy, the size of drug nanocrystals could be adjustable under 400 nm in principle. Subsequently, by IV injection, it can diffuse out from the blood through the leaky endothelium to accumulate in the tumor tissue by enhanced retention and permeation effect to achieve the effect of targeted therapy. In addition to this kind of passive targeting effect, drug nanocrystals could be functionalized with internalizing or targeting ligands to promote active substance uptake or accumulation in the tumor, respectively. During this process, the stabilizers are used to offset the effect of the high-energy drugs surface along with the particles size reduction process. These stabilizers mainly include polymers (e.g., poloxamers, cellulose derivatives) and surfactants (e.g., sodium dodecyl sulfate), providing a steric effect or electrostatic barriers to prevent aggregation where they stabilize the nanocrystals by being adsorbed to the surface of the particles (Verma et al. 2011).
Stability
The absence of Ostwald ripening is an exclusive characteristic of drug nanocrystals, which is attributed to its uniform particle size prepared by the milling/homogenization process, ensuring a long-term physical stability of aqueous drugs. Nowadays, several techniques can be utilized to prepare products with an ultrafine particle size, including sophisticated supercritical fluids with enhanced mass transfer (Song et al. 2012) and laser fragmentation (Rabinow et al. 2007), wherein the high-pressure homogenization and wet milling are the most common practices in the industry. The requirements of achieving multiple performances have revealed the advantages associated with the development of nanocrystals technology (Table 1).
A concern with amorphous nanocrystal drugs is the possibility undergoing crystallization on storage. They can be mitigated by proper polymer selection, drug loading optimization, and appropriate product packaging selection. Amorphous nanocrystal drugs can be rendered physically stable via kinetic stabilization, i.e., freezing the amorphous drug substance in the polymer matrix to restrict molecular mobility to prevent nucleation and crystal growth.
The polymer may stabilize an amorphous nanocrystal drugs via drug–polymer intermolecular interactions such as hydrogen bonding, Van der Waals forces. Drug loading can impact both kinetic and thermodynamic stability of amorphous nanocrystal drugs. For a thermodynamically stabilized amorphous nanocrystal drugs, increasing drug loading can saturate bonding sites and thus result in a less stable amorphous dispersion. As drug loading impacts both of these stabilizing mechanisms, it is critical to conduct accelerated stability studies on a range of drug loadings to arrive at a physically stable amorphous dispersion with an acceptable drug load. What’s more, packaging is critical when the amorphous nanocrystal drug is susceptible to destabilization by moisture absorption. Utilizing the appropriate dosage form, the packaging configuration can eliminate moisture contact and stabilize the amorphous product for an acceptable shelf life.
Formulation of nanocrystals
The small particle size of drug nanocrystals is either the inherent factor to their success or responsible for their physical instability. Drug nanocrystals system (nanosuspensions) consists of nanoparticles (originally hydrophobic) dispersed in a hydrophilic medium (e.g., water, ethanol), essentially rendering them as thermodynamically unstable systems (Kesisoglou et al. 2007). The small size and enormous surface area of these nanoparticles result in a high interfacial tension, correspondingly leading to an increase in the free energy of the system. In order to decrease their free energy, the nanoparticles have a tendency to reduce the interaction with the hydrophilic medium by crystal growth, flocculation, or aggregation. However, this process has an inevitable effect on the kernel characteristics of nanocrystals (small particle size and large surface area).
Correspondingly, these complications can be solved by the addition of various stabilizers. The purpose is to design a physically stable formulation, where the mechanism of action is to infiltrate the drug particles further to prevent agglomeration by providing an ionic or a steric barrier (Chan and Kwok 2011). For example, in the presence of polyvinylpyrrolidone (PVP) and hydroxypropyl methylcellulose (HPMC) polymers, a stable carbamazepine nanocrystal is prepared by the cosolvent technique comprising of polyethylene glycol (PEG) and water as the cosolvents. It was concluded that the additional stability could be attributed to the interaction between the two polymers, which prevents self-association of the HPMC molecules by the formation of hydrogen bonds (Bao and Krishnan 2005). The combination of PVP and HPMC along with the drug nanocrystals had the highest total concentration of polymers, also contributing toward the additional stability in the formulations.
Stabilizers could be polymers, surfactants or a mixture of both. Examples of polymeric stabilizers comprise of PVP, hydroxypropyl cellulose (HPC), HPMC, and polyvinyl alcohol (PVA) (Ghosh et al. 2011). The common examples of surfactants include poloxamer 188, sodium lauryl sulfate, and Tween 80 (Gao et al. 2013). For instance, in order to produce stable nanocrystals by nanomilling, it is necessary to build the steric and electrostatic stabilization by different stabilizers along with excellent wetting of the drug particles (George and Ghosh 2013).
Compared with common stabilizers, the multi-effect stabilizer that had electrostatic repulsion, steric hindrance, and hydrophilic effect could exhibit excellent performance to maintain the physical stability of nanocrystals. So far, the amphiphilic block copolymer (BCP) has been used, either premade or in situ formed by rapid coupling reactions during the mixing (Zhu 2013).
The cationic polymers are ideal stabilizer candidates to prevent particle aggregation by both electrostatic and steric stabilization effects. As a natural linear polysaccharide, chitosan is polycationic, biocompatible, biodegradable, and non-toxic. It contains primary amine groups in its repeating units. This special structure can produce both electrostatic repulsion and steric repulsion. However, the presence of amino groups in chitosan leads to a poor solubility in water or organic solvents apart from acidic aqueous solutions, limiting its effective utilization. To improve its solubility, the graft copolymerization of chitosan onto other polymers with high water solubility can be performed by chemical modifications. In particular, PEG is widely used as the grafted polymer material. It can cause cross-linking and form the hydrophilic outer shell on the surface of other graft copolymers. Besides, it is biocompatible and biodegradable without antigenicity, immunogenicity, and toxicity.
Preparation and production approach
With the continuous development of technology, several strategies are available to prepare nanosized drug particles (drug nanocrystals/nanosuspensions), which are broadly classified into three categories, i.e., top-down technologies, bottom-up technologies, and combination approaches (Fig. 2). The application of these strategies is based on a comprehensive evaluation, such as the physicochemical properties of molecules (firmness of the compound and solubility in organic solvent), the specifications of particle size, and economics. What’s more, there are different synthesis routes for different nanoformulations. They are broadly classified into five categories, i.e., dendrimers, polymeric nanoparticles, liposomes, nanoemulsions, polymer micelle. It is much dependent on the type of application and its functionality (Jeevanandam et al. 2016).
Production strategies to prepare nanocrystals (Pawar et al. 2014)
Top-down technology
The top-down production methods are high energy-consuming processes where the drug materials are reduced from micron-sized large particles to the nanodimension, for example, media milling and high-pressure homogenization (Latha et al. 2009).
Media milling
Media milling method is the classical technology for drug nanocrystals, which uses a pearl mill or a bead to reduce the particle size. A large percentage of products on the market are produced with this technology. It is feasible to scale-up the nanocrystals production with a pearl mill but is sized limited due to its high density. Firstly, the suspension is added to a milling container containing milling pearls, typically between 0.2 and 0.6 mm (Sinha et al. 2013a). Then, the materials are collided and ground between the moving pearls and container walls, wherein the pearls and suspensions are agitated for a certain time and frequency, and the resulting product is a nanosuspension. Based on the actual application, a series of smaller or larger coated milling pearls could be selected, which contain glass, stainless steel, ceramics (e.g., zirconium dioxide stabilized by yttrium or cerium), and highly cross-linked polystyrene resin-coated beads.
The wet-milling method could be used to produce drug nanosuspensions, which processes the crystalline aqueous suspension using different grinding mediums. However, there is a disadvantage in this process that the formulations will be confronted with the contamination of the attrition residue. Considering that the milling time can last several days, another common problem of this technology is the erosion of milling media during the process (Zhang et al. 2013). Also, the heat generated from the violent collision and friction processes would lead to thermal degradation of heat-sensitive drug ingredients. A viable solution is to install a temperature controlled cooling system outside of the milling container. Therefore, it is a prerequisite to carry out two formulation criteria for an efficient milling process, i.e., a relatively small contact angle (a measure of the degree of wetting under 70°) and a high dispersibility of the drug particles in the milling medium (Juhnke et al. 2012).
High-pressure homogenization
The high-pressure homogenization is a fluid mechanical technique processing suspensions homogeneous or uniform in composition, which could be used to homogenize large particles into nanometer size under high pressure. This technology breaks down the APIs into specified particle size accompanied by abundant energy consumption. The three most important processes in the technology include the microfluidization method, e.g., IDD-P™ technology (Van Eerdenbrugh et al. 2009), the supersonic fluid flow method, and the piston-gap homogenization method, either in water, e.g., Dissocubes® technology (Ali et al. 2011) or in water-reduced/non-aqueous media, e.g., Nanopure® technology (Mou et al. 2011).
