Abstract
Introduction
Reproductive health advantages have been reported among selected immigrants, but few studies have included new immigrants and refugees, nor simultaneously adjusted for socioeconomic, behavioral, and medical disparities.
Methods
We examined the risk of preterm birth (PTB, < 37 weeks’ gestation) among singleton live births in San Diego County from 2007 to 2012. Multivariable regression was used to compare PTB (1) by nativity within racial/ethnic groups and (2) among immigrants compared to United States (US) born Whites, while adjusting for sociodemographic, behavioral, reproductive and medical variables.
Results
Among 230,878 singleton live births, overall PTB prevalence was highest among parturient women who were US-born Blacks (10.9%), Philippine (10.8%) and US-born Filipinas (10.7%), and US-born Asians (8.6%) despite differences in socioeconomic and maternal risk factors, and lowest among Somali (5.5%) migrants. Blacks born in Somalia or outside of the US, had significantly lower overall PTB prevalence compared to US-born Blacks (5.5% vs 7.6% vs 10.9%). Compared to US-born Whites, spontaneous PTB risk was significantly lower among Somali migrants (4.8% vs 3.7%, adjusted relative risk, aRR 0.7 [95% Confidence Intervals 0.5–0.9]), but higher among Philippine migrants (4.8% vs 7.7%, aRR 1.4 [1.3–1.6]). The strongest risk factor for overall PTB among nulliparous US-born Blacks was preexisting diabetes (aRR 3.81 [2.05–7.08]), and preexisting hypertension among Filipinas (aRR: 3.27 [2.36–4.54] and US-born Asians (aRR: 3.64 [1.61–8.24]).
Conclusion
Black migrants had lower PTB prevalence compared to US-born Blacks, but this immigrant advantage was not observed in other racial/ethnic groups. Compared to US-born Whites, Somali migrants had significantly lower risk of spontaneous PTB while Filipinas had elevated risk.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Significance
Current Knowledge: Social disadvantage is associated with adverse reproductive health outcomes, but favorable outcomes have been observed among selected immigrant populations, albeit inconsistent results.
What Does This Study Add?: Preterm birth prevalence was highest among US-born Blacks, Filipinas (US and Philippine born) and US-born Asians despite differences in sociodemographic, behavioral, medical and reproductive characteristics. Compared to US-born Whites, migrants from Somalia had significantly lower PTB risk despite significantly more social disadvantages, infection, anemia, gestational diabetes, obesity, and shorter interpregnancy intervals, while Philippine born migrants had significantly higher PTB risk, despite higher education and few adverse risk behaviors.
Introduction
Adverse reproductive outcomes can manifest disabling effects, including, but not limited to, vision and hearing impairment at infancy, to metabolic abnormalities throughout the lifecourse (Howson et al. 2013; Blencowe et al. 2012; Raju et al. 2017). Preterm birth (PTN, < 37 weeks’ gestation) is the leading cause of death among children under 5 years of age, and prevalence is increasing globally, particularly in resource limited countries (Howson et al. 2013; Blencowe et al. 2012). Paradoxically, previous studies have reported similar or favorable reproductive outcomes among immigrant women compared to US-born women of the same race/ethnicity, and compared to US-born White women, despite disparities in health care access and socioeconomic status (Singh and Yu 1996; Flores et al. 2012). This “Healthy Migrant Effect” describes observations of favorable health status among selected migrants compared to the majority population in the host country, however this health advantage dissipates as health outcomes resemble the host country with longer migration and in subsequent generations of migrant progeny. Lower PTB prevalence has been reported among selected immigrants from Latin America, Asia, and sub-Saharan Africa (Flores et al. 2012; Miller et al. 2016; Elo et al. 2014; Oliver et al. 2018; Small et al. 2008; Belihu et al. 2016; Sorbye et al. 2014). However, some reports have shown inconsistent results, including disparities within racial/ethnic categories (Sanchez-Vaznaugh et al. 2016; Vang et al. 2015; Bartsch et al. 2017). Asian-Americans have low PTB prevalence when reported collectively, however Filipino, Hmong, Cambodian and Lao/Thai women have significantly higher PTB risk compared to Chinese, Japanese, Korean, Vietnamese and Asian-Indian women (Vang et al. 2015).
