Abstract
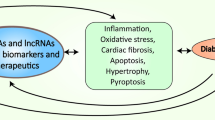
Diabetic cardiomyopathy (DCM) represents a distinct myocardial disorder elicited by diabetes mellitus, characterized by aberrations in myocardial function and structural integrity. This pathological condition predominantly manifests in individuals with diabetes who do not have concurrent coronary artery disease or hypertension. An escalating body of scientific evidence substantiates the pivotal role of programmed cell death (PCD)—encompassing apoptosis, autophagy, pyroptosis, ferroptosis, and necroptosis—in the pathogenic progression of DCM, thereby emerging as a prospective therapeutic target. Additionally, numerous non-coding RNAs (ncRNAs) have been empirically verified to modulate the biological processes underlying programmed cell death, consequently influencing the evolution of DCM. This review systematically encapsulates prevalent types of PCD manifest in DCM as well as nascent discoveries regarding the regulatory influence of ncRNAs on programmed cell death in the pathogenesis of DCM, with the aim of furnishing novel insights for the furtherance of research in PCD-associated disorders relevant to DCM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetic Cardiomyopathy (DCM) serves as a prevalent complication stemming from diabetes mellitus, typified by anomalous ventricular myocardial structure and functionality. The etiology of DCM exists independently of additional pathological factors such as hypertension, coronary heart disease, and valvular disorders. Notably, diabetic individuals are predisposed to a 2–fivefold elevated risk of heart failure in comparison to non-diabetic counterparts [1]. Hyperglycemia exerts detrimental impacts on cardiac function and structure, precipitating myocardial cellular hypertrophy, myocardial fibrosis, and impairments in left ventricular systolic and diastolic functionality, which invariably culminate in heart failure, arrhythmia, and cardiogenic shock [2].Currently, there is a lack of universal consensus regarding pharmacological interventions for DCM on a global scale. The primary clinical treatment strategies focus on glycemic control and the administration of ACEI inhibitors and β-adrenergic receptor blockers, aimed at decelerating disease progression. However, the prohibitive costs associated with novel targeted pharmacological agents, such as DPP-4 inhibitors and SGLT-2 inhibitors, restrict their clinical application. Furthermore, the pathogenesis of DCM remains complex and is not fully elucidated. Though incompletely understood, extant literature suggests that its pathogenesis may be associated with metabolic dysregulation, oxidative stress, systemic low-grade inflammatory responses, and multiple forms of programmed cell death including apoptosis, autophagy, pyroptosis, and ferroptosis [3]. Therefore, an exhaustive and in-depth examination of DCM’s pathogenesis is imperative for the identification of novel and efficacious therapeutic targets and pharmaceutical agents, bearing significant implications for the enhancement of patient prognosis and the amelioration of life quality.
Programmed cell death (PCD) is an integral biological process that all viable cells inevitably undergo at the terminus of their lifecycle [4]. Classical research primarily categorized cell death into apoptosis and necrosis [5]. Recent burgeoning literature indicates the emergence of a novel form of cell death distinct from apoptosis and necrosis, termed “programmed cell death,” encompassing autophagy, pyroptosis, ferroptosis, and necroptosis, each possessing distinct and independent regulatory pathways [6]. Accumulating evidence elucidates the interrelated nature of different PCD pathways at various molecular strata, playing pivotal roles in cardiovascular disorders and specifically in the progression of DCM [7].Strategies to regulate PCD in DCM have thus emerged as one of the focal points in current DCM preventive and therapeutic research. Recent studies indicate that non-coding RNA (ncRNA) plays a regulatory role in PCD within the context of DCM. Consequently, the conceptualization of therapeutic approaches targeting PCD via ncRNAs holds promise as a prospective strategy for DCM treatment. Based on these premises, we summarize the relationships between ncRNAs and four types of PCD (apoptosis, autophagy, pyroptosis, ferroptosis, and necroptosis) observed in DCM, elucidating the role of ncRNAs in modulating PCD for DCM treatment, with the objective of identifying novel therapeutic targets.
Apoptosis in diabetic cardiomyopathy: an in-depth review
Overview of apoptosis
Apoptosis, commonly acknowledged as a seminal and extensively investigated form of Programmed Cell Death (PCD), is characterized by a distinctive set of morphological features including cellular shrinkage, chromatin condensation, membrane blebbing, DNA fragmentation, and the generation of apoptotic bodies [8]. It serves as a critical biological mechanism for the elimination of superfluous, irreversibly damaged, or potentially deleterious cells, thus maintaining cellular homeostasis at an optimal turnover rate [9]. The process of apoptosis is principally instigated through two divergent pathways, specifically, the extrinsic and intrinsic pathways [10].The extrinsic pathway, also known as death receptor-mediated pathway, is initiated upon the binding of death ligands displayed on the cell membrane to their cognate death receptors. The principal receptors implicated in this pathway encompass FAS Cell Surface Death Receptor (FAS), TNF-related Apoptosis-Inducing Ligand Receptor (TRAIL-R), and TNF Receptor Superfamily Member 1A (TNFR1). The consequential ligation of these receptors and their ligands triggers the formation of the Death-Inducing Signaling Complex (DISC), subsequently facilitating the activation of caspase-8 [11]. This cascade culminates in the activation of effector caspases such as caspase-3 and caspase-7, thereby initiating extrinsic apoptotic responses [12].
Contrastingly, the intrinsic pathway—alternatively termed the mitochondrial-mediated pathway—is activated by endogenous stimuli such as hypoxia, DNA damage, ionizing radiation, and chemotherapeutic agents [13]. Under the influence of these stimuli, a dynamic imbalance between pro-apoptotic and anti-apoptotic members of the BCL-2 family is instigated, thereby triggering the intrinsic pathway [14]. BCL-2 family proteins, acting as key regulators in the intrinsic pathway, significantly modulate mitochondrial membrane permeability [15]. For instance, pro-apoptotic proteins (BAX, BAK, and BOK) and anti-apoptotic proteins (BCL-2, BCL-XL, and MCL-1) become activated during the apoptotic process, forming pores on the outer mitochondrial membrane, thereby releasing pro-apoptotic factors and inducing mitochondrial outer membrane permeabilization [16]. This permeabilization event subsequently elevates mitochondrial membrane permeability, facilitating the release of cytochrome c (Cyt-c) from the mitochondrial intermembrane space into the cytosol. Thereupon, Cyt-c forms a complex with pro-caspase-9 and APAF-1, generating the apoptosome complex, which further activates caspase-3 and caspase-7, thus inducing cellular apoptosis (Fig. 1).
Molecular mechanism diagram of apoptosis. Cellular apoptosis is induced through various external and internal pathways. Extrinsic apoptosis is triggered by the binding of death ligands (e.g., FasL, TNF-α) to their corresponding death receptors (e.g., Fas, TNF-R). This activates the death-inducing signaling complex (DISC), composed of FADD and TRADD, subsequently leading to the assembly of the DISC and death ligands. Caspase-8 is subsequently brought into close proximity and activated. This initial activation of caspase-8 triggers executioner caspases, specifically caspases-3 and -7, resulting in cellular apoptosis. Additionally, caspase-8 cleaves the protein Bid to produce tBid. The latter inhibits the anti-apoptotic protein Bcl-2 and induces the expression of pro-apoptotic proteins BAX/BAK, thereby promoting apoptosis. The permeabilization of the mitochondrial outer membrane (MOMP) serves as a critical step in apoptosis, leading to the release of intermembrane proteins such as cytochrome c. Cytochrome c forms a complex with Apaf-1, constituting the apoptosome, which in turn activates caspases-3 and -7, culminating in cellular apoptosis
Apoptosis in diabetic cardiomyopathy (DCM)
Both in vivo and clinical studies substantiate that cardiac cell apoptosis plays a pivotal role in the deterioration of cardiac function in diabetic patients. Critical target genes in the apoptotic process, such as pro-apoptotic genes caspase-3 and bax, and anti-apoptotic gene bcl-2, exert a crucial influence during the progression of DCM. For instance, one study demonstrated that the expression levels of caspase-3 and bax proteins were elevated in high-glucose (HG)-induced cardiomyocytes and in the hearts of DCM-induced rats, while the expression of the anti-apoptotic gene bcl-2 was diminished. Utilization of a specific caspase-3 inhibitor mitigated cellular apoptosis [2, 17]. Another study revealed that the p38MAPK and JNK signaling pathways serve as intermediaries in DCM-associated cellular apoptosis, and that HG-induced reactive oxygen species (ROS) could activate the MAPK signaling pathway, thereby promoting cardiomyocyte apoptosis [18]. Furthermore, Sirtuin 1 (SIRT1), a member of the Sirtuin family, displayed reduced expression in DCM rats and HG-induced cardiomyocytes. Enhancing its expression alleviated oxidative stress and inhibited cellular apoptosis in DCM [19]. Another study indicated that levels of SGLT1 were markedly elevated in the serum of diabetic patients as compared to non-diabetic subjects. Further research ascertained that the inhibition of SGLT1 led to a significant down-regulation of apoptotic markers, namely caspase-3 and bax, while upregulating the expression of anti-apoptotic protein bcl-2, thereby suggesting that the attenuation of apoptosis through SGLT1 inhibition could ameliorate cardiac function in DCM [18].
Endoplasmic reticulum (ER) stress and oxidative stress have been posited to play integral roles in the etiopathogenesis of DCM. In essence, persistent hyperglycemic stimulation induces ER stress, which in turn propels the cells toward apoptosis. Mechanistically, ER stress triggers the activation of caspase-12, which subsequently orchestrates the activation of downstream caspases, culminating in cellular apoptosis [21]. Additionally, multiple studies have confirmed that overactivation of the PI3K/AKT/mTOR signaling pathway may inhibit ERS and consequently suppress cellular apoptosis. Activation of the PI3K/Akt pathway promotes the phosphorylation of eNOS and mTOR. The activated eNOS further stimulates the production of nitric oxide (NO), a potent inhibitor of oxidative stress, thereby inhibiting cardiomyocyte apoptosis and exerting a protective effect in DCM [22]. Furthermore, heme oxygenase-1 (HO-1), an important signaling pathway in oxidative stress, mitigates cardiomyocyte apoptosis and ventricular remodeling in diabetic cardiomyopathy mouse models by activating the AKT/HO-1 signaling pathway, thereby exerting a cardioprotective role in DCM mice [23]. In summary, these findings indicate that cellular apoptosis is an empirically substantiated phenomenon in DCM and a significant contributor to the adverse outcomes of this disease. Future work necessitates a comprehensive and impartial analysis to identify key molecules exerting a specific impact on DCM.
Involvement of ncRNAs in cellular apoptosis in diabetic cardiomyopathy (DCM)
Modulatory influence of miRNAs on cardiomyocyte apoptosis in DCM
MiRNAs are small RNAs comprising fewer than 25 nucleotides, constituting less than 1% of the human genome. Predominantly localized in the cytoplasm, miRNAs function by directly binding to the 3' untranslated region (3'UTR) of target mRNA transcripts, thereby inhibiting the expression of specific genes. [24]. An escalating corpus of empirical evidence increasingly underscores the indispensable role of microRNAs (miRNAs) in orchestrating cellular apoptosis, thereby contributing to the etiopathogenesis and subsequent progression of Diabetic Cardiomyopathy (DCM). For example, exposure to elevated concentrations of glucose (HG) conspicuously elicits the upregulation of miR-34a in AC16 cardiomyocytes. Effective mitigation of HG-induced apoptosis in AC16 cells can be achieved through transfection with miR-34a inhibitory molecules. Furthermore, SIRT1 has been identified as a direct downstream target of miR-34a, a molecule with salient involvement in cardiomyocyte apoptosis. Through the downregulation of SIRT1, miR-34a thus exerts a pro-apoptotic effect on cardiomyocytes [25]. In addition, the transfection of AC16 cells with miR-34a mimetics significantly accentuates apoptosis and concurrently attenuates bcl-2 luciferase enzymatic activity. These findings collectively indicate that miR-34a modulates cellular apoptosis in DCM via its influence on multiple target genes [26]. In a parallel vein, miR-410-5p is found to be overexpressed in the myocardial tissue of DCM-afflicted rats as well as in HG-induced cardiomyocytes. Importantly, the application of miR-410-5p inhibitors engenders an upregulation of bcl-2, concomitant with the suppression of bax and caspase-3 expression levels. Such evidence posits that miR-410-5p downregulation might serve as an efficacious strategy for averting cardiomyocyte apoptosis. Subsequent inquiries identified PIM1 as a direct target of miR-410-5p, further implicating miR-410-5p in the promotion of cardiomyocyte apoptosis via the negative modulation of PIM1 [27]. Likewise, miR-483-3p experiences augmented expression in both streptozotocin (STZ)-induced diabetic mice and HG-induced cardiomyocytes. Concomitantly, a decrease is observed in the expression levels of its putative target gene, IGF1. These observations collectively substantiate the notion that miR-483-3p promotes cardiomyocyte apoptosis both in vitro and in vivo through the downregulation of anti-apoptotic proteins such as bcl-2 and IGF1 [28].
