Abstract
The search for new compounds effective against Mycobacterium tuberculosis is still a priority in medicine. The evaluation of microorganisms isolated from non-conventional locations offers an alternative to look for new compounds with antimicrobial activity. Endophytes have been successfully explored as source of bioactive compounds. In the present work we studied the nature and antimycobacterial activity of a compound produced by Streptomyces scabrisporus, an endophyte isolated from the medicinal plant Amphipterygium adstringens. The active compound was detected as the main secondary metabolite present in organic extracts of the streptomycete and identified by NMR spectroscopic data as steffimycin B (StefB). This anthracycline displayed a good activity against M. tuberculosis H37Rv ATCC 27294 strain, with MIC100 and SI values of 7.8 µg/mL and 6.42, respectively. When tested against the rifampin mono resistant M. tuberculosis Mtb-209 pathogen strain, a better activity was observed (MIC100 of 3.9 µg/mL), suggesting a different action mechanism of StefB from that of rifampin. Our results supported the endophyte Streptomyces scabrisporus as a good source of StefB for tuberculosis treatment, as this anthracycline displayed a strong bactericidal effect against M. tuberculosis, one of the oldest and more dangerous human pathogens causing human mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to WHO, tuberculosis (TB) remains a major disease in terms of mortality and morbidity. Almost one-third of the human population is infected with Mycobacterium tuberculosis, but less than 10% of those infected evolve to disease. In the remaining 90% of infected individuals, estimated as two billion persons worldwide, the disease remains in a latent state [1].
The career of anti-TB-drug discovery flourished in the mid-twentieth century with the finding of the first-line drugs: isoniazid, followed for rifampin in 1963 and continued later in 2017 with the development of new anti-TB-drugs [2]. Kumar et al. [3] summarize all new anti-tuberculosis agents based in new structural aspects, and reported 35 new structural classes, including benzothiazoles, coumarins, dihydropyridines, isoxazoles, mycobactin–artimisinin conjugates, and thiourea derivatives, among others.
Mycobacterium tuberculosis can develop resistance or multidrug-resistance to the antimicrobial drugs used for the disease treatment. Indeed, the WHO estimates that until 2015, 480,000 people worldwide have developed multidrug-resistant tuberculosis (MDR-TB) and 240,000 died in 2016. These facts increase the relevance for searching new antibiotics, particularly for those combating pathogenic drug-resistant strains like Mycobacterium tuberculosis [4].
The main sources of antibiotics are still natural products [5]. Among them, some microorganisms like actinobacteria, especially those from the genus Streptomyces, represent the most important source of these compounds. Indeed, about 80% of the known antibiotics come from this genus whose producing strains have been isolated mainly from soil [6]. On the contrary, the search for secondary metabolites from endophytes, began more recently and have shown to be a good source of bioactive substances [7], in special those isolated from medicinal plants [8].
One of the most used trees in traditional Mexican herbalism is Amphipterygium adstringens, which represents the main anti-ulcer remedy and has antitumor, antimicrobial, and anti-inflammatory activities [9]. Although widely used in rural areas of Mexico, as far as we know, there are not specific products obtained from A. adstringens approved by the FDA or any other agency.
Continuing our search on bioactive compounds from endophytes of A. adstringens, the aim of this study was to investigate the antimycobacterial activity and chemical nature of an organic extract produced as the major compound by a streptomycete isolated from this medicinal plant.
