Abstract
Despite that mutations in mitochondrial DNA (mtDNA) have been associated with major epilepsy syndromes, the role of mtDNA instability and mitochondrial dysfunction in epileptogenesis has not been comprehensively examined. In the present study, we investigated the role of mtDNA copy number, oxidative damage, and mtDNA variants as independent or combined risk factors for the development of intractable childhood epilepsy. We analyzed mtDNA copy number and oxidative damage by quantitative polymerase chain reaction (PCR), and mtDNA variants by dot blot in brain tissue specimens collected from 21 pediatric intractable epilepsy patients and 11 non-epileptic patients. Bayesian network and mechanistic hierarchical structure Markov chain Monte Carlo (MCMC) modeling were used to analyze the relationship between these variables. The combined effects of oxidative mtDNA damages and mtDNA copy number produced more significant correlation with epilepsy than that of mtDNA copy number alone with epilepsy. Epilepsy patients showed significant correlations with mtDNA single nucleotide polymorphisms (SNPs) — A1555G, G3196A, T3197C, G9952A, A10006G, A10398G, cortical dysplasia status, oxidative mtDNA damage and relative mtDNA copy number. Comparison of 12 mechanistic structure models suggested that female children who have the wild type allele 10398A and variant allele 9952A, and high mtDNA copy number and oxidative stress have increased probability of developing intractable epilepsy. Estimation of nuclear genes controlling mitochondrial biogenesis, cortical dysplasia, and the effect of the environment using MCMC method showed that these latent variables had a very significant contribution in the development of intractable epilepsy. These data suggest that mitochondrial genetics play a significant role in the pathogenesis of epilepsy in children, and findings of this study may guide the prospects for targeting mitochondria for therapeutic treatment of childhood intractable epilepsy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intractable epilepsy is a complex chronic neurological disorder. Over 30 % of epileptic patients are medically intractable or drug resistant (Lopez et al. 2007). The timing and possible molecular mechanisms responsible for the development of drug resistant epilepsy are still largely unknown. In the majority of cases, etiology of intractable or drug resistant epilepsy is unknown. Both genetic (inborn errors of metabolism, mutations in the mitochondrial DNA (mtDNA) polymerase gamma gene (POLG) and environmental (acquired central nervous system infections, hypoxic–ischemic injury) causes have been suggested for intractable epilepsy (Luna et al. 2011; Uusimaa et al. 2013). One of the most common etiologies in younger epilepsy patients undergoing neurosurgery is cortical dysplasia (CD) (Andres et al. 2005; Jizong et al. 2011). For example, about 25 % to 40 % of intractable childhood epilepsy has been attributed to CD and about 75 % of patients with CDs have epilepsy. The occurrence of CD is often associated with developmental brain abnormalities that consist of dysplastic neuronal lesions (Schwartzkroin and Walsh 2000; Hua and Crino 2003; Hader et al. 2004; Rickert 2006; Wong 2007). The treatments for epilepsy due to CD are often ineffective or limited (Wong 2009).
Mitochondrial dysfunction and oxidative stress have gained considerable interest as a potential cause of epileptic seizures and therapy-resistant forms of severe epilepsy (Waldbaum and Patel 2010a, b). Approximately half (53 %) of patients with intractable or recurrent status epilepticus, myoclonic seizures, infantile spasms, and epilepsia partialis continua are associated with mitochondrial diseases caused by mutations in either mitochondrial or nuclear genes (Bindoff and Engelsen 2012; Canafoglia et al. 2001; El Sabbagh et al. 2010). The most commonly studied epilepsy syndromes with mitochondrial disorders are mitochondrial myopathy, encephalopathy, lactic acidosis and stroke-like episodes (MELAS), myoclonus, epilepsy, ragged-red fibres (MERRF) and neuropathy, ataxia, retinitis, and pigmentosa (NARP). Some patients with the symptoms of MELAS syndrome and myoclonic seizures have a mutation at position 3243 in the mtDNA (Liang and Wong 1998). Other patients with the same symptoms, including the same type of seizures, have mutations in mtDNA of respiratory chains III and IV. The mutation in MERF and NARP patients is found at position 8344 and 8992 position in the mtDNA, respectively (Santorelli et al. 1997; Szuhai et al. 2001). Recently, mutations in the catalytic subunit of POLG (a nuclear gene that replicates mtDNA) have been shown to be a potentially important cause of severe intractable epilepsy (Uusimaa et al. 2013). Based on these findings, the expression of mitochondrial disorders-related intractable epilepsy can be ascribed to a number of qualitative as well as quantitative changes in mitochondria DNA or nuclear genes regulating mitochondria.
Although mutations in mtDNA have been associated with epilepsy syndromes, the role of mtDNA instability and mitochondrial dysfunction in epileptogenesis is not clearly understood. There is sparse clinical or molecular epidemiologic data comprehensively examining the role of mitochondria DNA in the pathogenesis of intractable epilepsy. Mitochondrial dysfunction can results from defects in mtDNA or nuclear DNA that affect the mitochondrial biogenesis, functioning of respiratory electron transport chain (ETC.), ADP phosphorylation and signaling between mitochondria and the nucleus (Felty and Roy 2005; Roy et al. 2007). It has been shown that in the temporal lobe epilepsy, a time-dependent increase in the frequency of mtDNA lesions accompanied by an increase in mitochondrial H2O2 production and a decrease of mtDNA repair capability have been reported (Waldbaum and Patel 2010ab). These reports suggested an increased in vivo evidence of mitochondrial oxidative injury to mtDNA by showing that mitochondria contribute to free radical production, subsequent inactivation of susceptible iron–sulfur enzymes, and seizure-induced neuronal death.
The discovery of molecular susceptibility factors (genes) for intractable epilepsy has been complicated due to the etiologic, genetic and phenotypic heterogeneity of intractable epilepsy and clinical overlap between different epilepsy syndromes in pediatric patients. Despite that mutations in mtDNA have been associated with major epilepsy syndromes, the role of mtDNA instability and mitochondrial dysfunction in epileptogenesis has not been comprehensively examined. To understand the role of mtDNA and oxidative stress in epileptogenesis, we examined mtDNA copy number, oxidative mtDNA damage, mitochondrial haplotypes, and mtDNA single nucleotide polymorphisms (SNPs) in the brain tissue specimens collected from 21 pediatric intractable epilepsy patients and 11 non-epileptic patients.
Materials and Methods
Collection of Brain Tissue from Pediatric Intractable Epilepsy Patients
Brain tissue samples from 21 pediatric non-neoplastic intractable epilepsy patients who have undergone brain resection surgery at the Miami Children’s Hospital, Miami, FL, during 2008–2009 were collected. Tissues obtained during surgical resection were immediately snap-frozen in liquid nitrogen and stored at −80 °C. There were three epilepsy cases that were missing gender information. We conducted multivariate analysis to identify variables that predicts gender. We identified that SNP A12308G alone was the best predictor of gender and imputed that all three subjects are female.
As references, 11 normal, non-epileptic, pediatric brain tissues were obtained from the NICHD Brain and Tissue Bank for Developmental Disorders at the University of Maryland, Baltimore, MD and stored at −80 °C. This study was approved by the Institutional Review Boards of Miami Children’s Hospital and Florida International University.