In contrast to the above-discussed miRNAs, which promote cardiomyocyte apoptosis in DCM by targeting specific mRNAs, certain miRNAs serve to counteract this apoptotic effect. For instance, a study delineated that miR-29a is underexpressed in both streptozotocin (STZ)-induced DCM in rats and high-glucose (HG)-induced H9C2 cells. Induction of miR-29a expression led to the inhibition of pro-apoptotic genes such as bax, caspase-3, and bak1, while simultaneously enhancing the expression of anti-apoptotic genes like bcl-2 and mcl-1. Further analysis identified the 3' untranslated region (UTR) of bak1 as a direct target of miR-29a, demonstrating that the overexpression of miR-29a mitigates cardiomyocyte apoptosis via the negative regulation of Bak1 [29]. A separate investigation illustrated that overexpression of miR-20a-5p attenuates cardiac dysfunction and HG-induced cardiomyocyte apoptosis in DCM rats. Moreover, the co-transfection with ROCK2 nullified the protective effects of miR-20a-5p overexpression on the heart, substantiating that miR-20a-5p exerts its anti-apoptotic and anti-inflammatory effects via targeting ROCK2 [30]. Similarly, miR-223 exhibits elevated expression levels in DCM and has been empirically substantiated, both in vitro and in vivo, to markedly impact cardiac fibrosis, activation of the NLRP3 inflammasome, and cellular apoptosis in DCM. Cumulative evidence from our research affirmatively suggests that the inhibition of miR-223 confers a significant protective effect against DCM, positing miR-223 as a potential therapeutic target [31]. Lastly, research conducted by Liu et al. ascertained that miR-186-5p is downregulated in HG-induced cardiomyocytes. The overexpression of miR-186-5p reverses HG-induced apoptosis, specifically impacting the expression of the pro-apoptotic protein caspase-3. Additionally, TLR3 has been corroborated as a direct target of miR-186-5p and is negatively regulated by it. In sum, miR-186-5p mitigates HG-induced cardiomyocyte apoptosis via modulating TLR3 expression [32].
LncRNAs and cardiomyocyte apoptosis in diabetic cardiomyopathy (DCM)
LncRNAs are a class of ncRNAs exceeding 200 nucleotides in length but lacking coding potential. Unlike miRNAs, which are solely localized in the cytoplasm, lncRNAs are present in both the cytoplasm and the nucleus. In the nucleus, lncRNAs can interact with transcription factors, thereby disrupting protein-coding genes. In the cytoplasm, they act as miRNA sponges, indirectly modulating cellular death processes. Additionally, lncRNAs directly target key genes and proteins involved in cellular apoptosis [33, 34]. For instance, MALAT1, one of the lncRNAs abundantly expressed in cardiomyocytes, demonstrates upregulated expression in both DCM rat hearts and high-glucose (HG)-induced cardiomyocytes. Silencing of MALAT1 significantly mitigates HG-induced cardiomyocyte apoptosis. Mechanistically, MALAT1 functions as a miRNA sponge for miR-185-5p and activates the RhoA/ROCK signaling pathway, thereby mediating HG-induced cardiomyocyte apoptosis [35]. Moreover, MALAT1 serves as a competing endogenous RNA (ceRNA) and prevents the binding of miR-181a-5p to p53, thus promoting cardiomyocyte apoptosis [36]. Further research by Tang et al. illustrates that another lncRNA, H19, is highly expressed in both DCM rat hearts and HG-induced cardiomyocytes. H19 serves as a molecular sponge for miR-29c and downregulates MAPK13 expression, thereby ameliorating cardiomyocyte apoptosis in DCM [37]. Similarly, under hyperglycemic conditions, the lncRNA GAS5 is upregulated in both in vivo and in vitro models of DCM. Inhibition of GAS5 expression significantly improves cardiac function and attenuates HG-induced cardiomyocyte apoptosis. Furthermore, through an amalgam of bioinformatics prediction, luciferase reporter assays, and RNA immunoprecipitation assays, miR-26a/b-5p was definitively identified as a target of GAS5. The silencing of GAS5 exerts a protective effect against cardiac fibrosis and HG-induced cardiomyocyte damage by negatively regulating miR-26a/b-5p [38].
LncRNAs exhibit bifunctionality; not only do some serve as molecular sponges for miRNAs but they also actively contribute to cardiomyocyte apoptosis in DCM. For instance, Zhao et al. discovered that both KCNQ1OT1 and PDCD4 are upregulated in HG-treated human cardiomyocytes and STZ-induced DCM mice, while miR-181a-5p was downregulated. The authors further delineated that KCNQ1OT1 functions as a competing endogenous RNA (ceRNA), elevating PDCD4 expression by sponging miR-34a, thereby promoting cardiomyocyte apoptosis in DCM [39]. A study by Wang et al. corroborated that MALAT1 is highly expressed in db/db mice and HG-induced cardiomyocytes. Silencing of MALAT1 manifested an ameliorative impact on both in vivo and in vitro cardiac function while inhibiting cardiomyocyte apoptosis. Additionally, MALAT1 was found to interact with EZH2 in cardiomyocytes, EZH2, in turn, modulates ABCA1 expression through repression of miR-22. MALAT1 promotes cardiomyocyte apoptosis by recruiting EZH2 to downregulate miR-22 expression, highlighting the role of the MALAT1/miR-22/EZH2/ABCA1 signaling cascade in cardiomyocyte damage and apoptosis [40]. According to research by Chen et al., lncRNA MEG3 is overexpressed in HG-treated AC16 cells. Knockout of MEG3 attenuated HG-induced AC16 cell apoptosis. Mechanistically, MEG3 directly interacts with miR-145 in AC16 cells, subsequently upregulating PDCD4 expression, thereby mitigating HG-induced cardiomyocyte apoptosis [41]. Zhou et al. elucidated that MIAT may function as a ceRNA by sponging miR-22-3p to upregulate DAPK2 expression, thereby contributing to cardiomyocyte apoptosis and implicating its role in the pathogenesis of DCM [42].
Apart from functioning as miRNA sponges to indirectly modulate cell death, certain lncRNAs also directly influence proteins associated with apoptosis in the progression of DCM. Multiple studies indicate that the hyperactivation of the PI3K/AKT/mTOR signaling pathway can inhibit endoplasmic reticulum stress (ERS) and cellular apoptosis. Through both in vivo and in vitro investigations, Wang et al. found that lncRNA H19 ameliorates diabetic cardiomyopathy-induced endoplasmic reticulum stress by activating the PI3K/AKT/mTOR signaling pathway, thereby inhibiting ERS-induced cellular apoptosis [22].
Involvement of circRNAs in cardiomyocyte apoptosis and the progression of diabetic cardiomyopathy (DCM)
CircRNAs represent a distinct class of single-stranded ncRNAs. Compared to miRNAs and lncRNAs, the covalently closed-loop structure of circRNAs enhances their stability. They exert regulatory effects by sequestering miRNAs, thereby influencing subsequent transcriptional control. Furthermore, circRNAs serve as sponges for RNA-binding proteins (RBPs) and facilitate the translation of target mRNA transcripts [43, 44]. In recent years, numerous circRNAs have been implicated in the progression of DCM by modulating cellular apoptosis. CircRNA CDR1as has been identified to exhibit elevated expression levels in DCM murine models and in cardiomyocytes induced by high glucose (HG). Knockout of CDR1as has been shown to downregulate the expression of apoptosis-related proteins, such as Bad and Caspase 3. Mechanistically, the silencing of CDR1as promotes ubiquitination of MST1, thereby inhibiting its expression. This culminates in a downstream cascade that decreases the levels of effector molecules LATS2 and p-YAP, ultimately ameliorating cardiac function in DCM mice and mitigating HG-induced cardiomyocyte apoptosis [45]. In a parallel line of inquiry, a significant negative correlation between circHIPK3 and PTEN has been reported in DCM patients. Subsequent in vitro investigations substantiated that overexpression of circHIPK3 attenuates the expression of PTEN in AC16 cells, thereby safeguarding the cells against HG-induced apoptosis (Fig. 2; Table 1) [46].
Mechanism diagram of non-coding RNA regulating apoptosis and intervening DCM. In DCM, cellular apoptosis is associated with dysregulation of ncRNAs. MiRNA modulates the progression of DCM by regulating the expression of apoptotic proteins. LncRNA and circRNA act either as miRNA sponges or as miRNA precursors to modulate the expression of apoptotic proteins. SIRT1:Silent information regulator 3,Bax-1:BCL2-associated X protein 1,Bcl-2:B-cell lymphoma 2,ROCK2:Rho-associated protein kinase 2,PIM1:Polymers of intrinsic microporosity,TLR3:Toll-like receptors 3,NLRP3:NOD-like receptor family pyrin domain containing 3,MALAT1:Metastasis-associated lung adenocarcinoma transcript 1,P53:Cellular tumor antigen p53,ABCA1:ATP binding cassette protein 1,MAPK13:Mitogen-activated protein kinase 13,PI3K/AKT:phosphatidylinositol 3-kinase/ protein kinase B,MEG3:Maternally expressed gene 3,KCNQIOT1:Potassium voltage-gated channel subfamily Q member 1 opposite strand 1,PDCD4:Programmed cell death protein 4,LATS2:Large tumor suppressorkinase2,MST1:Mammalian sterile 20-like kinase 1,PYAP:Phosphorylated yes-associated protein, PTEN:Phosphatase and Tensin Homologue
Autophagy and diabetic cardiomyopathy
Overview of autophagy
Autophagy represents a highly regulated intracellular catabolic process that operates both in the pathophysiological and physiological contexts within cellular systems. Typically, the activation of autophagy is provoked by factors such as nutrient deprivation and oxidative stress. Furthermore, this cellular mechanism is intricately associated with an array of physiological and pathological processes, including but not limited to development, differentiation, neurodegenerative disorders, stress responses, infection, and neoplasia [47].Depending on the mode of lysosomal delivery, autophagy can be categorized into three principal forms: microautophagy, chaperone-mediated autophagy (CMA), and macroautophagy [48]. Microautophagy primarily targets cellular organelles such as mitochondria, the nucleus, and peroxisomes. This mechanism entails the direct fusion of the lysosomal membrane with the substrate slated for degradation, thereby maintaining organelle size, membrane homeostasis, and cellular survival under conditions of nitrogen limitation [49]. Chaperone-mediated autophagy, conversely, represents a selective type of lysosomal degradation of cytosolic proteins within the cellular milieu [50]. The most extensively researched form of autophagy is macroautophagy, often referred to simply as autophagy for the purposes of this review [51].The autophagic process encompasses multiple sequential stages, namely initiation and nucleation, elongation, autophagosome formation, autolysosome formation, and ultimately degradation. This highly orchestrated cascade is mediated by a host of autophagy-related genes (ATGs) [52], as well as modulated by autophagy-associated signaling pathways, such as mTOR and AMPK. Although numerous scholarly reviews have elaborated on the molecular events involved in autophagy, we provide here only a cursory summary of the key steps. It is worth noting that moderate autophagy plays a salutary role in eliminating dysfunctional mitochondria that release reactive oxygen species and apoptosis-inducing factors, thereby mitigating cellular damage. Conversely, excessive activation of autophagy may precipitate unwarranted self-digestion and degradation of cellular components, leading to a form of programmed cell death known as autophagic cell death (Fig. 3).
Molecular mechanism diagram of autophagy. Activation of the insulin receptor stimulates the PI3K/AKT signaling pathway, subsequently promoting the expression of the autophagy regulatory factor mTOR, thereby inducing autophagy. AMPK serves as a key activator that inhibits mTOR, a negative regulator of autophagy. ULK1 functions as an autophagy-initiating kinase; AMPK triggers autophagy by directly inducing ULK1 phosphorylation and can also induce autophagy via Beclin-1. LC3 is indispensable for autophagy; the conversion of LC3-I to LC3-II indicates the induction of autophagy. ATG5 localizes on the outer membrane of autophagosomes and is critical for extension. p62 interacts with LC3-II and undergoes degradation along with its substrate, thereby delivering ubiquitinated proteins to the autophagosome for degradation to facilitate autophagy. TFEB is the principal transcriptional regulator of autophagy and lysosome biogenesis; its activation is vital for lysosomal homeostasis following lysosomal damage. GSK-3β promotes its phosphorylation and participates in the autophagy process
Autophagy in diabetic cardiomyopathy (DCM)
Autophagy is pivotal for cellular homeostasis and survival, and extant research has established its intimate association with the pathogenesis of Diabetic Cardiomyopathy (DCM). Prior studies have demonstrated an upregulation in the expression of autophagy-related proteins—namely LC3-I, LC3-II, and Beclin-1—in rat models of DCM. These proteins are considered crucial initiators of autophagic activation [53]. Furthermore, the upstream signaling pathways governing autophagy, specifically AMPK/mTOR, have been subjects of exhaustive inquiry. A burgeoning body of evidence elucidates the pivotal role these pathways play in the regulation of autophagy within the context of DCM. AMPK acts as the seminal activator that inhibits mTOR, which in turn serves as a negative regulator of autophagy [54]. In the course of DCM progression, attenuated activation of AMPK and heightened inhibition of mTOR contribute to diminished fatty acid oxidation and glucose uptake. These metabolic derangements culminate in cardiac lipotoxicity and lipomatous degeneration, thus exacerbating the advancement of DCM [55]. ULK1, functioning as an initiating kinase in autophagy, is situated downstream in the AMPK/mTOR signaling axis [56]. AMPK instigates autophagy by directly inducing phosphorylation of ULK1, thereby ameliorating glucose-induced myocardial damage and attenuating the incidence of DCM [57]. Consequently, targeting autophagy via AMPK activation or mTOR inhibition may represent a promising therapeutic intervention for DCM. Additionally, rat models of diabetic cardiac fibrosis have demonstrated a marked upregulation in the expression levels of phosphorylated PI3K and AKT, concomitant with decreased autophagic flux and a significant augmentation in apoptosis-related proteins. These findings suggest that the phosphorylation and excessive activation of the PI3K/AKT pathway may suppress autophagy and induce cellular apoptosis, thereby exacerbating myocardial fibrosis in diabetes [58].
