Abstract
Acrylamide (ACR) is an industrial chemical used to produce polyacrylamide, a synthetic polymer with a wide range of applications. Depending on the dosage, its presence in occupational and environmental sources poses potential health risks to humans and animals. ACR can be formed in starchy foods cooked at high temperatures. Its effects on human sperm are not well understood. Animal studies indicate that ACR induces toxicity in the male reproductive system through oxidative stress mechanisms. Exposure to ACR alters the normal structure of testicular tubules, leading to congestion, interstitial edema, degeneration of spermatogenic cells, formation of abnormal spermatid giant cells, and necrosis and apoptosis. It also disrupts the balance of important biomarkers such as malondialdehyde, nitric oxide, superoxide dismutase, catalase, and glutathione. ACR has a negative impact on mitochondrial function, antioxidant enzymes, ATP production, and sperm membrane integrity, resulting in decreased sperm quality. Furthermore, it interferes with the expression of steroidogenic genes associated with testosterone biosynthesis. This review explores the detrimental effects of ACR on sperm and testicular function and discusses the potential role of antioxidants in mitigating the adverse effects of ACR on male reproduction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acrylamide (ACR, CH2 = CH-CONH2), classified as a group 2 A human carcinogen, is extensively used in the production of paper, plastics, tobacco, and wastewater treatment, including sewage [1, 2]. The Swedish National Food Administration (SNFA) states that significant amounts of ACR are released when certain foods like cereal products and potatoes are cooked above 120 °C [3]. Human exposure to ACR can occur through skin absorption, inhalation, or ingestion [4]. Upon consumption, ACR is primarily absorbed in the gastrointestinal tract and distributed to peripheral tissues via the bloodstream [5]. Additionally, ACR can undergo conjugation with N-acetyl-S-(3-amino-3-oxopropyl)-cysteine by glutathione S-transferase (GST) [6], and the cytochrome P450 enzyme complex (CYP450) converts ACR to glycidamide (GA) [7]. ACR exposure has been associated with neurotoxicity, genotoxicity, carcinogenicity, hepatotoxicity, immunotoxicity, and reproductive toxicity [8,9,10,11,12,13,14].
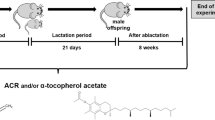
Neurotoxicity is the most prominent consequence of ACR exposure [15], characterized by symptoms such as skeletal muscle weakness, ataxia, and axon degeneration in both the central and peripheral nervous systems, even crossing the blood-brain barrier (BBB) [16, 17]. ACR can traverse the blood-placental barrier in the human placenta and the blood-breast milk barrier in nursing mothers [18]. It has been observed that ACR can breach the blood-testis barrier (BTB) within 1 h of oral administration in mice [19].
In rodents, a single dose of ACR ranging between 100 and 200 mg/kg is considered lethal, while repeated low-concentration exposures of 10 to 50 mg/kg can induce neuropathy [20]. ACR can induce liver and kidney toxicity through the PI3K/AKT/mTOR pathway and inflammatory factors like nuclear factor kappa B (NF-κB) and tumor necrosis factor-alpha (TNF-α) [21, 22]. ACR-induced hepatotoxicity may be indicated by increased levels of liver enzymes (AST, ALT, and ALK) [23]. In mouse bone marrow cells, ACR and its major metabolite, glycidamide, have been found to cause DNA damage, chromosomal aberrations, and micronuclei [24].
The metabolism of ACR by CYP450 E1 can generate reactive oxygen species (ROS) in reproductive organs, including the testis and ovary, leading to lipid peroxidation and cell death [20, 25,26,27,28]. However, research on the effects of ACR on the reproductive system has mainly concentrated on male subjects, resulting in a relative scarcity of data regarding its potential impacts on the female reproductive system [8]. Previous studies have indicated no significant increase in cancer mortality among industrial workers with prolonged exposure to high levels of ACR [29, 30], but a positive association has been observed between ACR exposure and reproductive cancers, such as endometrial and ovarian tumors, as well as estrogen receptor-positive breast cancer in postmenopausal women [31, 32]. Exposure to ACR has been linked to alterations in levels of various hormones involved in reproductive processes [33]. In one study conducted by Nagata and colleagues, which examined preschool-aged children exposed to ACR at an estimated intake level of 1 µg/kg/day, increased urinary levels of androstenediol, dehydroepiandrosterone (DHEA), testosterone (T), estrone (E1), and estradiol (E2) were observed. A positive correlation was found between urinary levels of T and androstenediol in boys, while in girls, no significant associations between ACR intake and hormone levels were found [34]. In another study, premenopausal Japanese women with the highest acrylamide intake showed significantly lower levels of total and free E2 (18.2% and 19.3% lower, respectively) and higher levels of follicle-stimulating hormone (FSH) (23.5% higher). However, there were no notable changes in plasma levels of dehydroepiandrosterone sulfate (DHEAS), luteinizing hormone (LH), prolactin, and sex hormone-binding globulin (SHBG) [35].
Interestingly, male animal studies have yielded complex and contradictory findings regarding the effects of ACR on reproductive hormones. For instance, one study demonstrated that a three-week administration of ACR (5 mg/kg) increased T levels in rats without affecting FSH or LH levels [36]. In contrast, another study found that ACR (10 mg/kg, administered for 20 days during pregnancy) decreased serum T, FSH, and LH levels in adult male rats [37]. Although the understanding of ACR’s impact on human spermatozoa is limited, the majority of animal studies consistently report detrimental effects of ACR on sperm parameters, including count, motility, morphology, and quality [36, 38,39,40,41,42,43,44,45]. This review primarily focuses on the effects of ACR on testicular and sperm function in animal models and explores the potential benefits of using antioxidants to mitigate ACR-induced damage.
Oxidative stress in human spermatozoa and testicles
Oxidative stress, triggered by an excess of ROS and reactive nitrogen species (RNS), significantly impairs the functionality of the male reproductive system, leading to a condition known as Male Oxidative Stress Infertility (MOSI) [46]. The dysfunction of male reproductive organs is closely associated with oxidative/nitrosative stress, as indicated by the presence of biochemical markers of damage [47, 48]. While a certain concentration of endogenous ROS is necessary for normal spermatozoa function during events like sperm-oocyte fusion, acrosome reaction, and capacitation, an excessive accumulation of ROS is a common pathological occurrence in the semen of infertile men [49]. Prolonged exposure to ROS in semen samples irreversibly damages various macromolecules, including polyunsaturated fatty acids in cell membranes, proteins, and nucleic acids, thereby impairing the functionality of germ cells, which are highly sensitive to elevated levels of free radicals [47, 50].
Several factors contribute to the high production of ROS. These include the development and proliferation of abnormal and immature spermatozoa [51], invasion of white blood cells [52], and defects in the scavenger/antioxidant system of the seminal fluid [53]. In the presence of triggers such as inflammation and infection, leukocytes in the seminal fluid can become activated and produce large amounts of ROS, often reaching concentrations up to 100 times higher than those found in sperm [54]. Activation of macrophages and polymorphonuclear neutrophils (PMNs) increases the production of ROS through a burst of respiratory activity and the generation of NADPH via the hexose monophosphate shunt [55]. In vitro sperm processing techniques, such as freeze/thaw procedures, excessive centrifugation, and low antioxidant activity in culture media, can also induce ROS formation in sperm samples [48]. Elevated levels of ROS, including hydroxyl radicals, superoxide radicals, nitric oxide, hydrogen peroxide, and peroxynitrite, adversely affect regular sperm production and quality by interacting with membrane proteins and lipids, as well as with the mitochondrial and nuclear genomes [56]. Testicular oxidative stress can impact sperm quality by causing peroxidative damage to their DNA [57]. Recent research on male infertility has focused on DNA damage, including DNA breaks, base mutations, DNA strand breaks, and chromatin cross-links, which are often observed in sperm from infertile males. These DNA abnormalities are attributed to increased levels of ROS in sperm, as intact DNA is crucial for successful fertilization [58, 59]. Sperm, like other aerobic cells rich in mitochondria, are susceptible to oxidative damage due to the presence of mitochondrial DNA (mtDNA). Some infertile men exhibit multiple losses of mtDNA, possibly due to free radical damage to spermatogonia [60].
