Abstract
MicroRNAs (miRNAs) are known as important regulators of gene expression and play important roles in diverse biological activities. However, the involvement of miRNAs in cerebral ischemia remains elusive. In the present study, using the middle cerebral artery occlusion (MCAO) model and oxygen-glucose deprivation/reperfusion (OGD/RP)-induced cell injury model, we found that the expression levels of miR-34c-5p were significantly reduced in MCAO rats and OGD/RP cells. Overexpression of miR-34c-5p could improve the increased brain infarction, brain water content and neurological scores in MCAO rats, as well as the abnormal expression of inflammatory cytokines (TNF-α, IL-6, COX-2, iNOS, IL-10) in OGD/RP cells. Moreover, overexpression of miR-34c-5p was found to inhibit the activity of nuclear factor-kappa B (NF-κB) by regulating the expression of nuclear receptor coactivator 1 (NCOA1), and increase the apoptotic rate of cortical neurons by inhibiting the expression of Caspase-3 and Bax and upregulating the expression of Bcl-2. Taken together, our findings demonstrated that miR-34c-5p plays an important role in cerebral ischemia/reperfusion injury, which may be mediated through inflammatory and apoptotic signaling pathways.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Stroke not only seriously endangers the physical and mental health of human beings, particularly of the elderly, but also imposes a huge economic burden on society. Among all types of stroke, ischemic stroke accounts for about 85% cases, which is mainly caused by nutrient and oxygen deficiency resulting from cerebrovascular embolization and infarction in the brain tissue (Pride et al. 2017). Although alteplase is known as an effective drug in the treatment of acute stroke, it cannot meet the needs of all stroke patients clinically due to the high risk in the thrombolysis process of alteplase and the limitation of treatment time window (Saver and Levine 2010; Bracard et al. 2016). Therefore, it is urgent to find more effective and safer drugs to treat stroke.
When cerebral ischemia occurs, in the central area of cerebral ischemia, blood flow is basically interrupted, sugar and oxygen are seriously deficient, and cell necrosis damage causes irreversible destruction of the brain tissue (Fan et al. 2017; Hu et al. 2017). Meantime, in the infarct peripheral area, the blood flow decreases significantly, further aggravating the self-destruction of cells affected by ischemia. Since the integrity of the cells in this area still exists, the damage is reversible at this time (Xia et al. 2017). Cerebral ischemia-reperfusion (I/R) can activate intracellular program death, such as cell necrosis, apoptosis or autophagy-related cell death (Deng et al. 2019), among which apoptosis is considered to be a major factor in ischemic brain injury (Yu et al. 2015; Xia et al. 2017). In addition, inflammatory response is known as another pivotal mechanism in cerebral I/R injury, which can lead to the activation of toxic enzyme, free radical overload and a series of tissue lesions. Therefore, it is speculated that anti-apoptosis and anti-inflammatory may be the potential effective measures in the treatment of cerebral I/R injury.
MiRNAs are important small molecules of endogenous RNAs with post-transcriptional regulation activities newly discovered in recent years (Lerner et al. 2011; Braicu et al. 2017). Several reports have demonstrated that MiRNAs are involved in the pathogenesis and progression of many ischemic diseases, including cerebral ischemia. Moreover, MiRNAs also hold great therapeutic potential (Malhas et al. 2010; Gao et al. 2018). In addition, it has been reported that miRNAs are involved in inflammatory response and apoptosis response after cerebral I/R injury. For example, miRNA-3473b contributes to stroke pathogenesis by enhancing post-stroke neuroinflammation injury by regulating the expression of SOCS3 (Wang et al. 2018). MiR-22 can prevent cerebral I/R injury through the attenuation of inflammation and neuron apoptosis (Deng et al. 2013). MiRNA-125b can aggravate cerebral I/R injury by regulating inflammatory cell aggregation and reactive oxygen species burst (Liang et al. 2018). MiR-34c-5p has been reported to function as a tumor suppressor in numerous cancer types (Wu et al. 2013). Moreover, it has been reported that downregulation of miR-34c-5p facilitates neuroinflammation in drug-resistant epilepsy, suggesting that miR-34c-5p also has an important role in neuroinflammation. In addition, it has been reported that up-regulation of miR-34c-5p induces cell apoptosis in many kind of cancer cells. We therefore speculated that miR-34c-5p might play an important role in cerebral I/R injury by regulating neuroinflammation and cell apoptosis.
Therefore, this study was to investigate the role and the underlying mechanism of miR-34c-5p in inflammatory response, neuronal proliferation and apoptosis during cerebral I/R injury, and shed light on the role of miR-34c-5p in the diagnosis of clinical cerebral I/R injury.
Materials and methods
Animals
Male Sprague-Dawley (SD) rats weighing 250–310 g were used in this study. Rats were housed in a 12 h light/dark cycle and temperature-controlled room. Rats were randomly divided into four groups (21 in each group) and experiments were performed in a blinded manner. All experimental protocols were performed in accordance with the Guidance of Third Affiliated Hospital of Nanchang University Animal Experimental and approved by the Ethics Committee of Third Affiliated Hospital of Nanchang University Animal Experimental.
