Abstract
Minimal hepatic encephalopathy is the term applied to the neuropsychiatric status of patients with cirrhosis who are unimpaired on clinical examination but show alterations in neuropsychological tests exploring psychomotor speed/executive function and/or in neurophysiological variables. There is no gold standard for the diagnosis of this syndrome. As these patients have, by definition, no recognizable clinical features of brain dysfunction, the primary prerequisite for the diagnosis is careful exclusion of clinical symptoms and signs. A large number of psychometric tests/test systems have been evaluated in this patient group. Of these the best known and validated is the Portal Systemic Hepatic Encephalopathy Score (PHES) derived from a test battery of five paper and pencil tests; normative reference data are available in several countries. The electroencephalogram (EEG) has been used to diagnose hepatic encephalopathy since the 1950s but, once popular, the technology is not as accessible now as it once was. The performance characteristics of the EEG are critically dependent on the type of analysis undertaken; spectral analysis has better performance characteristics than visual analysis; evolving analytical techniques may provide better diagnostic information while the advent of portable wireless headsets may facilitate more widespread use. A large number of other diagnostic tools have been validated for the diagnosis of minimal hepatic encephalopathy including Critical Flicker Frequency, the Inhibitory Control Test, the Stroop test, the Scan package and the Continuous Reaction Time; each has its pros and cons; strengths and weaknesses; protagonists and detractors. Recent AASLD/EASL Practice Guidelines suggest that the diagnosis of minimal hepatic encephalopathy should be based on the PHES test together with one of the validated alternative techniques or the EEG. Minimal hepatic encephalopathy has a detrimental effect on the well-being of patients and their care-givers. It responds well to treatment with resolution of test abnormalities and the associated detrimental effects on quality of life, liver-related mortality and morbidity. Patients will only benefit in this way if they can be effectively diagnosed. Corporate efforts and consensus agreements are needed to develop effective diagnostic algorithms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Definitions and diagnosis
The working party on hepatic encephalopathy, which reported in 2002 (Ferenci et al. 2002), did not provide a definition of minimal hepatic encephalopathy although it recognised that, at a semantic level, the term was applied to a population of individuals with cirrhosis who performed abnormally on psychometric tests but presented as essentially normal on clinical examination (Gitlin et al. 1986). They accepted that these individuals might also have abnormal neurophysiological test results but considered these to be non-specific and did not evaluate other proposed diagnostic tools, for example, the Sternberg test, as few, if any, published data were available for review. This working party made the obvious, but very important statement, that in the absence of a diagnostic ‘gold standard’ the validation of any proposed tests/test systems for the diagnosis of minimal hepatic encephalopathy would present major difficulties. In consequence, they called for a large study to redefine the neuropsychiatric abnormalities in people with liver disease, which would allow the diagnosis of minimal hepatic encephalopathy to be made on firm statistical grounds (Ferenci et al. 2002). As an interim measure they suggested that the diagnosis should be based on the results of at least two of four recommended psychometric tests viz. Number Connection Tests (NCT) A and B (Reitan 1955), and/or the Block Design and Digit Symbol subtests of the Wechsler Adult Intelligence Scales–Revised (Wechsler 1981); they also recommended use of the Psychometric Hepatic Encephalopathy Score (PHES), which derives from five tests viz.: NCT A and B, the Digit Symbol, Line Tracing and Serial Dotting tests (Weissenborn et al. 2001). They also stipulated that, where possible, quantitative neurophysiological variables such as the electroencephalogram (EEG) mean dominant frequency (MDF) and the P300 of the cognitive auditory evoked potential should be added.
The 2014 Practice Guideline on Hepatic Encephalopathy, published jointly by the American and European Associations for the Study of the Liver (AASLD/EASL) (Vilstrup et al. 2014), describes minimal hepatic encephalopathy as a condition where there is – psychometric or neuropsychological alterations of tests exploring psychomotor speed/executive functions or neurophysiological alterations without clinical evidence of mental change. The Guideline Development Group (GDG) suggested that the operative criterion should be ‘abnormal results of established psychometric or neuropsychological tests without clinical manifestations’. However, the advice they provide about screening for minimal hepatic encephalopathy is unclear. While conceding that testing for minimal hepatic encephalopathy is important and that ideally all patients at risk should be tested, the GDG expressed concern that this could prove costly and that difficulties could arise once patients were diagnosed because there is no clear management strategy particularly in relation to treatment. Thus, they suggest that testing should be reserved for those with impaired quality of life or in whom there are ‘complaints’— not specified— from the patient or their relatives. This later statement conflicts, however, with their statement that use of the term ‘minimal’ conveys that there are no clinical manifestations of hepatic encephalopathy.
The 2014 Practice GDG reviewed a number of possible diagnostic tests/test systems and conceded that there are no universal diagnostic criteria and that local standards and expertise are required. Nevertheless, they recommend that in multicentre studies the diagnosis of minimal hepatic encephalopathy should be based on at least two of the current validated testing strategies viz: the PHES test battery (Weissenborn et al. 2001) and either one of the computerised test systems e.g. Continuous Reaction Time (CRT) test, Inhibitory Control Test (ICT), Stroop or Scan tests OR a neurophysiological variable, for example, the EEG MDF or Critical Flicker Frequency (CFF). They recommend that in routine clinical practice or in single-centre studies clinicians/investigators should use tests they are familiar with/have access to, provided that adequate, local, normative data are available (Bajaj et al. 2011a).
This review aims to further qualify and quantify minimal hepatic encephalopathy bearing in mind the current guidelines but not constrained by them.
The diagnosis of minimal hepatic encephalopathy
As patients with minimal hepatic encephalopathy, by definition, have no recognizable clinical features of brain dysfunction, the primary prerequisite for the diagnosis is the careful exclusion of clinical symptoms and signs.
Clinical examination
The exclusion of overt, or clinically apparent, hepatic encephalopathy should be based on a careful and detailed neuropsychiatric history and examination (Montagnese et al. 2004) with particular attention paid to changes in memory, concentration and other aspects of cognition, and consciousness. A comprehensive neurological examination is mandatory looking particularly for evidence of subtle motor abnormalities. Other potential causes of neuropsychiatric abnormalities, for example, concomitant neurological disorders such as subdural haematoma, Wernicke’s encephalopathy or vascular dementia, and other metabolic abnormalities such as those associated with diabetes, renal failure, and drug or alcohol intoxication, must be ruled out.
Psychometric testing
A large number of psychometric tests have been utilized to assess cognitive function in patients with cirrhosis. Overall the domains most affected are those concerned with: (i) speed and accuracy in selection processes, particularly involving spatial conflicts or perceptual-semantic conflicts; (ii) inhibition; and, (iii) working memory. Simple reaction times or long-term verbal memory tasks are much less affected (Amodio et al. 2010; Bajaj et al. 2008). In tests of psychomotor speed alterations in selection processing occur before alteration in motor response (Schiff et al. 2005).
