Abstract
Temporal lobe epilepsy is the most common drug-resistant epilepsy. To cure epilepsy, drugs must target the mechanisms at the origin of seizures. Thus, the present investigation aimed to evaluate the antiepileptic- and anti-amnesic-like effects of an aqueous extract of Syzygium cumini against kainate-induced status epilepticus in mice, and possible mechanisms of action. Mice were divided into 7 groups and treated as follows: normal group or kainate group received po distilled water (10 mL/kg), four test groups received Syzygium cumini (28.8, 72, 144, and 288 mg/kg, po), and the positive control group treated intraperitoneally (ip) with sodium valproate (300 mg/kg). An extra group of normal mice was treated with piracetam (200 mg/kg, po). Treatments were administered 60 min before the induction of status epilepticus with kainate (15 mg/kg, ip), and continued daily throughout behavioral testing. Twenty-four hours after the induction, T-maze and Morris water maze tasks were successively performed. The animals were then sacrificed and some markers of oxidative stress and neuroinflammation were estimated in the hippocampus. The extract significantly prevented status epilepticus and mortality. In the T-maze, the aqueous extract markedly increased the time spent and the number of entries in the discriminated arm. In the Morris water maze, the extract significantly increased the time spent in the target quadrant during the retention phase. Furthermore, the aqueous extract induced a significant reduction of oxidative stress and neuroinflammation. These results suggest that the aqueous extract of Syzygium cumini has antiepileptic- and anti-amnesic-like effects, likely mediated in part by antioxidant and anti-inflammatory activities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
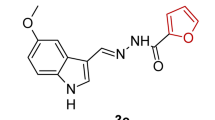
Epilepsies are chronic neurological conditions defined by the recurrence of two or more paroxysmal seizures (Chin 2012; Weaver and Cromwell 2019; Zhu et al. 2020; Wagner et al. 2020). They manifest as brief episodes of involuntary tremors affecting part or all of the body, with or without the loss of consciousness (Fisher et al. 2014; Falco-Walter et al. 2018; Fisher and Bonner 2018; Pack 2019). These seizures result from hyperexcitability and hypersynchrony of neurons (Stafstrom 2010; Fisher et al. 2014; Falco-Walter et al. 2018; Fisher and Bonner 2018). Epilepsies affect approximately 50–70 million people worldwide with a morbidity of 0.5% (Kuate et al. 2015; Vezzani et al. 2016; Kwon et al. 2019). According to the review of Singh and Sander (2020), over 80% of deaths resulting from this disease occur in low- and middle-income countries. Epilepsy is also a major economic burden in Africa for epilepsy patients and their families (Chin 2012; Weaver and Cromwell 2019; Wagner et al. 2020). Of all types of epilepsy, TLE deserves special attention because it affects a specific area of the brain and accounts for 60% of epilepsies (Téllez-Zenteno 2012; Jaimes-Bautista et al. 2015; Taiwe et al. 2015; Mante et al. 2017). Primary precipitating injuries of the TLE include head trauma, prolonged febrile seizures, infections, or status epilepticus (SE) (Curia et al. 2014; Rusina et al. 2021). The latter is a seizure lasting more than 30 min without recovery of consciousness between seizure episodes (Cherian and Thomas 2009; Curia et al. 2014). TLE is often associated with neuropsychiatric comorbidities, including anxiety, depression, and amnesia (Ismail et al. 2017; Kandeda et al. 2021a, b, 2022a, b; Vinti et al. 2021). However, the complex mechanisms underlying epileptogenesis, the onset of spontaneous seizures, and the associated comorbidity are not readily understood in clinical studies (Butler and Zeman 2008; Kimiskidis and Valeta 2012; Kandratavicius et al. 2014; Lima et al. 2021). Also, the relationship between TLE and amnesia is poorly understood (Hubens et al. 2014; Mosbah et al. 2014; Madar et al. 2021). Amnesia is defined as the inability of individuals to learn and remember acquired information (Mosbah et al. 2014; Madar et al. 2021). This memory impairment is often associated with epilepsy since nearly 80% of epilepsy patients have episodic memory impairment (Butler and Zeman 2008; Jaimes-Bautista et al. 2015; Mosbah et al. 2014; Madar et al. 2021). This is due to the spread of seizures in the regions of the brain involved in the control of memory (Groticke et al. 2008; Kiasalari et al. 2016; Kandeda et al. 2022a). In addition, patients with drug-resistant TLE have a higher risk of developing short- and long-term memory impairment (Groticke et al. 2008; Holler and Trinka 2014; Kiasalari et al. 2016; Tramoni-Negre et al. 2017). Therefore, the use of animals and appropriate methods is in great experimental demand to understand these mechanisms, one of them being the kainate model of epilepsy. The first experiments using intraperitoneal injection of kainate were done in 1970 (Rusina et al. 2021). The findings revealed that administration of kainate (12 mg/kg) caused ‘’wet dog shaking” seizures between 30–90 min. These seizures then evolved into generalized tonic-clonic seizures in 88% of rats (Lévesque et al. 2016; Rusina et al. 2021). The kainate model of TLE has long been used to understand the molecular and cellular mechanisms underlying spontaneous seizures in rodents (Lévesque and Avoli. 2013; Lévesque et al. 2016). In fact, the systemic injection of kainate to rodents is associated with endoplasmic reticulum stress, excitotoxicity, oxidative stress, glial activation, and inflammation (Ojo et al. 2019; Ramazi et al. 2020; Kandeda et al. 2021b, 2022a, b). The kainate model also exhibits behavioral, cognitive, histological, pharmacological, and electroencephalographic characteristics of human TLE (Lévesque and Avoli 2013; Lévesque et al. 2016). Despite many and growing efforts of modern pharmacology, the treatment of epilepsies remains a mystery. Indeed, the antiepileptics currently available are symptomatic and can neither cure nor prevent epilepsy. Moreover, the majority of the world’s population does not benefit from this treatment, especially in Africa where over 60% of epilepsy patients do not receive any treatment (Chin 2012; Winkler 2012; Ba-Diop et al. 2014; Esterhuizen et al. 2018; Wagner et al. 2020). Numerous studies have shown that TLE is generally drug-resistant and requires surgical intervention (Lévesque and Avoli 2013; Lévesque et al. 2016). For millennia, humans have always used medicinal plants to solve their health problems (Petrovska 2012; Dibong et al. 2015). According to the World Health Organization, nearly 80% of the population in developing countries use traditional medicine and these drugs cause fewer side effects (Ekor 2014; Iwuoha et al. 2020; Wagner et al. 2020). Syzygium cumini Skeels (S. cumini) (Myrtaceae) is a plant used in traditional medicine to treat many conditions, including bronchitis, asthma, anxiety, epilepsy, memory impairment, diabetes, depression, dementia, obesity, dysentery, cough, and stomatitis (Ayyanar and Subash-Babu 2012; Pai et al. 2013; Chauhan and Intelli 2015; Hossain et al. 2017; Ulla et al. 2017; Ezhilarasan et al. 2019). According to previous literature, no precision was given on the type of epilepsy or memory impairment cured by this plant (Pai et al. 2013; Chauhan and Intelli 2015; Hossain et al. 2017; Ulla et al. 2017). However, in Cameroon, the plant is mostly prescribed by traditional healers against TLE and dementia (personal communication). This plant is mainly known for its antioxidant, cardioprotective, antimicrobial, anti-inflammatory, antiobesity, anticancer, antifungal, and antidiabetes properties (Chanudom et al. 2015; Akhtar et al. 2016; Hossain et al. 2017; Jagetia et al. 2008; Ezhilarasan et al. 2019). The plant extracts or fractions were also reported to possess sedative, anticonvulsant, and potent central nervous system depressant effects (Chanudom and Tangpong 2015; De Lima et al. 1998). The seeds of S. cumini have been found to possess an anti-amnesic effect on the Alzheimer’s disease model in rats (Hossein et al. 2017). The methanolic extract of S. cumini also revealed an anti-amnesic effect of the extract against scopolamine-induced spatial memory impairment in rats (Alikatte et al. 2012). In addition, the hydroethanolic extract of the leaves of the plant showed anticonvulsant effects that appear to be mediated by antioxidant and anti-inflammatory activities (De Lima et al. 1998). Previous phytochemical studies on S. cumini stem bark revealed the presence of alkaloids, flavonoids, anthocyanins, terpenoids, essential oils, tannins, and polyphenols (Srivastava and Chandra 2013; Jha 2017). Compounds isolated from stem bark decoction, using HPLC analysis, revealed mainly betulinic acid, ellagic acid, ß-sitosterol, friedeanol, anthocyanin di-glucosides, epifriedeanol, and eugenin (Bijauliya et al. 2017; Abdin et al. 2020). This part of the plant equally contains ß-sitosterol-D-glucoside, kamepferol-3-0- glucoside, ellagitannins, quercetin, myricetin, friedelin, astragalin, and gallic acid (Ayyanar and Subash-Babu 2012; Srivastava and Chandra 2013; Bijauliya et al. 2017; Abdin et al. 2020). These compounds have shown various pharmacological effects, including antioxidant, antiulcer, antihyperlipidaemic, hepatoprotective, antiallergic, antiarthritic, anti-inflammatory, and antibacterial activities (Simões-Pires et al. 2009; Srivastava and Chandra 2013; Abdin et al. 2020). All of these allowed us to hypothesize that the plant extract could be endowed with antiepileptic- and anti-amnesic-like properties. The present study, therefore, aimed to evaluate the antiepileptic- and anti-amnesic-like effects of an aqueous extract of S. cumini in kainate-treated mice. Specifically, it was to determine the effects of the aqueous extract of S. cumini on some parameters of SE, amnesia, oxidative stress (GSH and MDA), and neuroinflammation (TNF, IL-6, and IL-1β).
Materials and methods
Plant material and identification
The bark of S. cumini was collected in July 2020, in the Adamawa region (Cameroon), Vina department, and precisely in the forest gallery (latitude 7.425, longitude 13.531, and altitude 1075.03 ± 11 m). This plant was identified by Professor Pierre Marie Mapongmetsem, botanist at the University of Ngaoundéré. The anatomical and morphological clues considered by the Professor are the follows:
-
- the leaves, 5–13 cm long, were dark green, leathery, shiny, glabrous, coriaceous, and oblong in shape. The apex was round, short, and obtuse; the stalk was light yellow and slender with 1.2–2 cm long; the side veins were fine, parallel, close together with tiny gland dots;
-
- the flowers, 6–13 mm long, were fragrant, numerous, white, greenish, or creamy. The calyx was 4 white, concave, and rounded petals of 3 mm; the pistil has an inferior ovary; the ovules were tiny, stout, and numerous; the style (5–8 mm long) was white;
-
- the fruits, 1.5–3.8 cm long and 2 cm in diameter, were fleshy, elliptically shaped, ovoid-oblong, berries, crowded in clusters with a single brown central seed (1–2 cm long). The pulp of the fruits was yellow or pale violet.
The plant was then authenticated at the National Herbarium of Cameroon (Yaoundé) where a voucher specimen number 57 903 HNC exists. The plant name was also checked on plantlist.org.
Preparation of the aqueous extract ofS. cumini.
The bark of S. cumini was cleaned, shade-dried, and then powdered. This crude powder was sieved and weighed, of which 50 g were placed in an aluminum container, containing 500 mL of distilled water. The whole was boiled for 15 min at 100 °C. After cooling at room temperature and filtration with Wattman No. 1 paper, a filtrate of 300 mL was obtained (Kandeda et al. 2017, 2022a). This filtrate was evaporated for 24 h, in an oven set at 45 °C. This operation allowed us to obtain 4.32 g of dry aqueous extract (dry mass), giving a yield of 8.64%. To prepare the different doses of the extract, 1.44 g of dry extract of S. cumini was weighed and introduced into a graduated cylinder. Then distilled water was added to the extract until a final volume of 50 mL was obtained. The mixture was stirred until complete dissolution to obtain a stock solution of 28.8 mg /mL concentration. The other three solutions were obtained by diluting the stock solution with distilled water in a ratio of 1/2, 1/4, and 1/10. Therefore, this gave solutions with concentrations of 14.4, 7.2, and 2.88 mg/mL, respectively. The doses administered to the animals were thus 28.8, 72, 144, and 288 mg/kg. The aqueous extract was administered po to the animals at a volume of 10 mL/kg body weight.
Chemicals
The following chemicals were purchased from Sigma Chemical, St. Louis (USA): kainate (cat no: 487-79-6), sodium valproate (cat no: 1069-66-5), piracetam (cat no: 7491-74-9), diazepam (cat no: 439-14-5), Ellman’s reagent (cat no: 69-78-3), NaCl (cat no: 7647-14-5), Tris-HCl (cat no: 1185-53-1), trichloroacetic acid (TCA, cat no: 76-03-9), and thiobarbituric acid (TBA, cat no: 504-17-6).