It is unclear if such health advantages among immigrant parturients are limited to selected countries within broadly reported geographic regions, or are observed among additional, albeit understudied migrants. Protective factors in these populations can inform interventions to reduce reproductive health disparities among all Americans. Relevant to these issues, one geographic setting that could be informative is a large and varied metropolitan, suburban and rural region at the southern-most border of California, San Diego County. The ethnic diversity in San Diego, its proximity to the busiest land border crossing in the Western Hemisphere (United States General Services Administration 2019) where subpopulations reside binationally, sizeable immigrant populations from Mexico and Asia, and long history of resettling refugees from Vietnam, Somalia, Iraq, Syria, and Afghanistan (Aguillera 2017; Refugee Arrivals Data San Diego County Health and Human Services Agency 2019) enable meaningful evaluation of reproductive outcomes by race/ethnicity and nativity.
Objectives
To determine if the prevalence and risk factors for preterm birth differ within the cultural context of selected racial/ethnic groups, we aimed to compare overall and spontaneous PTB risk among immigrant and US-born parturients within the same racial/ethnic categories. To identify health disparities and health advantages among selected immigrant women, our second objective was to compare PTB risk among immigrant women compared to US-born non-Hispanic White women, adjusting for sociodemographic, behavioral, medical and reproductive characteristics.
Methods
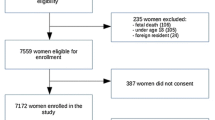
In this retrospective cohort study, our sample was drawn from singleton live births, born to women residing in San Diego County, California between January 1, 2007, and December 31, 2012. The sample was restricted to mothers and infants linked to a birth cohort database maintained by the California Office of Statewide Health Planning and Development. This database contains linked birth and death certificates, as well as detailed information on maternal and infant characteristics, hospital discharge diagnoses, and procedures recorded as early as 1 year before delivery and as late as 1 year post-delivery. Data files provided diagnoses and procedure codes based on the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM). Subjects with any of the following conditions were excluded from analyses: gestational age at delivery less than 20 weeks or more than 44 weeks based on the best obstetrical estimate reported on the birth certificate (Talge et al. 2014), unknown maternal age, and reported major congenital malformation of the infant (Baer et al. 2014).
Mother’s country of birth, race, and ethnicity were obtained from birth certificate records. Women were classified as Hispanic when listed as Mexican, Puerto Rican, Cuban, Central American, South American or other Spanish/Hispanic origin. Race was obtained from the single condensed race variable populated by consolidating three provided race categories. The consolidated races include White, Black, American Indian/Alaska Native, Asian, Hawaiian/Pacific Islander, Other, and two or more races. Women of Hispanic origin were only included in the Hispanic analyses. The three provided race categories (not the single consolidated race variable) were used to identify Filipina women, who were reported separately from Other Asians.
Mother’s age at birth, infant birthweight, and best obstetric estimated gestational age at birth were obtained from birth certificate records. When data were available, preterm births were categorized as either spontaneous (based on ICD-9-CM or birth certificate codes suggesting premature rupture of the membranes, spontaneous labor, or tocolytic administration) or indicated PTB (based on induction, artificial rupture of membrane, or cesarean section (C-section) ICD-9-CM or birth certificate codes). Other maternal characteristics derived from birth certificate data included: years of completed education, pre-pregnancy body mass index (BMI), smoking, illicit drug and alcohol use, mental health diagnosis, anemia, hypertension (preexisting or gestational with and without preeclampsia), diabetes (preexisting or gestational), and infection (based on the ICD-9-CM four digit codes contained in the hospital discharge files). Socioeconomic status was based on Medi-Cal (California’s Medicaid program) coverage for the delivery, and enrollment in the Special Supplementation Program for Women, Infants and Children (WIC). Among multiparous women, prior PTB, prior cesarean delivery, and interpregnancy interval (estimated as months from the completion of the prior pregnancy to conception of the current pregnancy) were also obtained.