DNA Extraction
Freshly excised human brain tissue was stored in liquid nitrogen and frozen in −80 °C until ready for processing. The frozen neuronal tissue was homogenized in which 1 ml of Trizol® was added. The homogenate was transferred to a 2.0-ml microcentrifuge tube. DNA was then isolated and purified via phenol–chloroform extraction. The precipitated DNA was pelleted and resuspended in 1× TE buffer. The integrity of the DNA was verified following electrophoresis through 2 % agarose gels.
Quantification of mtDNA Copy Number by Real-Time PCR
The relative mtDNA copy numbers were measured by quantitative real-time polymerase chain reaction (QPCR) and normalized by simultaneous quantification of nuclear gene — 18S rRNA. QPCR was performed in an ABI PRISM 7300 system (PE Biosystems, California, USA) using a SYBR green PCR master mix kit (Qiagen). A total of 50 ng of DNA was used in QPCR for the determination of the threshold cycle number (Ct) of the 18S rRNA and ND1 genes. The final volume of 25 μl reaction mixture contained 50 ng DNA template, 12.5 μl SYBR Green PCR Master Mix (Qiagen), and 10 mM of each primer. The sequences for the primers used for the amplification of the mitochondrial gene NADH Dehydrogenase 1 (ND1) were: mtF3212, 5′-CACCCAAGAACAGGGTTTGT-3′ and mtR3319, 5′-TGGCCATGGGATTGTTAA-3′. The sequences of the primer for the nuclear housekeeping gene 18S rRNA, used for the normalization in the QPCR analysis, were: 18S1546F, 5′-TAGAGGGACAAGTGGCGTTC-3′ and 18S650R, 5′-CGCTGAGCCAGTCAGTGT-3′ (Lin et al. 2008). The QPCR conditions were set up as follows: hot start at 95 °C for 10 min, followed by 40 cycles of 95 °C for 15 s and 60 °C for 1 min. The fluorescence intensity was measured at the end of the extension phase at 60 °C. All samples were performed in duplicate and a non-template negative control was included in each reaction. Ct values were used as a measure of input copy number and the Ct value differences were used to quantify the mtDNA copy number relative to the 18S rRNA gene with the following equation: Relative copy number = 2∆Ct, where ∆Ct is the Ct 18S rRNA – Ct ND1 (Szuhai et al. 2001; Bai et al. 2007, 2008; Lee et al. 2010). We performed Grubbs' test (extreme studentized deviate) to determine values that were 3-fold higher than the upper limit of 95 % confidence interval (CI), respectively, and these values were considered as significant outliers from the rest of the values.
Quantification of Oxidative Damage to mtDNA by QPCR
Since the degree of oxidative mtDNA damage is reflected by an abundance of 8-hydroxydeoxyguanosine (8-OHdG) formation in mtDNA, the content of 8-OHdG in mtDNA, an index for cellular oxidative damage, was determined by QPCR and presented as ∆Ct (Ayala-Torres et al. 2000). As indicated by Lin et al. (2008), the amplification efficiency would decrease after treatment of the DNA sample with hOGG1 to remove the 8-OHdG residue to form an abasic site. The content of 8-OHdG in the samples’ mtDNA was determined by treating the 200-ng sample with 2 units of hOGG1 (New England Biolabs, M024S) at 37 °C for 1 h and 5 min to remove the 8-OHdG residue to form a basic site. The digested mtDNA were amplified by QPCR using the primers for ND 1 gene. PCR amplification efficiencies of DNA templates containing a single 8-OHdG or two 8-OHdGs at least 13 base pairs apart are not significantly disturbed (Ct1), however, the presence of an abasic site in DNA after treatment of hOGG1 would dramatically reduce the PCR efficiency, thus, increasing the Ct value (Ct2) (Lin et al. 2008). The degree of oxidative mtDNA damage, mtDNA∆Ct, was defined as ∆Ct = Ct2 (hOGG1 treatment) − Ct1 (no hOGG1 treatment) (Lin et al. 2008; Su et al. 2010). Each analysis was performed in duplicate, and the mean value of ∆Ct was calculated for each sample. Hence, the larger the ∆Ct, the more abundant the 8-OHdG and more oxidative damage present in the sample.
mtDNA Genotyping
A total of 50 ng of DNA was used in QPCR to amplify the mitochondrial genome with 19 primer sets designed by Bai et al. (2007) to include the mtDNA regions containing ten reported mtDNA variations (SNPs). The mtDNA variations are distributed along the rRNA, tRNA, COIII, and ND3 regions of the mitochondrial genome.
QPCR assays to amplify 19 regions of the mitochondrial genome were performed using Applied Biosystems 7300 System with a final volume of 25 μl reaction mixture containing 50 ng DNA template, 12.5 μl SYBR Green PCR Master Mix (Qiagen), and 10 mM of each primer. The QPCR conditions were set up as follows: hot start at 95 °C for 10 min, followed by 40 cycles of 95 °C for 15 s and 60 °C for 1 min. Two microliters of QPCR products were spotted on Hybond N + membrane (GE). The allele-specific oligonucleotide (ASO) probes for the mtDNA variants described by Bai et al. (2007) were labeled with Dioxigenin (DIG) (Roche, DIG Oligonucleotide 3′-End Labeling Kit). Both the variant and wild type controls for each ASO blot were included as controls.
Determination of mtDNA Haplogroup
Haplogroups — L, J, L0, L1, L2, L3, M, T, U, and X — were investigated in DNA from both epilepsy and control brain samples based on the classification of SNPs described by Bai et al. (2007) and the Mitomap database.
Analysis of Association Between Intractable Epilepsy and Mitochondrial Haplogroup, mtDNA Copy Number, Oxidative Damage and mtSNPS
Data were logarithmically transformed, because the original values of the relative mtDNA copy number and the content of 8-OHdG in mtDNA did not show normal distribution. The continuous variables between groups were compared using the Student’s t-test and Fisher’s exact test for comparisons of the frequency of dichotomous features. Pearson’s correlation test was used to test the relationship between mtDNA copy number and the content of 8-OHdG in mtDNA. Analysis was carried out using Fisher’s exact test for each individual mtSNP and haplogroup.
Logistic regression was used to determine the adjusted odds ratio. Epilepsy patients were sub-divided as those being malformations of cortical development (cortical dysplasia, CD) and non-CD as per Barkovich CD classification system (Barkovich et al. 2005). Logistic regression was also used to explore if epilepsy, CD, or non-CD phenotypes were dependent on mtSNPs, haplogroups, level of mtDNA oxidative damage, and level of relative mtDNA copy number, model adjusted by age. Statistical analyses were performed using SPSS version 18.0 for Microsoft Windows.
Analysis of the Interaction of mtDNA Copy Number, Oxidative mtDNA Damage, and the mtSNPs with Epilepsy Status
We applied Bayesian Networks learning method to understand interactions between mtDNA variants, mtDNA copy number and mtDNA damages in female subjects with or without epilepsy (14 epilepsy and 11 control subjects). Interactions between mtDNA SNPs, mtDNA copy number and mtDNA damages were analyzed by ten independent 2-h Banjo analyses on an Intel T9900 3.0GHz machine (Yoo et al. 2002; Kunkle et al. 2013). Each simulation with random starts consisted of a total of 1 × 109 networks. Banjo scores each network using log of the BDe matric to assess the ability of Markov mtDNA SNPS to distinguish between normal and epilepsy samples in our analysis, Genie, a software tool for analyzing Bayesian networks developed by the University of Pittsburgh (Druzdze1999) was used to predict the probability of developing intractable epilepsy given certain expression states for its mtDNA SNPs network. This predicts key Markov causal mtDNA SNPs involved in the development of intractable epilepsy. In Bayesian network analysis this is done by learning the parameters of a given DAG structure.