Animals and ethics
The experiment was carried out in white mice, Mus musculus swiss, aged 10 ± 2 weeks and weighing 22 ± 4 g. These mice were provided by LANAVET (National Veterinary Laboratory of Garoua, Cameroon) and acclimatized to the animal biology laboratory (University of Ngaoundéré) for three days. Mice had free access to food and water, with 12 h /12 h in light and dark. The animals were kept 5 per cage (30 cm × 30 cm) at ambient temperature (24–26 °C) and relative humidity (52%). The study was conducted following the Cameroon National Ethical Committee (Ref No. FW-IRB00001954, 22 October 1987). Every effort was made to minimize the number of mice used and their suffering. All experiments were performed during the day (8:00 h – 17:00 h). Blinding and randomization procedures during experiments were accomplished according to ARRIVE 2.0 guidelines (https://arriveguidelines.org/arrive-guidelines). The sample size was determined based on previous laboratory estimation (Bertoglio et al. 2017; Khamse et al. 2015; Mohd et al. 2018; Zeng et al. 2009). We confirmed these numbers by using Power G software for size sample estimation (Lan et Lian2010) and the following formulae: sample size = (Z – score)2 * StdDev*(1 – StdDev) / (margin of error)2. Where Z: confident level; StdDev: standard deviation.
Grouping of animals and induction ofSEby kainate.
To assess the effects of S. cumini on the development of SE, 63 mice were divided into 7 groups and treated as follows (Hsieh et al. 2011; Puttachary et al. 2015; Rusina et al. 2021):
-
normal group of 6 mice was treated with distilled water (10 mL/kg, po);
-
kainate group of 12 mice was treated with distilled water (10 mL/kg, po);
-
test groups of 9 mice each were treated with the aqueous extract of S. cumini (28.8, 72, 144, and 288 mg/kg, po);
-
positive control group of 9 mice was treated intraperitoneally (ip) with sodium valproate (SV group, 300 mg/kg).
An extra/additional group (pira group) of 9 mice was treated with piracetam (300 mg/kg, po), a standard anti-amnesic drug. This group was treated with piracetam, one hour before kainate administration, but not assessed for seizures as the above groups. However, this group was treated daily with piracetam during behavioral experiments. Indeed, significant memory impairment is usually observed in rodents after 24 h or days following kainate-induced SE (Maia et al. 2014; Kiasalari et al. 2016; Kandashvili et al. 2022; Kandeda et al. 2022a). Hence, it was relevant to study this group during behavioral experiments.
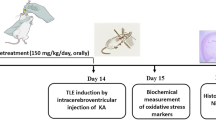
Based on previous laboratory findings, the injection of kainate is associated with high mortality in unprotected animals (Hsieh et al. 2011; Lévesque and Avoli 2013; Puttachary et al. 2015; Rusina et al. 2021). However, because of inter-individual variability, some animals are most susceptible to mortality than others (Lévesque and Avoli 2013; Puttachary et al. 2015; Bertoglio et al. 2017; Rusina et al. 2021). Therefore, the number of mice per group was ideally adjusted to 12 mice in the kainate group, and 9 mice in other experimental groups (Hsieh et al. 2011; Lévesque and Avoli 2013; Puttachary et al. 2015; Rusina et al. 2021). During the experimental procedure, a single administration of the different treatments was performed one hour before kainate injection. Thereafter, these treatments were administered daily for the duration of the behavioral experiments (Fig. 1).
Sixty minutes after the single administration of the above-mentioned treatments, each mouse was injected with kainate (15 mg/kg, ip), a glutamatergic agonist, used to induce epilepsy in rodents (Lévesque and Avoli 2013; Lévesque et al. 2016). However, the animals of the normal group were treated with distilled water (10 mL/kg, ip). Immediately after the injection of kainate or distilled water, each mouse was placed in a cage and their behavior was carefully observed for 80 min. Indeed, approximately 20 min after kainate injection, animals became hypoactive and displayed oro-facial movements, salivation, eye blinking, twitching of vibrissae, and yawning. A generalized tonic-clonic seizure, which marked the onset of SE was observed 40–80 min after kainate injection (Lévesque and Avoli 2013; Lévesque et al. 2016; Kandeda et al. 2022a, b). Thus, when the mouse developed tonic-clonic seizures, which marked the onset of SE (prolonged seizures, with or without loss of the righting reflex, lasting more than 30 min), the latency time and the duration of the SE were recorded. It is well known that stages 0–2 nonconvulsive seizures are observed approximately 14 min after kainate administration (Lévesque and Avoli 2013; Lévesque et al. 2016). These seizures are usually electroencephalogram seizures without behavioral signs. The first stage 3 seizure appeared after another additional 23 min, while the first convulsive seizure (stage 4 or 5) required a time interval of approximately 1 h. Stage 5 seizures only, occurred approximately 80 min after the treatment (Racine 1972; Lévesque et al. 2016; Sharma et al. 2018). The severity of seizures, referring to the most severe seizures exhibited by the mice, was assessed using the Racine scale (Racine 1972):
-
Stage 0: indicates no response;
-
Stage 1: indicates hyperactivity, vibrissae twitching, and chewing;
-
Stage 2: indicates head nodding, head clonus, and myoclonic jerks;
-
Stage 3: indicates unilateral forelimb clonus;
-
Stage 4: indicates rearing with bilateral forelimb clonus;
-
Stage 5: indicates generalized tonic-clonic seizures with loss of the righting reflex.
Furthermore, when SE was not observed during the above period, the animal was considered as protected against SE and the percentage of protection among alive mice was determined (Cherian and Thomas 2009; Lévesque et al. 2016; Sharma et al. 2018). The percentage of protection against death in mice that developed SE was also recorded during this period. At the end of observations, i.e. two hours following the onset of SE, diazepam (20 mg/kg, ip) was administered to the animals to terminate kainate-induced seizures or mortality (Fritsch et al. 2010; Qashu et al. 2010; Lévesque and Avoli 2013; Puttachary et al. 2015). Overall, the percentage of mice protected against the development of SE was calculated as follows: [(Number of mice that did not develop SE/ Number of alive mice used) * 100]. However, the percentage of mice death mice after SE was determined as follows: [(Number of dead mice after SE/ Number of mice that developed SE) * 100].
Twenty-four hours after SE, surviving mice were subjected to the T-maze task. One day later, i.e. 24 h after the 3-day T maze task protocol, the same mice were subjected to the Morris water maze task for 6 days. Twenty-four hours following the last session of the Morris water maze task, the open field test was performed for 1 day (Fig. 1). During behavioral assays, the above treatments were administered, once daily, until behavioral experiments were completed, i.e. 1 h before each session of the T-maze (3 sessions), Morris water maze (6 sessions), and the open field test (1 session). These mice were treated in this manner, once daily, at the same hours, until the end of the behavioral experiments (Fig. 1). Besides, the group receiving the piracetam (pira group), only used during behavioral experiments, served as the second positive control. Indeed, apart from evaluating the antiepileptic effect of the extract, the aim of this study was also to evaluate the anti-amnesic effect of the plant extract against memory impairment associated with seizures. It was, therefore, important to compare the anti-amnesic potential of the extract with a standard anti-amnesic drug such as piracetam. So, it is expected that animals receiving this treatment would show less memory impairment compared to the kainate group.
Behavioral tests
T-maze task
This test is based on the willingness of mice to explore a new arm rather than a familiar arm (Deacon and Rawlins 2006; Kandeda et al. 2017). The T-Maze is a “T” shaped device made of wood, black on the outside and white on the inside. It consists of a start compartment (starting arm), a central corridor, and two arrival corridors (arrival arms), perpendicular to the central corridor. The device has a wall of 20 cm high, 10 cm wide, and 30 cm long. An opaque guillotine door is placed at the exit of the departure compartment, as well as at the entrance to the arrival corridors. This makes it possible to control access to the different areas of the labyrinth. At the end of each arrival arm, there was a food reinforcer (a feeder) of 3 cm in diameter and 1 cm in height. This device was similar to that described by Kandeda et al. (2017). The T-maze test is used to detect drugs acting on working memory (Werk 2001; Deacon and Rawlins 2006; Yang and Mailman 2018). Working memory refers to a memory associated with the ability to remember a space or localization over a short period (Werk 2001; Deacon and Rawlins 2006). One day before the experiment (habituation phase), animals were individually placed in the starting arm for a 5-min exploration. When the animal entered the first one of the arrival arms, this arm was considered the preferred arm (opposite to discriminated arm). The next day, i.e. day 2 (acquisition phase), the animals were again placed in the T-maze for 5-min exploration. During this phase, the discriminated arm was closed, while the preferred arm was opened. Finally, during the retention phase, i.e. day 3 (retention phase), the animals were reintroduced to the T-maze for a 5-min testing period. On the new trial (both choice arms were opened), the animals were placed in a start arm and the number of entries and the time spent in the two arms were recorded. The device was cleaned with 70% ethanol to remove the odor left by the previous mouse.
Morris water maze task
The Morris water maze is an experimental device, designed by Richard Morris in 1980 (Morris et al. 1982). It is a circular device with 120 cm diameter and 75 cm height. It was divided into four virtual quadrants (north, south, east, and west). A stationary and transparent escape platform (30 cm in height and 5 cm diameter) was immersed at 3 cm below the surface of water. This platform was placed in an invariable frame (South-East). In addition, visual cues of various shapes were placed around the device and served as spatial cues for mice (Pahaye et al. 2017). The Morris water maze provides both accurate and reproducible measures of spatial learning and memory. It is also a highly sensitive tool for assessing hippocampal damage (Wenk 2004; Broadbent et al. 2006). In this apparatus, two types of memory can be assessed mainly, reference memory (spatial long-term memory) and working memory (a type of short-term memory). On the first day of the assay, during the habituation phase, each rat was acclimated for 60 s without the platform. Each rat then performed sessions of three-block with 30 min intervals between sessions. Thus, each block consisted of four successive trials of 60 s each. On each trial, animals were randomly released into the water from one of four quadrants facing the maze wall. The acquisition phase began on day 2 with the refuge platform and continued for 3 days with three sessions per day. The water in the device was clouded by adding liquid milk so that the platform was invisible from the surface of the water. The session time for each mouse to find the platform was 120 s, and the interval of time between sessions was 5 min. Once the animal found the platform, it was allowed to stay on it for 15 s. During the acquisition phase sessions, the time taken to find the hidden platform was recorded for each animal. Learning efficiency was then assessed during the retention phase on day 6. During this phase, which lasted 120 s, the platform was removed from the maze. Thus, the time spent in the target quadrant was recorded for each animal.
Open field test
The open field is a square enclosure (40 cm x 40 cm), with raised edges of 45 cm high and illuminated in its center. The device used was similar to that described by Taiwe et al. (2015). The exploration area is divided into 17 squares of 10 cm x 10 cm each (16 squares divide the interior area and 1 central square) (Moto et al. 2018). Each mouse was placed in the center of the device and had 5 min to explore the field. Thus, all animal behaviors were carefully observed, and the parameters recorded were the time spent in the center, the number of groomings, the number of straightenings, and the number of lines crossed. This assay makes it possible to evaluate ambulatory behavior, as well as environmental and dietary neophobia (Belzung 1999). At the end of the experimental session, the device was cleaned with 70% ethanol to remove the odors of the previous mouse.
Sacrification and preparation of homogenates
Immediately after the open field test, the animals were sacrificed by cervical decapitation. All brains were collected and washed with 0.9% NaCl, cleaned and placed in dishes containing 0.9% NaCl, and frozen for 1 h. After solidification, these organs were dissected and kept cold to extract the hippocampus. For each animal, a fixed mass of the hippocampus thus removed was estimated using a digital analytical microbalance (U.S. Solid, USA). Homogenates were prepared at 20% with Tris buffer (50 mM HCl; 150 mM KCl; pH 7.4) and then centrifuged at 10,000 rpm for 15 min at 4 °C (Kandeda et al. 2017; Pahaye et al. 2017). Indeed, protein concentration in the homogenate was quantified in each sample by grinding an equal amount of tissue (measured with a microbalance) in a fixed volume of buffer. In this way, the concentration of proteins in each sample was determined as follows: fixed mass of brain tissue (mg)/fixed volume of buffer (mL) (Dieckmann-Schuppert and Schnittler 1997). The obtained supernatant was introduced into a labeled Eppendorf tube, which was then stored at -20 °C in a freezer for subsequent analysis of biochemical parameters.
Determination of the concentration of some oxidative stress parameters in the hippocampus
Reduced glutathione (GSH) assay
The concentration of GSH was performed according to the protocol described by Ellman (1959). One and a half microliters of Ellman’s reagent were introduced into test tubes previously containing 100 µL of homogenate, while the blank tube contained 1 mL of Tris buffer (50 mM HCl; 150 KCl mM; pH 7.4). These mixtures were then incubated for 1 h at room temperature (24–26 oC). The absorbance was read by a spectrophotometer (Fisher Scientific; cat no: 108-88-3) at 412 nm.