Materials and methods
Microorganisms and culture conditions
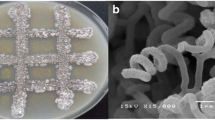
The Streptomyces sp. NF3 strain was isolated, as an endophyte from the medicinal plant Amphipterygium adstringens (Rodríguez-Peña et al. in preparation). This microorganism was chosen from other actinomycetes isolated from that tree because it exhibited the best antimicrobial activity against several Gram-positive microorganisms and Saccharomyces cerevisiae. This strain was maintained in viable conditions at the UNAM-48/WFCC (Mexico City). The plant was deposited at the National Herbarium of Mexico (specimen number 1366484). The NF3 strain was identified as Streptomyces scabrisporus from its 16S ribosomal DNA [10] and its sequence deposited in the GeneBank under the accession number KU579247. S. scabrisporus NF3 was grown in ISP-2 medium [11], supplemented with 2% CaCO3, in a 250-mL Erlenmeyer flask for 4 days at 29 °C on a rotary shaker at 180 rpm. From this culture, 250 µL were inoculated into four 1-L Erlenmeyer flasks, containing 250 mL of the same medium and cultivated for 17 days at the same temperature and shaking conditions. As reported for other streptomycetes, addition of CaCO3 to ISP-2 medium also promoted growth and antibiotic formation in this strain [12] likely due to its reported effect on cell permeability [13].
The Mycobacterium tuberculosis strains M.tb H37Rv ATCC 27294 (virulent strain used as reference), M.tb H37Ra (non-virulent strain) and a clinical virulent isolate resistant to rifampin (RMR M.tb-209), were preserved in BSL-3 conditions. For inoculum preparation, these strains were grown in 7H9-glycerol-10% ADC-0.01% tyloxapol (Sigma T8761) at 37 °C until reaching an OD of 0.4 at 600 nm. To get a workable bacterial solution, each inoculum was diluted 1:25 in 7H9-ADC 10%.
The assay organisms (Micrococcus luteus ATCC 9341, Listeria monocytogenes Scott A, Bacillus cereus ATCC 11778, Staphylococcus aureus ATCC 8855 [14] and S. aureus ATCC 25923), were kindly provided by Dr. B. García-Almendárez from Universidad Autónoma de Querétaro, México, and maintained in trypticase soy agar (BD Difco™).
Extraction and purification
After 29 days incubation, the culture broth (1-L) was centrifuged at 10,000×g for 10 min and the supernatant exhaustively extracted with hexane (HEX) and dichloromethane (DCM) until no color appeared in each extraction solvent. Extractions from supernatants and mycelia were previously tested and their effectiveness determined by TLC and bioautography assays. Under these conditions, a minor concentration (less than 5%) of the active compound was detected in the biomass. Both extracts, were evaporated to dryness under reduced pressure in a Büchi rotary evaporator R-215 coupled to the vacuum pump V-700. Afterwards, 7.5 mg of a colourless extract from HEX and 200 mg of an orange extract from DCM were obtained. From these extracts, only those from DCM showed inhibitory activity against M. luteus. The total DCM extract was poured into an open silica gel column chromatography and eluted with a dichloromethane-acetone (1:0 to 0:1) gradient. Based on their TLC pattern, seven fractions (F1 to F7) were pooled and their activity tested by bioautography against M. luteus. Among them, fraction 2 (F-2, 66 mg) exhibited the best antibacterial activity and were used for further analysis. Fraction 2 was separated on a silica gel column with a solvent system of CH2Cl2–MeOH (98:2 and 95:5) to produce eight subfractions (F2-1 to F2-8). Subfraction F-2-6 was further purified by preparative TLC, developed using CH2Cl2–MeOH (95:5), to yield compound 1.
