Abstract
To compare pregnancy outcomes of immigrants from Former-Soviet-Union (FSUI) and Ethiopia (EI) to those of Jewish-native-born Israelis (JNB), in context of universal health insurance. Birth outcomes of all singletons born in Soroka-University Medical-Center (1998–2011) of EI (n = 1,667) and FSUI (n = 12,920) were compared with those of JNB (n = 63,405). Low birthweight rate was significantly higher among EI (11.0 %) and slightly lower (7.0 %) among FSUI, compared to JNB (7.5 %). Preterm-delivery rates were similar to those of JNB. Both immigrant groups had significantly (p < 0.001) higher rates of perinatal mortality (PM) than JNB (21/1000 in EI, and 11/1000 in FSUI, compared to 9/1000). Using multivariable GEE models both immigrant groups had significantly increased risk for PM; however, EI had twice as much FSUI origin (OR 2.3, 95 % CI 1.6–3.4, and OR 1.3, 95 % CI 1.1–1.6, respectively). Universal health care insurance does not eliminate excess PM in immigrants, nor the gaps between immigrant groups.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Migratory processes create social conditions and medical challenges which may adversely affect the health of immigrant women and their children. Perinatal outcomes have been extensively studied among migrant in different countries, reporting mixed results among different migrant populations [1–3]. In some studies in European countries, perinatal outcomes were worse among immigrants compared to non-immigrants [4–8]. In contrast, other studies found that despite their disadvantaged socioeconomic status, immigrants had better perinatal outcomes. Compared with US-born women, immigrants had higher mean birthweight, lower risk of PTD, PM and hypertension [9, 10]. Similar results were reported in France and Belgium [2, 11, 12]. Other studies in Australia, Europe and Canada also found less preterm delivery (PTD) and low birth weight (LBW), but an excess of stillbirths [13]. The conflicting results suggest that immigrant status per se might not be a risk factor for adverse perinatal outcomes [14, 15]. A recent meta-analysis [2], stressed the importance of the country of origin, circumstances of migration, characteristics of the health care system in the receiving country, and time since immigration, as well as the socioeconomic status of immigrants [7, 16]. Lack of access to prenatal care for immigrants has been suggested as one of the explanations for gaps in birth outcomes between immigrants and natives [17]. Various studies have shown that over the years there is a trend of improvement in birth outcomes of immigrant women [18–20]. However, a recent study conducted in Israel has pointed out the increased perinatal risks of two generations of immigrants from Ethiopia to Israel, with no improvement over time [21]. Jewish immigration to Israel is viewed as a return to the homeland, and upon their arrival to Israel Jewish immigrants are entitled to a broad range of services from the government including full coverage under the national health insurance and free access to perinatal care [22].
The present study tests two hypotheses: A. Immigrants from Ethiopia (EI) and from the Former Soviet Union (FSUI) have worse pregnancy outcomes than those of Jewish native Israeli-born (JNB) B. Gaps between JNB women and immigrants are associated with the country of origin, as found by Gagnon et al. [2]. Namely, the gap between JNB and immigrants from Ethiopia, a country with high incidence of adverse birth outcomes, will be larger than that between JNB and immigrants from FSU, where the rate of adverse birth outcomes was only slightly higher than that of Israel. Using WHO 2012 data [23] neonatal mortality in Ethiopia was 28/1000, and in the FSU states it ranged from 2.0/1100 (Belarus) to 5.0/1000 in the Ukraine, while in the Jewish population in Israel the rate was 2.0/1000.
More than 75,000 Jewish Ethiopians have migrated to Israel between the mid-1980s and 1991 and about 3,000 per year immigrated to Israel in the 90s [24]. The immigration from Ethiopia is characterized by extreme changes in all areas of life: economy, education, culture, medicine, tradition and more. EI in Israel are generally of low socioeconomic position in terms of income and education [25].
Beginning in the 1990s, 150,000 Jews migrated from the FSU. Following the collapse of the Soviet regime in 1990, about one million people came to Israel in the next decade, most of them (74 %) from Russia and Ukraine. They differed from other groups of immigrants in their high level of education and in their participation in the labor market in their country of origin [25]. According to the Israeli Central Bureau of Statistics in 2012 there were in Israel 75,600 immigrants who were born in Ethiopia and 1.15 million who originated in the FSU [26].
Objectives
To compare birth outcomes of EI and FSUI with JNB living in the same geographical region and served by the same health care services, in the context of the availability of free access to perinatal and obstetric health care.