Estimation of Latent Variable Effects and Model Comparison
We developed 12 plausible mechanistic hierarchical structure models of intractable epilepsy based on prior knowledge and using observed variables — epilepsy, CD, mitochondrial oxidative damage, G9952A, A10398G, and mtDNA copy number and unobserved (latent) variables — nuclear DNA encoded subunits controlling mitochondrial biogenesis, Oxidative Stress1, Oxidative Stress2, Defective mtDNA Encoded Subunits, Respiratory Chain Dysfunction1, Respiratory Chain Dysfunction2, and Environment Factors (Fig. 1). We used the Markov chain Monte Carlo (MCMC) method to learn the best parameters for the latent variables using Gibbs Sampling (Geman and Geman 1984). Initially, the missing cases were filled with random states sampled equally from a uniform distribution over two states (0, 1). This resulted in a complete dataset. We iterated the following steps until a specified time runs out or a stopping condition (there is no change in the distribution) is met:
-
Step 1: Using the complete dataset, we updated the probability distribution of a model.
-
Step 2: For each missing value, condition on its parents’ values, we calculated the probability distribution of the missing value, i.e., Pr(X i |Parents of X i ), where X i represents a latent variable in the model. According to the distribution, randomly we selected a state for the missing value.
-
Step 3: Repeat Step 2, until we filled out all the missing values.
-
Step 4: Go to Step 1.
After we had obtained a complete dataset from Gibbs Sampling, we calculated the likelihood, P(D|S,K), where D is the complete dataset from Gibbs Sampling, S is a given model, and K is the prior knowledge, using the BDe metrics mentioned above. For example, we calculated the likelihood for the model of Fig. 1 in the following way:
where E, CD, ANG,OS2, OS1, NDS, DES, RCD2, RCD1, MOD, G, A, CN, EF represent Epilepsy, Cortical Dysplasia, Altered Neurogenesis Genes, Oxidative Stress2, Oxidative Stress1, Nuclear DNA encoded Subunits, Defective mtDNA Encoded Subunits, Respiratory Chain Dysfunction2, Respiratory Chain Dysfunction1, Mitochondrial Oxidative Damage, G9952A, A10398G, Copy Number, and Environment Factors, respectively, and subscript i represents the ith subject in the dataset. We calculated the posterior probabilities of relationships such as X → Y for any variables X and Y from the 12 structures using the following formula:
where T is a set of all 12 structures.
Results
Demographics and Clinical Information
The demographic and pathology information of the pediatric non-neoplastic intractable epilepsy patients are shown in Table 1 and for the 11 control samples in Table 2. There were 21 pediatric non-neoplastic intractable epilepsy patients (14 female and seven males), and 14 of them had CD. The age (mean ± SE) for female epilepsy patients was 8.9 ± 1.56 years (n = 14) and for female non-epileptic control subjects was 9.73 ± 1.74 years (n = 11). CD was present in approximately 57 % (eight out of 14) of all female patients that underwent epilepsy neurosurgery. The majority of patients with CD (92 %) were classified as malformations due to abnormal glial and neuronal proliferation. We investigated mitochondrial dysfunction in brain tissues from disease and control samples by measuring changes in the markers of mtDNA injury — mtDNA copy number, oxidative damage to mtDNA, and mtDNA mutation.
Increased mtDNA Copy Number in the Brain Tissues of Children with Epilepsy
We used QPCR to analyze the relative mtDNA copy number of the pediatric intractable epilepsy brain tissues (non-neoplastic) and non-epileptic control brain tissues after normalization of mitochondrial ND1 gene to a nuclear gene 18S rRNA. Table 3 shows the distribution of mtDNA copy number per cell in the intractable epilepsy patients versus non-epileptic control subjects. Tests of association between mtDNA copy number and gender in the intractable epileptic female patients were not statistically significant. There was no association between mtDNA copy number and age (data not shown). The overall mean mtDNA copy number per cell in brain tissues of intractable epileptic patients was 189.7 (56.06–323.6). The corresponding value in healthy control subjects was 23.9 (17–30), significantly different from patients with intractable epilepsy (p < 0.001). The ratio of ND1/18S rRNA in the intractable epileptic patients was 8-fold higher (p < 0.01) than its ratio in the control group (23.9 ± 3.4). The ratio of ND1/18S rRNA in 11 out of 14 intractable epilepsy samples exceeded the upper limit of 95 % CI of the controls, indicating that 78.6 % of intractable epilepsy patients had over-amplification of mtDNA. Similarly, the ratio of ND1/18S rRNA in the intractable epileptic patients with CD (112.99 ± 34.69) was 4.7-fold higher (p < 0.01) than its ratio in the control group (23.9 ± 3.4). The ratio of ND1/18S rRNA in six out of eight intractable epilepsy patients with CD exceeded the upper limit of 95 % CI of the controls, indicating that 75 % of intractable epilepsy with CD patients had over-amplification of mtDNA. In summary, our present findings revealed a significantly higher mtDNA copy number in intractable epilepsy patients, particularly in patients with severe CD as compared with the control group.
Higher Oxidative mtDNA Damages in the Brain Tissues of a Subset of Intractable Epilepsy Children Patients
The 8-OHdG content in mtDNA was measured as a marker of oxidative damage to mtDNA and oxidative stress by QPCR. The degree of oxidative mtDNA damage, mtDNA∆Ct, was determined as ∆Ct = Ct2 (hOGG1 treatment) – Ct1 (no hOGG1 treatment); thus, the larger the ∆Ct, the more abundant the 8-OHdG and more oxidative damage were considered to be present in the samples. Table 3 shows the distribution of mtDNA damage in the intractable epilepsy patients and non-epileptic control subjects. The overall mean of mtDNA damage in brain tissues of non-epileptic control subjects was 4.52 ± 0.64 (95 % CI 3.46–5.571), lower from patients with intractable epilepsy. The corresponding value in intractable epileptic patients was 6.26 ± 1.56 (95 % CI 3.69–8.82), which is 38 % higher than that of the control group. However, this difference was not significant (p < 0.32). The value of mtDNA damage in six out of 14 intractable epilepsy samples exceeded the upper limit of 95 % CI of the controls (10.26 ± 1.82; p < 0.01), indicating that 43 % of intractable epilepsy patients had higher oxidative damage to mtDNA from the brain of epileptic patients. Using the mean mtDNA damage of the control subjects (4.52) patients as the cut off value, we found high oxidative mtDNA damage (9.61 ± 1.59) in 58 % of intractable epileptic patients (p < 0.015) (Table 3). Pearson’s correlation also demonstrated that the high oxidative mtDNA damage were significantly associated with intractable epileptic (Pearson correlations = −0.449, p = 0.047) (Table 4). The mtDNA copy number and high oxidative mtDNA damage were also significantly associated with intractable epileptic patients (Pearson correlations = −0.503, p = 0.041). The oxidative mtDNA damage value in intractable epileptic patients with CD was 7.38 ± 1.63 (p < 0.13), which is 63 % higher than that of control group (Table 3). In summary, our findings revealed a higher mtDNA copy number and oxidative mtDNA damage in a subset of intractable epilepsy patients compared with control groups.