General experimental procedures
Nuclear magnetic resonance (NMR) spectra of F-2, was taken on a Bruker AVANCE III 400 (400 MHz) spectrometer, using tetramethylsilane (TMS) as internal standard. The high-resolution mass spectrometry (HRMS) using atmospheric pressure chemical ionization (HR-APCI-MS) was performed on a Perkin-Elmer AxION DSA/TOF (Perkin-Elmer, USA). Gas chromatography mass spectrometry (GC–MS) analyses of DCM extract was performed on an Agilent 6890 N series gas chromatograph coupled to a LECO time of flight mass spectrometer detector (MS-TOF; Agilent Technology, Palo Alto, CA, USA) and fitted with a 5% diphenyl-95% dimethyl polysiloxane (20 m × 0.18 mm i.d.; 0.18 µm film thickness) capillary column (Bellefonte, PA, USA). Helium was used as the carrier gas at a constant flow of 1 mL/min. The initial column temperature (40 °C), was raised to 300 °C with a rate of 20 °C/min and maintained for 5 additional min. The ionization electron energy was 70 eV and the mass range scanned was 40–400 m/z. Injector and MS transfer were set at 300 and 250 °C, respectively. The MS fragmentation patterns were compared with those of pure compounds in the spectral database of the National Institute of Standards and Technology (NIST) [15]. Column chromatography was carried out using silica gel 60, 0.06–0.2 mm (Merck KGaA, Darmstadt, Germany). Analytical TLC was carried out on precoated Silica gel 60 F254 (Merck KGaA, Darmstadt, Germany). Other chemicals were of the highest grade available.
Preparation of compounds for biological assays
Rifampin (RIF) and stock solutions of all tested fractions were prepared in 100% dimethyl sulfoxide (DMSO) at 10 mg/mL. For REMA (resazurin microtiter assay) tests, the compounds were diluted in 7H9 medium without tyloxapol (Sigma T8761). For reference drugs, stocks of 64 µg/mL were prepared and filter sterilized with 0.22 µm membranes (Millipore; Darmstadt, Germany). All working solutions were kept refrigerated at − 20 °C until evaluation.
Cytotoxicity assays
Cytotoxicity assays were addressed using the Vero cell line (kidney of African green monkey) ATCC® CCL-81. These cells were cultured in 96 well-plates, containing RPMI 1640 medium (Gibco 31800022) supplemented with 10% of FBS (Gibco) and non-essential amino acids.
To address cytotoxicity of the extracted compounds, Vero cells were placed in the plates (103 cells per well) and incubated for 24 h at 37 °C in 100 µL RPMI medium. After incubation, the plates were washed, supplemented with new fresh medium containing different concentrations of the tested compounds and incubated for 48 h in a 5% CO2 atmosphere. Furthermore, 10 µL of 5 mg/mL MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide) (Sigma) in sterile PBS, was added to each well and incubated again for 4 h, following the Mossman [16] report. Absorbance was determined at 570 nm and cytotoxicity calculated as % Toxicity = [1 − (ABS problem/ABS control)] * 100. As control, cells without treatment were utilized.
Antimicrobial susceptibility test by REMA
Assays were addressed as described by Collins and Franzablau [17]. Outer wells of 96 well-plates, were filled with 200 µL of sterile PBS to prevent dehydration (due to 8 days incubation). RIF was used as reference drug (0.001 to 16 µg/mL serial of twofold dilutions) in each plate. As controls DMSO, DMSO + Mtb, Medium, Medium + Mtb, and the compound alone, were also included. The compounds were evaluated using a range from 0.98 to 250 µg/mL. Triplicates from all compounds were made for the different assays. The plates were incubated for 6 days, and after addition of 30 µL 0.01% resazurin (weight/volume) (Sigma Aldrich) to each of the wells, incubated for 2 additional days. Colors were visually interpreted as blue (no growth) and pink (growth). The MIC was determined in the last well in which the blue color was observed.
Selectivity index (SI)
This value was obtained using the formula SI = IC50 in Vero cells/MIC100 by REMA (https://www.akadia.com/services/ora_index_selectivity.html).
Minimal bactericidal concentration (MBC)
From those wells + compounds that produced a shift in the color after re-incubation in fresh medium, the MBC values were determined. For this purpose, 5 µL of each well was added to fresh media (195 µL) and incubated for REMA assay as previously described.
Minimal inhibitory concentration (MIC) for non-mycobacteria
The MIC assay was performed by the 96-well microdilution method using the standard CLSI (The Clinical and Laboratory Standards Institute) protocol [18]. Mueller–Hinton agar was used for this method, adjusting the inoculum to 1.5 × 108 CFU/mL (0.5 McFarland). The antibiotics tested were penicillin (10 IU) and gentamycin (590 µg/mg) (Sigma-Aldrich). The plates were incubated at 37 °C for 24 h and the bacterial growth determined by using the microplate reader at 540 nm. Assays were carried out in triplicate and repeated twice.