Malondialdehyde (MDA) assay
Two hundred and fifty microliters of homogenate and Tris buffer (50 mM HCl; 150 mM KCl; pH 7.4) were introduced into the test tubes and the blank tube, respectively. In each of the aforementioned tubes, 125 µL of 20% TCA was then added, followed by 250 µL of 0.67% TBA. The tubes were closed with glass beads and incubated for 10 min at 90 °C in a water bath (MRC laboratory-instruments; cat no: WBO-100). Then, these tubes were cooled and centrifuged at 3000 rpm for 15 min at room temperature. The supernatant was pipetted and read on a spectrophotometer. The MDA reacts with TBA in a warm acidic medium to give a pink complex. This pink complex exhibits an absorption maximum at 530 nm (Wilbur et al. 1949). The intensity of the coloration was proportional to the presence of MDA in the sample.
Determination of the concentration of some pro-inflammatory cytokines in the hippocampus
The determination of the concentration of tumor necrosis factor (TNF), interleukin 6 (IL-6), and interleukin 1 beta (IL-1β) was carried out by the ELISA technique (Enzyme-Linked Immunosorbent Assay) using Quantikine Kit for TNF (Minneapolis, USA; cat no: RTA00) or IL-6 (Minneapolis, USA; cat no: R6000B) or IL-1β (Minneapolis, USA; cat no: RLB00) (Zhu et al., 2020). Fifty microliters of dilution solutions (RD1-42 for TNF, RD1-21 for IL-1β, and RD1-54 for IL-6) were added to each well of an ELISA plate, respectively. Then 50 µL of standard, control, or sample was added to each well. The mixture was homogenized by gently tapping the frame plate for 1 min. The microplates were incubated for 2 h at 37 °C. After incubation, each well was washed 5 times with the washing buffer (400 µL). Then, the specific antibody for each protein conjugated to biotin was added to each well at a rate of 100 µL for each cytokine. The preparations were again incubated for 2 h at 37 °C and washed 5 times with the washing buffer (100 µL). After washing, 100 µL of substrate consisting of streptavidin coupled with peroxidase were added to each well, and the preparation was incubated for 30 min at room temperature and protected from light. The enzymatic reaction was stopped by adding 100 µL of stop solution (HCl). Absorbance was measured at 450 nm with a microplate reader. The ELISA technique allows the specific detection of antigens (proteins) by the use of two specific antibodies. The concentration of each pro-inflammatory cytokine, expressed in pg/mL, was determined from the standard calibration curve.
Statistical analysis
The data presented in this study are expressed as mean ± SD. However, the number of mice that developed SE or the number of dead mice is expressed in percentage (%). These data were analyzed using Graph Pad Prism software version 8.0.1. The normality data was evaluated using the Shapiro-Wilk and Kolmogorov-Smirnov tests, while variance homogeneity between experimental groups was assessed using the Brown-Forsythe test. When the assumption of variance homogeneity was established, one-way ANOVA (some behavioral and biochemical tests) or two-way ANOVA (Morris water maze test) was performed. Thus, when the difference between means of experimental groups existed, Tukey post-hoc test was performed. Furthermore, when the data do not assume Gaussian distribution, Kruskal Wallis test followed by Dunn’s test post-hoc test was performed, and results were displayed as mean median and interquartile range. The difference between the number of mice that developed SE and the number of dead mice was determined using the Chi-square test (two-side) (Taiwe et al. 2015). For all analyses, the difference for which p < 0.05 was considered significant.
Results
The aqueous extract ofS. cuminidose-dependently prevented the development ofSEand protected mice againstSE-induced mortality.
There is no available antiepileptic drug that can prevent SE in people at risk (Cherian and Thomas 2009; Kim et al. 2021). Therefore, a drug or extract with a preventive effect on the development of SE should be sought.
Compared to animals of the normal group, 91.67% (p < 0.001) of animals in the kainate group had SE [Chi2 (1,11) = 4, p < 0.001] (Table 1 and supplement I.1). The aqueous extract of S. cumini at the dose of 72 mg/kg markedly (p = 0.01) prevented the development of SE in 57.14% (p = 0.01) of animals [Chi2 (1,7) = 4, p = 0.01], compared to the kainate group (Table 1). This effect of the extract was comparable to that of sodium valproate, a reference antiepileptic drug, which protected 55.56% (p = 0.01) of mice from developing SE [Chi2 (1,9) = 4, p = 0.01] (Table 1 and supplement I.1).
SE is known to cause sudden unexpected death in patients. Thus, a drug that can prevent SE-induced death is sought (Hsieh et al. 2011; Hockers 2019). In the present study, the preventive effect of the extract against SE-induced mortality was therefore evaluated.
In the kainate group, kainate caused 45.45% (p = 0.01) of death only between mice developing SE, unlike the normal group where no deaths were observed [Chi2 (1,11) = 4, p = 0.01] (Table 1 and supplement I.2.). However, the aqueous extract of S. cumini (144 and 288 mg/kg) significantly protected 100% (p < 0.001) of the mice against death also between mice that developed SE, compared to the kainate group [Chi2 (1,6) = 4, p < 0.001]. This protection was greater than that of sodium valproate, a standard antiepileptic drug that protected 25% (p = 0.05) of mice against death after SE [Chi2 (1,4) = 4, p = 0.05] (Table 1 and supplement I.2.).
The aqueous extract ofS. cuminiextract increased the latency and reduced the duration ofSE.
A drug may not prevent SE, but should at least delay its onset (Sharma et al. 2018; De Farias et al. 2022). The purpose of this trial was to test whether the extract could delay the onset of kainate-induced SE in mice not protected against SE.
There were significant inter-group differences in the latency to the onset of SE [F(6, 16) = 77.48, p < 0.0001] (Supplement II.1.). Administration of kainate to the kainate group resulted in a decrease (2.88 ± 0.26 min, p < 0.001) in SE latency time compared to the normal group (Fig. 2 A). Compared to the kainate group, the aqueous extract of S. cumini (144 mg/kg) remarkably increased this time by 64.56% (7.99 ± 0.01 min, p < 0.001). The effects of the extract were more marked than those of sodium valproate. Indeed, sodium valproate increased this time by 56.39% (6.26 ± 0.04 min, p = 0.0145) (Fig. 2 A).
The aqueous extract of S. cumini increased the latency (A) and decreased (B) duration of SE. Each value represents the mean ± SD (duration of SE) or mean with interquartile range (latency to onset of SE) of the group, n = 6. cp < 0.001; bp < 0.01 compared to the normal group and *** p < 0.001, * p < 0.05 compared to the kainate group. Normal = normal group treated with distilled water only ; Kainate = kainate group treated with distilled water; S.c28.8 – S.c288 = test groups treated with the different doses of the aqueous extract of S. cumini (28.8, 144, 72, and 288 mg/kg, respectively); SV = positive control group treated with sodium valproate (300 mg/kg) ; SE = status epilepticus ; min = minute
SE is a medical emergency associated with mortality in TLE patients (Hsieh et al. 2011; Gaínza-Lein et al. 2019; Kim et al. 2021). To improve quality of life and avoid unexpected death in patients, an antiepileptic drug must at least reduce the duration of SE (Hsieh et al. 2011; Gaínza-Lein et al. 2019; Kim et al. 2021). Thus, the effect of the extract on the duration of SE was assessed.
There were significant inter-group differences in the duration of SE [H (8) = 36.76, p < 0.0001] (Supplement II.2.). Administration of kainate to the kainate group resulted in a significant increase (17.14 ± 1.19 min, p < 0.001) in the duration of SE compared to the normal group (Fig. 2B). The extract (144 mg/kg) markedly decreased SE duration by 67.21% (5.82 ± 0.18 min, p < 0.001). The effects of the extract were similar to those of sodium valproate, which decreased this duration by 59.17% (6.88 ± 0.09 min, p = 0.05) (Fig. 2B).
The aqueous extract ofS. cuminiimproved the working memory of mice in the T-maze.
A major complaint in TLE patients is impairment of working memory (Groticke et al. 2008; Kiasalari et al. 2016; Kandeda et al. 2022a). Indeed, hippocampal sclerosis and the spread of seizures to the prefrontal cortex could explain why working memory is the most impaired, as this structure plays a critical role in the memory process (Abrahams et al. 1999; Groticke et al. 2008; Kiasalari et al. 2016; Mosiashvili et al. 2017). Therefore, the effect of the extract on working memory was evaluated by studying spontaneous alternation in the T-maze.
There were significant inter-group differences in the latency to choose the preferred arm in the T-maze [H (8) = 29.95, p < 0.001] (Supplement III.1.). Mice in the normal group took a long time to regain the preferred arm, while those in the kainate group took a shorter time to regain this preferred arm (p = 0.3098) (Fig. 3 A). Compared to the kainate group, the extract at all doses increased this time, with a greater effect (p < 0.001) at the dose of 144 mg/kg. Piracetam (standard nootropic and anti-amnesic drug) (p = 0.6638) and sodium valproate (standard antiepileptic drug) (p = 0.999) induced a nonsignificant increase in this time (Fig. 3 A).
The aqueous extract of S. cumini decreased the time taken to choose the preferred arm (A), decreased the number of returns in the starting arm (B), decreased the time spent in the preferred arm (C), increased the time spent in the discriminated arm (D), decreased the number of entries in the preferred arm (E), increased the number of entries in the discriminated arm (F). Each point represents the mean ± SD or mean with interquartile range (latency to choose preferred arm, and time spent in the preferred arm or discriminated), n = 6. bp < 0.01; ap < 0.05 compared to the normal group and *** p < 0.001; ** p < 0.01; * p < 0.05 compared to the kainate group. Normal = normal group treated with distilled water; Kainate = kainate group treated with distilled water ; S.c28.8 – S.c288 = test groups treated with the different doses of the aqueous extract of S. cumini (28.8, 72, 144, and 288 mg/kg, respectively) ; pira = positive control group treated with piracetam (200 mg/kg) ; SV = positive control group treated with sodium valproate (300 mg/kg); ns = nonsignificant
Significant inter-group differences were observed in the number of returns in the starting arm [F (7, 40) = 4.201, p = 0.0015] (Supplement III.2.). Mice from the normal group returned a few times in the starting arm, while those from the kainate group returned several times (p = 0.05) (Fig. 3B). Compared to the kainate group, the aqueous extract of S. cumini (144 mg/kg) markedly decreased the number of returns in the starting arm (p = 0.01). This decrease was more marked than that of piracetam (p = 0.05) (Fig. 3B).
Significant inter-group differences were observed in the time spent in the preferred arm [H (8) = 22.1, p < 0.001] or discriminated arm [H (8) = 23.6, p < 0.001] (Supplement III.3. and III.4.). Compared to the normal group, animals in the kainate group spent more time (p = 0.0209) in the preferred arm (Fig. 3 C) and few times (p = 0.999) in the discriminated arm (Fig. 3D). The aqueous extract of S. cumini (144 mg/kg) remarkably decreased (p < 0.001) the time spent in the preferred arm (Fig. 3 C) and increased (p < 0.001) this time in the discriminated arm (Fig. 3D), compared to the kainate group. piracetam induced a significant increase in the time spent in the discriminated arm (p = 0.481) (Fig. 3 C and D).
Significant inter-group differences were observed in the number of entries in the preferred arm [F (7, 40) = 4.262, p < 0.0013] or discriminated arm [F (7, 40) = 3.205, p < 0.0086] (Supplement III.5. and III.6.). Animals from the normal group entered the preferred arm (Fig. 3E) less than the discriminated arm (Fig. 3 F). However, those in the kainate group entered the preferred arm more than the discriminated arm (p = 0.01). Compared to the kainate group, the aqueous extract of S. cumini (144 mg/kg) remarkably decreased (p = 0.01) the number of entries in the preferred arm (Fig. 3E) and increased (p = 0.01) the number of entries in the discriminated arm (Fig. 3 F). The effects of the extract were greater than those of the positive control groups (piracetam and sodium valproate), which also increased this number in the discriminated arm (p = 0.05) (Fig. 3E and F).
The aqueous extract ofS. cuminireduced the long-term spatial memory of mice in the Morris water maze.
TLE is associated with impaired long-term spatial memory (Holler and Trinka 2014; Kiasalari et al. 2016; Tramoni-Negre et al. 2017). Therefore, an antiepileptic drug with ideally anti-amnesic effect against long-term memory is sought. The ability of the extract to prevent or reduce this memory impairment was evaluated in the Morris water maze.
Significant inter-group differences were observed in the time taken to find the hidden platform during the acquisition phase [F (7, 128) = 5.928, p < 0.0001] (Supplement IV.1.). Compared to the normal group, animals from the kainate group took longer (p = 0.01) to regain the platform during the last two days of the experiment (Fig. 4 A). The aqueous extract of S. cumini at all doses reduced (p < 0.001) the time spent to find the platform on the fourth day of the experiment, compared to the kainate group (Fig. 4 A). The effects of the extract were similar to those of piracetam (an anti-amnesic drug) (p < 0.001) (Fig. 4 A) and sodium valproate (an antiepileptic drug with GABA-enhancing effect) (p < 0.001) (Fig. 4 A).
