Abstract
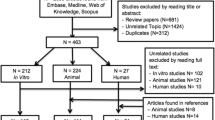
Osteoarthritis (OA) involves gradual destruction of articular cartilagemanifested by pain, stiffness of joints, and impaired movement especially in knees and hips. Non-vascularity of this tissue hinders its self-regenerative capacity and thus, the application of reparative or restorative modalities becomes imperative in OA treatment. In recent years, stem cell-based therapies have been explored as potential modalities for addressing OA complications. While mesenchymal stem cells (MSCs) hold immense promise, the recapitulation of native articular cartilage usingMSCs remains elusive. In this review, we have highlighted the chondrogenic potential of MSCs, factors guiding in vitro chondrogenic differentiation, biomaterials available for cartilage repair, their current market status, and the outcomes of major clinical trials. Our search on ClinicalTrials.gov using terms “stem cell” and “osteoarthritis” yielded 83 results. An analysis of the 29 trials that have been completed revealed differences in source of MSCs (bone marrow, adipose tissue, umbilical cord etc.), cell type (autologous or allogenic), and dose administered. Moreover, only 02 out of 29 studies have reported the use of matrix for cartilage repair. From future perspective, aconsensus on choice of cells, differentiation inducers, biomaterials, and clinical settings might pave a way for concocting robust strategies to improve the clinical applicability of biomimetic neocartilage constructs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis is a chronic, musculoskeletal degenerative disease which is mainly characterized by progressive degeneration of articular cartilage, bone sclerosis, formation of osteophyte and synoviopathy [1]. OA mainly affects elder people and it is the main cause of their physical disability. According to WHO, in population above 60 years of age, its prevalence is found to be higher in women (18%) than men (9.6%). The factors such as socioeconomic status, menopause, greater BMI, sedentary lifestyle, use of oral contraceptives and postmenopausal hormone-replacement therapy are positively associated with this [2]. Further, increase in average life span along with obesity has been associated with increasing cases of OA. According to the United Nations estimates, by 2050 world’s 20% population will be constituted by people above 60 years of age. This means throughout the world 130 million people will be affected by OA, by 2050 and out of these 40 million will be severely disabled by the disease [3]. Furthermore, in India, 15 million adults annually get affected by OA with a prevalence of 22–39% [4, 5]. Approximately 45% women with age of 65 years or more have been reported to show symptoms of OA which include pain, swelling, stiffness of joints, and impaired movement [4, 6]. Moreover, it has been found that approximately 80% of patients suffering from knee pain are affected with OA, out of which nearly 20% patients showed incapability in daily activities and around 11% need special care. Also, in 1990, it was estimated to be the 10th leading cause of nonfatal burden affecting socioeconomic health of the country [7].
Articular cartilage is a viscoelastic connective tissue which covers the ends of bone in the synovial joints and provides shock absorption and lubrication for easy movement. It is 2–4 mm thick and made up of 10% chondrocytes, 10–25% extracellular matrix (ECM) and 65–80% water. Chondrocytes are very important as they secrete and maintain the ECM of cartilage. This ECM is made up of mainly collagen type II, proteoglycans and glycosaminoglycans (GAGs) [8]. These chondrocytes are sparsely arranged in the tissue, have very limited regenerative potential and their degeneration is hallmark of OA [9]. Further, its avascular nature, absence of nerve supply and lymphatic system leads to extreme slow or no healing at all, predisposing us to progressive degeneration of articular cartilage [10,11,12]. The etiological factors which affect gradual loss of articular cartilage include normal wear and tear, aging, obesity, gender, genetic predisposition, bone density, muscle weakness, poor diet, joint laxity, and traumatic injury [2]. Besides this, other factorsthat contribute to pathology of OA include increase in level of accumulation of advanced glycation end products (AGEs), senescence related secretory phenotype and oxidative stress [13]. The pathology of disease affects all the components of joints including synovial membrane, subchondral bone and synovium membrane covering the joints. One of the main mechanisms in pathophysiology of OA is activation of chondrocytes by spreading of inflammation [14]. In such conditions, chondrocytes are not able to maintain a balance between their catabolic and anabolic activities which leads to degeneration of cartilage. The mechanism of cartilage degeneration iscompletely not knownbut it is postulatedthat increase in load on articular cartilage may initiate remodeling process which inhibits the restoration of normal cartilage. The cytokines that stimulate chondrocytes to degrade their matrix and aid apoptosis are mainly interleukin-1 (IL-1), interleukin-6 (IL-6), tumor necrosis factor-α (TNF-α), prostaglandins, reactive oxygen species (ROS) and nitric oxide (NO) [8].
OA can affect almost all joints, but its major targets are weight bearing knee and hip joints. These cartilage defects lead to pain and swelling in the area, which is accompanied by restriction in movement of joints. Besides physical health, it also affects mental health which altogether affects the quality of life. Further, OA has been reported to be a risk factor for development of heart diseases including myocardial infarction and coronary artery disease (CAD) [15].
At present no drugs are available to treat OA. Conventional treatments which are available focusesmainly on pain management and cannot treat or reverse OA. These include physiotherapy, exercise, and use of analgesics. Along with painkillers, intra-articular injections of corticosteroids and hyaluronic acid (HA) are also given, which can alleviate pain andhelp in restoring normal lubrication of the joints, respectively. However, none of these methods can lead to structural improvement of the damaged tissue. For structural improvement of the damaged tissue surgical techniquesincluding palliative, reparative and restorative are used depending on the severity of lesion. These surgical interventions differ on the basis of their capacities in healing the extent of defect [16].
Palliative techniques such as debridement and lavage are used for the treatment of smaller lesions manifested with minimal symptoms whereas reparative techniques for bone marrow stimulation like microfracture, subchondral drilling, and abrasion arthroplasty are used for the healing of full thickness defects. However, the efficiency of reparative procedures is very short termed and found to be effective in younger patients ranging 13–45 years in age only [17,18,19,20]. Besides, the restorative strategies such as osteochondral allograft or autograft transplantation (mosaicplasty), autologous chondrocyte implantation (ACI) and matrix-assisted autologous chondrocyte implantation (MACI) are the most advanced treatment modalities for long-term reestablishment of native articular surface. ACI involves isolation, expansion and transplantation of autologous chondrocytes surgically [19, 21, 22] whereas MACI involves use of a matrix for controlled and uniform delivery of chondrocytes [23]. However, the shortcomings of current therapies including donor-site morbidity, risk of disease transmission by allogenic grafts, high cost, complications related to harvesting of chondrocytes and their tendency to de-differentiate in vitro, compelled to search for alternative treatment options [24]. In last few decades, regenerative medicine has emerged as promising therapy which holds potential to heal or replace tissues or organs to restore their normal functioning. This field utilizes the application of tissue engineering, de novo generated cells and various other combinations for treatment of various degenerative diseases including cartilage defects. A better cognizance of various materials, cells and other factors involved in cartilage differentiation and remodeling may lead to the development of robust strategies to circumvent the challenges involved in recapitulating the native cartilage. In same line, this review focuses on potential of stem cell and matrix-based strategies in repairing of the defective cartilage, along with their outcomes in animal models and clinical settings, and further the underlying challenges in current therapies.
Stem cells in chondrogenic repair and restoration
Stem cell-based therapies have emerged as a promising tool in the field of regenerative medicines owing to their excellent regenerative potential. The three main categories of stem cells explored for developing cell-based therapies are MSCs, embryonic stem cells (ESCs), and induced-pluripotent stem cells (iPSCs). ESCs and iPSCs are pluripotent in nature and can differentiate into all types of cells. Whereas, MSCs are multipotent cells and can differentiate only into the cells of mesengenic lineage. Stem cells have been extensively explored in the regeneration of articular cartilage as the tissue possesses limited intrinsic healing capacity. Chondrogenesis from ESCs has been studied for approximately two decades. However, ethical concerns, risk of teratoma formation and allogenic transplant rejection makes them less suitable for clinical applications. Another stem cell type which has become popular in last few years is iPSCs. iPSCs possess similar properties that of ESCs and are generated by cellular reprogramming of somatic cells. It holds enormous potential for personalized cell-based repair strategies to treat musculoskeletal disorders [25], but the preparation of autologous iPSCs from each patient is an expensive & time-consuming process, and further possesses low reprogramming efficiency [26]. Moreover, iPSCs too, possess tumorigenic tendency probably due to accumulation of culture-induced genomic and epigenomic variations [27]. Contrarily, MSCs offer several advantages over other stem cells types for clinical use due to their ease of isolation, propagation, immunotolerance, non-tumorigenicity and less ethical concerns. Further, high yield of cells and immunomodulatory properties make them suitable for allogenic transplant.