As reference strains the Gram-positive M. luteus, L. monocytogenes, B. cereus, and S. aureus, were utilized.
Results and discussion
Identification of the chemical compound
The DCM extract obtained from fermentations of the S. scabrisporus strain. showed inhibitory activity against M. luteus. The extract was concentrated under reduced pressure and subjected to repeated silica gel column chromatography. The subfraction F-2-6 was further refined by preparative TLC developed with CH2Cl2/MeOH (95:5), to yield compound 1 (Rf = 0.48; 16.8 mg). The unknown compound 1 was identified as steffimycin B (StefB) (Table 1) by comparing spectroscopic and spectrometric data [HRMS, 1H NMR (Fig. S1), 13C NMR (Fig. S2), HSQC (Fig. S3), HMQC (Fig. S4), COSY (Fig. S5)], with reported values [19, 20]. StefB was initially isolated from the soil microorganisms Streptomyces elgreteus [21] and Streptomyces sp. BCC27095, an actinomycete obtained from a Thailand ground [22]. Steffimycin C (StefC) was also identified in the DCM extract [C29H35O12 as determined by HR-APCI-MS 575.2134 m/z [M+H]+ (calcd 575.2129 for C29H35O12)]. Other compounds, identified by GC–MS from the DCM extracts were the dicyclic peptides pyrrole-(1,2,a)-pyrazine-1,4-dione, hexahydro-3-(2-methylpropyl) (PPDHMP) also called cyclo(Leu-Pro) (Fig. S6A) and 1,4-bis (phenylmethyl), also called Cyclo-Phe-Pro (Fig. S6B). The tetrahydropyrrole 3-pyrrolidin-2-yl-propionic acid; and the heterobicyclic pentane 2,3,5-trioxabicyclo[2.1.0]pentane. PPDHMP has been also extracted from Staphylococcus sp. MB30 strain, exhibiting anticancer potential against lung (A549) and cervical (HeLa) cancer cells in vitro [23]. On the other hand, 2,3,5-trioxabicyclo [2.1.0] pentane and 1,4-bis(phenylmethyl), isolated from Streptomyces mangrovisoli sp. nov., present antioxidative activity [24]. The two cyclic dipeptides [cyclo(Leu-Pro) and cyclo(Phe-Pro)] represented the major compounds with 67% and 12%, respectively (Fig. 1). Both dipeptides have been reported as products of different endophytes, particularly, cyclo(Phe-Pro), which has antimicrobial properties [25, 26]. Additional compounds included 3-pyrrolidin-2-yl-propionic acid with 9%, 2,3,5-trioxabicyclo[2.1.0]pentane, 1,4-bis-(phenylmethyl) with 5%, 7-hexil-eicosane, with 3%, 1-(4-hydroxy-3-methoxyphenyl)-ethanone with 2% (also called apocynin), and 9-octyl-heptadecane with 1%. Apocynin structurally resembles vanillin and exhibits anti-inflammatory properties as result of its ability to inhibit NADPH oxidase activity preventing free radicals, oxygen ions, and peroxides formation in the body [27].
In vitro anti mycobacterium tuberculosis H37Rv activity
The inhibitory activities of the S. scabrisporus NF3 DCM extract, the compound 1 (StefB), and StefC, were evaluated on the virulent M. tuberculosis H37Rv strain using different amounts (1.98–500 µg/mL) of these samples in a serial of twofold dilutions. The anti-tuberculosis activities of the extracts and compounds were compared to RIF, usually indicated for Mycobacterium infections treatment. As shown in Table 2, RIF showed to be more active against M. tuberculosis H37Rv strain (MIC100 of 0.06 µg/mL) than the DCM extract (31.25 µg/mL) and StefB (7.8 µg/mL). Besides, StefB has a selectivity index (SI) value of 12.7, therefore can be validated as a good TB hit [28] and suitable as a good anti-tuberculosis compound by its potency against M. tuberculosis (Table 2). In agreement with other reports, StefC exhibited lower bioactivity than StefB (Compound 1) [20].
