Abstract
Serotoninergic system is one of the most important neurotransmission systems investigated in the field of psychiatry. Extensive evidence reveals how alterations of this system, and especially of the SLC6A4 gene, may be associated with psychiatric disorders. In this study we aimed to evaluate the pleiotropic nature of SLC6A4 alterations and their association with the overall risk of brain diseases rather than disorder-specific. SLC6A4 variants, namely 5HTTLPR, STin2, rs2066713, rs25531, rs4251417, rs6354 and rs7224199 were investigated in 4 independent cohorts of subjects with specific psychiatric disorders, including Alcohol dependence disorder (ALC), Alzheimer disease (ALZ), Schizophrenia (SCZ) and Bipolar disorder (BPD). Other variables (biochemical parameters and Psychiatric scales scores) were also tested for association. SLC6A4 polymorphisms are not associated with the risk of developing major psychiatric disorders (SCZ and BPD); however some signals were detected in ALC (HTTLPR pd = 9.25 × 10−03, pr = 7.24 × 10−03; rs2066713 pd = 6.35 × 10−08; rs25531 pd = 2.95 × 10−02; rs4251417 pd = 2.46 × 10−03), and ALZ (rs6354 pr = 1.22 × 10−02; rs7224199 pd = 1.00 × 10−08, pr = 2.65 × 10−02) cohorts. Some associations were also observed on exploratory analyses. Our findings did not reveal any major influence on SCZ and BPD development; On the other hand, some alteration of the SLC6A4 sequence were associated with an increased risk of ALC and ALZ disorders, suggesting common pathways. The results of this study should be carefully interpreted since it suffers of some inherent limitations (e.g. cohort size, slight ethnic heterogeneity). Further analyses may provide better detail on the molecular processes behind SLC6A4 alterations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Serotoninergic system is one of the main neurotransmission systems of the Central Nervous System (CNS) where primarily innervates forebrain and midbrain structures [1]. It plays a major role in a variety of biological functions, including memory, appetite, sleep, cognition [1] and it is able to modulate Dopamine (DA) and Norepinephrine (NE) neurotransmission systems [2]. Also, affective-related behavior, self-control and emotional stability appear to be strongly modulated by this system [3, 4].
Medical research, in particular the psychiatric field, much focused on molecular processes related to the propagation and signal transduction of serotonin (5-Hydroxytryptamine or 5-HT). Indeed, the data collected in the recent years presented substantial evidence of how alterations within the serotoninergic system may increase the liability of psychiatric disorders [5,6,7,8]. Its role as modulator of drug response was also widely investigated [9,10,11].
Specific key genes were originally investigated, including the ones encoding for monoamine oxidases (MAOs), Tryptophan hydroxylases (TPHs), Serotonin receptors (5HTRs) and the serotonin transporter (SLC6A4) [12, 13]. The latter, in particular, is believed to be one of most important modulators of serotonergic neurotransmission. SLC6A4 is localized on q11.1-q12 region of chromosome 17 and it encodes for a 12 trans-membrane spanning protein belonging to the family of sodium-and-chloride-dependent solute carrier family 6—member 4. The transporter is responsible for the selective reuptake of 5-HT at nerve terminals, thus regulating the concentration of the neurotransmitter in the synaptic cleft and influencing the magnitude and duration of 5-HT signaling [14,15,16]. It also has a balancing role in 5-HT levels since it stores back 5-HT molecules in presynaptic neurons, making them readily available for further use [17].
Variations of this transporter may be correlated to a wide range of causes: alteration of its structural amminoacidic sequence, expression variations caused by defective promoters, altered methylation mechanics and other epigenetic factors, enhancer/silencer variations and many other ones may all cause alterations from the wild type structure/expression levels. Further, both genetic and epigenetic processes may be susceptible to environmental influences which further increase the difficulty of the interpretation of the results from human association analyses. Despite these issues, functional and expression variations of SLC6A4 were widely investigated for susceptibility to the risk of psychiatric disorders [18,19,20]. Interestingly, despite the presence of several inconsistent results in literature, sequence alterations within this gene were associated with the risk for more than one psychiatric disorder. The data indicates how SLC6A4, as a central hub of serotoninergic-related molecular processes, may play a pivotal role in the development of these pathologies, though several other variables may influence this role as well.
In light of these observations, the aim of our study was to test whether a set of variants within SLC6A4 may increase susceptibility to multiple psychiatric disorders and the role of specific genotypes as modulating factor of symptomatology in a series of psychiatric disorders. Multiple loci were already investigated for associations with psychiatric disorders (with heterogeneous results). A total of seven polymorphisms were ultimately chosen for investigation in this study.