ROS-induced DNA damage increases the likelihood of apoptosis, a form of programmed cell death, in germ cells [58]. Apoptosis can be triggered by internal and/or external stimuli without the presence of inflammation. It can be initiated by cytokine/stress-induced kinases, leading to the overexpression of E-selectin in sperm vascular endothelium, which recruits neutrophils to the testicular tissue and further increases ROS levels, resulting in peroxidative damage to the cell membrane and induction of apoptosis in germ cells [61]. Under pathological conditions such as cryptorchidism, toxin exposure, or testicular torsion, apoptosis in germ cells is significantly elevated, leading to disruption of sperm functionality [62]. Apoptosis is a normal process in spermatogenesis for the elimination of immature spermatozoa [63]. Germ cell death has a profound impact on the testicular epithelium [64], and during acute induction, Sertoli cells engulf a large number of apoptotic germ cells, which can overwhelm normal Sertoli cell processes [65]. This biological process triggers the synthesis of pro-inflammatory mediators, including interleukin-1β (IL-1β), interleukin-6 (IL-6), and other pro-inflammatory molecules, through the activation of the NF-κB pathway. In summary, excessive production of ROS and RNS in the male reproductive system leads to oxidative stress, which impairs sperm functionality, causes DNA damage, induces apoptosis in germ cells, and disrupts normal spermatogenesis.
ACR changes sperm function in animals through ROS
Mitochondria in spermatozoa play a crucial role in ATP production, which is essential for sperm motility and fertilization, and the regulation of mitochondrial ATP production occurs through oxidative phosphorylation. Elevated levels of reactive oxygen species (ROS) in the cell can lead to disruptions in mitochondrial function, including a decrease in mitochondrial membrane potential (ΔΨm) and activation of inner mitochondrial membrane (IMM) enzymes involved in apoptosis, such as Caspase-3 and Caspase-9 (Fig. 1) [66]. Exposure to ACR at different doses (0.5–2 mM) has been shown to result in a decrease in ΔΨm in human spermatozoa [67]. A reduction in sperm motility is associated with increased ROS levels, decreased ΔΨm, and the formation of electrophilic aldehyde lipids (EALs) [68]. These EALs can hinder sperm motility by interfering with the mitochondrial electron transport chain and binding to proteins like dynein and AKAP-3/4, which are involved in regulating sperm motility [68]. Under oxidative stress conditions, BH3 protein, located in the outer mitochondrial membrane (OMM), becomes activated, leading to increased OMM permeability [69]. This leads to electron loss and the generation of free radicals, such as superoxide anion radical (O2−.), through their binding to O2 [69].
Possible mechanisms of mitochondrial dysfunction in testicular tissues and spermatozoa related to ACR administration and the defense mechanism against oxygen free radicals. ACR exposure leads to mitochondrial dysfunction due to the alteration of mitochondrial permeability transition pore (mPTP) activity, loss of ΔΨm, and decrease in ATP content. In addition, the overproduction of ROS in mitochondria leads to the release of apoptotic factors. Moreover, oxidative stress can activate several signaling pathways, such as inflammation and autophagy, via the activation of NF-κB and blocking of PI3K/AKT/mTOR. Therefore, such events may lead to DNA damage and apoptosis in spermatozoa, spermatogonia, and Leydig cells. Any damage to Leydig cells leads to lower production of testosterone, which in turn alters sperm parameters. On the other hand, antioxidant sources can counteract the production of ROS, and therefore intracellular antioxidant defenses such as SOD, CAT, GPx, and GSH can readily convert free radicals into H2O and O2
ACR may also affect ΔΨm by disrupting the function of adenine nucleotide transporters located in the IMM, causing apoptotic substances to move from the membrane space into the cytosol [70]. Increased sensitivity of sperm to free radicals may be due to the unsaturated fatty acids that are abundant in the sperm membrane. Some types of ROS, such as H2O2, can enter sperm cells inhibiting the activity of the enzyme glucose-6-phosphate dehydrogenase (G6PD), which is involved in the control of glucose influx and the intracellular presence of NADPH. Therefore, inhibition of G6PD/NADPH metabolism results in decreased glutathione levels and accumulation of glutathione oxidase in sperm. It is considered that the overproduction of ROS leads to a decrease in both nonenzymatic and enzymatic antioxidants in Leydig cells, which in turn impairs spermatogenesis and decreases sperm count (Fig. 1) [71]. ACR administration decreases SOD and TAC as well as some parameters in human spermatozoa, such as progressive/total motility and viability, while it can increase MDA levels [72]. Incubation of spermatozoa with ACR also resulted in decreased activity of GST, an enzyme involved in mitigating oxidative stress, and a decline in mitochondrial membrane potential when cellular ROS levels are elevated.
According to a study conducted by Haleem and colleagues in 2022, exposure to ACR was found to result in a decrease in the activity of LDH-X in testicular tissue [73], while Rajeh and Khayyat in 2017 found that the administration of ACR (45 mg/kg) for five consecutive days did not lead to changes in serum lactate dehydrogenase (LDH) concentration [74]. LDH-X, also known as testis-specific LDH, is a unique isoform of the enzyme LDH primarily found in spermatogenic cells (pachytene spermatocytes and Sertoli cells) within the testicular tissue, and its activity is considered an indicator that could reflect overall tissue damage. LDH-X is involved in energy metabolism in the testes, particularly in the conversion of lactate to pyruvate, which generates NADH, a reducing equivalent that contributes to the production of ATP through oxidative phosphorylation in mitochondria. The ATP generated through LDH-X-mediated energy metabolism is crucial for various processes involved in spermatogenesis, including DNA replication, chromatin remodeling, and sperm motility. Sperm motility, in particular, requires a significant amount of ATP to power the flagellar movement necessary for sperm to reach the egg for fertilization [75]. It has also been suggested that the overproduction of ROS following ACR exposure could cause mitochondrial membrane fragmentation and subsequent alteration of membrane-bound LDH-X activity [73]. Therefore, reduced LDH-X can lead to a decrease in ATP production, resulting in diminished energy availability for sperm motility.
Several studies have shown that ACR can decrease progressive/total sperm motility, sperm abnormalities, sperm concentration, chromatin condensation, and sperm DNA integrity, and increase sperm protamine deficiency and sperm DNA damage [36, 38, 76,77,78,79,80] (Table 1). Chapman and Michael in 2003 reported that the effects of ACR on sperm chromatin condensation may be due to a reduction in serum T levels [81]. Also, DNA damage induction in germ cells and spermatozoa could be due to the activation of cytochrome P450 2E1 (CYP2E1) [82, 83]. CYP2E1 is involved in the conversion of ACR to the highly reactive metabolite glycidamide and in dominant lethality. Indeed, the function of CYP2E1 depends on its activation by O2, so the destruction of the oxygen-enriched P450 complex releases the O2−., resulting in DNA damage and cell death (Fig. 2) [84]. One study showed for the first time that the major site where sperm DNA damage occurs is the epididymis because CYP2E1 is expressed there [85]. Also, the liver, spleen, brain, spermatocytes, and the midpiece of mature spermatozoa are the other sites where CYP2E1 is expressed [85,86,87].