MSCs have been reported to promote tissue repair by replacing the damaged tissue and recruiting endogenous cells to the injury site. Further, differentiated MSCs secrete collagen II, TIMPs (Tissue Inhibitors of Metalloproteinases) and GAGs which are important part of ECM of cartilage. However, paracrine factors released by MSCs have been documented to play major role in regeneration, immunomodulation and decreasing inflammation [28]. They decrease oxidative stress by regulating expression of vascular endothelial growth factor (VEGF), transforming growth factor-β (TGF-β) and matrix metalloproteinases (MMPs) [29]. Moreover, they regulate immune response by secretion of various molecules like interleukins, prostaglandin E2, Interferon γ [30].
Since their discovery by Friedenstein et al. in the early 1970s, MSCs have emerged as one of the key players in cell-based therapy [31]. MSCs offer several advantages over ex-vivo expanded ACs which are susceptible to removal from their natural microenvironment and de-differentiation to fibroblast-like phenotype [32]. MSCs also facilitate better remodeling and integration with the host surface zone [33]. These are fibroblast-like, spindle-shaped and multipotent cells. According to the International Society for Cellular Therapy (ISCT), MSCs must possess plastic-adherence and tri-lineage differentiation potential. Further, these must exhibit the presence of specific cell surface markers namely CD105, CD73, CD90 and the absence of hematopoietic markers namely CD45, CD34, CD14 or CD11b, CD79α or CD19, HLA-DR [34]. Additionally, several other markers have also been found on MSCs, which includes CD271, SCA-1, and STRO-1 [35,36,37].
Bone Marrow (BM) is the oldest source of MSCsand BMSCs have been found to possess good in vitro chondrogenic differentiation potential [31, 38]. MSCs derived from other sourcesinclude adipose tissue (ADSCs), synovium (SMSCs), articular cartilage, skin, muscle, endometrium, infrapatellar fat pad (IMSCs), dental pulp (DPSCs), subchondralcortico-spongious bone, amniotic fluid, placenta, umbilical cord (UCMSCs) and umbilical cord blood (UCBMSCs) [39]. After bone marrow, adipose tissue is the next widely used source for MSC isolation. ADSCs possess comparable chondrogenic potential to BMSCs [40] and have high proliferation potential. Further, as compared to bone marrow, isolation procedure of adipose tissue is less invasive and large amount of tissue can be collected easily. Initially, ADSCs were isolated using enzymatic method as per protocol devised by Rodbell et al. [41]. However, in recent years ADSCs have been easily isolated using explant method as well. This method is cost effective as well as minimizes the risk of contamination coming due to use of enzymes [42].
Another source of MSC used for cartilage repair is synovial fluid. Synovium MSCs are isolated from synovium of knee and hip region. Enzymatic method is used for isolation of MSCs from synovium tissue [39, 43]. A small synovial tissue biopsy can give good yield of autologous cells and these cells possess higher chondrogenic potential than MSCs from other sources. However, at present they have been used in pre-clinical settings only [28].
As MSCs from different sources are available, it is important to consider source-dependent heterogeneity of MSCs in terms of growth characteristics, marker profiling and chondrogenic differentiation potential before choosing the right candidate. For instance, BMSCs have been reported to show better chondrogenic potential than MSCs from other sources [44]. Similarly, Koga et al. [45] reported that SMSCs and BMSCs have better chondrogenic potential than ADSCs and muscle derived MSCs. Further, in a donor matched study, ADSCs were reported to have weaker chondrogenic potential than MSCs derived from infrapatellar fat [45]. Depending upon the source of MSCs used, the therapy is categorized as autologous and allogenic. Most of the autologous settings use only BMSCs. However, in every case use of autologous MSCs may not be possible because of old age of most OA patients, their disease condition and low yield of cells [46]. In this light, allogenic MSCs have come up as novel strategy conforming to low immunogenicity and its immunomodulatory properties. Additionally, allogenic source of MSCs can provide large number of homogenous populations which can be expanded, characterized and cryopreserved in advance to meet the growing need of MSCs in future.
Guiding factors for recapitulating articular cartilage
Accumulating evidences suggest that in vitro chondrogenesis of MSCs is susceptible to hypertrophic differentiation which may result in generation of neocartilage with fibrocartilage like properties rather than hyaline cartilage. This has emerged as a pressing concern as the regeneration of clinically effective engineered cartilage tissue is hindered. For instance, implantation of TGF-β3 induced MSC pellet, at ectopic sites in SCID mice orchestrated events that led to endochondral ossification rather than formation of stable cartilage phenotype indicating the premature induction of hypertrophic genes during in vitro chondrogenesis [32]. It has thus become incumbent to devise strategies to stringently mimic the endogenous biochemical, mechanical and physiological milieu for recapitulating the properties of native articular cartilage. In this regard, various approaches mimicking the biochemical, mechanical, and cellular regulatory factors during cartilage development have been extensively investigated. Growth factors, hypoxia, mechanical stimulation, 3D environments generated by micromass culture or scaffolds and co-culturing have shown to play important roles in promoting chondrogenic differentiation (Fig. 1).
Growth factors promoting chondrogenic differentiation of MSCs
MSCs are induced to undergo in vitro chondrogenic differentiation by culturing them in presence of growth factors that are added to the basal media. It mainly comprises of high-glucose DMEM supplemented with sodium pyruvate, l-proline, l-ascorbate-2-phosphate, ITS (Insulin, Transferrin, and Selenium) premix and Dexamethasone. Various culture conditions used in protocols for in vitro chondrogenic differentiation have been summarized in Table 1. Apart from defined growth factors and conventional differentiation medium, platelet rich plasma (PRP; 10%) and platelet lysate (PL; 5%) have also been used for in vitro chondrogenesis [47, 48].
Other than these, viral-mediated gene transfer has also been investigated to differentiate cells into chondrogenic lineage. In 1998, Mason et al. [63] demonstrated the feasibility of delivery of human BMP-7 via retroviral vector in rabbit periosteal cells for cartilage regeneration both in vitro and in vivo. Similarly, adenoviral vectors have also been used for mediating sustained delivery of growth factors, like TGF-β1, bone morphogenetic protein-2 (BMP-2), BMP-4 and insulin like growth factor-1 (IGF-1) in MSCs for elucidating their effects on cartilage repair [64,65,66,67].
Low oxygen tension or hypoxia
Hypoxia plays a pivotal role in chondrogenic differentiation of MSCs by inducing the expression of target genes of hypoxia inducible factor (HIF) including VEGFA, EGLN, and PGK1 via HIF complex. Accumulating evidence suggest that maintenance of hypoxic condition (2–5% O2) stimulates early chondrogenic commitment and promotes stabilization of HIF resulting in regeneration of better quality neocartilage by exerting inhibitory effect on hypertrophic differentiation of chondrocytes [68,69,70].
3D culture (pellet culture and scaffolds)
In chondrogenic differentiation studies, micromass or pellet culture or 3D pellet culture system or aggregate culture system [58] is very crucial and widely used as the packing of high cell density of MSCs. It is believed to mimic mesenchymal condensation during developmental chondrogenesis. However, these cannot be directly used in most clinical therapies because of the limitations in their mass sizes [71].