Test systems and assessed domains
None of the psychometric tests utilized for the diagnosis of this condition is specific. The test systems that access the key domains of attention and psychomotor speed are likely to have the best diagnostic performance. The PHES test battery (Schomerus et al. 1999) of five paper and pencil tests assesses motor speed and accuracy, visual perception, visuo-spatial orientation, visual construction, concentration, attention and, to a lesser extent, memory; it has a reported sensitivity of 96 % and specificity of 100 % for the diagnosis of Grade 1 hepatic encephalopathy (Schomerus and Hamster 1998; Weissenborn et al. 2001). The test-retest reliability exceeds 0.81 (Schomerus et al. 1999) and there is no significant learning effect if all four parallel versions of the test are used (Goldbecker et al. 2013). The PHES test battery is currently recommended as the ‘gold standard’ for the diagnosis of minimal hepatic encephalopathy (Ferenci et al. 2002; Randolph et al. 2009; Vilstrup et al. 2014), although the term ‘best clinical standard’ is probably more appropriate.
Computerized psychometric test batteries are being used increasingly in clinical medicine primarily because they are convenient, afford greater control over task stimuli, allow presentation to be standardized and data capture to be automated; as such they minimize inter-observer variance both in application and scoring. There is some evidence to support their use for the diagnosis of minimal hepatic encephalopathy but validation invariably relies on comparison with PHES test performance.
A test battery developed by Cognitive Drug Research (CDR) System Ltd. (Goring–on–Thames, United Kingdom) has been used extensively for the assessment of cognitive function in clinical trials and shows good test-retest reliability. Significant concordance was found between the results of the CDR and the PHES test in patients with minimal hepatic encephalopathy; in this context the sensitivity and specificity of the CDR, using the PHES test results as the comparator, were 86 % and 81 % respectively (Mardini et al. 2008). German control norms were used to score the PHES test results in this study; use of UK norms might have affected the diagnostic performance of the CDR battery. No further evaluations are available.
The Vienna Test System (VTS) (Dr Schuhfried Inc., Mödling, Austria) comprises a large number of computerized tests covering the entire range of psychological assessment (Vienna Test System 1999). The modular design of the VTS allows individual psychological tests to be combined to provide specific test batteries. Five of these tests, which between them provide 22 parameters designed to evaluate attention, concentration, visual perception and fine motor abilities, were used to assess neuropsychometric performance in patients with cirrhosis (Kircheis et al. 2002). The results of the VTS evaluation were used to grade neuropsychometric status in patients with cirrhosis in order to evaluate another test system; the presence of two or more abnormal tests was considered diagnostic for minimal hepatic encephalopathy in the absence of clinical symptoms and signs (Kircheis et al. 2002). The proportion of patients with abnormal VTS test results was considerably higher than the proportion with abnormal PHES test results but there was no head to head comparison of the results of the two systems. The interpretation of the results of this study have been criticized because the five VTS variables were considered abnormal if any one of the subtests was outside 1 standard deviation (SD) of the mean of the reference population rather than the 2SD criterion usually applied when evaluating psychometric test performance; this choice of cut-off might produce an unacceptably high false positive rate (Weissenborn 2015b). Use of the 1SD cut-off has been vigorously defended by the original workers who have continued to use the VTS system to evaluate several aspects of cerebral function in patients with minimal hepatic encephalopathy (Kircheis et al. 2014; Miese et al. 2006; Shah et al. 2008; Timmermann et al. 2008). They do concede, however, that use of the VTS battery is very time consuming and that it is not suitable for the routine evaluation of patients with cirrhosis in the clinical setting.
The Cogstate Research™ test battery includes four core cognitive domains viz: processing speed, attention, visual learning and working memory; and is customizable. The tests are the briefest available and the outcome measures and data are rapidly available for review via a secure web-based portal. The test-retest reliability is high. Preliminary results, in a small group of patients with cirrhosis, using accuracy of test performance and speed of completion as primary variables, found strong correlations between the International Shopping list tasks of the Cogstate Research™ test battery and the Digit Symbol test of the PHES battery. Further the results suggested that the Serial Dotting test of the PHES battery might not be discriminatory and that its replacement by the shopping list tasks of the Cogstate Research™ battery might enhance the diagnostic utility of the PHES (Cook et al. 2015, personal communication). However, if the PHES were to be modified in this way it would need to be revalidated.
Further evaluation and validation of these and other computer-based psychometric systems are needed.
Requirements for normative reference data
Psychometric test results can be influenced by a variety of factors including: innate intelligence, age, sex, education, ethnicity and even occupation. The effects differ from test to test on an individual basis. Thus, one of the key requisites for psychometric testing is the availability of adequate normative reference data.
Age is one of the most important confounders but the relationship between age and test performance may vary between tests (Figs. 1 and 2). The effects of innate intelligence and education vary depending on the difficulty of the task. Thus, the level of education has a small and generally negligible effect on performance of the NCT A but has an important effect on the performance of the STROOP test (Van der Elst et al. 2006; Weissenborn et al. 2001) (Fig. 2). The effects of gender have generally been less well studied but normative data obtained in a Dutch population showed that women outperformed men in the STROOP test over the entire age range, irrespective of the level of education (Van der Elst et al. 2006).
Correlation between age and the STROOP test error score, by level of education. Age dependence in the STROOP test results in young adults is minimal, but there is a steep relationship between age and STROOP Interference Score or Error Score in subjects over the age of 45 years (adapted after Van der Elst et al. 2006)
Ethnicity also impacts on psychometric test performance. Thus, significant differences have been observed between African Americans and Caucasians in several tests of attention and memory independent of age and level of education (Norman et al. 2011). Finally, long-life mental training and daily engagement in cognitively demanding activities can influence psychometric performance, probably reflecting the so-called cognitive reserve (Cona et al. 2014). This term refers to the functional/structural effects of training on the brain. Thus, individuals with well-developed pre-morbid skills maintain task performance related to these specific skills, despite objective decline in other dimensions of brain function (Montagnese et al. 2010).
The acquisition of normative reference data for psychometric tests is a difficult task as these must be validated on at least a national basis and regularly re-evaluated as changes in educational and life-style variables may impact on normative performance over time. This is particularly important as population mobility increases, as this can substantially change the ethnic mix of populations, particularly in large urban conurbations.
The PHES test was developed and standardized in Germany and was originally applied elsewhere using the German normative data. This was not ideal as thresholds which apply in one population do not necessarily apply in others (Amodio et al. 1996). However, normative reference data are now available in Italy (Amodio et al. 2008); Spain (Romero Gómez et al. 2006); the United Kingdom (Marks et al. 2008); Poland (Wunsch et al. 2013); South Korea (Seo et al. 2012); and Mexico (Duarte-Rojo et al. 2011); in addition, the PHES battery has been adapted and validated for use in India by replacing the Number Connection Test B with Figure Connection Test A to overcome possible unfamiliarity with the English alphabet (Kurmi et al. 2008).