Schematic representation of acrylamide (ACR)-induced testicular damage. ACR could be involved in the activation of inflammation (by increasing TNF-α, IL-1, IL-1β, IL-6, COX-2, NF-κB, and p38α MAPK levels), oxidative stress (by increasing MDA, NO, LPO, 8-OHdG or decreasing CAT, GPx, SOD, GSH, and GSSG activities) autophagy (by upregulating Beclin-1, LC3A, and LC3B expression), apoptosis (by upregulating Bax, Caspase-3, Cytochrome-C [Cyt-C], p53, and ERK and downregulating Bcl-2, Nrf2, and PI3K/AKT/mTOR signaling expression), and DNA damage (by upregulating the expression of CYP2E1) in sperm and testicular cells such as germ cells and Leydig cells (res arrows), which in turn could lead to the formation of abnormal spermatozoa. However, antioxidant therapy could alleviate these side effects (green arrow) and play an effective role in maintaining low levels of oxidative stress, thereby enabling normal cell signaling cascades and spermatogenic functions and preventing ROS-induced cell damage
ACR exposure during the prepubertal period could also change sperm production and function. For instance, prepubertal exposure to ACR (from postnatal day 23 (PND) to PND60) decreased total sperm production in a dose-response manner, reduced mitochondrial activity, decreased mRNA expression of early growth factor 2 (EGR2), RHCG (a transcriptional marker for spermatocytes), and LRRC34 (a transcriptional marker for spermatids), and increased androgen receptor (AR) expression at the transcriptional level in rats [88]. EGR2 is responsible for the proliferation and maintenance of spermatogonia A and B, and its expression also decreased during the differentiation of spermatogonia into pre-leptotene spermatocytes [89, 90]. Therefore, it appears that ACR can have negative effects on spermatogonial proliferation, leading to a decrease in sperm production, whereas higher expression of AR may be an attempt to restore spermatogonial proliferation and a compensatory mechanism against downregulated EGR2 expression.
It has been documented that the level of carboxymethyl lysine increases as a form of advanced glycation following the incubation of sperm with ACR [72]. Advanced glycation refers to a process in which sugars react with proteins, lipids, or nucleic acids, resulting in the formation of advanced glycation end products (AGEs) [91]. These AGEs can accumulate in various tissues, including the reproductive system. In the case of sperm, the accumulation of AGEs, particularly in the acrosomal region of the sperm head, can induce oxidative stress and inflammation, leading to impaired sperm function and reduced sperm quality [91]. Furthermore, the disruption of the BTB by AGEs can further compromise sperm DNA integrity and contribute to DNA damage [91].
Therefore, the available studies provide substantial evidence that exposure to ACR has detrimental effects on sperm health and function by interfering with mitochondrial function, reducing ΔΨm, and activating CYP2E1. ACR also promotes the formation of AGEs in sperm, compromising DNA integrity. These findings highlight the adverse effects of ACR on sperm parameters such as progressive/total sperm motility and reduced sperm concentration, underscoring the importance of maintaining mitochondrial health and oxidative balance for optimal sperm function.
ACR through inflammation, apoptosis, and autophagy alters testicular structure and function
ACR administration could result in severe damage to testicular tissues, such as degeneration and necrosis of spermatogonia, including primary spermatocytes and spermatids, vacuolization of Leydig cells and primary spermatocytes, enlargement of interstitial areas (edema) via induction of inflammatory cell infiltration and fibrosis, pyknosis of Leydig cells, focal hemorrhage, formation of giant cells in the spermatids, and debris from spermatozoa in the lumen of testicular tubules (Table 2) (Fig. 2) [28, 40, 73, 98,99,100,101,102,103]. It also appears that a reduction in testicular weight and reproductive accessory organs such as the epididymis may have resulted from ACR-induced tissue damage [92, 104, 105]. On the other hand, connective tissue deformities, multinucleated giant cells, reduced mean Johnson’s score, reduced testicular tubule diameter, and atrophic tubules were observed in the testes of the male offspring of rats whose mothers received ACR during pregnancy (Table 2) [37, 106]. Multinucleated giant cells observed in the testis are atypically large cells that contain multiple nuclei within a single cell. These cells are a specific type of degenerating germ cell, thought to derive from secondary spermatocytes and spermatids [107]. After toxic exposures in animals, their presence is frequently observed within the lumen of seminiferous tubules, indicating an underlying inflammatory process [108]. Also, Johnsen’s score is a commonly utilized system for evaluating testicular damage. It provides a comprehensive grading system using scores ranging from 10 to 1, which correspond to the level of histological findings [109]. A decrease in the number of cells involved in spermatogenesis within the seminiferous tubules is associated with lower scores.
Research suggests that ACR administration increases the expression of genes and the level of factors involved in testicular inflammation, such as NF-κB/p65, TNF-α, p38α mitogen-activated protein kinase (p38α MAPK), prostaglandin-endoperoxide synthase 2 (COX-2), IL-6, IL-1, and IL-1β [39, 42, 43, 73, 110]. The transcription of pro-inflammatory mediators such as interleukins is regulated by NF-κB, while p38α MAPK could regulate the inflammatory response in cells. Inflammation can impair BTB function in animals [111]. For example, NF-κB/p65 activation had negative feedback on the expression of proteins involved in the tight junction of BTB [73]. In 2001, Wachtel et al. demonstrated that the activation of NF-κB/p65 and TNF-α receptors can suppress occludin expression in astrocytes [112]. Therefore, the activation of NF-κB and p38α MAPK by ACR could induce changes in the inflammatory response in testicular cells, probably resulting in BTB damage and cell death. In the rat testes, a number of studies found that an administration of ACR decreased GSH levels and the activity of antioxidant enzymes such as SOD, GPx, and CAT while increasing DNA damage and levels of apoptotic parameters such as Bax, cytochrome-C (Cyt-C), p53, and Caspase-3, and autophagic parameters such as Beclin-1, LC3A, and LC3B [28, 41, 42, 82, 96, 110, 113, 114]. Among all types of spermatogenic cells, spermatogonia and spermatocytes responded more positively to Bax when rats were treated with ACR [115]. Kucukler et al. (2020) demonstrated that ACR can inhibit PI3K/AKT/mTOR signaling pathways [110]. PI3K, a key signaling molecule, regulates numerous cellular processes, such as apoptosis and cell growth. Furthermore, PI3K is responsible for activating AKT, and the downstream mTOR pathway, which is positively regulated by AKT, controls essential processes, including cell growth and autophagy. In addition, Beclin-1 has been shown to be a scaffolding protein for the formation of the PI3K complex as an autophagic protein [116]. Upon oxidative damage, LC3B, a type of autophagosome, is activated [116]; hence, autophagic or apoptotic testicular death induced by ACR may be due to inhibition of PI3K/AKT/mTOR signaling pathways [110]. In mice, ACR was unable to alter AKT levels in both Leydig cells and testes, whereas ACR exposure activated phosphorylation levels of extracellular signal-regulated kinase 1/2 (ERK1/2) in TM3 Leydig cells and mouse testicular tissue [98]. ERK is a signaling pathway that plays a crucial role in various cellular processes, including apoptosis. In the testis, ERK signaling has been implicated in regulating apoptotic pathways by regulating pro-apoptotic proteins and downregulating anti-apoptotic proteins [117]. ERK signaling could also interact with the PI3K/AKT pathway, activating caspase cascades in testicular germ cells [117]. Studies suggest that ACR can induce cell apoptosis by triggering the Caspase-3 and ERK pathways [118]. Therefore, ACR exposure leads to oxidative stress, decreased antioxidant activity, increased apoptotic and autophagic parameters, inhibition of the PI3K/AKT/mTOR signaling pathways, and activation of the ERK signaling, suggesting mechanisms underlying ACR-induced testicular cell injury and death.
ACR changes hormone production and steroidogenesis in male animals
Testicular physiology is affected by several hormones, including T, LH, and FSH. However, the effects of ACR on the production of T, LH, and FSH are controversial (Tables 1 and 2, and 3) [92, 124]. In mouse Sertoli and Leydig cell lines (TM4 and TM3, respectively) treated with ACR or glycidamide, the activity of 3β-hydroxysteroid dehydrogenase (3β-HSD, in Leydig cells) and 17β-hydroxysteroid (17β-HSD, in Sertoli cells) decreased (Table 3) [125]. Of the two cells mentioned, Leydig cells were more sensitive to the treatments compared with Sertoli cells [125]. These results suggest that ACR or GA may affect T biosynthesis in Leydig cells by suppressing steroidogenic enzyme activities. Additionally, ACR can decrease T levels by inducing abnormalities in the cytoskeleton of Leydig cells, which is involved in cholesterol uptake [124, 126]. Yildizbayrak and Erkan showed that administration of ACR (2 mmol/L, for one day) resulted in damage to TM3 and decreased T levels, probably via downregulating steroidogenic acute regulatory protein (StAR) and luteinizing hormone/choriogonadotropin receptor (LHCGR) expression, and upregulating CYP11A1 expression (Table 3) [127]. LHCGR is a crucial protein expressed on Leydig cells that, when bound to LH, stimulates T production. StAR plays a critical role in transporting cholesterol from the outer to the inner mitochondrial membrane of Leydig cells, where cholesterol is converted into steroid hormones, initiating steroidogenesis [128]. Thus, reduced expression of LHCGR and StAR can impact T production and alter its synthesis [99]. Hence, the increased activity of CYP11A1, involved in converting cholesterol to pregnenolone [129], in response to ACR treatment, maybe a compensatory mechanism of Leydig cells to maintain androgen formation balance, including T. Furthermore, ACR can disrupt the integrity of the basement membrane of testicular tubules by downregulating occludin, a crucial protein involved in the formation and maintenance of tight junctions expressed in Sertoli cells, leading to damage to the BTB (Fig. 2) [73, 123, 130]. A positive correlation has been found between lower expression of junctional proteins such as occludin and lower serum T levels [73]. ACR can also lead to the death of Leydig cells through the induction of oxidative stress and apoptosis [37], leading to decreased T production.