The microfluidization technology can be utilized to produce small particles by a collision between the two fluid streams under pressure up to 1700 bar. This process brings about a mixed effect containing collision forces, friction forces, cavitations forces, and shear forces (Wang et al. 2012) and could be carried out in a jet stream homogenizer like the microfluidizer. Under normal conditions, it requires a relatively high number of cycles; about 50–100 passes to reduce the particle size to an adequate range (Ma et al. 2013). Muller and coworkers (Muller et al. 2006) applied the piston-gap homogenizers for an alternative high-energy method, wherein the suspension passes a small gap with a significantly reduced cross-sectional area (e.g., 10 μm in height) with a high speed (e.g., 500 m/s). According to the Bernoulli theorem, the liquid flow is constant through each cross section in a closed system (Hanafy et al. 2007). When drug suspensions are transmitted through the gap, its dynamic pressure rises sharply, and the static pressure is drastically reduced, which causes the liquid to boil and form a large number of bubbles. After leaving the gap, the bubbles are affected by the atmospheric pressure and violently implode, and the drug particles are pulverized to nanometer size by a combined effect of collision of particles with the steel wall and each other as well as cavitations and shear forces from the liquid (Van Eerdenbrugh et al. 2008b). The usual production conditions are 1500 bar and 20 passes after the pretreatment process with 500 bar and up to five passes through the high-pressure homogenizer. All the drug materials in the homogenization processes of Dissocubes® technology are aqueous suspensions. Nanopure® technology is another homogenization method using the piston-gap homogenizer. The suspensions obtained by this approach could be directly filled into hard gelatin or HPMC capsules and soft gelatin capsules before the encapsulation process (Zhang et al. 2014). It requires restricted production conditions, for example, optional homogenization at a low temperature and the dispersion media (e.g., oils or hot-melted PEGs) with a low vapor pressure. The cavitation is very little or nonexistent in the homogenization gap with water-reduced/non-aqueous media. Even then, it is sufficient to reduce the large particles to nanoparticles by the remaining turbulences, shear forces, and particle collisions (Van Eerdenbrugh et al. 2008a). In order to protect the temperature labile drug and restrain hydrolysis phenomenon, it is the most optimized protocol to carry out the whole homogenizing process in a non-aqueous media at a low temperature.
Although the top-down technology is more feasible regarding industrialization than the other preparation procedures, a series of limitations cannot be ignored, such as the low efficiency of particle size reduction and high costs. For example, the top-down process commonly requires an extended period to reduce the particle size under 100 nm with the continuous energy consumption. Moreover, it is not practical to reduce the particle sizes beyond a certain limit using the standard top-down technology, which is about 150–300 nm in most cases (Ravi and Baskaran 2015). Moreover, during the milling process, some issues may occur, which are related to the solid-state changes and chemical degradation of the drug nanoparticles (Ain-Ai and Gupta 2008).
Bottom-up technologies
The bottom-up technology is a standard precipitation process, which is carried out in a liquid-phase environment. In this process, the pharmaceutical compounds are firstly dissolved in a liquid medium retaining the molecular state, then swelled into the particle by coagulation or condensation based on the nucleation of a supersaturated solution, which maintains the crystalline or amorphous states (Aditya et al. 2015). The system involves two liquid phases, i.e., the drug dissolved in a solvent and the stabilizers dissolved in an antisolvent where the two phases are miscible. When the solvent is added to the antisolvent, the drug appears in a supersaturated state in the mix, followed by precipitation. It is crucial to avoid the crystals growing up to the micron size and regulate the structure (amorphous vs. crystalline) of the particles in this process. The bottom-up technology could be suitable for most of the water-insoluble compounds, particularly the thermolabile drugs due to the advantages of low energy, low temperature, simple instrumentation, and relatively low cost (Aqil et al. 2013).
In recent decades, there are some patent and scientific publications per year on the preparation of nanoparticles, such as nanoemulsions, nanocrystals, and nanoliposomes based on precipitation technology. The precipitation processes are classified into three categories, i.e., mixing liquid solvent and antisolvent, removal of the solvent, and precipitation with supercritical fluid as the medium.
Hitherto, nanoprecipitation by liquid solvent–antisolvent is the most appealing among the various precipitation techniques, due to the ease of operation and cost-effectivity. There is a broad range of applications for this technology to prepare nanoparticles, not only for synthetic organic compounds but also for molecules from natural sources, such as deacetyl-mycoepoxydiene and tetrahydropalmatine. In order to obtain the smallest particle size, an optimum drug concentration is required. The particle size would increase when a drug concentration above this optimal level was used. With the drug concentration increasing, the nucleation rate is also increased due to a higher supersaturation. A higher nucleation rate would reduce the final particle size. What’s more, a decrease in the antisolvent temperature generally narrows the particle size distribution and reduces the particle size. A change in temperature could affect various parameters of the precipitation process. A reduction in temperature increases the degree of supersaturation and reduces the equilibrium solubility. As a result, higher supersaturation increases the nucleation rate and the reduction in solubility reduces the Ostwald ripening phenomenon (Sinha et al. 2013a, b).
It is essential to choose the appropriate medium of precipitation by solvent removal because they are difficult to be completely removed, which can result in instabilities and toxicity (D’Addio et al. 2012). Alternatively, researchers also use supercritical carbon dioxide to leach the internal phase of oil-in-water emulsions, successfully obtaining nanosized particles of nanosuspensions, which can occur as a batch or in a continuous manner (Khadka et al. 2014). This technique can effectively overcome the current limitations of eliminating the use of organic solvents in the conventional precipitation techniques. Furthermore, it can significantly shorten the processing time, increase product purity, and have a high manufacturability for process scale-up. As a result, this optimized method offers a viable alternative for constructive nanoparticles formation process.
Supercritical fluids technology (SCF) possesses special state of matter between the gaseous and liquid state when substances are at a temperature and pressure above its critical point. They can not only effuse through solids like gas but also dissolve in materials like a liquid. Consequently, the SCF is used in particle engineering, particularly suitable for thermolabile drugs (Sher et al. 2007). The common supercritical techniques that are used to prepare nanoparticles of organic compounds by precipitation include rapid expansion of a supercritical solution into a liquid solvent (RESOLV), the rapid expansion of supercritical solution (RESS), and supercritical antisolvent (SAS) (Galli 2006). Additionally, the suitable supercritical solvents contain ethane, ethylene, carbon dioxide (CO2), fluoroform, and ammonia. Comparably, CO2 is the most appropriate solvent because it can be easily converted into the supercritical state due to its low critical pressure (ca. 73.8 bar) and the near ambient critical temperature (ca. 31 °C) (Moschwitzer et al. 2004). Also, it is favorable for commercial use because of easy of availability, non-toxicity/flammability, and cost-effectiveness.
Combination approaches
In general, the combination technologies are a collocation between a pre-treatment step in which the crystals are precipitated into suspensions and a high-energy process step (usually high-pressure homogenization). According to the research of the quantitative relationship between the structure and the pharmacokinetics/activity, drug nanoparticles with a particle size below 100 nm may acquire novel physical properties compared to large particulate matter and significantly improve their permeation through various biological barriers (Niwa et al. 2010). The bottom-up technologies with further modifications can be used to generate smaller nanoparticles in combination with the top-down process. Some of the modified precipitation processes for producing micro-/nano-sized drug particles can be successfully scaled up, meeting the requirements of industrial production (Ranjita 2013).
The NanoEdge™ technology is a typical combination approach, which conducts precipitation process preceding the annealing step of high-pressure homogenization, which prevents the growth of the precipitated nanocrystals (Hu et al. 2014). However, the substantial disadvantage of this technology is that the large amounts of solvents need to be removed in the large-scale production process, which leads to more stringent production conditions and a high input cost. The smartCrystal® technology is also a process of various combinations, specialized in the ability to produce nanoparticles under 100 nm, which is impossible to reach by using high-pressure homogenization or precipitation technology alone (Morakul et al. 2013).
Evaluation and characterization methods
According to the required performance parameters, pharmacy researchers carry out the specific assessments of the quality of drug nanocrystals. For example, test items of a drug suspension used for injection include bacterium, pyrogen, hemolytic activity, permeability, and stability (Rabinow 2004). In order to maintain the pharmaceutical stability, the drug particles must have a minimal tendency to agglomerate or decompose, which could change the particle size and lead to the pharmacodynamic damage. The most ideal criteria are resuspendability and homogeneity as well as non-irritability and non-toxicity.
Application research showed that the bioavailability of drug nanocrystals eventually depends on the dissolution of the drug irrespective of the route of administration. The dissolution rates would continually be affected by the digestive/circulatory system factors, such as pH of the gastrointestinal fluid, gastric emptying time (GET), and gastrointestinal bloodstream velocity, and the nature of drug crystals such as crystal morphology and particle size. The in vivo dynamics of pharmacokinetics could be guided by a dissolution test in a biorelevant medium in vitro. Additionally, the absorption evaluation of drug nanocrystals could take the liposomal dosage forms in clinical trials as a reference where the drug levels in the blood should be separated into the free molecular section in blood plasma and bound fraction of nanocrystals plasma protein (Zhu et al. 2013).