The 2002 and 2014 guidelines stipulate that psychometric testing should be undertaken by trained examiners and emphasize that it is essential to administer and score tests as specified in the test manuals; deviations could invalidate the results. In addition, the normative reference data are valid only for the test version from which they were derived. Thus, any modification of the original test battery will require further validation. Riggio et al. (2011), showed that the PHES test battery could be shortened without loss of efficacy. Backward, logistic regression identified a shortened test comprising the Digit Symbol, Serial Dotting and Line Tracing tests, which was defined using the regression coefficients and the Z scores of the three selected tests. Exclusion of the remaining two tests did not significantly affect overall performance either in terms of the diagnosis of minimal hepatic encephalopathy or predicting the subsequent development of overt hepatic encephalopathy. However, a more recent attempt to shorten the PHES battery by removal of the Serial Dotting test (Kircheis et al. 2014) has been criticized because the cut-off between normal and abnormal test results, on the modified PHES battery, was based on the threshold which differentiated unimpaired patients from those with minimal hepatic encephalopathy using an independent psychometric test system rather than normative data from healthy controls (Weissenborn et al. 2015).
Co-morbid/co-occurring conditions confound psychometric test results
Chronic HCV infection and alcohol misuse, two of the most prevalent causes of cirrhosis, can affect cognition irrespective of the development of significant liver disease (Campagna et al. 2015). Anxiety, depression and impairment of health-related quality of life are common amongst people with cirrhosis and can significantly affect psychometric performance (Nardelli et al. 2013).
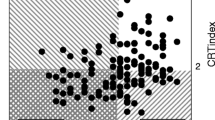
The attention deficits and psychomotor dysfunction, which are characteristics of hepatic encephalopathy, are also observed in other conditions co-morbid or co-occurring with cirrhosis (Weissenborn 2015a, b) such as renal failure, heart failure, respiratory failure and poorly controlled diabetes mellitus. In a small but well-conducted series (Lauridsen et al. 2015), abnormal PHES test results were observed in varying proportions of patients with heart failure, renal failure, poorly controlled type II diabetes mellitus or respiratory failure secondary to chronic obstructive pulmonary disease (COPD); the difference in mean values between patients with COPD and healthy controls was significant (Fig. 3). Abnormal results were also observed in the same patient groups for another diagnostic variable, the Continuous Reaction Time (CRT) (vide infra); in this instance the differences in mean values in both the patients with heart failure and those with respiratory failure were significantly reduced (Fig. 3).
Performance of the PHES and Continuous Reaction Time (CRT) tests in healthy controls and outpatients with either moderate to severe heart failure, renal failure: pre-dialysis, poorly controlled type II diabetes mellitus or respiratory failure secondary to chronic obstructive pulmonary disease. Horizontal lines indicate thresholds: PHES scores <−4 are considered abnormal; reaction time instability (CRTindex) < 1.9 is considered abnormal. Performance in all four groups is impaired compared to controls but the differences are only significant for the performance of CRT in heart failure and in both PHES and CRT in respiratory failure
Neurophysiology
The number of confounders or elements of variability in the assessment of psychometric performance provides a rational for use of a complementary, objective evaluation of brain function, which is preferably independent of demographic and education confounders and does not require patient engagement or co-operation. Electroencephalography is the electrophysiological technique most frequently used to diagnose, assess and monitor neuropsychiatric status in patients with cirrhosis. However, although the EEG provides data that are capable of objective quantification and are complementary to clinical findings and psychometric performance data neither the 2002 nor the 2014 guidelines encourage use of this technique citing the non-specificity of the findings, the lack of validation in the absence of a gold standard for the diagnosis of minimal hepatic encephalopathy and difficulties in accessing the requisite facilities.
The EEG has been used to diagnose hepatic encephalopathy since the 1950s, when monomorphic slow waves were first observed in the frontal regions of the EEG in patients with clinically overt hepatic encephalopathy (Foley et al. 1950). Subsequent observations in patients with cirrhosis identified a progressive generalised slowing of the background EEG MDF with an initial reduction in the 8–12 Hz alpha rhythm and its replacement by 5–7 Hz theta waves. Theta activity increases as the condition progresses with later replacement by even slower activity in the delta band (1–3 Hz), before the EEG finally becomes isoelectic. Triphasic waves may be observed at the stage of maximum theta activity.
Parsons-Smith et al. (1957), developed a grading system based on visual inspection of the EEG recordings in patients with cirrhosis and showed that the changes observed correlated fairly well with the degree of clinical neuropsychiatric change. However, none of the EEG findings is diagnostic for hepatic encephalopathy as similar changes are also observed in other metabolic and drug-induced encephalopathies (Niedermeyer 1999).
In their original series Parsons-Smith et al. (1957) identified EEG abnormalities in 43 % of a group of patients with cirrhosis who had no clinical evidence of hepatic encephalopathy. The authors did not realize the importance of this finding, which, in effect, identified the existence of minimal hepatic encephalopathy for the first time. There is no doubt that visual inspection of the EEG can identify slowing in patients with cirrhosis who are neuropsychiatrically unimpaired (Amodio et al. 2006) and there is a degree of concordance between the psychometric and neurophysiological findings in this patient group (Amodio et al. 2006; Montagnese et al. 2007). However, the agreement is not absolute although this is not surprising as each modality accesses different domains of cerebral activity.
A clear improvement in the quantification of EEG alterations in patients with cirrhosis was obtained by Van de Rijt et al. (1984) using spectral analysis of the digitized EEG to quantify the percentage theta activity and this was subsequently confirmed (Amodio et al. 1999a). Although the original spectral thresholds were derived for the detection of overt hepatic encephalopathy it was later determined that theta activity in excess of 35 % in a posterior lead derivation in a patient with cirrhosis with no clinical features of hepatic encephalopathy was diagnostic of minimal hepatic encephalopathy (Amodio et al. 1996; Quero et al. 1996). Subsequently it was shown that this theta threshold has prognostic value in patients with cirrhosis (Amodio et al. 2001), correlates with findings on psychometric testing (Amodio et al. 2008) and is reflective of caregivers' burden (Montagnese et al. 2012a) (Fig. 4).
Caregivers burden expressed as a total score in relation to the EEG findings in their charges; the EEG was classified as abnormal if the % theta activity ≥35 %. Data adapted from Montagnese et al. (2012a)
A more advanced techniques for spectral analysis of the EEG, the SEDACA spatio-temporal decomposition (Jackson and Sherratt 2004; Montagnese et al. 2007), can reduce the effect of noise and provide a cleaner signal for analysis. The SEDACA-derived spectral estimates correlate better with neuropsychiatric status than conventional estimates and allow differentiation of patients with minimal hepatic encephalopathy from a reference population (Montagnese et al. 2007).