It is demonstrated that ACR specifically affects T biosynthesis in Leydig cells by suppressing the activities of key proteins involved in steroidogenesis and disrupting the cytoskeleton responsible for cholesterol uptake. However, elevated serum T levels may be due to Leydig cell hyperplasia observed in studies where ACR upregulated the expression of Ki-67, a cell proliferation marker, in hyperplastic Leydig cells [36, 119]. In rats, one month of ACR administration decreased serum levels of FSH and T due to damage to spermatogenic cells and Leydig cells, while LH production increased, possibly because the number of Sertoli cells was unaffected [105]. Administration of ACR for 10 days (40 mg/kg) decreased FSH and increased LH levels [93], while its administration for 21 days (5 mg/kg) failed to alter the levels of LH and FSH in rats [36]. It seems the duration and dose of ACR treatment are indeed important factors that can influence the alternation of FSH and LH production. On the other hand, any disruption of hormone production of LH and FSH may be due to the effects of ACR on the pituitary gland (responsible for LH and FSH production). In this regard, a separate study conducted by Nadhim and AL-Derawi (2022) on rats demonstrated that the administration of ACR for a duration of six weeks (at a dose of 4 mg/kg) induced significant infiltration of inflammatory cells and degenerative changes in both the anterior and posterior regions of the pituitary gland [131]. Collectively, it is evident that ACR-induced testicular damage can occur through alterations in LH and FSH production. In Sertoli cells, the binding of FSH to its receptors (FSHR) expressed on these cells plays a crucial role in promoting spermatogenesis and T production. This binding activates adenylyl cyclase, leading to the formation of cyclic adenosine monophosphate (cAMP). Alongside T, cAMP is involved in regulating spermatogenesis. LH, on the other hand, binds to its receptors (LHR) located on Leydig cells, stimulating and regulating T synthesis. Therefore, any disruptions in T synthesis or spermatogenesis caused by ACR can have an impact on the normal histology of seminiferous tubules, potentially leading to structural changes.
Antioxidant therapy against ACR
The modern lifestyle is accompanied by an array of environmental pollutants and toxins, giving rise to concerns regarding their impact on human health. These hazardous substances have the ability to generate ROS, resulting in cellular damage to proteins, lipids, DNA, and overall cellular function. Consequently, the role of antioxidants as a potential defense mechanism against these harmful factors has garnered significant attention and research. Notably, antioxidants, including vitamins and various plant-derived compounds, play a crucial role in counteracting the detrimental effects of ROS by either neutralizing them or preventing their formation. Below, a compilation of studies demonstrating the ability of different types of antioxidants to counteract the deleterious effects of ACR is presented (Tables 1 and 2).
Capsaicin and thymoquinone treatment could have a protective effect against ACR-induced testicular injury and increase sperm motility and number [73, 95]. It has been shown that capsaicin plays a protective role against scrotal hyperthermia through its antiapoptotic and antioxidant properties [132]. Treatment with resveratrol, a phytoalexin found in a variety of plant species and used in traditional medicine [133], was able to attenuate DNA damage in both sperm and germ cells of mice treated with ACR over a long period of time [82]. Therefore, one of the mechanisms for resveratrol could be its inhibitory effect on CYP2E1 activity. One study showed that simultaneous supplementation of ACR-exposed rats with Portulaca oleracea seed extract was able to increase the expression of proliferating cell nuclear antigen (PCNA) in spermatogenic cells, decrease Caspase-3 expression in Leydig cells, and increase mRNA expression of two major genes involved in steroidogenesis, CYP11A1 and hydroxysteroid 17-beta dehydrogenase 3 (17β-HSD3), and increase testicular GSH and SOD [94]. Another study conducted by El-Beltagi et al. (2016) presented that oral administration of quercetin increased T levels and the activity of GSH and GST, whereas TNF-α levels decreased in testicular tissues of rats exposed to ACR [121].
In mice exposed to ACR for 35 days, treatment with vitamin E improved sperm chromatin quality [79]. Moreover, ACR exposure during pregnancy could lead to lifelong permanent damage, whereas daily intake of vitamin E could prevent testicular damage and hormonal changes in the offspring [37]. It was also demonstrated that ACR-induced damage to testicular tubules, characterized by shrinkage and atrophy, was mitigated when rats were treated with either vitamin E or 5-aminosalicylic acid [74]. Vitamin E, renowned for its antioxidative properties and capacity to scavenge free radicals, exhibits promising potential in ameliorating DNA integrity and sperm quality [134]. Furthermore, it has been observed to augment plasma antioxidant enzyme activity, elevate serum T levels, and enhance sperm motility and count in male rats [135]. Given its lipophilic nature, vitamin E readily accumulates within cell membranes, thereby effectively inhibiting lipid peroxidation and preserving membrane integrity. This protective mechanism may serve to shield cells from the injurious consequences of ACR exposure. Moreover, vitamin E has been postulated to enhance the body’s detoxification processes, encompassing the metabolism and elimination of ACR. Vitamin E holds promise in minimizing the adverse effects associated with their accumulation by facilitating the efficient clearance of ACR and its metabolites. Supplementation with garlic oil had a protective effect against ACR-induced testicular toxicity [102]. Garlic is a medicinal plant that has a wide range of biological activities due to its organosulfur compounds. The mechanism of action of garlic against reproductive toxicity induced by hazardous substances such as ACR may be due to its scavenging effect ROS, which increases GSH content in cells [136]. Cellular GSH depletion plays an important role in the genotoxicity of ACR [137]. Mechanistically, the initial phase of ACR biotransformation is due to the ability of ACR to form GSH-S conjugates by interacting with essential cellular nucleophiles that have an SH group and GSH [138].
Amino acids, such as L-cysteine can serve as an anti-oxidant and alleviate endocrine disrupting chemical-induced liver and reproductive cell injury [139]. The use of L-cysteine ameliorated testicular injury such as hyperplasia of Leydig cells induced by ACR in male albino rats by decreasing the production of NO and LPO via its activity against ROS and increasing the activity of antioxidant parameters including CAT, GSH, and SOD [120]. A treatment with L-cysteine could also decrease the number of multinucleated giant cells and protein expression of Bax and increase PCNA activity in a model of ACR-induced testicular toxicity [115]. An administration of N-acetylcysteine (derived from the amino acid L-cysteine, 10–40 mg/kg) was able to restore disorders of spermatogenesis by increasing the number of spermatogenic and Leydig cells and subsequently increasing serum levels of LH and testosterone in a dose-dependent manner [105]. Treatment with N-acetylcysteine was also able to suppress ACR-induced apoptosis in rat testes by reducing Fas mRNA expression (a marker of apoptosis) [97]. N-acetylcysteine possesses antioxidant properties, allowing it to counteract the harmful effects of free radicals and reduce oxidative stress in tissues. By mitigating oxidative stress, N-acetylcysteine has the potential to attenuate the inflammatory response and inhibit the excessive production of certain inflammatory molecules, including cytokines and chemokines. This ability to modulate inflammation may contribute to N-acetylcysteine’s protective effects against tissue injury induced by ACR.