Among them, an insertion-deletion polymorphism in the SLC6A4 promoter region (5-HTTLPR; rs4795541) has been associated with traits such as anxiety [21], emotional-related traits and psychiatric disorders as a whole [14]. This polymorphism consists in a variable repetition of a 20–23 base pair (bp) sequence. The two most common variants found in general population are defined as Long (L) allele with 16-repeats and Short (S) allele with 14-repeats [21]. From experimental data it was clear that the S allele causes a decreased transcriptional activity of SLC6A4, thus reducing the reuptake activity compared to the L form [21]. Some studies have also demonstrated that the presence of rs25531 G allele (a polymorphism localized in the same region of 5-HTTLPR) in combination with the 5-HTTLPR L allele (LG) results in expression levels similar to S- carriers [22]. Of note, there is some controversy in literature regarding the effect of SLC6A4 variation of expression induced by S and L alleles and disorders. Mainly, a decreased expression is related to an increased risk of psychiatric disorders [23], but several data also evidenced an opposite association [23,24,25].
An additional variant widely investigated is localized in SLC6A4 intron 2. It is named STin2 (variable number of tandem repeats or VNTR) and it consists in the repetition of a nearly identical 17 bp sequence. Previous genetic analyses evidenced two major alleles (STin2.10 and STin2.12) corresponding to 10-, or 12-repeat units, and a number of low frequency variants, with the nine-repeat units allele (STin2.9) being the most common [26]. This polymorphic VNTR region acts as a transcriptional regulator, with the 12 -repeat allele being associated with an increased SLC6A4 expression [26].
We also included in the study rs2066713, rs4251417, rs6354, rs7224199, a group of polymorphisms previously investigated by our group [9], which were chosen according to the criteria described below (see Methods sections) and to enhance the coverage of SLC6A4 gene.
Methods
Cohorts
For the present study, seven samples with Caucasian ancestry, previously recruited in the context of other studies, were analyzed. The subjects were grouped according to the psychiatric disorders and were separately tested for association with SLC6A4 polymorphisms.
Alcohol dependence disorder (ALC)
An Italian cohort (64 Subjects and 32 Healthy Controls) and a Greek cohort (105 Subjects and 117 Healthy Controls) were recruited for this group. The criteria for inclusion are described elsewhere [27]. Briefly, to be included in the study patients had to fulfill the DSM-IV (Diagnostic and Statistical Manual of mental disorders) diagnostic criteria for alcohol abuse/dependence—“primary alcoholism” and to give full voluntary consent to the study. Other inclusion criteria were: no recent alcohol intake, absence of serious physical illness, absence of other drug abuse, absence of DSM-IV axis I co-morbidity. Patients and their relatives were enrolled in two centres (1) the Drug and Alcohol Addiction Clinic of the Athens University Psychiatric Clinic at the Eginition Hospital in Athens, Greece. (2) the Policlinic Institute “A. Gemelli”—IRCCS, Università Cattolica del Sacro Cuore in Rome, Italy.
Alzheimer disease (ALZ)
An Italian cohort (59 Subjects and 30 Healthy Controls) and a Greek cohort (94 Subjects and 127 Healthy Controls) were recruited for this group. Details on these cohorts were already described in previous studies [28, 29]. Regarding the Greek cohort, subjects were assessed with of the mini-mental state examination (MMSE) [30], the cornell scale for depression in dementia (CSDD) [31], the neuropsychiatric inventory (NPI) [32], Alzheimer’s disease consensus—activity of daily living (ADCS-ADL) and clinical dementia rating (CDR) scale [33]. Patients of the Italian cohort were recruited among the subjects recruited for the GIGAS_LOAD project. All participants were assessed through the administration of the Cambridge Examination for Mental Disorders of Elderly Persons—Revised (CAMDEX-R) [34].
Bipolar disorder (BPD)
An Italian cohort (120 Subjects and 128 Healthy Controls) and a Spanish cohort (135 Subjects) were recruited for this group. For the Spanish cohort, BPD out-patients were enrolled in a naturalistic cohort study by the Hospital Clinic of Barcelona, in Barcelona, Spain. Inclusion criteria were a diagnosis of Bipolar Disorder (type I or II) according to DSM-IV-TR criteria and age of at least 18 years. Subjects were assessed through the semi-structured interviews for Axis I disorders according to DSM-IV-TR criteria (SCID I). Italian subjects were enrolled if they met DSM-IV criteria for a diagnosis of BD type I/II. Patients of the Italian cohort were recruited in two national psychiatric centers: (1) the Department of Biomedical and NeuroMotor Sciences, Bologna University. (2) the Psychiatric Unit of the University of Foggia, Italy. Further details are described elsewhere [35].