One of the criteria that a lead should exhibit against M. tuberculosis strains is its ability to eliminate a mono resistant strain. To further assess the StefB spectra, a clinical isolate resistant to RIF (RMR M.tb-209 strain) was evaluated (Table 3). As shown in this table, the observed StefB (Compound 1) MIC100 against RMR M.tb-209 was 3.9 µg/mL, a value even lower than that obtained for the virulent M.tb H37Rv (reference strain) and better than that obtained with RIF.
In the area of drug discovery against tuberculosis only one compound has so far been recently isolated from the Actinomycete Nonomuraea sp. MJM5123 (http://www.newtbdrugs.org/pipeline/clinical). This compound (ecumicin), is a macrocyclic tridecapeptideone, which shows an excellent activity against isolated MDR and XDR strains of M. tuberculosis [29]. Ecumicin targets the ClpC1 ATPase complex, which functions in protein breakdown with the ClpP1P2 protease, modulating intracellular protein levels to adapt to changes in both internal and external conditions [30].
Minimal inhibitory concentration (MIC) for non-mycobacteria
Although Brodsky and Reusser [21], initially reported StefB as an antitumor agent against L-1210 mouse leukemia cells, these authors also observed in vitro antibiotic activity against Gram-positive bacteria (Staphylococcus aureus UC-80, Streptococcus hemolyticus UC-152 and Streptococcus faecalis UC-3235). However, no activity was detected either against Gram-negative bacteria nor pathogenic fungi. Our results of antibiotic activity against Gram-positive bacteria, and the MICs obtained for the reference bacteria (Table 4) coincided with those reported in the literature [21, 22]. A strong activity against the food-borne L. monocytogenes, that causes high rates of morbidity and mortality, was also observed (MIC 4 µg/µL). Comparisons of this effect were not possible due to the lack of reports with this microorganism.
Regarding the StefB MIC values against the pathogenic M. tuberculosis (RMR Mtb-209) strain, this compound killed the pathogenic strain with a MIC value of 3.9 µg/µL. This value was even better than those observed for the virulent M. tuberculosis strain H37Rv.
Other anthracyclines like daunorubicin and doxorubicin, are of pharmaceutical importance. They were discovered in the early 1960s and are clinically used today for cancer treatment [31]. In the same decade, steffimycin A was discovered and a decade later StefB [32], but this was not able to exhibit the in vivo antibiotic activity of StefA [21]. Moreover, the discovery of other anthracyclines like idarubicin, which inhibits the M. tuberculosis primase DnaG [33], likely reduced the interest in StefB. Furthermore, the appearance of new antibiotics like the diarylquinoline bedaquiline, which targets the proton pump of ATP synthesis, reducing the ATP supply for bacterial metabolism [34] and the nitroimidazole delamanid, which inhibits production of mycolic acid component of the cell envelope [35], also delayed the study of StefB. Besides, in the present context, some molecules like linezolid, meropenem clavulanate and pyridomycin, among others, have been reevaluated and redeveloped showing a promising future in the treatment of this disease [36,37,38].
Concerning the StefB mechanism to kill M. tuberculosis, this may be different to that observed for RIF due that the RMR Mtb-209 strain is a rifampicin resistant mutant and still showed sensitivity to the anthracycline. The mechanism of action of RIF is the arrest of the DNA-directed RNA synthesis of M. tuberculosis by interacting with the β-subunit of RNA polymerase (RNAP) [39]. This effect does not interfere with substrate binding, catalytic activity, or the intrinsic translocation mechanism of the RNAP. In addition to RNAP, an efflux pump may be responsible for approximately 5% of clinical RIF-resistant M. tuberculosis strains. Regarding the StefB mechanism, a possible DNA intercalating effect may responsible of this effect, causing an increase in the TM value of the M. tuberculosis DNA. Indeed, StefB has been shown to bind DNA [40]. Computer simulation studies suggest that StefB has preference for the CpG base sequence more than for the TpA step, which is similar to the sequence specificity exhibited for other anthracyclines like daunomycin [41] and nogalamycin. However, this property might not be the only mode of action of this compound and will require further exploration.