Administration of selenium was able to increase the synthesis of T hormone in the ACR-treated rats via upregulation of the expression of CYP17A1, HSD17β1, and StAR [93]. Selenium is an essential trace mineral that acts as a cofactor for several antioxidant enzymes, including glutathione peroxidases, which help neutralize harmful free radicals and reduce oxidative stress in tissues [140]. Therefore, enhancing the antioxidant defense system may help protect the testes from oxidative damage induced by ACR and mitigate testicular injury.
Plant extracts have been found to be effective in alleviating some environmental toxicant-induced health effects. Treatment of ACR-exposed rats with propolis extract (a honey-related product) ameliorated the deleterious effects of ACR on some reproductive parameters, such as sperm and hormones (LH, FSH, and T) [92]. ACR toxicity in the testes decreased when animals (rats) received 5-aminosalicylic acid [77], while eugenol (the major compound of clove oil) treatment enhanced sperm quality parameters, elevated levels of amino acids in seminal plasma, improved testicular oxidative/nitrosative stress biomarkers, and altered AMPK/p-AKT/mTOR signaling pathway in the rat exposed to ACR [123]. Administration of icariin (a flavonoid from Herba Epimedii) restored the number of some spermatogonial cells such as spermatocytes, spermatids, as well as Leydig and Sertoli cells in the testes of rats exposed to ACR [104]. A three-week administration of crocin (as a component of saffron) had a protective effect against ACR-induced testicular damage [103]. Crocin treatment improved testicular histopathological parameters in rats, such as testicular epithelial height, mean diameter of testicular tubules, and Johnson’s score, and increased hormone levels (T, FSH, LH) and levels of CAT, GSH, and SOD [103]. A 3-month treatment with green tea (Camellia sinensis) improved testicular histopathology and increased serum T levels due to its antioxidant properties [122]. Another experimental study found that administration of earthworm extract reduced the expression of Ki-67 in Leydig cells and the expression of p53 in spermatogenic cells of rats treated with ACR [36]; down-regulation of these two parameters could explain how earthworm extract could restore T production and increase sperm count in the ACR-treated group [36]. Plant extracts offer a multifaceted approach to combating testicular injuries caused by toxic agents. Acrylamide is a toxic compound known to induce oxidative stress and inflammation in testicular tissue. However, plant extracts abundant in antioxidants, such as polyphenols and flavonoids, can effectively scavenge the free radicals generated by ACR. This scavenging action reduces oxidative stress and safeguards the testes from damage. These extracts possess anti-inflammatory properties that assist in mitigating the inflammatory response triggered by ACR exposure, while some plant extracts may exhibit detoxifying effects, aiding in the elimination of ACR from the body and diminishing its harmful impact on the testes. Overall, incorporating plant antioxidants provides a natural and potentially effective approach to mitigate the adverse effects of ACR on reproductive health.
Conclusion
Due to the growing consumption of harmful compounds in daily life, the incidence of infertility within human populations is increasing. ACR is one of these compounds which can lead to male infertility. ACR has been shown to increase serum T levels as a result of Leydig cell hyperplasia. In contrast, numerous studies have explained that T production decreases in ACR models, as the overproduction of ROS subsequently results in damage to Leydig cells Furthermore, ACR can induce cellular autophagy by inhibiting the PI3K/AKT/mTOR signaling pathway and triggering apoptotic factors through the disruption of mitochondrial function. This leads to morphological damage in testicular tissues, sperm dysfunction, and ultimately DNA damage and cell death. This review shows that different concentrations of ACR have adverse effects on testicular tubule architecture (induction of vacuolization and hemorrhage), sperm parameters (viability and motility), sperm head and tail integrity, production of hormones (LH, FSH, and T), mitochondrial membrane potential, and antioxidant levels (SOD, CAT, GPx, and GSH) through increasing oxidative stress and production of ROS, while the use of antioxidants could act against ACR and attenuate the above adverse effects of ACR.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- ACR:
-
Acrylamide
- GA:
-
Glycidamide
- TAS:
-
Total Antioxidant Status
- TOS:
-
Total Oxidant Status
- CAT:
-
Catalase
- MDA:
-
Malondialdehyde
- SOD:
-
Superoxide Dismutase
- GPx:
-
Glutathione Peroxidase
- GSH:
-
Glutathione
- GSTs:
-
Glutathione S-Transferases
- γ-GT:
-
γ-Glutamyl Transpeptidase
- GSSG:
-
Glutathione Disulfide
- EALs:
-
Electrophilic Aldehyde Lipids
- H2O2 :
-
Hydrogen Peroxide
- NO:
-
Nitric Oxide
- LPO:
-
Lipid Peroxidation
- MPO:
-
Myeloperoxidase
- OS:
-
Oxidative Stress
- ROS/RNS:
-
Reactive Oxygen and Nitrogen Species
- LDH-X:
-
Lactate Dehydrogenase Isoenzyme-X
- CYP450:
-
Cytochrome P450 Enzyme Complex
- StAR:
-
Steroidogenic Acute Regulatory Protein
- 3β-HSD:
-
3β-Hydroxysteroid Dehydrogenase
- PCNA:
-
Proliferating Cell Nuclear Antigen
- 17β-HSD:
-
17β-Hydroxysteroid Dehydrogenase
- CYP11A1:
-
Cytochrome P450 Family 11 Subfamily A Member 1
- NF-κB:
-
Nuclear Factor Kappa B
- TNF-α:
-
tumor necrosis factor-alpha
- PI3Ks:
-
Phosphoinositide 3-Kinases
- PKB, or AKT:
-
Protein Kinase B
- mTOR:
-
Mammalian Target of Rapamycin
- p38α MAPK:
-
p38α Mitogen-Activated Protein Kinase
- COX-2:
-
Prostaglandin-Endoperoxide Synthase 2
- IL-1β:
-
Interleukin 1 Beta
- LC3A:
-
Microtubule-Associated Protein 1 Light Chain 3 Alpha
- LC3B:
-
Microtubule-Associated Protein 1 Light Chain 3 Beta
- ERK1/2:
-
Extracellular Signal-Regulated Kinase 1/2
- NADPH:
-
Nicotinamide Adenine Dinucleotide Phosphate
- ATP:
-
Adenosine Triphosphate
- ΔΨm:
-
Mitochondrial Membrane Potential
- DHEA:
-
Dehydroepiandrosterone
- DHT:
-
Dihydrotestosterone
- T:
-
Testosterone
- E1:
-
Estrone
- E2:
-
Estradiol
- LH:
-
Luteinizing Hormone
- SHBG:
-
Sex hormone-binding globulin
- FSH:
-
Follicle-Stimulating Hormone
- PND:
-
Postnatal Day
- AGEs:
-
Advanced Glycation End Products
- BTB:
-
Blood-Testis Barrier
- IP:
-
Intraperitoneal Injection
References
Kito K et al (2020) Variations in the estimated intake of acrylamide from food in the Japanese population. Nutr J 19:1–9
Maan AA et al (2022) Acrylamide formation and different mitigation strategies during food processing–a review. Food Reviews Int 38(1):70–87
Arisseto AP et al (2007) Determination of acrylamide levels in selected foods in Brazil. Food Addit Contam 24(3):236–241
Virk-Baker MK et al (2014) Dietary acrylamide and human cancer: a systematic review of sliterature. Nutr Cancer 66(5):774–790
Fennell TR, Friedman MA (2005) Comparison of acrylamide metabolism in humans and rodents. In Chemistry and Safety of Acrylamide in food. Springer
Miller M, Carter D, Sipes I (1982) Pharmacokinetics of acrylamide in Fisher-334 rats. Toxicol Appl Pharmcol 63(1):36–44
Sumner SC et al (1999) Role of cytochrome P450 2E1 in the metabolism of acrylamide and acrylonitrile in mice. Chem Res Toxicol 12(11):1110–1116
Tyl RW, Friedman MA (2003) Effects of acrylamide on rodent reproductive performance. Reprod Toxicol 17(1):1–13
Wei Q et al (2014) Reproductive toxicity in acrylamide-treated female mice. Reprod Toxicol 46:121–128
Zamani E et al (2017) Acrylamide induces immunotoxicity through reactive oxygen species production and caspase-dependent apoptosis in mice splenocytes via the mitochondria-dependent signaling pathways. Biomed Pharmacother 94:523–530
Rice JM (2005) The carcinogenicity of acrylamide. Mutat Research/Genetic Toxicol Environ Mutagen 580(1–2):3–20
Ghanayem BI et al (2005) Absence of acrylamide-induced genotoxicity in CYP2E1-null mice: evidence consistent with a glycidamide-mediated effect. Mutat research/fundamental Mol Mech Mutagen 578(1–2):284–297
Zhang L et al. Acrylamide induced hepatotoxicity through oxidative stress: mechanisms and interventions. Antioxidants and Redox Signaling, 2022(ja).