The particle size is one of the most important properties of drug nanocrystals. There are several efficient methods for particle size determination, including light/electron microscopy, laser diffraction (LD), dynamic light scattering (DLS), scanning ion occlusion sensing (SIOS), single-particle tracking analysis, and field-flow fractionation (Moorthi and Kathiresan 2013). Under normal conditions, both LD and DLS could be employed to determine the hydrodynamic diameter of nanoparticles as well as the particle size distribution. The LD determines the particles parameters by measuring the different scattered light angles when the laser beam passes through the dispersed sample particles. Compared to DLS, LD has a much broader detection range from several hundred nanometers to several millimeters, but on the other hand, it has a poor resolution for smaller particles. The DLS is also known as quasi-elastic light scattering or photon correlation spectroscopy. It is a sensitive and rapid method for particle size measurement, especially for those in the lower nanometer range. Due to its excellent performance, DLS is often applied for routine measurements and early formulation development requiring only small quantities of particles. However, the detection limit of DLS is only 6 µm (Li et al. 2014), which restricts the scope of application on bigger particles or aggregates. Moreover, there is a common problem in both LD and DLS that the particle size is gradually altered in the detection process because the nanoparticles are in continuous dissolution. In order to avoid this phenomenon, the saturated solution of the original drug substance is utilized to dilute the sample with higher solubility (Gardikis et al. 2010). It is more feasible to combine several different analytical techniques to obtain the reliable amount of data. For example, to combine LD or DLS with single-particle tracking analysis would be a practical method.
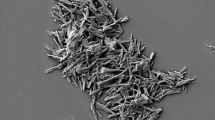
Apart from characterizing the mean particle size and particle size distribution, attention should also be focused on characterizing the other vital parameters of nanocrystals, such as morphological structure detected by atomic force microscopy (AFM), scanning electron microscopy (SEM), and transmission electron microscope (TEM), as well as the zeta potential measured using the zeta potential meter. The AFM (a) and SEM (b) pictures of Nanomorph® drug nanocrystals are shown in Fig. 3. The particle size and morphology of nanocrystals formulations which present different crystalline states are usually different. The Nanomorph® drug nanocrystals in amorphous state are spherical, and the crystalline nanoparticles are cuboid.
AFM image of Nanomorph® drug nanocrystals in amorphous state (a) and SEM image Nanomorph® drug nanocrystals in crystalline state (b) (Shegokar and Muller 2010)
Administration evaluation of nanocrystals
Drug nanocrystals consist of 100 % active drugs in contrast to other traditional nanoparticle systems which are dependent on a number of carriers (Wu et al. 2011). The nanocrystals possess several advantages including high drug loading, easy scale-up for industrial production, and suitability for a variety of administration routes, such as oral, intravenous, pulmonary, ocular, and dermal delivery. Also, they can be used for targeted delivery where its behavior affected by surface properties can easily be altered in vivo (Kawakami 2012). The surface engineering can promote targeting of nanoparticles by adding various surface coatings. As a result, the prospects of drug nanocrystals are higher due to multi-effects, simple preparation process, and ease of industrial production.
Oral administration
For most treatment programs, the oral route is usually the first choice of drug delivery because of several advantages including high safety, convenient administration, and low cost. However, the oral administration of poorly water-soluble drugs exhibits many deficiencies in bioavailability, such as low effect, the retarded onset of action, variable pesticide effect resulting from fed/fast state, and large dosage (Shegokar et al. 2011). The production of drug nanocrystals provides a solution with performance parameters suitable for oral drug delivery. Also, the survey suggests that the formulations of drug nanocrystal in the market are mostly used for oral delivery.
It has been observed in preclinical tests that the uptake of intact gastrointestinal polymeric particles occurs by reducing the particle size to the submicron level (Kim and Lee 2010). The plausible underlying mechanism ensues that the drug nanocrystals are ingested and transported by membranous/microfold cells (M-cells) in Peyer’s patches of the gastrointestinal lymphoid tissue (Custodio et al. 2008). M-cells can be used as a transportation channel between the enteric cavity and the mesenteric lymph ducts, and the drug nanocrystals delivered by them are subsequently emptied into the systemic blood circulation via the thoracic duct. This approach can produce two aspects of beneficial results: it not only avoids the first-pass effect of liver and spleen, but it is used for targeted therapy of lymphatic-mediated diseases (Pawar et al. 2014). For example, it gives an intuitive display of drug delivery that the hypothetic oral absorption process for Nimodipine (NMD) nanocrystals as shown in Fig. 4. However, there is a deficiency in this process that the drug uptake is low via this pathway. The drug particles are coated with agents-like vitamin B12 to improve the absorption, which promotes the combination of the drug with transporter receptors on the intestinal epithelium (Das and Suresh 2011). Several receptors are expressed on the surface of the cells. Some of them are responsible for the internalization of nutrients, such as folate and transferring and some are in rapidly dividing cells, such as the cancer cells where they are upregulated and can thus be differentially targeted. Consequently, numerous investigations have focused on the use of drug moieties conjugated to receptor substrates for internalization by receptor-mediated endocytosis. Moreover, it has been found that the use of surfactants has an impact on both, the interference with lipidic chylomicron transport systems and decoupling the intestinal P-glycoprotein drug efflux pump (Teeranachaideekul et al. 2008). For oral formulations, the dissolution process is considered as a decisive step for absorption effect. Drug nanocrystals provide smaller particle size and greater surface area for dissolution, thus raising the saturation solubility, which ultimately increases the dissolution rate, followed by enhanced absorption.
Illustration of the hypothetic oral absorption process for Nimodipine (NMD) nanocrystals (Fu et al. 2013a)
The bioavailability of poorly water-soluble drugs usually shows an increased or accelerated tendency when administered with food. They may be attributed to the enhanced dissolution rate in GIT controlled by the food effect, which causes several physiological changes, such as more secretion of gastric juices/bile, increased pH in gastric fluid, increased blood flow to the digestive organs, and delayed GET (Epstein et al. 2007). The absorption process would be limited by permeability whether in the fed or fasting state. For many traditional formulations, its bioavailability is weakened because of the absorption difference between the fasted and fed conditions. However, the variation in bioavailability resulting from the food effect can be minimized when poorly water-soluble drugs are prepared as formulations of nanocrystals. It is competent enough for the dissolution rate of drug nanocrystals to generate an efficient absorption even under the fasted state.
Pulmonary administration
The lungs are highly perfused organs because of the fully expanded surface area roughly equivalent to three standard football fields. Consequent to avoiding the first-pass effect of the liver, molecular dispersion of drug is rapidly transported into the systemic circulation with high efficiency.
The analysis of the 2002–2012 literature showed that the pulmonary delivery was a crucial area of focus with the proportion of 22 % in all routes of administration (Ambrus et al. 2009). Recently, it has been demonstrated that when the pulmonary delivery of baicalein nanocrystals was compared with oral and IV administration, the pulmonary baicalein nanocrystals had rapid and extensive absorption and pharmacokinetic parameters that were nearly identical to those of the IV baicalein injection. In conventional dispersions of solid in liquid, the particle size of a solid drug is at par with that of the aerosol. Hence, this may lead to statistical inhomogeneity in the phase of drug particles dispersing in the carrier droplets. By increasing the number of particles per droplet, drug nanocrystals with nanoscale particle size would improve the evenness. Conventional modalities of deep lung drug deposition have been modified by tailoring the size of nanocrystals. In summary, the pulmonary route for drug nanocrystals comes across as a viable option for delivery of therapeutics (Negi et al. 2013).
During the delivery process from the pharynx to lungs, the biggest obstacle of drug particles was cleared by the immune system as antigen (Li et al. 2013). The involved sites of activity mainly include the inner surface distributing mucus and cilium in the upper airways, as well as pulmonary macrophage widely distributed in the lung interstitium. Following pulmonary administration of the drug nanocrystals, there is a relatively small amount of drug deposition on the surface of the respiratory tract compared to adsorption amount of macrophage. Compared with the microparticles, nanocrystals would avoid be transported out of the lungs by cilia movement and could adhere onto the mucosal surface for a longer time. What’s more, the very low fraction of microparticles in the nanocrystals and narrow particle size distribution could reduce undesired deposition of particles in the mouth and pharynx, thereby decreasing local and systemic side effects of the drugs. For example, after taking the nanoparticles of insulin, the protein drug was degraded by phagolysosomal after the pulmonary macrophage uptake (Crisp et al. 2007). Nevertheless, macrophage uptake precisely provides an approach to achieve sustained release of some molecules which possess stability in an acidic environment and an appropriate dynamic curve of solubility with pH. Also, nanoparticles and modification of the surfactant coating could be incorporated by Van der Waals forces, where they form an intriguing system with large porous particles. The modified nanoparticles can simultaneously provide several advantages such as tenacious adsorption and minimal phagocytosis to ensure maximal dissolution (Fu et al. 2013b). Therefore, nanocrystal is a promising method to improve the efficacy of pulmonary delivery by minimizing systemic exposure and corresponding side effects.
Intravenous administration
Drug nanocrystals can be prepared as IV injection to give 100 % bioavailability accredited to the effect of small particle size and safe composition (Ige et al. 2013; Ramirez-Rigo et al. 2014). After IV injection, drug nanocrystals may give rise to passive targeting referenced to colloidal drug carriers. Concurrently, some active targeting would also be achieved when nanoparticles surface was modified with special stabilizers (Fuhrmann et al. 2014).