Logistic regression was used to calculate relative risk (RR) and 95% confidence intervals [95% CI] comparing overall, spontaneous, and indicated PTB by nativity within racial and ethnic groups. Adjusted RRs were calculated adjusting for sociodemographic, behavioral, medical and reproductive characteristics that differed significantly between foreign-born and US-born women of the same race/ethnicity. US-born women within each race/ethnicity comprised the referent group for the first objective.
Similar analyses were performed for the second objective, comparing PTB prevalence and risk among foreign-born women with US-born non-Hispanic White women, where the latter comprised the referent group. Among groups with the highest PTB prevalence, multivariable analysis was performed among nulliparous women to identify covariates associated with PTB without the confounding effects of prior PTB.
All analyses were performed using Statistical Analysis Software version 9.4 (Cary, NC). Methods and protocols for the study were approved by the Committee for the Protection of Human Subjects within the Health and Human Services Agency of the State of California.
Results
Between 2007 and 2012, linked birth certificate and hospitalization data were available for 230,878 singleton live births with available maternal race/ethnicity and nativity data. As shown in Table 1, almost half of the parturients were Hispanic (45.5%), followed by non-Hispanic Whites (30.7%), Filipinas (4.4%), Other Asians (6.3%), Blacks (3.8%), and women of Other race/ethnicity (2.7%). Almost half (41.3%) of all parturients were immigrants, but this proportion varied by race/ethnicity, where over half (55.9%) of Hispanic, three-fourths (74.1%) of Filipina, and the majority (83.9%) of other Asian mothers were foreign-born. Comparatively, one-fourth (23.8%) of Black parturients, 15.1% of women of Other race/ethnicity, and 12.5% of White mothers were foreign-born. The majority of foreign-born Hispanic and Black women were born in Mexico and Somalia respectively.
Foreign-born women were more likely to be older and less likely to be nulliparous or obese, to have a diagnosed mental illness, or use drugs or alcohol during pregnancy compared to US-born women within the same racial/ethnic group. Other maternal factors, such as years of education, socioeconomic status (based on Medi-Cal coverage and WIC participation), preexisting diabetes and hypertension, previous cesarean delivery, and interpregnancy interval were not consistent by nativity (Supplemental Table 1).
Preterm birth prevalence was highest among US-born Black women (10.9%), followed by Filipinas whether born in the Philippines (10.8%) or the US (10.7%), and US-born Asian (8.6%) women, and lowest among foreign-born Somali (5.5%), “Other” (5.7%), White (6.0%) and Mexican women (6.1%, Table 2). These observations persisted when limited to spontaneous PTBs. Table 2 shows adjusted relative risk differed by nativity within racial/ethnic categories. Adjusted PTB risk was significantly lower among infants of women born in Somalia compared to US-born Black women (5.5% vs 10.9%; aRR: 0.6, 95% CI [0.5–0.8]), and these observations persisted when limited to spontaneous PTB (3.7% vs 8.1%, aRR: 0.6 [0.4–0.8], Table 2). Similarly, other foreign-born Black women (not born in Somalia) also had lower risk of spontaneous PTB compared to US-born Black women (5.0% vs 8.1%, aRR: 0.7 [0.5–0.9]. Compared to US-born Hispanics, migrant Mexican women had marginally lower risk of overall (6.1% vs 7.2%, aRR: 0.9 [0.9–1.0] and spontaneous PTB (4.5% vs 5.4%, aRR: 0.9 [0.9–1.0], p < 0.05), however PTB risk did not differ between US-born versus foreign-born Hispanics (not born in Mexico, Table 2). No differences in overall or spontaneous PTB risk were observed by nativity among Whites, non-Mexican Hispanics, Filipinas, Asians, nor women of “Other” race/ethnic categories. Indicated PTBs did not differ by nativity within any racial/ethnic categories (Table 2).
