Abstract
Arterial hypertension is a disease that often coexists with dyslipidemia. Both disorders can produce oxidative stress. Studies in vivo and in vitro have proven that oxidative stress can induce an increment of the erythrocyte apoptosis (eryptosis), through the rise of free intracellular calcium concentration ([Ca2+]i). Higher levels of eryptosis have not been described in patients with hypertension, dyslipidemia, or both combined. This study involved 81 men between 26 and 50 years old, assorted into four groups: normotensive with and without dyslipidemia, and hypertensive with and without dyslipidemia. Hypertensive and/or dyslipidemic patients had double mean lipid peroxidation and 30% less mean GSH concentration than the normotensive non-dyslipidemic patients. Mean [Ca2+]i in hypertensive patients was 100 and 200% higher, in patients without and with dyslipidemia, respectively, compared to normotensive patients. Dyslipidemic normotensive patients had three times higher mean PS externalization than the normotensive non-dyslipidemic patients, and the hypertension condition doubled this difference. Hypertensive patients had higher eryptosis associated with higher levels of [Ca2+]i and oxidative stress, suggesting that eryptosis participates in the pathophysiological mechanisms of hypertension. The quantitative analysis, when the dyslipidemic factor is included, shows that oxidative stress–[Ca2+]i–eryptosis do not follow a unique pattern in the different groups and suggests the existence of mechanisms of induction and molecular pathways alternative or additional to oxidative stress and [Ca2+]i, respectively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arterial hypertension (AH) is a pathology characterized by an elevated arterial pressure, either systolic or diastolic [1]. According to the WHO, one out of three adults in the world suffers from AH [2]. Cardiovascular and renal complications produced by AH result in high economic costs and deterioration of the quality of life and can be exacerbated by other conditions, such as smoking, alcoholism, psychological stress, diabetes mellitus, or dyslipidemia [3,4,5]. Dyslipidemia is an alteration of the concentration of triglycerides or cholesterol in the blood [6]; it is also widely distributed and is frequently associated with AH and believed to intensify its complications [5, 7]. Some works have associated the oxidative stress with AH: hypertensive patients present a high production of hydrogen peroxide, superoxide ion, and nitric oxide in leukocytes [8,9,10], elevated lipid peroxidation in erythrocytes, and high concentrations of 8-isoprostanes in plasma [11]. Patients with moderate untreated AH presented a high lipid peroxidation in erythrocytes in comparison with normotensive individuals and treated hypertensive patients [12], and heightened concentration of 8-isoprostanes in urine compared to patients with treated AH [13]. On the other hand, treated hypertensive patients with evolution time between five and ten years showed a low lipid peroxidation in blood [14].
Regarding the antioxidant response, untreated hypertensive patients presented a low concentration of GSH in erythrocytes [15, 16], low activity of catalase (CAT), superoxide dismutase (SOD), and glutathione peroxidase (GPx) in erythrocytes [11] and blood [14], compared to normotensive patients. Hypertensive patients with dyslipidemia also had a lower total antioxidant capacity and lower activity of SOD and CAT in plasma [17]. On the contrary, treated hypertensive patients showed a higher concentration of GSH in blood with respect to normotensive patients [18]. Dyslipidemia, associated with other pathologies such as obesity and diabetes mellitus type II, can intensify the oxidative stress [19, 20].
Oxidative damage has been associated with high levels of eryptosis through a rise of intracellular free calcium concentration [Ca2+]i, as shown in vitro studies [21,22,23,24], in patients intoxicated with lead [25], and in diabetic patients with chronic renal damage [26]. Patients with uncontrolled AH also have high [Ca2+]i [27], though these authors did not study either oxidative damage or eryptosis. To the present, there are not studies that associate eryptosis with AH, even though high levels of eryptosis could be involved in the pathophysiological mechanisms of micro- and macrovascular complications of AH [26, 28]. The increment of [Ca2+]i is not the only known pathway to produce higher rates of eryptosis [29]; besides oxidative stress, energetic, mechanical, and osmotic stresses can also induce eryptosis [23].
This work focuses on eryptosis, oxidative damage, and [Ca2+]i in normotensive patients with and without dyslipidemia, and hypertensive patients with and without dyslipidemia; patients with hypertension and dyslipidemia were under pharmacological treatment. The purpose is to determine if AH alone or associated with dyslipidemia generates higher levels of eryptosis induced by oxidative stress and having elevated [Ca2+]i as the signaling pathway.