Non-coding RNAs and autophagy in diabetic cardiomyopathy (DCM)
Role of miRNAs in autophagy within the context of DCM
MicroRNAs (miRNAs) exert regulatory control over autophagy in DCM by directly targeting autophagy-related genes. For instance, miR-494 is upregulated in the myocardium and cardiomyocytes of DCM rats induced by high-glucose (HG) conditions. Functionally, its overexpression amplifies HG-induced cellular apoptosis and autophagy. Mechanistically, miR-494 orchestrates these cellular processes by modulating the PI3K/AKT/mTOR signaling pathway, thereby mitigating myocardial cell damage following HG induction [59]. LAMP2, a transmembrane protein intricately associated with autophagy, is abundantly expressed in cardiac and skeletal muscle tissues, miR-207 can directly target LAMP2, inhibiting cardiomyocyte autophagy and thereby promoting apoptosis [60]. According to research by Ni et al., miR-34a expression is elevated in the myocardial tissue of diabetic mice and HG-induced cardiomyocytes, inhibiting its expression is beneficial for augmenting mitochondrial autophagy, eliminating damaged or aberrant mitochondria, and thereby maintaining cellular homeostasis [61]. Moreover, Nandi et al. employed transcriptomic sequencing to explore the role of miR-133a and the mTOR pathway in DCM. The inhibition of mTOR, a known autophagy suppressor, occurs through the downregulation of miR-133a, resulting in the upregulation of autophagy in diabetic heart failure patients. This finding suggests that miR-133a may offer a viable therapeutic strategy by modulating the mTOR signaling cascade to attenuate DCM progression [62]. Foxo3 is a crucial pro-autophagic factor in cardiomyocytes and has been identified as a potential therapeutic target for DCM associated with autophagy dysregulation. According to a study by Ucar et al., the overexpression of miR-212 leads to the downregulation of Foxo3, subsequently impairing basal autophagy at normal levels and inducing severe heart failure in mice [63].
Recent investigations have demonstrated that miR-21 is upregulated in the cardiac tissue of diabetic mice and HG-induced cardiomyocytes. Post-transfection with a miR-21 inhibitor, a pronounced increase in the protein levels of SPRY1 and a significant decrease in the levels of phosphorylated ERK and mTOR were observed. These data collectively indicate that miR-21 modulates autophagy via the SPRY1/ERK/mTOR signaling pathway [64]. Additionally, a study by Chen et al. revealed that the overexpression of miR-30c in db/db mice led to a decline in BECN1 levels and the LC3-II:I ratio, suggesting the suppression of autophagic flux, thereby potentially preserving cardiac function in diabetic db/db mice [65].
Involvement of long non-coding RNAs (lncRNAs) in autophagy in diabetic cardiomyopathy (DCM)
Emerging evidence delineates the contributory role of various lncRNAs in the orchestration of cellular autophagy, thereby implicating their significance in the pathophysiology of DCM. For instance, GAS5 is underexpressed in both streptozotocin (STZ)-induced diabetic rats and high-glucose (HG)-treated cardiomyocytes. The overexpression of GAS5 facilitates myocardial autophagy and subsequently ameliorates cardiac function in DCM by sponging miR-221-3p to upregulate P27 expression [66]. A study by Feng et al. revealed an upregulation of lncRNA DCRF in the myocardium of diabetic rats and HG-treated cardiomyocytes. Mechanistically, the knockdown of DCRF attenuates myocardial cell autophagy, alleviates myocardial fibrosis, and enhances cardiac function. This is mediated through the augmented inhibitory action of miR-551b-5p on PCDH17, thereby retarding the progression of myocardial autophagy and DCM [67]. Recently, multiple studies have substantiated the pivotal role of lncRNA H19 in modulating autophagy in the development of DCM. A study by Zhuo et al. reported the significant activation of autophagy-related proteins and autophagosomes, such as LC3-II, BECN1, and ATG7, in a streptozotocin-induced diabetic rat model; despite the reduced expression of H19 in the myocardium, its overexpression attenuates autophagy and ameliorates left ventricular dysfunction associated with hyperglycemia, and this regulatory effect is attributed to the interaction of H19 with PRC2, which epigenetically inhibits the transcription of DIRAS3, thereby mitigating autophagy in myocardial cells (Fig. 4; Table 2) [68].
Mechanism diagram of non-coding RNA regulating autophagy and intervening DCM. In the context of dilated cardiomyopathy (DCM), autophagy is related to the dysregulation of non-coding RNA (ncRNA). MicroRNA (miRNA) modulates the progression of DCM by regulating the expression of autophagy-related proteins. Long non-coding RNA (lncRNA) acts either as a miRNA sponge or as a miRNA precursor to modulate the expression of autophagy-associated proteins. PI3K/AKT/mTOR:phosphatidylinositol 3-kinase/ protein kinase B/ mammalian target of rapamycin,SPRY1:Sprouty 1,Foxo3:Forkhead box 3,P27:Cellular tumor antigen p27,LAMP2:lysosomal-associated membrane protein 2,DIRAS3:GTP-binding protein Di-Ras3,ATG7:Autophagy protein 7,GAS5:Growth arrest specific transcript 5,DCRF:DCM-related factor, PCDH17: Protocadherin 17
Pyroptosis and diabetic cardiomyopathy (DCM)
Overview of pyroptosis
In 2001, Cookson and Brennan identified a novel form of regulated cell death in macrophages infected with Salmonella typhimurium that was caspase-1-dependent, as opposed to caspase-3-dependent, this led them to coin the term “pyroptosis” to describe this unique modality of cell death [69]. Pyroptosis is characterized as a caspase-1-dependent form of programmed cell death with pro-inflammatory consequences. Morphologically, it bears similarities to both necrosis and apoptosis but is distinctly different in its hallmark features, which include the formation of transmembrane pores, cellular membrane swelling, rupture, and the release of pro-inflammatory contents [70]. In 2011, Kayagaki et al. discovered that pyroptotic cell death in macrophages infected with Escherichia coli was dependent on caspase-11 rather than caspase-1. They proposed this as an atypical inflammasome-driven pyroptotic pathway [71]. Subsequent studies conducted independently by Shi et al. and Kayagaki et al. in 2015 identified gasdermin D (GSDMD) as a critical downstream target of both caspase-1 and caspase-11 [70, 72]. Furthermore, as insights into the molecular mechanisms of pyroptosis have deepened, caspase-3, caspase-8, and GSDME have also been delineated as participating elements in the pyroptotic process [73].
According to the classification posited by Kayagaki et al., pyroptotic pathways can be dichotomized into the caspase-1-mediated canonical inflammasome pathway and the caspase-4/5/11-mediated non-canonical inflammasome pathway [71]. The initiation of the canonical inflammasome pathway is critically contingent upon the activation of classic inflammasomes, which are intimately associated with intracellular receptor proteins like NLRP1/3, NLRC4, and AIM2, with NLRP3 inflammasome research being the most extensively studied [70]. The NLRP3 inflammasome complex comprises the apoptosis-associated speck-like protein containing a CARD (ASC), NLRP3, and pro-caspase-1. It is principally activated through a two-step signaling process [74]. The first step predominantly involves recognition by pattern recognition receptors (PRRs) of pathogen-associated molecular patterns (PAMPs) present on the surface of toxins, viruses, and bacteria, or damage-associated molecular patterns (DAMPs) produced following tissue or cellular insult. Concomitantly, under PRR stimulation, the inflammasome complex autocatalytically cleaves pro-caspase-1 into its active form, caspase-1, which subsequently enzymatically processes pro-IL-1β and pro-IL-18 into their mature secreted forms, thereby instigating an inflammatory response [75]. The second step predominantly involves the activation of pro-caspase-1 into caspase-1 within the inflammasome. The activated caspase-1 cleaves GSDMD into its N-terminal (GSDMD-NT) and C-terminal (GSDMD-CT) fragments. The formation of membrane pores at the N-terminus ultimately precipitates the release of cytokines, efflux of potassium ions, cellular swelling, and lysis [76]. Moreover, mature IL-1β and IL-18 are generated from pro-IL-1β and pro-IL-18 through caspase-1 cleavage and are extracellularly discharged through GSDMD pores. This culminates in the recruitment of immune cells and the establishment of an inflammatory microenvironment, consequently instigating pyroptotic cell death [77].
Distinct from the caspase-1-mediated canonical inflammasome pathway, the non-canonical inflammasome pathway is principally orchestrated by caspase-11 in mice and caspase-4/5 in humans. These caspases can be directly activated by lipopolysaccharides (LPS), components of Gram-negative bacteria, thereby fulfilling functions analogous to those of caspase-1 [78]. It is well established that caspase-11 is indispensable for LPS-induced pyroptosis in murine cells [79], while caspase-4/5 serve a functionally comparable role in human cells. Intriguingly, within the ambit of the non-canonical inflammasome pathway, pyroptosis induced by activated caspase-4/5/11 does not directly catalyze the maturation of pro-IL-1β and pro-IL-18. Instead, it operationalizes this process indirectly through the activation of the NLRP3/ASC/caspase-1 axis, thereby facilitating the maturation and secretion of IL-1β and IL-18 [80]. In summary, both the caspase-1-mediated canonical inflammasome pathway and the caspase-4/5/11-mediated non-canonical inflammasome pathway converge functionally in the orchestration of pyroptotic cell death, sharing several key regulatory elements (Fig. 5).
Molecular mechanism diagram of Pyroptosis. In the canonical pathway, danger-associated molecular patterns (DAMPs) or pathogen-associated molecular patterns (PAMPs), as well as LPS stimulation, activate the TLR4/NF-κB classical signaling pathway. Subsequently, NLRP3 recruits the adaptor ASC, which in turn recruits procaspase-1, leading to the maturation and release of bioactive IL-1β and IL-18, culminating in pyroptosis. In the non-canonical pathway, LPS directly activates procaspase-4/5/11. Upon binding of procaspase-4/5/11 to LPS, it cleaves GSDMD into GSDMD-NT. The activation of caspase-4/5/11 can stimulate the Pannexin-1 channel, thereby releasing cellular ATP and prompting the opening of the cytoplasmic channel P2X7, ultimately leading to potassium ion efflux and triggering NLRP3-mediated pyroptosis
Pyroptosis in diabetic cardiomyopathy (DCM)
Inflammatory responses represent a pivotal pathological process in the progression of Diabetic Cardiomyopathy (DCM), with pyroptosis serving as a form of programmed cell death closely associated with inflammation and implicated in the development of DCM [81]. Initial observations employing electron microscopy have revealed the presence of swollen collagen fibers and mitochondrial characteristics in dying cardiomyocytes of diabetic rats and mice, which are morphologically congruent with pyroptotic events [82]. Recent investigations have accentuated the seminal role of NLRP3 inflammasomes in mediating cardiomyocyte pyroptosis in the context of DCM [83]. During the development of DCM, elevated glucose levels contribute to an increase in reactive oxygen species (ROS), which subsequently activate NF-κB and trigger the activation of NLRP3, culminating in the release of IL-1β and IL-18, thus promoting pyroptotic progression in DCM [84]. Emerging evidence substantiates that, in comparison to cardiac tissues from non-diabetic individuals, those from diabetic patients exhibit an upregulation of NLRP3 inflammasome activation and cardiomyocyte pyroptosis. Further investigations have elucidated that elevated glucose levels (35 mM glucose) significantly induce the expression of NLRP3, caspase-1, and IL-1β in human ventricular cardiomyocytes, accompanied by a marked occurrence of pyroptosis. These findings corroborate the unique role of NLRP3 inflammasome-mediated pyroptosis in the pathogenesis of DCM [85]. Additionally, according to a study by Luo et al., NLRP3 inflammasomes and caspase-1-mediated pyroptosis are expressed in the myocardium of diabetic rats, the inhibition of NLRP3 expression ameliorated cardiac inflammation, pyroptosis, and myocardial function [86].