Recently, a study found that the active ingredients existed in the majority of the water-insoluble drugs for therapeutic applications, such as bacterial/viral infections, oncology, and central nervous system (CNS) (Mauludin et al. 2009b). With the increase in a patient population suffering from these diseases, more attention is focused on the injectable dosage form of the nanocrystals. Intramuscular (IM) injection is another parenteral route of suspension injections, which takes a longer absorption time compared to the IV injection (Zhao et al. 2010). In general, there are several factors that can cause the variability in the drug absorption of IM injection, such as hydrophilic–lipophilic balance (HLB) of drug, extent of tissue perfusion, and differences in adipose layer thickness. For IM aqueous administration, the dissolution rate is the rate-limiting step for drug absorption, which is controlled by different stages including diffusion of water and suspension, as well as dissemination of the drug into the bloodstream. In 2005, Abraxane® (amorphous particles of 130 nm) was approved for production, which is a nanoparticulate IV dosage form consisting of paclitaxel entrapped in an albumin matrix (Junyaprasert and Morakul 2015). Until now, a considerable amount of the nanoparticulate drug formulations has been successfully exercised to human clinical trials. It will be easier to predict the therapeutic responses and the associated toxicity of IV administration with less limitation on the volume.
Drug nanocrystals formulations containing ascularine, melarsoprol, oridonin, itraconazole, and curcumin have been successfully developed, providing benefits like increase in maximum concentration (C max) and the area under the curve (AUC) of the drug concentration in the plasma versus time (Mathew et al. 2014). These advantages are an open invitation to pharmaceutical scientists for exploiting the nanocrystals technology comprising of notorious water-insoluble drugs for IV delivery. Although the other benefits can be considered as ideal parameters for every drug, the IV route is limited because of the use of harmful solvent and excipients. They are used during formulation development and coadministered with the drug, which can cause serious side effects rather than the drug itself (Tuomela et al. 2015). On the contrary, drug nanocrystals could be considered as the ideal candidates for IV delivery because their developmental processes do not need an overdose of such harmful excipients.
Targeting drug delivery of nanocrystals
Nowadays, the broad-spectrum pharmaceutical formulation for treating a localized disease is no longer acceptable. For example, chemotherapeutics intended for benign tumors cause extensive adverse effects, wherein the entire body is stressed due to non-selective drug distribution (Ting et al. 2014). Therefore, it becomes exceedingly important to design new formulations which ensure targeted delivery. The mechanism of targeting drugs requires an exhaustive investigation of their physicochemical and biopharmaceutical properties to ensure that it can improve the current therapeutic profile of various APIs.
Nanotechnology has dramatically transformed the drug delivery in recent years. It has motivated researchers and pharmaceutical industry to alter the methods of formulating new as well as existing drugs extending their lifespan in the process. As described by the Ostwald–Freundlich equation, the kinetic solubility of the minute drug particles increases in the characteristic nonlinear pattern (Cooper 2010). However, the mechanism of action is only suitable for particles in the submicrometer size range. This formulation is exploited by the administration of insoluble drugs without targeted effect, which adds little cosolvents or solubilizing agents. For targeted nanocrystals delivery, enhanced dissolution complicates the treatment effect because of off-target drug delivery. The phenomenon may be caused by shedding of the targeting/stabilizing agents in active targeting, as well as an insufficient circulation time in passive targeting. Currently, passive targeting based on the development of retention effect and enhanced permeation is studied in greater detail (Pardeike et al. 2011).
Nanocrystals could be used for targeted drug delivery because their surface properties can be effortlessly altered by combining with the carrier, ligand, or antibody. The surface properties can determine the adsorption patterns between the drug nanocrystals and the blood proteins qualitatively and quantitatively (Dumarey et al. 2011). Furthermore, they can determine the subsequent distribution and metabolism in vivo, such as crossing the blood–brain barrier. Because of scalable industrial production and the formulation versatility, the development of commercially viable nanocrystals can be achieved (Gao et al. 2012). For example, Piao et al. prepared surface-modified nanocrystals of buparvaquone with mucoadhesiveness and then studied its targeted therapy for cryptosporidiosis (Piao et al. 2011). Compared to the buparvaquone nanocrystals without mucoadhesive polymers, the surface-modified ones obtained a tenfold increment in inhibiting the infectivity of cryptosporidiosis (Han et al. 2014). It can be attributed to the prolonged residence at the infection site, followed by a high plasma concentration. Similarly, amphotericin B nanocrystals in connection with the stealth liposomes can provide targeted therapy to pulmonary aspergillosis (Ali et al. 2009).
Safety and toxicity of nanocrystals
Previously, the advantages of nanoparticles were dominant in many different fields as compared to their safety concerns. In the recent years, the adverse reactions of drug nanocrystals caused great attentions toward nanotoxicity. Because the nanoparticles have a strong permeability to enter the cells causing concentration enrichment, they may lead to single cells’ damage or even systemic adverse reactions such as irritation of the immune system (Wang et al. 2013). Hence, it is indispensable to consider cellular interactions and uptake during the research and development of drugs nanoparticles.
The most outstanding advantages of the nanocrystal strategy for the development of water-insoluble compounds are decrease in the potential toxicity of the formulation on patients or animal models with improving the tolerability of the delivered drug. Previous approaches for developing poorly soluble API have mainly focused on cosolvents and solubilizers, including cyclodextrin (Sun et al. 2012). Although these methods could solve the solubility problem, the potential toxicity of the excipients gives rise to multiple side effects and a high frequency of serious adverse reactions in clinical treatments. Furthermore, these strategies are also limited by their capacity to keep a compound in solution after delivery into the body.
The MPS is a widely distributed system of free and fixed macrophages derived from the bone marrow. It is an important part of the body’s defense structure identifying and removing foreign particles from the body. Once the nanoparticles are detected as foreign matters by the MPS cells, they are withdrawn from the bloodstream by phagocytosis rapidly and efficiently, leading to accumulation in special organs and tissues, such as the brain, liver, lung, kidney and spleen (Sun and Yeo 2012). For example, during IV administration of drug nanocrystals, if the particle size of the nanocrystals is significantly larger than 100 nm and the surface modification of the particles is not good enough to avoid opsonization, the nanocrystals will be opsonized in the circulation and cleared immediately by the phagocytic cells of MPS. For the IV injection of nanocrystals, the situation is more complex. On one hand, complete dissolution of drug nanocrystals with the particle size about 100 nm in vivo typically takes 5–10 min (Dong et al. 2014), and on the other hand, within 5 min post injection, the injected dose of up to 90 % is absorbed by the Kupffer cells versus about 5 % by the spleen macrophages (Li et al. 2011). As a result, a significant portion of insolubilized nanocrystals is absorbed by the liver than the spleen, which would lead to several biological consequences. The rapid clearance of nanocrystals will result in toxic accumulation in the liver and kidney if they are not designed to provide targeted therapy for such organs. For example, a typical case is delivering anticancer drugs of chemotherapeutic agents. Moreover, a concentration of drug nanocrystals with cytotoxicity may cause apoptosis in liver and spleen. Hence, it is a compelling issue to avoid recognition and rapid clearance by MPS. It is reported that Nevirapine nanocrystals with the stabilizer of PEG1000 can reduce the intake by macrophages in vitro (Yao et al. 2012).
For the development of a novel drug delivery system through the parenteral route, the carrier system should not be phagocytosed by the reticuloendothelial system and Kupffer cells. Ordinarily, the particle size below 100 nm is preferred for the parenteral nanocrystals (Merisko-Liversidge and Liversidge 2011). The macrophages are in a position to swallow all types of biodegradable particles, and the drug nanocrystals can be engulfed faster than the inert particles by the phagolysosomes (Sinha et al. 2013b). The rapid uptake of drug nanoparticles may exert burden on the macrophages. Consequently, the reticuloendothelial system may be overloaded by excessive phagocytic activity. Besides, more critical situations will occur in case the phagocytic overload is continued, for example, reticuloendothelial blockage. However, the drug accumulated in the liver by phagocytosis could be slowly released into the blood, positively affecting some treatments as a substitute for persistent infusion. Moreover, drug nanocrystals providing sustained release in delivery brings about a minimizing risk of toxic concentration for cells and organs. It is essential to reduce the drug nanoparticles size to effectively avoid capillary blockage.
Commercial drug nanocrystals
Recently, nanocrystals technology has been globally applied to pharmaceutical research, improving pharmacokinetics and pharmacodynamics of drugs, and achieving significant progress (Lai et al. 2014).