MCAO model
Rats were anesthetized intraperitoneally with chloral hydrate (35 mg/kg) throughout the whole experiments. Body temperature and respiration rate were monitored perioperatively. MCAO model experiments were carried out as previously described (Fang et al. 2021). Briefly, a vertical midline cervical incision was made, then the right common carotid artery was exposed and dissected. The external carotid artery was divided (leaving 3–4 mm) after all branches of the external carotid artery were isolated, coagulated and transected. Then, the internal carotid artery was isolated, and the pterygopalatine artery was ligated close to its origin. The common carotid artery was clamped by a 5 mm aneurysm clip. A 4.0 monofilament nylon suture with an enlarged and round tip was inserted through the internal carotid artery after the external carotid artery stump was reopened. Insertion was stopped when resistance was felt, occluding the origin of the right MCAO. The suture was withdrawn to allow for reperfusion after 2 h of occlusion. Then, the external carotid artery was ligated, and the aneurysm clip was removed. Finally, the skin was sutured, and the animal was allowed to recover. In the sham group, the internal carotid artery was separated, clamped and the clamped for the same time as the model rats, but no wire plug was placed. The four groups included sham operation group (control), MCAO group (I/R), MCAO + scrambling group (Ad-scramble) and MCAO + miR-34c-5p group (Ad-miR-34c-5p).
Construction of the miR-34c-5p expression vector and gene transfer in vivo
Adenovirus expressing miR-34c-5p (Ad-miR-34c-5p) was constructed. Briefly, a DNA segment encompassing the miR-34c-5p was synthesized by Genechem (Shanghai, China). The obtained sequences were fully sequenced (Sangon, Shanghai, China). Ad-miR-34c-5p or control Ad-Scramble was generated using the ViraPower Adenoviral Expression System (Invitrogen, Carlsbad, CA) following the manufacturer’s instructions. The obtained adenoviruses were further packaged and amplified in HEK293 cells, and then purified using CsCl banding. In addition, sh-NCOA1 lentiviral particles were obtained from Santa Cruz Biotechnology (sc-36,555-V, Santa Cruz, CA). For in vivo gene transfer, the injected rats underwent dextral MCAO/reperfusion 3 d post-injection. Rats were anesthetized with 3% sodium pentobarbital and placed in a stereotactic instrument (RWD Life Science). Two sites on the right cortex surrounding the infarcted lesions were targeted for injection at the following coordinates: 1.0 mm rostral to the bregma, 2.0 mm lateral to the midline and 1.2 mm ventral to the dura; 3.0 mm caudal to the bregma, 1.5 mm lateral to the midline and 1.2 mm ventral to the dura. The Ad-miR-34c-5p (1 × 109 PFU), Ad-Scramble (1 × 109 PFU) or saline were injected at the indicated sites with a rate of 0.3 μl/min and a total volume of 2 μl per site. At the end of injection, the micro-injector was kept inserted for 5 min before withdrawal.
Immunofluorescence
Virus delivery was determined by observing green fluorescent protein (GFP) as previously described (Khodanovich et al. 2020). GFP-positive cells were observed at 3 d after injection to determine whether the virus had successfully transfected into cortical neurons. In brief, under deep anesthesia with 3% sodium pentobarbital (30 mg/kg body weight), rats were transcardially perfused with phosphate-buffered saline, followed by perfusion and immersion in 4% paraformaldehyde. Tissues were sliced into 10-μm-thick sections to observe GFP-positive cells using a laser scanning confocal microscope (Nikon 1R, Japan).
Evaluation of MCAO model
Rats were decapitated 24 h after cerebral ischemia-reperfusion injury. The whole brain was taken out, and left and right brain were separated. After removing the cerebellum and lower brainstem, the remaining forebrain was weighed. The right forebrain was then sectioned along the coronal plane. The sections were placed in TTC solution for 30 min and then moved to 10% formaldehyde fixator. The percentage of infarction was calculated as previously described (Men et al. 2015). The ZeaLonga scoring method was used to evaluate the neurological impairment. The specific criteria were as following: 0 point was without neurological injury symptoms; 1 point was that the forepaw on the opposite side of I/R brain could not be fully extended; 2 point was that the forepaw rotated to the opposite side of I/R brain during walking; 3 point was that the forepaw tilted to the opposite side of I/R brain during walking; 4 point was that the forepaw could not be fully extended. After 24 h of cerebral I/R injury, rats were decapitated, the olfactory bulb, cerebellum and lower brainstem were removed. Then, the wet mass of the remaining forebrain was weighed. After baking, dry mass was weighed again.
Primary cortical neuron culture
The primary cortical neurons were obtained from SD rats as described in literature (Li et al. 2010). Briefly, the cortex at embryonic day 17 (E17) and E18 of SD rats was collected and minced. The lysis was then stopped using DMEM/F12 medium. The cell suspension was centrifuged. The cell density was adjusted to 1 × 106 / mL and plated on a 96-well poly-L-lysine-coated plate. Cells were maintained in neurobasal medium (Gibco BRL, Rockville, MD, USA) with 2% B-27 (Gibco) supplement. After 72 h, arabinosylcytosine was added to the cultures to stop cell proliferation of astroglia and microglia, and the purity of neuronal cultures was more than 90%. After 24 h, the medium was changed, and then half of the medium was changed every 2 d. Cells were cultured in an incubator at 37 °C with a humidified atmosphere of 5% CO2. Cells were cultured for 7–8 d for subsequent experiments.