Schizophrenia (SCZ)
An Italian cohort (209 Subjects and 105 Healthy Controls) of SCZ subjects was included in this study as the SCZ cohort. Subjects that met the criteria of schizophrenia according to DSM-IV manual were recruited (1) among psychiatric inpatients of “San Raffaele Villa dei Fiori” facility, Rome, Italy, (2) by the Mental Health Department of ASL Roma 1 and (3) by the Psychiatric Unit, Department of Psychiatry, University of Bologna, Italy. Exclusion criteria were the presence of severe medical conditions or moderate to severe dementia. Clinical and demographic characteristics of patients were assessed at the recruitment. Details on the cohorts were described elsewhere [35].
Healthy control
Healthy subjects were recruited as controls in all of the centers involved in the study (controls divided between the cohorts, with partial overlap). No significant differences in genetic distributions was observed within the five control cohorts. All subjects were included in the study only if they did not present any neurologic/psychiatric disease history or abnormal physical examinations.
All subjects and controls signed written informed consent and all protocols were approved by the local ethical committees as described in previous papers on the same cohorts referenced above.
Selection of polymorphisms
The following criteria were applied to select polymorphisms: (1) literature evidence of involvement with psychiatric disorders (2) reported prevalence of at least 5% for the variant allele among Caucasians (data from http://hapmap.ncbi.nlm.nih.gov/); and (3) availability of a validated assay in the laboratories. The list of genotyped polymorphisms is shown in Table 1. For each polymorphism is reported the wild type and the alternative allele. Their positions on the gene are reported in Fig. 1.
Genomic DNA was purified with an automated workstation (Maxwell, Promega, Fitchburg, MA, USA) and checked for quality with spectrophotometry (NanoDrop, Thermo Scientific). Genotyping was performed using (1) restriction fragment length polymorphism, (2) allele-specific oligonucleotide and melting curve analysis on Applied BioSystems 7500 Real-Time PCR system (Thermo Fisher Scientific Inc., Waltham, MA, USA) and (3) High-throughput genotyping with the MassARRAY System (Agena Bioscience Inc., Hamburg, Germany). Genotyping was performed according to the manufacturer’s standard protocols. Forward and reverse primers’ sequences are available upon request.
Outcomes under investigation
The main aim of the study was to test the associations between the investigated polymorphisms and the risk of developing a psychiatric disorder. Analyses were performed independently for each disease. Also, each subgroup was separately investigated as exploratory analysis in order to evaluate possible differences between populations. Finally, for each cohort further exploratory analyses were performed on the available biochemical parameters and psychiatric scales scores (for details please refer to Supplementary Table 1).
Statistical analysis
Haploview3.2 was used to test Hardy–Weinberg Equilibrium(HWE) [36]. The effect of markers was tested through logistic regression models in all groups to evaluate the risk of developing a psychiatric disorder. Dominant and Recessive models were tested in the cohorts and their subgroups. Further tests were performed on the additional variables (Supplementary Table 1) where available. The combination of 5-HTTLPR and rs25531 was investigated by comparing LA/LA carriers versus other haplotypes as previously suggested [37]. Covariates were selected according to their impact on outcomes. IBM SPSS package (http://www.ibm.com/analytics/us/en/technology/spss/) was used for the analyses.
In single marker analysis each group provided enough power (0.80) to detect risk alleles with odds ratios ≥ 1.89, ≥ 1.90, ≥ 1.79 and ≥ 1.90 for ALC, ALZ, BPD and SCZ respectively. The power was calculated through G*Power software v3.1.9.2.
To limit the probability of false positive finding we applied Bonferroni correction to our statistical tests. We took in consideration the number of SNPs tested for significance (7) and the number of datasets analyzed (7). Significance was considered for \(p < \frac{0.05}{7 \times 7} = 0.00102\).
Results
Details of the cohorts under investigation are summarized in Supplementary Table 2. The genotypic distribution and results of HWE testing are reported in Supplementary Table 3.
Primary outcomes
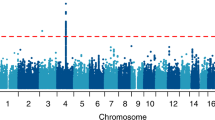
According to our analyses, in all cohorts SLC6A4 polymorphisms showed some influence in the risk of developing psychiatric disorders. The charts below report the effects (indicated as odd ratios) that SLC6A4 polymorphisms have on the risk. Both dominant and recessive model data have been reported. Details of these analyses and the results obtained from the diagnostic groups are reported in Supplementary Table 4 (Charts 1, 2).