Most recent cartilage engineering approaches have focused on the use of combination of cells, scaffolds and bioactive factors to regenerate functional cartilage tissue. The use of tissue specific ECM composition has been shown to direct the differentiation of stem cells down the same lineage [72]. Many scaffolds made up of synthetic polymers or natural biomaterials have been extensively developed and used in tissue engineering as cell carriers both in vitro and in vivo.
Mechanical factors
The exposure of native articular cartilage to a myriad of mechanical stimuli such as dynamic compression, fluid shear, and hydrostatic pressure is essential for the maintenance of structural integrity of the tissue. Considering the mechanical function of articular cartilage, proper mechanical stimulation during (dynamic compression, fluid shear, and hydrostatic pressure) in vitro culture can also play a key role in regulating the chondrogenic differentiation of MSCs.
In an exemplary study, Schätti et al. [73] showed that a combination of shear and compression forces led to cumulative enhancement of chondrogenesis rather than either stimulus alone. For this analysis, they mixed hBMSCs with fibrin hydrogel and seeded it on a porous polyurethane (PU) scaffold. This scaffold and scaffold/cell construct were subjected to mechanical conditioning and histological analysis was done to check their impact on chondrogenesis. Similarly, reports have been published using MSCs embedded on different matrix like porous PU matrix [74] and collagen [75].
Co-culture of MSCs and articular chondrocytes (ACs)
Another strategy that has been explored to rebuild hyaline-like cartilage involves co-culturing ACs and MSCs. ACs are capable of producing stable and non-mineralized cartilage tissue, however, they tend to undergo de-differentiation into fibroblast-like cells during in vitro proliferation [76]. It is believed that co-culturing of ACs and MSCs can provide physiological cues and create suitable milieu for regulated differentiation. ACs can suppress the undesired hypertrophy, promote chondrogenesis and help in suppression of inflammatory activity upon co-culturing with MSCs [47, 77, 78]. The soluble factors secreted by MSCs mediate cartilage regeneration by exerting paracrine effects on ACs, which can be characterized by changes in their cellular morphology, proliferation, gene expression and ECM production. According to a study, indirect co-culture of human umbilical cord blood MSCs (hUC-BMSCs) and hAC at low density (0.6 × 104 cells) exhibited the potential to induce hUC-BMSCs differentiation into hyaline chondrocytes [79]. In another study, increased expression of cartilage-specific genes by hUC-MSCs when co-cultured indirectly with OA patients derived ACs, revealed that ACs promoted chondrogenic differentiation. Further, suppression of expression of COX2, collagen X, MMP13 in ACs suggested that hUC-MSC inhibited inflammatory activity in OA chondrocytes. This study thus illustrates that the co-culture of hUC-MSCs and OA chondrocytes may provide a therapeutic potential in OA treatment [78].
Biomaterials in cartilage repair
Biomaterials play a very important role in cartilage tissue engineering. They help in cell proliferation, adhesion and act as carrier for delivery of stem cells at the defect site preventing their loss. Moreover, it also helps in guiding the growth of newly formed tissue. To fulfill its role, an ideal 3D-scaffold for cartilage tissue engineering should be biocompatible, biodegradable, non-antigenic, highly porous, osteoconductive, possess good mechanical strength and capable of maintaining the cells in differentiated and functional state [80]. In addition, the scaffold material should exhibit mechanical properties in terms of compressive strength and Young’s modulus like the native tissue. Various scaffolds made up of natural as well as synthetic matrix have been used alone or along with cells for repair of cartilage lesions. Natural, biodegradable matrices are mainly made up of silk, collagen, chitosan, agarose, gelatin, alginate and HA [81]. Natural polymers like collagen and fibrin are highly biocompatible, promote cell adhesion and do not elicit immune response. But they have weak mechanical strength and their rate of degradation cannot be controlled. Whereas, synthetic materials used for cartilage repair have advantage over natural ones as their rate of degradation and mechanical strength can be controlled by making different combinations and using different methods for synthesis and cross-linking [82]. These are mainly made up of PLGA, PLA, PEG, PCL and PEG [83]. However, natural polymers are preferred over synthetic polymers because later are expensive, can elicit immune response and their byproducts may lead to inflammatory reaction in the host. Therefore, it is necessary to find out the right combinations of matrix and their methods of synthesis so that their shortcomings can be avoided, and an ideal scaffold can be prepared. Many in vitro studies have been conducted emphasizing benefits of these scaffolds for cartilage repair. In same line, few important in vitro studies using various scaffolds and their combinations have been summarized in Table 2.
Status of marketed scaffolds
Based on positive outcomes of using combination of cells & matrix for cartilage repair in in vitro and in vivo model, several scaffolds have been introduced with clinical advantages. At present, various products have been marketed internationally for treatment of cartilage related injuries. These products are mostly made up of collagen, HA, or synthetic polymers seeded with autologous chondrocytes (Supplementary Table 1). Most of other polymers used in animal studies have yet not been opted for clinical use because of chances of immune reaction and disease transmission. These matrices are used either alone or in combination with cells (autologous chondrocytes). Most common matrix used in these products is collagen [100,101,102] which is the main component of ECM of chondrocytes [103]. Collagen matrix seeded with autologous chondrocytes has shown better results than scaffold alone and is available in market in name of CaRes in Australia, NeoCart and Novocart in USA [104,105,106]. Apart from collagen matrix, hyaline matrix-based product seeded with autologous chondrocytes was marketed in name of Hyalograft. However, it has been withdrawn in 2013 [107]. Other than these natural polymers, allograft collagen matrix harboring autologous chondrocytes have been used [108]. Among synthetic polymers, only poly (ethylene oxide-terephthalate)/poly (butylene terephthalate) (PEOT/PBT) biodegradable scaffold seeded with autologous chondrocytes is available in name of INSTRUCT, Netherland, which is CE certified [109].
Considering their advantages, some of these products are available for treatment since long but many are still available only in restricted areas for clinical trials only. Additionally, their high cost is the major limiting factor for its utilization for lower middle-income economies. In USA, the cost of autologous chondrocyte transplant for cartilage repair is around $40,000 [110]. Similarly, in National Health Service (NHS), UK, transplant of scaffold with autologous chondrocytes cost approximately £12,000, which includes £2,500 for harvesting and regrowing the cells [111]. Therefore, even at present the approach using biomaterials for cartilage repair has not yet become available for patients either because of high cost, associated rejection risks or problems in approval for human use.
Pre-clinical studies
Promising therapeutic candidate for cartilage repair can be evaluated through pre-clinical trials in appropriate animal models that mimic the histopathology and symptoms of OA. These animal models are mostly created surgically [112]. The most used surgical method of inducing OA is anterior cruciate ligament transection (ACLT), meniscectomy and ovariectomy. The other method of OA induction in animals is by injecting chemicals directly in the joints of animals. The most commonly used chemicals for this purpose include papain, collagenase and mono-iodoacetate (MIA) [113]. These animal models are transplanted withundifferentiated stem cells, pre-differentiated stem cells with or without matrix. Further, the efficiency of therapeutic candidate in recapitulating the damaged tissue can be evaluated by following grading systems such as ICRS (International Cartilage Research Society) and OAS (Oswestry Arthroscopy Score) [114].
These studies have been performed in small as well as large animals including murine, porcine, canine and equine models. Studies on small animals are comparatively easy as these animals can be housed easily, and experiments are cost effective. However, these animals possess intrinsic cartilage healing and bear weight on all the limbs, limiting the full extrapolation of outcomes of these studies to repair of human cartilage defect. But at the same time, the results give us proof of concept, to design studies at larger scale and in large animals, thus saving the time and cost. All major pre-clinical studies in this regard using small animals namely mice, rat, rabbit and large animal such as Brazilian pigs have been summarized in Supplementary Table 2. The promising outcomes of such studies have given us lead for taking these options from bench to bedside.