The aqueous extract of S. cumini reduced the time taken to find the hidden platform during the acquisition phase (A) and increased the time spent in the target quadrant during the retention phase (B). Each point or curve represents the time performed by the animals in each group, and each point in the middle of each curve indicates the mean ± SD, n = 6. cp < 0.001; bp < 0.01 compared to the kainate group and *** p < 0.001; ** p < 0.01; * p < 0.05 compared to the kainate group. Normal = normal group treated with distilled water ; Kainate = kainate group treated with distilled water ; S.c28.8 – S.c288 = test groups treated with the aqueous extract of S. cumini (28.8, 72, 144, and 288 mg/kg, respectively) ; pira = positive control group treated with piracetam (200 mg/kg) ; SV = positive control group treated with sodium valproate (300 mg/kg) ; s = second; D = day; ns = nonsignificant
Significant inter-group differences were observed in the time spent in the target quadrant during the retention phase in the Morris water maze [H (8) = 24.4, p < 0.001] (Supplement IV.2.). The animals of the kainate group spent less time in the target quadrant (p = 0.690) as compared to the normal group (Fig. 4B). Compared to the kainate group, the animals treated with the extract (144 mg/kg) spent a greater time (p < 0.001) in the target quadrant (Fig. 4B). The effects of the aqueous extract of S. cumini were more marked than those of piracetam, a nootropic and anti-amnesic drug, which failed to induce a significant decrease (p = 0.282) (Fig. 4B).
The aqueous extract ofS. cuminiattenuated anxiety-like behavior in the open field.
Devices used to assess memory disorders are associated with anxiety, due to their anxiogenic environment (Rodgers and Dalvi 1997; Harrison et al. 2009). Therefore, performing such a test may lead to false-positive results, if a drug or extract is devoid of anxiolytic properties. To exclude the influence of anxiety on memory performance during testings, the anxiolytic effect of the extract was therefore determined.
Significant inter-group differences were observed in the time spent [H (8) = 29, p < 0.0001] and the number of lines crossed [F (7, 38) = 5.511, p < 0.0004] in the center of the open field (Supplement V.1 and V.2.). The animals in the kainate group crossed few lines (p = 0.01) (Fig. 5 A) and spent few times (p = 0.01) (Fig. 5B) in the center of the device, compared to the normal group. Compared to the kainate group, the aqueous extract of S. cumini (144 mg/kg) markedly increased the number of lines crossed (p < 0.001) (Fig. 5 A) and the time spent (p = 0.01) (Fig. 5B) in the center of the device. The effects of the extract were similar to those of piracetam, which increased the number of lines crossed (p < 0.001) (Fig. 5 A) and the time spent (p = 0.05) (Fig. 5B) in the center of the device.
The aqueous extract of S. cumini increased the time spent in the center (A), the number of lines crossed in the center (B), increased the number of straightenings (C), and reduced the number of groomings (D) in the open field. Each point represents the mean ± SD or mean with interquartile range (time spent in the center, number of straightenings, and number of groomings) of the group, n = 6. bp < 0.01; ap < 0.05 compared to the normal group and *** p < 0.001; ** p < 0.01; * p < 0.05 compared to the kainate group. Normal = normal group treated only with distilled water; Kainate = kainate group treated with distilled water ; S.c28.8 – S.c288 = test groups treated with the different doses of the aqueous extract of S. cumini (28.8, 72, 144, and 288 mg/kg, respectively); pira = positive control group treated with piracetam (200 mg/kg) ; SV = positive control group treated with sodium valproate (300 mg/kg) ; s = seconds; ns = nonsignificant
Significant inter-group differences were observed in the number of straightenings [H (8) = 20.92, p = 0.0039] and groomings [H (8) = 20.68, p = 0.0043] in the open field (Supplement V.3. and V.4.). Animals in the kainate group performed few straightenings (Fig. 5 C) and more groomings (p = 0.0164) (Fig. 5D), compared to the normal group. Compared to the kainate group, S. cumini extract (144 mg/kg) remarkably (p < 0.001) increased the number of straightenings (Fig. 5 C) and decreased the number of groomings (p = 0.01) (Fig. 5D). The effects of the extract were greater than those of the positive control groups, which failed to significantly increase the number of straightenings (Fig. 5 C) and decrease the number of groomings (Fig. 5 A).
The aqueous extract ofS. cuminireduced the concentration of some oxidative stress parameters in the hippocampus.
Oxidative stress is the first event that follows the permanent activation of NMDA receptors during kainate-induced SE (Cheng et al. 2004; Liang et al. 2007; Shin et al. 2011). Thus, a drug or extract with antioxidant properties could help to prevent the development of epilepsy or its aggravation.
Significant inter-group differences were observed in the concentration of MDA [F (7, 15) = 6.645, p < 0.0011] or GSH [F (7, 15) = 5.101, p = 0.0040] in the hippocampus (Supplement VI.1. and VI.2.). In the animals of the kainate group, kainate increased the concentration of MDA (p = 0.01) (Fig. 5 A) and decreased that of GSH (p = 0.05) (Fig. 6B), compared to the normal group. However, the extract decreased the concentration of MDA at the dose of 144 mg/kg (p < 0.001) (Fig. 6 A), while it increased that of GSH at the doses of 144 and 288 mg/kg (p = 0.01) (Fig. 6B), compared to the kainate group. The effects of the extract were greater than those of the positive control groups, which also decreased the concentration of MDA (p = 0.01) (Fig. 6 A) and increased that of GSH (p = 0.01) (Fig. 6B).
The aqueous extract of S. cumini reduced the concentration of MDA (A) and increased that of GSH (B) in the hippocampus. Each point represents the mean ± SD of the group, n = 6. bp < 0.01; ap < 0.05 compared to the normal group and *** p < 0.001; ** p < 0.01; * p < 0.05 compared to the kainate group. Normal = normal group treated only with distilled water ; Kainate = kainate group treated with distilled water ; S.c28.8- S.c288 = test groups treated with the different doses of the aqueous extract of S. cumini (28.8, 72, 144, and 288 mg/kg, respectively); pira = positive control group treated with piracetam (200 mg/kg) ; SV = positive control group treated with sodium valproate (300 mg/kg) ; MDA = malondialdehyde ; GSH = reduced glutathione
The aqueous extract ofS. cuminireduced in a dose-dependent manner the concentration of some pro-inflammatory cytokines in the hippocampus.
During kainate-induced SE, inflammatory response contributes to accelerating or exacerbating the development of epilepsy (Oprica et al. 2003; Lee et al. 2008; Ramazi et al. 2020). Thus, a drug or extract with anti-inflammatory properties could prevent or reduce the development of epilepsy or its aggravation.
Significant inter-group differences were observed in the concentration of TNF [F (7, 40) = 95.88, p < 0.0001], IL-6 [H (8) = 24.27, p = 0.0010], and IL-1β [H (8) = 42.36, p < 0.0001] in the hippocampus (Supplement VII.1, 2, and 3). Data show that there is an increase in the concentration of TNF (p < 0.001) (Fig. 7 A), IL-1β (p < 0.001) (Fig. 7B), and IL-6 (Fig. 7 C) in the animals of the kainate group compared to the normal group. Compared to animals in the kainate group, the aqueous extract at all doses and reference drugs lowered the concentration of TNF (p < 0.001) (Fig. 7 A). However, the effects of the extract (144 mg/kg) on the IL-6 and IL-1β concentrations were greater (p < 0.001) than those of the positive control groups (Fig. 7B and D).
The aqueous extract of S. cumini reduced in a dose-dependent manner the concentration of TNF (A), IL-6 (B), and IL-1β (C) in the hippocampus. Each point represents the mean ± SD or mean with interquartile range (concentration of IL-1β or IL-6), n = 6. cp < 0.001; bp < 0.01 compared to the normal group and *** p < 0.001; * p < 0.05 compared to the kainate group. Normal = normal group treated with distilled water only ; Kainate = kainate group treated with distilled water ; S.c28.8 – S.c288 = test groups treated with the different doses of the aqueous extract of S. cumini (28.8, 72, 144, and 288 mg/kg, respectively) ; pira = positive control group treated with piracetam (200 mg/kg) ; SV = positive control group treated with sodium valproate (300 mg/kg); TNF = tumor necrosis factor; IL-6 = interleukin six; IL-1β = interleukin 1 beta; ns = nonsignificant
Discussion
The objective of the present study was to assess the effects of an aqueous extract of S. cumini on SE and amnesia in mice treated with kainate. Thus, the aqueous extract of S. cumini significantly prevented the development of SE and protected mice from SE-induced mortality as compared to sodium valproate. In addition, the extract attenuated working memory impairment in the T-maze and long-term spatial memory in the Morris water maze as compared to piracetam. Neurochemical tests revealed that the aqueous extract significantly reduced oxidative stress and prevented inflammatory responses in the hippocampus.
TLE is a form of epilepsy characterized by the occurrence of partial complex seizures with secondary generalization (Golechha et al. 2011; Kandratavicius et al. 2014). This condition is due to excessive and hypersynchronous discharges that start in the temporal lobe and spread to the whole brain as secondarily generalized seizures (Golechha et al. 2011; Kandratavicius et al. 2014). The kainate model, developed by Ben-Ari in late 1970, is widely used to understand hippocampal hyperexcitability and epileptogenesis (Ben-Ari et al. 1979; Lévesque and Avoli 2013; Lévesque et al. 2016). Hence, the administration of kainate induces a severe and prolonged seizure called SE, which marks the starting point of the disease (Lévesque et al. 2016). SE is a prolonged or repeated seizure, that last at least 30 min, without a return to consciousness between seizures (Cherian and Thomas 2009; Curia et al. 2014; Moto et al. 2018). In the present study, kainate caused the development of SE in the kainate group. The administration of kainate also increased SE-induced mortality, increased the duration of SE, and reduced the latency to SE. These results corroborate those of Solomonia et al. (2010) and Hsieh et al. (2011) who induced TLE with kainate in mice and obtained similar results. Moreover, studies have pointed out the role of the kainate receptor complex in neuronal depolarization that causes hyperexcitability (Vincent and Mulle 2009; Falcon-Moya et al. 2018). The latter could be associated with a selective loss of inhibitory interneurons and major cells in the dentate gyrus, CA3, and CA1 regions (Tuunanen et al. 1996; Smith and Dudek 1997; Lévesque and Avoli 2013; Rattka et al. 2013; Holler et al. 2014). This hypothesis could therefore explain in part the development of SE and SE-induced mortality in mice (Cherian and Thomas 2009; Kim et al. 2021). It is well known that the interneurons in the dentate gyrus are generally GABA neurons. Since GABA neurons regulate the hyperexcitability of the pyramidal neurons in the dentate gyrus, the loss or alterations of these neurons could lead to SE or sudden unexpected death because of prolonged seizures (Wang et al. 2016; Dudek 2020). The aqueous extract of S. cumini, in a dose-dependent manner, significantly reduced the development of SE, with greater effect at the dose of 72 mg/kg. The extract at all doses protected mice against SE-induced mortality with complete protection at the doses of 72 and 144 mg/kg. In this study, we equally noticed that the highest doses of the extract (144 and 288 mg/kg) led to a high mortality rate, i.e. immediately after kainate injection. Since the injection of kainate could lead to death in rodents (Kandeda et al. 2022a, b), the administration of high doses of the extract could also explain some death in mice in this study. Hence, the mortality observed in the present study could be the action of high doses of the extract alone rather than the random effect of kainate injection. In addition, the fact that a normal group treated only with the extract was not added in the present study, the results obtained make it difficult to attribute the mortality observed in mice to the only action of kainate. In future studies, a toxicity study of the high doses of the extract will be performed to exclude the possibility of a toxic effect of the extract. Furthermore, the extract (144 mg/kg) significantly increased the latency to SE. The extract also significantly reduced the duration of SE with a greater effect at the dose of 144 mg/kg. Given that the extract significantly protected mice against the development of SE, and increased the latency to SE or decreased the duration of SE in non-protected mice, these results suggest that the extract may possess antiepileptic-like properties (Hsieh et al. 2011; Mante et al. 2017; Hockers 2019; Wang et al. 2021). These findings also are corroborated by previous studies on the anticonvulsant and sedative effects of the plant in rats (Chanudom and Tangpong 2015; De Lima et al. 1998). The fact that the effect of the extract was comparable to that of sodium valproate (Mattson et al. 1992; Romoli et al. 2019), an antiepileptic drug widely prescribed against TLE, these results suggest the extract could be effective against partial complex seizures (Mattson et al. 1992; Romoli et al. 2019). Further studies using other models of temporal epilepsy should be performed to confirm the obtained results. Additionally, these properties of the extract could be related to the presence of kaempferol, triterpenoids, and polyphenols, which are abundant in the extract. These compounds have been found to reduce the number and duration of seizures in electrical and chemical models of seizures in mice (De Lima et al. 1998; Luna et al. 2014; Taiwe et al. 2015). Also, studies reported beneficial effects of flavonoids and kaempferol on epilepsy, particularly in TLE (Kwon et al. 2019; Kandeda et al. 2021a, b).