Moreover, diverse cell types, including cardiac fibroblasts (CFs), cardiomyocytes, and endothelial cells, undergo pyroptosis upon stimulation by high glucose levels, inevitably exacerbating the onset and progression of DCM [7]. For instance, during DCM, NLRP3 inflammasomes exacerbate cardiac fibrosis and promote the activation of CFs induced by elevated glucose [87]. In the context of DCM progression, CFs are activated and transdifferentiate into myofibroblasts under hyperglycemic (HG) conditions; concurrently, inflammasomes within CFs are activated, facilitating the production of IL-1β and IL-18 [88, 89]. Similarly, a hyperglycemic environment promotes the hyperactivation of NLRP3 in cardiomyocytes. The activated NLRP3 assembles with ASC and pro-caspase-1 to form inflammasomes, inducing the activation of GSDMD-N, pore formation on the cell membrane, and the subsequent maturation and secretion of IL-18 and IL-1β, ultimately leading to cardiomyocyte pyroptosis and the accelerated progression of DCM [90]. Furthermore, it is worth noting that endothelial cell pyroptosis is implicated in the developmental course of DCM. Elevated glucose levels induce the formation and activation of NLRP3 inflammasome complexes in mouse coronary artery endothelial cells; silencing of NLRP3 expression resulted in a near disappearance of caspase-1 activity [91], indicating that high-glucose-induced NLRP3 inflammasomes contribute to endothelial cell dysfunction. In summary, the NLRP3 inflammasome and its associated induction of pyroptosis manifest a unique role in DCM, offering potential therapeutic targets for its treatment through the inhibition of pyroptotic signaling pathways. However, research related to DCM is still in its nascent stage, and numerous questions await further exploration.
Non-coding RNAs (ncRNAs) and pyroptosis in diabetic cardiomyopathy (DCM)
MicroRNAs (miRNAs) and pyroptosis in DCM
Copious empirical evidence underscores the pivotal role of microRNAs (miRNAs) in modulating pyroptosis through a multifaceted repertoire of mechanisms. For example, in cardiomyocytes subjected to high-glucose (HG) treatment, miR-214-3p demonstrates a significant downregulation. Augmenting the expression of this miRNA has been shown to attenuate the levels of critical pyroptosis-associated markers such as NLRP3, caspase-1, and IL-1β, thereby substantially mitigating HG-induced cardiomyocyte pyroptosis [92]. In the same vein, Foxo3a and ARC, integral transcription factors in regulating cellular apoptosis, manifest notable downregulation in HG-induced cardiomyocytes. Intriguingly, miR-30d efficaciously represses Foxo3a and ARC expression both in vivo and in vitro. This downregulation culminates in an elevated expression of caspase-1 and pro-inflammatory cytokines IL-1β and IL-18, which subsequently impede HG-induced cardiomyocyte pyroptosis [93]. In a seminal study led by Prince Jeyabal et al., ELAVL1 is identified as a prospective molecular target of miR-9. Inhibition of miR-9 results in a consequential elevation of ELAVL1 protein expression, alongside an upregulation of caspase-1 and IL-1β, thereby inhibiting the pyroptosis of HG-treated cardiomyocytes [85]. Moreover, the miR-18a-3p/GSDMD signaling axis is modulated by berberine, an inherently anti-DCM (Diabetic Cardiomyopathy) compound extracted from traditional herbal medicine. Berberine has been shown to inhibit pyroptosis in HG-treated H9C2 cells via this signaling axis, thereby retarding the progression of DCM [94]. Analogous to the aforementioned studies, lenalidomide is reported to stimulate the expression of miR-135b in cardiac fibroblasts under HG conditions, this miRNA directly interacts with caspase-1, and its overexpression inhibits the levels of IL-1β and GSDMD, thereby constraining cardiac fibroblast pyroptosis and diminishing collagen deposition [95].
In a compelling departure, certain miRNAs serve to promote the development of DCM by facilitating cardiomyocyte pyroptosis. A study by Peng et al. unveils miR-21-3p as an activator of pyroptosis, its overexpression leading to an augmented accumulation of NLRP3 and caspase-1 in both STZ-induced diabetic cardiac fibrotic tissue and HG-treated cardiac fibroblasts, thus accelerating HG-induced cardiac fibroblast pyroptosis [96]. Further corroborating this paradigm, a study by Zhao et al. discloses an upregulation of miR-223-3p in HG-treated cardiomyocytes, concomitant with an elevated SPI1 expression. Transfection with a miR-223-3p inhibitor induces a subsequent SPI1 downregulation and attenuates the expression levels of NLRP3, GSDMD-N, caspase-1, and IL-1β. These findings substantiate that miR-223-3p exacerbates DCM progression by inducing cardiomyocyte pyroptosis through upregulating SPI1 [97].
lncRNAs and cellular pyroptosis in diabetic cardiomyopathy (DCM)
Emerging data over the past few years increasingly substantiate the pivotal role of long non-coding RNAs (lncRNAs) as crucial regulators in cellular pyroptosis. For instance, according to a study by Xiong et al., the expression levels of pyroptosis-associated proteins, such as NLRP3, caspase-1, IL-1β, and IL-18, are markedly upregulated in high-glucose (HG) treated cardiomyocytes. However, following the transfection of HOTAIR plasmid, the lncRNA interacts with FUS to activate SIRT3 expression, resulting in the downregulation of NLRP3, caspase-1, IL-1β, and IL-18, subsequently attenuating cellular pyroptosis in DCM [98].
A multitude of studies have corroborated that various lncRNAs, including MIAT, MALAT1, GAS5, and kcnq1ot1, partake in the pathophysiological progression of DCM by modulating cellular pyroptosis. Prior investigations revealed that lncRNA MIAT is implicated in diverse pathological mechanisms such as microvascular dysfunction, myocardial ischemia–reperfusion injury, and diabetes. Recent findings demonstrate elevated MIAT expression both in the serum of diabetic patients and in HG-induced cardiomyocytes, as well as in the serum of diabetic mice. Both in vivo and in vitro silencing of MIAT ameliorate cellular pyroptosis in DCM. Mechanistically, MIAT acts as a competitive endogenous lncRNA, and it inhibits miR-214-3p, which in turn regulates the expression of its downstream target CASP1. The regulation of pyroptosis in diabetic cardiomyopathy by lncMIAT may thus be orchestrated through targeting the MIAT/miR-214-3p/CASP1 axis [92]. Similarly, MALAT1 expression surges in HG-treated cardiomyocytes. Upon MALAT1 knockdown, levels of pyroptosis-related proteins such as ASC, GSDMD-N, caspase-1, and NLRP3 are diminished, accompanied by an increase in GSDMD and miR-141-3p expression, suggesting that MALAT1 might participate in DCM pathogenesis by targeting miR-141-3p and regulating the expression of pyroptosis-related proteins [99]. Furthermore, GAS5 is found to be underexpressed in the cardiac tissues of DCM mice and in HG-induced HL-1 cells. Overexpression of GAS5 suppresses NLRP3, caspase-1, Pro-caspase-1, IL-1β, and IL-18, thereby improving cardiac function. Subsequent studies reveal that GAS5 functions as a competing endogenous RNA that ‘sponges’ miR-34b-3p to facilitate AHR expression, thereby inhibiting NLRP3 inflammasome-mediated pyroptosis and ameliorating DCM [100]. Kcnq1ot1, a widely investigated lncRNA, exhibits augmented expression in diabetic patients, in HG-induced AC16 cardiomyocytes, and in cardiac tissues of diabetic mice. Silencing Kcnq1ot1 suppresses caspase-1 through miR-214-3p in cardiomyocytes, thereby inhibiting cellular pyroptosis [101].
CircRNAs and cellular pyroptosis in diabetic cardiomyopathy (DCM)
Recent investigations have illuminated the instrumental role circRNAs play in the progression of DCM, predominantly acting as molecular sponges for miRNAs via the competing endogenous RNA (ceRNA) mechanism to modulate downstream gene expression and target cellular pyroptosis. According to a study by Fu et al., circ_0071269 was observed to be significantly upregulated in high-glucose (HG)-treated H9c2 cells, the overexpression of circ_0071269 facilitates pyroptosis in DCM cells by sponging and upregulating miR-145, which in turn augments the expression of GSDMA [102]. Employing bioinformatic prediction methodologies, Yang and colleagues identified circRNA CACR, subsequent experiments corroborated its elevated expression in both HG-treated cardiomyocytes and the serum of diabetic patients. Mechanistically, the silencing of CACR significantly mitigates HG-induced cellular pyroptosis. CACR operates as a competing endogenous RNA and its silencing is proposed to sponge miR-214-3p, thereby inhibiting the expression of caspase and attenuating cellular pyroptosis in DCM [103].
In addition to its role as a miRNA sponge, circRNAs have also been found to exert direct influence on gene expression, thus contributing to the pathological progression of DCM. For example, in a study conducted by Yuan et al., pyroptosis-related proteins such as GSDMD, ASC, NLRP3, and caspase-1 were substantially activated in both in vivo models of Type 2 Diabetes Mellitus (T2DM) and in vitro cardiomyocytes treated with AGEs (Advanced Glycation End-products). The overexpression of circRNA DICAR significantly inhibited the activation of these pyroptosis-related proteins. Moreover, further clinical trials have indicated that DICAR expression levels in diabetic patients were considerably lower than those in healthy controls. This concurs with the downregulation of DICAR in the cardiac tissues of diabetic mice, suggesting that DICAR overexpression could potentially serve as a novel therapeutic target for the inhibition of cardiomyocyte pyroptosis and the subsequent amelioration of diabetic cardiomyopathy (Fig. 6; Table 3) [104].
Mechanism diagram of non-coding RNA regulating pyroptosis and intervening DCM. In the context of DCM, microRNA (miRNA) modulates the progression by regulating the expression of pyroptotic proteins. Long non-coding RNA (lncRNA) and circular RNA (circRNA) either act as miRNA sponges or function as miRNA precursors to regulate the expression of proteins involved in pyroptosis.NLRP3:NLR family pyrin domain containing 3,Foxo3a:Forkhead box 3a,ARC:Activity regulated cytoskeleton,SPI1:Salmonella pathogenicity island 1,GSDMD:Gasdermin D,IL-1 β:interleukin‐1β,IL-18:interleukin-18,GAS5:Growth arrest specific transcript 5,KCNQIOT1:Potassium voltage-gated channel subfamily Q member 1 opposite strand 1,MIAT:Myocardial infarction associated transcript, HOTAIR:Hox transcript antisense intergenic RNA
Ferroptosis and diabetic cardiomyopathy (DCM)
Overview of ferroptosis
Ferroptosis, a distinct iron-dependent regulated form of cellular death, was initially identified and characterized by Dixon et al. in 2012 [105]. Morphologically divergent from other modalities of cell death, ferroptosis is principally characterized by intact cellular nuclei, reduced mitochondrial size and cristae, along with mitochondrial membrane rupture [106]. The hallmark biochemical features of this form of cell death are the accumulation of free iron and reactive oxygen species (ROS), and it is intricately linked with iron metabolism, lipid peroxidation, and compromised antioxidative defense systems [107]. Below, we elucidate the specific mechanisms underpinning ferroptosis.
Iron is an indispensable trace element pivotal for maintaining cellular energy metabolism. In biological systems, it predominantly exists in its Fe2+ and Fe3+ states, participating in a plethora of metabolic pathways [108]. Under physiological conditions, the Transferrin Receptor 1 (TFR1) recognizes Fe3+ by binding to free transferrin (TF) on the cell membrane, which is then reduced to Fe2+ under the action of ferrireductases [109]. Subsequently, Divalent Metal Transporter 1 (DMT1) shuttles Fe2+ into the cytoplasmic Labile Iron Pool (LIP) for participation in various metabolic processes. Excessive iron is stored in the form of Fe3+ within ferritin or exported out of the cell via Ferroportin (FPN) [110, 111]. The Fe2+ within the LIP not only induces ferroptosis through the synthesis of key lipid peroxidation enzymes like Lipoxygenases (LOXs) but also participates in Fenton reactions with hydrogen peroxide, generating hydroxyl radicals that target cellular components and thereby cause ferroptosis [112]. Ferritin, as a primary iron storage protein complex, undergoes autophagic degradation in the cytoplasm or lysosomes, a process referred to as ferritinophagy. This, in turn, leads to elevated cellular iron levels, resulting in unstable iron overload, subsequent lipid peroxidation, and accumulation of ROS, thereby precipitating ferroptosis [113]. Furthermore, the Nuclear Receptor Coactivator 4 (NCOA4) serves as a crucial receptor in the ferritinophagy process and plays an indispensable role in maintaining iron homeostasis. The silencing of NCOA4 expression can inhibit ferritinophagy, thus averting iron overload, lipid peroxidation, and ferroptosis [114, 115].