Dominant model. Association results on the risk. In the above diagram are showed the results of association tests under a dominant model construct. In this model the presence of at least one mutated (-) allele was tested against the homozygous wild-type genotype (wt/wt). The Odds Ratios (plus Confidence Intervals) are reported on the X axis in a logarithmic scale. Data on the right of Y axis indicates causative effects toward the risk. Data on the left indicates protective effects. An * indicates the significant results from our analyses. The pValues are here summarized: ALC (HTTLPR pd = 9.25 × 10−03; rs2066713 pd = 6.35 × 10−08; rs25531 pd = 2.95 × 10−02; rs4251417 pd = 2.46 × 10−03) and ALZ (rs7224199 pd = 1.00 × 10−08). For more details please refer to Supplementary Table 4
Recessive model. Association results on the risk. In the above diagram are showed the results of association tests under a recessive model construct. The -/- genotype was tested against wt/- and wt/wt genotypes. The Odds Ratios (plus Confidence Intervals) are reported on the X axis in a logarithmic scale. Data on the right of Y axis indicates causative effects toward the risk. Data on the left indicates protective effects. An * indicates the significant results from our analyses. The pValues are here summarized: ALC (HTTLPR pr = 7.24 × 10−03; HTTLPR × rs25531 pr = 7.85 × 10−03) and ALZ (rs6354 pr = 1.22 × 10−02; rs7224199 pr = 2.65 × 10−02). For more details please refer to Supplementary Table 4
Secondary outcomes
The exploratory outcomes tested for association showed some significant data. In particular, rs7224199 genotype seems to be correlated with blood levels of Triglycerides in Greek Alcoholic subjects (Recessive model pr = 2.17 × 10−03, Genotypic pg = 6.97 × 10−03).
Greek Alzheimer subjects have shown variations of B12 levels related to rs4251417 genotype (Recessive model pr = 2.18 × 10−03, Genotypic pg = 1.06 × 10−02); of LPA levels related to rs7224199 genotype (Recessive model pr = 5.07 × 10−05, Genotypic pg = 1.79 × 10−04).
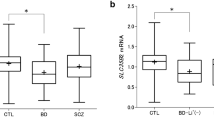
The BPD cohort revealed associations between Hamilton depression rating scale (HDRS) scores and HTTLPR genotype (Dominant model pd = 1.03 × 10−02, Genotypic pg = 2.11 × 10−03). In the same cohort young mania rating scale (YMRS) scores resulted modulated by rs7224199 genotype (Recessive model pr = 6.82 × 10−04, Genotypic pg = 4.11 × 10−04). No other significant associations were found in the cohorts under analysis. Further details are reported in Supplementary Table 5.
Discussion
Overview of findings
The serotonin transporter gene (SLC6A4) has been subject to relevant interest, since the central role of the coded protein in the serotonin neuronal activity [38], especially in relation to psychiatric disorders. According to our results, several of the polymorphisms investigated resulted having some modulatory effects.
HTTLPR polymorphism was associated with the risk of developing Alcohol dependence in the cohort under analysis. In particular the significance of associations under both dominant and recessive models, indicated that only one S allele is needed to significantly increase the risk compared to a wild type genotype and two S allele further increase the possibility. Taking into consideration the combination with rs25531, only the recessive model maintained a significant association. Of note, in further exploratory analyses on the greek cohort after stratification in early and late onset subgroups this variant showed no significant associations (data not shown). While the loss of significance may be attributed to the limited sample size (49 and 56 subjects respectively for early and late subgroups), it may also be related to the different genetic architectures behind the two manifestations of Alcohol dependence.
The expression of the 5-HTT gene is influenced by a 44 bp insertion/deletion polymorphism in its promoter region (5-HTTLPR). In vitro studies have shown that the long (L) 5-HTTLPR variant led to a higher transcriptional activity compared to the short (S) variant [39]. It is also interesting to note that the presence of the S allele may impact on the development of cerebral structures, like amygdala, important in the emotion processing [40].
Overall this result suggests that a decreased concentration of SLC6A4 gene products (S alleles reduces transcription levels of SLC6A4 mRNA) concur to increase the risk of Alcohol dependence liability, as supported by some literature evidence ([41] and references therein). It has to be noted, though, that some large meta analyses reported no association for this variants with Alcohol dependence disorder [41], as such the data should be carefully evaluated.
Of note, according to our exploratory analyses, HTTLPR genotype can significantly influence depressive symptoms severity (HDRS scale) in the BPD cohort. S carriers showed the lower scores compared to L carriers; the lowest scores were evidenced in heterozygous subjects.
Rs2066713 A allele has shown an increased risk for ALC (dominant model). No data was present in literature regarding the association of this SNPs and the this disorder, however Yang et al. found rs2066713 being associated to another substance dependence-related disorder (nicotine) [42]. In silico sequence analyses through Human Splicing Finder software [43] revealed that the A allele breaks a potential consensus sequence for an Exonic Splicing Silencer (Motif 3—TCTCCCAA). Consequently, the A allele may alter the regulation mechanics of SLC6A4 mRNA maturation. However, no related experimental data was found in literature.
