Abstract
Emerging evidence has shown that ursolic acid exerts antidepressant-like effects, however, its ability to elicit an antidepressant-like response in rodents subjected to stress model that mimics behavioral and neurochemical alterations found in depression remains to be determined. Thus, this study investigated the possible antidepressant-like effect of ursolic acid in mice subjected to chronic unpredictable stress (CUS) for 14 days, and whether this effect could be associated with the modulation of serum corticosterone levels and hippocampal Bcl-2/Bax mRNA expression. Our results indicated that CUS induced a depressive-like behavior, as demonstrated by an increase in the immobility time and latency to first grooming in the tail suspension test and splash test, respectively. Conversely, the repeated administration of ursolic acid (0.1 mg/kg, p.o.) or fluoxetine (10 mg/kg, p.o.) in the last 7 days of CUS completely prevented CUS-induced behavioral alterations, suggesting an antidepressant-like effect. Additionally, CUS significantly increased the mRNA expression of Bax (pro-apoptosis marker), but not Bcl-2 (anti-apoptosis marker) in the hippocampus. Moreover, reduced hippocampal mRNA expression of Bcl-2/Bax ratio was detected in CUS-exposed mice. Ursolic acid, but not fluoxetine, prevented CUS-induced increase in the expression of Bax, but both ursolic acid and fluoxetine prevented CUS-induced reduction on Bcl-2/Bax ratio. Furthermore, neither CUS nor treatments with ursolic acid or fluoxetine altered serum corticosterone levels. Our study unveils the ability of ursolic acid to prevent the depressive-like behavior induced by stress and the modulation of Bcl-2/Bax expression could be associated with this response.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Major depressive disorder (MDD) is a highly prevent psychiatric disorder that affects nearly 350 million people worldwide (World Health Organization 2017). Currently, this medical condition is the main cause of disability resulting in elevated costs to the economy and a great burden for society (Otte et al. 2016; World Health Organization 2017). Although MDD has multifactorial pathophysiology, stressful life events are major predisposing risk factors for developing this disorder, and indeed roughly 80% of MDD episodes are preceded by a stress event (Goodyer et al. 2000; Pariante and Lightman 2008). These findings are supported by preclinical studies using animal stress paradigms such as chronic unpredictable stress, a stress-based model able to induce depressive-like behavior in rodents which is counteracted by antidepressant medications (Manosso et al. 2016; Liu et al. 2017; Gawali et al. 2017; Zhang et al. 2019). Notably, chronic stress may lead to the hypothalamic-pituitary-adrenal (HPA) axis dysfunction resulting in high systemic levels of glucocorticoids, namely cortisol in humans and corticosterone in rodents (Watson and Mackin 2006; Cox et al. 2011).
In the central nervous system, glucocorticoids may damage the hippocampus, a brain region that expresses a high density of glucocorticoid receptors and is critical for the regulation of the HPA axis feedback mechanism (Lee et al. 2002; Mizoguchi et al. 2003; Anacker et al. 2011). Particularly, compelling reports have demonstrated that glucocorticoids induce neural cell death in the hippocampus by reducing the trophic support, mainly the brain-derived neurotrophic factor (BDNF) levels, besides stimulating the inflammatory and pro-apoptosis pathways (Kosten et al. 2008; Zhang et al. 2015; Liu et al. 2016). Accordingly, repeated stress may impair the balance between anti-apoptosis/pro-apoptosis proteins in the hippocampus, as shown by the reduced expression of anti-apoptosis protein B-cell lymphoma 2 (Bcl-2) and increased expression of pro-apoptosis protein Bcl-2-associated death promoter (Bax) (Kosten et al. 2008; Liu et al. 2016). In turn, these events may result in depressive-like behavior since the hippocampus is also responsible for mood modulation (Lee et al. 2002; Watson and Mackin 2006).
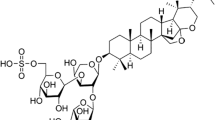
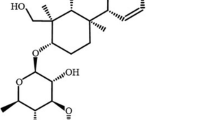
Given this background, compounds with the ability to protect against the deleterious effects of glucocorticoids may exhibit antidepressant-like effects. Importantly, this strategy may be useful since the currently available antidepressants require a long time-lag for eliciting therapeutic effect, have low rates of efficacy, and may produce several side effects including nausea, insomnia, dizziness, weight gain, sexual dysfunction, and sleep disturbances (Crisafulli et al. 2011; Kaster et al. 2016). Within this context, ursolic acid, a natural pentacyclic triterpenoid widely found in plants, is a promising candidate to exert antidepressant effects (Ramos-Hryb et al. 2017a). It has been shown that this triterpenoid has low toxicity in rodents and humans (Zhu et al. 2013; Wang et al. 2013), may cross the blood-brain barrier in rodents (Chen et al. 2011), and exhibits neuroprotective, antioxidant, anti-inflammatory, and anti-apoptotic properties (Shih et al. 2004; Tsai and Yin 2008; Hong et al. 2012; Yoon et al. 2014; Rai et al. 2019). Remarkably, the antidepressant-like effect of ursolic acid in the tail suspension test and forced swim test was reported in previous studies, an effect dependent on the monoaminergic systems (Machado et al. 2012; Colla et al. 2014), and the modulation of protein kinase A (PKA), protein kinase C (PKC), Ca2+/calmodulin-dependent protein kinase II (CAMK-II), and mitogen-activated protein kinase (MAPK) pathway (Ramos-Hryb et al. 2017b). Furthermore, in silico and in vitro studies have revealed that monoamine oxidase-A inhibition and GABA-A receptors modulation may be targets underpinning the antidepressant effect of ursolic acid (Khan et al. 2016; Singla et al. 2017).