Recently spectral analysis of the EEG in patients with cirrhosis have been reassessed to allow definitions of thresholds for MDF and relative delta power and relative theta power for the diagnosis of any degree of hepatic encephalopathy. New thresholds were calculated, for these three individual variables using conventional Receiver Operator Characteristics (ROC) curve analysis while an extended multivariable ROC-like (MV ROC) analysis was used to test every combination of thresholds for MDF, relative delta power and relative theta power to select the set that had the best performance (Jackson et al. 2014, personal communication) (Table 1). The utility of the thresholds defined using the MV ROC procedure for the diagnosis of any degree of hepatic encephalopathy were superior to the conventional and ROC-derived thresholds and these findings were validated in two separate populations (Table 2). Adoption of these new spectral thresholds would significantly improve the diagnostic utility of the EEG for the diagnosis of minimal hepatic encephalopathy, particularly when used in conjunction with an assessment of psychometric performance.
One of the cited criticisms of the EEG as a diagnostic tool for minimal hepatic encephalopathy is its inaccessibility to clinicians. However, commercially available, low-cost, wireless headsets are now available, and provide quantified parameters in patients with cirrhosis and hepatic encephalopathy which are comparable to those obtained with professional high-quality equipment (Schiff et al. 2014, personal communication). Access to this technology, which provides operator- and patient-independent data, might encourage more wide-spread use of the EEG for the diagnosis and monitoring of hepatic encephalopathy.
Other assessment techniques
Very little information on alternative diagnostic test systems for minimal hepatic encephalopathy was available to the working group formulating the 2002 guideline but information on several systems was evaluated in the 2014 review.
The Inhibitory Control Test (ICT) is a computerized, chronometric test of attention and response inhibition, which can be freely downloaded from www.hecme.tv. Patients are shown a series of random letters and are asked to respond by pressing a mouse key when an X is followed by a Y, or a Y is followed by an X (alternating presentation, termed targets); they are instructed not to respond to X following X or Y following Y (non-alternating presentation, termed lures). High lure and low target responses indicate poor psychometric performance.
A lure threshold of >5 was identified as the key variable for the diagnosis of minimal hepatic encephalopathy (Bajaj et al. 2007a; Bajaj et al. 2008). In the initial studies ICT exhibited a sensitivity of 88 % and a specificity of 77 % for the diagnosis of minimal hepatic encephalopathy; showed good test-retest reliability and equivalence to standard psychometric tests (Bajaj et al. 2007a; Bajaj et al. 2008). However, it is now generally agreed that the initial lure threshold was set too low—most likely reflecting the high educational attainments of the selected control population—and that lure thresholds need to be adjusted to reflect local population norms (Sharma et al. 2013). Subsequently other workers have found that ICT results: (i) correlate poorly with the results of other tests used for the diagnosis of minimal hepatic encephalopathy; (ii) are influenced by demographic variables; (iii) exhibits some learning effect; and, (iv) have greater diagnostic utility if the number of lures (inhibitory ability) is adjusted by target accuracy (attention ability) (Amodio et al. 2010). In addition, patients generally prefer other test systems (Sharma et al. 2013).
The Stroop Color and Word Test or Stroop Test is a short test based on the Stroop effect of interference in the recognition reaction time to a task. Thus, when the name of a colour is printed in a colour different to the name e.g. the word red is printed in blue rather than red ink, naming the colour of the word takes longer and is more prone to errors than when the colour of the ink and the name match (Fig. 5). This test evaluates executive aspects of control such as attention, information processing speed, selective attention and cognitive flexibility. It has been used previously to study the defects in attention observed in patients with cirrhosis (Amodio et al. 2005; Felipo et al. 2012).
The Stroop Test is based on the Stroop effect. In Panel 1 the name of the words and their colours are concordant whereas in Panel 2 the names and colours are discordant The naming of the colour of a visually presented word slows, if the content of the word contradicts the colour, for example, the word ‘red’ is presented in yellow, green or blue. (Color figure online)
Recently a smartphone application for the Stroop task (EncephalApp_Stroop) has been used to diagnose minimal hepatic encephalopathy in patients with cirrhosis (www.encephalapp.com) (Bajaj et al. 2013, 2014). The Stroop test has an ‘Off’ state with neutral stimuli and an ‘On’ state with incongruent stimuli. Outcomes include the time to complete five correct runs as well as the number of trials needed in on (Ontime) and off (Offtime) states. Stroop performance measured as the Ontime + Offtime was found to be significantly impaired in patients with minimal hepatic encephalopathy and the level of agreement with the results of the PHES test was good (Kappa statistic 0.7). However, the patients with cirrhosis included in these studies were relatively young with a mean age of around 52 years and overall had relatively high educational attainments. In addition, the performance of the Stroop test is known to be affected by a number of confounders including age, education, gender, and an education by gender interaction (Llinàs-Reglà et al. 2013; Moering et al. 2004; Van der Elst et al. 2006) (Fig. 2); which were not sufficiently well accounted for in these studies. Further studies are underway.
Critical Flicker Frequency ( CFF ), is a technique which centers on the perception of light as flickering or fused as its frequency changes. It assesses visual discrimination ability and general arousal (Kircheis et al. 2002). More recently the neurophysiological basis of CFF testing has been addressed in more detail using functional magnetic resonance imaging and spectroscopy, and magnetoencephalography (Miese et al. 2006; Shah et al. 2008; Timmermann et al. 2008; Zafiris et al. 2004).
Kircheis et al. (2002), reported that a CFF threshold of 39 Hz allowed 100 % separation of patients with overt hepatic encephalopathy from neuropsychiatrically unimpaired patients with cirrhosis and normal controls and that the same frequency allowed separation of patients with minimal hepatic encephalopathy from unimpaired patients with a sensitivity of 55 % and a specificity of 100 %. In a later study, by another group, a CFF cut-off of 38 Hz identified patients with minimal hepatic encephalopathy, diagnosed using the PHES test, with a sensitivity of 72.4 % and a specificity of 77.2 % and an observed agreement of 75 % (Romero-Gómez et al. 2007). Low CFF readings predict the development of overt hepatic encephalopathy during follow-up (Romero-Gómez et al. 2007); predict the development of overt hepatic encephalopathy following TIPS insertion more accurately than the PHES test (Berlioux et al. 2014); and predict poor post-TIPS outcomes (Kircheis et al. 2009).
Variables such as gender, level of education and time of day do not appear to significantly affect CFF results (Kircheis et al. 2002), although there is some evidence of differential effects in relation to age (Dhiman et al. 2010; Goldbecker et al. 2013) and the aetiology of the underlying liver disease (Kircheis et al. 2002). Testing requires optimization of test runs, careful standardization of operating procedures, and intact binocular vision. In addition, one of the available commercial machines utilizes a red light and so can not be used in individuals who are red-green colour blind. Patients find this test system very acceptable (Sharma et al. 2013).