Rapamune®
The active drug of Rapamune® is sirolimus (SRL), derived from Streptomyces hygroscopicus. The SRL is a type of macrolides immunosuppressant with the average molecular weight of 914.17 (Waksman et al. 2004). The solid dosage form of SRL is the first product using nanocrystals technology approved by the Food and Drug Administration (FDA). SRL is unstable under light and heat, requiring dark and sealed storage at 4–8 °C (Kocbek et al. 2006). The oral solution of SRL contains a surfactant, ethanol, and grease, with a bioavailability of about 14 %. After oral administration, the drug will precipitate from the solution when in contact with the aqueous medium in GIT. The precipitated drug rapidly forms large size solid particles that are difficult to be directly absorbed via the digestive tract. In 1999, oral solutions of SRL appeared on the market in the USA for the first time, prepared by Wyeth Pharmaceutical Company Ltd. The mass concentration of this kind of SRL is 1 mg/mL with the specifications of 60 mL and 150 mL. In 2000, the nanocrystals of SRL tablets with a specification of 1 mg listed in the USA using nanotechnology of Elan Chemical Company Inc (Guo et al. 2013). The nanocrystals tablets have an improved bioavailability of 21 % compared to the oral solution. The single dose of oral SRL nanocrystals tablet is 1 or 2 mg, and the total tablet weight being approximately 365 mg for 1 mg formulation, thus indicating that the product contains a very low percentage of nanocrystals in its total weight.
Megace ES®
In 2003, the FDA approved Par Pharmaceutical Companies Inc. (Spring Valley, NY) to produce nanocrystals of Megace ES® (ES represents high stability), which contains megestrol acetate (MA) as the active drug, to treat patients with loss of appetite, mental depression, and weight loss because of AIDS (Zhou et al. 2015). Usually, the original dosage form of MA is oral administration after supper, despite a poor appetite in such patients, which is further aggravated because of the high viscosity of the drug. The viscosity of MA nanocrystals is reduced to 1/16th of the initial dosage form. Thus, its solubility and bioavailability were improved significantly (Wu et al. 2004). Consequently, the patients received an oral administration of 5 mL/day compared to the 20 mL of the original dosage, significantly reducing the burden of administration and decreasing the pharmacodynamic differences in fasting plasma or full abdomen (Choudhury et al. 2014).
Tricor®
As one of the most successful cases, Tricor® is produced by Abbott Laboratories, containing fenofibrate as the active ingredient. Tricor® is designed for adult patients with primary hypercholesterolemia or mixed dyslipidemia such as IIa and IIb of Fredrickson type. The main mechanism includes reducing low-density lipoprotein cholesterol (LDL-C), triglycerides (TG), apolipoprotein B (Apo B) or total cholesterol (Total-C), and increasing high-density lipoprotein cholesterol (HDL-C) (Baek et al. 2014). The new formulation of Tricor® is prepared by nanocrystals technology from Elan Chemical Company Inc. Irrespective of the food factor, fenofibrate nanocrystals have a faster dissolution in GIT and complete absorption (Rahim et al. 2012). The dose specifications of TriCor® include 48 mg and 145 mg per tablet, which is significantly preferred than the conventional dosage tablets, demanding 54 mg and 160 mg/tablet, respectively, achieving the same therapeutic effect (Setua et al. 2010).
Table 2 shows examples of currently marketed pharmaceutical products utilizing nanocrystalline formulations.
Conclusions and perspectives
Drug nanocrystals were proposed at the beginning of the 1990s for promoting the delivery of poorly water-soluble drugs. It is a unique approach to solving bioavailability-related issues. Industrially feasible manufacturing techniques have served to transfer nanocrystals from the laboratory to clinical application at an accelerated rate. As a result, they are regarded as suitable candidates for delivery of poorly water-soluble drugs taking into account the reduced side effects and potential advantages. For oral administration, many articles expounded useful advantages of nanocrystals to improve in vivo performances, such as pharmacokinetics, pharmacodynamics, safety and targeted delivery. Additionally, the transformation of nanocrystals to final formulations and future trends were described in this review. Nanocrystals decorated with functionalized ligands have achieved fruitful progress by being able to target various organs with higher affinity. Moreover, incorporation of appropriate stabilizers followed by drying (freeze/spray) can ensure their long-term stability. Dried nanocrystals are suitable for pharmaceutical processing such as granulation, which might usher a new era of second generation nanocrystals. Drug nanocrystals might also be an opportunity to produce generic versions of presently available expensive drugs. Undoubtedly, the engineered nanocrystals technology has an imminent prospective in the pharmaceutical industry with more commercial products that could be applied to additional administration routes in an acceptable and effective dosage form.
Although drug nanocrystals are considered as a sophisticated formulation method, there are still several issues, such as the uncertain nanotoxicity, scientific complexities, and rigorous government approvals. Drug nanocrystals are considered as harmless because all the applied drugs are micrometer particles at the end of its dissolution based on the qualitative understanding. However, the limited studies of cytotoxicity for viability references usually display an unfavorable outcome. Thus, this classification is apparently inaccurate as there are no contradictory reports, thereby necessitating a thorough investigation at the molecular level, including loss of potassium from inside the cells, lactate dehydrogenase (LDH) release, and the production of cytokines, on the solid lipid nanoparticles. Scale-up on pharmaceutical manufacturing process is a translation involving the transformation from microscopic (molecular) laboratory level to macroscopic (bulk) industrial commercial-scale production. The success of any formulation development depends on its transferability to large scale and all the nanocrystals products already in the market might be efficient. In summary, a scalable formulation/method will strictly enforce all the three levels of study, i.e., the laboratory, pilot magnification, and industry.
Future research warrants main focus on the following: (a) By grafting various functional groups on the hydrophilic chains of nanocrystals, for example, pH-sensitive groups could be increasing the local concentration in a particular environment of drug release and helping to improve the BA. (b) To increase the hydrophilicity and reduce plasma protein adsorption on the crystal surface via surface modification of insoluble drugs nanocrystals, thus enhancing the BA of drugs. (c) To strengthen the research of invisibility of nanocrystals avoiding mononuclear phagocyte system, MPS identification and quick elimination of drugs nanocrystals. Furthermore, in-depth in vivo and in vitro studies of the biological effects, optimizing synthesis technology as well as processing methods of drugs nanocrystals are required.
Abbreviations
- SND:
-
Synthetic new drugs
- C s :
-
Saturation solubility
- API:
-
Active pharmaceutical ingredient
- S :
-
Surface area
- dm/dt :
-
Dissolution velocity
- GIT:
-
Gastrointestinal tract
- IV:
-
Intravenous
- MPS:
-
Mononuclear phagocyte system
- PVP:
-
Polyvinylpyrrolidone
- HPMC:
-
Hydroxypropyl methylcellulose
- PEG:
-
Polyethylene glycol
- HPC:
-
Hydroxypropyl cellulose
- PVA:
-
Polyvinyl alcohol
- BCP:
-
Amphiphilic block copolymer
- SCF:
-
Supercritical fluids technology
- RESOLV:
-
Rapid expansion of a supercritical solution into a liquid solvent
- RESS:
-
Rapid expansion of supercritical solution
- SAS:
-
Supercritical antisolvent
- CO2 :
-
Carbon dioxide
- GET:
-
Gastric emptying time
- LD:
-
Laser diffraction
- DLS:
-
Dynamic light scattering
- SIOS:
-
Scanning ion occlusion sensing
- AFM:
-
Tomic force microscopy
- SEM:
-