Association Between Intractable Epilepsy and Mitochondrial Haplogroup
The European (I and J), African (L and M), and Asian (M) haplogroups were found in both intractable epilepsy patients and control subjects. Control subjects had higher frequencies of the haplogroup I, J, L, M, and U5 compared to epilepsy patients. The European haplogroup (U5) was only found in mtDNA of non-epileptic control subjects, but not in the epilepsy patients. There was no association between any of the haplogroups and risk of developing epilepsy when comparing with the controls, except haplogroup M. The 10398G genotype represents European haplogroup I, J, K and Asian-specific super haplogroup M (Fig. 2). This G allele is more frequent than the 10398A genotype in Asians and the frequency of G allele is smaller in Europeans. The frequencies of the 10398A (wild type) and 10398G (variant) genotypes were 92.86 % and 7.14 % (1/14) in intractable epilepsy and 0 % and 100 % in controls, respectively (Table 5). There was a positive correlation between the non-M haplogroup (10398A) and risk of conditional probability of intractable epilepsy (r = 0.917, p = 0.0001) (Table 4).
Association Between mtDNA Content and Haplogroup
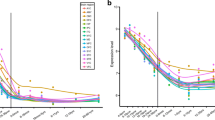
There was a positive correlation between the haplogroup J (13708A — variant) and mtDNA copy number (r = 0.433, p = 0.019) in female epileptic patients (Table 4). The G to A variation at 13708 position increased conditional probability of high mitochondrial copy number from 7 % to 68 % in female epileptic patients (Fig. 2).
Gender Differences in Susceptibility
We found a variation A to G at 10044 position in mtDNA in both male and female intractable epilepsy patients. The frequencies of the 10044A (wild type) and 10044G (variant) genotypes were 64.3 % and 35.7 % (5/14) in female and 55.6 % and 44.4 in male intractable epilepsy patients. This variation has been reported as pathogenic, in patients with sensorineural hearing impairment (SNHI) in the Finnish population (Lehtonen et al. 2003). This A to G variation at 10044 position alone increased conditional probability of developing epilepsy (53 % became 60 %) in female patients, but not in male patients (Fig. 3). This along with high mtDNA copy number increased conditional probability of developing epilepsy to 65 %. The combination of high mtDNA copy number, a variant 10044G and a wild type T9997 (wild type) further increased conditional probability of developing epilepsy to 79 %.
Identification of Intractable Epileptogenic-Related mtDNA Variants
For further identification of the specific mtDNA variants that may be implicated in the epileptogenic effects of mitochondrial haplogroup, we amplified mtDNA regions containing ten reported mtDNA variations (SNPs). The mtDNA variations are distributed along the rRNA, tRNA, COIII and ND3 regions of the mitochondrial genome. We selected these mtDNA variations for the present study because they have been reported in patients with varying diseases such as: Alzheimer’s disease, Parkinson’s disease, Leber’s hereditary optic neuropathy (LHON), deafness, chronic progressive external ophthalmoplegia (CPEO), chronic intestinal pseudo-obstruction (CIPO) and other diseases (Bai et al. 2007, 2008; Baron et al. 2007; Cardaioli et al. 1999; DiMauro 2001; Chinnery and Hudson 2013; Filiano et al. 2002; Hanna et al. 1998; Howell et al. 2003). In the 16S rRNA gene (MT-RNR2), two variations were found at 3196GA and 3197TC positions. These mutations are thought to be associated with Rett syndrome, MELAS, and Alzheimer and Parkinson disease, respectively (Grazina et al. 2006; Hsieh et al. 2001; Shoffner et al. 1993; MITOMAP 2009). The frequencies of the 3196G (wild type) and 3196A (variant) genotypes were 85.71 % and 14.29 % (2/14) in epilepsy patients and 0 % and 100 % in controls, respectively (Table 5). The frequencies of the 3197T (wild type) and 3197C (variant) genotypes were 100 % and 0 % in epilepsy patients and 18.18 % and 81.81 % in controls, respectively. The frequencies of the G9952 (wild type) and 9952A (variant) genotypes were 71.43 % (10/14) and 28.57 % (4/14) in epilepsy patients and 100 % and 0 % in controls, respectively (Table 5). The G9552A variant was not detected in non-disease controls. The presence of the variant in disease sample, but not in non-disease controls supports previous observation that it is not inherited maternally and this is perhaps a point mutation. This point mutation is located in the gene for subunit III of COX and is predicted to result in the loss of the last 13 amino acids of the highly conserved C-terminal region of this subunit (Hanna et al. 1998). The frequencies of the 10006A (wild type) and 10006G (variant) genotypes were 85.71 % and 14.29 % (2/14) in disease and 0 % and 100 % in controls, respectively (Table 5).
To assess the relation between mtSNPs, mtDNA copy number, mtDNA damage, CD and epilepsy measurements, the pairwise correlation coefficient was calculated. The correlations were very high between individuals (r > 0.92). We used parametric analysis to find the degree of interaction between epileptic status and variables. The following variables showed significant correlations (p < 0.05) with epilepsy: A1555G, G3196A, T3197C, G9952A, A10006G, A10398G, MCD status, mitochondrial copy number, and oxidative mtDNA damage and mtDNA copy number. To find a causal association, we used Bayesian Network modelling to determine the interaction of mtDNA copy number, oxidative mtDNA damage, and the mtSNPs with epilepsy status. Reverse engineering of 37 mtDNA SNPs, and other variables, such as, age, gender, oxidative stress (mtDNA damage) and mtDNA copy number using Bayesian Network analysis produced a network for intractable epilepsy, and ‘key mtDNA SNPs’ were identified. This was accomplished by identifying a set of Markov Blanket mtDNA SNPs. This allowed us to define a set of neighboring mtDNA SNPS that are sufficient to predict the probability of developing intractable epilepsy. Six different mtDNA SNPs A1555G, G3196A, T3197C, G9952A, A10006G, and A10398G found to be most influential in affecting the probability of developing intractable epilepsy (Fig. 2). The influence score, which represents the degree of interaction, showed a stronger interaction of mtDNA SNPs G3196A, T3197C A10398G with epilepsy (Table 5). We examined individual Markov blanket variable effect as well as joint effects of interaction between Markov Blanket variables on the conditional probability of developing intractable epilepsy. We found that mtDNA copy number and oxidative mtDNA damage were significantly associated with increased probability of developing intractable epilepsy. An increase in the mtDNA copy number resulted in a 13 % higher conditional probability of developing epilepsy (48 % became 61 %). The mtDNA copy number and oxidative mtDNA damage combined together resulted in 23 % higher conditional probability of developing epilepsy (48 % became 71 %). mtDNA copy number and oxidative mtDNA damage together with a variant G9952 resulted in 33 % higher conditional probability of developing epilepsy (48 % became 81 %). Joint effects of a wild 10398A allele, a variant 9952A, high mtDNA copy number and high oxidative damage to mtDNA increased the probability of developing intractable epilepsy from 48 % to 91 %.