Materials and methods
This study involved 81 Mexican mestizo men from the city of Durango, Dgo, Mexico, with age range between 26 and 50 years, belonging to the middle class. The study groups consisted of 15 normotensive non-dyslipidemic patients (NT), 27 normotensive patients with dyslipidemia (ND), 12 hypertensive non-dyslipidemic patients (HT), and 27 hypertensive patients with dyslipidemia (HTD). All patients were diagnosed and treated at the Durango State Public Health Centers by specialists in internal medicine, according to the criteria established by the American Heart Association [2, 6].
Hypertensive patients were diagnosed as patients with essential hypertension and were treated with captopril or enalapril (ACE inhibitors), and patients with dyslipidemia with bezafibrate or atorvastatin. Treatments were distributed in the different groups as follows: ND: 10 were treated with atorvastatin and 17 with bezafibrate; HT: 4 were treated with captopril and 8 with enalapril; HTD: 9 were treated with captopril, of which 4 were treated with bezafibrate and 5 with atorvastatin; the other 18 HTD patients were treated with enalapril, of which 9 also received bezafibrate and 9 received atorvastatin.
No patient ever suffered uncontrolled hypertension or received treatments unrelated to hypertension or dyslipidemia; none presented clinical evidence of either renal, endocrine, gastrointestinal, or cardiovascular diseases.
The study protocol was approved by the Ethics Committee of the Institute of Scientific Research of the Universidad Juárez del Estado de Durango, México, according to the Declaration of Helsinki and the second title, Chapter 1, Article 17, paragraph 2 of the Law General Health research. All subjects provided written informed consent, and participation was voluntary.
Blood pressure determination
Arterial pressure was measured in seated participants after they rested for 5 min with the use of a pneumatic baumanometer on the left arm, according to the criteria established in the Seventh Report of the Joint National [30].
Blood sample collection
Blood was collected by venipuncture into heparinized tubes. The samples were maintained at 4 °C until use. An aliquot of the blood was used for obtaining erythrocytes and plasma, each sample of blood was centrifuged at 700×g for 10 min at 4 °C, the plasma was preserved by freezing until its use, and the white cells were discarded.
Biochemical parameters
Glucose, total cholesterol, triglycerides, C-HDL, and C-LDL were measured using colorimetric and enzymatic methods.
Lipid peroxidation
Lipid peroxidation in erythrocytes was measured by the concentration of thiobarbituric acid-reactive substances (TBARS) at 532 nm of absorbance using a spectrophotometer UV/125 VIS 730 (Beckman). The TBARS are expressed as nmol malondialdehyde equivalents per ml of erythrocytes (nmol/ml), according to a calibration curve of malondialdehyde [31,32,33].
GSH concentration
The concentration of reduced glutathione in erythrocytes was measured using a Glutathione Assay Kit (Sigma CS0260), limiting the procedure to the determination of reduced glutathione. Erythrocytes were washed with PBS by centrifugation at 600×g for 10 min. Erythrocytes were incubated for 5 min with 200 μl of 5-sulfosalicylic acid (5%), and the supernatant was recovered after 10 min of centrifugation at 10,000×g. The quantification in each sample was made in duplicate; the samples were further incubated with the final concentration of the components in the reaction mixtures (95 mM potassium phosphate buffer, pH 7.0, 0.95 mM EDTA, 0.031 mg/ml DNTB, and 0.24% 5-sulfosalicylic acid). The TNB was measured at 412 nm in a Stat Fax 4200 microplate reader [34].
Assessment of [Ca2+]i
Erythrocytes were suspended in HEPES buffer saline, containing 144 mM NaCl, 5 mM KCl, 10 mM HEPES, 5 mM glucose, 1.8 mM MgCl2, and 1.5 mM CaCl2; erythrocytes were loaded with 1 μM Fluo-3 AM in the dark at 37 °C. Loaded cells were centrifuged at 500×g, and the final concentration of packed erythrocytes was 1% in isotonic buffer; for fluorescence measurements, 100 μl of cell suspension was added to 2.5 ml of isotonic buffer at 37 °C and under constant magnetic stirring using a spectrofluorophotometer (RF-Shimadzu 5301PC). The sample was measured with the pair excitation/emission at 500/515 nm. Calibrations were performed as previously described [27, 33].
PS externalization
The erythrocytes were diluted 1:100 in a binding buffer consisting of 10 mM HEPES-Na, pH 7.4, 136 mM NaCl, and 2.5 mM KCl, 2 mM MgCl2, 1 mM NaH2PO4, 5 mM glucose, 5 mg/ml BSA, and 2.5 mM CaCl2. An aliquot of 100 μM Annexin V-FITC was added to a concentration of 100 μM of propidium iodide buffer. Samples were incubated at room temperature in the dark. Erythrocytes were analyzed by flow cytometry after staining. The cells were analyzed by forward and side scatter, the fluorescence intensity of Annexin V was measured in the FL-1 channel with an excitation wavelength of 488 nm and an emission wavelength of 530 nm. Cytometric analysis was performed by a FACSCalibur flow cytometer (Bekcton Dickinson, Heidelberg, Germany); 100% of the externalization of phosphatidylserine in erythrocytes was achieved by incubating them with ionophore calcium ionomycin at a concentration of 1 μM [25, 35].