The Scan Package is a computerized reaction time test based on a digit recognition memory task. It assesses cognitive attention, psychomotor speed and working memory, in a ‘modular’ fashion, with three increasing levels of difficulty viz: simple reaction time, choice reaction time and scan reaction time. The Scan test software provides an overall Z score, which is corrected for age/educational attainment. There is relatively little information on the utility of the Scan package for the diagnosis of minimal hepatic encephalopathy per se as the studies to date have looked at the whole spectrum of neuropsychiatric impairment in patients with cirrhosis (Amodio et al. 1999b; Montagnese et al. 2012b). It has been shown that both the simple and choice reaction times are predictive of survival (Montagnese et al. 2012b). The Scan test is influenced by visual stimulus encoding defects, impairment in the stage of selection and output of response, altered memory scanning, reduced short-term memory, sustained attention, and motor speed. It is likely to be subject to leaning effects. Further evaluation of the utility of the Scan package for the diagnosis of minimal hepatic encephalopathy is underway.
The Continuous Reaction Time ( CRT ) test (EKHO, Bitmatic, Aarhus, Denmark), is a 10-min computerized test of motor reaction time stability to 150 auditory stimuli designed to test sustained attention and attention stability. The key variable is the CRTindex, which is the variation coefficient of the test reaction times; a CRTindex threshold of <1.9 defines abnormality. The concordance of results with CRT and PHES for the diagnosis of minimal hepatic encephalopathy is relative poor at 60 % but use of the two tests can categorize patients into risk categories for the development of overt hepatic encephalopathy and for mortality (Lauridsen et al. 2011, 2015). The results are independent of age and gender (Lauridsen et al. 2012) and there is no learning effect. Results are susceptible to the confounding effects of external distraction, psychoactive drugs, and possibly sleep disturbances (Lauridsen et al. 2014).
A multimodal approach
There is no gold standard for the diagnosis of minimal hepatic encephalopathy. Some tests/test systems are better validated than others e.g. the PHES and so these often serves as the ‘best clinical standard’ for validation of new or alternatives tests/test systems. However, as hepatic encephalopathy may affect different cognitive domains in different patients a better approach might be to identify a combination of tests which cover all bases. The merit of this approach is illustrated in the following two clinical scenarios (Tables 3 and 4)
-
Patient 1 (Table 3), a 66-year-old man with HCV-related cirrhosis presented 14 months after successful TIPS insertion, for uncontrollable variceal bleeding, complaining of difficulties multitasking at work. His liver disease was well compensated and his clinical condition was otherwise stable. His PHES score was normal; his EEG MDF and CFF results were at the lower end of the reference range; his Scan test result was borderline abnormal while his fasting venous ammonia level was high. The results were not conclusive for a diagnosis of minimal hepatic encephalopathy but in view of his stated cognitive difficulties he was started on treatment with lactulose. Treatment resulted in an improvement in his symptoms, overall cognitive performance and the results of his EEG and CFF; there was also a significant decrease in his blood ammonia levels. This case illustrates two important points: (i) test results may lie within references ranges but still be abnormal for that patient; knowledge of patients' premorbid performance will allow these distinctions to be made and; (ii) the decision to treat should not be based solely on test results but should also take into account patient and caregivers assessments of performance and quality of life.
-
Patient 2 (Table 4), a 69-year-old man with alcohol-related cirrhosis was evaluated because his family and carers reported worsening mental performance. The assessment of his test results was complicated by the fact that he was already on treatment with lactulose and rifaximin. However, his significant memory problems and low Mini Mental State Evaluation (Folstein et al. 1975) warranted cerebral imaging, which showed evidence of diffuse cerebrovascular disease and cerebral atrophy. A diagnosis of cerebrovascular and/or alcohol-related dementia was made. Six months later there was further worsening of his mental function in the absence of any deterioration in his liver disease. This case illustrates the importance of not assuming that all changes in mental status in patients with cirrhosis are a consequence of hepatic encephalopathy.
While it is not realistic to suggest that such comprehensive evaluations are performed routinely, they should certainly be considered in patients with cirrhosis with neuropsychiatric impairment if: (i) blood ammonia levels are normal; (ii) there is no response to ammonia-lowering treatment; and (iii) there are possible alternative causes for the clinical findings (Vilstrup et al. 2014; Montagnese et al. 2015).
Summary and conclusion
A number of test systems have utility for the diagnosis of minimal hepatic encephalopathy; combining tests increases diagnostic efficacy. The 2014 Practice Guideline provided suggestions on how these diagnostic tests should be used. However, one of the major difficulties in taking this forward is the level of disagreement within the field over the selection and utilization of the various diagnostic tools. International, collaborative studies are required in which investigators' preference is not allowed to dictate study design and where the predictive validity of tests and the effects of associated co-morbidities on test performance is explored. In addition, to ensure that studies are truly International the inability of collaborators, particularly in America, to access certain test systems should be challenged by National Professional Associations to ensure that they can participate.
There was recognition in both the 2002 and 2014 guidelines that the presence of minimal hepatic encephalopathy has a detrimental effect on well-being. Thus, its presence is associated with significant impairment in the ability to perform complex tasks, such as driving (Bajaj et al. 2007b; Schomerus et al. 1981; Wein et al. 2004); a detrimental effect on quality of life (Groeneweg et al. 1998; Schomerus and Hamster 2001); patient safety (Roman et al. 2011); and, ultimately, survival (Patidar et al. 2014). Its presence also poses a substantial burden for the caregivers of affected individuals (Bajaj et al. 2011b) and a significant financial burden on health-care systems (Patidar et al. 2014; Poordad 2007).
There is clear evidence from a number of studies that minimal hepatic encephalopathy responds to treatment with: (i) resolution of psychometric/neurophysiological abnormalities and the detrimental effects on quality of life; and (ii) improved liver-related mortality and morbidity (Luo et al. 2011; Gluud et al. 2015). Nevertheless, the 2014 Practice Guideline did not recommend routine screening for minimal hepatic encephalopathy nor did they recommend that patients should be treated except on a case by case basis (Vilstrup et al. 2014). This effectively means that patients with minimal hepatic encephalopathy will go unrecognized and will be denied the benefits of treatment. It is clear that corporate efforts and consensus agreements are needed to develop effective diagnostic algorithms and move the field on so that the issues of screening and treatment can be revisited.