Estimates of Latent Nuclear Genes, Defective Mitochondrial Functions and Environmental Effects on Intractable Epilepsy Outcomes
The nuclear genes, defective mitochondrial functions, genetic and environmental variables contribute to the differences in intractable epilepsy outcomes is defined by the mechanistic hierarchical structure MCMC model. The model follows a hierarchical form since multiple parameter measures with advancing time within the same patient and the estimation of external and internal environment exposure contributions are constrained to follow expectations by inheritance of maternal mtSNPs. The relationship between the variables in the dataset where the nature of the relationship was specified in terms of the biochemical and molecular processes that were thought to have given rise to the intractable epilepsy. Given the network structures based on observed and unobserved variable, we estimated the conditional probability distribution of each variable from both, the latent and real life dataset to deduce a best model by MCMC sampling in hierarchical Bayesian calibration of intractable epilepsy models. This is achieved by using Gibbs Sampling with MCMC method, whereby the search space is iteratively reduced resulting in the required convergence within a reasonable computation time. A total of 12 given the network structures were evaluated by Gibbs Sampling (Fig. 1). Significance was evaluated for the main effects of interaction of latent and measured variables on the probability of producing intractable epilepsy (the null model [H0], removed an arc from CD to epilepsy: the mtDNA variants, copy number, mtDNA damage and their interaction had no effect on the conditional probability of developing intractable epilepsy, vs. H1): one or more of the mtDNA variants, copy number, mtDNA damage and/or their interaction had an effect on the conditional probability of developing intractable epilepsy) using the Gibbs sampling and calculating the maximum log-likelihood. Based on the log-likelihood, we reject the null hypothesis with p = 0.000135 and the model 4 shown in Fig. 1 was 8.2 × 105 times better than that of model 5 (null, H0) (Table 6). This model suggested that female children who have the wild type allele 10398A and variant allele 9952A, and high mtDNA copy number and oxidative stress (mtDNA damage) have drastically increased probability of developing intractable epilepsy compared to those who had no effect on the conditional probability of developing intractable from the mtDNA variants, copy number, mtDNA damage and their interaction. To further validate our findings of our model, we conducted individual analysis of following paired variants (represented as X and Y) — Environment → mtDNA Copy Number, Environment → mtDNA Damage, Environment → Epilepsy, mtDNA Damage → Epilepsy, and CD → Epilepsy using P(X → Y| D, K) from the 12 structures, which also showed that environment, mtDNA copy number, mtDNA damage had a very significant contribution in the development of intractable epilepsy (Table 7).
Discussion
Our study produced several major novel findings, including identification of a key set of mtDNA SNPs highly associated with intractable epilepsy, identification of several key signature mitochondrial injury markers important to the development of intractable epilepsy, and identification of a possible mechanism which may explain the pathway identified as important to development of intractable epilepsy. Qualitative changes in mitochondrial genome with specific mutations or deletions in mtDNA have been frequently reported in patients with mitochondrial diseases (Bindoff and Engelsen 2012; Canafoglia et al. 2001; El Sabbagh et al. 2010). Many studies have investigated acute consequences of status epilepticus on cellular constituents but less is known about the role of oxidative stress and mitochondrial dysfunction in intractable epilepsy. To our knowledge, this is the first study to explore comprehensively the effects of mtDNA copy number, oxidative stress, mtDNA damage, and mtDNA variants in pediatric intractable epilepsy patients. In the present study, we examined individual mtDNA SNP or individual mitochondrial injury marker — the copy number of mtDNA per cell, oxidative mtDNA damage and the presence of the mtDNA mutation effect as well as the joint effects of interaction between these variables on the conditional probability of developing intractable epilepsy. Our present findings revealed that high mitochondrial copy number, the presence of the 9952A mutation or high mtDNA damage was strongly predictive of increased risk of developing intractable epilepsy. Joint effects of a wild 10398A allele, a variant 9952A, high mtDNA copy number and high oxidative damage to mtDNA dramatically increased the conditional probability of developing intractable epilepsy (43 % became 91 %). Findings of our study have major implications in understanding the development of intractable pediatric epilepsy. This study not only identified key important molecular determinants, it also proposes a new paradigm critical to the development of intractable epilepsy that merits future validation of these our findings in a cohort population of epilepsy patients with a bigger sample size to understand the exact role of mtDNA defects in intractable epilepsy may also lay the ground for the development of new therapies.
The molecular mechanisms responsible for the development of intractable epilepsy or drug resistant epilepsy are not fully understood. A considerable interest in mitochondrial dysfunction and oxidative stress has been evolving as potential causes of epileptogenesis and therapy-resistant forms of severe epilepsy (Shah et al. 2002; Waldbaum and Patel 2010a, b). The key role of mitochondria in neurodegenerative diseases is evident from the recent discoveries of mitochondrial alterations, such as, Autism, Alzheimer's disease, Parkinson's disease (Baron et al. 2007; Chen et al. 2007; Filiano et al. 2002). In the last decade, the research related to mitochondrial dysfunction in neurological diseases has been steadily growing. In this study, we examined the role of mitochondrial dysfunction in brain tissues from intractable epileptic children and control samples by measuring changes in the markers of mtDNA injury — mtDNA copy number, oxidative damage to mtDNA, and mtDNA mutation. Hypoglycemia and lactic acidosis are often observed with intractable seizures (Luna et al. 2011). Whether mitochondrial dysfunction or pediatric intractable epilepsy is the cause or consequence is still debatable. A key event in brain development is proliferation which begins around the 20th week of gestation (Lenroot and Giedd 2006). Mitochondria are intimately involved in pathways leading to the abnormal growth and death of neurons — one of the characteristic of epileptic lesions (Luna et al. 2011). We have discussed here the importance of each mtDNA injury marker in intractable epileptogenesis. A child's brain is highly susceptible to oxidative stress. The major reason for a child’s brain vulnerable to oxidative stress-induced damage is due to a large number of mitochondria per cell, high content of easily oxidizable substrates such as unsaturated lipids, high oxygen consumption and inherently high flux of ROS generated during neurochemical reactions, such as, dopamine oxidation and energy metabolism, and less antioxidant capacity than other tissues. In neurons, mitochondria are highly dynamic organelles that constantly move, divide, and fuse. Mitochondria are one of the major sources of reactive oxygen and nitrogen species in the brain (Luna et al. 2011). mtDNA is more susceptible to oxidative damage by ROS due to its lack of histones and limited capacity to repair DNA damage, thus, consequently acquires mutations at greater rates than nuclear DNA (Thomas and Roy 2001). We report for the first time that the content of 8-OHdG in mtDNA (a marker of oxidative damage to mtDNA and oxidative stress) was significantly higher in the brain tissue of a subset of intractable epilepsy patients compared with control groups. There have been several other reports showing that oxidative stress may be an important mechanism of CNS damage. Oxidative stress plays an important role in brain damage in children and this damage correlates with disease state (Fukuda et al. 2008; Waldbaum and Patel 2010a, b; Patil et al. 2011). Temporal lobe epilepsy studies have suggested that preceding neuronal death, after status epilepticus, is the increased level of ROS observed in brain slices and slice cultures of several models of experimental epilepsy, such as kainite-induced hippocampal damage or pilocarpine damage (Baron et al. 2007). Based on these findings it appears that an increase in oxidative stress may be associated with higher oxidative damage to mtDNA leading to increased probability of developing intractable epilepsy.