Statistical analysis
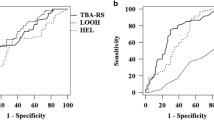
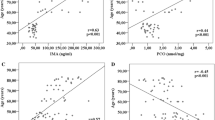
All tests were performed using R [36]. To compare the effects of dyslipidemia and hypertension on different variables, we used robust versions of two-way ANOVA with the package WRS2 [37]. We applied Wilcoxon rank-sum test (Mann–Whitney test) for selected pairwise comparisons. Statistical significance level was set at p = 0.05. Many of our samples failed to adjust to a normal distribution, as observed from Shapiro–Wilk test and Q–Q graphs, and there is no universal consensus as to what two-way ANOVA should be preferred in this event. We decided to employ robust versions of this test (trimmed mean comparisons, two-median comparisons, M-estimators) and the standard two-way ANOVA, and compare their results. Only in two cases (of the 16 tests), different outcomes were produced. We chose those results where most of the tests concurred. In all variables—[Ca2+]i, TBARS, GSH, and PS externalization—we found statistical significance. We then tested pairwise differences selecting as few comparisons as possible, to reduce the increase of type I error. Mann–Whitney test (Wilcoxon rank-sum test) is a standard choice when normality is violated, and it is efficient even under normality conditions. Multivariate procedures supporting Fig. 1 were done with the fcp package [38].
Discrimination of the four studied groups according to the patient values of TBARS and [Ca2+]i. Normotensive non-dyslipidemic patients (NT) (non-filled square), normotensive patients with dyslipidemia (ND) (filled square), hypertensive non-dyslipidemic patients (HT) (non-filled circle), and hypertensive patients with dyslipidemia (HTD) (filled circle)
Results
The age range of the different groups of patients was as follows: normotensive and non-dyslipidemic, 27–43; normotensive with dyslipidemia, 25–47; hypertensive and non-dyslipidemic, 36–58; and hypertensive with dyslipidemia, 37–59 years. The diagnosis and treatment of the patients were performed between 1 and 10 years before the beginning of this study (Table 1).
Treated hypertensive patients (with or without dyslipidemia) showed discrete but statistically significantly higher arterial pressure (Table 1).
The mean concentration of blood glucose was similar in all patients. In 63% of the dyslipidemic normotensive patients, we found abnormal values in two or more parameters of the lipid profile; hypertensive patients with dyslipidemia presented similar conditions in 86% of the cases. Triglyceride concentrations were particularly higher (~200% of the concentration presented in non-dyslipidemic patients). The atherogenic index was higher (~40%) in dyslipidemic patients compared to the non-dyslipidemic ones (Table 1).
As shown in Table 2, hypertensive patients with and without dyslipidemia and dyslipidemic normotensive patients had 1.8, 2.1, and two times, respectively, higher mean lipid peroxidation compared to normotensive non-dyslipidemic patients. In the case of GSH concentration, the mean values were lower (26, 32, and 37%, respectively) in the same groups than in normotensive non-dyslipidemic patients.
Mean [Ca2+]i in hypertensive patients without dyslipidemia were higher (~100%) and even higher (~200%) in hypertensive patients with dyslipidemia, compared to normotensive patients with and without dyslipidemia (Table 3).
The mean PS externalization in hypertensive patients with and without dyslipidemia was 2.3 times higher than that in dyslipidemic normotensive patients and seven times higher than that in normotensive patients without dyslipidemia. Dyslipidemic normotensive patients presented three times higher mean PS externalization than normotensive patients without dyslipidemia (Table 3).
Simple and multiple correlation tests between and among the physiological and biochemical variables (diastolic and systolic pressures, triglycerides, HDL, LDL, total cholesterol) and molecular variables ([Ca2+]i, TBARS, GSH, PS externalization), produced low and non-significant values of r. In order to determine if the analyzed pathological conditions can be associated to a different set of values in the molecular variables, we used the k-means method of classification, to group patients based on the similitude of their molecular parameters. This analysis formed clusters that remarkably corresponded to the four studied groups. Principal component analyses led us to project the whole population, with labels for each group, in the TBARS—[Ca2+]i plane, and the result is shown in Fig. 1. No other combination of two variables or the addition of a third variable to the TBARS—[Ca2+]i pair produced better discrimination. Basically, [Ca2+]i values below 60 nM correspond to normotensive patients, those between 60 and 80 nM were observed in hypertensive non-dyslipidemic patients, whereas patients with both pathologies have the [Ca2+]i values above 80 nM. TBARS separates the normotensive non-dyslipidemic patients from the others, the limiting value being 1.0 nmol/ml.