Table 3 compares demographic, behavioral, medical, and reproductive history among US-born Whites compared to foreign-born parturients. Compared to US-born White women, foreign-born Hispanics and Mexicans were more likely to give birth as teenagers (ages < 18 years), while migrants from the Philippines and other Asian countries had older maternal age, higher education, and were less likely to be overweight or obese compared to US-born White women. All migrants were less likely to smoke, use drugs/alcohol use, have a mental health diagnosis, but were more likely to have gestational diabetes compared to US-born White women. With the exception of Asian women, all migrants were more likely to receive Medi-Cal insurance and WIC, to have anemia, to enter prenatal care in the second trimester of pregnancy, and were less likely to be nulliparous compared to US-born White women. Among multiparous women, compared to White women, foreign-born Mexican and other Hispanic women were less likely to have a prior PTB. Compared to US-born Whites, immigrant Mexican, other Hispanic, other Black, and Filipina women were more likely to have had a cesarean delivery. Foreign-born Mexican, Hispanics, Filipinas, Asians and women of “Other” race/ethnicity were less likely to have short (6 to 23 months) interpregnancy intervals, however foreign-born Somali and women of “Other” race/ethnicity were more likely to have very short (< 6 months) interpregnancy intervals compared to US-born White women.
Table 4 compares PTB outcomes among US-born Whites compared to migrants by race/ethnicity, adjusting for maternal factors differing between foreign-born and US-born White women identified in Table 3. Compared to US-born Whites, foreign-born Somali women had lower risk of spontaneous PTB (4.8% vs 3.7, aRR: 0.7 [0.5–0.9] and a marginally lower risk of overall PTB (6.4% vs 5.5%, aRR: 0.8 [0.6–1.0], p < 0.05). Whereas, compared to US-born Whites, Philippine born migrants had significantly higher prevalence of overall (6.4% vs 10.8%, aRR: 1.4 [1.3–1.6], spontaneous (4.8% vs 7.7%, aRR: 1.4 [1.3–1.6], and indicated (1.3% vs 2.4%, aRR: 1.4 [1.2–1.7] PTBs. Foreign-born Somali women had the highest prevalence of infections during pregnancy, late entry into prenatal care, very short interpregnancy intervals, multiparity, and socioeconomic disadvantage (Table 3). Multivariable analysis among Somalia born women showed that a short interpregnancy interval (6 to 23 months) was inversely associated with PTB (aRR: 0.5 [0.3–0.9], while hypertension, previous cesarean delivery, and mental illness were independently associated with PTB (data not shown). Whereas, Philippine born women had the highest prevalence of gestational diabetes, preexisting hypertension, gestational hypertension, and years of education (Table 3), and low prevalence of social disadvantage, inadequate prenatal care, obesity and risky behaviors. Multivariable analysis showed that among Philippine born women, previous PTB, preexisting hypertension, gestational hypertension, and gestational diabetes were independently associated with PTB (data not shown).
Table 5 shows covariates associated with PTB in multivariable analysis among nulliparous women with the highest PTB prevalence, namely, US-born Black, Filipina (US and Philippine born) and US-born Asians. Among nulliparous US-born Black women, preexisting and gestational hypertension, preexisting and gestational diabetes, having fewer than 3 prenatal care visits, drug/alcohol use, and infection were associated with PTB, and these risk factors were similar for spontaneous PTB, except for the number of prenatal care visits (Table 5). Among nulliparous Filipinas, born in the US or the Philippines, preexisting and gestational hypertension, preexisting diabetes, infection, and having fewer than 3 prenatal visits were associated with PTB, while preexisting and gestational hypertension, infection, drug/alcohol use, and having less than 3 prenatal visits were associated with spontaneous PTB. Among US-born Asian women, preexisting and gestational hypertension, and preexisting diabetes were the only covariates associated with PTB, while preexisting diabetes and overweight were independently associated with spontaneous PTB. The proportion with modifiable risk behaviors was small including 3.0% of US-born Blacks and 2.8% of Filipinas with fewer than < 3 prenatal visits, and 2.2% of Filipinas with reported drug/alcohol use.