Erkekoglu P, Baydar T (2014) Acrylamide neurotoxicity. Nutr Neurosci 17(2):49–57
Miller MS, Spencer PS (1985) The mechanisms of acrylamide axonopathy. Annu Rev Pharmacol Toxicol 25(1):643–666
Kopanska M et al (2018) Acrylamide toxicity and cholinergic nervous system. J Physiol Pharmacol 69(6):847–858
Zhao M, Zhang B, Deng L (2022) The mechanism of acrylamide-induced neurotoxicity: current status and future perspectives. Front Nutr, 9
Sörgel F et al (2002) Acrylamide: increased concentrations in homemade food and first evidence of its variable absorption from food, variable metabolism and placental and breast milk transfer in humans. Chemotherapy 48(6):267–274
Marlowe C et al (1986) The distribution of [14 C] acrylamide in male and pregnant swiss-Webster mice studied by whole-body autoradiography. Toxicol Appl Pharmcol 86(3):457–465
Rifai L, Saleh FA (2020) A review on acrylamide in food: occurrence, toxicity, and mitigation strategies. Int J Toxicol 39(2):93–102
Ozturk I et al (2023) Therapeutic role of melatonin on acrylamide-induced hepatotoxicity in pinealectomized rats: effects on oxidative stress, NF-κB signaling pathway, and hepatocellular proliferation. Food and Chemical Toxicology, p 113658
Kandemir FM et al (2020) Protective effects of morin against acrylamide-induced hepatotoxicity and nephrotoxicity: a multi-biomarker approach. Food Chem Toxicol 138:111190
Ansar S et al (2016) Hepatoprotective effect of Quercetin supplementation against Acrylamide-induced DNA damage in Wistar rats. BMC Complement Altern Med 16:1–5
Alzahrani HAS (2011) Protective effect of l-carnitine against acrylamide-induced DNA damage in somatic and germ cells of mice. Saudi J Biol Sci 18(1):29–36
Yousef M, El-Demerdash F (2006) Acrylamide-induced oxidative stress and biochemical perturbations in rats. Toxicology 219(1–3):133–141
Zhang L et al (2017) Protective property of mulberry digest against oxidative stress–A potential approach to ameliorate dietary acrylamide-induced cytotoxicity. Food Chem 230:306–315
Aldawood N et al (2020) Acrylamide impairs ovarian function by promoting apoptosis and affecting reproductive hormone release, steroidogenesis and autophagy-related genes: an in vivo study. Ecotoxicol Environ Saf 197:110595
Üremiş MM et al (2024) Protective role of vitamin E against acrylamide-induced testicular toxicity from pregnancy to adulthood: insights into oxidative stress and aromatase regulation. Naunyn-Schmiedeberg’s Archives of Pharmacology, 397(2):829–841.
Sobel W et al (1986) Acrylamide cohort mortality study. Occup Environ Med 43(11):785–788
Marsh GM et al (2013) Long-term health experience of jet engine manufacturing workers: VI: incidence of malignant central nervous system neoplasms in relation to estimated workplace exposures. J Occup Environ Med 55(6):654–675
Thonning Olesen P et al (2008) Acrylamide exposure and incidence of breast cancer among postmenopausal women in the Danish Diet, Cancer and Health Study. Int J Cancer 122(9):2094–2100
Hogervorst JG et al (2007) A prospective study of dietary acrylamide intake and the risk of endometrial, ovarian, and breast cancer. Cancer Epidemiol Biomarkers Prev 16(11):2304–2313
Exon J (2006) A review of the toxicology of acrylamide. J Toxicol Environ Health Part B 9(5):397–412
Nagata C et al (2018) Associations of acrylamide intake with urinary sex hormone levels among preschool-age Japanese children. Am J Epidemiol 187(1):75–81
Nagata C et al (2015) Associations of acrylamide intake with circulating levels of sex hormones and prolactin in premenopausal Japanese women. Cancer Epidemiol Biomarkers Prev 24(1):249–254
Ahmed MM et al (2022) Reproductive injury in male rats from acrylamide toxicity and potential protection by earthworm methanolic extract. Animals 12(13):1723
Erdemli Z et al (2019) The effects of acrylamide and Vitamin E administration during pregnancy on adult rats testis. Andrologia 51(7):e13292
Kermani-Alghoraishi M et al (2010) The effects of acrylamide on sperm parameters and membrane integrity of epididymal spermatozoa in mice. Eur J Obstet Gynecol Reproductive Biology 153(1):52–55
Soliman MM et al (2023) Taify Pomegranate Juice Extract Abrogates Testicular Dysfunction Induced by Acrylamide: Role of Inflammatory, Antioxidants, and Oxidative Stress Biomarkers Andrologia, 2023
Bhuiyan MEJ et al (2023) Protective roles of vitamin C and 5-aminosalicylic acid on reproduction in acrylamide intoxicated male mice. Saudi J Biol Sci 30(8):103738
Gao Y et al (2023) Acrylamide-induced meiotic arrest of spermatocytes in adolescent mice by triggering excessive DNA strand breaks: potential therapeutic effects of resveratrol. Human & Experimental Toxicology, 42:09603271231188293
Sengul E et al (2023) Effects of naringin on oxidative stress, inflammation, some reproductive parameters, and apoptosis in acrylamide-induced testis toxicity in rat. Environ Toxicol 38(4):798–808
Mokhlis HA et al (2023) Hydrogen sulfide alleviates acrylamide-induced testicular toxicity in male rats. Toxicol Environ Health Sci 15(1):41–51
Çebi A (2024) Acrylamide intake, its effects on tissues and cancer, in Acrylamide in food. Elsevier, pp 65–93
Mostafa-Hedeab G et al (2023) Green synthesized zinc oxide nanoparticles using moringa olifera ethanolic extract lessens acrylamide-induced testicular damage, apoptosis, and steroidogenesis-related gene dysregulation in adult rats. Antioxidants 12(2):361
Arafa M et al (2020) Efficacy of antioxidant supplementation on conventional and advanced sperm function tests in patients with idiopathic male infertility. Antioxidants 9(3):219
Agarwal A, Prabakaran SA, Said TM (2005) Prevention of oxidative stress injury to sperm. J Androl 26(6):654–660
Sikka SC (2001) Relative impact of oxidative stress on male reproductive function. Curr Med Chem 8(7):851–862
Fraczek M, Kurpisz M (2007) Inflammatory mediators exert toxic effects of oxidative stress on human spermatozoa. J Androl 28(2):325–333
Chianese R, Pierantoni R (2021) Mitochondrial reactive oxygen species (ROS) production alters sperm quality. Antioxidants 10(1):92
Gil-Guzman E et al (2001) Differential production of reactive oxygen species by subsets of human spermatozoa at different stages of maturation. Hum Reprod 16(9):1922–1930
Ollero M et al (2001) Characterization of subsets of human spermatozoa at different stages of maturation: implications in the diagnosis and treatment of male infertility. Hum Reprod 16(9):1912–1921
Sharma RK et al (2001) Relationship between seminal white blood cell counts and oxidative stress in men treated at an infertility clinic. J Androl 22(4):575–583
Pasqualotto FF et al (2000) Relationship between oxidative stress, semen characteristics, and clinical diagnosis in men undergoing infertility investigation. Fertil Steril 73(3):459–464
Blake D, Allen R, Lunec J (1987) Free radicals in biological systems—a review orientated to inflammatory processes. Br Med Bull 43(2):371–385
Yenİ D et al (2010) Seasonal variation of oxidative stress parameters in ram seminal plasma. J Anim Veterinary Adv 9(1):49–54
Agarwal A, Said TM (2003) Role of sperm chromatin abnormalities and DNA damage in male infertility. Hum Reprod Update 9(4):331–345
Sakkas D et al (2002) Nature of DNA damage in ejaculated human spermatozoa and the possible involvement of apoptosis. Biol Reprod 66(4):1061–1067
Duran E et al (2002) Sperm DNA quality predicts intrauterine insemination outcome: a prospective cohort study. Hum Reprod 17(12):3122–3128
Kao S-H, Chao H-T, Wei Y-H (1998) Multiple deletions of mitochondrial DNA are associated with the decline of motility and fertility of human spermatozoa. Mol Hum Reprod 4(7):657–666
Lysiak JJ et al (2001) Essential role of neutrophils in germ cell-specific apoptosis following ischemia/reperfusion injury of the mouse testis. Biol Reprod 65(3):718–725