TLE is often associated with memory disorders that affect short- and long-term memories (Abrahams et al. 1999; Groticke et al. 2008; Bonansco and Fuenzalida 2016; Kiasalari et al. 2016; Mosiashvili et al. 2017; Postnikova et al. 2017; Zhu et al. 2020).
Of all types of memory, working memory has gained much attention as evidenced by extensive literature. Working memory is the manipulation and retention of information for a short period in the prefrontal cortex or hippocampus (Zhao et al. 2014; Mosiashvili et al. 2017). Working memory impairment has clinical importance not only because it leads to altered quality of life, but also because of its relation to long-term memory (Abrahams et al. 1999; Groticke et al. 2008; Kiasalari et al. 2016; Mosiashvili et al. 2017). In the present study, the injection of kainate to the distilled water treated mice caused an increase in the number of entries and the time spent in the preferred arm of the T-maze. However, it decreased these parameters in the discriminated arm. These results are in agreement with those of Gorantla et al. (2016) and Kandeda et al. (2021b) who induced TLE with kainate in rodents and obtained similar results. The fact that the mice did not remember the first choice suggests an alteration of working memory (Wenk 2001; Lainiola et al. 2014; Prieur and Jadavji 2019; Kandeda et al. 2022a). Studies showed that epileptic patients are often subjected to working memory impairment (Abrahams et al. 1999; Kiasalari et al. 2016; Mosiashvili et al. 2017). Indeed, working memory amnesia is associated with a decrease in synaptic plasticity in the hippocampus (Rattka et al. 2013; Postnikova et al. 2017) and correlated dysfunction in the prefrontal cortex (Jin and Maren 2015; Mosiashvili et al. 2017). The aqueous extract of S. cumini, in a dose-dependant manner, with the greatest effect at the dose of 144 mg/kg, significantly increased the number of entries and time spent in the discriminated arm, indicating that the mice recall the preferred arm that they visited. These results suggest therefore anti-amnesic-like properties of the extract against working memory impairment (Hasselmo 2006; Vorhees and Williams 2014; Hussein et al. 2018; Kandeda et al. 2021b). These effects could be mediated by an interaction of the extract with the cholinergic neurotransmission. Indeed, several studies revealed the presence of major compounds such as betulinic acid, Beta-sitosterol, and kaempferol-3-0- glucoside in the extract. However, these compounds have been shown to modulate and interact with cholinergic neurotransmission (Ayaz et al. 2017; Rebas et al. 2020; Lee et al. 2021). Thus, further studies have to be performed to determine the direct action of the extract on the cholinergic neurotransmission. The anti-amnesic effect of the extract could be also mediated by the protective effect against the loss of the neurons involved in the working memory process (Abrahams et al. 1999; Hasselmo 2006; Groticke 2008; Kiasalari et al. 2016; Mosiashvili et al. 2017). Thus, further studies are needed to determine the exact mechanism of action by which the extract exerts its anti-amnesic effect. The fact that the seeds of the same plant have been shown to improve memory in Alzheimer’s disease models in rats, these findings equally suggest the presence of bioactive molecules with anti-amnesic potential (Hossain et al. 2017). Furthermore, the anti-amnesic effect of the extract could be correlated to its antiepileptic-like activities. Indeed, limiting the excessive discharge and neuronal loss in the hippocampus has been shown to reduce memory impairment in rodents (Nygaard et al. 2015; Clossen and Reddy 2017).
Memory impairments are common in TLE patients, where memory-related brain regions are involved in the generation of epileptic discharge (Tramoni-Negre et al. 2017). Accumulating evidence suggested that TLE may also alter long-term memory. This condition generates therefore the loss of autobiographical information and an inability to store new information over a long period (Holler and Trinka 2014; Kiasalari et al. 2016). In this study, the Morris water maze test was used to assess long-term spatial memory deficit. The results of this test showed that kainate significantly increased the time taken to find the hidden platform during the acquisition phase in the kainate group. It equally decreased the time spent in the target quadrant during the retention phase in the same group. These data corroborate those of Zeng et al. (2013), Kandeda et al. et al. (2022a), and Kandashvili et al. (2022) who induced long-term spatial memory loss in the Morris water maze with kainate and made similar observations. Numerous studies showed that in rodents, an injury in the hippocampus (part of the brain involved in long-term memorization) leads to a deficit in the processes of spatial learning and memory (Shors et al. 1992; Luine et al. 1994; Tramoni-Negre et al. 2017; Voss et al. 2017). Treatment of mice with the aqueous extract of S. cumini, at the doses of 144 and 288 mg/kg, reversed these effects as compared to the kainate group. These effects were greater than those of piracetam, a nootropic and anti-amnesic drug (Chaudhry et al. 1992; Pohle et al. 1997; Fisher et al. 2004; Chaudhari et al. 2013). These data suggest therefore that the aqueous extract possesses anti-amnesic-like properties against long-term spatial memory (Bolanos et al. 1998; Hubens et al. 2014). Furthermore, the seeds or the methanolic extract of the same plant showed an anti-amnesic effect against long-term memory in an animal model of Alzheimer’s disease (Alikatte et al. 2012; Hossain et al. 2017). These observations also suggest the presence of bioactive molecules in the extract with an anti-amnesic effect against long-term spatial memory impairment (De Lima et al. 1998; Alikatte et al. 2012; Ayyanar and Subash-Babu 2012; Bijauliya et al. 2017; Hossain et al. 2017; Abdin et al. 2020). Further studies have to be performed in other models of long-term memory impairment to confirm the obtained results, and to unravel the mechanism of action of the extract.
Devices used to evaluate memory impairments are often associated with anxiety-like behavior, due to their anxiogenic configuration (Rodgers and Dalvi 1997; Harrison et al. 2009). Therefore, to exclude the influence of anxiety-like behavior on memory performance during testings, the anxiolytic effect of the extract was performed. In the present study, the locomotor activity of each animal was assessed in the open field. The results showed that kainate caused a significant decrease in the number of lines crossed, straightenings, and time spent in the center as compared to the kainate group. It also increased the number of groomings. These conditions demonstrated an increase in anxiety-like behavior in animals (Maia et al. 2014; Mohd et al. 2018; Kandeda et al. 2021). Kainate increases GABA-transaminase activity and decreases brain GABA concentration, as well as the density of GABA receptors in the striatum, frontal cortex, and hippocampus (Sperk et al. 2003; Ngo Bum et al. 2012; Kandeda et al. 2022a, b). This dysfunction is at the origin of the excitability of the brain, and consequently of the anxious state of animals (Maia et al. 2014; Mohd et al. 2018). Treatment of mice with the aqueous extract of S. cumini, with greater effect at the dose of 144 mg/kg, alleviated these alterations and induced opposite effects to those of the kainate group. These results suggest that the aqueous extract of S. cumini may contain compounds with anxiolytic-like properties (Ngo Bum et al. 2009; Beppe et al. 2015; Kandeda et al. 2022a). These findings are confirmed by the sedative effect of the extract demonstrated by Hossein et al. (2017). In addition, these results also suggest that the anti-amnesic-like effects of the extract are possibly favored by its anxiolytic effect. Indeed, anxiolytic drugs promote exploratory behavior in animals by reducing anxiety and stress caused by an anxiogenic device environment (Kilfoil et al. 1989; Cryan and Sweeny 2011). Hence, exploratory behavior is strongly associated with a memory-enhancing activity (Kilfoil et al. 1989; Cryan and Sweeny 2011).
Oxidative stress is an imbalance between the production of radical (or reactive) oxygen species and antioxidant cellular capacities (Hsieh et al. 2011; Aguiar et al. 2021; Pizzino et al. 2017). Oxidative stress participates in the pathogenesis of many neurodegenerative diseases (Wang et al. 2005; Shin et al. 2011; Ngo Bum et al. 2012; Cenini et al. 2019). In the present research, data revealed that kainate caused oxidative stress in the hippocampus of the kainate group. This was marked by an increase in the concentration of MDA. The kainate also decreased that of GSH. These results corroborate those of Huang et al. (2012) and Ramazi et al. (2020). It is well known that following the injection of kainate to rodents, this molecule activates kainate receptors and leads to increased glutamate concentration in the synaptic cleft. This in turn generates excitotoxicity associated with dysfunction of the mitochondrial respiratory chain, ROS or free radicals production, and subsequent neuronal damage (Cheng et al. 2004; Liang et al. 2007; Shin et al. 2011). With a reduced supply of GSH, free radicals or ROS react quickly with neighboring macromolecules such as (DNA, proteins, lipoproteins, and membrane phospholipids with MDA production) and damage them (Jacoby et al. 2015; Vezzani et al. 2016; Liu et al. 2017). Besides, the injection of kainate could increase the density of glutamatergic receptors and decrease the number of gabaergic receptors in the hippocampus. These dysfunctions also contribute to excitotoxicity, and subsequently to ROS production (Khamse et al. 2015; Taiwe et al. 2015; Lin et al. 2020). Administration of the aqueous extract of S. cumini (at all doses) is remarkably associated with a decrease in the concentration of MDA and an increase in that of GSH as compared to the kainate group. The brain possesses antioxidant systems including catalase, reduced glutathione, and superoxide dismutase. These proteins have been shown to alleviate oxidative stress-induced damage (Khamse et al. 2015). The fact that the extract reduced oxidative stress in treated mice, these results suggest an antioxidant-like property of S. cumini (Hsieh et al. 2011; Huang et al. 2012; Cheng et al. 2021). These results also confirm the abundant literature on the antioxidant-like properties of S. cumini (Katiyar et al. 2016; Santos et al. 2020). Otherwise, these properties of the extract could be related to their richness in alkaloids, anthocyanins, flavonoids triterpenoids, and flavonoids, whose neuroprotective-like properties are strongly correlated to their ability to eliminate free radicals or ROS (Adebesin et al. 2015; Foyet et al. 2015). Other studies have to be performed to unravel the antioxidant mechanisms of the extract.
Inflammation is considered to be one of the most important mechanisms contributing to the pathogenesis or recurrence of seizures (Renaud et al. 2015; Feng et al. 2016; Ramazi et al. 2020). In addition, excitotoxicity, inflammatory response, and oxidative stress are three processes involved in the development of so-called secondary lesions during the chronic phase of epilepsy (Renaud et al. 2015; Feng et al. 2016; Ramazi et al. 2020). Accumulating studies in rodents suggested the involvement of inflammatory processes in the pathogenesis of TLE (Golechha et al. 2011). Pro-inflammatory cytokines such as TNF, IL-1β, and IL-6 are overexpressed following the injection of chemoconvulsants such as kainate (Golechha et al. 2011). Thus, therapeutic strategies that target inflammatory pathways constitute a hope to find a cure against TLE. The pro-inflammatory cytokine assay in the present study showed that kainate markedly increased the concentration of all cytokines tested (TNF, IL-6, and IL-1β) in the hippocampus of the kainate group. These results are consistent with those of Hsieh et al. (2011), Ho et al. (2015), Vezzani et al. (2015), and Kandeda et al. (2021a) who reported that the injection of kainate to rodents is associated with a significant increase in the concentration of TNF, IL-6, and IL-1β. Indeed, the administration of kainate is highly associated with pro-inflammatory cytokine synthesis (Feng et al. 2016; Ojo et al. 2019; Lin et al. 2020). The inflammatory reaction after kainate-induced SE leads to the activation of nitric oxide synthase inducible (iNOS). This latter causes the synthesis of nitric oxide which reacts with ROS and exacerbates oxidative stress in kainate-induced SE (Lin et al. 2020). According to several studies, this synthesis is caused by the activation of microglia, macrophages, endothelial cells, and neutrophils (Mohd et al. 2015; Feng et al. 2016; Lin et al. 2020). Treatment of mice with the aqueous extract of S. cumini, in a dose-dependent manner, significantly decreased the concentration of all cytokines tested as compared to the kainate group. These results demonstrate that the aqueous extract of S. cumini is likely endowed with anti-inflammatory properties (Golechha et al. 2011; Mohd et al. 2015, 2018; Kandeda et al. 2021b). The results corroborate previous findings on the anti-inflammatory properties of S. cumini stem bark (Muruganandan et al. 2001). These activities could be related to the presence in this extract of phenolic compounds such as triterpenoids and flavonoids (Muruganandan et al. 2001; Lim 2012; Jagetia et al. 2008; Koepp et al. 2017). Triterpenoids have been shown to interact with intracellular neuronal or glial signaling pathways involved in inflammation (Luna et al. 2014). Also, flavonoids were revealed to reduce the expression of pro-inflammatory cytokines, as well as the activation of nuclear factor-κB (NFkB) in neurons (Khamse et al. 2015; Koepp et al. 2017). Regarding the implications of several factors in vivo assays, in vitro studies need to be performed for a better understanding of the exact molecular mechanisms of the extract.