OGD/RP and adenovirus infection
OGD/RP experiments were carried out as previously described (Liu et al. 2018). Cortical neurons were infected with the control adenovirus or miR-34c-5p-expressing adenovirus for 6 h and then replaced with standard culture medium. At 72 h after adenovirus treatment, cells were subjected to OGD/R. Cortical neurons were exposed to glucose-free aCSF solution and incubated in an incubator with 1% O2/94% N2/5% CO2 at 37 °C for 6 h to produce OGD. Then, glucose-free aCSF was added, and cells were further cultured in an incubator with 5% CO2 and 95% O2 for 12 h. For cell transfection, a mixture of transfection agent Lipofectermine 2000 and Ad-miR-34c-5p or Ad-scramble were prepared and added into a 24-well plate where cells were cultured to make a final concentration of 100 nM. After 6 h of exposure to these mixtures, cells were cultured in standard medium for another 48 h. At the end, cells were collected for protein, apoptosis and other analyses.
Total RNA extraction and quantitative real time PCR
qRT-PCR was performed as described in the reference (Moltzahn et al. 2011). Total RNAs were extracted from primary cultured neurons using TRIzol reagent (Haigene, Haerbin, China). PCRs were performed using the ViiA™ 7 real-time PCR system (Life Technologies, Grand Island, NY). PCR conditions were: 95 °C for 10 min, 95 °C for 30 s, and 60 °C for 30 s, followed by 38 cycles of 74 °C for 25 s. The expression levels of miR-34c-5p and P65 were calculated using the 2-ΔΔCT method. The expression levels of P65 and miR-34c-5p were normalized to β-actin and U6, respectively. The primers sequences were as following: P65, forward: 5’-CCGCACCTCCACTCCATCC-3′, reverse: 5’-ACATCAGCACCCAAGGACACC3’; β-actin, forward: 5’-CCCATCTATGAGGGTTACGC-3′, reverse: 5’-TTTAATGTCACGCACGATTTC-3′; miR-34c-5p, forward: 5’-ATGGTTCGTGGGAGGCAGTGTAGTTAGCT-3′, reverse: 5’-GCAGGGTCCGAGGTATTC-3′; U6, forward: 5’-CTCGCTTCGGCAGCCCA-3′, reverse: 5’-AACGCTTCACGAATTTGGGT-3′.
Luciferase activity assay
The wild type (WT) or mutant (MUT) NCOA1 binding to miR-34c-5p was subcloned into pGL3 Basic vector. MiR-34c-5p (RiboBio, Guangzhou, China) was co-transfected into primary cortical neurons with 10 μg of pLUC-WT-NCOA1 or pLUC-MUT-NCOA1. After 48 h, luciferase activity was tested using a dual luciferase assay system (Promega Corporation, Fitchburg, WI, USA).
Western blotting
Western blotting was performed as previously described (Sayre et al. 2010). Protein concentrations were quantified using the BCA Protein Assay Kit. After denaturing in boiling water for 10 min, protein samples were separated using SDS-PAGE gel (10%), followed by transferring to PVDF membrane. The membrane was incubated with anti-P65 antibody (1:500, Youliante, Wuhan, China), Bcl-2 antibody (1:1000, Youliante, Wuhan, China), Bax antibody (1:1000, Youliante, Wuhan, China), COX-2 antibody (1:500, Youliante, Wuhan, China), iNOS antibody (1:500, Youliante, Wuhan, China), NCOA1 antibody (1:500, Youliante, Wuhan, China) and β-actin antibody (1:1000, Hengyuan, Shanghai, China) overnight. Then anti-rabbit secondary antibody (1:1000, Hengyuan, Shanghai, China) was added for incubation of another 1 h.
Elisa
The expression of IL-6, TNF-α and IL-10 were measured by ELISA kits (Primegene, Shanghai, China). Following the instructions, 20 μL of sample was taken, which allowed to perform only one ELISA test. The results were read by Wallac 1420 Victor 2 multilabel counter (Wallac, Turku, Finland). All samples were tested on the same day to eliminate any inter-assay variation. Quality control was performed using a standardized kit with internal controls and automated washes and detection.
Detection of apoptotic cells by flow cytometry
After OGD/RP treatment, cells were plated at a density of 5 × 105 cells per well, and cells were harvested and counted when grown to logarithmic growth phase. After centrifugation, cells were resuspended by adding 195 μL of Annexin V-FITC binding solution. Next, 5 μL of Annexin V-FITC and 10 μL of propidium iodide staining solution were added to mix, followed by an ice bath.
Caspase-3 activity assay
Caspase-3 activity was measured by the Caspase-3 Fluorometric Assay Kit (Amyjet, Wuhan, China) following the manufacturer’s instructions. After 24 h, cells were incubated with Caspase-Glo reagent for 30 min. Absorbance value (560 nm) was determined by a TECAN GenioPro plate reader.
Statistical methods
Data were analyzed by SPSS 19.0 statistical software. All data were presented as the mean ± stand deviation (SD). One-way ANOVA was used to assess the differences, and Tukey’s honestly Significant Difference (Tukey’s HSD) was used for subsequent analysis. P < 0.05 was considered as statistically significant difference.