Regarding rs4251417, we found some associations in the ALC group. In particular, the T allele was significantly more frequent on controls rather than ALC subjects. No correlations were found in literature between rs4251417 and the investigated disorders. However, the potential capacity of rs4251417 genotype to influence DNA methylation in SLC6A4 has been reported, thus impacting in the overall expression of the gene [44]. However, in silico analysis of the sequence with CpG island finder software (http://dbcat.cgm.ntu.edu.tw/) did not evidence any methylation focal point around the mutation. The in silico analysis for splicing alterations revealed that a G > A change of rs4251417 cause the creation of a branch point site. Also, the change causes the destruction of the consensus sequence for the Exonic Splicing Enhancer SRp40 protein. These alterations, though, do not seem to be sufficent to cause a significant impact on splicing. Of note, in the ALZ Greek subgroup, rs4251417 genotype was associated with vitamin B12 concentration variations in blood (C carriers showed lower values compared to TT carriers).
Recessive model association tests evidenced a correlation between rs6354 GG genotype and the risk of Alzheimer disease. Though in silico analysis (CpG island finder) did not evidence any methylation focal point, literature data suggest a possible role of rs6354 in the regulation of DNA methylation in SLC6A4 sequence, thus impacting in the overall expression of the gene [44]. In silico analysis on possible splicing alterations related to this polymorphism revealed that the T > G change causes the creation of a branch point site. Also, G carriers have a consensus sequence for an Exonic Splicing Silencer (Motif 3—TCTCCCAA). However, given the localization of the polymorphism and the strength of these alterations, rs6354 genotype does not seem to cause a significant impact on splicing.
Rs7224199 T allele (dominant model) and TT genotype (recessive model) have a protective effect against ALZ. This trend (but not significant overall) could also be observed in the other disorders. According to exploratory analyses, rs7224199 may also influence the severity of manic symptoms in BPD subjects, with TT carriers exhibiting higher scores compared to G carriers. Of note, Biochemical parameters like Triglycerides and LPA in Greek ALC and ALZ subgroups, respectively were found different between subjects and controls. In silico analysis on possible splicing alterations related to this polymorphism revealed that the G > T change cause the loss of a splice site and of an Exonic Splicing Silencer consensus sequence. According to the software, it also introduces an Exonic Splicing Enhancer consensus sequence. However, these changes do not seem to cause a significant impact on splicing. Also, no role on methylation mechanic was proposed for this polymorphism.
No associations were observed for STin2 in the primary analyses. STin2 is localized in a enhancing region, whose activity/efficiency is significantly correlated with the number of repeats within STin2. In particular, it was demonstrated that the higher the number of repeats, the more enhancing factors are recruited in this region. As such, the 2.12 allele translates in a higher expression activity of SLC6A4 [26]. Despite this, this change in expression levels does not seem to be enough to influence risk in our cohorts.
Limitations
The results of this study should be carefully interpreted since limited sample size, slight ethnic heterogeneity, and deviation from HWE of some SNPs which may have acted as confounding factors for the analyses. It has to be noted that deviation from HWE seems to be a common occurrence for SLC6A4 polymorphisms [9, 45]. We did not extensively investigate the genetic structure of SLC6A4, as such our data does not consider the presence/absence of other variants.
Conclusion
Variants within SLC6A4 sequence were found to be correlated mainly with ALC and ALZ disorders. We observed a correlation between HTTLPR S allele with an increased risk of developing an Alcohol dependence, in line with some literature data. No correlations were found between HTTLPR variants and ALZ. This lack of association is also supported in literature [46]. About the other variants, rs2066713 was associated with the risk of Alcohol dependence and rs6354 with Alzheimer. Also, rs7224199 variations seemed to play a protective role against Alzheimer.
The central serotonergic functioning is correlated of with impulsivity and aggression [47], moreover, the level of 5-HT functioning may impact the behavioral effect of alcohol as observed in literature data [48].
According to the data, SLC6A4 may indeed play a role in the molecular processes correlated with ALC and ALZ, but, at least in our cohorts, this role cannot be extended to all psychiatric disorders. Indeed, despite the amount of support in literature, we failed to correlate SLC6A4 alterations with any of the major psychiatric disorders (BPD and SCZ). Although the limited sample size could explain the lack of associations, recent works described the possibility of a more limited role for this gene compared to what we were used to know by literature [49]. It is possible for this gene to be capable of influencing the risk of psychiatric disorders, but only in specific genetic subsets of the population. Thus, more specific criteria for recruitment should be taken in consideration, in order to avoid the heterogeneity typical of large studies, as evidenced by Cai et al. [50]. In particular, with respect to alcohol use disorder, a stratification in early and late onset subgroups may better define the role of SLC6A4 variants, since the significance may vary among the two groups [51]. Further analyses may help to better detail the molecular processes behind SLC6A4 variants, because it is not enough to explain the complex molecular picture behind these disorders. As such, further interactions with other key element should be considered for future investigations.