Mitochondrial function is compromised as a result of oxidative stress. Oxidative stress causes excess ROS production resulting in further oxidative damage, because the increase of ROS production from a defective respiratory chain plays a role in the increase of mitochondrial content. The increase of mtDNA copy number is also dependent on the level of oxidative stress, the capacity of intracellular antioxidant system, the quality of mitochondria and mtDNA. Another consequence of the oxidative stress is to produce damage to mtDNA. The increase in mtDNA replication, as a response to oxidative damage, provides a propagation of mtDNA that has not been damaged by oxidative stress. The resulting mtDNA copies do not contain the damage (DNA adducts), presenting an overall lower oxidative mtDNA damage. Thus, the increase in undamaged mtDNA dilutes the presence of damage mtDNA. Oxidative damage induces an increase in mitochondria and mtDNA to compensate for the decline in the function of mitochondrial respiration (Shen et al. 2010). In parallel, ROS act as a second messenger to trigger the expression of nuclear respiratory factors and mitochondrial transcription factor to induce mitochondrial biogenesis and mitochondrial proliferation (Felty and Roy 2005). Oxidative stress stimulates mitochondrial proliferation to meet the energy needs for cell survival including repair of damage and synthesis of new proteins. ROS resulting from persistent oxidative stress also interact with signaling molecules to regulate cell cycle gene expression (Okoh et al. 2011), which may contribute to abnormal proliferative growth of neurons and non-neuronal cells leading to CD.
There are limited studies that have addressed the change in mtDNA copy number as a marker of mitochondrial injury and intractable epilepsy. We report for the first time that pediatric intractable epilepsy patients have significantly higher mtDNA copy number than controls. It is unclear how copy number of mtDNA and the abundance of mitochondria are regulated under different physiological and developmental conditions. The increased mitochondrial copy number observed in this study may be an influence of phenotypic expression or a compensatory response to mitochondrial injury. In humans, 100–10,000 separate copies of mtDNA are usually present per cell. mtDNA copy numbers can be modulated when physiological conditions are changed. Increase in mtDNA copy number has been found in other neurological diseases. For example, the mtDNA copy number in leukocytes from patients aged 30 years and younger with MELAS and MERFF showed an increase in mtDNA copy number, and a depletion of mtDNA was found in patients 40 years and older (Liu et al. 2006). Brinckmann et al. (2010) found increased mtDNA copy number in the brain tissue of a 16-year-old girl with MERRF. Chen et al. (2007) found increased total mtDNA copy number in peripheral leukocytes in Huntington’s disease patients. Lee and Wei (2005) reported that an increase in mtDNA copy number is associated with elevated levels of oxidative stress in the aging tissues, brain, lung, and skeletal muscle of aged individuals. Alterations in intracellular level of ROS are associated with changes in mitochondrial abundance, mtDNA copy number, and the expression of respiratory genes. Persistent oxidative stress in mitochondria not only contributes to the somatic mtDNA mutations but also alter mtDNA replication rate, leading to an overall decline in the mitochondrial respiratory function. mtDNA copy number may be modulated according to the energy needs of the cell. Changes in mtDNA copy number in response to exercise and hormone treatment have been observed (Lee and Wei 2005; Roy et al. 2007). Treatment of human cells with H2O2 and buthionine suphoximine, which deplete intracellular glutathione, an anti-oxidant, induces an increase in mtDNA copy number and mitochondrial mass (Lee et al. 2000). Gamma-irradiated mice show an increase in relative mtDNA copy number in brain and spleen tissues, suggesting that the major mechanisms for maintenance of the mitochondrial genome is the induction of synthesis of new mtDNA copies because the repair systems in the mitochondria function at a low level efficiency (Malakhova, et al. 2005). Based on these findings it appears that mtDNA copy number and oxidative mtDNA damage contributes to the increased probability of developing intractable epilepsy. The increase in relative mtDNA copy number observed in intractable pediatric epilepsy patients may be as a result of compensatory responses for defective mitochondria bearing impaired respiratory chain or mutated mtDNA. Understanding the molecular mechanism of alterations in mtDNA copy number is important for the development of novel drugs to prevent and treat intractable epilepsy.
The role of mtDNA variants in mitochondrial injury and the pathogenesis of intractable epilepsy is not well understood. Many mitochondrial disorders caused by mutations, acquired or inherited, in mtDNA or in nuclear genes that code for mitochondrial components have seizure as part of their phenotype (Luna et al. 2011; Hsieh et al. 2001; Pieczenik and Neustadt 2007; MITOMAP 2009). mtDNA mutations have been implicated with epilepsy syndromes (Hsieh et al. 2001). The results of the present study suggest that mitochondria may play a critical role in the development of epilepsy, mitochondrial dysfunction observed in epilepsy could be attributed to the increase in mtDNA damages and copy number, as well as to the and variations in the mitochondrial genes involved in encoding the proteins of ETC. We found a mutation 9952 G>A in 28.57 % (4/14) in intractable epilepsy patients, which has been reported as pathogenic in a patient with encephalopathy and exercise intolerance (Hanna et al. 1998). This point mutation is located in 3′ end of the gene for the subunit of COIII and is thought to result in the loss of the last 13 amino acids of the C-terminal region of this subunit. The mtDNA variant 9952A, which code for COIII, was found in higher frequencies in the intractable epilepsy patients. The G9552A variant was not detected in non-disease controls. It is believed that the majority of the ROS are generated by complexes III, likely due to the release of electrons by NADH and FADH into the ETC. However, these results highlight the difficulty in determining the pathogenicity of a mtDNA mutation because it is identified only in a small sample size of patients. Therefore, we suggest that a bigger sample size should be screened before the pathogenic nature of an mtDNA mutation can be verified in intractable childhood epilepsy. Epilepsy patients showed significant correlations with mtDNA SNPs — A1555G, G3196A, T3197C, G9952A, A10006G, A10398G, CD status, oxidative mtDNA damage and relative mtDNA copy number. Comparison of 12 mechanistic structure models suggested that female children who have the wild type allele 10398A, which codes for ND3, and variant allele 9952A, and high mtDNA copy number and oxidative stress have increased probability of developing intractable epilepsy. Our results suggest that both COX III and ND3 are important factors in the development of intractable drug resistant epilepsy and could help explain the role of complex I and III in drug resistant epilepsy expression. The explanation for the pathological mechanism of the 10398 polymorphism is that the 10398A allele may cause a greater ROS production than 10398G. Complex I and III normally produces ROS during cellular activity; however, when these complexes are compromised or inhibited, generation of ROS is enhanced, leading to oxidative stress (Felty and Roy 2005). Macromolecules, lipids, proteins, and mtDNA within target tissue are particularly susceptible to oxidative damage by ROS. Excessive oxidative stress over time may be one of the mechanisms responsible for the degeneration of neurons and developmental brain abnormalities that consist of dysplastic neuronal lesions. Estimation of nuclear genes controlling mitochondrial biogenesis, CD and the effect of the environment using MCMC method showed that these latent variables had a very significant contribution in the development of intractable epilepsy. These data suggest that mitochondrial genetics play a significant role in the pathogenesis of epilepsy in children. Therefore, the mitochondrial injuries from changes in the copy number of mtDNA per cell, oxidative mtDNA damage and the presence of the mtDNA mutation resulting from oxidative stress, specific mtDNA SNPs plus environment could act jointly to cause intractable epilepsy. Overall, findings of this study indicate a role of mitochondria dysfunction in intractable epilepsy.