Results
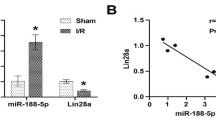
MiR-34c-5p was down-regulated after I/R treatment
GFP-positive cells were observed at 3 d after gene injection (Fig. 1A), suggesting that the cortical neurons were successfully transfected by virus. As shown in Fig. 1B, after 24 h of reperfusion, the expression levels of miR-34c-5p were significantly reduced in I/R group (F(3,20) = 140.011, t = 3.131, P = 0.014) and Ad-scramble group (F(3,20) = 140.011, t = 3.243, P = 0.012) compared with the control group (Fig. 1B, I/R group, p < 0.05; Ad-scramble group, p < 0.05). After 3 d of infection, the expression levels of the miR-34c-5p were significantly increased compared with that in the control group (Fig. 1B, p < 0.01) (F(3,20) = 140.011, t = −14.337, P < 0.01) and Ad-scramble group (Fig. 1B, p < 0.01) (F(3,20) = 140.011, t = −17.580, P < 0.01). In addition, as shown in Fig. 1C, miR-34c-5p was significantly down-regulated in the OGD group (F(3,8) = 145.016, t = 2.773, P = 0.024) and the Ad-scramble group (F(3,8) = 145.016, t = 2.693, P = 0.027) compared with that in the control group (Fig. 1C, OGD group, p < 0.05; Ad-scramble group, p < 0.05). Compared with the control group (F(3,8) = 145.016, t = −15.012, P < 0.01) and the Ad-scramble group (F(3,8) = 145.016, t = −17.705, P < 0.01), the expression levels of miR-34c-5p were significantly increased in Ad-miR-34c-5p-transfected neurons (Fig. 1C, p < 0.01). These results suggested that I/R treatment induced down-regulation of miR-34c-5p.
The expression of miR-34c-5p after brain I/R. (a) Immunofluorescence pictures (200 × magnification, bar = 100 μm) of Ad-miR-34c-5p in rat brain (cortex) after cerebral I/R injury. (b) The expression of miR-34c-5p in I/R rat model. N = 6. (c) The expression of miR-34c-5p in OGD treated cortical cells. N = 3. * P < 0.05, ** P < 0.01 vs control; ## P < 0.01 vs I/R or OGD group
Effects of miR-34c-5p on brain infarction, brain water content and neurological symptoms
To investigate the effects of miR-34c-5p on cerebral ischemia, the infarct volume of the brain was first assessed using TTC staining. As shown in Fig. 2A, the infarct volume was significantly increased in I/R groups compared with that in the control group (F(3,20) = 106.340, t = −16.327, P < 0.01) (Fig. 2A, p < 0.01), while it was significantly reduced in Ad-miR-34c-5p group compared with that in Ad-scramble group (F(3,20) = 106.340, t = 11.225, P < 0.01) (Fig. 2A, p < 0.01). Furthermore, the neurological score (F(3,20) = 116.667, t = −16.181, P < 0.01) and brain water content (F(3,20) = 45.663, t = −9.257, P < 0.01) were significantly increased in I/R group compared with that in the control group (Fig. 2B and C, p < 0.01), while they were significantly reduced in Ad-miR-34c-5p group compared with that in Ad-scramble group (Fig. 2B, F(3,20) = 116.667, t = 8.090, P < 0.01; Fig. 2C, F(3,20) = 45.663, t = 6.685, P < 0.01) (Fig. 2B and C, p < 0.01). These results indicated that overexpression of miR-34c-5p had a neuroprotective effect on cerebral ischemia.
The effect of miR-34c-5p on infarct volume, neurological scores, and brain water content. (a) Quantitative analysis of TTC staining and infarct volume in brain sections of the control, Scramble and miR-34c-5p overexpressing groups. (b) Neurological score 24 h after reperfusion. (c) Brain water content within 24 h after brain reperfusion. N = 6. ** P < 0.01 vs control; ## P < 0.01 vs I/R or OGD group
Inflammatory cytokines were involved in the action of miR-34c-5p in OGD/RP induced injury
To further explore the underlying mechanism of miR-34c-5p in cerebral ischemia, Western blotting and ELISA were performed. As shown in Fig. 3A-3E, the expression levels of iNOS (F(3,8) = 42.720, t = −9.101, P < 0.01), COX-2 (F(3,8) = 54.139, t = −10.088, P < 0.01), TNF-α (F(3,8) = 24.696, t = −7.546, P < 0.01) and IL-6 (F(3,8) = 25.184, t = −7.251, P < 0.01) in primary cortical neurons in the OGD group were significantly increased compared with that in the control group (Fig. 3A-3D, p < 0.01), while the expression levels of IL-10 (F(3,8) = 49.199, t = 10.049, P < 0.01) were significantly decreased (Fig. 3E, p < 0.01). Compared with the Ad-scramble group, overexpression of miR-34c-5p in cortical neurons significantly inhibited the expression of iNOS (F(3,8) = 42.720, t = 6.500, P < 0.01), COX-2 (F(3,8) = 54.139, t = 7.417, P < 0.01), TNF-α (F(3,8) = 24.696, t = 3.487, P = 0.008) and IL-6 (F(3,8) = 25.184, t = 4.512, P = 0.002) (Fig. 3A-3D, p < 0.05, p < 0.01), but significantly increased the expression levels of IL-10 (F(3,8) = 49.199, t = −6.544, P < 0.01) in Ad-miR-34c-5p group (Fig. 3E, p < 0.01). These results indicated that inflammatory cytokines were involved in the effect of miR-34c-5p on cerebral ischemia.