These studies have used primed as well as undifferentiated cells from different sources to elucidate their role in cartilage repair. Mostly studies have been carried out using BMSCs and ADSCs. However, in last few years SMSCs have emerged as potential alternative candidate for cartilage repair because of their ease of isolation, better in vivo immunosuppression, better chondro-differentiation, and secretion of large amount of ECM [115,116,117]. Recently, DPSCs have also been used for cartilage repair and tested in Brazilian pigs; a large animal model for cartilage repair for the first time [118]. These MSCs from various sources have been transplanted with or without scaffold to test their efficacies. In most of the studies, it has been reported that cells transplanted on scaffolds give better results in cartilage repair than cells or scaffolds alone [119]. Further, type of cell being used for transplantation is a big concern. Previous studies have employed use of only undifferentiated cells for transplantation. Moreover, a recent study has also reported same outcome where they have transplanted autologous SMSCs derived from synovial cavity of rabbits at the site of cartilage defect and observed that differentiated cells lead to fibrous tissue formation whereas hyaline tissue like structure was found in animals transplanted with undifferentiated MSCs. It is believed that pre-differentiation leads to weakening of stemness of MSCs and alters their paracrine effect. Therefore, they focus on using undifferentiated cells [34,35,36, 120, 121] considering the release of paracrine factors by MSCs which help in faster cartilage healing. But in recent years, use of differentiated cells has shown better outcomes and healing than undifferentiated cells. Scaffolds loaded with cells and TGF-β1 has been reported to have better cartilage regeneration than one without TGF-β1 [33]. Similarly, other factors like BMP2, BMP4, IGF-1 have been used for chondro-differentiation which helps in synthesizing hyaline cartilage like structure with reduced hypertrophy shown by use undifferentiated cell population.In another study led by Prasadam et al. [122], mixed cultures of BMSCs and ACs have been transplanted and shown to exhibit better chondro protection and regeneration than their monocultures. However, in clinical settings it may not be possible to isolate both ACs and MSCs in autologous therapy. Therefore, there is a pressing need to devise strategies which will minimize the drawbacks of these cell types and help us utilize them efficiently for repair of articular cartilage.
Clinical studies
Stem cells from various sources have been used in vitro by harnessing their chondrogenic differentiation potential. Various growth factors have been used in these protocols to enhance the mineralization and inhibit rapid cell death after long in vitro protocols. Based on promising results shown by stem cells in in vitro models and pre-clinical settings, several clinical trials have been done in case of OA, to evaluate its safety, feasibility, efficacy and stability. Information regarding clinical trials was searched using terms “stem cell” & “osteoarthritis” on ClinicalTrials.gov. As per the database, till date, 83 clinical trials have been registered using stem cells. Out of these, 29 trials have been completed where 16 trials used BMSCs and 07 trials used ADSCs, 03 trials used UCMSCs, UCBMSCs and WJ-MSCs and the remaining 03 studies did not reveal the source of MSCs. Also, most of the studies have reported use of autologous stem cells to avoid immune rejection, with only 06 trials completed using allogenic stem cells. The outcomes of MSCs administration are measured based on safety assessment, serological measurement of immune cells, MRI, KooS score, HooS score and WOMAC score. Majority of the studies using autologous cells have shown follow up of 12 months except for two studies which have follow up of 48 months and 36 months, respectively, showing the safety and long-term efficacy of MSCs. Whereas, only 01 trial administering allogenic MSCs has reported follow up of 24 months, supporting its safety and efficacy. At present, more trials using allogenic MSCs with their long term follow up are warranted to validate and strengthen the outcomes. Further, none of the study has used primed or differentiated cells which might increase the efficiency of regeneration and may reduce the chances of fibrocartilage formation. Moreover, out of 29, only 02 studies have used matrix along with cells which have shown successful results (Supplementary Table 3 and 4). This combinatorial approach has proven very beneficial as per available pre-clinical studies data also. However, this needs to be explored in depth in clinical settings to reach some conclusion and take it to therapeutics.
Future prospects
Today, regenerative therapy using cells and growth factors along with use of biomaterials is becoming widely available option for the repair of joint surface lesions and OA. A lot of in vitro & in vivo studies have been done in past, which have shown promising results. Undifferentiated as well as differentiated cells in combination with biomaterials have been used in these studies. Some of their results have been translated to clinical studies as wellwhich haveshown variegated results. The use of MSCs has proven to be safe in long term follow ups and it also increases the quality of life of patients. But, none of these studies has reported restoration of original hyaline cartilage in long term follow ups.The important reasons for this unclear picture are mainly selection of stem cell type, matrix as well as design of clinical study.
First issue to be addressed remains with standardization of protocols for efficient homogenous MSCs isolation, their characterization and efficient cartilage differentiation. MSCs from aged donor have found to undergo senescence earlier [123], and they exhibit lower expression of surface markers along with reduced regeneration ability. Similarly, MSCs of later passages have reported to show poor differentiation ability as compared to cells of early passages. Therefore, definingage of donor, passage of cells, growth conditions and factors required for in vitro differentiation becomes critical in order to move to clinical settings. Despite lack of standardization of isolation protocols, because of their established safety and regenerative potential, MSCs have been extensively used in clinical settings and around 83 clinical trials using MSCs for cartilage repair are registered on ClinicalTrials.gov. These trials have shown safety of MSCs in long term, but it is difficult to conclude their efficacy in regeneration because of various reasons. Key reasons for these lacunae include non-uniformity of number of patients included in the study, degree of injury, follow up criteria, type of cell administered, adjuvant therapy, selection of control etc.
Further, in past few years, implantation of biomaterials in cartilage defect models has shown promising results. Results of pre-clinical studies have demonstrated that biomaterials in combination with stem cells can enhance their regeneration potential and result in better cartilage repair as compared to stem cells alone.
Despite these studies, none of the combination of stem cell and biomaterial has achieved success in mimicking features identical to native cartilage. Till date only one such study has been done in patients where stem cells along with collagen scaffold have been transplanted in OA patients, but it has not posted results on ClinicaltTrials.gov showing unknown status. However, the approach taken by this study has opened the gateway for undertaking similar studies using combination of stem cells and scaffold for cartilage repair. 3D bioprinting has emerged as promising method of designing scaffolds with proper and defined arrangement of cells and matrix in layer by layer manner. This arrangement may provide constructs having proper zonal distribution ofcells, matrix and growth factors in 3D which may mimic native cartilage more closely and may prove to have better regeneration than scaffolds designed by conventional methods [124].
Other potent candidates which have emerged recently for cartilage repair include use of exosomes and gene therapy. Exosomes are nano scale extracellular vesicles secreted by almost all cells including MSCs. These have been successfully used for treatment of many diseases including OA in animal models [125]. It is postulated that these exosomes may protect cartilage by increasing expression of chondrocyte marker and decreasing expression of catabolic and inflammatory markers [126]. These may also participate in migration and proliferation of chondrocytes [127]. These exosomes when transplanted with hydrogel in rabbit cartilage defect model were found to regenerate cartilage after 12 weeks [128]. These exosomes may provide “cell free therapeutic paradigm” with low immunogenicity and no risk of tumor formation. Gene therapy has also come up as promising option for various degenerative diseases including OA. This approach focuses on synthesizing the proteins in mammalian cell lines, which can help restoring the balance of anabolic and catabolicmechanism which is lost in OA. In this line, Kolon Tissue GeneInc., USA, in November 2018, treated first OA patient using their product Invossa™(TG-C). Invossa™ involves a single intra-articular injection of allogenic primary chondrocytes and irradiated GP2-293 cells transduced with viral vector over expressing TGF-β1 which possibly promotes regeneration of the tissue [129].
Conclusion
In last few years, OA has emerged as a major socioeconomic burden and its prevalence is continuously increasing due toaging of population and emergence of sedentary lifestyle. Considering non-availability of satisfactory treatment, regenerative medicine using stem cells, scaffolds and growth factors has been worked upon extensively both in vitro and in vivo and shown promising outputs. Despite, there exists a lot of missing links and lacunae in this approach which warrants a lot of effort at both basic and clinical research level. Based on previous studies, the choice of right matrix for the support and differentiation of cells, choice of cells, inducers and antioxidants in the media remain key areas to be ventured. Further, in clinical studies dose and type of cells to be administered, inclusion of right controls and long term follow up, adjuvant therapy remain few of the key issues which needs to be addressed, before this approach becomes clinically available for patient care. However, the extensive research and their positive results using stem cells and scaffolds validate that in future this combination may come up as “off the shelf” therapy for cartilage repair in OA patients.