Discussion
Mean arterial pressure in hypertensive patients is slightly above the mean found in the non-hypertensive ones; this fact, together with the absence of cardiovascular complications, indicates that the pharmacological treatment is controlling the AH.
Dyslipidemic patients, in spite of being pharmacologically treated, presented alterations in the concentrations of cholesterol, triglycerides, C-LDL, and C-HDL and atherogenic index; however, the absence of other chronic degenerative diseases indicates that dyslipidemia is moderately controlled in these patients.
Hypertensive patients with or without dyslipidemia and with only dyslipidemia had a high lipid peroxidation, which implies that both pathologies either isolated or combined produce oxidative damage. There was not an additive effect when both pathologies were present; chronic renal damage and diabetes mellitus produced such an additive effect, both being chronic degenerative pathologies that produce oxidative damage [26]. The absence of additive effect in our case can be accounted for by the effect of antihypertensive drugs (captopril and enalapril) which might also have an antioxidant effect and hence limit the oxidative damage, as has been reported: lipid peroxidation in erythrocytes of treated hypertensive patients was lower than that of the untreated hypertensive ones [12]. Also, hypertensive patients treated for 9 weeks [39] or 3 months [40] presented lower oxidative damage in plasma.
On the other hand, in spontaneously hypertensive rats, treatment with enalapril reduced the TBARS levels and prevented the renal dysfunction, which did occur in untreated rats [41]. One possible mechanism is that the inhibitors of the convertase enzyme reduce the levels of angiotensin II, which stimulates NADP oxidase enzyme and in turn produces superoxide ion. Other pharmacological treatments for patients with hypertension and dyslipidemia also reduced oxidative stress [42].
It is worth to mention that there are other antioxidant mechanisms—besides GSH, not assessed in this study—that could prevent major increments of oxidative damage induced by additive or synergetic insults [43, 44].
Concerning the antioxidant mechanism dependent on GSH, in this work we found that both pathologies, either alone or combined, presented lower levels of GSH than the level found in normotensive non-dyslipidemic patients, which indicates an oxidative stress characterized by an oxidative damage and consumption of GSH. Other authors have found both in erythrocytes and in the blood of hypertensive patients lower levels of GSH compared to those found in normotensive subjects [15, 16, 40]. Moreover, patients with acute myocardial infarction and dyslipidemia also presented lower levels of GSH compared to the control group [45]. The consumption of GSH is effectively compensated by NADPH; therefore, there is a threshold for GSH that is independent of the sort and strength of the insult [44].
According to our results, hypertension is a conditioning factor for higher [Ca2+]i. Hypertensive non-dyslipidemic patients had a higher [Ca2+]i than that found in normotensive patients, and hypertensive dyslipidemic patients had even higher [Ca2+]i, which suggests that lipid alterations in erythrocytes of hypertensive patients either increase the entrance of Ca2+ through calcium channels type L(TPR6), or diminishes the Ca2+ extrusion due to the inhibition of calcium ATPase. Oxidative stress, and even more the lowering of GSH concentration, can induce an increment in [Ca2+]i through the activation of the non-selective cation channels which allow a higher entrance of Ca2+ [46]. However, the high [Ca2+]i concentration found in hypertensive patients with dyslipidemia does not correspond to a lower concentration of GSH or a higher oxidative damage, which suggests that another type of stress might be involved in the increment of [Ca2+]i in erythrocytes of these patients, as has been suggested with other models and conditions [23, 29, 47]. Further research should seek to reveal mechanisms of entry and expulsion of calcium in erythrocytes of hypertensive patients, as we have already performed in lead-incubated erythrocytes and in lead-intoxicated patients [35, 48].
It is known that oxidative stress can affect the extrusion of Ca2+ by reducing the activity of plasma membrane Ca2+ pump, and that endogenous and exogenous prostaglandins can increase the activity of the calcium non-selective cationic channels through mechanical or osmotic stress. These mechanisms might also occur in hypertensive patients with hydroelectrolytic alterations, where a dyslipidemic condition or a peripheral vascular resistance could intensify its effects [49, 50].
Patients with dyslipidemia alone did not have a higher [Ca2+]i, despite the increment of oxidative damage and the reduction of the GSH concentration, which accentuates the peculiarity of the hypertensive condition and hints that oxidative stress is not the main factor that causes an increment in the [Ca2+]i. In this case, the lipidic condition of erythrocytes must be studied with respect to Ca2+ erythrocytic mobility independently of an oxidative stress condition, taking into account the energetic status and the structural stability of erythrocytes [47].