More importantly, the protective effect of ursolic acid against corticosterone-induced cytotoxicity in the HT22 mouse hippocampal neuronal cell line was reported to be dependent on the modulation of glucocorticoid receptors and PKA, PKC, and CaMKII (Ramos-Hryb et al. 2019). Furthermore, the ability of ursolic acid to counteract the forskolin-stimulated cortisol release in the H295R human adrenal tumor cell line was shown in a prior report (Richard et al. 2016). These studies raise the speculations about ursolic acid’s ability to modulate glucocorticoid/stress-related disorders, however, the antidepressant-like effect of ursolic acid in a stress-induced animal model remains to be determined. Therefore, this study investigated the possible antidepressant-like effect of ursolic acid in mice subjected to the chronic unpredictable stress protocol, and whether this effect could be associated with the modulation of serum corticosterone levels and Bcl-2/Bax mRNA expression in the hippocampus.
Materials and methods
Animals
The experiments were conducted using male Swiss mice (30–40 g, 45–60 days of age) maintained under controlled temperature (21 ± 1 °C) and humidity (50 ± 20%), with a 12:12 h light/dark cycle (lights on at 7:00 a.m.). Animals were housed in groups of 8 in a cage (41 × 34 × 16 cm) with free access to food and water. The experiments were carried out between 9:00 a.m. and 4:00 p.m., in accordance with the National Institute of Health Guide for the Care and Use of Laboratory Animals. The protocols were approved by the Institutional Ethics Committee. All efforts were done to minimize animal suffering and to reduce their number to the minimum necessary to demonstrate consistent effects in the experiments.
Chronic unpredictable stress model and pharmacological treatments
Chronic unpredictable stress (CUS) protocol consisted of multiple stressors randomly applied at different times of day for 14 days to prevent habituation (Table 1). Mice were divided into control (non-stressed) and CUS (stressed) groups (n = 6–8/group), which were maintained in separate rooms to avoid the interference of stress odors, as previously described (Lu et al. 2006; Moretti et al. 2012). To conduct the protocol, mice were divided into six groups: (1) control + vehicle, (2) control + ursolic acid, (3) control + fluoxetine, (4) CUS + vehicle, (5) CUS + ursolic acid, and (6) CUS + fluoxetine. The following stressors were used in the CUS procedure: restraint, cold swim, wet wood shavings/box housing tilted (45°), cold restraint, tail pinch, forced swim, and inescapable foot shock. The forced swim was carried out by placing the animals in an open cylindrical container (diameter 10 cm, height 25 cm) containing 19 cm of water at 25 ± 1 °C or 15 ± 1 °C. The foot shock was applied in an apparatus consisting of a plastic box (50 × 25 × 25 cm) with a front glass wall and parallel 10-mm bronze bars on the floor. Mice were gently placed on the grid and received a scrambled 0.7-mA, 0.5 s/min foot shock for 3 min. Tail pinch was performed by applying a clothespin placed at 1 cm from the base of the tail. Ursolic acid (0.1 mg/kg, p.o.) and fluoxetine (10 mg/kg, p.o.) were administered in the last 7 days of CUS protocol, i.e. from 8th day to 14th day. Drugs were obtained from Sigma Chemical Co. (St. Louis, USA), freshly prepared before administration and administered orally (p.o.) by gavage in a volume of 10 ml/kg body weight. Ursolic acid was dissolved in distilled water with 2% Tween 80 and fluoxetine diluted in distilled water. On the 15th day, 24 hours after the last administration of the treatments, mice were subjected to the behavioral tests as follows: tail suspension test, open-field test, and splash test, 10 min apart, as previously reported (Neis et al., 2016). The dose of ursolic acid was based in a previous study that investigated the antidepressant-like dose-response of ursolic acid in mice (Machado et al. 2012). The dose of fluoxetine and time points of administration were chosen based on previous studies (Moretti et al. 2012; Colla et al. 2014). After the behavioral tests, mice were deeply anesthetized with isoflurane and immediately euthanized by decapitation, and the serum and hippocampus were collected for biochemical analysis, as shown in Fig. 1.
Schedule of treatments, behavioral tests, and biochemical analyses. Male Swiss mice were subjected to the CUS protocol, which consists of a variety of stressors randomly applied at different times of day for 14 days. Ursolic acid (0.1 mg/kg, p.o.) or fluoxetine (10 mg/kg, p.o.) were administered in the last 7 days of CUS protocol, i.e. from 8th day to 14th day. On the 15th day, 24 hours after the last administration of ursolic acid or fluoxetine, mice were subjected to the tail suspension test, open-field test, and splash test, 10 min apart. After the behavioral tests, mice were immediately euthanized by decapitation and the serum and hippocampus were collected
Tail suspension test
The tail suspension test is one of the most widely used tests for assessing antidepressant-like activity in mice. The total immobility time of mice suspended by the tail was measured as previously proposed (Steru et al. 1985). Briefly, visually isolated mice were suspended 50 cm above the floor by adhesive tape placed approximately 1 cm from the tip of the tail. Immobility time was recorded during a 6-min period by an experienced observer blinded to the experimental groups. Mice were considered immobile only when they hung passively and completely motionless.
Open-field test
The locomotor activity of mice was assessed in the open-field apparatus, which consists of a wooden box (40 × 60 cm × 50 cm) with the floor divided into 12 equal squares (Rodrigues et al. 1996). At the start of each trial, mice were placed in the left corner of the field and allowed to freely explore the arena. The number of crossings (squares crossed with all paws) and total time in the center zone was registered for 6 min. The arena floor was cleaned with 10% ethanol between the tests.
Splash test
The splash test consists of squirting a 10% sucrose solution (w/v) on the dorsal coat of mice placed in a clear box (13 × 20 × 30 cm). Due to its viscosity, the sucrose solution dirties the mice which then initiate grooming behavior. After applying the sucrose, the time spent until the first grooming episode and the total time of grooming were recorded for 5 min, as an index of self-care and motivational behavior, considering any apathetic behavior as symptoms of depression (Willner 2005; Moretti et al. 2012). The apparatus was cleaned with 10% ethanol between tests.