Discussion
Preterm birth prevalence was highest among US-born Blacks, Filipinas (regardless of birthplace) and US-born Asians despite differences in sociodemographic, behavioral, medical and reproductive characteristics. When stratified by nativity, compared to US-born Black women, Somali migrants had lower risk of both overall and spontaneous PTB, while foreign-born Black women had lower risk of spontaneous PTB. Compared to US-born White women, migrants from Somalia had lower risk of spontaneous PTB despite more social disadvantage, while Philippine born migrants had significantly higher risk of overall, spontaneous, and indicated PTB, despite higher education and few adverse risk behaviors compared to US-born White women.
Health advantages were evident among black immigrants born outside of the US, but unlike previous studies, these health advantages were not observed among immigrant White, Hispanic, Filipina, Asian, nor women of “Other” race/ethnicities compared to their US-born counterparts. The “healthy migrant” effect observed in other cohorts were not observed in such women. Compared to US-born Whites, migrants from Somalia had significantly lower risk of PTB despite significantly more social disadvantages, infection, anemia, gestational diabetes and preexisting diabetes, underweight as well as obesity, and shorter interpregnancy intervals. Our analysis showed that shorter interpregnancy intervals were protective against PTB among Somali migrants, but was otherwise unable to identify covariates associated with this apparent health advantage among Somali migrants. Prospective studies that include long-term Somali migrants and US-born Somali women, could inform modifiable practices that could benefit high risk populations.
Our findings of lower PTB risk among foreign-born Blacks are consistent with prior reports among Black migrants born in sub-Saharan Africa compared to Caribbean born and US-born Blacks (Elo et al. 2014; Oliver et al. 2018). The health advantage reported by Elo et al. among Sub-Saharan African-born and Caribbean-born black women compared to US-born non-Hispanic black women was not explained by sociodemographic characteristics, health behaviors, nor medical risk factors, similar to our observations (Elo et al. 2014). A meta-analysis of pregnancy outcomes among 10,431 Somali-born migrants compared with parturients born in Australia, Belgium, Canada, Finland, Norway and Sweden, also showed significantly lower PTB prevalence among Somali migrants compared to non-immigrants (Small et al. 2008) Our results are similar to those of a population-based study in Australia, where Somalia born women had significantly lower PTB prevalence compared to Australia born women, however PTB prevalence did not differ among migrants from other East African countries, including Eritrea, Ethiopia, and Sudan compared to Australia born parturients (Belihu et al. 2016). Moreover, our observations mirror those of a population-based study in Norway where overall and spontaneous PTB prevalence was lowest among Somalia born migrants compared to Norway-born parturients, and PTB was highest among migrants from the Philippines (Sørbye et al. 2014). Our observations were also consistent with a population-based study in Ontario, Canada, where PTB risk was highest among migrants from the Philippines compared to other Asian migrants (Bartsch et al. 2017).
Preterm birth prevalence has historically been highest among US-born Black mothers, and lowest for Asian-Americans, (Martin et al. 2017) but collective reporting of all Asian subgroups, including with Pacific Islanders, obscures important health disparities. Filipinos comprise almost half (43%) of Asian/Pacific Islanders in San Diego County, (County of San Diego, Health & Human Services Agency, Public Health Services 2013) and disaggregating Filipinos from Asians showed that PTB prevalence was nearly identical among US-born Blacks and Filipinas (both Philippine and US-born). Philippine born mothers had the highest prevalence of both gestational hypertension and gestational diabetes in our sample, consistent with Northern California data (Hedderson et al. 2012). Previous PTB, preexisting hypertension, gestational hypertension, and gestational diabetes were the strongest determinants of PTB among Philippine born migrants in our sample. A study among 60 Filipino parturients in Hawaii showed genetic variants and higher levels of the hormone relaxin were associated with an increased risk of premature rupture of fetal membranes and spontaneous PTBs (Rocha et al. 2013).