We found that hypertension is associated to heightened levels of eryptosis. Hypertensive patients, with or without dyslipidemia, had a higher percentage of PS externalization than the normotensive patients had. An increment in PS externalization has been associated with a corresponding increment in [Ca2+]i [23, 28], but dyslipidemic hypertensive patients presented the highest [Ca2+]i, which does not correspond to the higher values of PS externalization. It is possible that an upper threshold concentration of erythrocytes with PS externalization is imposed by the removal that macrophages implement, which would make unattainable the determination of higher concentrations of such erythrocytes, even if they occur.
In hypertensive dyslipidemic patients, the remarkably high levels of [Ca2+]i do not correspond to the levels found in PS externalization, which could also be possibly due to a reduction in the activity of scramblase. It has been suggested that the increment of cholesterol in plasma corresponds to an increment of cholesterol in erythrocyte membrane [51]. It is also known that the translocase responsible for PS externalization can lose sensitivity to [Ca2+]i due a rise in the concentration of cholesterol in the plasmatic membrane [52]. In in vitro studies in both human erythrocytes and liposomes enriched with cholesterol, the scramblase activity is inhibited [53], despite the increment of [Ca2+]i which dissociates the [Ca2+]i and PS externalization. It would be necessary to determine the concentration of cholesterol and scramblase activity in erythrocytes in hypertensive dyslipidemic patients to ascertain this possible explanation.
Dyslipidemic patients without hypertension had a higher PS externalization than normotensive non-dyslipidemic patients, which does not correspond to the absence of a statistically significant difference of [Ca2+]i. The fact that normotensive dyslipidemic patients were in oxidative stress and oxidative damage strengthens the idea that oxidative stress is not the main factor for the increment of [Ca2+]i. Besides, the increment in PS externalization in these patients implies that there are other signaling pathways, in the case of dyslipidemia, which lead to eryptosis.
Other authors have proposed that oxysterols, which can be found in high concentrations in patients with familial combined hyperlipidemia [54], can also generate PS externalization through the increment in the concentration of PGE2 in human erythrocytes in vitro [55].
The former analysis concentrated on the effect of the pathologies upon each molecular variable considered individually. To see if the set of molecular variables as a whole reflected distinctly the effect of each pathology considered alone or in combination, we used principal coordinates techniques to project on a plane, for each patient, the set of values of the four variables ([Ca2+]i, TBARS, PS externalization, and GSH). The components of the principal coordinates indicated that two variables were sufficient to produce such a distinction: TBARS and [Ca2+]i. The TBARS values were enough to separate the groups of patients with pathologies from the clinically healthy group, whereas the [Ca2+]i values discriminate normotensive from hypertensive patients, and within the latter, dyslipidemic from the non-dyslipidemic patients. The graph also hints that [Ca2+]i is a major signaling both in dyslipidemia and hypertension, and that the perturbation in [Ca2+]i is higher in hypertension which is a more severe pathology. The [Ca2+]i is affected by different causes and not necessarily is produced by oxidation. The fact that adding PS externalization to the graph does not improve the separation between the groups supports the idea that PS externalization has not [Ca2+]i as a unique signaling in the eryptotic process.
The results of this work indicate that hypertensive patients show oxidative stress, increments of [Ca2+]i, and also higher levels of eryptosis. These results should be compared under different clinical conditions to determine its possible value in the prognosis of stages and treatment response for hypertension. Our results also show that these pathologies and their interaction involve complex molecular signals. The participation of mechanical, osmotic, and energetic stresses should be considered, for these mechanisms have been suggested to affect erythrocytes of patients with these pathologies; thus, the oxidative stress would be relegated to a partial participation. Likewise, [Ca2+]i cannot account for the quantitative increments in eryptosis; therefore, other molecular signals must be found. Additionally, metabolic factors that modify [Ca2+]i and PS externalization, such as ATP and cholesterol concentration in erythrocytes, should also be considered. Future work addressing the scramblase activity, prostaglandin concentration, ceramide, and cholesterol in erythrocytes might help identify signaling paths that correspond to hypertension and dyslipidemia pathologies.