The strength of this study is the direct measurements of relative mtDNA copy number, oxidative mtDNA damage, and genotyping for mtSNPs from the lesioned brain tissues resected from the pediatric epilepsy patients. A major limitation of this study is the small sample size. However, results from this study provide the foundation for proper determination of sample size in pediatric intractable epileptics, such as the frequency of mtSNPs in pediatric epilepsy patients, and the mean and standard deviation for further research regarding measurement of oxidative mtDNA damage. In order to better explore the oxidative mtDNA damage, mtDNA copy number, and mtSNPs in children with intractable epilepsy a bigger sample size from a multi-facility (and institution) study is needed. Findings from this study raise the possibility that inhibition of mitochondrial dysfunction may play a role in successful treatment of intractable epilepsy.
In summary, the major novel findings which emerged from this study are that several novel potentially harmful mtDNA variants and increased mtDNA content are associated with intractable epileptogenesis. Joint effects of a wild 10398A allele, a variant 9952A, high mtDNA copy number and high oxidative damage to mtDNA dramatically increased dramatically the conditional probability of developing intractable epilepsy. Further validation of these findings in a cohort population of epilepsy patients with a bigger sample size to understand the exact role of mtDNA defects in epilepsy may lay the ground for the development of new therapies.
References
Andres M, Andre VM, Nguyen S, Salamon N, Cepeda C, Levine MS, Leite JP, Neder L, Vinters HV, Mathern GW (2005) Human cortical dysplasia and epilepsy: an ontogenetic hypothesis based on volumetric MRI and NeuN neuronal density and size measurements. Cereb Cortex 15:194–210
Ayala-Torres S, Chen Y, Svoboda T, Rosenblatt J, Van Houten B (2000) Analysis of gene-specific DNA damage and repair using quantitative polymerase chain reaction. Methods 22:135–147
Bai RK, Leal SM, Covarrubias D, Liu A, Wong LJ (2007) Mitochondrial genetic background modifies breast cancer risk. Cancer Res 67:4687–4694
Bai R, Wong L, Leal SM (2008) Mitochondrial DNA variant interactions modify breast cancer risk. J Hum Genet 53:924–928
Barkovich AJ, Kuzniecky RI, Jackson GD, Guerrini R, Dobyns WB (2005) A developmental and genetic classification for malformations of cortical development. Neurology 65:1873–1887
Baron M, Kudin A, Kunz W (2007) Mitochondrial dysfunction in neurodegenerative disorders. Biochem Soc Trans 35:1228–1231
Bindoff LA, Engelsen BA (2012) Mitochondrial diseases and epilepsy. Epilepsia 53(suppl 4):92–97
Brinckmann A, Weiss C, Wilbert F, von Moers A, Zwirner A, Stoltenburg-Didinger G, Wilichowski E, Schuelke M (2010) Regionalized pathology correlates with augmentations of mtDNA copy numbers in patients with myoclonic epilepsy with ragged-red fibers (MERRF-Syndrome). PLoS ONE 5:e13513
Canafoglia L, Franceschetti S, Antozzi C, Carrara F, Farina L, Granata T, Lamantea E, Savoiardo M, Uziel G, Villani F, Zeviani M, Avanzini G (2001) Epileptic phenotypes associated with mitochondrial disorders. J Neurol 56:1340–1346
Cardaioli E, Dotti MT, Hayek G, Zappella M, Federico A (1999) Studies on mitochondrial pathogenesis of Rett syndrome: ultrastructural data from skin and muscle biopsies and mutational analysis at mtDNA nucleotides 10463 and 2835. J Submicrosc Cytol Pathol 31:301–304
Chen C, Wu Y, Cheng M, Liu JL, Lee YM, Lee PW, Soong BW, Chiu DT (2007) Increased oxidative damage and mitochondrial abnormalities in the peripheral blood of Huntington’s disease patients. Biochem Biophys Res Commun 359:335–340
Chinnery PF, Hudson G (2013) Mitochondrial genetics. Br Med Bull 106:135–159
DiMauro S (2001) Lessons from mitochondrial DNA mutations. Semin Cell Dev Biol 9:397–405
El Sabbagh S, Lebre A-S, Bahi-Buisson N, Delonlay P, Soufflet C, Boddaert N, Rio M, Rçtig A, Dulac O, Munnich A, Desguerre I (2010) Epileptic phenotypes in children with respiratory chain disorders. Epilepsia 51:1225–1235
Felty Q, Roy D (2005) Estrogen, mitochondria, and growth of cancer and non-cancer cells. J Carcinog 4:e1
Filiano JJ, Goldenthal MJ, Rhodes H, Marín-García J (2002) Mitochondrial dysfunction in patients with hypotonia, epilepsy, autism, and developmental delay: HEADD syndrome. J Child Neurol 17:435–439
Fukuda M, Yamauchi H, Yamamoto H, Aminakab M, Murakamia H, Kamiyamaa N, Miyamotoa Y, Koitabashia Y (2008) The evaluation of oxidative DNA damage in children with brain damage using 8-hydroxyguanosine levels. Brain Dev 30:131–136
Geman S, Geman D (1984) Stochastic relaxation, Gibbs distributions and the Bayesian restoration of images. IEEE Trans Pattern Anal Mach Intell 6:721–742
Grazina M, Pratas J, Silva F, Oliveira S, Santana I, Oliveira C (2006) Genetic basis of Alzheimer’s dementia: role of mtDNA mutations. Genes Brain Behav 5(Suppl 2):92–107
Hader WJ, Mackay M, Otsubo H, Chitoku S, Weiss S, Becker L, Snead OC 3rd, Rutka JT (2004) Cortical dysplastic lesions in children with intractable epilepsy: role of complete resection. J Neurosurg 100:110–117
Hanna M, Nelson P, Rahman S, Lane RJM, Land L, Heales S, Cooper MJ, Schapira AHV, Morgan-Hughes JA, Wood NW (1998) Cytochrome c oxidase deficiency associated with the first stop-codon point mutation in human mtDNA. Am J Genet 63:29–36
Howell N, Oostra R, Bolhuis P, Spruijt L, Clarke LA, Mackey DA, Preston G, Herrnstadt C (2003) Sequence analysis of the mitochondrial genomes from Dutch pedigrees with Leber Hereditary Optic Neuropathy. Am J Genet 72:1460–1469
Hsieh RH, Li J-Y, Pang C-Y, Wei Y-H (2001) A novel mutation in the mitochondrial 16S rRNA gene in a patient with MELAS syndrome, diabetes mellitus, hyperthyroidism and cardiomyopathy. J Biomed Sci 8:328–335
Hua Y, Crino PB (2003) Single cell lineage analysis in human focal cortical dysplasia. Cereb Cortex 13:693–699
MITOMAP: A Human Mitochondrial Genome Database (2009) http://www.mitomap.org/MITOMAP.