Conclusions
The objective of the present investigation was to study the antiepileptic- and anti-amnesic-like effects of the aqueous extract of S. cumini on kainate-treated mice, and possible mechanisms of action. Compared to the normal control group, the administration of kainate caused SE in all mice of the kainate group and altered the working memory in these mice by increasing the time spent in the preferred arm. The injection of kainate equally altered the long-term memory in mice by increasing the time spent in the target quadrant during the retention phase. Treatment with the aqueous extract of S. cumini, as well as with sodium valproate (a widely prescribed antiepileptic drug), effectively protected the mice against kainate-induced SE or mortality. The aqueous extract of S. cumini also improved working memory and long-term memory in mice by increasing the time spent in the discriminated arm and the time spent in the target quadrant, respectively. Furthermore, the extract significantly increased the concentration of GSH and decreased that of MDA. The concentration of pro-inflammatory cytokines (TNF, IL-1β, and IL-6) in the hippocampus was also reduced following the administration of the aqueous extract of S. cumini. These results suggest that the aqueous extract of S. cumini possesses antiepileptic- and anti-amnesic-like effects. These effects are likely mediated in part by antioxidant and anti-inflammatory activities. Although the study of other parameters is essential to understanding the pharmacodynamic effects of this extract, these results validate the traditional use of the aqueous extract of S. cumini against epilepsy and associated comorbidities.
Data Availability
Data used to support the findings of this study are available from the corresponding author upon request.
Abbreviations
- S. cumini :
-
Syzygium cumini.
- SE :
-
status epilepticus.
- TLE:
-
temporal lobe epilepsy.
- MDA:
-
malondialdehyde.
- GSH:
-
reduced glutathione.
- TNF:
-
tumor necrosis.
- IL-6:
-
interleukin six.
- IL-1β:
-
interleukin one beta.
- SV:
-
sodium valproate.
- pira:
-
piracetam.
- SD:
-
standard deviation.
- ANOVA:
-
analysis of variance.
- ROS:
-
reactive oxygen species.
- i.p.:
-
intraperitoneally.
- po :
-
per os.
References
Abdin M, Hamed YS, Akhtar HMS, Chen D, Chen G, Wan P, Zeng X (2020) Antioxidant and anti-inflammatory activities of target anthocyanins di‐glucosides isolated from Syzygium cumini pulp by high-speed counter‐current chromatography. J Food Biochem 44(6):1050–1062
Abrahams S, Morris RG, Polkey CE, Jarosz JM, Cox TC, Graves M, Pickering A (1999) Hippocampal involvement in spatial and working memory: a structural MRI analysis of patients with unilateral mesial temporal lobe sclerosis. Brain Cogn 41(1):39–65
Adebesin I, Akindele A, Adeyemi O (2015) Evaluation of neuropharmacological effects of aqueous leaf extract of Albizia glaberrima (Leguminosae) in mice. J Ethnopharmacol 160:101–108
Aguiar CC, Almeida AB, Araújo PV, Abreu RN, Chaves EM, Vale OC, Macêdo DS, Woods DJ, Fonteles MM, Vasconcelos SM (2021) Oxidative stress and epilepsy: literature review. Oxid Med Cell Longev 2012: :795259
Akhtar M, Randhawa MA, Iqbal Z (2016) Nutritional, Therapeutic and Food Applications of Jamum (Syzygium cumini). Can J Food Sci Technol 1:1–8
Alikatte KL, Akondi BR, Yerragunta VG, Veerareddy PR, Palle S (2012) Antiamnesic activity of Syzygium cumini against scopolamine-induced spatial memory impairments in rats. Brain Dev 34(10):844–851
Ayaz M, Junaid M, Ullah F, Subhan F, Sadiq A, Ali G, Ahmad S (2017) Anti-Alzheimer’s studies on β-sitosterol isolated from Polygonum hydropiper L. Front Pharmacol 8:697
Ayyanar M, Subash-Babu P (2012) Syzygium cumini (L.) Skeels: A review of its phytochemical constituents and traditional uses. Asian Pac J Trop Biomed 2(3):240–246
Ba-Diop A, Marin B, Druet-Cabanac M, Ngougou M, Newton C, Preux P (2014) Epidemiology, causes, and treatment of epilepsy in sub-Saharan Africa. Lancet Neurol 13(10):1029–1044
Belzung C (1999) Measuring rodent exploratory behavior. Techniques Behavioral and neural sciences. Vol. 13. Elsevier, 1999. 738–749
Ben-Ari Y, Lagowska J, Tremblay E, Le GSG (1979) A new model of focal status epilepticus: intra-amygdaloid application of kainic acid elicits repetitive secondarily generalized convulsive seizures. Brain Res 163:176–179
Beppe G, Dongmo A, Foyet H, Tsabang N, Olteanu Z, Cioanca O (2015) Memory-enhancing activities of the aqueous extract of Albizia adianthifolia leaves in the 6-hydroxydopamine-lesion rodent model of Parkinson’s disease. Evid Based Complementary Altern 14:1–11
Bertoglio D, Amhaoul H, Van Eetveldt A, Houbrechts R, Van De Vijver S, Ali I, Dedeurwaerdere S (2017) Kainic acid-induced post status epilepticus models of temporal lobe epilepsy with diverging seizure phenotype and neuropathology. Front Neurol 8:588
Bijauliya RK, Alok S, Singh M, Mishra SB (2017) Morphology, phytochemistry and pharmacology of Syzygium cumini (Linn.)-an overview. Int J Pharm Sci Res 8(6):2360–2371
Bolanos AR, Sarkisian M, Yang Y, Hori A, Helmers SL, Mikati M, Tandon P, Stafstrom CE, Holmes GL (1998) Comparison of valproate and phenobarbital treatment after status epilepticus in rats. Neurology 51(1):41–48
Bonansco C, Fuenzalida M(2016) Plasticity of hippocampal excitatory-inhibitory balance: Missing the synaptic control in the epileptic brain.Neural Plast1–13
Broadbent NJ, Larry RS, Robert EC (2006) Reversible hippocampal lesions disrupt water maze performance during both recent and remote memory tests. Learn Mem 13(2):187–191
Butler CR, Zeman AZ (2008) Recent insights into the impairment of memory in epilepsy: transient epileptic amnesia, accelerated long-term forgetting, and remote memory impairment. Brain 131(9):2243–2263
Cenini G, Lloret A, Cascella R (2019) Oxidative stress in neurodegenerative diseases: from a mitochondrial point of view. Oxi Med Cell Long 2019: 2105607
Chanudom L, Tangpong J (2015) Anti-inflammation property of Syzygium cumini (L.) skeels on indomethacin-induced acute gastric ulceration. Gastroenterol Res Pract 2015:343642
Chaudhari SR, Dhande PP, Pandit VA (2013) Role of piracetam on cognitive function in epilepsy and with antiepileptics in rats. Int J Basic Clin Pharmacol 2(5):634
Chaudhry HR, Najam N, De Mahieu C, Raza A, Ahmad N (1992) Clinical use of piracetam in epileptic patients. Curr Ther Res 52(3):355–360
Chauhan A, Intelli (2015) Syzygium cumini (Jamun): Potential Benefits in Hyperglycemia. SOJ Pharm Pharm Sci 2(3):1–3
Cheng H, Fu YS, Guo JW (2004) Ability of GDNF to diminish free radical production leads to protection against kainate-induced excitotoxicity in hippocampus. Hippocampus 14(1):77–86
Cheng Y, Cui Y, Zhai Y, Xin W, Yu Y, Liang J, Li S, Sun H (2021) Neuroprotective effects of exogenous irisin in kainic acid-induced status epilepticus. Front Cell Neurosci 2021:396
Cherian A, Thomas SV (2009) Status epilepticus. Ann Indian Acad Neurol 12(3):140
Chin JH (2012) Epilepsy treatment in sub-Saharan Africa: closing the gap. Afr Health Sci 12(2):186–192
Clossen BL, Reddy DS (2017) Novel therapeutic approaches for disease-modification of epileptogenesis for curing epilepsy. Biochim Biophys Acta Mol Basis Dis 1863(6):1519–1538
Cryan JF, Sweeney FF (2011) The age of anxiety: role of animal models of anxiolytic action in drug discovery. Br J Pharmacol 164(4):1129–1161
Curia G, Lucchi C, Vinet J, Gualtieri F, Marinelli C, Torsello A, Costantino L, Biagini G (2014) Pathophysiogenesis of mesial temporal lobe epilepsy: is prevention of damage antiepileptogenic? Curr Med Chem 21(6):663–688
Deacon RM, Rawlins JN (2006) T-Maze Alternation in the Rodent. Nat Protoc 1:7–12
De Lima TC, Klüeger PA, Pereira PA, Macedo-Neto WP, Morato GS, Farias MR (1998) Behavioural effects of crude and semi‐purified extracts of Syzygium cuminii linn. skeels. Phytother Res 12(7):488–493
De Farias ACS, de Pieri Pickler K, Bernardo HT, Baldin SL, Dondossola ER, Rico EP (2022) Melatonin Pretreatment Protects Against status epilepticus, glutamate transport, and oxidative stress induced by kainic acid in zebrafish. Mol Neurobiol 59(1):266–275
Dibong SD, Mvogo PB, Vandi D, Ndjib RC, Monkam TF Mpondo
E (2015) Ethnobotanique des plantes médicinales anti hémorroïdaires des marchés
et villages du Centre et du Littoral Cameroun. J Appl Biosci 96: 9072–9093
Dieckmann-Schuppert A, Schnittler HJ (1997) A simple assay for quantification of protein in tissue sections, cell cultures, and cell homogenates, and protein immobilized on solid surfaces. Cell Tissue Res 288(1):119–126
Dudek FE (2020) Loss of GABAergic Interneurons in Seizure-Induced Epileptogenesis—Two Decades Later and in a More Complex World. Epilepsy Curr 20(6):70–72
Ekor M (2014) The growing use of herbal medicines: issues relating to adverse reactions and challenges in monitoring safety. Front Pharmacol 4:177
Ellman GL (1959) Tissue sulfhydryl groups. Arch Biochem Biophys 82(1):70–77
Ezhilarasan D, Apoorva VS, Ashok Vardhan N (2019) Syzygium cumini extract induced reactive oxygen species-mediated apoptosis in human oral squamous carcinoma cells. J Oral Pathol Med 48(2):115–121
Esterhuizen AI, Carvill GL, Ramesar RS, Kariuki SM, Newton CR, Poduri A, Wilmshurst JM (2018) Clinical application of epilepsy genetics in Africa: is now the time? Front Neurol 9:276
Feng B, Tang Y, Chen B, Xu C, Wang Y, Dai Y, Wu D, Zhu J, Wang S, Zhou Y, Shi L, Hu W, Zhang X (2016) Transient increase of interleukin-1beta after prolonged febrile seizures promotes adult epileptogenesis through long-lasting up-regulating endocannabinoid signaling. Sci Rep 581:482–492
Falco-Walter JJ, Scheffer IE, Fisher RS (2018) The new definition and classification of seizures and epilepsy. Epilepsy Res 139:73–79
Falcon-Moya R, Sihra TS, Rodríguez-Moreno A (2018) Kainate receptors: role in epilepsy. Front Mol Neurosci 11:217
Fischer W, Kittner H, Regenthal R, Russo E, De Sarro G (2004) Effects of piracetam alone and in combination with antiepileptic drugs in rodent seizure models. J Neural Transm 111(9):1121–1139
Fisher R, Acevedo C, Arzimanoglou A (2014) ILAE official report: a practical clinical definition of epilepsy. Epilepsia 55:475–482
Fisher RS, Bonner AM (2018) The revised definition and classification of epilepsy for neurodiagnostic technologists. Neurodiagn J 58(1):1–10
Foyet H, Abdou B, Ngatanko A, Eglantine W, Emmanuel A, Ciobica A (2015) Emilia coccinae Extract improves memory impairment, cholinergic dysfunction, and oxidative stress damage in scopolamine-treated rats Evid-Based. Complement Altern Med 13:1–12
Fritsch B, Stott JJ, Joelle Donofrio J, Rogawski MA (2010) Treatment of early and late kainic acid-induced status epilepticus with the noncompetitive AMPA receptor antagonist GYKI 52466. Epilepsia 51(1):108–117
Gaínza-Lein M, Fernández IS, Ulate-Campos A, Loddenkemper T, Ostendorf AP (2019) Timing in the treatment of status epilepticus: from basics to the clinic. Seizure 68:22–30
Golechha M, Bhatia J, Ojha S, Arya DS(2011) Hydroalcoholic extract of Emblica officinalis protects against kainic acid-induced status epilepticus in rats: Evidence for an antioxidant, anti-inflammatory, and neuroprotective intervention.Pharm Biol1–9