Lipid peroxidation is a cardinal step in the cascade of events constituting ferroptosis, operating as a free-radical mediated reaction. The primary substrates involved in this process are polyunsaturated fatty acids (PUFA). Phospholipids with PUFA as substrates undergo transformation into lipid hydroperoxides under the enzymatic influence of Acyl-CoA Synthetase Long-Chain Family Member 4 (ACSL4) and Lysophosphatidylcholine Acyltransferase 3 (LPCAT3). Moreover, Fe2+ contributes to the Fenton reaction with lipid hydroperoxides, engendering toxic lipid radicals [116, 117]. These toxic lipid radicals are capable of inflicting cellular damage, thereby precipitating ferroptosis. Additionally, Nuclear Factor Erythroid 2-Related Factor 2 (NRF2), a quintessential regulatory element in cellular antioxidative stress responses, translocates to the nucleus to instigate the transcription of genes containing antioxidant response elements (ARE). The NRF2 pathway mitigates PUFA oxidation, attenuating lipid peroxidation, and ultimately inhibiting ferroptosis [118]. Furthermore, enzymatic reactions mediated by Arachidonate Lipoxygenase (ALOXs) or Cytochrome P450 Oxidoreductase (POR) have also been shown to accelerate lipid peroxidation, thereby inducing ferroptosis [119].
The deactivation of intracellular oxidative defense mechanisms leads to the insufficient clearance of lipid peroxides, resulting in their extensive accumulation within the cell and the subsequent onset of ferroptosis. The Cystine/Glutamate Antiporter System (System Xc-) serves as a salient antioxidative system within the cell. Composed of two subunits, SLC7A11 and SLC3A2, which are ubiquitously distributed across the cell membrane, cystine and glutamate are reciprocally exchanged intracellularly and extracellularly via System Xc- [112]. Thus, by inhibiting the activity of System Xc-, the uptake of cystine can be obstructed, consequently impairing the synthesis of Glutathione (GSH) and reducing the activity of Glutathione Peroxidase 4 (GPX4). This, in turn, compromises cellular antioxidative capabilities [120]. Additionally, p53 downregulates SLC7A11 expression, thereby attenuating the uptake of cystine by the System Xc- across the organism. This results in the deactivation of cystine-dependent Glutathione Peroxidase, culminating in lipid peroxidation and ferroptosis (Fig. 7) [121].
Molecular mechanism diagram of ferroptosis. Free PUFA can be converted into PUFA-phospholipids (PUFA-PL) via ACSL4 and LPCAT3 enzymes. When PUFA-PLs undergo oxidation to lipid peroxides under the influence of arachidonate lipoxygenases (ALOXs), this triggers ferroptosis within the cell. AIFM2, a Coenzyme Q10 (CoQ10) oxidoreductase, functions in a parallel pathway with GPX4 to mitigate lipid peroxidation. GPX4 converts glutathione (GSH) to its oxidized form (GSSG), and the GSH/GSSG system acts as an antioxidant mechanism that inhibits ferroptosis by reducing reactive oxygen species (ROS). Intracellular iron in the form of Fe2 + is transported by transferrin and stored in an unstable iron pool as ferritin (FTH and FTL). C-reactive protein captures and oxidizes it to Fe3 + , which binds with transferrin (TF) and transferrin receptor (TFR) in the circulatory system. NCOA1 mediates autophagic degradation of ferritin in the lysosome, promoting the release of Fe2 + . Excess Fe2 + undergoes Fenton reaction with hydrogen peroxide, leading to lipid peroxidation and subsequent ferroptosis. Additionally, in the GCH1 protective pathway, GCH1 serves as the rate-limiting enzyme for the biosynthesis of tetrahydrobiopterin (BH4), and also regulates pantothenate levels
Role of ferroptosis in diabetic cardiomyopathy (DCM)
Ferroptosis, recognized as a novel form of regulated programmed cell death, plays an indispensable role in the pathogenesis and progression of Diabetic Cardiomyopathy (DCM). Studies have ascertained that systemic iron overload not only precipitates the onset of Type 2 Diabetes Mellitus (T2DM) and exacerbates the risk of insulin resistance, but also amplifies cardiovascular complications via the Fenton reaction [122]. Additional research indicates that elevated glucose levels in diabetic patients lead to an augmentation of Advanced Glycation End-products (AGEs). These terminal metabolites facilitate intracellular lipid accumulation and the ensuing lipotoxicity [123]. Subsequent studies delineate that both AGEs and intracellular lipid accumulation culminate in the excessive production of reactive oxygen and nitrogen species, thereby catalyzing the onset and progression of DCM [124]. Moreover, investigations in myocardial tissue from murine models of T2DM-induced DCM and rats with Heart Failure with Preserved Ejection Fraction (HFpEF) reveal an inhibited Xc-/GSH/GPX4 axis, accompanied by an overexpression of Transferrin Receptor 1 (TFR1) and Ferritin Heavy Chain (FTN-H) [125]. Furthermore, the expression levels of Nuclear Factor Erythroid 2-Related Factor 2 (NRF2), SLC7A11, and Glutathione (GSH) were observed to be significantly downregulated in myocardial tissue treated with AGEs and in murine models of DCM. The diminished expression of these ferroptosis-associated proteins compromises cellular functionality and intensifies lipid peroxidation, thereby engendering ferroptosis and serving as a pivotal pathogenic factor in the development of DCM [126].
Interplay between ncRNA and ferroptosis in diabetic cardiomyopathy (DCM)
Recent investigations underscore the pivotal role of long non-coding RNA (lncRNA)-mediated regulation of ferroptosis in the progression of DCM. Ni et al. delineated that in the left ventricular myocardial tissue of db/db mice and high-glucose (HG)-treated cardiomyocytes, lncRNA ZFAS1 was markedly upregulated, concomitant with an increase in ferroptosis. The inhibition of ZFAS1 was found to restore the expression levels of Ferritin Heavy Chain 1 (FTH1) and Glutathione Peroxidase 4 (GPX4), as well as to attenuate the expression of 4-Hydroxynonenal (4-HNE). Subsequent studies revealed that ZFAS1 inhibition potentially ameliorates cardiomyocyte ferroptosis by sponging miR-150-5p to activate Cyclin D2 (CCND2), thereby mitigating ferroptotic cardiomyocyte death and attenuating DCM progression [127].Currently, research pertaining to lncRNA-mediated regulation of ferroptosis in DCM is rather limited and predominantly confined to cellular and molecular experiments; thus, there is a conspicuous dearth of clinical studies. Future endeavors should integrate both clinical and molecular investigations to broaden the scope of DCM-related research. Moreover, microRNA (miRNA) and circular RNA (circRNA) have been established as critical regulatory factors in ferroptosis [128, 129]. However, extant evidence concerning the role of miRNA and circRNA in modulating ferroptosis during the progression of DCM remains scant. Subsequent lines of inquiry should prioritize the elucidation of the mechanistic roles of miRNA and circRNA in the targeted regulation of ferroptosis within the context of DCM.
Necroptosis and diabetic cardiomyopathy (DCM)
Overview of necroptosis
Necroptosis was initially identified by Degterev and colleagues in 2005 as a unique form of cell death governed by a signaling cascade that could be inhibited by necrostatin-1 (Nec-1) [130]. In 2018, the Nomenclature Committee on Cell Death formally designated this caspase-independent mode of cell death as "necroptosis" [131]. This phenomenon amalgamates characteristics of both necrosis and apoptosis, primarily manifesting as cellular volume augmentation, organelle swelling, membrane integrity disruption, and ultimate activation of cellular disintegration [132]. Necroptosis can be induced by a multitude of factors, including Tumor Necrosis Factor α (TNF-α), Fas ligand (FASL), TNF-Related Apoptosis-Inducing Ligand (TRAIL), Interferon-γ (IFN-γ), lipopolysaccharides (LPS), double-stranded RNA (dsRNA), and viral infections. Among these, the pathway mediated by TNF-α/TNF Receptor 1 (TNFR1) has been most extensively scrutinized [133]. Preliminary investigations reveal that TNF-α, upon binding to its membrane receptor TNFR1, instigates a conformational change in the TNFR1 trimer. Subsequently, TNFR1 recruits a multitude of proteins, including RIPK1/3, TRADD (TNFR-Associated Death Domain), cIAP1 (Cellular Inhibitor of Apoptosis Protein 1), cIAP2, and TRAF2/5 (TNFR-Associated Factors 2/5), to form a supramolecular structure termed “Complex I” [134]. Within Complex I, RIPK1 plays a dual role in modulating cellular survival and death. On one hand, its ubiquitination by cIAP1/2 enhances Complex I stability, thus activating the nuclear factor kappa B (NF-κB) pathway and promoting cellular survival. On the other hand, its deubiquitination by cylindromatosis (CYLD) leads to inhibition of the NF-κB pathway, thereby activating the cell death signaling cascade and enhancing the cell’s susceptibility to necroptosis [135, 136]. Moreover, deubiquitinated RIPK1, under the influence of CYLD, dissociates from Complex I, leading to the formation of Complex IIb, which includes FADD, pro-caspase-8, RIPK3, and RIPK1. This promotes the activation of caspase-8 and initiates cellular apoptosis [137, 138]. However, when the activity of caspase-8 is suppressed by caspase inhibitors such as zVAD or FLICE inhibitory protein (FLIP), Complex IIb transmutes into a necrosome, thereby inducing necroptosis (Fig. 8) [139].
Molecular mechanism diagram of necroptosis. Upon binding with its receptor TNFR, TNF-α recruits a cohort of proteins, including TRADD, RIPK1, and TRAF2/5, to form Complex I. Ubiquitination of RIPK1 in the upstream pathway activates NF-κB signaling. Complex I can subsequently evolve into Complex II, consisting of caspase-8, TRADD, RIPK1, and RIPK3. RIPK1 undergoes autophosphorylation, enabling its RHIM domain to bind with RIPK3 and form filamentous heterodimeric scaffolds known as necrosomes. Necrosomes recruit additional RIPK3, mediating its homodimerization, autophosphorylation, and activation, eventually leading to the phosphorylation of MLKL, which culminates in membrane rupture and necroptotic death. Distinct from the above mechanism, TLR3 can recognize viral double-stranded RNA and directly induce necroptotic death through a complex composed of TRIF, RIPK3, FADD, and caspase-8. On the other hand, TLR4 recognizes LPS through a complex that includes TRIF, RIP1, and RIP3. Phosphorylation of RIP1 and RIP3, along with the receptor interactions between TRIF and RIP3, leads to the phosphorylation of MLKL, triggering necroptotic death
Necroptosis in diabetic cardiomyopathy (DCM)
In contrast to other modalities of cell death, the role of necroptosis in DCM is in its nascent stage, and research explicitly linking necroptosis to DCM is relatively scant. Receptor-interacting protein kinase 3 (RIPK3) has been postulated to act as a pivotal regulator of necroptosis in diabetes, in a RIPK1-dependent manner. Preliminary investigations have elucidated that hyperglycemia markedly augments the expression of RIPK3 and mixed lineage kinase domain-like pseudokinase (MLKL) necroptotic signaling in both cardiac myocytes and the heart. Furthermore, the inhibition of RIPK3 can forestall MLKL phosphorylation and necroptosis in cardiac myocytes under hyperglycemic conditions [140, 141]. A recent study has disclosed that under high glucose (HG) stimulation, the activity and expression of aldehyde dehydrogenase 2 (ALDH2) are diminished, concomitant with an escalation in the expression of key necroptotic mediators such as RIPK3, RIPK1, and MLKL. Additionally, the upregulation of ALDH2 and downregulation of reactive oxygen species (ROS) expression can effectively quell necroptosis, thereby mediating cardioprotective effects under hyperglycemic conditions [142]. Sirtuin 3 (SIRT3), a deacetylase ubiquitously present in the heart, has been demonstrated to exacerbate mitochondrial damage induced by hyperglycemia, facilitate ROS accumulation, and promote the expression of necroptotic factors RIPK1 and RIPK3. It further activates the NLRP3 inflammasome, consequently aggravating the pathological manifestation of DCM in murine models [143]. In a novel revelation, Calcium/calmodulin-dependent protein kinase II (CaMKII), recognized as a new substrate for RIPK3, has been found to mediate myocardial necroptosis induced by ischemia and oxidative stress. Recent investigations indicate that its phosphorylation and oxidation are markedly enhanced in DCM mice and cardiac myocytes stimulated by advanced glycation end-products (AGEs). Silencing RIPK3 expression was shown to mitigate CaMKII activation and ameliorate necroptosis in DCM mice [144, 145].