References
World Health Organization (2013) Global brief on hypertension—silent killers, global public health crisis, World health day 2013. http://apps.who.int/iris/bitstream/10665/79059/1/WHO_DCO_WHD_2013.2_eng.pdf?ua=1
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussoli-no ME, Nichol G, Paynter NP, Schreiner PJ, Sorlie PD, Stein J, Turan TN, Virani SS, Wong ND, Woo D, Turner MB, on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee (2012) Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation 127:e6–e245. doi:10.1161/CIR.0b013e31823ac046
Haffner SM, Lehto S, Rönnemaa T, Pyörälä K, Laakso M (1998) Mortality from coronary heart disease in subjects with type 2 diabetes and nondiabetic subjects with and without prior myocardial infarction. N Engl J Med 339:229–234. doi:10.1056/NEJM199807233390404
Davy KP, Hall JE (2004) Obesity and hypertension: two epidemics or one? Am J Physiol Regul Integr Comp Physiol 286(5):R803–R813. doi:10.1152/ajpregu.00707.2003
Dalal JJ, Padmanabhan TNC, Jain P, Patil S, Vasnawala H, Gulati A (2012) Lipitension: interplay between dyslipidemia and hypertension. Indian J Endocrinol Metab 16(2):240–245. doi:10.4103/2230-8210.93742
Reiner Z, Catapano AL, De Backer G, Graham I, Taskinen MR, Wiklund O, Agewall S, Alegria E, Chapman MJ, Durrington P, Erdine S, Halcox J, Hobbs R, Kjekshus J, Filardi PP, Riccardi G, Storey RF, Wood D (2011) ESC/EAS guidelines for the management of dyslipidemias. Eur Heart J 32:1769–1818. doi:10.1093/eurheartj/ehr158
Halperin RO, Sesso HD, Jing M, Buring JE, Stampfer MJ, Gaziano M (2006) Dyslipidemias and the risk of incident hypertension in men. Hypertension 47(1):45–50. doi:10.1161/01.HYP.0000196306.42418.0e
Touyz RM (2004) Reactive oxygen species, vascular oxidative stress, and redox signaling in hypertension. What is the clinical significance? Hypertension 44(3):248–252. doi:10.1161/01.HYP.0000138070.47616.9d
Minuz P, Patrignani P, Gaino S, Seta F, Capone M, Tacconelli S, Degan M, Faccini G, Fornasiero A, Talamini G, Tommasoli R, Arosio E, Santonastaso C, Lechi A, Patrono C (2004) Determinants of platelet activation in human essential hypertension. Hypertension 43:64–70. doi:10.1161/01.HYP.0000105109.44620.1B
Grossman E (2008) Does increase oxidative stress cause hypertension? Diabetes Care 31:2. doi:10.2337/dc08-s246
Rodrigo R, Prat H, Passalacqua W, Araya J, Guichard C, Bachler JP (2007) Relation between oxidative stress and essential hypertension. Hypertens Res 30(12):1159–1167. doi:10.1291/hypres.30.1159
Cvetkovic T, Velickovic- Radovanovic R, Djordjevic V, Radenkovic S, Vlahovic P, Stefanovic N (2012) Evidences for oxidative stress in essential hypertension. Cent Eur J 7(5):610–616. doi:10.2478/s11536-012-0043-7
Ward NC, Hodgson JM, Puddey IB, Mori TA, Beilin LJ, Croft KD (2004) Oxidative stress in human hypertension: association with antihypertensive treatment, gender, nutrition, and lifestyle. Free Radic Biol Med 36:226–232. doi:10.1016/j.freeradbiomed.2003.10.021
Lima Vasconcelos S, Fonseca Goulart M, Mendoca da Silva M, Manfredini V, Benfato M, Antas Rabelo L, Fontes G (2011) Markers of redox imbalance in the blood of hypertensive patients of a community in Northeastern Brazil. Arq Bras Cardiol 97(2):141–147. doi:10.1590/S0066-782X2011001100008
Muda P, Kampus P, Zilmer M, Zilmer K, Kairane C, Ristimae T, Fischer K, Teesalau R (2003) Homocysteine and red blood cell glutathione as indices for the middle. Aged untreated essential hypertension patients. J Hypertens 21:2329–2333. doi:10.1097/01.hjh.0000098158.70956.85
Redón J, Oliva M, Tormos C, Giner V, Chaves J, Iradi R, Sáez G (2003) Antioxidant activities and oxidative stress byproducts in human hypertension. Hypertension 41:1096–1101. doi:10.1161/01.HYP.0000068370.21009.38
Shantha Kumari N, Hemalatha, Sheethal KC, Shwetha, Rashmi TM (2013) Antioxidant status, oxidative stress and lipid profile in essential hypertensive men. JEMDS 2(17):2950–2955. doi:10.14260/jemds/640