Mexican migrants in our sample had marginally lower PTB risk compared to US-born Latinas. Prior reports from Utah showed foreign-born Hispanics showed lower PTB risk compared to US-born Whites, and lower PTB risk compared to US-born Hispanics, (Flores et al. 2012) while in California, Mexican and other Hispanic migrants had similar PTB risk, after adjusting for social disadvantage (Sanchez-Vaznaugh et al. 2016). Guendelman et al. showed PTB prevalence among Mexican immigrants in California was significantly higher compared to parturients in Mexico, and persisted after controlling for age, education and healthcare (Guendelman et al. 2015) We did not have information on years since immigration, but the observed marginal health advantages among Mexican immigrants in San Diego compared to previous studies might be due to, presumably, shorter duration of migration in San Diego, or maintaining a binational lifestyle, given the proximity to Mexico. This proximity may have enhanced access to protective, traditional practices, and social support for maternal and infant care.
The etiology of selected health advantages among migrants compared to US-born White women remains unclear, and was not explained by differences in demographic, behavioral, anthropometric, medical nor reproductive characteristics. Migrant women were significantly less likely to engage in high risk behaviors, however smoking prevalence (4.5%) and drug/alcohol use (1.8%) use were infrequently recorded in the total sample. Reproductive health advantages have been hypothesized to be related to stronger social ties and support, (Almeida 2014) however, we did not have access to such information.
Our strengths include a large, ethnically diverse sample size, where almost half (41.3%) of parturients are immigrants or refugee populations, including the second largest Somali population in the US. The population based linked birth certificate and hospitalization dataset offers external validity, enables ascertainment of selected conditions, including distinguishing spontaneous from indicated PTBs, and includes sociodemographic, anthropometric, behavioral, medical, and reproductive information.
The limitations include the absence of paternal data, immigration data such as age at and years since migration, English fluency, refugee status, including secondary refugee status if San Diego was not the primary resettlement assignment, a broad spectrum of cultural variables, and social support data. Selected health systems information were also not available, including barriers such as health care access, availability of language interpreters, gender concordant providers for selected cultural preferences, and fiscal resources for co-payments and medication.
The absence of recent data and the demographic shifts in migration patterns also require acknowledgement. San Diego resettled 3100 refugees in 2016, and an average of 2000 refugees annually in previous years, (Morrisey 2017; San Diego County Health and Human Services Agency 2019) however this number has declined significantly, with just 844 refugee arrivals between October 2017 and September 2018 (Aguillera 2017). Further, fewer Somali refugees arrived after 2014, where the majority of refugee arrivals have been from Iraq, Syria, Afghanistan, and in recent years, from Haiti and the Democratic Republic of Congo (Aguillera 2017). Birth outcomes to Iraqi, Syrian, and Afghan migrants and refugees were not disaggregated from Other or unspecified racial/ethnic categories, or might have been classified as foreign-born Whites. Information bias might have been present if behavioral data were self-reported, such that women might have underreported their smoking, illicit drug, and alcohol use during pregnancy and/or these behaviors were not documented. Such behavioral data were not validated, nor was reproductive history, particularly among pregnancies which occurred outside of San Diego County. Among the multiparous women, the prevalence of previous PTB was unusually low, and is likely limited to previous births in San Diego County. Similarly, interpregnancy intervals were computed based on available birth certificate records for each woman, and did not represent non-San Diego births, nor pregnancies resulting in stillbirths or fetal losses which would have been at risk for PTB.