RNA extraction, cDNA synthesis, and RT-qPCR analysis
After the behavioral tests, mice were deeply anesthetized with isoflurane and immediately euthanized by decapitation. Brains were removed, and the hippocampus was rapidly dissected at 4 ºC, placed in liquid nitrogen and stored at − 80 °C until use. Total RNA was extracted using Trizol reagent (Invitrogen, USA) and samples were incubated with DNase I, Amplification Grade (Invitrogen, USA). Complementary DNA synthesized using 0.4 µg of total RNA was reverse transcribed to cDNA using High Capacity cDNA reverse transcription kit (Applied Biosystems, USA). Reaction mix, in a final volume of 20 µl, was incubated at 25 °C for 10 min, at 48 °C for 1 h, and then at 95 °C for 5 min. The obtained cDNA solution was diluted 1:5. Quantitative real-time (qRT-PCR) was performed using 0.3 mM of each primer, 5 µl of Maxima SYBR® Green/ROX qPCR Master Mix 2× (Thermo Fisher Scientific, São Paulo, Brazil) and 2 µl of each diluted cDNA, in a 7900 HT Fast Real-Time PCR System (Thermo Fisher Scientific). Amplification conditions were 50 °C for 2 min, 90 °C for 10 min followed by 40 cycles of 95 °C for 15 s and 60 °C for 1 min. The primers used were designed with Primer Express software version 3.0 (Applied Biosystems, USA) and the sequences are described as follows: Bcl-2 forward (5’-GGTGAACTGGGGGAGGATTGT-3’) and reverse (5’-CTTCAGAGACAGCCAGGAGAA-3’), Bax forward (5’-AGAGGATGATTGCCGCCGT-3’) and reverse (5’-CAACCACCCTGGTCTTGGATC-3’), and β-actin forward (5’-AAATCGTGCGTGACATCAAAGA-3’) and reverse (5’-GCCATCTCCTGCTCGAAGTC-3’). Results were analyzed by the software Sequence Detection Systems (SDS) version 2.4 software (Applied Biosystems, CA, USA). Primers efficiency was tested using the standard curve method. For this purpose, a serial dilution (1:3, 1:7, 1:15, 1:31, 1:63) made from a single cDNA sample consisted of a pool of all cDNAs from the different treatments. Only primers that showed efficiencies between − 2.9 and − 3.3 were used. The specificity of the qPCR products was analyzed by a dissociation curve performed after amplification, observing a single peak at the expected Tm. Furthermore, the stability of the control gene was verified by RefFinder online tool. Results were analyzed by a standard curve-based method in which arbitrary numbers were given for each one of the five points in a logarithmic base 10 scales (Siteneski et al. 2018). Controls were confronted against the curves resulting in the relative value of amplicons. Results were normalized by β-actin values and converted into percentage considering control values as 100%.
Serum corticosterone assay
After mice were deeply anesthetized with isoflurane and immediately euthanized by decapitation, the trunk blood was harvested and serum collected and stored at − 80 °C for corticosterone analysis. The hormone analysis was carried out using a quantitative competitive enzyme immunoassay kit (Corticosterone EIA Kit Assay Designs® Inc., MI, USA) according to the manufacturer’s instructions. Intra-assay measures of variability were 5%. Serum corticosterone concentrations were determined from the standard curve and expressed in nanograms per milliliter.
Statistical analysis
The D’Agostino-Pearson test was used to assess data normality. Differences among experimental groups were determined by one-way or two-way analysis of variance (ANOVA) followed by Newman-Keuls post hoc test, when appropriate. Values of P < 0.05 were considered significant. The results are expressed as means ± standard error of the mean (S.E.M).
Results
Effect of repeated treatment with ursolic acid or fluoxetine in the tail suspension test, open-field test, and splash test
To investigate the antidepressant-like effect of ursolic acid in mice subjected or not to the CUS model, mice were treated for 7 days with ursolic acid (0.1 mg/kg, p.o.) and subjected to the tail suspension, open-field test, and splash test 24 hours after its last administration. Fluoxetine (10 mg/kg, p.o.), a selective serotonin reuptake inhibitor, was used as a positive control to validate the experiments.
Figure 2 shows the influence of CUS protocol and/or the repeated treatment with ursolic acid (0.1 mg/kg, p.o.) or fluoxetine (10 mg/kg, p.o.) on the immobility time in the tail suspension test (panel A), the number of crossings (panel B) and time spent in the center of the open-field apparatus (panel C). Two-way ANOVA revealed significant differences for treatment [F (2, 42) = 73.08, P < 0.01], CUS [F (1, 42) = 12.78, P < 0.01], and treatment × CUS interaction [F (2, 42) = 3.40, P < 0.05]) in the immobility time (panel A). Post-hoc analysis showed that repeated treatment of ursolic acid, similar to fluoxetine, significantly reduced the immobility time when compared to the vehicle-administered control group (P < 0.01), suggesting an antidepressant-like effect. Moreover, CUS protocol significantly induced a depressive-like behavior as observed by the increased immobility time in the tail suspension test (P < 0.01), but this effect was not observed in mice treated with ursolic acid or fluoxetine (P < 0.01). No significant alterations were observed in the number of crossings (panel B) in mice subjected to the open-field test, ruling out the possibility of interference of CUS and/or treatments in the locomotor activity (treatment [F (2, 42) = 0.58, P = 0.57], CUS [F (1, 42) = 4.02, P = 0.06], treatment × CUS interaction [F (2, 42) = 0.97, P = 0.39]). Furthermore, no effects were observed in the time spent in the center of the apparatus (panel C) in mice subjected to the open-field test (treatment [F (2, 42) = 1.15, P = 0.33], CUS [F (1, 42) = 0.54, P = 0.47], treatment × CUS interaction [F (2, 42) = 0.13, P = 0.88]).