Conclusions
The anthracycline StefB structure was elucidated as the main compound produced by the endophytic S. scabrisporus, grown in ISP-2 medium. This compound was effective against several M. tuberculosis strains and when evaluated by REMA, showed a MIC100 value of 7.8 µg/mL against the virulent M.tb H37Rv strain. StefB also inhibited the pathogenic mono resistant RIF strain RMR Mtb 209, suggesting a different StefB action mechanism from that of RIF. Our results encourage identification of bottlenecks for moving forward to hyperproduce and scale up StefB levels, as this anthracycline displayed a strong bactericidal effect against Gram-positive pathogens as M. tuberculosis, one of the oldest and more dangerous human pathogen causing high human mortality. On the other hand, the potential of endophytes as sources of bioactive compounds is evident and it is worth re-evaluating already known molecules, in order to exploit their pharmacological potential.
References
Silva-Miranda M, Breiman A, Allain S, Deknuydt F, Altare F (2012) The tuberculous granuloma: an unsuccessful host defense mechanism providing a safety shelter for the bacteria? Clin Dev Immunol. 2012:139127
Wong E, Cohen K, Bishai W (2013) Rising to the challenge: new therapies for tuberculosis. Trends Microbiol 21(9):493–501
Kumar V, Patel S, Jain R (2016) New structural classes of antituberculosis agents. Med Res Rev 38(2):1–57
Demain AL, Sanchez S (2015) The need for new antibiotics. In: Sanchez S, Demain AL (eds) Antibiotics, current innovations and future trends. Caister Academic Press, North Folk, pp 65–82
Genilloud O (2014) The re-emerging role of microbial natural products in antibiotic discovery. Antonie Van Leeuwenhoek 106:173–188
Berdy J (2015) Microorganisms producing antibiotics. In: Sanchez S, Demain AL (Eds) Antibiotics, current innovations and future trends. Caister Academic Press, North Folk, pp 49–64
Martínez-Klimova E, Rodríguez-Peña K, Sánchez S (2017) Endophytes as sources of antibiotics. Biochem Pharmacol 134:1–17
Gutiérrez MP, González MN, Ramírez AM (2012) Compounds derived from endophytes: a review of phytochemistry and pharmacology. Curr Med Chem 19:2992–3030
Rodriguez-Garcia A, Peixoto IT, Verde-Star MJ, De la Torre-Zavala S, Aviles-Arnaut H, Ruiz AL (2015) In vitro antimicrobial and antiproliferative activity of Amphipterygium adstringens. Evid Based Complementary Alternat Med 2015:175497
Vazquez-Hernández M, Ceapa CD, Rodríguez-Luna SD, Rodríguez-Sanoja R, Sánchez S (2017) Draft genome sequence of Streptomyces scabrisporus NF3, endophyte isolated from Amphipterigium adstringens. Genome Announc 5:e00267–e00217
Shirling EB, Gottlieb D (1966) Methods for characterization of Streptomyces species. Int J Syst Bacteriol 16:313–340
Gohar YM, El-Naggar MY (2001) Induction of sporulation and antibacterial activity in the aerial mycelium negative mutants of Streptomyces nasri. Egypt J Biol3:23–35
Thomas KJ, Rice CV (2014) Revised model of calcium and magnesium binding to the bacterial cell wall. Biometals 27:1361–1370
Alvarado C, García-Almendárez B, Martin S, Regalado C (2005) Anti-Listeria monocytogenes bacteriocin-like inhibitory substances from Enterococcus faecium UQ31 isolated from artisan mexican-style cheese. Curr Microbiol 51:110–115