Rybka J, Kupczyk D, Kedziora-Kornatowska K, Motyl J, Czuczejko J, Szewczyk-Golec K, Kozakiewicz M, Pawluk H, Carvalho LA, Kedziora J (2011) Glutathione-related antioxidant defense system in elderly patients treated for hypertension. Cardiovasc Toxicol 11:1–9. doi:10.1007/s12012-010-9096-5
Matsuda M, Shimomura I (2013) Increased oxidative stress in obesity: implications for metabolic syndrome, diabetes, hypertension, dyslipidemia, atherosclerosis, and cancer. Obes Res Clin Pract 7:e330–e341. doi:10.1016/j.orcp.2013.05.004
Tangvarasittichai S (2015) Oxidative stress, insulin resistance, dyslipidemia and type 2 diabetes mellitus. World J Diabetes. doi:10.4239/wjd.v6.i3.456
Myssina S, Huber SM, Birka C, Lang PA, Lang KS, Friedrich B, Risler T, Wiede T, Lang F (2003) Inhibition of erythrocyte cation channels by erythropoietin. J Am Soc Nephrol 14(11):2750–2757. doi:10.1097/01.ASN.0000093253.42641.C1
Lang KS, Lang PA, Bauer C, Duranton C, Wieder T, Huber SM, Lang F (2005) Mechanisms of suicidal erythrocyte death. Cell Physiol Biochem 15(5):195–202. doi:10.1159/000086406
Lang E, Lang F (2015) Triggers, inhibitors, mechanisms, and significance of eryptosis: the suicidal erythrocyte death. Biomed Res Int 2015(2015):513–518. doi:10.1155/2015/513518
Lang PA, Beringer O, Nicolay JP, Amon O, Kempe DS, Hermle T, Attanasio P, Akel A, Schafer R, Friedrich B, Risler T, Baur M, Olbricht CJ, Zimmerhackl LB, Zipfel PF, Wieder T, Lang F (2006) Suicidal death of erythrocytes in recurrent hemolytic uremic syndrome. J Mol Med 84(5):378–388. doi:10.1007/s00109-006-0058-0
Aguilar-Dorado IC, Hernández G, Quintanar-Escorza MA, Maldonado-Vega M, Rosas-Flóres M, Calderón-Salinas JV (2014) Eryptosis in lead-exposed workers. Toxicol Appl Pharmacol 281(2):195–202. doi:10.1016/j.taap.2014.10.003
Calderón-Salinas JV, Muñoz-Reyes EG, Guerrero-Romero JF, Morán Rodríguez-, Bracho-Riquelme MRL, Carrera-Gracia MA, Quintanar-Escorza MA (2011) Eryptosis and oxidative damage in type 2 diabetic mellitus patients with chronic kidney disease. Mol Cell Biochem 357(1–2):171–179. doi:10.1007/s11010-011-0887-1
Lindner A, Hinds TR, Davidson RC, Vicenzi FF (1993) Increased cytosolic free calcium in red blood cells is associated with essential hypertension in humans. Am J Hypertens 6(9):771–779. doi:10.1093/ajh/6.9.771
Lang F, Qadri SM (2012) Mechanisms and significance of eryptosis, the suicidal death of erythrocytes. Blood Purif 33(1–3):125–130
Lang E, Bissinger R, Gulbins E, Lang F (2015) Ceramide in the regulation of eryptosis, the suicidal erythrocyte death. Apoptosis 5:758–767. doi:10.1007/s10495-015-1094-4
Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr et al (2003) The National High Blood Pressure Education Program Coordinating Committee. Seventh report of the joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 42:1206–1252
Jain SK, McVie R, Duett J, Herbst JJ (1989) Erythrocyte membrane lipid peroxidation and glycosylated hemoglobin in diabetes. Diabetes 38(12):1539–1543. doi:10.2337/diab.38.12.1539
Quintanar-Escorza MA, González-Martínez MT, Navarro L, Maldonado M, Arévalo B, Calderón-Salinas JV (2007) Intracellular free calcium concentration and calcium transport in human erythrocytes of lead-exposed workers. Toxicol Appl Pharmacol 220:1–8. doi:10.1016/j.taap.2006.10.016
Rendón-Ramírez AL, Maldonado-Vega M, Quintanar-Escorza MA, Hernández G, Arévalo-Rivas BI, Zentella-Dehesa A, Calderón-Salinas JV (2014) Effect of vitamin E and C supplementation on oxidative damage and total antioxidant capacity in lead-exposed workers. Environ Toxicol Pharmacol 37(1):45–54. doi:10.1016/j.etap.2013.10.016
Akerboom TPM, Sies H (1981) Assay of glutathione, glutathione disulfide, and glutathione mixed disulfides in biological samples. Methods Enzymol 77:373–382. doi:10.1016/S0076-6879(81)77050-2
Tait JF, Gibson D (1992) Phospholipid binding of annexin V: effects of calcium and membrane phosphatidylserine content. Arch Biochem Biophys 298:187–191. doi:10.1016/0003-9861(92)90111-9
R Core Team (2016). R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/
Mair P, Schoenbrodt F, Wilcox R (2015) WRS2: Wilcox robust estimation and testing