Effects of repeated treatment with ursolic acid (UA; 0.1 mg/kg, p.o.) or fluoxetine (FLX; 10 mg/kg p.o.) on the immobility time (a), number of crossings (b), and time in the center of the open-field apparatus (c) in mice subjected or not to CUS protocol. Values are expressed as means ± S.E.M (n = 8). **P < 0.01 as compared with the vehicle-administered control group; ##P < 0.01 as compared with the vehicle-administered CUS group (two-way ANOVA followed by Newman-Keuls post-hoc test)
Figure 3 shows the influence of CUS protocol and/or the repeated treatment with ursolic acid (UA; 0.1 mg/kg, p.o.) or fluoxetine (FLX; 10 mg/kg, p.o.) in the grooming latency (panel A) and time spent grooming (panel B). Two-way ANOVA revealed significant differences for CUS [F (1, 42) = 5.11, P < 0.05] and treatment × CUS interaction [F (2, 42) = 3.48, P < 0.05], but not for treatment [F (2, 42) = 2.44, P = 0.10] in the grooming latency (panel A). Post-hoc analysis showed an increased grooming latency in mice subjected to CUS protocol when compared with their non-stressed counterparts (P < 0.01), and this effect was completely prevented by treatment with ursolic acid or fluoxetine (P < 0.01). Furthermore, two-way ANOVA revealed significant differences for treatment × CUS interaction [F (2, 42) = 4.73, P < 0.05], but not for treatment [F (2, 42) = 0.59, P = 0.56] and CUS [F (1, 42) = 1.77, P = 0.19] in the time spent grooming (panel B). Post-hoc analysis showed that CUS protocol and/or treatments did not alter the time spent grooming in mice subjected to the splash test.
Effects of repeated treatment with ursolic acid (0.1 mg/kg, p.o.) or fluoxetine (10 mg/kg p.o.) on the latency to start the first grooming (a) and total time spent grooming (b) in mice subjected or not to CUS protocol. Values are expressed as means ± S.E.M (n = 8). **P < 0.01 as compared with the vehicle-administered control group; ##P < 0.01 as compared with the vehicle-administered CUS group (two-way ANOVA followed by Newman-Keuls post-hoc test)
Effects of repeated treatment with ursolic acid or fluoxetine on corticosterone levels and Bcl-2/Bax mRNA expression
The effects of CUS protocol and/or treatments with ursolic acid or fluoxetine on serum corticosterone levels and Bcl-2/Bax mRNA expression in the hippocampus were subsequently evaluated. Figure 4 shows the levels of serum corticosterone (panel A) and mRNA expression of Bcl-2 (Panel B), Bax (panel C), and Bcl-2/Bax ratio (Panel D) in the hippocampus of mice subjected to CUS protocol and/or repeated administration of ursolic acid (0.1 mg/kg, p.o.) or fluoxetine (10 mg/kg, p.o.). Two-way ANOVA revealed no significant differences for treatment [F (2, 30) = 2.70, P = 0.08], CUS [F (1, 30) = 0.06, P = 0.82], and treatment × CUS interaction [F (2, 30) = 0.18, P = 0.83] in the levels of serum corticosterone (panel A). Likewise, two-way ANOVA revealed no significant differences for treatment [F (2, 30) = 1.11, P = 0.36], CUS [F (1, 30) = 0.89, P = 0.36], and treatment × CUS interaction [F (2, 30) = 0.60, P = 0.56] in the Bcl-2 mRNA expression (panel B). However, two-way ANOVA indicated significant differences for treatment [F (2, 30) = 4.82, P < 0.05], CUS [F (1, 30) = 5.05, P < 0.05], and treatment × CUS interaction [F (2, 30) = 4.82, P < 0.05] in the Bax mRNA expression (panel C). Post-hoc analysis showed that the CUS protocol significantly increased the Bax mRNA expression in the hippocampus when compared with the vehicle-administered control group (P < 0.05). However, this alteration was significantly prevented by the repeated treatment with ursolic acid (P < 0.01), but not with fluoxetine. Furthermore, concerning the Bcl-2/Bax mRNA expression ratio in the hippocampus, two-way ANOVA indicated significant differences for treatment [F (2, 30) = 60.56, P < 0.01], CUS [F (1, 30) = 37.87, P < 0.01], and treatment × CUS interaction [F (2, 30) = 70.55, P < 0.01]. Post-hoc analysis showed that CUS protocol significantly decreased the mRNA expression ratio of Bcl-2/Bax in the hippocampus when compared with the vehicle-administered control group (P < 0.01), but this alteration was completely prevented by the repeated treatment with ursolic acid or fluoxetine (P < 0.01).
Effects of repeated treatment with ursolic acid (UA; 0.1 mg/kg, p.o.) or fluoxetine (FLX; 10 mg/kg p.o.) on corticosterone levels in the serum (a) and mRNA expression of Bcl-2 (b), Bax (c), and Bcl-2/Bax ratio (d) in the hippocampus of mice subjected or not to CUS protocol. Values are expressed as means ± S.E.M (n = 6). *P < 0.05 and **P < 0.01 as compared with the vehicle-administered control group; ##P < 0.01 as compared with the vehicle-administered CUS group (two-way ANOVA followed by Newman-Keuls post-hoc test)
Discussion
In the present study, we showed to our knowledge for the first time that the repeated treatment with a low dose of ursolic acid was effective in eliciting an antidepressant-like effect in a stress-induced model of depression in mice. The impaired mRNA expression of Bax and Bcl-2/Bax ratio in the hippocampus induced by chronic stress was completely prevented by the treatment with ursolic acid. Noteworthy, the behavioral and neurochemical effects exerted by ursolic acid were similar to those triggered by the conventional antidepressant drug fluoxetine.