Change history
22 January 2020
The following authors have double affiliations: <Emphasis Type="Bold">Stefania Boccia, Marco Di Nicola</Emphasis> and they should read
22 January 2020
The following authors have double affiliations: Stefania Boccia, Marco Di Nicola and they should read
References
Fuller RW (1996) Mechanisms and functions of serotonin neuronal systems: opportunities for neuropeptide interactions. Ann NY Acad Sci 780:176–184
Hensler JG, Artigas F, Bortolozzi A, Daws LC, De Deurwaerdere P, Milan L, Navailles S, Koek W (2013) Catecholamine/serotonin interactions: systems thinking for brain function and disease. Adv Pharmacol 68:167–197
Lesch KP, Merschdorf U (2000) Impulsivity, aggression, and serotonin: a molecular psychobiological perspective. Behav Sci Law 18(5):581–604
Linnoila VM, Virkkunen M (1992) Aggression, suicidality, and serotonin. J Clin Psychiatry 53(Suppl):46–51
Dell’Osso L, Carmassi C, Mucci F, Marazziti D (2016) Depression, serotonin and tryptophan. Curr Pharm Des 22(8):949–954
Mahmood T, Silverstone T (2001) Serotonin and bipolar disorder. J Affect Disord 66(1):1–11
Cross AJ (1990) Serotonin in Alzheimer-type dementia and other dementing illnesses. Ann NY Acad Sci 600:405–415 discussion 415-407
Gorwood P, Lanfumey L, Hamon M (2004) Alcohol dependence and polymorphisms of serotonin-related genes. Med Sci (Paris) 20(12):1132–1138
Calabro M, Fabbri C, Crisafulli C, Albani D, Forloni G, Kasper S, Sidoti A, Velardi E, Zohar J, Juven-Wetzler A, Souery D, Montgomery S, Mendlewicz J, Serretti A (2018) The serotonin transporter and the activity regulated cytoskeleton-associated protein genes in antidepressant response and resistance: 5-HTTLPR and other variants. Hum Psychopharmacol 33(6):e2682
Coplan JD, Gopinath S, Abdallah CG, Berry BR (2014) A neurobiological hypothesis of treatment-resistant depression - mechanisms for selective serotonin reuptake inhibitor non-efficacy. Front Behav Neurosci 8:189
Hofer P, Schosser A, Calati R, Serretti A, Massat I, Kocabas NA, Konstantinidis A, Mendlewicz J, Souery D, Zohar J, Juven-Wetzler A, Montgomery S, Kasper S (2016) The impact of serotonin receptor 1A and 2A gene polymorphisms and interactions on suicide attempt and suicide risk in depressed patients with insufficient response to treatment–a European multicentre study. Int Clin Psychopharmacol 31(1):1–7
Rotondo A, Mazzanti C, Dell’Osso L, Rucci P, Sullivan P, Bouanani S, Gonnelli C, Goldman D, Cassano GB (2002) Catechol o-methyltransferase, serotonin transporter, and tryptophan hydroxylase gene polymorphisms in bipolar disorder patients with and without comorbid panic disorder. Am J Psychiatry 159(1):23–29
Ho LW, Furlong RA, Rubinsztein JS, Walsh C, Paykel ES, Rubinsztein DC (2000) Genetic associations with clinical characteristics in bipolar affective disorder and recurrent unipolar depressive disorder. Am J Med Genet 96(1):36–42
Bevilacqua L, Goldman D (2011) Genetics of emotion. Trends Cogn Sci 15(9):401–408
Thompson MD, Kenna GA (2016) Variation in the serotonin transporter gene and alcoholism: risk and response to pharmacotherapy. Alcohol Alcohol 51(2):164–171
Nomura M, Kaneko M, Okuma Y, Nomura J, Kusumi I, Koyama T, Nomura Y (2015) Involvement of serotonin transporter gene polymorphisms (5-HTT) in impulsive behavior in the japanese population. PLoS ONE 10(3):e0119743
Albani D, Prato F, Tettamanti M, Lovati C, Galimberti D, Restelli I, Mariani C, Quadri PL, Scarpini E, Lucca U, Forloni G (2009) The serotonin transporter promoter polymorphic region is not a risk factor for Alzheimer’s disease related behavioral disturbances. J Alzheimers Dis 18(1):125–130
Prasad HC, Steiner JA, Sutcliffe JS, Blakely RD (2009) Enhanced activity of human serotonin transporter variants associated with autism. Philos Trans R Soc Lond B Biol Sci 364(1514):163–173
Rao S, Leung CS, Lam MH, Wing YK, Waye MM, Tsui SK (2017) Resequencing three candidate genes discovers seven potentially deleterious variants susceptibility to major depressive disorder and suicide attempts in Chinese. Gene 603:34–41