In summary, we found health advantages, including lower risk of spontaneous PTB among Somali and other foreign-born Blacks compared to US-born Blacks, and a marginally lower risk among Mexican migrants compared to US-born Hispanics. Compared to US-born White women, women born in Somalia had significantly lower risk of spontaneous PTB, while Philippine born women had significantly higher risk of spontaneous and indicated PTB. The etiology of PTB among these migrant women warrants further investigation, including protective factors which can inform interventions to reduce preterm births and consequent co-morbidities among all Americans. Finally, despite disparate social disadvantages, body size, and behaviors, PTB prevalence was similarly elevated among US-born Blacks, Filipinas, and US-born Asians, with preexisting and gestational hypertension and diabetes as the most important risk factors for PTB. Primary Care providers and Obstetricians/Gynecologists should consider screening for and managing gestational hypertension and diabetes among high risk women. Etiologic studies to understand the pathophysiology of these disparities, which include myriad influences such as the vaginal microbiome, genetic, epigenetic and metabolomic factors, immigrant and refugee related variables, social support, cultural behaviors and beliefs, stress, racism and microaggressions, resiliency, and coping mechanisms, and health systems variable are urgently need to inform effective interventions to benefit all women and infants.
References
Aguillera, E. (2017). San Diego welcomes more refugees than any other California county. July 20. Retrieved July 5, 2019, from https://calmatters.org/articles/san-diego-welcomes-refugees-california-county/.
Almeida, J., Mulready-Ward, C., Bettegowda, V. R., & Ahluwalia, I. B. (2014). Racial/ethnic and nativity differences in birth outcomes among mothers in New York City: The role of social ties and social support. Maternal and Child Health Journal,18, 90–100.
Baer, R. J., Norton, M. E., Shaw, G. M., Flessel, M. C., Goldman, S., Currier, R. J., et al. (2014). Risk of selected structural abnormalities in infants after increased nuchal translucency measurement. American Journal of Obstetrics and Gynecology,211, 675.e1–675.e19.
Bartsch, E., Park, A. L., Jairam, J., & Ray, J. G. (2017). Concomitant preterm birth and severe small-for-gestational age birth weight among infants of immigrant mothers in Ontario originating from the Philippines and East Asia: A population-based study. British Medical Journal Open,7(7), e015386.
Belihu, F. B., Davey, M. A., & Small, R. (2016). Perinatal health outcomes of East African immigrant populations in Victoria, Australia: A population based study. BMC Pregnancy Childbirth,16, 86.
Blencowe, H., Cousens, S., Oestergaard, M. Z., Chou, D., Moller, A. B., Narwal, R., et al. (2012). National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: A systematic analysis and implications. Lancet,379, 2162–2172.
Elo, I. T., Vang, Z., & Culhane, J. F. (2014). Variation in birth outcomes by mother’s country of birth among non-Hispanic black women in the United States. Maternal and Child Health Journal,18, 2371–2381.
Flores, M. E., Simonsen, M. E., Manuck, T. A., Dyer, J. M., & Turok, D. K. (2012). The “Latina Epidemiologic Paradox”: Contrasting patterns of adverse birth outcomes in US-born and foreign-born Latinas. Womens Health Issues,22, e501–e507.
Guendelman, S., Thornton, D., Perez-Cuevas, R., & Walsh, J. (2015). Preterm delivery among first-time Mexico-born mothers: A binational population-based comparison of deliveries in California and Mexico. Journal of Epidemiology and Community Health,69, 35–40.
Hedderson, M., Ehrlich, S., Sridhar, S., Darbinian, J., Moore, S., & Ferrara, A. (2012). Racial/ethnic disparities in the prevalence of gestational diabetes mellitus by BMI. Diabetes Care,35, 1492–1498.
Howson, C. P., Kinney, M. V., McDougall, L., & Lawn, J. E. (2013). Born too soon preterm birth action group. Born too soon: Preterm birth matters. Reproductive Health,10(Suppl 1), S1.