Linstrom PJ, Mallard WG (2015) NIST Chemistry WebBook, NIST Standard Reference Database. National Institute of Standards and Technology, Gaithersburg; 20899. http://webbook.nist.gov/chemistry/
Mossman T (1983) Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J Immunol Methods 65:55–63
Collins L, Franzablau SG (1997) Microplate alamar blue assay versus BACTEC 460 system for high-throughput screening of compounds against Mycobacterium tuberculosis and Mycobacterium avium. Antimicrob Agents Chemother 41:1004–1009
Enyinnaya F, Cruz P, Buttner MP, Cross C, Woodard DR (2017) Comparison of clinical and laboratory standards institute standards in antimicrobial susceptibility among the carbapenemase producing Enterobacteriaceae. Future Sci OA 3(4):FSO245
Kelly RC, Schletter I, Koert JM, MacKellar FA, Wiley PF (1977) Structures of steffimycin and steffimycin B1. J Organic Chem 42:3591–3596
Brodasky TF, Mizsak S, Hoffstetter JR (1985) Steffimycin C, a new member of the steffimycin anthracyclines. Isolation and structural characterization. J Antibiot (Tokyo) 38(7):849–855
Brodasky TF, Reusser F (1974) Steffimycin B, a new member of the steffimycin family: isolation and characterization. J Antibiot 27:809–813
Intaraudom C, Bunbamrung N, Dramae A, Danwisetkanjana K, Rachawee P, Pittayakhajonwut P (2015) Antimalarial and antimycobacterial agents from Streptomyces sp. BCC27095. Tetradehon Lett 56:6875–6877
Lalitha P, Veena V, Vidhyapriya P, Lakshmi P, Krishna R, Sakthivel N (2016) Anticancer potential of pyrrole (1,2,a) pyrazine 1,4-dione, hexahydro 3-(2-methyl propyl) (PPDHMP) extracted from a new marine bacterium, Staphylococcus sp. strain MB30. Apoptosis 21(5), 566–577
Ser H-L, Palanisamy UD, Yin W-F, Abd Malek SN, Chan K-G, Goh B-H, Lee L-H (2015) Presence of antioxidative agent, Pyrrolo[1,2-a]pyrazine-1,4-dione, hexahydro—in newly isolated Streptomyces mangrovisoli sp. nov. Front Microbi 6:854
Nirjanta D, Wahab F (2012) Antimicrobial properties of endophytic fungi isolated from medicinal plant Camellia sinesis. Int J Pharm Bio Sci. 3:P420–P427
Melo IS, Santos SN, Rosa LH, Parma MM, Silva LJ, Queiroz SCN, Pellizari VH (2014) Isolation and biological activities of an endophytic. Mortierella alpina strain from the Antarctic moss Schistidium antarctici. Extremophiles 18:15–23
Li N, Zhang G, Yi FX, Zou AP, Li PL (2005) Activation of NAD(P)H oxidase by outward movements of H+ ions in renal medullary thick ascending limb of Henle. Am J Physiol Renal Physiol 289(5):F1048–F1056
Katsuno K, Burrows JN, Duncan K, van Huijsduijnen RH, Kaneko T, Kita K, Schmatz D, Warner P, Slingsby BT (2015) Hit and lead criteria in drug discovery for infectious diseases of the developing world. Nat Rev Drug Discov 14:751–758
Gao W, Kim JY, Anderson JR, Akopian T, Hong S, Jin YY, Kandror O, Kim JW, Lee IA, Lee SY, McAlpine JB, Mulugeta S, Sunoqrot S, Wang Y, Yang SH, Yoon TM, Goldberg AL, Pauli GF, Suh JW, Franzblau SG, Cho S (2014) The cyclic peptide ecumicin targeting ClpC1 is active against Mycobacterium tuberculosis in vivo. Antimicrobial Agents Chemother 59(2):880–889