The effect of overexpression of miR-34c-5p on cerebral cortical neuronal cytokines (TNF-α, IL-6, IL-10, COX-2 and iNOS) after OGD treatment. The expression of iNOS (a) and COX-2 (b). MiR-34c-5p overexpresses mRNA expression of IL-6 (c), TNF-α (d) and IL-10 (e). N = 3. * P < 0.05, ** P < 0.01 vs control; #P < 0.05, ##P < 0.01 vs I/R or OGD group
Effect of miR-34c-5p on the activity of nuclear factor-kappa B (NF-κB)
The effect of miR-34c-5p on NF-кB activity was then explored. As shown in Fig. 4A and B, the expression levels of P65 in OGD group were significantly increased compared with that in the control group (p < 0.01) at both mRNA (F(3,8) = 32.577, t = −8.026, P < 0.01) and protein (F(3,8) = 42.994, t = −9.134, P < 0.01) levels. However, compared with Ad-scramble group, overexpression of miR-34c-5p in primary cortical neurons significantly inhibited the expression of P65 (Fig. 4A, F(3,8) = 32.577, t = 5.418, P = 0.001; Fig. 4B, F(3,8) = 42.994, t = 6.462, P < 0.01) (p < 0.01), indicating that miR-34c-5p could regulate the expression of P65. In addition, as shown in Fig. 4C, the expression levels of NCOA1 (F(3,8) = 43.272, t = −9.031, P < 0.01) in the primary cortical neurons of OGD group were significantly increased compared with that in the control group (p < 0.01). However, compared with Ad-scramble group, overexpression of miR-34c-5p in primary cortical neurons significantly inhibited the expression of NCOA1 (F(3,8) = 43.272, t = 6.503, P < 0.01) (p < 0.01), indicating that miR-34c-5p could regulate the expression of NCOA1. Moreover, GFP-positive cells were observed at 3 d after gene injection (Fig. 4D), suggesting that the cortical neurons were successfully transfected by virus. To assess the interaction between miR-34c-5p and NCOA1, bioinformatics analysis (Fig. 6A) and luciferase reporter assay (F(3,8) = 36.236, t = 8.378, P < 0.01) (WT-NC-mimic vs WT-miR-34c-5p-mimic) (Fig. 6B, p < 0.01) were performed and the results showed that NCOA1 was targeted by miR-34c5p in primary cortical neurons (Fig. 6). In addition, with the downregulation of NCOA1 by transfection of SI-NCOA1 (vs Control, F(2,6) = 111.327, t = 3.138, P = 0.020; vs OGD, F(2,6) = 111.327, t = 14.203, P = 0.020) (Fig. 4 E, p < 0.01), the expression of P65 (F(2,6) = 38.666, t = 4.237, P = 0.022), infarct volume of MCAO model rats (F(2,15) = 141.631, t = 6.037, P = 0.001) and apoptotic rate of primary cortical neurons after OGD/RP treatment (F(2,6) = 71.029, t = 4.428, P = 0.004) were all decreased (Fig. 4F, p < 0.05; 4G and 4H, p < 0.01). These results demonstrated that miR-34c-5p regulated NF-кB activity by regulating NCOA1.
The effect of miR-34c-5p on NF-кB activity. (a) The expression of p65. (b) The expression levels of p65. (c) The expression levels of NCOA1. Adenovirus expressing miR-34c-5p was infected in cortical neuronal cells. (d) Immunofluorescence pictures (200× magnification, bar = 100 μm) of sh-NCOA1 in rat brain (cortex) after cerebral I/R injury. (e) The expression of NCOA1 in cortical neuron cells infected with lentiviral particles expressing NCOA1 shRNA. (f) The expression of p65 after knockdown of NCOA1. (g) Quantitative analysis of TTC staining and infarct volume in brain sections of the control, I/R and sh-NCOA1 overexpressing groups. N = 3. * P < 0.05, ** P < 0.01 vs control; #P < 0.05, ##P < 0.01, vs I/R or OGD group
The effects of miR-34c-5p on neuronal apoptosis
The effect of miR-34c-5p on neuronal apoptosis was further investigated. As shown in Fig. 5A, compared with the control group, the apoptosis rate of primary cortical neurons in OGD group was significantly increased (F(3,8) = 61.609, t = −11.630, P < 0.01) (Fig. 5A, p < 0.01), while it was decreased in Ad-miR-34c-5p group compared with that in Ad-scramble group (F(3,8) = 61.609, t = 5.926, P < 0.01) (Fig.5A, p < 0.01). As shown in Fig. 5B-5D, the expression levels of caspase-3 (F(3,8) = 72.742, t = −12.456, P < 0.01) and Bax (F(3,8) = 43.341, t = −9.574, P < 0.01) were significantly increased in OGD group compared with that in the control group (p < 0.01), while the expression levels of Bcl-2 (F(3,8) = 54.135, t = 6.663, P < 0.01) was significantly decreased (p < 0.01). However, compared with Ad-scramble group, overexpression of miR-34c-5p in primary cortical neurons reduced the expression levels of caspase-3 (F(3,8) = 72.742, t = 7.323, P < 0.01) and Bax (F(3,8) = 43.341, t = 5.858, P < 0.01) (p < 0.01), but increased the expression levels of Bcl- 2 (F(3,8) = 54.135, t = −10.423, P < 0.01) (p < 0.01). Taken together, these results suggested that apoptotic factors are involved in the effect of miR-34c-5p on cerebral ischemia (Fig. 6).
The effect of miR-34c-5p on neuronal apoptosis. (a) Flow cytometry measured apoptosis of cortical neurons. (b) Overexpression of miR-34c-5p inhibited caspase-3 activation. (c) The expression of Bcl-2. (d) The expression levels of Bcl-2. N = 3. * P < 0.05, ** P < 0.01 vs control; ##P < 0.01 vs I/R or OGD group
Discussion
Ischemic stroke is one of the most common life-threatening neurologic diseases and the leading cause of serious long-term disability. Currently, thrombolytic drug therapy is used for treating acute ischemic stroke, but the curative effect is limited. It has been reported that miRNAs are closely related to the development, differentiation and biological functions of the nervous system (De et al. 2013). Moreover, miRNAs were reported to be involved in the occurrence of ischemic cerebrovascular disease (Kim et al. 2018),(Zhou et al. 2016). In the present study, we found that the expression levels of miR-34c-5p were significantly reduced in MCAO rats and OGD/RP cells. Overexpression of miR-34c-5p could improve I/R injury in MCAO rats and OGD/RP cells, and the improvement role of miR-34c-5p might be mediated by inflammation and apoptosis signaling pathway.