The beneficial effects of ursolic acid for the management of psychiatric disorders have been described (Ramos-Hryb et al. 2017a). Here, in the first set of results, we demonstrated that repeated treatment with ursolic acid (0.1 mg/kg, p.o.) for 7 days, similar to fluoxetine (10 mg/kg, p.o.), significantly reduced the immobility time (a despair-like behavior marker) in non-stressed mice subjected to the tail suspension test, a predictive behavioral test widely used to screen antidepressant-like efficacy of compounds. Our results are supported by previous evidence showing the ability of ursolic acid administered acutely to exert an antidepressant-like effect in the tail suspension test and forced swim test in naïve mice (Machado et al. 2012; Colla et al. 2014; Khan et al. 2016; Ramos-Hryb et al. 2017b). In search of the mechanisms underlying the antidepressant effect of ursolic acid, compelling studies have postulated that this triterpenoid could act similarly to the conventional antidepressants (Machado et al. 2012; Colla et al. 2014; Khan et al. 2016; Ramos-Hryb et al. 2017b; Singla et al. 2017). In silico and in vitro studies have revealed that monoamine oxidase-A inhibition and GABA-A receptors modulation may be targets underpinning the antidepressant effect of ursolic acid (Khan et al. 2016; Singla et al. 2017). In vivo studies have shown that the monoaminergic systems are implicated in the antidepressant-like effect of ursolic acid (Machado et al. 2012; Colla et al. 2014). Particularly, the antidepressant-like effect of acute administration of ursolic acid in the tail suspension test was mediated by the modulation of dopamine D1 and D2 receptors (Machado et al. 2012). Reinforcing these results, a sub-effective dose of ursolic acid in combination with sub-effective doses of bupropion, a dual dopamine/noradrenaline reuptake inhibitor, exerted an antidepressant-like effect in the tail suspension test (Machado et al. 2012). Moreover, the combined administration of sub-effective doses of ursolic acid and fluoxetine or reboxetine, selective serotonin/noradrenaline reuptake inhibitors, respectively, elicited an antidepressant-like effect in the tail suspension test (Colla et al. 2014). Additionally, acute administration of ursolic acid elicited an antidepressant-like effect in the tail suspension test through the modulation of PKA, PKC, CAMK-II, and MAPK pathway (Ramos-Hryb et al. 2017b). However, it remained to be determined whether ursolic acid is effective to exert an antidepressant-like effect in a model of depression induced by stress.
A growing body of consistent evidence has demonstrated that CUS protocol is capable of mimicking the behavioral and neurochemical alterations observed in patients with MDD (Li et al. 2011; Moretti et al. 2012; Zhang et al. 2015; Gawali et al. 2017). This model has a predictive, face, and construct validity, which makes it a useful tool to study the mechanisms underlying the neurobiology of MDD (Planchez et al. 2019). Notably, CUS-induced alterations are completely prevented or counteracted by conventional antidepressant drugs (Manosso et al. 2016; Liu et al. 2017; Gawali et al. 2017; Zhang et al. 2019) and fast-acting antidepressant agents (Li et al. 2011; Neis et al. 2016). Here, we demonstrated that CUS protocol consistently induced a depressive-like behavior, as demonstrated by an increase in the immobility time and latency to first grooming (a self-care marker) in the tail suspension test and splash test, respectively, without affecting locomotor activity in the open-field test. These results are in agreement with previous studies that used the CUS protocol to induce depressive-like behavior in mice (Moretti et al. 2012; Kaster et al. 2015; Liu et al. 2017). However, no effect was observed in the total time of grooming (an anhedonic-like behavior marker) and time in the center of the open-field apparatus (an anxious-like behavioral marker). Conversely, the repeated treatment of ursolic acid (0.1 mg/kg, p.o.), similar to fluoxetine (10 mg/kg, p.o.), completely prevented the increased immobility time and grooming latency induced by CUS protocol, suggesting an antidepressant-like effect of this compound. Supporting these results, ursolic acid was reported to be effective to protect the HT22 cell line against corticosterone-induced cytotoxicity by modulating glucocorticoid receptors and PKA, PKC, and CaMKII (Ramos-Hryb et al. 2019). In addition, the results triggered by fluoxetine in mice subjected to CUS protocol are in consonance with previous studies (Moretti et al. 2012; Manosso et al. 2016; Liu et al. 2017; Shen et al., 2019).
In the next step of the study, we decided to shed light on the possible mechanisms associated with the antidepressant-like effect of ursolic acid. Of special interest, we investigated whether the modulation of serum corticosterone levels and the expression of pro/anti-apoptosis proteins in the hippocampus could be associated with the antidepressant-like effect of ursolic acid. Particularly, high levels of corticosterone induced by chronic stress may cause neural cell death in the hippocampus, which in turn amplifies the HPA axis dysfunction since under normal conditions this brain region regulates the HPA axis negative feedback mechanism (Lee et al. 2002; Mizoguchi et al. 2003). Additionally, it is thought that stimulation of pro-apoptotic pathways induced by corticosterone is one of the mechanisms underlying the cell death and consequently the atrophy in the hippocampus (Liu et al. 2011; Latt et al. 2018). Noteworthy, previous studies reported that hippocampal atrophy and neuronal apoptosis exist in patients with MDD (Sheline et al. 1996; Lucassen et al. 2001) and stress-induced animal models (Kosten et al. 2008; Liu et al. 2016; Shen et al. 2019). However, in the present study, CUS protocol and/or treatment with ursolic acid or fluoxetine did not alter the levels of serum corticosterone in mice. This result agrees with previous studies that also used similar protocols of chronic stress (Noschang et al. 2009; Moretti et al. 2012). Indeed, alterations on the serum corticosterone levels have been reported in rodents subjected to longer protocols of chronic stress (Garcia et al. 2009; Jindal et al. 2013). Therefore, one may suppose that a longer period of CUS protocol could be necessary to induce alterations on serum corticosterone levels. However, we cannot rule out that CUS protocol could have affected the corticosterone levels and glucocorticoids receptors expression in the hippocampus or other brain regions involved with mood modulation (prefrontal cortex), which express a high density of glucocorticoid receptors and are involved with HPA axis regulation (Lee et al. 2002; McKlveen et al. 2013). Furthermore, although we did not find any alteration on serum corticosterone levels in any experimental group, it cannot be ruled out the possibility that ursolic acid may exert a modulatory effect on corticosterone levels in mice submitted to other stress protocols. The ability of this triterpenoid to counteract the forskolin-stimulated cortisol (functional role equivalent to corticosterone) release in the H295R human adrenal tumor cell line was previously shown (Richard et al. 2016).