Gorantla VR, Pemminati S, Bond V, Meyers DG, Millis RM (2016) Effects of swimming exercise on learning and memory in the kainate-lesion model of temporal lobe epilepsy. J Clin Diagn Res 10(11):1–5
Groticke I, Hoffmann K, Loscher W (2008) Behavioral alterations in a model of temporal epilepsy induced by injection of kainate acid. Exp Neurol 213(1):71–83
Hasselmo ME (2006) The role of acetylcholine in learning and memory. Curr Opin Neurobiol 16(6):710–715
Harrison FE, Hosseini AH, McDonald MP (2009) Endogenous anxiety and stress responses in water maze and Barnes maze spatial memory tasks. Behav Brain Res 198(1):247–251
Ho YH, Lin YT, Wu CWJ, Chao YM, Chang AY, Chan JY (2015) Peripheral inflammation increases seizure susceptibility via the induction of neuroinflammation and oxidative stress in the hippocampus. J Biomed Sci 22(1):1–14
Hockers S (2019) Why do patients die after status epilepticus? Epilepsy Behav 101:106567
Holler Y, Trinka E (2014) What do temporal lobe epilepsy and progressive mild cognitive impairment have in common. Front Syst Neurosci 8:58
Hossain S, Islam J, Bhowmick S, Haque M, Rahaman A (2017) Effects of Syzygium cumini seed extract on the memory loss of Alzheimer’s disease model rats. Adv Alzheimer Dis 6(3):53–73
Hsieh PF, Hou CW, Yao PW, Wu SP, Peng YF, Shen ML, Lin CH, Chao YY, Chang MH, Jeng KC (2011) Sesamin ameliorates oxidative stress and mortality in kainic acid-induced status epilepticus by inhibition of MAPK and COX-2 activation. J Neuroinflam 8(1):1–10
Huang HL, Lin CC, Jeng KC, Yao PW, Chuang LT, Kuo SL, Hou CW (2012) Fresh green tea and gallic acid ameliorate oxidative stress in kainic acid-induced status epilepticus. J Agric Food Chemistry 60(9):2328–2336
Hubens CJ, Kaptein PS, Horst JP, Voskuyl RA, Schenk GJ (2014) Kainate-induced epileptogenesis alters circular hole board learning strategy but not the performance of C57BL/6J mice. Epilepsy Behav 41:127–137
Hussein AM, Bezu M, Korz V(2018) Evaluating working memory on a T-maze in male rats.Bio Protoc8(14)
Iwuoha VC, Ezinwann NEzeibe, Ezeibe CC (2020) Glocalization of COVID-19 responses and management of the pandemic in Africa. Local Env 25(8):641–647
Ismail F, Fatemi A, Johnston M (2017) Cerebral plasticity windows of opportunity in the developing brain. Europ J Paediatr Neurol 21:23–48
Jacoby A, Snape D, Lane S, Baker G (2015) Self-reported anxiety and sleep problems in people with epilepsy and their association with quality of life. Epilepsy Behav 43:149–158
Jaimes-Bautista AG, Rodríguez-Camacho M, Martínez-Juárez IE, Rodríguez-Agudelo Y(2015) Semantic processing impairment in patients with temporal lobe epilepsy. Epilepsy Res Treat 2015: 746745
Jagetia GC, Shetty PC, Vidyasagar MS (2008) Treatment of mice with leaf extract of jamun (Syzygium cumini linn. Skeels) protects against the radiation-induced damage in the intestinal mucosa of mice exposed to different doses of γ-radiation. Pharmacologyonline 1:169–195
Jha S (2017) Transgenesis and Secondary Metabolism.Cham. Springer, Switzerland, pp 1–20
Jin J, Maren S (2015) Prefrontal-hippocampal interactions in memory and emotion. Front Syst Neurosci 9:170
Kimiskidis VK, Valeta TJ (2012) Epilepsy and anxiety: epidemiology, classification, aetiology, and treatment. Epileptic Disord 14(3):248–256
Kiasalari Z, Khalili M, Shafiee S, Roghani (2016) The effect of vitamin E on learning and memory deficits in intrahippocampal kainate-induced temporal lobe epilepsy in rats. Indian J Pharmacol 48(1):11–14
Kandashvili M, Gamkrelidze G, Tsverava L, Lordkipanidze T, Lepsveridze E, Lagani V, Burjanadze M, Dashniani M, Kokaia M, Solomonia R (2022) Myo-inositol limits kainic acid-induced epileptogenesis in rats. Int J Mol Sci 23(3):1198
Kandeda KA, Taiwe SG, Moto FC, Ngoupaye TG, Nkantchoua G, Njapdounke SK, Omam JP, Pale S, Kouemou N, Ngo bum E (2017) Antiepileptogenic and neuroprotective effects of Pergularia daemia on pilocarpine model of epilepsy. Front Pharmacol 8:426–440
Kandeda KA, Moto FCO, Ayissi MRE, Omam OJP, Ojong L, Ngo Bum E (2021a) Pergularia daemia hydro-ethanolic extract protects against pentylenetetrazole kindling-induced seizures, oxidative stress, and neuroinflammation in mice. J Ethnopharmacol 279:114338
Kandeda KA, Moto FCO, Omam OJP, Ayissi MRE, Ojong L, Ngo Bum E (2021b) Pergularia daemia alters epileptogenesis and attenuates cognitive impairment in kainate-treated mice: Insight into anti-inflammatory mechanisms. Epilepsy Behav 1:115:107707
Kandeda KA, Mabou ST, Moutchida C (2022a) An aqueous extract of Lantana camara attenuates seizures, memory impairment, and anxiety in kainate-treated mice: Evidence of GABA level, oxidative stress, immune and neuronal loss modulation. Epilepsy Behav 129:108611
Kandeda KA, Lewale S, Djeuzong E, Kouamouo J, Dimo T(2022b) An aqueous extract of Khaya senegalensis (Desv.) A. Juss. (Meliaceae) prevents seizures and reduces anxiety in kainate-treated rats: Modulation of GABA neurotransmission, oxidative stress, and neuronal loss in the hippocampus. Heliyon 8 (5): e09549
Kandratavicius L, Balista P, Lopes-Aguiar C, Ruggiero R, Umeoka E, Garcia Cairasco N (2014) Animal models of epilepsy use and limitations. Neuropsychiatr Dis Treat 10:1693–1705
Katiyar D, Singh V, Ali M (2016) Recent advances in pharmacological potential of Syzygium cumini. Adv Appl Sci Res 7:1–12
Khamse S, Sadr SS, Roghani M, Hasanzadeh G, Mohammadian M (2015) Rosmarinic acid exerts a neuroprotective effect in the kainate rat model of temporal lobe epilepsy: Underlying mechanisms. Pharm Biol 53(12):1818–1825
Kilfoil T, Michel A, Montgomery D, Whiting RL (1989) Effects of anxiolytic and anxiogenic drugs on exploratory activity in a simple model of anxiety in mice. Neuropharmacology 28(9):901–905
Kim D, Kim JM, Cho YW, Yang KI, Kim DW, Lee ST, No YJ, Seo JG, Byun JI, Kang KW, Kim KT (2021) Antiepileptic drug therapy for status epilepticus. J Clin Neurol 17(1):11
Koepp M, Arstad E, Eurwaerdere S, Friedman A, Potschka H, Ravizza T, Baram T (2017) Neuroinflammation imaging markersstatus for epileptogenesis. Epilepsia 58:11–19
Kuate T, Doumbe J, Kammegne Y, Noubissi G, Djientcheu V (2015) Les épilepsies du sujet âge aspect épidémiologiques dans deux centres de santé urbains de la ville de Douala (Cameroun). Heath Sci Dis 16:1–6
Kwon JY, Jeon MT, Jung UJ, Kim DW, Moon GJ, Kim SR (2019) Perspective: Therapeutic potential of flavonoids as alternative medicines in epilepsy. Adv Nutr 10:778–790
Lan L, Lian Z (2010) Application of statistical power analysis–How to determine the right sample size in human health, comfort and productivity research. Build Env 45(5):1202–1213
Lainiola M, Procaccini C, Linden AM (2014) mGluR3 knockout mice show a working memory defect and an enhanced response to MK-801 in the T-and Y-maze cognitive tests. Behav Brain Res 266:94–103
Lee JK, Won JS, Singh AK, Singh I (2008) Statin inhibits kainic acid-induced seizure and associated inflammation and hippocampal cell death. Neurosci Lett 440(3):260–264
Lee S, Jung W, Eom S, Yeom HD, Park HD, Lee JH (2021) Molecular regulation of betulinic acid on α3β4 nicotinic acetylcholine receptors. Molecules 26(9):2659
Lévesque M, Avoli MJ (2013) The kainic acid model of temporal lobe epilepsy. Neurosci Biobehav Rev 37(10):2887–2899
Lévesque M, Avoli M, Bernard C (2016) Animal models of temporal lobe epilepsy following systemic chemoconvulsant administration. J Neurosci Methods 260:45–52
Liang LP, Beaudoin ME, Fritz MJ, Fulton R, Patel M (2007) Kainate-induced seizures, oxidative stress and neuronal loss in aging rats. Neuroscience 147(4):1114–1118
Lim TK (2012) Edible medicinal and non-medicinal plant. Springer, London, pp 745–759
Lima EM, Gois J, Paiva ML, Vincentiis S, Moschetta S, Valente KD (2021) Anxiety symptoms are the strongest predictor of quality of life in temporal lobe epilepsy. Seizure 88:78–82
Lin TK, Chen SD, Lin KJ, Chuang YC (2020) Seizure-induced oxidative stress in status epilepticus: is antioxidant beneficial? Antioxidants 9(11):1029
Liu Z, Zhou T, Ziegler AC, Dimitrion P, Zuo L(2017) Oxidative stress in neurodegenerative diseases: from molecular mechanisms to clinical applications. Oxid Med Cell Longev 2017
Luna B, Bhatia S, Yoo C, Felty Q, Sandberg D, Duchowny M, Khatib Z, Miller I, Ragheb J, Prasanna J, Roy D (2014) Bayesian network and mechanistic hierarchical structure modeling of increased likelihood of developing intractable childhood epilepsy from the combined effect of mtDNA variants oxidative damage and copy number. J Mol Neurosci 54:752766
Luine V, Villegas M, Martinez C, McEwen BS (1994) Repeated stress causes reversible impairments of spatial rnemory performance. Brain Res 639:167–170
Madar A, Pfammatter J, Bordenave J, Plumley E, Ravi S, Cowie M, Wallace E, Hermann B, Maganti R, Jones M (2021) Deficit in Behavioural and Neuronal Pattern Seperation in TLE. J Neurosci 41(46):9669–9686
Maia GH, Quesado JL, Soares JI, do Carmo JM, Andrade PA, Andrade JP, Lukoyanov NV (2014) Loss of hippocampal neurons after kainate treatment correlates with behavioral deficits. PLoS ONE 9(1):e84722
Mante PK, Adongo DW, Woode E (2017) Anticonvulsant effects of Antiaris toxicaria aqueous extract: investigation using animal models of temporal lobe epilepsy. BMC Res Notes 10:167
Mattson RH, Cramer JA, Collins JF (1992) A comparison of valproate with carbamazepine for the treatment of complex partial seizures and secondarily generalized tonic-clonic seizures in adults. New Engl J Med 327(11):765–771
Mohd SNS, Sirajudeen KN, Asari MA, Muzaimi M, Mummedy S, Sulaiman SA(2015) Kainic acid-induced excitotoxicity experimental model: protective merits of natural products and plant extracts. Evid Complementary Altern Med 2015: 972623
Mohd SNS, Sirajudeen KN, Muzaimi M, Mummedy S, Asari MA, Sulaiman SA(2018) Tualang honey reduced neuroinflammation and caspase-3 activity in rat brain after kainic acid-induced status epilepticus. Evid Compl Alt Med 2018
Morris RG, Garrud P, Rawlins JN, O’Keefe J(1982) Place navigation impaired in rats with
hippocampal lesions.Nature297:681–683
Mosbah A, Tramoni E, Guedj E, Aubert S, Daquin G, Ceccaldi M, Felician O, Bartolomei F (2014) Clinical, neuropsychological, and metabolic characteristics of transient epileptic amnesia syndrome. Epilepsia 55(5):699–706
Mosiashvili Z, Kasradze S, Gagoshidze T (2017) Working memory deficit in patients with temporal and frontal lobe epilepsy. JSM Brain Sci 2(2):1015–1021
Moto FCO, Arsa’a A, Ngoupaye GT, Taiwe GS, Njapdounke JSK, Kandeda KA, Nkantchoua GCN, Omam JP, Pale S, Kouemou NE, Ayissi MER, Pahaye DB, Ojong L, Mairara V, Ngo Bum E (2018) Anxiolytic and Antiepileptic Properties of the Aqueous Extract of Cissus quadrangularis (Vitaceae) in Mice Pilocarpine Model of Epilepsy. Front Pharmacol 9:751
Muruganandan S, Srinivasan K, Chandra S, Tandan SK, Lal J, Raviprakash V (2001) Anti-inflammatory activity of Syzygium cumini bark. Fitoterapia 72(4):369–375
Ngo Bum E, Taiwe G, Moto F, Ngoupaye G, Nkantchoua G, Pelanken M, Rakotonirina S, Rakotonirina A (2009) Anticonvulsant, anxiolytic, and sedative properties of the roots of Nauclea latifolia Smith in mice. Epilepsy Behav 15(4):434–440