Sudden recovery of ischemia during reperfusion causes a large number of neutrophils to enter the ischemic tissue from the circulating blood, resulting in an acute inflammatory response (Shi et al. 2017). The activation and release of inflammatory cells can change the structure of myocardium, and regulating the activity and release of inflammatory cells can effectively prevent heart disease. Studies have shown that inflammatory factors substantially increase when inflammatory responses are exacerbated under stress conditions (Zhang et al. 2014a). Inflammatory mediators such as TNF-α, IL-6, iNOS and COX-2 play key roles in brain I/R injury (Yun et al. 2016; Park et al. 2017). Previous studies have reported that multiple miRNAs involves in inflammatory responses in various human diseases including miR-9-5p in myocardial infarction (Xiao et al. 2019), miR-32-5p in mycobacterial infection (Zhang et al. 2017) and miR-1252 in papillary thyroid cancer (Hu et al. 2020). In the present study, it was found that the expression levels of COX-2, iNOS, TNF-α and IL-6 were increased in primary cortical neurons treated by OGD, while the expression levels of IL-10 were decreased. However, overexpression of miR-34c-5p inhibited the expression of TNF-α, IL-6, iNOS and COX-2, and increased the expression levels of IL-10. These results suggest that overexpression of miR-34c-5p activates endogenous anti-inflammatory factors, thereby protecting neurons from injury.
NF-κB plays a key role in cerebral I/R injury and is considered to be the initiating factor of the inflammatory cascade after cerebral ischemia (Meng et al. 2017). Studies have found that initiation of NF-κB in neuronal cells promotes the formation of cerebral infarction (Zhang et al. 2014a, b). The activation of NF-κB after cerebral I/R injury is mainly expressed in the ischemic and ischemic peripheral areas. Activated NF-κB regulates the expression of cytokines, such as TNF-α, iNOS and IL-1β, which in turn affects the inflammatory cascade, amplifies the inflammatory effect and ultimately leads to aggravation of brain damage. Inhibition of NF-κB activation can significantly reduce the brain injury after cerebral ischemia (Ning et al. 2017). NCOA1 can affect the activity of sex hormone receptors by interacting with nuclear receptors on DNA, thereby affecting biological functions such as growth, development and inflammation of the body (Qin et al. 2014). In this study, we found that there was a significant P65 subunit translocation, and overexpression of miR-34c-5p inhibited p65 activity. Moreover, the expression levels of NCOA1 were reduced in cortical neurons overexpressing miR-34c-5p. Furthermore, the activity of NF-кB was inhibited by si-NCOA1. These results demonstrated that miR-34c-5p regulated NF-кB activity by NCOA1. The main pathological feature of I/R injury is apoptosis. Studies have confirmed the existence of cardiomyocyte apoptosis at the edge of infarcted area after I/R injury (Zhao et al. 2017). Our study also demonstrated that the apoptotic rate of primary cortical neurons increased after OGD treatment. In addition, we found that overexpression of miR-34c-5p in cortical neurons inhibited the apoptotic rate of primary cortical neurons after OGD treatment.
The Bcl-2 family includes the proapoptotic protein Bax and the anti-apoptotic protein Bcl-2, the external stimuli can be transmitted to the mitochondria to activate Caspase-3 to induce apoptosis (Salakou et al. 2007). Studies have shown that overexpression of Bcl-2 significantly reduces infarct size and cardiomyocyte apoptosis after I/R injury (Rosca et al. 2012). This study found that the expression levels of Caspase-3 and Bax were increased in OGD/RP cells, while the expression levels of Bcl-2 were decreased. Overexpression of miR-34c-5p could down-regulate the increased expression of Caspase-3 and Bax in OGD/RP cells, and up-regulate the decreased expression of Bcl-2 in OGD/RP cells. These results suggest that miR-34c-5p may be used to treat the cerebral I/R injury, and its neuroprotective role may be mediated through inflammatory and apoptotic signaling pathways.
Conclusion
In conclusion, miR-34c-5p reduced the cerebral I/R injury by inhibiting inflammatory and apoptotic signaling pathways. Our findings provide new insights into the mechanism by which miR-34c-5p involves in the cerebral I/R injury. MiR-34c-5p may be a potential targets for attenuating cerebral I/R injury.
Data availability
The analyzed data sets generated during the study are available from the corresponding author on reasonable request.