Scanning electron microscopy
- TEM:
-
Transmission electron microscope
- NMD:
-
Nimodipine
- CNS:
-
Central nervous system
- IM:
-
Intramuscular
- HLB:
-
Hydrophilic–lipophilic balance
- C max :
-
Maximum concentration
- AUC:
-
Area under the curve
- SRL:
-
Sirolimus
- FDA:
-
Food and drug administration
- MA:
-
Megestrol acetate
- LDL-C:
-
Low-density lipoprotein cholesterol
- TG:
-
Triglycerides
- Apo B:
-
Apolipoprotein B
- Total-C:
-
Total cholesterol
- HDL-C:
-
High-density lipoprotein cholesterol
- LDH:
-
Lactate dehydrogenase
References
Aditya NP, Yang H, Kim S, Ko S (2015) Fabrication of amorphous curcumin nanosuspensions using beta-lactoglobulin to enhance solubility, stability, and bioavailability. Colloids Surf B 127:114–121. doi:10.1016/j.colsurfb.2015.01.027
Ain-Ai A, Gupta PK (2008) Effect of arginine hydrochloride and hydroxypropyl cellulose as stabilizers on the physical stability of high drug loading nanosuspensions of a poorly soluble compound. Int J Pharm 351:282–288. doi:10.1016/j.ijpharm.2007.09.029
Ali HS, York P, Blagden N (2009) Preparation of hydrocortisone nanosuspension through a bottom-up nanoprecipitation technique using microfluidic reactors. Int J Pharm 375:107–113. doi:10.1016/j.ijpharm.2009.03.029
Ali HS, York P, Ali AM, Blagden N (2011) Hydrocortisone nanosuspensions for ophthalmic delivery: a comparative study between microfluidic nanoprecipitation and wet milling. J Control Release 149:175–181. doi:10.1016/j.jconrel.2010.10.007
Ambrus R, Kocbek P, Kristl J, Sibanc R, Rajko R, Szabo-Revesz P (2009) Investigation of preparation parameters to improve the dissolution of poorly water-soluble meloxicam. Int J Pharm 381:153–159. doi:10.1016/j.ijpharm.2009.07.009
Aqil F, Munagala R, Jeyabalan J, Vadhanam MV (2013) Bioavailability of phytochemicals and its enhancement by drug delivery systems. Cancer Lett 334:133–141. doi:10.1016/j.canlet.2013.02.032
Baek I-H, Kim J-S, Ha E-S, Choo G-H, Cho W, Hwang S-J, Kim M-S (2014) Dissolution and oral absorption of pranlukast nanosuspensions stabilized by hydroxypropylmethyl cellulose. Int J Biol Macromol 67:53–57. doi:10.1016/j.ijbiomac.2014.03.006
Bao Y, Krishnan KM (2005) Preparation of functionalized and gold-coated cobalt nanocrystals for biomedical applications. J Magn Magn Mater 293:15–19. doi:10.1016/j.jmmm.2005.01.037
Chan HK, Kwok PC (2011) Production methods for nanodrug particles using the bottom-up approach. Adv Drug Deliv Rev 63:406–416. doi:10.1016/j.addr.2011.03.011
Cheng CL, Yu LX, Lee HL, Yang CY, Lue CS, Chou CH (2004) Biowaiver extension potential to BCS Class III high solubility-low permeability drugs: bridging evidence for metformin immediate-release tablet. Eur J Pharm Sci 22:297–304. doi:10.1016/j.ejps.2004.03.016
Chin WW, Parmentier J, Widzinski M, Tan EH, Gokhale R (2014) A brief literature and patent review of nanosuspensions to a final drug product. J Pharm Sci 103:2980–2999. doi:10.1002/jps.24098
Choudhury H et al (2014) Improvement of cellular uptake, in vitro antitumor activity and sustained release profile with increased bioavailability from a nanoemulsion platform. Int J Pharm 460:131–143. doi:10.1016/j.ijpharm.2013.10.055
Cooper ER (2010) Nanoparticles: a personal experience for formulating poorly water soluble drugs. J Control Release 141:300–302. doi:10.1016/j.jconrel.2009.10.006
Crisp MT, Tucker CJ, Rogers TL, Williams RO 3rd, Johnston KP (2007) Turbidimetric measurement and prediction of dissolution rates of poorly soluble drug nanocrystals. J Control Release 117:351–359. doi:10.1016/j.jconrel.2006.11.011
Custodio JM, Wu CY, Benet LZ (2008) Predicting drug disposition, absorption/elimination/transporter interplay and the role of food on drug absorption. Adv Drug Deliv Rev 60:717–733. doi:10.1016/j.addr.2007.08.043
D’Addio SM et al (2012) Effects of block copolymer properties on nanocarrier protection from in vivo clearance. J Control Release 162:208–217. doi:10.1016/j.jconrel.2012.06.020
Das S, Suresh PK (2011) Nanosuspension: a new vehicle for the improvement of the delivery of drugs to the ocular surface. Application to amphotericin B. Nanomedicine 7:242–247. doi:10.1016/j.nano.2010.07.003
Dong Y, Ng WK, Hu J, Shen S, Tan RB (2014) Clay as a matrix former for spray drying of drug nanosuspensions. Int J Pharm 465:83–89. doi:10.1016/j.ijpharm.2014.02.025
Donoso MD, Haskell RJ, Schartman RR (2012) Surfactant choice and the physical stability of nanosuspensions as a function of pH. Int J Pharm 439:1–7. doi:10.1016/j.ijpharm.2012.09.012
Dumarey M, Wikström H, Fransson M, Sparén A, Tajarobi P, Josefson M, Trygg J (2011) Combining experimental design and orthogonal projections to latent structures to study the influence of microcrystalline cellulose properties on roll compaction. Int J Pharm 416:110–119. doi:10.1016/j.ijpharm.2011.06.018
Epstein H, Berger V, Levi I, Eisenberg G, Koroukhov N, Gao J, Golomb G (2007) Nanosuspensions of alendronate with gallium or gadolinium attenuate neointimal hyperplasia in rats. J Control Release 117:322–332. doi:10.1016/j.jconrel.2006.10.030
Fu Q et al (2013a) Nimodipine nanocrystals for oral bioavailability improvement: role of mesenteric lymph transport in the oral absorption. Int J Pharm 448:290–297. doi:10.1016/j.ijpharm.2013.01.065
Fu Q et al (2013b) Nimodipine nanocrystals for oral bioavailability improvement: preparation, characterization and pharmacokinetic studies. Colloids Surf B 109:161–166. doi:10.1016/j.colsurfb.2013.01.066
Fuhrmann K, Gauthier MA, Leroux JC (2014) Targeting of injectable drug nanocrystals. Mol Pharm 11:1762–1771. doi:10.1021/mp5001247
Galli C (2006) Experimental determination of the diffusion boundary layer width of micron and submicron particles. Int J Pharm 313:114–122. doi:10.1016/j.ijpharm.2006.01.030
Gao L, Liu G, Ma J, Wang X, Zhou L, Li X (2012) Drug nanocrystals: in vivo performances. J Control Release 160:418–430. doi:10.1016/j.jconrel.2012.03.013
Gao L et al (2013) Paclitaxel nanosuspensions coated with P-gp inhibitory surfactants: i. Acute toxicity and pharmacokinetics studies. Colloids Surf B 111:277–281. doi:10.1016/j.colsurfb.2013.06.004
Gardikis K, Tsimplouli C, Dimas K, Micha-Screttas M, Demetzos C (2010) New chimeric advanced drug delivery nano systems (chi-aDDnSs) as doxorubicin carriers. Int J Pharm 402:231–237. doi:10.1016/j.ijpharm.2010.10.007
George M, Ghosh I (2013) Identifying the correlation between drug/stabilizer properties and critical quality attributes (CQAs) of nanosuspension formulation prepared by wet media milling technology. Eur J Pharm Sci 48:142–152. doi:10.1016/j.ejps.2012.10.004
Ghosh I, Bose S, Vippagunta R, Harmon F (2011) Nanosuspension for improving the bioavailability of a poorly soluble drug and screening of stabilizing agents to inhibit crystal growth. Int J Pharm 409:260–268. doi:10.1016/j.ijpharm.2011.02.051
Gramdorf S, Hermann S, Hentschel A, Schrader K, Müller RH, Kumpugdee-Vollrath M, Kraume M (2008) Crystallized miniemulsions: influence of operating parameters during high-pressure homogenization on size and shape of particles. Colloids Surf A 331:108–113. doi:10.1016/j.colsurfa.2008.07.016
Guo JJ et al (2013) Development and in vivo/in vitro evaluation of novel herpetrione nanosuspension. Int J Pharm 441:227–233. doi:10.1016/j.ijpharm.2012.11.039
Han M, Yu X, Guo Y, Wang Y, Kuang H, Wang X (2014) Honokiol nanosuspensions: preparation, increased oral bioavailability and dramatically enhanced biodistribution in the cardio-cerebro-vascular system. Colloids Surf B 116:114–120. doi:10.1016/j.colsurfb.2013.12.056
Hanafy A, Spahn-Langguth H, Vergnault G, Grenier P, Tubic Grozdanis M, Lenhardt T, Langguth P (2007) Pharmacokinetic evaluation of oral fenofibrate nanosuspensions and SLN in comparison to conventional suspensions of micronized drug. Adv Drug Deliv Rev 59:419–426. doi:10.1016/j.addr.2007.04.005
Hu X, Chen X, Zhang L, Lin X, Zhang Y, Tang X, Wang Y (2014) A combined bottom-up/top-down approach to prepare a sterile injectable nanosuspension. Int J Pharm 472:130–139. doi:10.1016/j.ijpharm.2014.06.018
Ige PP, Baria RK, Gattani SG (2013) Fabrication of fenofibrate nanocrystals by probe sonication method for enhancement of dissolution rate and oral bioavailability. Colloids Surf B 108:366–373. doi:10.1016/j.colsurfb.2013.02.043