Brinkworth M et al (1995) Identification of male germ cells undergoing apoptosis in adult rats. Reproduction 105(1):25–33
Matsui Y (1998) Regulation of germ cell death in mammalian gonads. Apmis 106(1–6):142–148
Lysiak JJ et al (2005) Activation of the nuclear factor kappa B pathway following ischemia-reperfusion of the murine testis. J Androl 26(1):129–135
Cudicini C et al (1997) Human leydig cells and sertoli cells are producers of interleukins-1 and-6. J Clin Endocrinol Metabolism 82(5):1426–1433
Chai RR et al (2017) Prohibitin involvement in the generation of mitochondrial superoxide at complex I in human sperm. J Cell Mol Med 21(1):121–129
Omidi Z, Piravar Z, Ramezani M (2020) The effect of acrylamide on mitochondrial membrane potential and glutathione extraction in human spermatozoa: a laboratory study. Int J Reproductive Biomed 18(10):855
Juárez-Rojas AL et al (2015) Intrinsic and extrinsic apoptotic pathways are involved in rat testis by cold water immersion-induced acute and chronic stress. Syst Biology Reproductive Med 61(4):211–221
Nichi M et al (2017) Evaluation of epididymis storage temperature and cryopreservation conditions for improved mitochondrial membrane potential, membrane integrity, sperm motility and in vitro fertilization in bovine epididymal sperm. Reprod Domest Anim 52(2):257–263
Barbonetti A et al (2016) In vitro exposure of human spermatozoa to bisphenol A induces pro-oxidative/apoptotic mitochondrial dysfunction. Reprod Toxicol 66:61–67
Cao L, Leers-Sucheta S, Azhar S (2004) Aging alters the functional expression of enzymatic and non-enzymatic anti-oxidant defense systems in testicular rat leydig cells. J Steroid Biochem Mol Biol 88(1):61–67
Kashani MH, Ramezani M, Piravar Z (2021) The effect of acrylamide on sperm oxidative stress, total antioxidant levels, tyrosine phosphorylation, and carboxymethyl-lysine expression: a laboratory study. Int J Reproductive Biomed 19(7):625
Abd Al Haleem EN, Hasan WYS, Arafa HMM (2022) Therapeutic effects of thymoquinone or capsaicin on acrylamide-induced reproductive toxicity in rats mediated by their effect on oxidative stress, inflammation, and tight junction integrity. Drug Chem Toxicol 45(5):2328–2340
Rajeh NA, Khayyat D (2017) Effect of the combined administration of vitamin-E and 5-aminosalicylic acid on acrylamide-induced testicular toxicity. J Taibah Univ Med Sci 12(5):445–454
Piomboni P et al (2012) The role of mitochondria in energy production for human sperm motility. Int J Androl 35(2):109–124
Pourentezari M et al (2014) Effects of acrylamide on sperm parameters, chromatin quality, and the level of blood testosterone in mice. Iran J Reproductive Med 12(5):335
Rajeh N, Ali H, ElAssouli S (2014) Protective effects of 5-aminosalicylic acid on acrylamide toxicity in the testis and blood leukocytes of the rat. Kuwait Med J 46(1):32–43
Tukey H Effect of Acrylamide Ingestion on Reproductive Organs of Adult Male Wistar Rats
Anvari M et al (2020) Effects of acrylamide in the presence of vitamin E on sperm parameters, chromatin quality, and testosterone levels in mice. Clin Experimental Reproductive Med 47(2):101
Khalili MA et al (2014) Comparing the roles of sperm chromatin integrity and apoptosis in intrauterine insemination outcomes of couples with mild male and female factor infertility. J Reprod Infertility 15(1):35–40
Chapman JC, Michael SD (2003) Proposed mechanism for sperm chromatin condensation/decondensation in the male rat. Reproductive Biology Endocrinol 1(1):1–7
Katen AL et al (2016) Chronic acrylamide exposure in male mice induces DNA damage to spermatozoa; potential for amelioration by resveratrol. Reprod Toxicol 63:1–12
Rajeh N, Ali H, ElAssouli S (2014) Protective effects of 5-aminosalicylic acid on acrylamide toxicity in the testis and blood leukocytes of the rat. KMJ-Kuwait Med J 46(1):32–43
Cederbaum AI (2008) CYP2E1–Biochemical and toxicological aspects and role in Alcohol-Induced Liver Injury. Adv Bioactivation Res, p. 1–36
Katen AL et al (2017) Epididymal CYP2E1 plays a critical role in acrylamide-induced DNA damage in spermatozoa and paternally mediated embryonic resorptions. Biol Reprod 96(4):921–935
Ghanayem BI et al (2005) Comparison of germ cell mutagenicity in male CYP2E1-null and wild-type mice treated with acrylamide: evidence supporting a glycidamide-mediated effect. Biol Reprod 72(1):157–163
Nixon BJ et al (2014) Mouse spermatocytes express CYP2E1 and respond to acrylamide exposure. PLoS ONE 9(5):e94904
Ivanski F et al (2020) Prepubertal acrylamide exposure causes dose-response decreases in spermatic production and functionality with modulation of genes involved in the spermatogenesis in rats. Toxicology 436:152428
Baksi A et al (2018) Correlation between the aberrant human testicular germ-cell gene expression and disruption of spermatogenesis leading to male infertility bioRxiv, p. 394049
Guo R et al (2004) Stage-specific and tissue‐specific expression characteristics of differentially expressed genes during mouse spermatogenesis. Mol Reprod Development: Incorporating Gamete Res 67(3):264–272
Omolaoye TS, du SS, Plessis (2020) Male infertility: a proximate look at the advanced glycation end products. Reprod Toxicol 93:169–177
Ghazi A, Ulaiwi HK, Jary S (2013) The role of local propolis extract against harmful effects of acrylamide on some male reproductive parameters in rats. Al-Qadisiyah J Veterinary Med Sci, 12(1)
Yildirim S et al (2022) Effects of Selenium on Some Reproductive Parameters in Acrylamide-Induced Testis Toxicity in Rats
Farag OM et al (2021) Portulaca oleracea seeds’ extract alleviates acrylamide-induced testicular dysfunction by promoting oxidative status and steroidogenic pathway in rats. BMC Complement Med Ther 21:1–15
Hasan W, Arafa H (2020) Effects of thymoquinone or capsaicin against acrylamide-induced testicular failure in rats: impact oxidative stress, NF-Κb/P65, and occludin. Authorea Preprints
Abd-Elsalam RM et al (2021) Eruca sativa seed extract modulates oxidative stress and apoptosis and up-regulates the expression of Bcl-2 and Bax genes in acrylamide-induced testicular dysfunction in rats. Environ Sci Pollut Res 28(38):53249–53266
Shahrzad E et al (2021) Effects of N-Acetylcysteine on FAS gene expression level in testicular tissue of acrylamide-treated adult rats. J Adv Biomedical Sci 11(2):3848–3856
Zhang J et al (2023) Exposure to acrylamide inhibits testosterone production in mice testes and leydig cells by activating ERK1/2 phosphorylation. Food Chem Toxicol 172:113576
Yildirim S et al (2024) Selenium reduces acrylamide-induced testicular toxicity in rats by regulating HSD17B1, StAR, and CYP17A1 expression, oxidative stress, inflammation, apoptosis, autophagy, and DNA damage. Environmental Toxicology
Yadegari M et al (2024) Effect of vitamin C on histomorphometric changes of testis, epididymis, prostate, and seminal vesicle induced by acrylamide in rat. Naunyn Schmiedebergs Arch Pharmacol 397(1):549–557
Wang J et al (2023) Research Progress of Programmed Cell Death Induced by Acrylamide Journal of Food Quality, 2023
Fiedan I, Ahmed E, Omar H (2015) Acrylamide induced testicular toxicity in rats: protective effect of garlic oil. Biomarkers 1(1):5
Gül M et al (2021) Protective effects of crocin on acrylamide-induced testis damage. Andrologia 53(9):e14176
Doctor Arastoye Marandi M et al (2020) Effects of icariin on histomorphometric changes of testis and prostate induced by acrylamide in mice. Int J Med Lab 7(3):197–211
Shahrzad E et al (2020) Protective effect of N-acetylcysteine on changes in serum levels of pituitary–gonadal axis hormones and testicular tissue in acrylamide-treated adult rats. Adv Hum Biology 10(1):16–21
Şen E, Tunali Y, Erkan M (2015) Testicular development of male mice offsprings exposed to acrylamide and alcohol during the gestation and lactation period. Human & Experimental Toxicology, 34(4):401–414.