References
Hayami T, Pickarski M, Zhuo Y, Wesolowski GA, Rodan GA, Duong LT (2006) Characterization of articular cartilage and subchondral bone changes in the rat anterior cruciate ligament transection and meniscectomized models of osteoarthritis. Bone 38(2):234–243
Kaur R, Ghosh A, Singh A (2018) Prevalence of knee osteoarthritis and its determinants in 30–60 years old women of Gurdaspur, Punjab. Int J Med Sci Public Health 7(10):825–831
Parkinson L, Moorin R, Peeters G, Byles J, Blyth F, Caughey G, Cunich M, Magin P, March L, Pond D (2016) Incident osteoarthritis associated with increased allied health services use in ‘baby boomer’ Australian women. Aust NZ J Public Health 40:356–361
Pal CP, Singh P, Chaturvedi S, Pruthi KK, Vij A (2016) Epidemiology of knee osteoarthritis in India and related factors. Indian J Orthop 50(5):518
Azad CS, Singh AK, Poorti Pandey P, Singh M, Chaudhary P, Tia N, Rastogi A, Gambhir IS (2017) Osteoarthritis in India: an epidemiologic aspect. Int J Recent Sci Res 8(10):20918–20922
Zhang Y, Jordan JM (2010) Epidemiology of osteoarthritis. Clin Geriatr Med 26(3):355–369
Symmons D, Turner G, Webb R, Asten P, Barrett E, Lunt M, Scott D, Silman A (2002) The prevalence of rheumatoid arthritis in the United Kingdom: new estimates for a new century. Rheumatology 41(7):793–800
Roseti L, Desando G, Cavallo C, Petretta M, Grigolo B (2019) Articular cartilage regeneration in osteoarthritis. Cells 8(11):1305
Nakamura A, Kapoor M (2016) mTOR: a critical mediator of articular cartilage homeostasis. Molecules to medicine with mTOR. Elsevier, Amsterdam, pp 57–68
Jeng L, Kwong FN, Spector M (2011) Chapter 42—articular cartilage. In: Atala A, Lanza R, Thomson JA, Nerem R (eds) Principles of regenerative medicine, 2nd edn. Academic Press, San Diego, pp 761–777. https://doi.org/10.1016/B978-0-12-381422-7.10042-2
Reinold MM, Macrina LC, Ostrander RV, CainEL DJR (2006) Rehabilitation after articular cartilage repair procedures: osteochondral autograft transplantation and autologous chondrocyte implantation. Postsurgical orthopedic sports rehabilitation knee and shoulder. Elsevier, Saint Louis, pp 383–407
Fisher M, Ackley T, Richard K, Oei B, Dealy CN (2019) Osteoarthritis at the cellular level: mechanisms, clinical perspectives, and insights from development. Reference module in biomedical sciences encyclopedia of biomedical engineering. Elsevier, Amsterdam, pp 660–676
Dubey NK, Mishra VK, Dubey R, Syed-Abdul S, Wang JR, Wang PD, Deng W-P (2018) Combating osteoarthritis through stem cell therapies by rejuvenating cartilage: a review. Stem Cells Int. https://doi.org/10.1155/2018/5421019
Maumus M, Pers Y-M, Ruiz M, Jorgensen C, Noël D (2018) Mesenchymal stem cells and regenerative medicine: future perspectives in osteoarthritis. Med Sci (Paris) 34(12):1092–1099. https://doi.org/10.1051/medsci/2018294
Vina ER, Kwoh CK (2018) Epidemiology of osteoarthritis: literature update. Curr Opin Rheumatol 30(2):160
Cole BJ, Pascual-Garrido C, Grumet RC (2009) Surgical management of articular cartilage defects in the knee. JBJS 91(7):1778–1790
Bhatia S, Hsu A, Lin EC, Chalmers P, Ellman M, Cole BJ, Verma NN (2012) Surgical treatment options for the young and active middle-aged patient with glenohumeral arthritis. Adv Orthop. https://doi.org/10.1155/2012/846843
McGowan KB, Stiegman G (2013) Regulatory challenges for cartilage repair technologies. Cartilage 4(1):4–11
Browne JE, Branch TP (2000) Surgical alternatives for treatment of articular cartilage lesions. J Am Acad Orthop Surg 8(3):180–189
Steadman JR, Briggs KK, Rodrigo JJ, Kocher MS, Gill TJ, Rodkey WG (2003) Outcomes of microfracture for traumatic chondral defects of the knee: average 11-year follow-up. Arthroscopy 19(5):477–484
Niemeyer P, Albrecht D, Andereya S, Angele P, Ateschrang A, Aurich M, Baumann M, Bosch U, Erggelet C, Fickert S (2016) Autologous chondrocyte implantation (ACI) for cartilage defects of the knee: a guideline by the working group “Clinical Tissue Regeneration” of the German Society of Orthopaedics and Trauma (DGOU). Knee 23(3):426–435
Zhang Z, Zhong X, Ji H, Tang Z, Bai J, Yao M, Hou J, Zheng M, Wood DJ, Sun J (2014) Matrix-induced autologous chondrocyte implantation for the treatment of chondral defects of the knees in Chinese patients. Drug Des Dev Ther 8:2439
Mandelbaum B, Browne JE, Fu F, Micheli LJ, Moseley JB, Erggelet C, Anderson AF (2007) Treatment outcomes of autologous chondrocyte implantation for full-thickness articular cartilage defects of the trochlea. Am J Sports Med 35(6):915–921
Brittberg M (2009) Cell carriers as the next generation of cell therapy for cartilage repair: a review of the matrix-induced autologous chondrocyte implantaion procedure. Am J Sports Med 38(6):1259–1271
Guzzo RM, Gibson J, Xu RH, Lee FY, Drissi H (2013) Efficient differentiation of human iPSC-derived mesenchymal stem cells to chondroprogenitor cells. J Cell Biochem 114(2):480–490
Ohnuki M, Takahashi K (2015) Present and future challenges of induced pluripotent stem cells. Philos Trans R Soc B 370(1680):20140367
Lund RJ, Närvä E, Lahesmaa R (2012) Genetic and epigenetic stability of human pluripotent stem cells. Nat Rev Genet 13(10):732
Zhang R, Ma J, Han J, Zhang W, Ma J (2019) Mesenchymal stem cell related therapies for cartilage lesions and osteoarthritis. Am J Transl Res 11(10):6275
Caplan AI, Dennis JE (2006) Mesenchymal stem cells as trophic mediators. J Cell Biochem 98:1076–1084
Yi T, Song SU (2012) Immunomodulatory properties of mesenchymal stem cells and their therapeutic applications. Arch Pharmacal Res 35(2):213–221
Frieedenstein A, Petrakova K, Kurolesova A, Frolova G (1968) Hetrotopic of bone marrow. Analysis of precursor cells for osteogenic and hematopoetic tissue. Transplantacion 6(2):230
Pelttari K, Winter A, Steck E, Goetzke K, Hennig T, Ochs BG, Aigner T, Richter W (2006) Premature induction of hypertrophy during in vitro chondrogenesis of human mesenchymal stem cells correlates with calcification and vascular invasion after ectopic transplantation in SCID mice. Arthritis Rheum 54(10):3254–3266
Wang W, Li B, Yang J, Xin L, Li Y, Yin H, Qi Y, Jiang Y, Ouyang H, Gao C (2010) The restoration of full-thickness cartilage defects with BMSCs and TGF-beta 1 loaded PLGA/fibrin gel constructs. Biomaterials 31(34):8964–8973
Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, Deans R, Keating A, Prockop D, Horwitz E (2006) Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 8(4):315–317
Kohli N, Al-Delfi IR, Snow M, Sakamoto T, Miyazaki T, Nakajima H, Uchida K, Johnson WE (2019) CD271-selected mesenchymal stem cells from adipose tissue enhance cartilage repair and are less angiogenic than plastic adherent mesenchymal stem cells. Sci Rep 9(1):3194