Miller, L. S., Robinson, J. A., & Cibula, D. A. (2016). Healthy immigrant effect: Preterm births among immigrants and refugees in Syracuse, NY. Maternal and Child Health Journal,20, 484–493.
Morrisey, K. (2017). San Diego still top county for refugee arrivals despite reductions. The San Diego Union Tribune. Oct 6, 2017.
Oliver, E. A., Klebanoff, M., Yossef-Salameh, L., Oza-Frank, R., Moosavinasab, S., Reagan, P., et al. (2018). Preterm birth and gestational length in four race-nativity groups, including Somali Americans. Obstetrics and Gynecology,131(2), 281–289.
Martin, J. A., Hamilton, B. E., Osterman, M. J. K., et al. (2017). Births: Final data for 2015. National vital statistics report (Vol. 66, No. 1, p. 53). Hyattsville, MD: National Center for Health Statistics. Table 18.
Raju, T. N. K., Buist, A. S., Blaisdell, C. J., Moxey-Mims, M., & Saigal, S. (2017). Adults born preterm: A review of general health and system-specific outcomes. Acta Paediatrica,106(9), 1409–1437.
Refugee Arrivals Data San Diego County Health and Human Services Agency. (2019). Retrieved July 5, 2019, from https://www.sandiegocounty.gov/content/sdc/hhsa/programs/sd/community_action_partnership/OfficeofRefugeeCoord2.html.
Rocha, F. G., Slavin, T. P., Li, D., Tiirikainen, M. I., & Bryant-Greenwood, G. D. (2013). Genetic associations of relaxin: Preterm birth and premature rupture of fetal membranes. American Journal of Obstetrics and Gynecology,209, 258.e1–258.e8.
San Diego County Demographics Profile. County of San Diego, Health & Human Services Agency, Public Health Services, Community Health Statistics Unit. (2013). March, p. 11.
Sanchez-Vaznaugh, E. V., Braveman, P. A., Egerter, S., March, K. S., Heck, K., & Curtis, M. (2016). Latina birth outcomes in California: Not so paradoxical. Maternal and Child Health Journal,20, 1849–1860.
Singh, G. K., & Yu, S. M. (1996). Adverse pregnancy outcomes: Differences between US- and foreign-born women in major US racial and ethnic groups. American Journal of Public Health,86, 837–843.
Small, R., Gagnon, A., Gissler, M., Zeitlin, J., Bennis, M., Glazier, R., et al. (2008). Somali women and their pregnancy outcomes postmigration: Data from six receiving countries. BJOG: an International Journal of Obstetrics and Gynaecology,115, 1630–1640.
Sørbye, I. K., Daltveit, A. K., Sundby, J., & Vangen, S. (2014). Preterm subtypes by immigrants’ length of residence in Norway: A population-based study. BMC Pregnancy Childbirth,14, 239.
Talge, N. M., Mudd, L. M., Sikorskii, A., & Basso, (2014). United States birth weight reference corrected for implausible gestational age estimates. Pediatrics,133, 844–853.
United States General Services Administration. (2019). San Ysidro Land Port of Entry Project Facts. Retrieved July 6, 2019, from https://www.gsa.gov/about-us/regions/welcome-to-the-pacific-rim-region-9/land-ports-of-entry/san-ysidro-land-port-of-entry.
Vang, Z. M., Elo, I. T., & Nagano, M. (2015). Preterm birth among the Hmong, other Asian subgroups and non-Hispanic whites in California. BMC Pregnancy Childbirth,15, 184.
Funding
Supported by the California Preterm Birth Initiative within the University of California San Francisco, and the San Diego Study of Mothers and Infants (SOMI).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Araneta, M.R.G., Baer, R.J., Muglia, L.J. et al. Health Advantages and Disparities in Preterm Birth Among Immigrants Despite Disparate Sociodemographic, Behavioral, and Maternal Risk Factors in San Diego, California. Matern Child Health J 24, 153–164 (2020). https://doi.org/10.1007/s10995-019-02836-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-019-02836-y