Luo L et al (2013) Multinucleated cells are involved in normal development and apoptosis in mouse testes. Mol Med Rep 8(3):865–870
Figueiredo A et al (2021) Activation of C–C motif chemokine receptor 2 modulates testicular macrophages number, steroidogenesis, and spermatogenesis progression. Cell Tissue Res 386:173–190
Dolatkhah MA et al (2020) Fumaria parviflora regulates oxidative stress and apoptosis gene expression in the rat model of varicocele induction. Andrologia 52(11):e13826
Kucukler S et al (2020) Morin attenuates acrylamide-induced testicular toxicity in rats by regulating the NF-κB, Bax/Bcl-2 and PI3K/Akt/mTOR signaling pathways. Life Sci 261:118301
Pérez CV et al (2014) IL17A impairs blood–testis barrier integrity and induces testicular inflammation. Cell Tissue Res 358:885–898
Wachtel M et al (2001) Down-regulation of occludin expression in astrocytes by tumour necrosis factor (TNF) is mediated via TNF type‐1 receptor and nuclear factor‐κB activation. J Neurochem 78(1):155–162
Alturki HA, Elsawy HA, Famurewa AC (2022) Silymarin abrogates acrylamide-induced oxidative stress‐mediated testicular toxicity via modulation of antioxidant mechanism, DNA damage, endocrine deficit and sperm quality in rats. Andrologia 54(9):e14491
Camacho L et al (2012) Effects of acrylamide exposure on serum hormones, gene expression, cell proliferation, and histopathology in male reproductive tissues of Fischer 344 rats. Toxicol Lett 211(2):135–143
Kaçar S et al (2018) L-cysteine partially protects against acrylamide-induced testicular toxicity. Balkan Med J 35(4):311–319
Xu H-D, Qin Z-H (2019) Beclin 1, Bcl-2 and autophagy Autophagy: Biology and Diseases: Basic Science, pp. 109–126
Cagnol S, Chambard JC (2010) ERK and cell death: mechanisms of ERK-induced cell death–apoptosis, autophagy and senescence. FEBS J 277(1):2–21
Sumizawa T, Igisu H (2007) Apoptosis induced by acrylamide in SH-SY5Y cells. Arch Toxicol 81:279–282
Wang H et al (2010) Reproductive toxicity of acrylamide-treated male rats. Reprod Toxicol 29(2):225–230
Omar HE-DM et al (2015) L-cysteine ameliorated testicular toxicity induced by acrylamide in rats. Eur J Biol Res 5(2):1–8
El-Beltagi HS, Ahmed MM (2016) Assessment the protective role of quercetin on acrylamide‐induced oxidative stress in rats. J Food Biochem 40(6):715–723
Yassa HA et al (2014) Camellia sinensis (green tea) extract attenuate acrylamide induced testicular damage in albino rats. Environ Toxicol 29(10):1155–1161
Saleh DO et al (2024) Eugenol alleviates acrylamide-induced rat testicular toxicity by modulating AMPK/p-AKT/mTOR signaling pathway and blood–testis barrier remodeling Scientific Reports, 14(1):1910
Zirkin BR, Papadopoulos V (2018) Leydig cells: formation, function, and regulation. Biol Reprod 99(1):101–111
Aydin Y (2018) Acrylamide and its metabolite glycidamide can affect antioxidant defenses and steroidogenesis in Leydig and sertoli cells. Toxicol Environ Chem 100(2):247–257
Rogers SL, Gelfand VI (2000) Membrane trafficking, organelle transport, and the cytoskeleton. Curr Opin Cell Biol 12(1):57–62
Yildizbayrak N, Erkan M (2018) Acrylamide disrupts the steroidogenic pathway in Leydig cells: possible mechanism of action. Toxicol Environ Chem 100(2):235–246
Shoorei H et al (2023) Different types of bisphenols alter ovarian steroidogenesis: special attention to BPA. Heliyon 9(6):e16848
Hales DB (2002) Testicular macrophage modulation of Leydig cell steroidogenesis. J Reprod Immunol 57(1–2):3–18
Morrow CM et al (2010) Claudin and occludin expression and function in the seminiferous epithelium. Philosophical Trans Royal Soc B: Biol Sci 365(1546):1679–1696
Nadhim AA, Al-Derawi KH (2022) Histological, biochemical and chromosomal aberrations of pituitary gland induced by acrylamide in male rats. Iran J Ichthyol 9:412–423
Park S et al (2017) Capsaicin attenuates spermatogenic cell death induced by scrotal hyperthermia through its antioxidative and anti-apoptotic activities. Andrologia 49(5):e12656
Zhang L-X et al (2021) Resveratrol (RV): a pharmacological review and call for further research. Biomedicine & pharmacotherapy. 143:112164
Gual-Frau J et al (2015) Oral antioxidant treatment partly improves integrity of human sperm DNA in infertile grade I varicocele patients. Hum Fertility 18(3):225–229
Sönmez M, Yüce A, Türk G (2007) The protective effects of melatonin and vitamin E on antioxidant enzyme activities and epididymal sperm characteristics of homocysteine treated male rats. Reprod Toxicol 23(2):226–231
Musavi H et al (2018) Effect of garlic (Allium sativum) on male fertility: a systematic review. J Herbmed Pharmacol 7(4):306–312
Lamy E et al (2008) Ethanol enhanced the genotoxicity of acrylamide in human, metabolically competent HepG2 cells by CYP2E1 induction and glutathione depletion. Int J Hyg Environ Health 211(1–2):74–81
Lebda M, Gad S, Gaafar H (2014) Effects of lipoic acid on acrylamide induced testicular damage. Materia socio-medica 26(3):208
Chen H et al (2019) A review of toxicity induced by persistent organic pollutants (POPs) and endocrine-disrupting chemicals (EDCs) in the nematode Caenorhabditis elegans. J Environ Manage 237:519–525
Ahsan U et al (2014) Role of selenium in male reproduction—A review. Anim Reprod Sci 146(1–2):55–62
Acknowledgements
We appreciate everybody who helped us to write this paper. We also appreciate Dr. Seyedeh Fahimeh Talebi for drawing figures with Adobe Illustrator software.
Funding
This study received no funding.
Author information
Authors and Affiliations
Contributions
Hamed Shoorei and Ramji Kumar Bhandari: Conceptualization, writing – review & editing, Data curation, Investigation. Mohammad Seify and Neda Abedpour: Supervision. Yeganeh Koohestanidehaghi, Vajihe Hazari, and Mehrdad Mehrara: Conceptualization. Seyedeh Fahimeh Talebi: Visualization.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Seify, M., Abedpour, N., Talebi, S.F. et al. Impacts of Acrylamide on testis and spermatozoa. Mol Biol Rep 51, 739 (2024). https://doi.org/10.1007/s11033-024-09677-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11033-024-09677-1