Mak J, Jablonski C, Leonard C, Dunn JF, Raharjo E, Matyas J, Biernaskie J, Krawetz R (2016) Intra-articular injection of synovial mesenchymal stem cells improves cartilage repair in a mouse injury model. Sci Rep 6:23076
Neumann K, Dehne T, Endres M, Erggelet C, Kaps C, Ringe J, Sittinger M (2008) Chondrogenic differentiation capacity of human mesenchymal progenitor cells derived from subchondral cortico-spongious bone. J Orthop Res 26(11):1449–1456
Johnstone B, Hering TM, Caplan AL, Goldberg VM, Yoo JU (1998) In vitro chondrogenesis of bone marrow-derived mesenchymal progenitor cells. Exp Cell Res 238:265–272
Berebichez-Fridman R, Montero-Olvera PR (2018) Sources and clinical applications of mesenchymal stem cells: state-of-the-art review. Sultan Qaboos Univ Med J 18(3):e264–e277. https://doi.org/10.18295/squmj.2018.18.03.002
Winter A, Breit S, Parsch D, Benz K, Steck E, Hauner H, Weber RM, Ewerbeck V, Richter W (2003) Cartilage-like gene expression in differentiated human stem cell spheroids: a comparison of bone marrow–derived and adipose tissue–derived stromal cells. Arthritis Rheum 48(2):418–429
Rodbell M (1966) Metabolism of isolated fat cells II. The similar effects of phospholipase C (Clostridium perfringens α toxin) and of insulin on glucose and amino acid metabolism. J Biol Chem 241(1):130–139
Priya N, Sarcar S, Majumdar AS, SundarRaj S (2014) Explant culture: a simple, reproducible, efficient and economic technique for isolation of mesenchymal stromal cells from human adipose tissue and lipoaspirate. J Tissue Eng Regen Med 8(9):706–716
Hatakeyama A, Uchida S, Utsunomiya H, Tsukamoto M, Nakashima H, Nakamura E, Pascual-Garrido C, Sekiya I, Sakai A (2017) Isolation and characterization of synovial mesenchymal stem cell derived from hip joints: a comparative analysis with a matched control knee group. Stem Cells Int. https://doi.org/10.1155/2017/9312329
Im G-I, Shin Y-W, Lee K-B (2005) Do adipose tissue-derived mesenchymal stem cells have the same osteogenic and chondrogenic potential as bone marrow-derived cells? Osteoarthritis Cartilage 13(10):845–853
Koga H, Muneta T, Nagase T, Nimura A, Ju Y, Mochizuki T, Sekiya I (2008) Comparison of mesenchymal tissues-derived stem cells for in vivo chondrogenesis: suitable conditions for cell therapy of cartilage defects in rabbit. Cell Tissue Res. 333(2):207–215. https://doi.org/10.1007/s00441-008-0633-5
Roobrouck VD, Ulloa-Montoya F, Verfaillie CM (2008) Self-renewal and differentiation capacity of young and aged stem cells. Exp Cell Res 314(9):1937–1944
Ramezanifard R, Kabiri M, Ahvaz HH (2017) Effects of platelet rich plasma and chondrocyte co-culture on MSC chondrogenesis, hypertrophy and pathological responses. EXCLI J 16:1031
Hassan G, Bahjat M, Kasem I, Soukkarieh C, Aljamali M (2018) Platelet lysate induces chondrogenic differentiation of umbilical cord-derived mesenchymal stem cells. Cell Mol Biol Lett 23(1):11
Boeuf S, Steck E, Pelttari K, Hennig T, Buneß A, Benz K, Witte D, Sültmann H, Poustka A, Richter W (2008) Subtractive gene expression profiling of articular cartilage and mesenchymal stem cells: serpins as cartilage-relevant differentiation markers. Osteoarthritis Cartilage 16(1):48–60
Shimaya M, Muneta T, Ichinose S, Tsuji K, Sekiya I (2010) Magnesium enhances adherence and cartilage formation of synovial mesenchymal stem cells through integrins. Osteoarthritis Cartilage 18(10):1300–1309
Farrell E, Both SK, Odörfer KI, Koevoet W, Kops N, O'Brien FJ, De Jong RJB, Verhaar JA, Cuijpers V, Jansen J (2011) In-vivo generation of bone via endochondral ossification by in-vitro chondrogenic priming of adult human and rat mesenchymal stem cells. BMC Musculoskelet Disord 12(1):31
Hamid AA, Idrus RBH, Saim AB, Sathappan S, Chua K-H (2012) Characterization of human adipose-derived stem cells and expression of chondrogenic genes during induction of cartilage differentiation. Clinics 67(2):099–106
Lee HH, O'Malley MJ, Friel NA, Chu CR (2013) Effects of doxycycline on mesenchymal stem cell chondrogenesis and cartilage repair. Osteoarthritis Cartilage 21(2):385–393
Murphy MK, Huey DJ, Hu JC, Athanasiou KA (2015) TGF-β1, GDF-5, and BMP-2 stimulation induces chondrogenesis in expanded human articular chondrocytes and marrow-derived stromal cells. Stem Cells 33(3):762–773
Nakagawa Y, Muneta T, Otabe K, Ozeki N, Mizuno M, Udo M, Saito R, Yanagisawa K, Ichinose S, Koga H (2016) Cartilage derived from bone marrow mesenchymal stem cells expresses lubricin in vitro and in vivo. PLoS ONE 11(2):e0148777
Ogata Y, Mabuchi Y, Yoshida M, Suto EG, Suzuki N, Muneta T, Sekiya I, Akazawa C (2015) Purified human synovium mesenchymal stem cells as a good resource for cartilage regeneration. PLoS ONE 10(6):e0129096
Xu F-T, Li H-M, Zhao C-Y, Liang Z-J, Huang M-H, Li Q, Chen Y-C, Chi G-Y (2015) Characterization of chondrogenic gene expression and cartilage phenotype differentiation in human breast adipose-derived stem cells promoted by ginsenoside Rg1 in vitro. Cell Physiol Biochem 37(5):1890–1902
Yoo JU, Barthel TS, Nishimura K, Solchaga L, Caplan AI, Goldberg VM, Johnstone B (1998) The chondrogenic potential of human bone-marrow-derived mesenchymal progenitor cells. JBJS 80(12):1745–1757
Hu T, Xu H, Wang C, Qin H, An Z (2018) Magnesium enhances the chondrogenic differentiation of mesenchymal stem cells by inhibiting activated macrophage-induced inflammation. Sci Rep 8(1):1–13
Sorrell JM, Somoza RA, Caplan AI (2018) Human mesenchymal stem cells induced to differentiate as chondrocytes follow a biphasic pattern of extracellular matrix production. J Orthop Res 36(6):1757–1766
Huang X, Zhong L, Hendriks J, Post J, Karperien M (2018) The effects of the WNT-signaling modulators BIO and PKF118-310 on the chondrogenic differentiation of human mesenchymal stem cells. Int J Mol Sci 19(2):561
Al-Yamani A, Kalamegam G, Ahmed F, Abbas M, Sait KHW, Anfinan N, Al-Wasiyah MK, Huwait EA, Gari M, Al-Qahtani M (2018) Evaluation of in vitro chondrocytic differentiation: a stem cell research initiative at the King Abdulaziz University, Kingdom of Saudi Arabia. Bioinformation 14(2):53
Mason JM, Grande DA, Barcia M, Grant R, Pergolizzi RG, Breitbart AS (1998) Expression of human bone morphogenic protein 7 in primary rabbit perisoteal cells: potential utility in gene therapy for osteochondral repair. Gene Ther 5:1098–1104
Steinert AF, Palmer GD, Pilapil C, Nöth U, Evans CH, Ghivizzani SC (2008) Enhanced in vitro chondrogenesis of primary mesenchymal stem cells by combined gene transfer. Tissue Eng A 15(5):1127–1139