Jeevanandam J, Chan YS, Danquah MK (2016) Nano-formulations of drugs: recent developments, impact and challenges. Biochimie. doi:10.1016/j.biochi.2016.07.008
Juhnke M, Martin D, John E (2012) Generation of wear during the production of drug nanosuspensions by wet media milling. Eur J Pharm Biopharm 81:214–222. doi:10.1016/j.ejpb.2012.01.005
Junyaprasert VB, Morakul B (2015) Nanocrystals for enhancement of oral bioavailability of poorly water-soluble drugs. Asian J Pharm Sci 10:13–23. doi:10.1016/j.ajps.2014.08.005
Kawakami K (2012) Modification of physicochemical characteristics of active pharmaceutical ingredients and application of supersaturatable dosage forms for improving bioavailability of poorly absorbed drugs. Adv Drug Deliv Rev 64:480–495. doi:10.1016/j.addr.2011.10.009
Keck CM (2010) Particle size analysis of nanocrystals: improved analysis method. Int J Pharm 390:3–12. doi:10.1016/j.ijpharm.2009.08.042
Keck CM, Muller RH (2006) Drug nanocrystals of poorly soluble drugs produced by high pressure homogenisation. Eur J Pharm Biopharm 62:3–16. doi:10.1016/j.ejpb.2005.05.009
Kesisoglou F, Panmai S, Wu Y (2007) Nanosizing–oral formulation development and biopharmaceutical evaluation. Adv Drug Deliv Rev 59:631–644. doi:10.1016/j.addr.2007.05.003
Khadka P et al (2014) Pharmaceutical particle technologies: an approach to improve drug solubility, dissolution and bioavailability. Asian J Pharm Sci 9:304–316. doi:10.1016/j.ajps.2014.05.005
Kim S, Lee J (2010) Effective polymeric dispersants for vacuum, convection and freeze drying of drug nanosuspensions. Int J Pharm 397:218–224. doi:10.1016/j.ijpharm.2010.07.010
Kocbek P, Baumgartner S, Kristl J (2006) Preparation and evaluation of nanosuspensions for enhancing the dissolution of poorly soluble drugs. Int J Pharm 312:179–186. doi:10.1016/j.ijpharm.2006.01.008
Kratz F, Warnecke A (2012) Finding the optimal balance: challenges of improving conventional cancer chemotherapy using suitable combinations with nano-sized drug delivery systems. J Control Release 164:221–235. doi:10.1016/j.jconrel.2012.05.045
Lai F, Pini E, Corrias F, Perricci J, Manconi M, Fadda AM, Sinico C (2014) Formulation strategy and evaluation of nanocrystal piroxicam orally disintegrating tablets manufacturing by freeze-drying. Int J Pharm 467:27–33. doi:10.1016/j.ijpharm.2014.03.047
Latha S, Selvamani P, Kumar CS, Sharavanan P, Suganya G, Beniwal VS, Rao PR (2009) Formulation development and evaluation of metronidazole magnetic nanosuspension as a magnetic-targeted and polymeric-controlled drug delivery system. J Magn Magn Mater 321:1580–1585. doi:10.1016/j.jmmm.2009.02.089
Lee J, Lee SJ, Choi JY, Yoo JY, Ahn CH (2005) Amphiphilic amino acid copolymers as stabilizers for the preparation of nanocrystal dispersion. Eur J Pharm Sci 24:441–449. doi:10.1016/j.ejps.2004.12.010
Lemke A, Kiderlen AF, Petri B, Kayser O (2010) Delivery of amphotericin B nanosuspensions to the brain and determination of activity against Balamuthia mandrillaris amebas. Nanomedicine 6:597–603. doi:10.1016/j.nano.2009.12.004
Li W et al (2011) Preparation and in vitro/in vivo evaluation of revaprazan hydrochloride nanosuspension. Int J Pharm 408:157–162. doi:10.1016/j.ijpharm.2011.01.059
Li TJ, Huang CC, Ruan PW, Chuang KY, Huang KJ, Shieh DB, Yeh CS (2013) In vivo anti-cancer efficacy of magnetite nanocrystal–based system using locoregional hyperthermia combined with 5-fluorouracil chemotherapy. Biomaterials 34:7873–7883. doi:10.1016/j.biomaterials.2013.07.012
Li W et al (2014) Influence of drug physicochemical properties on absorption of water insoluble drug nanosuspensions. Int J Pharm 460:13–23. doi:10.1016/j.ijpharm.2013.10.038
Liu P et al (2011) Nanosuspensions of poorly soluble drugs: preparation and development by wet milling. Int J Pharm 411:215–222. doi:10.1016/j.ijpharm.2011.03.050
Ma Q, Sun H, Che E, Zheng X, Jiang T, Sun C, Wang S (2013) Uniform nano-sized valsartan for dissolution and bioavailability enhancement: influence of particle size and crystalline state. Int J Pharm 441:75–81. doi:10.1016/j.ijpharm.2012.12.025
Mathew AP, Oksman K, Karim Z, Liu P, Khan SA, Naseri N (2014) Process scale up and characterization of wood cellulose nanocrystals hydrolysed using bioethanol pilot plant. Ind Crops Prod 58:212–219. doi:10.1016/j.indcrop.2014.04.035
Mauludin R, Muller RH, Keck CM (2009a) Development of an oral rutin nanocrystal formulation. Int J Pharm 370:202–209. doi:10.1016/j.ijpharm.2008.11.029
Mauludin R, Muller RH, Keck CM (2009b) Kinetic solubility and dissolution velocity of rutin nanocrystals. Eur J Pharm Sci 36:502–510. doi:10.1016/j.ejps.2008.12.002
Merisko-Liversidge E, Liversidge GG (2011) Nanosizing for oral and parenteral drug delivery: a perspective on formulating poorly-water soluble compounds using wet media milling technology. Adv Drug Deliv Rev 63:427–440. doi:10.1016/j.addr.2010.12.007
Moorthi C, Kathiresan K (2013) Fabrication of highly stable sonication assisted curcumin nanocrystals by nanoprecipitation method. Drug Invent Today 5:66–69. doi:10.1016/j.dit.2013.02.003
Morakul B, Suksiriworapong J, Leanpolchareanchai J, Junyaprasert VB (2013) Precipitation-lyophilization-homogenization (PLH) for preparation of clarithromycin nanocrystals: influencing factors on physicochemical properties and stability. Int J Pharm 457:187–196. doi:10.1016/j.ijpharm.2013.09.022
Morgenthal G, Sánchez Corriols A, Bendig B (2014) A GPU-accelerated pseudo-3D vortex method for aerodynamic analysis. J Wind Eng Ind Aerodyn 125:69–80. doi:10.1016/j.jweia.2013.12.002
Moschwitzer J, Achleitner G, Pomper H, Muller RH (2004) Development of an intravenously injectable chemically stable aqueous omeprazole formulation using nanosuspension technology. Eur J Pharm Biopharm 58:615–619. doi:10.1016/j.ejpb.2004.03.022
Mou D, Chen H, Wan J, Xu H, Yang X (2011) Potent dried drug nanosuspensions for oral bioavailability enhancement of poorly soluble drugs with pH-dependent solubility. Int J Pharm 413:237–244. doi:10.1016/j.ijpharm.2011.04.034
Muller RH, Runge S, Ravelli V, Mehnert W, Thunemann AF, Souto EB (2006) Oral bioavailability of cyclosporine: solid lipid nanoparticles (SLN) versus drug nanocrystals. Int J Pharm 317:82–89. doi:10.1016/j.ijpharm.2006.02.045
Muller RH, Gohla S, Keck CM (2011) State of the art of nanocrystals–special features, production, nanotoxicology aspects and intracellular delivery. Eur J Pharm Biopharm 78:1–9. doi:10.1016/j.ejpb.2011.01.007
Negi LM, Tariq M, Talegaonkar S (2013) Nano scale self-emulsifying oil based carrier system for improved oral bioavailability of camptothecin derivative by P-glycoprotein modulation. Colloids Surf B 111:346–353. doi:10.1016/j.colsurfb.2013.06.001
Niwa T, Nakanishi Y, Danjo K (2010) One-step preparation of pharmaceutical nanocrystals using ultra cryo-milling technique in liquid nitrogen. Eur J Pharm Sci 41:78–85. doi:10.1016/j.ejps.2010.05.019
Pardeike J, Strohmeier DM, Schrodl N, Voura C, Gruber M, Khinast JG, Zimmer A (2011) Nanosuspensions as advanced printing ink for accurate dosing of poorly soluble drugs in personalized medicines. Int J Pharm 420:93–100. doi:10.1016/j.ijpharm.2011.08.033
Pawar VK, Singh Y, Meher JG, Gupta S, Chourasia MK (2014) Engineered nanocrystal technology: in vivo fate, targeting and applications in drug delivery. J Control Release 183:51–66. doi:10.1016/j.jconrel.2014.03.030
Piao H, Kamiya N, Cui F, Goto M (2011) Preparation of a solid-in-oil nanosuspension containing l-ascorbic acid as a novel long-term stable topical formulation. Int J Pharm 420:156–160. doi:10.1016/j.ijpharm.2011.08.025
Rabinow BE (2004) Nanosuspensions in drug delivery. Nature reviews Drug discov 3:785–796. doi:10.1038/nrd1494
Rabinow B et al (2007) Itraconazole IV nanosuspension enhances efficacy through altered pharmacokinetics in the rat. Int J Pharm 339:251–260. doi:10.1016/j.ijpharm.2007.02.030
Rahim S, Sasani Ghamsari M, Radiman S (2012) Surface modification of titanium oxide nanocrystals with PEG. Sci Iran 19:948–953. doi:10.1016/j.scient.2012.03.009
Ramirez-Rigo MV, Olivera ME, Rubio M, Manzo RH (2014) Enhanced intestinal permeability and oral bioavailability of enalapril maleate upon complexation with the cationic polymethacrylate Eudragit E100. Eur J Pharm Sci 55:1–11. doi:10.1016/j.ejps.2014.01.001