References
Amodio P, Quero JC, Del Piccolo F, Gatta A, Schalm SW (1996) Diagnostic tools for the detection of subclinical hepatic encephalopathy: comparison of standard and computerized psychometric tests with spectral-EEG. Metab Brain Dis 11(4):315–327
Amodio P, Marchetti P, Del Piccolo F, de Tourtchaninoff M, Varghese P, Zuliani C (1999a) Spectral versus visual EEG analysis in mild hepatic encephalopathy. Clin Neurophysiol 110(8):1334–1344
Amodio P, Del Piccolo F, Marchetti P, Angeli P, Iemmolo R, Caregaro L, Merkel C, Gerunda G, Gatta A (1999b) Clinical features and survival of cirrhotic patients with subclinical cognitive alterations detected by the number connection test and computerized psychometric tests. Hepatology 29(6):1662–1667
Amodio P, Del Piccolo F, Petteno E, Mapelli D, Angeli P, Iemmolo R, Muraca M, Musto C, Gerunda G, Rizzo C, Merkel C, Gatta A (2001) Prevalence and prognostic value of quantified electroencephalogram (EEG) alterations in cirrhotic patients. J Hepatol 35(1):37–45
Amodio P, Schiff S, Del Piccolo F, Mapelli D, Gatta A, Umilta C (2005) Attention dysfunction in cirrhotic patients: an inquiry on the role of executive control, attention orienting and focusing. Metab Brain Dis 20(2):115–127
Amodio P, Pellegrini A, Ubiali E, Mathy I, Piccolo FD, Orsato R, Gatta A, Guerit JM (2006) The EEG assessment of low-grade hepatic encephalopathy: comparison of an artificial neural network-expert system (ANNES) based evaluation with visual EEG readings and EEG spectral analysis. Clin Neurophysiol 117(10):2243–2251
Amodio P, Campagna F, Olianas S, Iannizzi P, Mapelli D, Penzo M, Angeli P, Gatta A (2008) Detection of minimal hepatic encephalopathy: normalization and optimization of the psychometric hepatic encephalopathy score. A neuropsychological and quantified EEG study. J Hepatol 49(3):346–353
Amodio P, Ridola L, Schiff S, Montagnese S, Pasquale C, Nardelli S, Pentassuglio I, Trezza M, Marzano C, Flaiban C, Angeli P, Cona G Bisiacchi P., Gatta A, Riggio O (2010) Improving detection of minimal hepatic encephalopathy using the inhibitory control task. Gastroenterology 139(2): 510–518
Bajaj JS, Saeian K, Verber MD, Hischke D, Hoffmann RG, Franco J, Varma RR, Rao SM (2007a) Inhibitory control test is a simple method to diagnose minimal hepatic encephalopathy and predict development of overt hepatic encephalopathy. Am J Gastroenterol 102(4):754–760
Bajaj JS, Hafeezullah M, Hoffmann RG, Saeian K (2007b) Minimal hepatic encephalopathy: a vehicle for accidents and traffic violations. Am J Gastroenterol 102(9):1903–1909
Bajaj JS, Hafeezullah M, Franco J, Varma RR, Hoffmann RG, Knox JF, Hischke D, Hammeke TA, Pinkerton SD, Saeian K (2008) Inhibitory control test for the diagnosis of minimal hepatic encephalopathy. Gastroenterology 135(5):1591–1600
Bajaj JS, Cordoba J, Mullen KD, Amodio P, Shawcross DL, Butterworth RF, Morgan MY; International Society for Hepatic Encephalopathy and Nitrogen Metabolism (ISHEN) (2011a) The design of clinical trials in hepatic encephalopathy–an international society for hepatic encephalopathy and nitrogen metabolism (ISHEN) consensus statement.. Aliment Pharmacol Ther 33(7): 739–747
Bajaj JS, Wade JB, Gibson DP, Heuman DM, Thacker LR, Sterling RK, Stravitz RT, Luketic V, Fuchs M, White MB, Bell DE, Gilles H, Morton K, Noble N, Puri P, Sanyal AJ (2011b) The multi-dimentional burden of cirrhosis and hepatic encephalopathy on patients and caregivers. Am J Gastroenterol 106(9):1646–1653
Bajaj JS, Thacker LR, Heuman DM, Fuchs M, Sterling RK, Sanyal AJ, Puri P, Siddiqui MS, Stravitz RT, Bouneva I, Luketic V, Noble N, White MB, Monteith P, Unser A, Wade JB (2013) The stroop smartphone application is a short and valid method to screen for minimal hepatic encephalopathy. Hepatology 58(3):1122–1132
Bajaj JS, Heuman DM, Sterling RK, Sanyal AJ, Siddiqui M, Matherly S, Luketic V, Stravitz RT, Fuchs M, Thacker LR, Gilles H, White MB, Unser A, Hovermale J, Gavis E, Noble NA, Wade JB (2015) Validation of EncephalApp, smartphone-based stroop test, for the diagnosis of covert hepatic encephalopathy. Clin Gastroenterol Hepatol 13(10):1828–1835
Berlioux P, Robic MA, Poirson H, Métivier S, Otal P, Barret C, Lopez F, Péron JM, Vinel JP, Bureau C (2014) Pre-transjugular intrahepatic portosystemic shunts (TIPS) prediction of post-TIPS overt hepatic encephalopathy: the critical flicker frequency is more accurate than psychometric tests. Hepatology 59(2):622–629
Campagna F, Montagnese S, Schiff S, Ruzzoli M, Biancardi A, Iannizzi P, Pujatti PL, Angeli P, Gatta A, Merkel C, Leandro G, Mapelli D, Amodio P (2015) Confounders in the detection of minimal hepatic encephalopathy: a neuropsychological and quantified EEG study. Liver Int 35(5):1524–15320
Cona G, Montagnese S, Bisiacchi PS, Gatta A, Cillo U, Angeli P, Amodio P, Schiff S (2014) Early markers of neural dysfunction and compensation: a model from minimal hepatic encephalopathy. Clin Neurophysiol 125(6):1138–1144
Dhiman RK, Kurmi R, Thumburu KK, Venkataramarao SH, Agarwal R, Duseja A, Chawla Y (2010) Diagnosis and prognostic significance of minimal hepatic encephalopathy in patients with cirrhosis of liver. Dig Dis Sci 55(8):2381–2390
Duarte-Rojo A, Estradas J, Hernández-Ramos R, Ponce-de-León S, Córdoba J, Torre A (2011) Validation of the psychometric hepatic encephalopathy score (PHES) for identifying patients with minimal hepatic encephalopathy. Dig Dis Sci 56(10):3014–3023
Felipo V, Ordono JF, Urios A, El Mlili N, Gimenez-Garzo C, Aguado C, Gonzalez-Lopez O, Giner-Duran R, Serra MA, Wassel A, Rodrigo JM, Salazar J, Montoliu C (2012) Patients with minimal hepatic encephalopathy show impaired mismatch negativity correlating with reduced performance in attention tests. Hepatology 55(2):530–539
Ferenci P, Lockwood AH, Mullen K, Tarter R, Weissenborn K, Blei AT (2002) Hepatic encephalopathy–definition, nomenclature, diagnosis, and quantification: final report of the working party at the 11th world congresses of gastroenterology, Vienna, 1998. Hepatology 35(3):716–721
Foley JM, Watson CW, Adams RD (1950) Significance of electroencephalographic changes in hepatic coma. Trans Am Neurol Assoc 51:161–165
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3):189–198
Gitlin N, Lewis DC, Hinkley L (1986) The diagnosis and prevalence of subclinical hepatic encephalopathy in apparently healthy, ambulant, non-shunted patients with cirrhosis. J Hepatol 3(1):75–82
Gluud LL, Vilstrup H, Morgan MY (2015) Nonabsorbable disaccharides for hepatic encephalopathy in people with cirrhosis. Cochrane Database of Systematic Reviews (in press)
Goldbecker A, Weissenborn K, Hamidi Shahrezaei G, Afshar K, Rümke S, Barg-Hock H, Strassburg CP, Hecker H, Tryc AB (2013) Comparison of the most favoured methods for the diagnosis of hepatic encephalopathy in liver transplantation candidates. Gut 62(10):1497–1504
Groeneweg M, Quero JC, De BI, Hartmann IJ, Essink-bot ML, Hop WC, Schalm SW (1998) Subclinical hepatic encephalopathy impairs daily functioning. Hepatology 28(1):45–49
Jackson C, Sherratt M (2004) A novel spatio-temporal decomposition of the EEG: derivation, validation and clinical application. Clin Neurophysiol 115(1):227–237