Shi M, Hu J, Dong X, Gao Y, An G, Liu W, Chen L, Sun X (2008) Association of unipolar depression with gene polymorphisms in the serotonergic pathways in Han Chinese. Acta Neuropsychiatr 20(3):139–144
Lesch KP, Bengel D, Heils A, Sabol SZ, Greenberg BD, Petri S, Benjamin J, Muller CR, Hamer DH, Murphy DL (1996) Association of anxiety-related traits with a polymorphism in the serotonin transporter gene regulatory region. Science 274(5292):1527–1531
Shiroma PR, Drews MS, Geske JR, Mrazek DA (2014) SLC6A4 polymorphisms and age of onset in late-life depression on treatment outcomes with citalopram: a sequenced treatment alternatives to relieve depression (STAR*D) report. Am J Geriatr Psychiatry 22(11):1140–1148
Kenna GA, Roder-Hanna N, Leggio L, Zywiak WH, Clifford J, Edwards S, Kenna JA, Shoaff J, Swift RM (2012) Association of the 5-HTT gene-linked promoter region (5-HTTLPR) polymorphism with psychiatric disorders: review of psychopathology and pharmacotherapy. Pharmacogenom Personal Med 5:19–35
Thompson MD, Kenna GA (2016) Variation in the serotonin transporter gene and alcoholism: risk and response to pharmacotherapy. Alcohol Alcohol (Oxford, Oxfordshire) 51(2):164–171
Stacey D, Cohen-Woods S, Toben C, Arolt V, Dannlowski U, Baune BT (2013) Evidence of increased risk for major depressive disorder in individuals homozygous for the high-expressing 5-HTTLPR/rs25531 (L(A)) allele of the serotonin transporter promoter. Psychiatr Genet 23(5):222–223
MacKenzie A, Quinn J (1999) A serotonin transporter gene intron 2 polymorphic region, correlated with affective disorders, has allele-dependent differential enhancer-like properties in the mouse embryo. Proc Natl Acad Sci USA 96(26):15251–15255
Drago A, Liappas I, Petio C, Albani D, Forloni G, Malitas P, Piperi C, Politis A, Tzavellas EO, Zisaki KK, Prato F, Batelli S, Polito L, De Ronchi D, Paparrigopoulos T, Kalofoutis A, Serretti A (2009) Epistasis between IL1A, IL1B, TNF, HTR2A, 5-HTTLPR and TPH2 variations does not impact alcohol dependence disorder features. Int J Environ Res Public Health 6(7):1980–1990
Serretti A, Olgiati P, Politis A, Malitas P, Albani D, Dusi S, Polito L, De Mauro S, Zisaki A, Piperi C, Liappas I, Stamouli E, Mailis A, Atti AR, Morri M, Ujkaj M, Batelli S, Forloni G, Soldatos CR, Papadimitriou GN, De Ronchi D, Kalofoutis A (2009) Lack of association between interleukin-1 alpha rs1800587 polymorphism and Alzheimer’s disease in two independent European samples. J Alzheimers Dis 16(1):181–187
De Ronchi D, Berardi D, Menchetti M, Ferrari G, Serretti A, Dalmonte E, Fratiglioni L (2005) Occurrence of cognitive impairment and dementia after the age of 60: a population-based study from Northern Italy. Dement Geriatr Cogn Disord 19(2–3):97–105
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3):189–198
Alexopoulos GS, Abrams RC, Young RC, Shamoian CA (1988) Cornell scale for depression in dementia. Biol Psychiatry 23(3):271–284
Cummings JL, Mega M, Gray K, Rosenberg-Thompson S, Carusi DA, Gornbein J (1994) The Neuropsychiatric Inventory: comprehensive assessment of psychopathology in dementia. Neurology 44(12):2308–2314
Morris JC (1993) The clinical dementia rating (cdr): current version and scoring rules. Neurology 43(11):2412–2414
Roth M, Tym E, Mountjoy CQ, Huppert FA, Hendrie H, Verma S, Goddard R (1986) CAMDEX. A standardised instrument for the diagnosis of mental disorder in the elderly with special reference to the early detection of dementia. Br J Psychiatry 149:698–709
Corponi F, Bonassi S, Vieta E, Albani D, Frustaci A, Ducci G, Landi S, Boccia S, Serretti A, Fabbri C (2019) Genetic basis of psychopathological dimensions shared between schizophrenia and bipolar disorder. Prog Neuropsychopharmacol Biol Psychiatry 89:23–29
Barrett JC, Fry B, Maller J, Daly MJ (2005) Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics 21(2):263–265
Porcelli S, Fabbri C, Serretti A (2012) Meta-analysis of serotonin transporter gene promoter polymorphism (5-HTTLPR) association with antidepressant efficacy. Eur Neuropsychopharmacol 22(4):239–258