Ranjita S (2013) Nanosuspensions: a new approach for organ and cellular targeting in infectious diseases. J Pharm Sci 43:1–26. doi:10.1007/s40005-013-0051-x
Rasenack N, Hartenhauer H, Müller BW (2003) Microcrystals for dissolution rate enhancement of poorly water-soluble drugs. Int J Pharm 254:137–145. doi:10.1016/s0378-5173(03)00005-x
Ravi H, Baskaran V (2015) Biodegradable chitosan-glycolipid hybrid nanogels: a novel approach to encapsulate fucoxanthin for improved stability and bioavailability. Food Hydrocoll 43:717–725. doi:10.1016/j.foodhyd.2014.08.004
Setua S, Menon D, Asok A, Nair S, Koyakutty M (2010) Folate receptor targeted, rare-earth oxide nanocrystals for bi-modal fluorescence and magnetic imaging of cancer cells. Biomaterials 31:714–729. doi:10.1016/j.biomaterials.2009.09.090
Shegokar R, Jansch M, Singh KK, Muller RH (2011) In vitro protein adsorption studies on nevirapine nanosuspensions for HIV/AIDS chemotherapy. Nanomedicine 7:333–340. doi:10.1016/j.nano.2010.10.012
Shegokar R, Muller RH (2010) Nanocrystals: industrially feasible multifunctional formulation technology for poorly soluble actives. Int J Pharm 399:129–139. doi:10.1016/j.ijpharm.2010.07.044
Sher P, Ingavle G, Ponrathnam S, Pawar A (2007) Low density porous carrierdrug adsorption and release study by response surface methodology using different solvents. Int J Pharm 331:72–83. doi:10.1016/j.ijpharm.2006.09.013
Shi L, Riziotis VA, Voutsinas SG, Wang J (2014) A consistent vortex model for the aerodynamic analysis of vertical axis wind turbines. J Wind Eng Ind Aerodyn 135:57–69. doi:10.1016/j.jweia.2014.10.002
Sinha B, Muller RH, Moschwitzer JP (2013a) Bottom-up approaches for preparing drug nanocrystals: formulations and factors affecting particle size. Int J Pharm 453:126–141. doi:10.1016/j.ijpharm.2013.01.019
Sinha B, Muller RH, Moschwitzer JP (2013b) Systematic investigation of the cavi-precipitation process for the production of ibuprofen nanocrystals. Int J Pharm 458:315–323. doi:10.1016/j.ijpharm.2013.10.025
Song N, Wu X, Gao Z, Zhou G, Zhang WJ, Liu W (2012) Enhanced expression of membrane transporter and drug resistance in keloid fibroblasts. Hum Pathol 43:2024–2032. doi:10.1016/j.humpath.2011.12.026
Sosnik A, Das Neves J, Sarmento B (2014) Mucoadhesive polymers in the design of nano-drug delivery systems for administration by non-parenteral routes: a review. Prog Polym Sci 39:2030–2075. doi:10.1016/j.progpolymsci.2014.07.010
Sun B, Yeo Y (2012) Nanocrystals for the parenteral delivery of poorly water-soluble drugs. Curr Opin Solid State Mater Sci 16:295–301. doi:10.1016/j.cossms.2012.10.004
Sun W, Tian W, Zhang Y, He J, Mao S, Fang L (2012) Effect of novel stabilizers–cationic polymers on the particle size and physical stability of poorly soluble drug nanocrystals. Nanomed–Nanotechnol 8:460–467. doi:10.1016/j.nano.2011.07.006
Teeranachaideekul V, Junyaprasert VB, Souto EB, Muller RH (2008) Development of ascorbyl palmitate nanocrystals applying the nanosuspension technology. Int J Pharm 354:227–234. doi:10.1016/j.ijpharm.2007.11.062
Thorat AA, Dalvi SV (2012) Liquid antisolvent precipitation and stabilization of nanoparticles of poorly water soluble drugs in aqueous suspensions: recent developments and future perspective. Chem Eng J 181–182:1–34. doi:10.1016/j.cej.2011.12.044
Ting Y, Jiang Y, Ho C-T, Huang Q (2014) Common delivery systems for enhancing in vivo bioavailability and biological efficacy of nutraceuticals. J Funct Foods 7:112–128. doi:10.1016/j.jff.2013.12.010
Tran T-H, Nguyen T-D (2011) Controlled growth of uniform noble metal nanocrystals: aqueous-based synthesis and some applications in biomedicine. Colloids Surf B 88:1–22. doi:10.1016/j.colsurfb.2011.07.017
Tuomela A et al (2015) Solid formulations by a nanocrystal approach: critical process parameters regarding scale-ability of nanocrystals for tableting applications. Int J Pharm 485:77–86. doi:10.1016/j.ijpharm.2015.03.009
Van Eerdenbrugh B, Froyen L, Van Humbeeck J, Martens JA, Augustijns P, Van Den Mooter G (2008a) Alternative matrix formers for nanosuspension solidification: dissolution performance and X-ray microanalysis as an evaluation tool for powder dispersion. Eur J Pharm Sci 35:344–353. doi:10.1016/j.ejps.2008.08.003
Van Eerdenbrugh B, Van den Mooter G, Augustijns P (2008b) Top-down production of drug nanocrystals: nanosuspension stabilization, miniaturization and transformation into solid products. Int J Pharm 364:64–75. doi:10.1016/j.ijpharm.2008.07.023
Van Eerdenbrugh B, Vermant J, Martens JA, Froyen L, Van Humbeeck J, Augustijns P, Van den Mooter G (2009) A screening study of surface stabilization during the production of drug nanocrystals. J Pharm Sci 98:2091–2103. doi:10.1002/jps.21563
Verma S, Kumar S, Gokhale R, Burgess DJ (2011) Physical stability of nanosuspensions: investigation of the role of stabilizers on Ostwald ripening. Int J Pharm 406:145–152. doi:10.1016/j.ijpharm.2010.12.027
Waksman R et al (2004) Oral rapamycin to inhibit restenosis after stenting of de novo coronary lesions. JACC 44:1386–1392. doi:10.1016/j.jacc.2004.06.069
Wang GD, Mallet FP, Ricard F, Heng JYY (2012) Pharmaceutical nanocrystals. Curr Opin Chem Eng 1:102–107. doi:10.1016/j.coche.2011.12.001
Wang Y et al (2013) In vitro and in vivo anticancer activity of a novel puerarin nanosuspension against colon cancer, with high efficacy and low toxicity. Int J Pharm 441:728–735. doi:10.1016/j.ijpharm.2012.10.021
Wu Y et al (2004) The role of biopharmaceutics in the development of a clinical nanoparticle formulation of MK-0869: a Beagle dog model predicts improved bioavailability and diminished food effect on absorption in human. Int J Pharm 285:135–146. doi:10.1016/j.ijpharm.2004.08.001
Wu L, Zhang J, Watanabe W (2011) Physical and chemical stability of drug nanoparticles. Adv Drug Deliv Rev 63:456–469. doi:10.1016/j.addr.2011.02.001
Yao L et al (2012) In vitro and in vivo evaluation of camptothecin nanosuspension: a novel formulation with high antitumor efficacy and low toxicity. Int J Pharm 423:586–588. doi:10.1016/j.ijpharm.2011.11.031
Zhang J, Lv H, Jiang K, Gao Y (2011) Enhanced bioavailability after oral and pulmonary administration of baicalein nanocrystal. Int J Pharm 420:180–188. doi:10.1016/j.ijpharm.2011.08.023
Zhang J, Huang Y, Liu D, Gao Y, Qian S (2013) Preparation of apigenin nanocrystals using supercritical antisolvent process for dissolution and bioavailability enhancement. Eur J Pharm Sci 48:740–747. doi:10.1016/j.ejps.2012.12.026
Zhang Y, Che E, Zhang M, Sun B, Gao J, Han J, Song Y (2014) Increasing the dissolution rate and oral bioavailability of the poorly water-soluble drug valsartan using novel hierarchical porous carbon monoliths. Int J Pharm 473:375–383. doi:10.1016/j.ijpharm.2014.07.024
Zhao YX, Hua HY, Chang M, Liu WJ, Zhao Y, Liu HM (2010) Preparation and cytotoxic activity of hydroxycamptothecin nanosuspensions. Int J Pharm 392:64–71. doi:10.1016/j.ijpharm.2010.03.027
Zhou Y, Wu W-H, Zhao Q-B, Wang X-Y, Bao B (2015) Inhibition of HMG-CoA reductase by MFS, a purified extract from the fermentation of marine fungus FusaFusarium solani FG319, and optimization of MFS production using response surface methodology. Chin J Nat Med 13:346–354. doi:10.1016/s1875-5364(15)30025-x
Zhu Z (2013) Effects of amphiphilic diblock copolymer on drug nanoparticle formation and stability. Biomaterials 34:10238–10248. doi:10.1016/j.biomaterials.2013.09.015
Zhu J, Chew DAS, Lv S, Wu W (2013) Optimization method for building envelope design to minimize carbon emissions of building operational energy consumption using orthogonal experimental design (OED). Habitat Int 37:148–154. doi:10.1016/j.habitatint.2011.12.006
Acknowledgments
This work was supported by the National Natural Science Foundation of China (No: 81302711).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhou, Y., Du, J., Wang, L. et al. State of the art of nanocrystals technology for delivery of poorly soluble drugs. J Nanopart Res 18, 257 (2016). https://doi.org/10.1007/s11051-016-3575-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11051-016-3575-y