Ngo Bum E, Ngah E, Ngo R, Minkoulou D, Talla E, Moto F, Ngoupaye G, Taiwe G, Rakotonirina A (2012) Decoctions of Bridelia micrantha and Croton macrostachyus may have anticonvulsant and sedative effects. Epilepsy Behav 24:319–323
Nygaard HB, Kaufman AC, Sekine-Konno T, Huh LL, Going H, Feldman SJ, Kostylev MA, Strittmatter SM (2015) Brivaracetam, but not ethosuximide, reverses memory impairments in an Alzheimer’s disease mouse model. Alzheimer’s Res Ther 7(1):1–2
Ojo E, Ishola I, Ben-Azu B, Afolayan O, James A, Ajayi A, Umukoro S, Adeyemi O (2019) Ameliorative influence of Cnestis ferruginea vahl ex DC (Connaraceae) root extract on kainic acid-induced temporal lobe epilepsy in mice: role of oxidative stress and neuroinflammation. J Ethnopharmacol 243:1121117
Oprica M, Eriksson C, Schultzberg M(2003) Inflammatory mechanisms associated with brain damage induced by kainic acid with special reference to the interleukin-1 system. J Cell Mol Med 2003 7(2):127–140
Pack A (2019) Epilepsy Overview and Revised Classification of seizures and Epilepsies. Continuum 25(2):306–321
Pahaye DB, Ngo Bum E, Taïwé GS, Ngoupaye GT, Sidiki N, Moto FCO, Kouemou N, Njapdounké SJK, Nkantchoua G, Kandeda A, Omam JPO, Mairaira V, Ojong JL (2017) Neuroprotective and antiamnesic effets of Mitragyna intermis Willd (Rubiaceae) on scopolamine-induced memory impairment in Mice. Behav Neurol 2017:5952897
Pai RJ, Valder B, Palatty PL, Shivashankara AR, Baliga MS (2013) Bioactive food as dietary interventions for liver and gastrointestinal disease. 1st edition. Elsevier, USA, pp 369–380
Petrovska BB (2012) Historical review of medicinal plants’ usage. Pharmacogn Rev 6(11):1–5
Pizzino G, Irrera N, Cucinotta M, Pallio G, Mannino F, Arcoraci V, Squadrito F, Altavilla D, Bitto A(2017) Oxidative stress: harms and benefits for human health. Oxid Med Cell Longev 2017: 8416763
Pohle W, Becker A, Grecksch G, Juhre A, Willenberg A (1997) Piracetam prevents pentylenetetrazol kindling-induced neuronal loss and learning deficits. Seizure 6(6):467–474
Postnikova TY, Zubareva OE, Kovalenko AA, Kim KK, Magazanik LG, Zaitsev AV (2017) Status epilepticus impairs synaptic plasticity in rat hippocampus and is followed changes in expression of NMDA receptors. Biokhimiya 82:418–428
Prieur EA, Jadavji NM (2019) Assessing spatial working memory using the spontaneous alternation Y-maze test in aged male mice. Bio Protoc 9(3):3162
Puttachary S, Sharma S, Tse K, Beamer E, Sexton A, Crutison J, Thippeswamy T (2015) Immediate epileptogenesis after kainate-induced status epilepticus in C57BL/6J mice: evidence from long-term continuous video-EEG telemetry. PLoS ONE 10(7):0131705
Qashu F, Figueiredo TH, Aroniadou-Anderjaska V, Apland JP, Braga MF (2010) Diazepam administration after prolonged status epilepticus reduces neurodegeneration in the amygdala but not in the hippocampus during epileptogenesis. Amino Acids 38(1):189–197
Racine R(1972) Modification of seizure activity by electrical stimulation II Motor
seizure.Clin Neurophysiol32:281–294
Ramazi S, Fahanik-Babaei J, Mohamadi-Zarch S, Tashakori-Miyanroudi M, Nourabadi D, Nazari-Serenjeh M, Roghani M (2020) Neuroprotective and anticonvulsant effects of sinomenine in kainate rat model of temporal lobe epilepsy: Involvement of oxidative stress, inflammation, and pyroptosis. J Chem Neuroanat 108:101800
Rattka M, Brandt C, Löscher W (2013) The intrahippocampal kainate modal of temporal lobe epilepsy revisited: epileptogenesis behavioral and cognitive alterations, pharmacology response, and hippocampal damage in epileptic rats. Epilepsy Res 103:135–152
Rebas E, Rzajew J, Radzik T, Zylinska L (2020) Neuroprotective polyphenols: a modulatory action on Neurotransmitter pathways. Curr Neuropharmacol 18(5):431–445
Renaud J, Thérien HM, Plouffe M, Martinoli1 MG (2015) La neuroinflammation.Médecine31:979–988
Rodgers RJ, Dalvi A (1997) Anxiety, defence and the elevated plus-maze. Neurosci Biobehav Rev 21(6):801–810
Romoli M, Mazzocchetti P, D’Alonzo R, Siliquini S, Rinaldi VE, Verrotti A, Calabresi P, Costa C (2019) Valproic acid and epilepsy: from molecular mechanisms to clinical evidences. Curr Neuropharmacol 17(10):926–946
Rusina E, Bernard C, Williamson A(2021) The kainic acid models of temporal lobe epilepsy.Eneuro8(2)
Santos CA, Almeida FA, Quecán BXV, Pereira PAP, Kelly M, Gandra B, Cunha LR, Pinto UM (2020) Bioactive Properties of Syzygium cumini (L.) Skeels pulp and seed phenolic extracts. Front Microbiol 11:1–16
Simões-Pires CA, Vargas S, Marston A, Ioset JR, Paulo MQ, Matheeussen A, Maes L (2009) Ellagic acid derivatives from Syzygium cumini stem bark: investigation of their antiplasmodial activity. Nat Prod Commun 4(10):1371–1376
Singh G, Sander J (2020) The global burden of epilepsy report: implications for low- and middle-income countries. Epilepsy Behav 105:106949
Sharma S, Puttachary S, Thippeswamy A, Kanthasamy AG, Thippeswamy T (2018) Status epilepticus: behavioral and electroencephalography seizure correlates in kainate experimental models. Front Neurol 9:7
Shin EJ, Jeong JH, Chung YH, Kim WK, Ko KH, Bach JH, Hong JS, Yoneda Y, Kim HC (2011) Role of oxidative stress in epileptic seizures. Neurochem Int 59(2):122–137
Shors TJ, Weiss C, Thompson RF (1992) Stress-induced facilitation of classical conditioning. Science 257:537–539
Smith BN, Dudek FE (1997) Enhanced population responses in the basolateral amygdala of kainate-treated, epileptic rats in vitro. Neurosci Lett 222:1–4
Solomonia R, Mikautadze E, Nozadze M, Kuchiashvili N, Lepsveridze E, Kiguradze T (2010) Myo-inositol treatment prevents biochemical changes triggered by kainate-induced status epilepticus. Neurosci Lett 468(3):277–281
Sperk G, Schwarzer C, Heilman J, Furtinger S, Reimer RJ, Edwards RH, Nelson NJ (2003) Expression of plasma membrane GABA transporters but not of the vesicular GABA transporter in dentate granule cells after kainic acid seizures. Hippocampus 13(7):806–815
Srivastava S, Chandra D (2013) Pharmacological potentials of Syzygium cumini: a review. J Sci Food Agri 93(9):2084–2093
Stafstrom CE (2010) Pathophysiological mechanisms of seizures and epilepsy: a primer. Epilepsy: mechanisms, models, and translational perspectives. CRC Press, pp 3–19
Taiwe SG, Moto F, Ayissi E, Ngoupaye G, Njapdounke J, Nkantchoua G, Kouemou N, Omam J, Kandeda A, Pale S, Pahaye D, Ngo Bum E (2015) Effects of a lyophilized aqueous extract of Feretia apodanthera Del (Rubiaceae) on pentylenetetrazole-induced kindling, oxidative stress and cognitive impairment in mice. Epilepsy Behav 43:100–108
Tramoni-Negre E, Lambert I, Bartolomei F, Felician O (2017) Long-term memory deficits in temporal lobe epilepsy. Rev Neurol 173(7–8):490–497
Téllez-Zenteno, Jose F, Lizbeth, Hernández-Ronquillo(2012) “A review of the epidemiology of temporal lobe epilepsy. Epilepsy Res Treat 2012: 630853
Tuunanen J, Halonen T, Pitkanen A(1996) Status epilepticus causes selective regional
damage and loss of GABAergic neurons in the rat amygdaloid complex.Europ J Neurosci8:2711–2725
Ulla A, Alam MA, Sikder B, Sumi FA, Rahman MM, Habib ZF, Mohammed MK, Subhan N, Hossain H, Reza HM (2017) Supplementation of Syzygium cumini seed powder prevented obesity, glucose intolerance, hyperlipidemia and oxidative stress in high carbohydrate high fat diet induced obese rats. BMC Comp Alt Med 17(1):1–13
Vezzani A, Fujinami R, White H (2016) Infections, inflammation and epilepsy. Acta Neuropathol 131:211–234
Vincent P, Mulle C (2009) Kainate receptors in epilepsy and excitotoxicity. Neuroscience 158(1):309–323
Vinti V, Dell’Isola GB, Tascini G, Mencaroni E, Di Cara G, Striano P, Verrotti A (2021) Temporal lobe epilepsy and psychiatric comorbidity. Front Neurol 12:775781
Vorhees CV, Williams MT (2014) Assessing spatial learning and memory in rodents. ILAR J 55(2):310–332
Voss JL, Bridge DJ, Cohen NJ, Walker JA (2017) A closer look at the hippocampus and memory. Trends Cogn Sci 21(8):577–588
Wagner RG, Kabudula CW, Forsgren L, Ibinda F, Lindholm L, Kahn K, Tollman S, Newton CR (2020) Epilepsy care cascade, treatment gap and its determinants in rural South Africa. Seizure 80:175–180
Wang Q, Yu S, Simonyi A, Sun GY, Sun AY (2005) Kainic acid-mediated excitotoxicity as a model for neurodegeneration. Mol Neurobiol 31(1):3–16
Wang YF, Luo Y, Hou GL, He RJ, Zhang HY, Yi YL, Zhang Y, Cui ZQ (2021) Pretreatment with Methylene Blue Protects Against Acute Seizure and Oxidative stress in a kainic acid-induced status epilepticus model. Med Sci Mon 27:9334691–93346910
Wang X, Song X, Wu L, Nadler JV, Zhan RZ (2016) Persistent hyperactivity of hippocampal dentate interneurons after a silent period in the rat pilocarpine model of epilepsy. Front Cell Neurosci 10:94
Weaver MR, Cromwell EA (2019) Epilepsy in Africa: Can we end suffering and financial hardship due to lack of access to effective and affordable care ? EClin Med 9:9–10
Wenk GL (2001) Assessment of spatial memory using the T maze. Curr Protoc Neurosci 4(1):8–5A
Wenk GL (2004) Assessment of spatial memory using the radial arm maze and Morris water maze. Curr Protoc Neurosci 26(1):8–5A
Wilbur KM Bernheim F, Shapiro OW(1949) The thiobarbituric acid reagent as a test for the oxidation of unsaturated fatty acids by various agents.Arch Biochem24 (2):305–313
Winkler AS (2012) Measuring the epilepsy treatment gap in sub-Saharan Africa. Lancet Neurol 11(8):655–657
Yang Y, Mailman RB (2018) Strategic neuronal encoding in medial prefrontal cortex of spatial working memory in the T-maze. Behav Brain Res 343:50–60
Zhao F, Kang H, You L, Rastogi P, Venkatesh D, Chandra M (2014) Neuropsychological deficits in temporal lobe epilepsy: A comprehensive review. Ann Indian Acad Neurol 17(4):374
Zeng LH, Rensing NR, Wong M (2009) The mammalian target of rapamycin signaling pathway mediates epileptogenesis in a model of temporal lobe epilepsy. J Neurosci 29(21):6964–6972
Zeng LH, Zhang HD, Xu CJ, Bian YJ, Xu XJ, Xie QM, Zhang RH (2013) Neuroprotective effects of flavonoids extracted from licorice on kainate-induced seizure in mice through their antioxidant properties. J Zhejiang University Sci 14(11):1004–1012
Acknowledgements
The authors thank the Universities of Ngaoundéré (Cameroon) and Yaoundé I (Cameroon) for providing laboratory apparatus for this study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
AKK and SN designed the study, performed all behavioral studies, accomplished data analysis, and drafted the manuscript. AKK and SMT critically reviewed the manuscript for important intellectual content. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was conducted following the Cameroon National Ethical Committee guidelines (Ref No. FW-IRB00001954, 22 October 1987). All efforts were made to minimize the number of mice used and their suffering.
Competing Interests
The authors have no relevant financial or nonfinancial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kandeda, A.K., Nodeina, S. & Mabou, S.T. An aqueous extract of Syzygium cumini protects against kainate-induced status epilepticus and amnesia: evidence for antioxidant and anti-inflammatory intervention. Metab Brain Dis 37, 2581–2602 (2022). https://doi.org/10.1007/s11011-022-01052-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-022-01052-y