Ho PS, Shih MC, Ma KH, Huang WS, Ho KK, Yen CH, Lu RB, Huang SY (2011) Availability of the serotonin transporter in patients with alcohol dependence. World J Biol Psychiatry 12(2):134–142
Wendland JR, Martin BJ, Kruse MR, Lesch KP, Murphy DL (2006) Simultaneous genotyping of four functional loci of human SLC6A4, with a reappraisal of 5-HTTLPR and rs25531. Mol Psychiatry 11(3):224–226
Kobiella A, Reimold M, Ulshofer DE, Ikonomidou VN, Vollmert C, Vollstadt-Klein S, Rietschel M, Reischl G, Heinz A, Smolka MN (2011) How the serotonin transporter 5-HTTLPR polymorphism influences amygdala function: the roles of in vivo serotonin transporter expression and amygdala structure. Transl Psychiatry 1:e37
Villalba K, Attonito J, Mendy A, Devieux JG, Gasana J, Dorak TM (2015) A meta-analysis of the associations between the SLC6A4 promoter polymorphism (5HTTLPR) and the risk for alcohol dependence. Psychiatr Genet 25(2):47–58
Yang J, Li MD (2014) Association and interaction analyses of 5-HT3 receptor and serotonin transporter genes with alcohol, cocaine, and nicotine dependence using the SAGE data. Hum Genet 133(7):905–918
Desmet FO, Hamroun D, Lalande M, Collod-Beroud G, Claustres M, Beroud C (2009) Human splicing finder: an online bioinformatics tool to predict splicing signals. Nucleic Acids Res 37(9):e67
Lam D, Ancelin ML, Ritchie K, Freak-Poli R, Saffery R, Ryan J (2018) Genotype-dependent associations between serotonin transporter gene (SLC6A4) DNA methylation and late-life depression. BMC Psychiatry 18(1):282
Janssen PK, Olivier B, Zwinderman AH, Waldinger MD (2014) Measurement errors in polymerase chain reaction are a confounding factor for a correct interpretation of 5-HTTLPR polymorphism effects on lifelong premature ejaculation: a critical analysis of a previously published meta-analysis of six studies. PLoS ONE 9(3):e88031
Yamazaki K, Yoshino Y, Mori T, Okita M, Yoshida T, Mori Y, Ozaki Y, Sao T, Iga J, Ueno S (2016) Association study and meta-analysis of polymorphisms, methylation profiles, and peripheral mrna expression of the serotonin transporter gene in patients with alzheimer’s disease. Dement Geriatr Cogn Disord 41(5–6):334–347
Dolan M, Anderson IM, Deakin JF (2001) Relationship between 5-HT function and impulsivity and aggression in male offenders with personality disorders. Br J Psychiatry 178:352–359
LeMarquand D, Pihl RO, Benkelfat C (1994) Serotonin and alcohol intake, abuse, and dependence: findings of animal studies. Biol Psychiatry 36(6):395–421
Border R, Johnson EC, Evans LM, Smolen A, Berley N, Sullivan PF, Keller MC (2019) No support for historical candidate gene or candidate gene-by-interaction hypotheses for major depression across multiple large samples. Am J Psychiatry 176(5):376–387
Cai N, Kendler KS, Flint J (2018) Minimal phenotyping yields GWAS hits of low specificity for major depression. BioRxiv. https://doi.org/10.1101/440735
Chen YC, Prescott CA, Walsh D, Patterson DG, Riley BP, Kendler KS, Kuo PH (2011) Different phenotypic and genotypic presentations in alcohol dependence: age at onset matters. J Stud Alcohol Drugs 72(5):752–762
Acknowledgements
We thank all patients who gave their consent for the analysis of their data.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors were actively involved in the design of the study, the analytical method of the study, the selection and review of all scientific content. All authors had full editorial control during the writing of the manuscript and finally approved it.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or conflict with that can be associated with the subject matter discussed in this manuscript.
Ethical approval
The authors declare that all procedures followed were approved by the national ethical committee. Further, all patients gave their written consent for the analysis of their data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Calabrò, M., Mandelli, L., Crisafulli, C. et al. Psychiatric disorders and SLC6A4 gene variants: possible effects on alcohol dependence and alzheimer’s disease. Mol Biol Rep 47, 191–200 (2020). https://doi.org/10.1007/s11033-019-05119-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-019-05119-5