Jizong Z, Zhou F, Hongmin B (2011) Surgical treatment of intractable epilepsy associated with focal cortical dysplasia. In Humberto Foyaca-Sibat (Ed.) Novel treatment of epilepsy, ISBN: 978-953-307-667-6: http://www.intechopen.com/books/novel-treatment-of-epilepsy/surgicaltreatment-of-intractable-epilepsy-associated-with-focal-cortical-dysplasia
Kunkle BW, Yoo C, Roy D (2013) Reverse engineering of modified genes by Bayesian Network analysis defines molecular determinants critical to the development of glioblastoma. PLoS ONE 8(5):e64140
Lee H, Wei Y (2005) Mitochondrial biogenesis and mitochondrial DNA maintenance of mammalian cells under oxidative stress. Int J Biochem Cell Biol 37:822–834
Lee H, Yin P, Lu C, Chi CW, Wei YH (2000) Increase of mitochondria and mitochondrial DNA in response to oxidative stress in human cells. Biochem J 348:425–432
Lee J, Park K, Im J, Kim MY, Lee DC (2010) Mitochondrial DNA copy number in peripheral blood associated with cognitive function in apparently healthy elderly women. Clin Chim Acta 411:592–596
Lehtonen MS, Moilanen JS, Majamaa K (2003) Increased variation in mtDNA in patients with familial sensorineural hearing impairment. Hum Genet 113:220–227
Lenroot R, Giedd J (2006) Brain development in children and adolescents: insights from anatomical magnetic resonance imaging. Neurosci Biobehav Rev 30:718–729
Liang MH, Wong LJ (1998) Yield of mtDNA mutation analysis in 2,000 patients. Am J Med Genet 77:395–400
Lin C, Wang L, Tsai C, Wei YH (2008) Low copy number and low oxidative damage of mitochondrial DNA are associated with tumor progression in lung cancer tissues after neoadjuvant chemotherapy. Interact Cardiovasc Thorac Surg 7:954–958
Liu C, Cheng W, Lee C, Ma YS, Lin CY, Huang CC, Wei YH (2006) Alterations in the copy number of mitochondrial DNA in leukocytes of patients with mitochondrial encephalomyopathies. Acta Neurol Scand 113:334–341
Lopez J, Gonzalez M, Lorigados L, Morales L, Riverón G, Bauzá JY (2007) Oxidative stress in surgically treated patients with refractory epilepsy. Clin Biochem 40:292–298
Luna B, Bhatia B, Ragheb B, Miller I, Jayakar P, Felty Q, Roy D (2011) Malformations of cortical development and epilepsy in children. Encycl Environ Health Gene Environ Interact 2:595–602
Malakhova L, Bezlepkin V, Antipova V, Ushakova T, Fomenko L, Sirota N, Gaziev AI (2005) The increase in mitochondrial DNA copy number in the tissue of γ-irradiated mice. Cell Mol Biol Lett 10:721–732
Okoh V, Deoraj A, Roy D (2011) Estrogen-induced ROS mediated redox signaling contributes in the development of breast cancer. Biochem Biophys Acta 1815:115–133
Patil C, Ahire Y, Pathade P, Pathade VV, Mali PR (2011) Free radical epilepsy and anti-oxidant: an overview. Int Res J Pharm 2:64–71
Pieczenik S, Neustadt J (2007) Mitochondrial dysfunction and molecular pathways of disease. Exp Mol Pathol 83:84–92
Rickert CH (2006) Cortical dysplasia: neuropathological aspects. Childs Nerv Syst 22:821–826
Roy D, Felty Q, Narayan S, Jayakar P (2007) Signature of mitochondria of steroidal hormones-dependent normal and cancer cells: potential molecular targets for cancer therapy. Front Biosci 12:154–173
Santorelli FM, Tanji K, Shanske S, DiMauro S (1997) Heterogeneous clinical presentation of the mtDNA NARP/T8993G mutation. Neurology 49:270–273
Schwartzkroin PA, Walsh CA (2000) Cortical malformations and epilepsy. Ment Retard Dev Diagn 6:268–280
Shah NS, Mitchell WG, Boles RG (2002) Mitochondrial disorders: a potential under-recognized etiology of infantile spasms. J Child Neurol 17:369–372
Shen J, Platek M, Mahasneh A, Ambrosone CB, Zhao H (2010) Mitochondrial copy number and risk of breast cancer: a pilot study. Mitochondrion 10:62–68
Shoffner JM, Brown MD, Torroni A, Lott MT, Cabell MF, Mirra SS, Beal MF, Yang CC, Gearing M, Salvo R, Watts RL, Juncos JL, Hansen LA, Crain BJ, Fayad M, Reckord CL, Wallace DC (1993) Mitochondrial DNA variants observed in Alzheimer disease and Parkinson disease patients. Genomics 17:171–184
Su S, Jou S, Cheng W, Lin T, Li J, Huang C, Lee Y, Soong B, Liu C (2010) Mitochondrial DNA damage in spinal and bulbar muscular atrophy patients and carriers. Clin Chim Acta 411:626–630
Szuhai KS, van den Ouweland JM, Dirks RW, Lemaître M, Truffert J, Janssen G, Tanke H, Holme E, Maassen J, Raap A (2001) Simultaneous A8344G heteroplasmy and mitochondrial DNA copy number quantification in myoclonus epilepsy and ragged-red fibers (MERRF) syndrome by multiplex molecular beacon based real-time fluorescence PCR. Nucleic Acids Res 29:e13
Thomas RD, Roy D (2001) Modifications in mitochondrial DNA by stilbene estrogen and hepatocarcinogenicity. Oncol Rep 8:1035–1038
Uusimaa J, Gowda V, McShane A, Smith C, Evans J, Shrier A, Narasimhan M, O'Rourke A, Rajabally Y, Hedderly T, Cowan F, Fratter C, Poulton J (2013) Prospective study of POLG mutations presenting in children with intractable epilepsy: prevalence and clinical features. Epilepsia 54:1002–1011
Waldbaum S, Patel M (2010a) Mitochondrial dysfunction and oxidative stress: a contributing link to acquired epilepsy. J Bioenerg Biomembr 42:449–455
Waldbaum S, Patel M (2010b) Mitochondria, oxidative stress, and temporal lobe epilepsy. Epilepsy Res 88:23–45
Wong M (2007) Mechanisms of epileptogenesis in tuberous sclerosis complex and related malformations of cortical development with abnormal glioneuronal proliferation. Epilepsia 48:617–630
Wong M (2009) Animal models of focal cortical dysplasia and tuberous sclerosis complex: recent progress towards clinical applications. Epilepsia 50(Suppl):34–44
Yoo C, Thorsson V, Cooper GF (2002) Discovery of causal relationships in a gene-regulation pathway from a mixture of experimental and observational DNA microarray data. Pac Symp Biocomput 7:498–509
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Luna, B., Bhatia, S., Yoo, C. et al. Bayesian Network and Mechanistic Hierarchical Structure Modeling of Increased likelihood of Developing Intractable Childhood Epilepsy from the Combined Effect of mtDNA Variants, Oxidative Damage, and Copy Number. J Mol Neurosci 54, 752–766 (2014). https://doi.org/10.1007/s12031-014-0364-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-014-0364-x