Kircheis G, Wettstein M, Timmermann L, Schnitzler A, Häussinger D (2002) Critical flicker frequency for quantification of low-grade hepatic encephalopathy. Hepatology 35(2):357–366
Kircheis G, Bode JG, Hilger N, Kramer T, Schnitzler A, Häussinger D (2009) Diagnostic and prognostic values of critical flicker frequency determination as new diagnostic tool for objective HE evaluation in patients undergoing TIPS implantation. Eur J Gastroenterol Hepatol 21(12):1383–1394
Kircheis G, Hilger N, Häussinger D (2014) Value of critical flicker frequency and psychometric hepatic encephalopathy score in diagnosis of low-grade hepatic encephalopathy. Gastroenterology 146(4):961–969
Kurmi R, Dhiman RK, Reddy K, et al (2008) Psychometric hepatic encephalopathy score, critical flicker frequency and p300 event related potentials for the diagnosis of minimal hepatic encephalopathy: evidence that psychometric hepatic encephalopathy score is enough. Indian J Gastroenterol 27(Suppl 1):S1
Lauridsen MM, Jepsen P, Vilstrup H (2011) Critical flicker frequency and continuous reaction times for the diagnosis of minimal hepatic encephalopathy. A comparative study of 154 patients with liver disease. Metab Brain Dis 26(2):135–139
Lauridsen MM, Grønbæk H, Næser EB, Leth ST, Vilstrup H (2012) Gender and age effects on the continuous reaction times method in volunteers and patients with Cirrhosis. Metab Brain Dis 27(4):559–565
Lauridsen MM, Frøjk J, de Muckadell OB, Vilstrup H (2014) Opposite effects of sleep deprivation on the continuous reaction times in patients with liver cirrhosis and normal Persons. Metab Brain Dis 29(3):655–660
Lauridsen MM, Schaffalitzky de Muckadell OB, Vilstrup H (2015) Minimal hepatic encephalopathy characterized by parallel use of the continuous reaction time and portosystemic encephalopathy tests. Metab Brain Dis 30(5):1187–1192
Llinàs-Reglà J, Vilalta-Franch J, López-Pousa S, Calvó-Perxas L, Garre-Olmo J (2013) Demographically adjusted norms for Catalan older adults on the stroop color and word test. Arch Clin Neuropsychol 28(3):282–296
Luo M, Li L, Lu C-Z, W-K C (2011) Clinical efficacy and safety of lactulose for minimal hepatic encephalopathy: a meta-analysis. Euro L Gastroenterol Hepatol 23(12):1250–1257
Mardini H, Saxby BK, Record CO (2008) Computerized psychometric testing in minimal encephalopathy and modulation by nitrogen challenge and liver transplant. Gastroenterology 135(5):1582–1590
Marks M, Jackson CD, Montagnese S, Jenkins CW, Head IM, Morris RW, Morgan MY (2008) Derivation of a normative UK database for the psychometric hepatic encephalopathy score (PHES): confounding effect of ethnicity and test scoring. J Hepatol 48(Suppl 2):S119–S300
Miese F, Kircheis G, Wittsack HJ, Wenserski F, Hemker J, Mödder U, Häussinger D, Cohnen M (2006) 1 H-MR spectroscopy, magnetization transfer, and diffusion-weighted imaging in alcoholic and nonalcoholic patients with cirrhosis with hepatic encephalopathy. AJNR Am J Neuroradiol 27(5):1019–1026
Moering RG, Schinka JA, Mortimer JA, Graves AB (2004) Normative data for elderly African Americans for the stroop color and word test. Arch Clin Neuropsychol 19(1):61–71
Montagnese S, Amodio P, Morgan MY (2004) Methods for diagnosing hepatic encephalopathy in patients with cirrhosis: a multidimensional approach. Metab Brain Dis 19(3–4):281–312
Montagnese S, Jackson C, Morgan MY (2007) Spatio-temporal decomposition of the electroencephalogram in patients with cirrhosis. J Hepatol 46(3):447–458
Montagnese S, Cona G, Schiff S, Maresio G, Gatta A, Merkel C, Amodio P (2010) The hunter and the pianist: two hepatic encephalopathy tales. J Clin Gastroenterol 45(6):563–566
Montagnese S, Amato E, Schiff S, Facchini S, Angeli P, Gatta A, Amodio P (2012a) A patients' and caregivers' perspective on hepatic encephalopathy. Metab Brain Dis 27(4):567–572
Montagnese S, Schiff S, Turco M, Bonato CA, Ridola L, Gatta A, Nousbaum JB, Riggio O, Merkel C, Amodio P (2012b) Simple tools for complex syndromes: a three-level difficulty test for hepatic encephalopathy. Dig Liver Dis 44(11):957–960
Montagnese S, Schiff S, Amodio P (2015) Quick diagnosis of hepatic encephalopathy: fact or fiction? Hepatology 61(1):405–406
Nardelli S, Pentassuglio I, Pasquale C, Ridola L, Moscucci F, Merli M, Mina C, Marianetti M, Fratino M, Izzo C, Merkel C, Riggio O (2013) Depression, anxiety and alexithymia symptoms are major determinants of health related quality of life (HRQoL) in cirrhotic patients. Metab Brain Dis 28(2):239–243
Niedermeyer E (1999) Metabolic Central Nervous System Disorders. In: Niedermeyer E, Lopes Da Silva F (eds) Electroencephalography. Basic principles, clinical applications, and related fields, 4th edn. Williams & Wilkins, Baltimore, pp. 416–431
Norman MA, Moore DJ, Taylor M, Franklin D Jr, Cysique L, Ake C, Lazarretto D, Vaida F, Heaton RK; HNRC Group (2011) Demographically corrected norms for African Americans and Caucasians on the Hopkins verbal learning test-revised, brief visuospatial memory test-revised, stroop color and word test, and Wisconsin card sorting test 64-card version. J Clin Exp Neuropsychol 33(7): 793–804
Parsons-Smith BG, Summerskill WHJ, Dawson AM, Sherlock S (1957) The electroencephalograph in liver disease. Lancet 273(7001):867–871
Patidar KR, Thacker LR, Wade JB, Sterling RK, Sanyal AJ, Siddiqui MS, Matherly SC, Stravitz RT, Puri P, Luketic VA, Fuchs M, White MB, Noble NA, Unser AB, Gilles H, Heuman DM, Bajaj JS (2014) Covert hepatic encephalopathy is independently associated with poor survival and increased risk of hospitalization. Am J Gastroenterol 109(11):1757–1763
Poordad FF (2007) Review of the burden of hepatic encephalopathy. Aliment Pharmacol Ther 25(Suppl 1):3–9
Quero JC, Hartmann IJ, Meulstee J, Hop WC, Schalm SW (1996) The diagnosis of subclinical hepatic encephalopathy in patients with cirrhosis using neuropsychological tests and automated electroencephalogram analysis. Hepatology 24(3):556–560
Randolph C, Hilsabeck R, Kato A (2009) International society for hepatic encephalopathy and nitrogen metabolism (ISHEN). neuropsychological assessment of hepatic encephalopathy: ISHEN practice guidelines. Liver Int 29(5):629–635
Reitan RM (1955) The relation of the trail making test to organic brain damage. J Consult Psychol 19(5):393–394
Riggio O, Ridola L, Pasquale C, Pentassuglio I, Nardelli S, Moscucci F, Merli M, Montagnese S, Amodio P, Merkel C (2011) A simplified psychometric evaluation for the diagnosis of minimal hepatic encephalopathy. Clin Gastroenterol Hepatol 9(7):613–616
Roman E, Córdoba J, Torrens M, Torras X, Villanueva C, Vargas V, Guarner C, Soriano G (2011) Minimal hepatic encephalopathy is associated with falls. Am J Gastroenterol 106(3):476–482
Romero Gómez M, Córdoba J, Jover R, del Olmo J, Fernández A, Flavià M, Compañy L, Poveda MJ, Felipo V; Red Nacional de Investigación en Encefalopatía Hepática (2006) Normality tables in the Spanish population for psychometric tests used in the diagnosis of minimal hepatic encephalopathy. Med Clin 127 (7): 246–249.