Non-coding RNA (ncRNA) and necroptosis in diabetic cardiomyopathy (DCM)
Although the overarching theme of this article pertains to the role of ncRNA-mediated programmed cell death (PCD) in DCM, it is imperative to note that existing research on ncRNA-mediated necroptosis remains relatively scarce, thereby indirectly impeding the advancement of studies in the domain of necroptosis. Despite the limited body of work on ncRNA-mediated necroptosis in the context of DCM, select ncRNAs implicated in necroptosis in diseases associated with diabetes or cardiac dysfunction warrant considerable attention as potential therapeutic targets for DCM. For instance, Gao et al. observed that the expression of circRNA CNEACR is diminished post-myocardial ischemia–reperfusion (I/R), leading to myocardial necroptosis, whereas its overexpression ameliorates cardiac injury and enhances myocardial cell survival by upregulating Foxa2 and inhibiting RIPK3 transcription through a direct interaction with HDAC7 [146]. Similarly, Zhang et al. demonstrated that the expression of miR-325-3p is downregulated in myocardial infarction (MI) mice, and its overexpression attenuates the expression of necroptotic proteins such as RIPK1 and RIPK3, as well as phosphorylated MLKL, thereby mitigating the extent of infarction and tissue damage [147]. Corroborating these findings, Qin and colleagues verified through in vivo and in vitro assays that both miR-223-5p and -3p are expressed in myocardial tissues and target DR6, TNFR1, and the NLRP3 inflammasome, collectively dampening myocardial I/R-induced necroptosis [148]. While these ncRNAs have not yet been proven to function in DCM specifically, their study presents an intriguing avenue for future research into ncRNA-mediated PCD in DCM.
Discussion
The incidence of diabetes has been on an upward trajectory in recent years, and DCM, as one of the significant cardiovascular complications of diabetes, presents a considerable threat to human health. Characterized by structural and functional anomalies in myocardial tissues induced by long-term diabetes or hyperglycemia, DCM eventually culminates in heart failure. Given the intricate pathophysiological mechanisms underlying DCM and the absence of effective therapeutics explicitly targeting this disorder, a deeper exploration into the cellular and molecular mechanisms, as well as potential biomarkers in DCM, is urgently needed. Increasing attention has been paid to various forms of PCD as they have been closely implicated in the pathogenesis and progression of various diseases, including DCM. Myocardial PCD is considered a critical pathological factor in the onset and development of DCM, and targeting the regulation of myocardial PCD could serve as an essential therapeutic strategy. Moreover, accumulating evidence indicates that dysregulated ncRNAs play a pivotal role in DCM progression by modulating PCD. Therefore, elucidating the intricate interplay between ncRNA and PCD, along with their regulatory mechanisms in DCM, will contribute to a more comprehensive understanding of DCM's etiology and pathogenesis, thereby offering new avenues for diagnosis and treatment.
Emerging from the comprehensive review presented herein, it becomes unequivocally evident that distinct modalities of cell death are intrinsically involved in the progression of Diabetic Cardiomyopathy (DCM). Furthermore, the inhibition of virtually any form of PCD, excluding autophagy, has been shown to substantially alleviate impairments in myocardial structure and function, thereby highlighting these distinct forms of cell death as potential therapeutic targets for DCM. However, it is pivotal to recognize that PCD is a dynamically evolving process, exerting divergent impacts at different stages of disease progression. For instance, autophagy is traditionally considered vital in maintaining cardiac structure and function. Yet, both the inhibition and hyperactivation of cardiac autophagy yield significant repercussions on DCM. Numerous studies underscore the dual role of autophagy across various DCM subtypes; for example, autophagic markers are elevated in the hearts of type 2 diabetic patients, but diminished in primary myocardial cells cultured in high glucose and in type-1 diabetic myocardium [56]. This underscores the intricate regulation of cardiac autophagy within a diabetic milieu as a conundrum warranting expansive future research, including the development of novel autophagy modulators for DCM treatment. Additionally, it is important to delineate that different cell death modalities do not operate in isolation, rather, they engage in mutual crosstalk. For instance, miR-207 has been shown to inhibit autophagy while augmenting apoptosis in neonatal mouse cardiomyocytes [60], indicating a concerted involvement of both autophagy and apoptosis in DCM pathogenesis. Furthering this discourse, one study demonstrated that metformin could activate the AMPK signaling pathway, thereby promoting autophagy via inhibition of the mTOR signaling pathway and, in turn, suppressing NLRP3 inflammasome-induced pyroptosis in DCM [149]. Another investigation substantiated a connection between autophagy and necroptosis, where RIPK1 and RIPK3, along with their phosphorylated forms, are upregulated in HGF-treated cardiac fibroblasts and diabetic rat myocardial tissue. Inhibition of either RIPK1 or RIPK3 restored autophagic flux in HGF-treated cardiac fibroblasts, indicating that shared molecular mechanisms between necroptosis and autophagy could serve as promising therapeutic targets for DCM [150]. In summary, our findings elucidate that various types of cell death might co-exist and potentially occur concurrently during the onset and progression of DCM. Interfering with any single modality of cell death could potentially induce compensatory changes in other forms of cell death, thereby exacerbating the complexity of DCM's pathogenic mechanisms and complicating its treatment landscape. Therefore, a nuanced understanding of the intricate crosstalk between diverse PCD modalities and their predominant roles in the pathogenesis of DCM is indispensable. This knowledge will be instrumental in the future development of combined therapeutic strategies targeting multiple types of PCD.
In addition to the overarching themes discussed, this review consolidates the evidence concerning the interplay between non-coding RNA (ncRNA) and Programmed Cell Death (PCD) in Diabetic Cardiomyopathy (DCM). The data underpin the immense therapeutic potential of ncRNAs as regulators of PCD modalities, thereby positing them as promising targets for DCM intervention. Nonetheless, our investigation harbors certain limitations that must be candidly acknowledged. For instance, the complexity of miRNA–target gene interactions is multifaceted; a single miRNA can regulate multiple target genes, and conversely, a single target gene can be modulated by multiple miRNAs. As a case in point, LAMP2 not only possesses binding sites for miR-207 but also for other miRNAs like miR-221, which can inhibit autophagy by directly targeting LAMP2 and thus modulate TGF-β1-induced activation of hepatic stellate cells [151]. Additionally, miRNAs may also govern PCD through the regulation of other target genes, thereby exerting a significant influence on the course of DCM. Moreover, lncRNA and circRNA do not act via singular signaling pathways in their regulatory roles on PCD within the DCM context; rather, they function as competing endogenous RNAs (ceRNAs), sequestering miRNAs to modulate the expression of target genes. Such intricate dynamics, involving the orchestrated mediation of lncRNAs and miRNAs, circRNAs and miRNAs, in the progression of PCD in DCM, propose the modulation of ncRNA-mediated PCD as a novel strategic approach for DCM therapy. Of note, existing studies have demonstrated that the transfection or injection of ncRNA analogs, agonists, and antagonists could effectively decelerate DCM progression [64, 92, 104]. However, the expression levels and roles of ncRNAs can vary across different samples, and the bulk of current research is confined to molecular biology and disease model experimentation. The translational leap from bench science to clinical implementation remains a long traverse. Furthermore, while a plethora of studies focus on ncRNA-mediated regulation of autophagy, apoptosis, pyroptosis, and ferroptosis in DCM, there is a relative paucity of research pertaining to ncRNA-regulated necroptosis in DCM. As such, future investigations will prioritize elucidating the role of ncRNA-mediated necroptosis in DCM pathogenesis. In spite of these challenges, there exists cogent justification for optimism. With an increasingly sophisticated understanding of ncRNA-mediated PCD in DCM and the delineation of the underpinning mechanisms, we remain sanguine that new avenues for intervention will be uncovered in the prevention and treatment of DCM.
Data Availability
Enquiries about data availability should be directed to the authors.
References
Gao J, Liu J, Meng Z et al (2021) Ultrasound-assisted C3F8-filled PLGA nanobubbles for enhanced FGF21 delivery and improved prophylactic treatment of diabetic cardiomyopathy. Acta Biomater 130:395–408
Ouyang C, You J, Xie Z (2014) The interplay between autophagy and apoptosis in the diabetic heart. J Mol Cell Cardiol 71:71–80
Elshenawy DSA, Ramadan NM, Abdo VB, Ahour ARH (2022) Sacubitril/valsartan combination enhanced cardiac glycophagy and prevented the progression of murine diabetic cardiomyopathy [published correction appears in Biomed Pharmacother. Dec 156:113867]. Biomed Pharmacother 2022(153):113382
Kabbage M, Kessens R, Bartholomay LC, Williams B (2017) The life and death of a plant cell. Annu Rev Plant Biol 68:375–404
Del Re DP, Amgalan D, Linkermann A, Liu Q, Kitsis RN (2019) Fundamental mechanisms of regulated cell death and implications for heart disease. Physiol Rev 99(4):1765–1817
Mishra AP, Salehi B, Sharifi-Rad M et al (2018) Programmed cell death, from a cancer perspective: an overview. Mol Diagn Ther 22(3):281–295
Zhang L, Ai C, Bai M, Niu J, Zhang Z (2022) NLRP3 inflammasome/pyroptosis: a key driving force in diabetic cardiomyopathy. Int J Mol Sci 23(18):10632
Peng F, Liao M, Qin R et al (2022) Regulated cell death (RCD) in cancer: key pathways and targeted therapies. Signal Transduct Target Ther 7(1):286
Liu X, Yang W, Guan Z et al (2018) There are only four basic modes of cell death, although there are many ad-hoc variants adapted to different situations. Cell Biosci 8:6
Moujalled D, Strasser A, Liddell JR (2021) Molecular mechanisms of cell death in neurological diseases. Cell Death Differ 28(7):2029–2044
Wang E, Zhou S, Zeng D, Wang R (2023) Molecular regulation and therapeutic implications of cell death in pulmonary hypertension. Cell Death Discov 9(1):239
Jiang M, Qi L, Li L, Wu Y, Song D, Li Y (2021) Caspase-8: a key protein of cross-talk signal way in “PANoptosis” in cancer. Int J Cancer 149(7):1408–1420
Kaloni D, Diepstraten ST, Strasser A, Kelly GL (2023) BCL-2 protein family: attractive targets for cancer therapy. Apoptosis 28(1–2):20–38
Zhou X, Zeng Y, Zheng R et al (2023) Natural products modulate cell apoptosis: a promising way for treating endometrial cancer. Front Pharmacol 14:1209412
Carberry S, D’Orsi B, Monsefi N et al (2018) The BAX/BAK-like protein BOK is a prognostic marker in colorectal cancer. Cell Death Dis 9(2):125
Quarato G, Mari L, Barrows NJ et al (2023) Mitophagy restricts BAX/BAK-independent, Parkin-mediated apoptosis. Sci Adv 9(21):eadg8156
Belali OM, Ahmed MM, Mohany M et al (2022) LCZ696 protects against diabetic cardiomyopathy-induced myocardial inflammation, ER stress, and apoptosis through inhibiting AGEs/NF-κB and PERK/CHOP signaling pathways. Int J Mol Sci 23(3):1288