Next, we investigated the effects of CUS and/or treatments in the expression of pro/anti-apoptosis markers. Although the CUS protocol did not alter the mRNA expression of Bcl-2 (anti-apoptosis marker) in the hippocampus, it increased the mRNA expression of Bax (pro-apoptosis marker) and decreased the Bcl-2/Bax ratio, suggesting a possible event of apoptosis triggered by stress. Importantly, the balance between Bax and Bcl-2 expression is tightly controlled in the cell, although it may be disrupted in rodents exposed to chronic stress (Gross and Katz 2017). In line with this, some studies have shown alterations in Bcl-2/Bax expression in the hippocampus (Liu et al. 2016; Shen et al. 2019) and prefrontal cortex (Kosten et al. 2008), of rodents subjected to chronic stress. Notably, chronic stress caused a downregulation in the expression of Bcl2 and upregulation in the expression Bax, which partially agrees with our results (Shen et al. 2019). However, it has been shown that chronic stress can selectively decrease the expression of Bcl-2 in the prefrontal cortex, but not in the hippocampus (Kosten et al. 2008). Consistent with the notion that hippocampal apoptosis is implicated in the depressive-like behavior elicited by stress, here we show that the repeated treatment with ursolic acid completely prevented the increased mRNA expression of Bax in the hippocampus induced by CUS protocol. Reinforcing this result, ursolic acid was also capable of preventing the CUS-induced reduction on Bcl-2/Bax ratio, an effect also exerted by fluoxetine. Importantly, the ability of fluoxetine to neutralize the impaired Bax expression induced by stress in the hippocampus was previously reported (Shen et al. 2019). These results suggest that the modulation of Bcl-2/Bax apoptosis-related proteins could be associated with the antidepressant-like effect of ursolic acid in mice subjected to CUS. In support of this assumption, it has been demonstrated that the clinically effective antidepressants duloxetine, mirtazapine, fluoxetine, reboxetine, tranylcypromine, imipramine, as well as the fast-acting antidepressant ketamine, can modulate apoptosis-related pathways, an effect likely associated with their antidepressant-like property (Kosten et al. 2008; Engel et al. 2013; Liu et al. 2016; Lieberknecht et al. 2020). However, although the repeated treatment with ursolic acid was effective to modulate BAX expression and Bcl-2/BAX expression ratio in the hippocampus of CUS-exposed mice, additional experiments using western blotting and immunohistochemistry analyses could be undertaken to ascertain this response. Moreover, further studies targeting other apoptosis-related markers could provide novel insights into the effects elicited by ursolic acid.
In summary, our study unveils the ability of ursolic acid to prevent the depressive-like behavior induced by stress in two distinct behavioral paradigms, the tail suspension test, and the splash test. Furthermore, we provide evidence that ursolic acid abrogated the stress-induced increased expression of Bax and reduced Bcl-2/Bax ratio in the hippocampus, and these effects could be implicated in its antidepressant-like effect. Finally, our study reinforces the notion that ursolic acid, a compound that is reported to be well-tolerated for human use and that has several beneficial effects against brain-related disorders (Zhu et al. 2013; Wang et al. 2013; Ramos-Hryb et al. 2017b) should not be underestimated as a promising antidepressant agent. However, it is important to mention that although ursolic acid was well-tolerated by healthy volunteers and patients with advanced tumors, a few side effects have been reported, particularly at doses 74 and 98 mg/m2, such as nausea, diarrhea, and abdominal distention after a single administration and skin pruritus, arthralgia, and triglyceride elevation after the 14-day continuous infusion (Zhu et al. 2013; Wang et al. 2013). Therefore, we should bear in mind that some caveats need to be considered for the use of ursolic acid in humans. Despite these caveats, the ability of ursolic acid to counteract the stress-induced hippocampal imbalance on apoptosis-related proteins may be of interest for the management of MDD associated with other brain disorders in which hippocampal apoptosis play a crucial role such as neurodegenerative disorders (Ramos-Hryb et al. 2017b).
Data availability
All data generated or analyzed during this study are included in this published article.