Abbreviations
- I/R:
-
Ischemia-Reperfusion
- miRNAs:
-
MicroRNAs
- SD:
-
Sprague-Dawley
References
Bracard S, Ducrocq X, Mas JL, Soudant M, Oppenheim C, Moulin T, Guillemin F, THRACE investigators (2016) Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol 15(11):1138–1147
Braicu OL, Budisan L, Buiga R, Jurj A, Achimas-Cadariu P, Pop L, Braicu C, Irimie A, Berindan-Neagoe I (2017) miRNA expression profiling in formalin-fixed paraffin-embedded endometriosis and ovarian cancer samples. Oncotarget Ther 10:4225–4238
De SÉ, Walter LT et al (2013) Developmental and functional expression of miRNA-stability related genes in the nervous system. PLoS One 8(5):e56908
Deng XH, Zhong Y, Gu LZ, Shen W, Guo J (2013) MiR-21 involve in ERK-mediated upregulation of MMP9 in the rat hippocampus following cerebral ischemia. Brain Res Bull 94:56–62
Deng Y, Ma G, Dong Q, Sun X, Liu L, Miao Z, Gao F (2019) Overexpression of miR4 alleviates apoptosis from cerebral ischemia reperfusion injury by targeting FIP200. J Cell Biochem 120(10):17151–17158
Fan YY, Hu WW et al (2017) Postconditioning-induced neuroprotection, mechanisms and applications in cerebral ischemia. Neurochem Int 107:S0197018616303680
Fang H, Li HF et al. (2021) HDAC3 Downregulation improves cerebral ischemic injury via regulation of the SDC1-dependent JAK1/STAT3 signaling pathway through miR-19a Upregulation. Molecular Neurobiology
Gao G, Tian Z et al. (2018) miRNA-133b targets FGFR1 and presents multiple tumor suppressor activities in osteosarcoma. Cancer cell international 18(1)
Hu GQ, Du X et al (2017) Inhibition of cerebral ischemia/reperfusion injury-induced apoptosis: nicotiflorin and JAK2/STAT3 pathway. Neural Regen Res 12(1):96–102
Hu ZG, Zhao PX et al (2020) Hsa_circ_0011290 regulates proliferation, apoptosis and glycolytic phenotype in papillary thyroid cancer via miR-1252/FSTL1 signal pathway. Arch Biochem Biophys 685:108353
Khodanovich MY, Akulov AE, Anan’ina TV, Kudabaeva MS, Pishchelko AO, Krutenkova EP, Nemirovich-Danchenko NM, Svetlik MV, Tumentceva YA, van den Haute C, Gijsbers R, Daniëls V, Thiry I, Pershina AG, Shadrina MM, Naumova AV (2020) Tissue-specific ferritin- and GFP-based genetic vectors visualize neurons by MRI in the intact and post-ischemic rat brain. Int J Mol Sci 21(23)
Kim JO, Bae J, Kim J, Oh SH, An HJ, Han IB, Oh D, Kim OJ, Kim NK (2018) Association of MicroRNA biogenesis genes polymorphisms with ischemic stroke susceptibility and post-stroke mortality. J Stroke 20(1):110–121
Lerner M, Lundgren J, Akhoondi S, Jahn A, Ng HF, Moqadam FA, Oude Vrielink JAF, Agami R, den Boer ML, Grandér D, Sangfelt O (2011) MiRNA-27a controls FBW7/hCDC4-dependent cyclin E degradation and cell cycle progression. Cell Cycle 10(13):2172–2183
Li JH, Wang YH et al (2010) Developmental changes in localization of NMDA receptor subunits in primary cultures of cortical neurons. Eur J Neurosci 10(5):1704–1715
Liang Y, Xu J, Wang Y, Tang JY, Yang SL, Xiang HG, Wu SX, Li XJ (2018) Inhibition of MiRNA-125b decreases cerebral ischemia/reperfusion injury by targeting CK2α/NADPH oxidase signaling. Cell Physiol Biochem Int J Exp Cell Physiol Biochem Pharmacol 45(5):1818–1826
Liu Y, Wang H, Yang M, Liu N, Zhao Y, Qi X, Niu Y, Sun T, Li Y, Yu J (2018) Cistanche deserticola polysaccharides protects PC12 cells against OGD/RP-induced injury. Biomed Pharmacother 99:671–680
Malhas A, Saunders NJ, Vaux DJ (2010) The nuclear envelope can control gene expression and cell cycle progression via miRNA regulation. Cell Cycle 9(3):531–539
Men M, Zhang L, Li T, Mi B, Wang T, Fan Y, Chen Y, Shen G, Liang L, Ma A (2015) Prognostic value of the percentage of neutrophils on admission in patients with ST-elevated myocardial infarction undergoing primary percutaneous coronary intervention. Arch Med Res 46(4):274–279
Meng QT, Chen R, Chen C, Su K, Li W, Tang LH, Liu HM, Xue R, Sun Q, Leng Y, Hou JB, Wu Y, Xia ZY (2017) Transcription factors Nrf2 and NF-κB contribute to inflammation and apoptosis induced by intestinal ischemia-reperfusion in mice. Int J Mol Med 40(6):1731–1740
Moltzahn F, Olshen AB, Baehner L, Peek A, Fong L, Stöppler H, Simko J, Hilton JF, Carroll P, Blelloch R (2011) Microfluidic-based multiplex qRT-PCR identifies diagnostic and prognostic microRNA signatures in the sera of prostate Cancer patients. Cancer Res 71(2):550–560
Ning Z, Xiang Y et al. (2017) Schisandrin B prevents hind limb from ischemia-reperfusion-induced oxidative stress and inflammation via MAPK/NF-κB pathways in rats. 2017(5): 1-8
Park J, Chung T et al (2017) Ascofuranone inhibits lipopolysaccharide–induced inflammatory response via NF-kappaB and AP-1, p-ERK, TNF-α, IL-6 and IL-1β in RAW 264.7 macrophages. PloS One 12(2):e0171322