Hennig C (2015) fpc: flexible procedures for clustering. R package version 2.1-10. https://CRAN.R-project.org/package=fpc
Deoghare S, Kantharia N (2013) Effect of atenolol and enalapril treatment on oxidative stress parameters in patients with essential hypertension. Int J Basic Clin Pharmacol 2(3):252–256. doi:10.5455/2319-2003.ijbcp20130604
Donmez G, Derici U, Erbas D, Arinsoy T, Onk A, Sindel S, Hasanoglu E (2002) The effects of losartan and enalapril therapies on the levels of nitric oxide, malondialdehyde, and glutathione in patients with essential hypertension. Jpn J Physiol 52:435–440. doi:10.2170/jjphysiol.52.435
Chandran G, Sirajudeen K, Yussof N, Swany M, Samarendra M (2014) Effect of the antihypertensive drug enalapril on oxidative stress markers and antioxidant enzymes in kidney of spontaneously hypertensive rat. Oxid Med Cell Longev. doi:10.1155/2014/608512
Gómez-García A, Martínez Torres G, Ortega-Pierres L, Rodríguez-Ayala E, Álvarez-Aguilar C (2007) Rosuvastatin and metformin decrease inflammation and oxidative stress in patients with hypertension and dyslipidemia. Rev Esp Cardiol 60(12):1242–1249
Maurya PK, Kumar P, Chandra P (2015) Biomarkers of oxidative stress in erythrocytes as a function of human age. World J Methodol 5(4):216–222. doi:10.5662/wjm.v5.i4.216
Pandey KB, Rizvi SI (2011) Biomarkers of oxidative stress in red blood cells. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 155(2):131–136
Bashar T, Akhter N (2014) Study on oxidative stress and antioxidant level in patients with acute myocardial infarction before and after regular treatment. Bangladesh Med Res Counc Bull 40:79–84. doi:10.13140/RG.2.1.4062.2481
Lang KS, Duranton C, Poehlmann H, Myssina S, Bauer C, Lang F, Wieder T, Huber SM (2003) Cation channels trigger apoptotic death of erythrocytes. Cell Death Differ 10(2):249–256. doi:10.1038/sj.cdd.4401144
Pretorius E, du Plooy JN, Bester J (2016) A comprehensive review on eryptosis. Cell Physiol Biochem 39(5):1977–2000
Calderón-Salinas JV, Quintanar-Escorza MA, Hernández-Luna CE, González-Martínez MT (1999) Effect of lead on the calcium transport in human erythrocyte. Hum Exp Toxicol 18(3):146–153
Adrogué H, Madias N (2007) Sodium and potassium in the pathogenesis of hypertension. N Engl J Med 356:1966–1978. doi:10.1056/NEJMra064486
Mayet J, Hughes A (2003) Cardiac and vascular pathophysiology in hypertension. Heart 89:1104–1109. doi:10.1136/heart.89.9.1104
Gottlieb MH (1980) Rates of cholesterol exchange between human erythrocytes and plasma lipoproteins. Biochim Biophys Acta 600:530–541
Van Zwieten R, Bochem A, Hilarius P, Van Bruggen R, Bergkamp F, Hovingh G, Verhoeven A (2012) The cholesterol content of the erythrocyte membrane is an important determinant of phosphatidylserine exposure. Biochim Biophys Acta 1821(12):1493–1500. doi:10.1016/j.bbalip.2012.08.008
Arashiki N, Saito M, Koshino I, Kamata K, Hale J, Mohandas N, Manno S, Takakuwa Y (2016) An unrecognized function of cholesterol: regulating the mechanism controlling membrane phospholipid asymmetry. Biochemistry 55:3504–3513. doi:10.1021/acs.biochem.6b00407
Arca M, Natoli S, Micheletta F, Riggi S, Di Angelantonio E, Montali A, Antonini TM, Antonini R, Diczfalusy U, Iuliano L (2007) Increased plasma levels of oxysterols, in vivo markers of oxidative stress, in patients with familial combined hyperlipidemia: reduction during atorvastatin and fenofibrate therapy. Free Radic Biol Med 42(5):698–705
Tesoriere L, Attanzio A, Allegra M, Cilla A, Gentile C, Livrea M (2014) Oxysterol mixture in hypercholesterolemia-relevant proportion causes oxidative stress-dependent eryptosis. Cell Physiol Biochem 34:1075–1089. doi:10.1159/000366322
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pinzón-Díaz, C.E., Calderón-Salinas, J.V., Rosas-Flores, M.M. et al. Eryptosis and oxidative damage in hypertensive and dyslipidemic patients. Mol Cell Biochem 440, 105–113 (2018). https://doi.org/10.1007/s11010-017-3159-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-017-3159-x