References
Anacker C, Zunszain PA, Carvalho LA, Pariante CM (2011) The glucocorticoid receptor: Pivot of depression and of antidepressant treatment? Psychoneuroendocrinology 36:415–425
Chen Q, Luo S, Zhang Y, Chen Z (2011) Development of a liquid chromatography - Mass spectrometry method for the determination of ursolic acid in rat plasma and tissue: Application to the pharmacokinetic and tissue distribution study. Anal Bioanal Chem 399:2877–2884
Colla ARS, Oliveira Á, Pazini FL et al (2014) Serotonergic and noradrenergic systems are implicated in the antidepressant-like effect of ursolic acid in mice. Pharmacol Biochem Behav 124:108–116
Cox BM, Alsawah F, McNeill PC et al (2011) Neurochemical, hormonal, and behavioral effects of chronic unpredictable stress in the rat. Behav Brain Res 220:106–111
Crisafulli C, Fabbri C, Porcelli S et al (2011) Pharmacogenetics of antidepressants. Front Pharmacol FEB:1–21
Engel D, Zomkowski ADE, Lieberknecht V et al (2013) Chronic administration of duloxetine and mirtazapine downregulates proapoptotic proteins and upregulates neurotrophin gene expression in the hippocampus and cerebral cortex of mice. J Psychiatr Res 47:802–808
Garcia LSB, Comim CM, Valvassori SS et al (2009) Ketamine treatment reverses behavioral and physiological alterations induced by chronic mild stress in rats. Prog Neuropsychopharmacol Biol Psychiatry 33:450–455
Gawali NB, Bulani VD, Gursahani MS et al (2017) Agmatine attenuates chronic unpredictable mild stress-induced anxiety, depression-like behaviours and cognitive impairment by modulating nitrergic signalling pathway. Brain Res 1663:66–77
Goodyer IM, Herbert J, Tamplin A, Altham PME (2000) Recent life events, cortisol, dehydroepiandrosterone and the onset of major depression in high-risk adolescents. Br J Psychiatry 177:499–504
Gross A, Katz SG (2017) Non-apoptotic functions of BCL-2 family proteins. Cell Death Differ 24:1348–1358
Hong SY, Jeong WS, Jun M (2012) Protective effects of the key compounds isolated from Corni fructus against β-amyloid-induced neurotoxicity in pc12 cells. Molecules 17:10831–10845
Jindal A, Mahesh R, Bhatt S (2013) Etazolate rescues behavioral deficits in chronic unpredictable mild stress model: Modulation of hypothalamic-pituitary-adrenal axis activity and brain-derived neurotrophic factor level. Neurochem Int 63:465–475
Richard EJ, Illuri R, Bethapudi B et al (2016) Anti-stress activity of Ocimum sanctum: Possible effects on hypothalamic-pituitary-adrenal axis. Phyther Res 30:805–814
Kaster MP, Machado NJ, Silva HB et al (2015) Caffeine acts through neuronal adenosine A2A receptors to prevent mood and memory dysfunction triggered by chronic stress. Proc Natl Acad Sci U S A 112:7833–7838
Kaster MP, Moretti M, Cunha MP, Rodrigues ALS (2016) Novel approaches for the management of depressive disorders. Eur J Pharmacol 771:236–240
Khan I, Karim N, Ahmad W et al (2016) GABA-A receptor modulation and anticonvulsant, anxiolytic, and antidepressant activities of constituents from Artemisia indica Linn. Evid Based Complement Alternat Med 2016:1215393
Kosten TA, Galloway MP, Duman RS et al (2008) Repeated unpredictable stress and antidepressants differentially regulate expression of the Bcl-2 family of apoptotic genes in rat cortical, hippocampal, and limbic brain structures. Neuropsychopharmacology 33:1545–1558
Latt HM, Matsushita H, Morino M et al (2018) Oxytocin inhibits corticosterone-induced apoptosis in primary hippocampal neurons. Neuroscience 379:383–389
Lee AL, Ogle WO, Sapolsky RM (2002) Stress and depression: Possible links to neuron death in the hippocampus. Bipolar Disord 4:117–128
Li N, Liu RJ, Dwyer JM et al (2011) Glutamate N-methyl-D-aspartate receptor antagonists rapidly reverse behavioral and synaptic deficits caused by chronic stress exposure. Biol Psychiatry 69:754–761
Lieberknecht V, Engel D, Rodrigues ALS, Gabilan NH (2020) Neuroprotective effects of mirtazapine and imipramine and their effect in pro- and anti-apoptotic gene expression in human neuroblastoma cells. Pharmacol Rep 72:563–570
Liu B, Zhang H, Xu C et al (2011) Neuroprotective effects of icariin on corticosterone-induced apoptosis in primary cultured rat hippocampal neurons. Brain Res 1375:59–67
Liu WX, Wang J, Xie ZM et al (2016) Regulation of glutamate transporter 1 via BDNF-TrkB signaling plays a role in the anti-apoptotic and antidepressant effects of ketamine in chronic unpredictable stress model of depression. Psychopharmacology 233:405–415
Liu Y-M, Shen J-D, Xu L-P et al (2017) Ferulic acid inhibits neuro-inflammation in mice exposed to chronic unpredictable mild stress. Int Immunopharmacol 45:128–134
Lu XY, Kim CS, Fraser A, Zhang W (2006) Leptin: A potential novel antidepressant. Proc Natl Acad Sci U S A 103:1593–1598
Lucassen PJ, Müller MB, Holsboer F et al (2001) Hippocampal apoptosis in major depression is a minor event and absent from subareas at risk for glucocorticoid overexposure. Am J Pathol 158:453–468
Machado DG, Neis VB, Balen GO et al (2012) Antidepressant-like effect of ursolic acid isolated from Rosmarinus officinalis L. in mice: Evidence for the involvement of the dopaminergic system. Pharmacol Biochem Behav 103:204–211
Manosso LM, Moretti M, Colla AR et al (2016) Involvement of glutamatergic neurotransmission in the antidepressant-like effect of zinc in the chronic unpredictable stress model of depression. J Neural Transm 123:339–352
McKlveen JM, Myers B, Flak JN et al (2013) Role of prefrontal cortex glucocorticoid receptors in stress and emotion. Biol Psychiatry 74:672–679
Mizoguchi K, Ishige A, Aburada M, Tabira T (2003) Chronic stress attenuates glucocorticoid negative feedback: Involvement of the prefrontal cortex and hippocampus. Neuroscience 119:887–897
Moretti M, Colla A, De Oliveira Balen G et al (2012) Ascorbic acid treatment, similarly to fluoxetine, reverses depressive-like behavior and brain oxidative damage induced by chronic unpredictable stress. J Psychiatr Res 46:331–340