Lin N, Lin H, Yang Q et al (2021) SGLT1 inhibition attenuates apoptosis in diabetic cardiomyopathy via the JNK and p38 pathway. Front Pharmacol 11:598353
Ren BC, Zhang YF, Liu SS et al (2020) Curcumin alleviates oxidative stress and inhibits apoptosis in diabetic cardiomyopathy via Sirt1-Foxo1 and PI3K-Akt signalling pathways. J Cell Mol Med 24(21):12355–12367
Joubert M, Manrique A, Cariou B, Prieur X (2019) Diabetes-related cardiomyopathy: the sweet story of glucose overload from epidemiology to cellular pathways. Diabetes Metab 45(3):238–247
Shi H, Zhou P, Ni YQ et al (2021) In vivo and in vitro studies of Danzhi Jiangtang capsules against diabetic cardiomyopathy via TLR4/MyD88/NF-κB signaling pathway. Saudi Pharm J 29(12):1432–1440
Wang S, Duan J, Liao J et al (2022) LncRNA H19 inhibits ER stress induced apoptosis and improves diabetic cardiomyopathy by regulating PI3K/AKT/mTOR axis. Aging (Albany NY) 14(16):6809–6828
Ni J, Li Y, Xu Y, Guo R (2021) Salidroside protects against cardiomyocyte apoptosis and ventricular remodeling by AKT/HO-1 signaling pathways in a diabetic cardiomyopathy mouse model. Phytomedicine 82:153406
Taheriazam A, Bayanzadeh SD, Heydari Farahani M et al (2023) Non-coding RNA-based therapeutics in cancer therapy: an emphasis on Wnt/β-catenin control. Eur J Pharmacol 951:175781
Chen R, Chen H, Yang Z et al (2023) Danlou tablet inhibits high-glucose-induced cardiomyocyte apoptosis via the miR-34a-SIRT1 axis. Heliyon 9(3):e14479
Park IH, Song YS, Joo HW et al (2020) Role of MicroRNA-34a in anti-apoptotic effects of granulocyte-colony stimulating factor in diabetic cardiomyopathy. Diabetes Metab J 44(1):173–185
Xia X, Liang Y, Zheng W, Lin D, Sun S (2020) miR-410-5p promotes the development of diabetic cardiomyopathy by suppressing PIM1-induced anti-apoptosis. Mol Cell Probes 52:101558
Qiao Y, Zhao Y, Liu Y et al (2016) miR-483-3p regulates hyperglycaemia-induced cardiomyocyte apoptosis in transgenic mice. Biochem Biophys Res Commun 477(4):541–547
Wang X, Zhang Z, Wang M (2022) MiR-29a regulates cardiomyocyte apoptosis by targeting Bak1 in diabetic cardiomyopathy. J Biochem 171(6):663–671
Liu X, Guo B, Zhang W, Ma B, Li Y (2021) MiR-20a-5p overexpression prevented diabetic cardiomyopathy via inhibition of cardiomyocyte apoptosis, hypertrophy, fibrosis and JNK/NF-κB signalling pathway. J Biochem 170(3):349–362
Xu D, Zhang X, Chen X, Yang S, Chen H (2020) Inhibition of miR-223 attenuates the NLRP3 inflammasome activation, fibrosis, and apoptosis in diabetic cardiomyopathy. Life Sci 256:117980
Liu Y, Zheng W, Pan Y, Hu J (2019) Low expression of miR-186-5p regulates cell apoptosis by targeting toll-like receptor 3 in high glucose-induced cardiomyocytes. J Cell Biochem 120(6):9532–9538
Huang W, Li H, Yu Q, Xiao W, Wang DO (2022) LncRNA-mediated DNA methylation: an emerging mechanism in cancer and beyond [published correction appears in J Exp Clin Cancer Res. 2022 Aug 27;41(1):262]. J Exp Clin Cancer Res. 41(1):100
Toden S, Zumwalt TJ, Goel A (2021) Non-coding RNAs and potential therapeutic targeting in cancer. Biochim Biophys Acta Rev Cancer 1875(1):188491
Wang T, Li N, Yuan L et al (2023) MALAT1/miR-185-5p mediated high glucose-induced oxidative stress, mitochondrial injury and cardiomyocyte apoptosis via the RhoA/ROCK pathway. J Cell Mol Med 27(17):2495–2506
Cheng Y, Li J, Wang C et al (2020) Inhibition of long non-coding RNA metastasis-associated lung adenocarcinoma transcript 1 attenuates high glucose-induced cardiomyocyte apoptosis via regulation of miR-181a-5p. Exp Anim 69(1):34–44
Tang H, Zhong H, Liu W et al (2022) Melatonin alleviates hyperglycemia-induced cardiomyocyte apoptosis via regulation of long non-coding RNA H19/miR-29c/MAPK axis in diabetic cardiomyopathy. Pharmaceuticals (Basel) 15(7):821
Zhu C, Zhang H, Wei D, Sun Z (2021) Silencing lncRNA GAS5 alleviates apoptosis and fibrosis in diabetic cardiomyopathy by targeting miR-26a/b-5p. Acta Diabetol 58(11):1491–1501
Zhao SF, Ye YX, Xu JD et al (2021) Long non-coding RNA KCNQ1OT1 increases the expression of PDCD4 by targeting miR-181a-5p, contributing to cardiomyocyte apoptosis in diabetic cardiomyopathy. Acta Diabetol 58(9):1251–1267
Wang C, Liu G, Yang H et al (2021) MALAT1-mediated recruitment of the histone methyltransferase EZH2 to the microRNA-22 promoter leads to cardiomyocyte apoptosis in diabetic cardiomyopathy. Sci Total Environ 766:142191
Chen Y, Zhang Z, Zhu D, Zhao W, Li F (2019) Long non-coding RNA MEG3 serves as a ceRNA for microRNA-145 to induce apoptosis of AC16 cardiomyocytes under high glucose condition. Biosci Rep 39(6):BSR20190444
Zhou X, Zhang W, Jin M et al (2017) lncRNA MIAT functions as a competing endogenous RNA to upregulate DAPK2 by sponging miR-22-3p in diabetic cardiomyopathy. Cell Death Dis 8(7):e2929
Abdelmohsen K, Panda AC, Munk R et al (2017) Identification of HuR target circular RNAs uncovers suppression of PABPN1 translation by CircPABPN1. RNA Biol 14(3):361–369
Kristensen LS, Andersen MS, Stagsted LVW, Ebbesen KK, Hansen TB, Kjems J (2019) The biogenesis, biology and characterization of circular RNAs. Nat Rev Genet 20(11):675–691
Shao Y, Li M, Yu Q et al (2022) CircRNA CDR1as promotes cardiomyocyte apoptosis through activating hippo signaling pathway in diabetic cardiomyopathy. Eur J Pharmacol 922:174915
Jiang J, Gao G, Pan Q et al (2022) Circular RNA circHIPK3 is downregulated in diabetic cardiomyopathy and overexpression of circHIPK3 suppresses PTEN to protect cardiomyocytes from high glucose-induced cell apoptosis. Bioengineered 13(3):6272–6279
Peng Q, Liu H, Luo Z et al (2022) Effect of autophagy on ferroptosis in foam cells via Nrf2. Mol Cell Biochem 477(5):1597–1606
Lin L, Zhang MX, Zhang L et al (2022) Autophagy, pyroptosis, and ferroptosis: new regulatory mechanisms for atherosclerosis. Front Cell Dev Biol 9:809955
Khan F, Khan H, Khan A et al (2022) Autophagy in adipogenesis: molecular mechanisms and regulation by bioactive compounds. Biomed Pharmacother 155:113715
Madrigal-Matute J, Cuervo AM, Sluimer JC (2022) Chaperone-mediated autophagy protects against atherosclerosis. Autophagy 18(10):2505–2507
Ravikumar B, Sarkar S, Davies JE et al (2010) Regulation of mammalian autophagy in physiology and pathophysiology. Physiol Rev 90(4):1383–1435
Al-Bari MAA (2020) A current view of molecular dissection in autophagy machinery. J Physiol Biochem 76(3):357–372
Su Y, Fan X, Li S et al (2022) Scutellarin improves Type 2 diabetic cardiomyopathy by regulating cardiomyocyte autophagy and apoptosis. Dis Mark 2022:3058354
Escobar KA, Cole NH, Mermier CM et al (2019) Autophagy and aging: maintaining the proteome through exercise and caloric restriction. Aging Cell 18(1):e12876
Kim J, Kundu M, Viollet B et al (2011) AMPK and mTOR regulate autophagy through direct phosphorylation of Ulk1. Nat Cell Biol 13(2):132–141
Wang H, Wang L, Hu F et al (2022) Neuregulin-4 attenuates diabetic cardiomyopathy by regulating autophagy via the AMPK/mTOR signalling pathway. Cardiovasc Diabetol 21(1):205
Lu Q-B, Ding Y, Liu Y et al (2022) Metrnl ameliorates diabetic cardiomyopathy via inactivation of cGAS/STING signaling dependent on LKB1/AMPK/ULK1-mediated autophagy. J Adv Res 51:161–179
Zhao J, Wu Q, Yang T et al (2022) Gaseous signal molecule SO2 regulates autophagy through PI3K/AKT pathway inhibits cardiomyocyte apoptosis and improves myocardial fibrosis in rats with type II diabetes. Korean J Physiol Pharmacol 26(6):541–556
Ning SW, Zhang SQ, Guo ZK (2023) MicroRNA-494 regulates high glucose-induced cardiomyocyte apoptosis and autophagy by PI3K/AKT/mTOR signalling pathway. ESC Heart Fail 10:1401–1411
Xing R, Liu D, Cheng X, Tian X, Yan C, Han Y (2019) MiR-207 inhibits autophagy and promotes apoptosis of cardiomyocytes by directly targeting LAMP2 in type 2 diabetic cardiomyopathy. Biochem Biophys Res Commun 520(1):27–34
Ni T, Lin N, Lu W et al (2020) Dihydromyricetin prevents diabetic cardiomyopathy via miR-34a suppression by activating autophagy. Cardiovasc Drugs Ther 34(3):291–301
Nandi SS, Duryee MJ, Shahshahan HR et al (2015) Induction of autophagy markers is associated with attenuation of miR-133a in diabetic heart failure patients undergoing mechanical unloading. Am J Transl Res 7(4):683–696
Ucar A, Gupta SK, Fiedler J et al (2012) The miRNA-212/132 family regulates both cardiac hypertrophy and cardiomyocyte autophagy. Nat Commun 3:1078
Li X, Meng C, Han F et al (2021) Vildagliptin attenuates myocardial dysfunction and restores autophagy via miR-21/SPRY1/ERK in diabetic mice heart. Front Pharmacol 12:634365
Chen C, Yang S, Li H et al (2017) Mir30c is involved in diabetic cardiomyopathy through regulation of cardiac autophagy via BECN1. Mol Ther Nucleic Acids 7:127–139
Chen D, Zhang M (2021) GAS5 regulates diabetic cardiomyopathy via miR-221-3p/p27 axis-associated autophagy. Mol Med Rep 23(2):135
Feng Y, Xu W, Zhang W et al (2019) LncRNA DCRF regulates cardiomyocyte autophagy by targeting miR-551b-5p in diabetic cardiomyopathy. Theranostics 9(15):4558–4566
Zhuo C, Jiang R, Lin X, Shao M (2017) LncRNA H19 inhibits autophagy by epigenetically silencing of DIRAS3 in diabetic cardiomyopathy. Oncotarget 8(1):1429–1437
Brennan MA, Cookson BT (2000) Salmonella induces macrophage death by caspase-1-dependent necrosis. Mol Microbiol 38(1):31–40
Shi J, Zhao Y, Wang K et al (2015) Cleavage of GSDMD by inflammatory caspases determines pyroptotic cell death. Nature 526(7575):660–665
Kayagaki N, Warming S, Lamkanfi M et al (2011) Non-canonical inflammasome activation targets caspase-11. Nature 479(7371):117–121
Kayagaki N, Stowe IB, Lee BL et al (2015) Caspase-11 cleaves gasdermin D for non-canonical inflammasome signalling. Nature 526(7575):666–671
Orning P, Weng D, Starheim K et al (2018) Pathogen blockade of TAK1 triggers caspase-8-dependent cleavage of gasdermin D and cell death. Science 362(6418):1064–1069
Li T, Zheng G, Li B, Tang L (2021) Pyroptosis: a promising therapeutic target for noninfectious diseases. Cell Prolif 54(11):e13137
Broz P, Dixit VM (2016) Inflammasomes: mechanism of assembly, regulation and signalling. Nat Rev Immunol 16(7):407–420
Sun P, Zhong J, Liao H et al (2022) Hepatocytes are resistant to cell death from canonical and non-canonical inflammasome-activated pyroptosis. Cell Mol Gastroenterol Hepatol 13(3):739–757
An S, Hu H, Li Y et al (2020) Pyroptosis plays a role in osteoarthritis. Aging Dis 11(5):1146–1157
Downs KP, Nguyen H, Dorfleutner A, Stehlik C (2020) An overview of the non-canonical inflammasome. Mol Aspects Med 76:100924
Yang D, He Y, Muñoz-Planillo R et al (2015) Caspase-11 requires the pannexin-1 channel and the purinergic P2X7 pore to mediate pyroptosis and endotoxic shock. Immunity 43(5):923–932
Shi J, Zhao Y, Wang Y et al (2014) Inflammatory caspases are innate immune receptors for intracellular LPS. Nature 514(7521):187–192
Liu C, Yao Q, Hu T et al (2022) Cathepsin B deteriorates diabetic cardiomyopathy induced by streptozotocin via promoting NLRP3-mediated pyroptosis. Mol Ther Nucleic Acids 30:198–207
Zeng C, Wang R, Tan H (2019) Role of pyroptosis in cardiovascular diseases and its therapeutic implications. Int J Biol Sci 15(7):1345–1357
Xie Y, Huang Y, Ling X et al (2020) Chemerin/CMKLR1 axis promotes inflammation and pyroptosis by activating NLRP3 inflammasome in diabetic cardiomyopathy rat. Front Physiol 11:381
Peng M, Liu Y, Xu Y et al (2021) Cathelicidin-WA ameliorates diabetic cardiomyopathy by inhibiting the NLRP3 inflammasome. Cell Cycle 20(21):2278–2290
Jeyabal P, Thandavarayan RA, Joladarashi D et al (2016) MicroRNA-9 inhibits hyperglycemia-induced pyroptosis in human ventricular cardiomyocytes by targeting ELAVL1. Biochem Biophys Res Commun 471(4):423–429