Lee H, Suh JW (2016) Anti-tuberculosis lead molecules from natural products targeting Mycobacterium tuberculosis ClpC1. J Ind Microbiol Biotechnol 43(2–3):205–212
Tacar O, Sriamornsak P, Dass CRJ (2013) Doxorubicin: an update on anticancer molecular action, toxicity and novel drug delivery systems. J Pharm Pharmacol 65(2):157–170
Gullón S, Olano C, Abdelfattah MS, Braña AF, Rohr J, Méndez C, Salas JA (2006) Isolation, characterization, and heterologous expression of the biosynthesis gene cluster for the antitumor anthracycline steffimycin. Appl Environ Microbiol 72(6):4172–4183
Gajadeera C, Willby MJ, Green KD, Shaul P, Fridman M, Garneau-Tsodikova S, Posey JE, Tsodikov OV (2015) Antimycobacterial activity of DNA intercalator inhibitors of Mycobacterium tuberculosis primase DnaG. J Antibiot (Tokyo) 68(3):153–157
Andries K, Verhasselt P, Guillemont J, Göhlmann HW, Neefs JM, Winkler H, Van Gestel J, Timmerman P, Zhu M, Lee E, Williams P, de Chaffoy D, Huitric E, Hoffner S, Cambau E, Truffot-Pernot C, Lounis N, Jarlier VA (2005) A diarylquinoline drug active on the ATP synthase of Mycobacterium tuberculosis. Science 307(5707):223–227
Diacon AH, Dawson R, Hanekom M, Narunsky K, Venter A, Hittel N, Geiter LJ, Wells CD, Paccaly AJ, Donald PR (2011) Early bactericidal activity of delamanid (OPC-67683) in smear-positive pulmonary tuberculosis patients. Int J Tuberc Lung Dis 15(7):949–954
Cragg GM, Grothaus PG, Newman DJ (2014) New horizons for old drugs and drug leads. J Nat Prod 77(3):703–723
D’Ambrosio L, Centis R, Sotgiu G, Pontali E, Spanevello A, Migliori GB (2015) New anti-tuberculosis drugs and regimens: 2015 update. ERJ Open Res 1(1):00010–2015
Hartkoorn RC, Sala C, Neres J, Pojer F, Magnet S, Mukherjee R, Uplekar S, Boy-Röttger S, Altmann K-H, Cole ST (2012) Towards a new tuberculosis drug: pyridomycin – nature’s isoniazid. EMBO Mol Med 4(10):1032–1042
Pang Y, Lu J, Wang Y, Song Y, Wang S, Zhao Y (2013) Study of the rifampin monoresistance mechanism in Mycobacterium tuberculosis. Antimicrob Agents Chemother 57:893–900
Reusser F (1975) Steffimycin B, a DNA binding agent. Biochim Biophys Acta Nucleic Acids Protein Synthesis 383(3):266–273
Wang AH-J (1992) Intercalative drug binding to DNA. Curr Opin Struct Biol 2:361–368
Acknowledgements
This work was partially supported by the NUATEI program from Instituto de Investigaciones Biomédicas, and by PAPIIT (IN202216), DGAPA UNAM, México. We are indebted to Beatriz Ruiz-Villafán and Erika Segura Salinas for technical assistance in this work. The help of Marco A. Ortiz-Jiménez for strain preservation studies is recognized. We thank the support of CONACYT Project Number INFR-2017-01 279880, which allowed the acquisition of an HPLC masses.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no conflict of interests.
Ethical statement
This article does not contain any studies with human participants performed by any of the authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Trenado-Uribe, M., Silva-Miranda, M., Rivero-Cruz, J.F. et al. Antimycobacterial activity of an anthracycline produced by an endophyte isolated from Amphipterygium adstringens. Mol Biol Rep 45, 2563–2570 (2018). https://doi.org/10.1007/s11033-018-4424-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-018-4424-0