Neis VB, Bettio LEB, Moretti M et al (2016) Acute agmatine administration, similar to ketamine, reverses depressive-like behavior induced by chronic unpredictable stress in mice. Pharmacol Biochem Behav 150–151:108–114
Noschang CG, Pettenuzzo LF, von Pozzer Toigo E et al (2009) Sex-specific differences on caffeine consumption and chronic stress-induced anxiety-like behavior and DNA breaks in the hippocampus. Pharmacol Biochem Behav 94:63–69
Otte C, Gold SM, Penninx BW et al (2016) Major depressive disorder. Nat Rev Dis Primers 2:1–21
Pariante CM, Lightman SL (2008) The HPA axis in major depression: classical theories and new developments. Trends Neurosci 31:464–468
Planchez B, Surget A, Belzung C (2019) Animal models of major depression: drawbacks and challenges. J Neural Transm 126:1383–1408
Rai SN, Zahra W, Singh S, Sen et al (2019) Anti-inflammatory activity of ursolic acid in MPTP-induced parkinsonian mouse model. Neurotox Res 36:452–462
Ramos-Hryb AB, Pazini FL, Kaster MP, Rodrigues ALS (2017a) Therapeutic potential of ursolic acid to manage neurodegenerative and psychiatric diseases. CNS Drugs 31:1029–1041
Ramos-Hryb AB, Cunha MP, Pazini FL et al (2017b) Ursolic acid affords antidepressant-like effects in mice through the activation of PKA, PKC, CAMK-II and MEK1/2. Pharmacol Rep 69:1240–1246
Ramos-Hryb AB, Platt N, Freitas AE et al (2019) Protective effects of ursolic acid against cytotoxicity induced by corticosterone: role of protein kinases. Neurochem Res 44:2843–2855
Rodrigues ALS, Rocha JBT, Mello CF, Souza DO (1996) Effect of perinatal lead exposure on rat behaviour in open-field and two-way avoidance tasks. Pharmacol Toxicol 79:150–156
Sheline YI, Wang PW, Gado MH et al (1996) Hippocampal atrophy in recurrent major depression. Proc Natl Acad Sci U S A 93:3908–3913
Shen J, Qu C, Xu L et al (2019) Resveratrol exerts a protective effect in chronic unpredictable mild stress–induced depressive-like behavior: involvement of the AKT/GSK3β signaling pathway in hippocampus. Psychopharmacology 236:591–602
Shih YH, Chein YC, Wang JY, Fu YS (2004) Ursolic acid protects hippocampal neurons against kainate-induced excitotoxicity in rats. Neurosci Lett 362:136–140
Singla RK, Scotti L, Dubey AK (2017) In Silico studies revealed multiple neurological targets for the antidepressant molecule ursolic acid. Curr Neuropharmacol 15:1100–1106
Siteneski A, Cunha MP, Lieberknecht V et al (2018) Central irisin administration affords antidepressant-like effect and modulates neuroplasticity-related genes in the hippocampus and prefrontal cortex of mice. Prog Neuropsychopharmacol Biol Psychiatry 84:294–303
Steru L, Chermat R, Thierry B, Simon P (1985) The tail suspension test: A new method for screening antidepressants in mice. Psychopharmacology 85:367–370
Tsai SJ, Yin MC (2008) Antioxidative and anti-inflammatory protection of oleanolic acid and ursolic acid in PC12 cells. J Food Sci 73:174–178
Wang XH, Zhou SY, Qian ZZ et al (2013) Evaluation of toxicity and single-dose pharmacokinetics of intravenous ursolic acid liposomes in healthy adult volunteers and patients with advanced solid tumors. Expert Opin Drug Metab Toxicol 9:117–125
Watson S, Mackin P (2006) HPA axis function in mood disorders. Psychiatry 5:166–170
Willner P (2005) Chronic mild stress (CMS) revisited: Consistency and behavioural- neurobiological concordance in the effects of CMS. Neuropsychobiology 52:90–110
World Health Organization (2017) Depression and other common mental disorders: global health estimates. World Health Organization, Geneva, pp 1–24
Yoon JH, Youn K, Ho CT et al (2014) P-coumaric acid and ursolic acid from corni fructus attenuated β-amyloid25 – 35-induced toxicity through regulation of the NF-κB signaling pathway in PC12 cells. J Agric Food Chem 62:4911–4916
Zhang Y, Liu L, Liu Y-Z et al (2015) NLRP3 inflammasome mediates chronic mild stress-induced depression in mice via neuroinflammation. Int J Neuropsychopharmacol 18:1–8
Zhang YQ, Wang XB, Xue RR et al (2019) Ginsenoside Rg1 attenuates chronic unpredictable mild stress-induced depressive-like effect via regulating NF-κB/NLRP3 pathway in rats. Neuroreport 30:893–900
Zhu Z, Qian Z, Yan Z et al (2013) A phase I pharmacokinetic study of ursolic acid nanoliposomes in healthy volunteers and patients with advanced solid tumors. Int J Nanomedicine 8:129–136
Acknowledgements
The authors thank funding agencies CNPq and CAPES by the financial support, and the Laboratório Multiusuário de Estudos em Biologia (LAMEB) by technical support.
Funding
This study was supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq, #310113/2017-2 and #150082/2018-5), and Coordenação de Aperfeiçoamento de Pessoal de Ensino Superior (CAPES). ALSR is a CNPq Research Fellow.
Author information
Authors and Affiliations
Contributions
Ana Lúcia S. Rodrigues and André R.S. Colla designed the study and wrote the protocol. André R.S. Colla, Francis L. Pazini, Vicente Lieberknecht, and Anderson Camargo performed the behavioral and biochemical tests and undertook the statistical analysis. All authors wrote the first draft of the manuscript, as well as approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
All procedures were carried out in accordance with the National Institute of Health Guide for the Care and Use of Laboratory Animals and the protocols were approved by the Institutional Ethics Committee.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Colla, A.R.S., Pazini, F.L., Lieberknecht, V. et al. Ursolic acid abrogates depressive-like behavior and hippocampal pro-apoptotic imbalance induced by chronic unpredictable stress. Metab Brain Dis 36, 437–446 (2021). https://doi.org/10.1007/s11011-020-00658-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-020-00658-4