Steinert AF, Proffen B, Kunz M, Hendrich C, Ghivizzani SC, Nöth U, Rethwilm A, Eulert J, Evans CH (2009) Hypertrophy is induced during the in vitro chondrogenic differentiation of human mesenchymal stem cells by bone morphogenetic protein-2 and bone morphogenetic protein-4 gene transfer. Arthritis Res Ther 11(5):R148
Gelse K, von der Mark K, Aigner T, Park J, Schneider H (2003) Articular cartilage repair by gene therapy using growth factor–producing mesenchymal cells. Arthritis Rheum 48(2):430–441
Palmer GD, Steinert A, Pascher A, Gouze E, Gouze J-N, Betz O, Johnstone B, Evans CH, Ghivizzani SC (2005) Gene-induced chondrogenesis of primary mesenchymal stem cells in vitro. Mol Ther 12(2):219–228
Portron S, Hivernaud V, Merceron C, Lesoeur J, Masson M, Gauthier O, Vinatier C, Beck L, Guicheux J (2015) Inverse regulation of early and late chondrogenic differentiation by oxygen tension provides cues for stem cell-based cartilage tissue engineering. Cell Physiol Biochem 35(3):841–857
Taheem DK, Foyt DA, Loaiza S, Ferreira SA, Ilic D, Auner HW, Grigoriadis AE, Jell G, Gentleman E (2018) Differential regulation of human bone marrow mesenchymal stromal cell chondrogenesis by hypoxia inducible factor-1α hydroxylase inhibitors. Stem Cells 36(9):1380–1392
Gómez-Leduc T, Desancé M, Hervieu M, Legendre F, Ollitrault D, de Vienne C, Herlicoviez M, Galéra P, Demoor M (2017) Hypoxia is a critical parameter for chondrogenic differentiation of human umbilical cord blood mesenchymal stem cells in type I/III collagen sponges. Int J Mol Sci 18(9):1933
Fan J, Varshney RR, Ren L, Cai D, Wang D-A (2009) Synovium-derived mesenchymal stem cells: a new cell source for musculoskeletal regeneration. Tissue Eng B 15(1):75–86
Tamaddon M, Burrows M, Ferreira S, Dazzi F, Apperley J, Bradshaw A, Brand D, Czernuszka J, Gentleman E (2017) Monomeric, porous type II collagen scaffolds promote chondrogenic differentiation of human bone marrow mesenchymal stem cells in vitro. Sci Rep 7:43519
Schätti O, Grad S, Goldhahn J, Salzmann G, Li Z, Alini M, Stoddart M (2011) A combination of shear and dynamic compression leads to mechanically induced chondrogenesis of human mesenchymal stem cells. Eur Cell Mater 22(214–225):b97
Cochis A, Grad S, Stoddart M, Fare S, Altomare L, Azzimonti B, Alini M, Rimondini L (2017) Bioreactor mechanically guided 3D mesenchymal stem cell chondrogenesis using a biocompatible novel thermo-reversible methylcellulose-based hydrogel. Sci Rep 7:45018
Cao W, Lin W, Cai H, Chen Y, Man Y, Liang J, Wang Q, Sun Y, Fan Y, Zhang X (2019) Dynamic mechanical loading facilitated chondrogenic differentiation of rabbit BMSCs in collagen scaffolds. Regen Biomater 6(2):99–106
Cooke M, Allon A, Cheng T, Kuo A, Kim H, Vail T, Marcucio R, Schneider R, Lotz J, Alliston T (2011) Structured three-dimensional co-culture of mesenchymal stem cells with chondrocytes promotes chondrogenic differentiation without hypertrophy. Osteoarthritis Cartilage 19(10):1210–1218
Pleumeekers MM, Nimeskern L, Koevoet J, Karperien M, Stok KS, van Osch GJ (2018) Trophic effects of adipose-tissue-derived and bone-marrow-derived mesenchymal stem cells enhance cartilage generation by chondrocytes in co-culture. PLoS ONE 13(2):e0190744
Wang H, Yan X, Jiang Y, Wang Z, Li Y, Shao Q (2018) The human umbilical cord stem cells improve the viability of OA degenerated chondrocytes. Mol Med Rep 17(3):4474–4482
Li X, Duan L, Liang Y, Zhu W, Xiong J, Wang D (2016) Human umbilical cord blood-derived mesenchymal stem cells contribute to chondrogenesis in coculture with chondrocytes. Biomed Res Int. https://doi.org/10.1155/2016/3827057
Cao Z, Dou C, Dong S (2014) Scaffolding biomaterials for cartilage regeneration. J Nanomater 2014:4
Armiento A, Stoddart M, Alini M, Eglin D (2018) Biomaterials for articular cartilage tissue engineering: learning from biology. Acta Biomater 65:1–20
Lam AT, Reuveny S, Oh SK-W (2020) Human mesenchymal stem cell therapy for cartilage repair: review on isolation, expansion, and constructs. Stem Cell Res 44:101738
Rai V, Dilisio MF, Dietz NE, Agrawal DK (2017) Recent strategies in cartilage repair: a systemic review of the scaffold development and tissue engineering. J Biomed Mater Res A 105(8):2343–2354
Estes BT, Wu AW, Guilak F (2006) Potent induction of chondrocytic differentiation of human adipose-derived adult stem cells by bone morphogenetic protein 6. Arthritis Rheum 54(4):1222–1232
Kafienah W, Mistry S, Perry MJ, Politopoulou G, Hollander AP (2007) Pharmacological regulation of adult stem cells: chondrogenesis can be induced using a synthetic inhibitor of the retinoic acid receptor. Stem Cells 25(10):2460–2468
Xu J, Wang W, Ludeman M, Cheng K, Hayami T, Lotz JC, Kapila S (2008) Chondrogenic differentiation of human mesenchymal stem cells in three-dimensional alginate gels. Tissue Eng A 14(5):667–680
Kurth T, Hedbom E, Shintani N, Sugimoto M, Chen F, Haspl M, Martinovic S, Hunziker EB (2007) Chondrogenic potential of human synovial mesenchymal stem cells in alginate. Osteoarthritis Cartilage 15(10):1178–1189
Yang Z, Wu Y, Li C, Zhang T, Zou Y, Hui JH, Ge Z, Lee EH (2011) Improved mesenchymal stem cells attachment and in vitro cartilage tissue formation on chitosan-modified poly (l-lactide-co-epsilon-caprolactone) scaffold. Tissue Eng A 18(3–4):242–251
Wu J, Xue K, Li H, Sun J, Liu K (2013) Improvement of PHBV scaffolds with bioglass for cartilage tissue engineering. PLoS ONE 8(8):e71563
Kim J, Lin B, Kim S, Choi B, Evseenko D, Lee M (2015) TGF-β1 conjugated chitosan collagen hydrogels induce chondrogenic differentiation of human synovium-derived stem cells. J Biol Eng 9(1):1
Focaroli S, Teti G, Salvatore V, Orienti I, Falconi M (2016) Calcium/cobalt alginate beads as functional scaffolds for cartilage tissue engineering. Stem Cells Int. https://doi.org/10.1155/2016/2030478
Xiao T, Guo W, Chen M, Hao C, Gao S, Huang J, Yuan Z, Zhang Y, Wang M, Li P (2017) Fabrication and in vitro study of tissue-engineered cartilage scaffold derived from Wharton’s jelly extracellular matrix. Biomed Res Int. https://doi.org/10.1155/2017/5839071
Wise JK, Yarin AL, Megaridis CM, Cho M (2009) Chondrogenic differentiation of human mesenchymal stem cells on oriented nanofibrous scaffolds: engineering the superficial zone of articular cartilage. Tissue Eng A 15(4):913–921
Galeano-Garces C, Camilleri ET, Riester SM, Dudakovic A, Larson DR, Qu W, Smith J, Dietz AB, Im H-J, Krych AJ (2017) Molecular validation of chondrogenic differentiation and hypoxia responsiveness of platelet-lysate expanded adipose tissue-derived human mesenchymal stromal cells. Cartilage 8(3):283–299
Shie M-Y, Chang W-C, Wei L-J, Huang Y-H, Chen C-H, Shih C-T, Chen Y-W, Shen Y-F (2017) 3D printing of cytocompatible water-based light-cured polyurethane with hyaluronic acid for cartilage tissue engineering applications. Materials 10(2):136