Luo B, Li B, Wang W et al (2014) NLRP3 gene silencing ameliorates diabetic cardiomyopathy in a type 2 diabetes rat model. PLoS ONE 9(8):e104771
Luo B, Huang F, Liu Y et al (2017) NLRP3 inflammasome as a molecular marker in diabetic cardiomyopathy. Front Physiol 8:519
Hutchinson KR, Lord KC, West TA et al (2013) Cardiac fibroblast-dependent extracellular matrix accumulation is associated with diastolic stiffness in Type 2 diabetes. PLoS ONE 8:e72080
Kawaguchi M, Takahashi M, Hata T et al (2011) Inflammasome activation of cardiac fibroblasts is essential for myocardial ischemia/reperfusion injury. Circulation 123(6):594–604
Gao G, Fu L, Xu Y et al (2022) Cyclovirobuxine D ameliorates experimental diabetic cardiomyopathy by inhibiting cardiomyocyte pyroptosis via NLRP3 in vivo and in vitro. Front Pharmacol 13:906548
Chen Y, Wang L, Pitzer AL et al (2016) Contribution of redox-dependent activation of endothelial Nlrp3 inflammasomes to hyperglycemia-induced endothelial dysfunction. J Mol Med (Berl) 94(12):1335–1347
Xiao W, Zheng D, Chen X et al (2021) Long non-coding RNA MIAT is involved in the regulation of pyroptosis in diabetic cardiomyopathy via targeting miR-214–3p. iScience 24(12):103518
Li X, Du N, Zhang Q et al (2014) MicroRNA-30d regulates cardiomyocyte pyroptosis by directly targeting foxo3a in diabetic cardiomyopathy. Cell Death Dis 5(10):e1479
Yang L, Cheng CF, Li ZF et al (2023) Berberine blocks inflammasome activation and alleviates diabetic cardiomyopathy via the miR-18a-3p/Gsdmd pathway. Int J Mol Med 51(6):49
Ren L, Chen X, Nie B et al (2022) Ranolazine inhibits pyroptosis via regulation of miR-135b in the treatment of diabetic cardiac fibrosis. Front Mol Biosci 9:806966
Shi P, Zhao XD, Shi KH et al (2021) MiR-21-3p triggers cardiac fibroblasts pyroptosis in diabetic cardiac fibrosis via inhibiting androgen receptor. Exp Cell Res 399(2):112464
Zhao S, Tan Y, Qin J et al (2022) MicroRNA-223–3p promotes pyroptosis of cardiomyocyte and release of inflammasome factors via downregulating the expression level of SPI1 (PU. 1). Toxicology 476:153252
Xiong J, Zhou Q (2023) The lncRNA HOTAIR attenuates pyroptosis of diabetic cardiomyocytes by recruiting FUS to regulate SIRT3 expression. Kaohsiung J Med Sci 39(5):458–467
Wu A, Sun W, Mou F (2021) lncRNA-MALAT1 promotes high glucose-induced H9C2 cardiomyocyte pyroptosis by downregulating miR-141-3p expression. Mol Med Rep 23(4):259
Xu Y, Fang H, Xu Q et al (2020) LncRNA GAS5 inhibits NLRP3 inflammasome activation-mediated pyroptosis in diabetic cardiomyopathy by targeting miR-34b-3p/AHR. Cell Cycle 19(22):3054–3065
Yang F, Qin Y, Wang Y et al (2018) LncRNA KCNQ1OT1 mediates pyroptosis in diabetic cardiomyopathy. Cell Physiol Biochem 50(4):1230–1244
Fu L, Zhang J, Lin Z, Li Y, Qin G (2022) CircularRNA circ_0071269 knockdown protects against from diabetic cardiomyopathy injury by microRNA-145/gasdermin A axis. Bioengineered 13(2):2398–2411
Yang F, Li A, Qin Y et al (2019) A novel circular RNA mediates pyroptosis of diabetic cardiomyopathy by functioning as a competing endogenous RNA. Mol Ther Nucleic Acids 17:636–643
Yuan Q, Sun Y, Yang F et al (2023) CircRNA DICAR as a novel endogenous regulator for diabetic cardiomyopathy and diabetic pyroptosis of cardiomyocytes. Signal Transduct Target Ther 8(1):99
Dixon SJ, Lemberg KM, Lamprecht MR et al (2012) Ferroptosis: an iron-dependent form of nonapoptotic cell death. Cell 149(5):1060–1072
Xie Y, Hou W, Song X et al (2016) Ferroptosis: process and function. Cell Death Differ 23(3):369–379
Sun Y, Li Q, Guo H et al (2022) Ferroptosis and iron metabolism after intracerebral hemorrhage. Cells 12(1):90
Galaris D, Barbouti A, Pantopoulos K (2019) Iron homeostasis and oxidative stress: an intimate relationship. Biochim Biophys Acta Mol Cell Res 1866(12):118535
Yu Y, Yan Y, Niu F et al (2021) Ferroptosis: a cell death connecting oxidative stress, inflammation and cardiovascular diseases. Cell Death Discov 7(1):193
Han C, Liu Y, Dai R et al (2020) Ferroptosis and its potential role in human diseases. Front Pharmacol 11:239
Li H, Lin L, Xia YL et al (2022) Research progress on the role of ferroptosis in cardiovascular disease. Front Cardiovasc Med 9:1077332
Chen J, Wang Y, Wu J et al (2020) The potential value of targeting ferroptosis in early brain injury after acute CNS disease. Front Mol Neurosci 13:110
Hou W, Xie Y, Song X et al (2016) Autophagy promotes ferroptosis by degradation of ferritin. Autophagy 12(8):1425–1428
Mancias JD, Wang X, Gygi SP et al (2014) Quantitative proteomics identifies NCOA4 as the cargo receptor mediating ferritinophagy. Nature 509(7498):105–109
Fang Y, Chen X, Tan Q et al (2021) Inhibiting ferroptosis through disrupting the NCOA4-FTH1 interaction: a new mechanism of action. ACS Cent Sci 7(6):980–989
Deng L, He S, Guo N et al (2023) Molecular mechanisms of ferroptosis and relevance to inflammation. Inflamm Res 72(2):281–299
Xing L, Liu XY, Zhou TJ et al (2021) Photothermal nanozyme-ignited Fenton reaction-independent ferroptosis for breast cancer therapy. J Control Release 339:14–26
Dodson M, Castro-Portuguez R, Zhang DD (2019) NRF2 plays a critical role in mitigating lipid peroxidation and ferroptosis. Redox Biol 23:101107
Yang WS, Kim KJ, Gaschler MM et al (2016) Peroxidation of polyunsaturated fatty acids by lipoxygenases drives ferroptosis. Proc Natl Acad Sci USA 113(34):E4966–E4975
Yang WS, SriRamaratnam R, Welsch ME et al (2014) Regulation of ferroptotic cancer cell death by GPX4. Cell 156(1–2):317–331
Liu Y, Gu W (2022) p53 in ferroptosis regulation: the new weapon for the old guardian. Cell Death Differ 29(5):895–910
Altamura S, Müdder K, Schlotterer A et al (2021) Iron aggravates hepatic insulin resistance in the absence of inflammation in a novel db/db mouse model with iron overload. Mol Metab 51:101235
Palomer X, Salvadó L, Barroso E et al (2013) An overview of the crosstalk between inflammatory processes and metabolic dysregulation during diabetic cardiomyopathy. Int J Cardiol 168(4):3160–3172
Wilson AJ, Gill EK, Abudalo RA et al (2018) Reactive oxygen species signalling in the diabetic heart: emerging prospect for therapeutic targeting. Heart 104(4):293–299
Du S, Shi H, Xiong L et al (2022) Canagliflozin mitigates ferroptosis and improves myocardial oxidative stress in mice with diabetic cardiomyopathy. Front Endocrinol (Lausanne) 13:1011669
Wang X, Chen X, Zhou W et al (2022) Ferroptosis is essential for diabetic cardiomyopathy and is prevented by sulforaphane via AMPK/NRF2 pathways. Acta Pharm Sin B 12(2):708–722
Ni T, Huang X, Pan S et al (2021) Inhibition of the long non-coding RNA ZFAS1 attenuates ferroptosis by sponging miR-150-5p and activates CCND2 against diabetic cardiomyopathy. J Cell Mol Med 25(21):9995–10007
Jiang M, Jike Y, Liu K et al (2023) Exosome-mediated miR-144-3p promotes ferroptosis to inhibit osteosarcoma proliferation, migration, and invasion through regulating ZEB1. Mol Cancer 22(1):113
Cen J, Liang Y, Feng Z et al (2023) Hsa_circ_0057105 modulates a balance of epithelial-mesenchymal transition and ferroptosis vulnerability in renal cell carcinoma. Clin Transl Med 13(8):e1339
Teng X, Degterev A, Jagtap P et al (2005) Structure-activity relationship study of novel necroptosis inhibitors. Bioorg Med Chem Lett 15(22):5039–5044
Galluzzi L, Vitale I, Aaronson SA et al (2018) Molecular mechanisms of cell death: recommendations of the nomenclature committee on cell death 2018. Cell Death Differ 25(3):486–541
Khan I, Yousif A, Chesnokov M et al (2021) A decade of cell death studies: breathing new life into necroptosis. Pharmacol Ther 220:107717
Degterev A, Huang Z, Boyce M et al (2005) Chemical inhibitor of nonapoptotic cell death with therapeutic potential for ischemic brain injury [published correction appears in Nat Chem Biol. 2005 Sep;1(4):234]. Nat Chem Biol 1(2):112–119
Zhu F, Zhang W, Yang T et al (2019) Complex roles of necroptosis in cancer. J Zhejiang Univ Sci B 20(5):399–413
Feoktistova M, Geserick P, Kellert B et al (2011) cIAPs block ripoptosome formation, a RIP1/caspase-8 containing intracellular cell death complex differentially regulated by cFLIP isoforms. Mol Cell 43(3):449–463
McComb S, Cheung HH, Korneluk RG et al (2012) cIAP1 and cIAP2 limit macrophage necroptosis by inhibiting Rip1 and Rip3 activation. Cell Death Differ 19(11):1791–1801
Wang L, Du F, Wang X (2008) TNF-alpha induces two distinct caspase-8 activation pathways. Cell 133(4):693–703
Dondelinger Y, Aguileta MA, Goossens V et al (2013) RIPK3 contributes to TNFR1-mediated RIPK1 kinase-dependent apoptosis in conditions of cIAP1/2 depletion or TAK1 kinase inhibition. Cell Death Differ 20(10):1381–1392
Cho YS, Challa S, Moquin D et al (2009) Phosphorylation-driven assembly of the RIP1-RIP3 complex regulates programmed necrosis and virus-induced inflammation. Cell 137(6):1112–1123
Apaijai N, Jinawong K, Singhanat K et al (2021) Necrostatin-1 reduces cardiac and mitochondrial dysfunction in prediabetic rats. J Endocrinol 251(1):27–39
Cao T, Ni R, Ding W et al (2022) MLKL-mediated necroptosis is a target for cardiac protection in mouse models of type-1 diabetes. Cardiovasc Diabetol 21(1):165
Fang T, Cao R, Wang W et al (2018) Alterations in necroptosis during ALDH2-mediated protection against high glucose-induced H9c2 cardiac cell injury. Mol Med Rep 18(3):2807–2815
Song S, Ding Y, Dai GL et al (2021) Sirtuin 3 deficiency exacerbates diabetic cardiomyopathy via necroptosis enhancement and NLRP3 activation. Acta Pharmacol Sin 42(2):230–241
Chen Y, Li X, Hua Y et al (2021) RIPK3-mediated necroptosis in diabetic cardiomyopathy requires CaMKII activation. Oxid Med Cell Longev 2021:6617816
Zhang T, Zhang Y, Cui M et al (2016) CaMKII is a RIP3 substrate mediating ischemia- and oxidative stress-induced myocardial necroptosis. Nat Med 22(2):175–182
Gao XQ, Liu CY, Zhang YH et al (2022) The circRNA CNEACR regulates necroptosis of cardiomyocytes through Foxa2 suppression. Cell Death Differ 29(3):527–539
Zhang DY, Wang BJ, Ma M, Zhang XW et al (2019) Correction to: MicroRNA-325–3p protects the heart after myocardial infarction by inhibiting RIPK3 and programmed necrosis in mice. BMC Mol Biol. 20(1):18
Qin D, Wang X, Li Y et al (2016) MicroRNA-223-5p and -3p cooperatively suppress necroptosis in ischemic/reperfused hearts. J Biol Chem 291(38):20247–20259
Yang F, Qin Y, Wang Y et al (2019) Metformin inhibits the NLRP3 inflammasome via AMPK/mTOR-dependent effects in diabetic cardiomyopathy. Int J Biol Sci 15(5):1010–1019
Qiao S, Hong L, Zhu Y et al (2022) RIPK1-RIPK3 mediates myocardial fibrosis in type 2 diabetes mellitus by impairing autophagic flux of cardiac fibroblasts. Cell Death Dis 13(2):147
Cheng R, Xu H, Hong Y (2021) miR-221 regulates TGF-β1-induced HSC activation through inhibiting autophagy by directly targeting LAMP2. Mol Med Rep 24(5):777
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Contributions
ZBR contributed to the conception and design of this manuscript. ZL has critically revised the entire manuscript. WH, ZJW, and CC are responsible for manuscript structure and English grammar. All authors participated in manuscript revision, read and approved the submitted version. All authors revised and approved the final manuscript. “The author(s) read and approved the final manuscript.”
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, B., Wu, H., Zhang, J. et al. The study of the mechanism of non-coding RNA regulation of programmed cell death in diabetic cardiomyopathy. Mol Cell Biochem 479, 1673–1696 (2024). https://doi.org/10.1007/s11010-023-04909-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-023-04909-7