Pride GL, Fraser JF, Gupta R, Alberts MJ, Rutledge JN, Fowler R, Ansari SA, Abruzzo T, Albani B, Arthur A, Baxter B, Bulsara KR, Chen M, Delgado Almandoz JE, Gandhi CD, Heck D, Hetts SW, Hirsch JA, Hussain MS, Klucznik R, Lee SK, Mack WJ, Leslie-Mazwi T, McTaggart R, Meyers PM, Mocco J, Prestigiacomo C, Patsalides A, Rasmussen P, Starke RM, Sunenshine P, Frei D, Jayaraman MV, Standards and Guidelines Committee of the Society of NeuroInterventional Surgery (SNIS) (2017) Prehospital care delivery and triage of stroke with emergent large vessel occlusion (ELVO): report of the standards and guidelines Committee of the Society of Neurointerventional surgery. J NeuroIntervention Surg 9(8):802–812
Qin L, Wu YL, Toneff MJ, Li D, Liao L, Gao X, Bane FT, Tien JCY, Xu Y, Feng Z, Yang Z, Xu Y, Theissen SM, Li Y, Young L, Xu J (2014) NCOA1 directly targets M-CSF1 expression to promote breast Cancer metastasis. Cancer Res 74(13):3477–3488
Rosca AM, Matei C et al (2012) Cardiomyocyte apoptosis in ischaemia-reperfusion due to the exogenous oxidants at the time of reperfusion. Cell Biol Int 36(12):1207–1215
Salakou S, Kardamakis D et al (2007) Increased Bax/Bcl-2 ratio up-regulates caspase-3 and increases apoptosis in the thymus of patients with myasthenia gravis. Vivo 21(1):123
Saver JL, Levine SR (2010) Alteplase for ischaemic stroke--much sooner is much better. Lancet 375(9727):1667–1668
Sayre KR, Dodd RY et al (2010) False–positive human immunodeficiency virus type 1 western blot tests in noninfected blood donors. Transfusion 36(1):45–52
Shi J, Dai W et al. (2017) Therapeutic hypothermia reduces the inflammatory response following ischemia/reperfusion injury in rat hearts. Therapeutic Hypothermia & Temperature Management
Wang XY, Chen SS et al. (2018) miRNA-3473b contributes to neuroinflammation following cerebral ischemia. Cell Death Dis 9
Wu H, Huang M, Lu M, Zhu W, Shu Y, Cao P, Liu P (2013) Regulation of microtubule-associated protein tau (MAPT) by miR-34c-5p determines the chemosensitivity of gastric cancer to paclitaxel. Cancer Chem Pharmacol 71(5):1159–1171
Xia M, Ding Q et al (2017) Remote limb ischemic preconditioning protects rats against cerebral ischemia via HIF-1α/AMPK/HSP70 pathway. Cell Mol Neurobiol 37(6):1–10
Xiao YM, Zhang YX et al (2019) Inhibition of MicroRNA-9-5p protects against cardiac remodeling following myocardial infarction in mice. Hum Gene Ther 30(3):286–301
Yu H, Wu M, Zhao P, Huang Y, Wang W, Yin W (2015) Neuroprotective effects of viral overexpression of microRNA–22 in rat and cell models of cerebral ischemia–reperfusion injury. J Cell Biochem 116(2):233–241
Yun HC, Na BH et al (2016) Anti-inflammatory function of 4-tert-butylphenyl salicylate through down-regulation of the NF-kappa B pathway. Arch Pharm Res 39(3):1–8
Zhang G-Y et al (2014b) Expression of Bcl-2 and NF-κB in brain tissue after acute renal ischemia-reperfusion in rats. Asian Pac J Trop Med 7(5):386–389
Zhang MJ, Wu XW et al (2017) The cystathionine beta-synthase/hydrogen sulfide pathway contributes to microglia-mediated neuroinflammation following cerebral ischemia. Brain Behav Immun 66:332–346
Zhang R, Wugeti N, Sun J, Yan H, Guo Y, Zhang L, Ma M, Guo X, Jiao C, Xu W, Li T, Liu H, Ma Y (2014a) Effects of vagus nerve stimulation via cholinergic anti-inflammatory pathway activation on myocardial ischemia/reperfusion injury in canine. Int J Clinic Exp Med 7(9):2615–2623
Zhao Q, Cui Z, Zheng Y, Li Q, Xu C, Sheng X, Tao M, Xu HX (2017) Fenofibrate protects against acute myocardial I/R injury in rat by suppressing mitochondrial apoptosis as decreasing cleaved caspase-9 activation. Cancer Biomark 19(4):455–463
Zhou Y, Chen Q, Lew KS, Richards AM, Wang P (2016) Discovery of potential therapeutic miRNA targets in cardiac ischemia-reperfusion injury. J Cardiovasc Pharmacol Ther 21(3):296–309
Author information
Authors and Affiliations
Contributions
YRT, YH contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All experimental protocols were performed in accordance with the Third Affiliated Hospital of Nanchang University Animal Experimental Guide and approved by the Third Affiliated Hospital of Nanchang University Animal Experimental Ethics Committee.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary Figure 1
Full-size immunoblots related to all western blot examples that were shown. (DOCX 166 kb)
Rights and permissions
About this article
Cite this article
Tu, Y., Hu, Y. MiRNA-34c-5p protects against cerebral ischemia/reperfusion injury: involvement of anti-apoptotic and anti-inflammatory activities. Metab Brain Dis 36, 1341–1351 (2021). https://doi.org/10.1007/s11011-021-00724-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-021-00724-5