Huang S, Song X, Li T, Xiao J, Chen Y, Gong X, Zeng W, Yang L, Chen C (2017) Pellet coculture of osteoarthritic chondrocytes and infrapatellar fat pad-derived mesenchymal stem cells with chitosan/hyaluronic acid nanoparticles promotes chondrogenic differentiation. Stem Cell Res Ther 8(1):264
Calabrese G, Forte S, Gulino R, Cefalì F, Figallo E, Salvatorelli L, Maniscalchi ET, Angelico G, Parenti R, Gulisano M (2017) Combination of collagen-based scaffold and bioactive factors induces adipose-derived mesenchymal stem cells chondrogenic differentiation in vitro. Front Physiol 8:50
Sanjurjo-Rodríguez C, Castro-Viñuelas R, Hermida-Gómez T, Fuentes-Boquete IM, de Toro FJ, Blanco FJ, Díaz-Prado SM (2017) Human cartilage engineering in an in vitro repair model using collagen scaffolds and mesenchymal stromal cells. Int J Med Sci 14(12):1257
Barlian A, Judawisastra H, Alfarafisa NM, Wibowo UA, Rosadi I (2018) Chondrogenic differentiation of adipose-derived mesenchymal stem cells induced by l-ascorbic acid and platelet rich plasma on silk fibroin scaffold. PeerJ 6:e5809
Huang H, Xu H, Zhang J (2019) Current tissue engineering approaches for cartilage regeneration. https://doi.org/10.5772/intechopen.84429
https://fintel.io/doc/sec-hsgx-histogenics-10k-annual-report-2019-march-21-17977
https://www.aesculapbiologics.com/en/patients/novocart-3d.html
https://www.ema.europa.eu/en/medicines/human/withdrawn-applications/hyalograft-c-autog
https://www.smith-nephew.com/professional/products/all-products/mosaicplasty/
https://www.cellcotec.com/www.cellcotec.com/technology.phppage28/
Harrison L (2015) Chondrocyte therapy effective in knee cartilage repair. https://www.medscape.com/viewarticle/842043
BROOKS A Me and my operation: cartilage transplant. https://www.dailymail.co.uk/health/article-76501/Me-operation-cartilage-transplant.html
Bapat S, Hubbard D, Munjal A, Hunter M, Fulzele S (2018) Pros and cons of mouse models for studying osteoarthritis. Clin Transl Med 7(1):36
Kuyinu EL, Narayanan G, Nair LS, Laurencin CT (2016) Animal models of osteoarthritis: classification, update, and measurement of outcomes. J Orthop Surg Res 11(1):19
Van den Borne M, Raijmakers N, Vanlauwe J, Victor J, De Jong S, Bellemans J, Saris D (2007) International Cartilage Repair Society (ICRS) and Oswestry macroscopic cartilage evaluation scores validated for use in Autologous Chondrocyte Implantation (ACI) and microfracture. Osteoarthritis Cartilage 15(12):1397–1402
Lee W, Maeng G, Jeon R, Rho G, Lee S (2011) 210 comparative characterization of mesenchymal stem cells derived from miniature pig synovium, synovial fluid and bone marrow. Reprod Fertil Dev 24(1):217–217
Prado AAF, Favaron PO, da Silva LCLC, Baccarin RYA, Miglino MA, Maria DA (2015) Characterization of mesenchymal stem cells derived from the equine synovial fluid and membrane. BMC Vet Res 11(1):281
Zayed M, Caniglia C, Misk N, Dhar MS (2017) Donor-matched comparison of chondrogenic potential of equine bone marrow-and synovial fluid-derived mesenchymal stem cells: implications for cartilage tissue regeneration. Front Vet Sci 3:121
Fernandes TL, Shimomura K, Asperti A, Pinheiro CCG, Caetano HVA, Oliveira CRG, Nakamura N, Hernandez AJ, Bueno DF (2018) Development of a novel large animal model to evaluate human dental pulp stem cells for articular cartilage treatment. Stem Cell Rev Rep 14(5):734–743
Meng F, Zhang Z, Huang G, Chen W, Zhang Z, He A, Liao W (2016) Chondrogenesis of mesenchymal stem cells in a novel hyaluronate-collagen-tricalcium phosphate scaffolds for knee repair. Eur Cell Mater 31:79–94
Hermeto L, DeRossi R, Oliveira R, Pesarini J, Antoniolli-Silva A, Jardim P, Santana A, Deffune E, Rinaldi J, Justulin L (2016) Effects of intra-articular injection of mesenchymal stem cells associated with platelet-rich plasma in a rabbit model of osteoarthritis. Genet Mol Res 15(3):gmr-15038569
Kohli N, Al-Delfi IR, Snow M, Sakamoto T, Miyazaki T, Nakajima H, Uchida K, Johnson WE (2019) CD271-selected mesenchymal stem cells from adipose tissue enhance cartilage repair and are less angiogenic than plastic adherent mesenchymal stem cells. Sci Rep 9(1):1–12
Prasadam I, Akuien A, Friis TE, Fang W, Mao X, Crawford RW, Xiao Y (2018) Mixed cell therapy of bone marrow-derived mesenchymal stem cells and articular cartilage chondrocytes ameliorates osteoarthritis development. Lab Invest 98(1):106–116
Knuth CA, Kiernan CH, Palomares Cabeza V, Lehmann J, Witte-Bouma J, ten Berge D, Brama PA, Wolvius EB, Strabbing EM, Koudstaal MJ (2018) Isolating pediatric mesenchymal stem cells with enhanced expansion and differentiation capabilities. Tissue Eng C 24(6):313–321
Daly AC, Freeman FE, Gonzalez-Fernandez T, Critchley SE, Nulty J, Kelly DJ (2017) 3D bioprinting for cartilage and osteochondral tissue engineering. Adv Healthc Mater 6(22):1700298
Wang Y, Yu D, Liu Z, Zhou F, Dai J, Wu B, Zhou J, Heng BC, Zou XH, Ouyang H (2017) Exosomes from embryonic mesenchymal stem cells alleviate osteoarthritis through balancing synthesis and degradation of cartilage extracellular matrix. Stem Cell Res Ther 8(1):189
Mianehsaz E, Mirzaei HR, Mahjoubin-Tehran M, Rezaee A, Sahebnasagh R, Pourhanifeh MH, Mirzaei H, Hamblin MR (2019) Mesenchymal stem cell-derived exosomes: a new therapeutic approach to osteoarthritis? Stem Cell Res Ther 10(1):340
Miyaki S, Lotz MK (2018) Extracellular vesicles in cartilage homeostasis and osteoarthritis. Curr Opin Rheumatol 30(1):129
Liu X, Yang Y, Li Y, Niu X, Zhao B, Wang Y, Bao C, Xie Z, Lin Q, Zhu L (2017) Integration of stem cell-derived exosomes with in situ hydrogel glue as a promising tissue patch for articular cartilage regeneration. Nanoscale 9(13):4430–4438
Mobasheri A (2019) Future cell and gene therapy for osteoarthritis (OA): potential for using mammalian protein production platforms, irradiated and transfected protein packaging cell lines for over-production of therapeutic proteins and growth factors. Cell Biol Transl Med 8:17–31
Acknowledgements
The authors gratefully acknowledge DattMediproducts Pvt. Ltd. for supporting the work and providing the space for research work. This work did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) do not have any conflicts of interest relevant to this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kakkar, A., Singh, A., Saraswat, S.K. et al. Cartilage repair using stem cells & biomaterials: advancement from bench to bedside. Mol Biol Rep 47, 8007–8021 (2020). https://doi.org/10.1007/s11033-020-05748-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-020-05748-1