Romero-Gómez M, Córdoba J, Jover R, del Olmo JA, Ramírez M, Rey R, de Madaria E, Montoliu C, Nuñez D, Flavia M, Compañy L, Rodrigo JM, Felipo V (2007) Value of the critical flicker frequency in patients with minimal hepatic encephalopathy. Hepatology 45(4):879–885
Schiff S, Vallesi A, Mapelli D, Pellegrini A, Orsato R, Umiltà CA, Amodio P (2005) Response inhibition impairment precede motor alteration in the early stage of liver cirrhosis. A behavioural and electrophysiological study. Metab Brain Dis 20(4):381–392
Schomerus H, Hamster W (2001) Quality of life in cirrhotics with minimal hepatic encephalopathy. Metab Brain Dis 16(1–2):37–41
Schomerus H, Hamster W, Blunck H, Reinhard U, Mayer K, Dolle W (1981) Latent portasystemic encephalopathy. I Nature of cerebral functional defects and their effect on fitness to drive. Dig Dis Sci 26(7):622–630
Schomerus H, Weissenborn K, Hamster W, Rückert N, Hecker H (1999) PSE-Syndrom-Test. Psychodiagnostisches Verfahren zur quantitativen Erfassung der (minimalen) portosystemischen Encephalopathie (PSE). Frankfurt: Swets & Zeitlinger BV, Swets Test Services
Schomerus H, Hamster W (1998) Neuropsychological aspects of portal-systemic encephalopathy. Metab Brain Dis 13(4):361–377
Seo YS, Yim SY, Jung JY, Kim CH, Kim JD, Keum B, An H, Yim HJ, Lee HS, Kim CD, Ryu HS, Um SH (2012) Psychometric hepatic encephalopathy score for the detection of minimal hepatic encephalopathy in Korean patients with liver cirrhosis. J Gastroenterol Hepatol 27(11):1695–1704
Shah NJ, Neeb H, Kircheis G, Engels P, Häussinger D, Zilles K (2008) Quantitative cerebral water content mapping in hepatic encephalopathy. NeuroImage 41(3):706–717
Sharma P, Kumar A, Singh S, Tyagi P, Kumar A (2013) Inhibitory control test, critical flicker frequency, and psychometric tests in the diagnosis of minimal hepatic encephalopathy in cirrhosis. Saudi J Gastroenterol 19(1):40–44
Timmermann L, Butz M, Gross J, Ploner M, Südmeyer M, Kircheis G, Häussinger D, Schnitzler A (2008) Impaired cerebral oscillatory processing in hepatic encephalopathy. Clin Neurophysiol 119(2):265–272
Van de Rijt CC, Schalm SW, De Groot GH, De VM (1984) Objective measurement of hepatic encephalopathy by means of automated EEG analysis. Electroencephalogr Clin Neurophysiol 57(5):423–426
Van der Elst W, Van Boxtel MP, Van Breukelen GJ, Jolles J (2006) The stroop color-word test: influence of age, sex, and education; and normative data for a large sample across the adult age range. Assessment 13(1):62–79
Vienna test system (WINWTS), version 4.50. Mödling, Austria: Dr G. Schuhfried GmbH, (1999)
Vilstrup H, Amodio P, Bajaj J, Cordoba J, Ferenci P, Mullen KD, Weissenborn K, Wong P (2014) Hepatic encephalopathy in chronic liver disease: 2014 practice guideline by the American association for the study of liver diseases and the European association for the study of the liver. Hepatology 60(2):715–735
Wechsler D (1981) Wechsler adult intelligence scale-revised. Psychological Corporation, New York
Wein C, Koch H, Popp B, Oeher G, Schauder P (2004) Minimal hepatic encephalopathy impairs fitness to drive. Hepatology 39(3):739–745
Weissenborn K (2015a) Challenges in diagnosing hepatic encephalopathy. Neurochem Res 40(2):265–273
Weissenborn K (2015b) Diagnosis of minimal hepatic encephalopathy. J Clin Exp Hepatol 5(Suppl 1):S54–S59
Weissenborn K, Ennen JC, Schomerus H, Rückert N, Hecker H (2001) Neuropsychological characterization of hepatic encephalopathy. J Hepatol 34(5):768–773
Weissenborn K, Hecker H, Rückert N (2015) Pitfalls in psychometric testing. Gastroenterology 148(3):664–665
Wunsch E, Koziarska D, Kotarska K, Nowacki P, Milkiewicz P (2013) Normalization of the psychometric hepatic encephalopathy score in Polish population. A prospective, quantified electroencephalography study. Liver Int 33(9):1332–1340
Zafiris O, Kircheis G, Rood HA, Boers F, Häussinger D, Zilles K (2004) Impaired visuo-spatial decision making in hepatic encephalopathy relates to attenuated BOLD-signal in the right inferior parietal cortex. NeuroImage 22(2):541–552
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Morgan, M.Y., Amodio, P., Cook, N.A. et al. Qualifying and quantifying minimal hepatic encephalopathy. Metab Brain Dis 31, 1217–1229 (2016). https://doi.org/10.1007/s11011-015-9726-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-015-9726-5