Methods
Setting
A population-based retrospective cohort study was conducted in Soroka University medical Center (SUMC), the regional hospital of southern Israel, where almost all births in the area occur (during the study period there were about 13,000 births in SUMC per year). SUMC serves all Beer-Sheva district, where 17 % of EIs and 20.7 % of FSUI in Israel live [27].
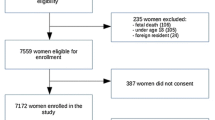
Study Population
The sample size included 111,807 deliveries of Jewish women during the years 1988–2011. The study population included only women with complete obstetric history, i.e. their first birth was in SUMC (77,992 deliveries). Of those, there were 1,667 deliveries of EI (730 mothers), 12,920 deliveries of FSUI (7406 mothers) and 63,405 deliveries of JNB (26,290 mothers). Births of non-Jewish women, and women not born in Israel, Ethiopia or FSU and multiple gestations were excluded.
Data
Data were collected from the computerized perinatal database of information recorded immediately after delivery by an obstetrician, and checked by trained data clerks.
Variables
Risk factors:
-
1.
Maternal characteristics: age, parity, history of obstetric failure (any of the following: three or more spontaneous first trimester abortions; spontaneous mid trimester abortions; preterm deliveries; stillbirths; low birth weight infants; and neonatal deaths).
-
2.
Pregnancy and labor complications: Mild/severe pre-eclampsia (systolic blood pressure of >140 mmHg or a diastolic blood pressure of >90 mmHg and systolic blood pressure >160 mmHg or a diastolic blood pressure of >110 mmHg, respectively, in two occasions at least 6 h apart after 20 weeks gestation), pregestational diabetes mellitus, anemia, out of hospital birth, lack of prenatal care (LOPC), polyhydramnios, oligohydramnios, HIV, meconium stained amniotic fluid, cephalopelvic disproportion, and caesarian section.
Birth outcomes:
Very low birthweight (VLBW <1500 g, low birth weight (LBW)- < 2500 g, small for gestational age (SGA)-weight below the 10th percentile for the gestational age according to local charts, large for gestational age (LGA)-weight above the 90th percentile for the gestational age according to local charts), preterm delivery (PTD-less than 37 weeks gestation, post term delivery-more than 42 weeks gestation, intrauterine fetal death (IUFD), intrapartum death (IPD), postpartum death (PPD) and total perinatal mortality (PM).
Data Analysis
Risk factors and incidence of adverse birth outcomes of EI FSUI were compared to JNB at the univariate level, using t test, Chi-square test or Fisher’s exact test, as appropriate. Odds ratios (OR) and their 95 % confidence interval were computed. p < 0.05 was considered statistically significant. Following the univariate analysis, multivariate models were assessed. The models included all risk factors found to be significantly associated with both ethnicity and the outcome variables in the univariate analysis. GEE analyses were used to control for multiple births of the same mother. Statistical analysis was performed with SPSS package version 17 (SPSS, Chicago, IL, USA).
Results
Table 1 compares demographic and obstetric characteristics of the two immigrant groups (EI and FSUI) to that of the JNB group. Both groups of immigrants were younger than the JNB. The FSU group was of lower parity than both the EI group and the JNB. History of obstetric failure was more prevalent among EI than among FSUI and JNB. EI but not FSUI were more likely than JNB women to have not used prenatal care. HIV was rare in all study groups and seen mostly among EI (1.1 %).
Compared to JNB, EI experienced significantly higher rates of severe preeclampsia, oligohydramnios, cephalopelvic disproportion, caesarean sections and meconium stained amniotic fluids and were more likely to give birth out of the hospital.
Comparison of the FSUI with JNB shows a higher prevalence of mild/moderate pre-eclampsia, severe pre-eclampsia, diabetes and anemia, while rate of polyhydramnios was significantly lower. At birth, more FSUI experienced caesarean section.
Comparison of birth outcomes between each group of immigrants and JNB is presented in Table 2.
EI compared to JNB, had significantly higher rates of VLBW, LBW, SGA, IUFD, IPD and PPD resulting in an overall 2.5 times risk of total PM. FSUI had a higher risk for VLBW and LGA but significantly lower risks for LBW and SGA. The risk for overall PM was slightly higher, mainly reflecting higher rates of fetal deaths.
Table 3 presents the results of the multivariable analyses of adverse birth outcomes in the two immigrants groups. As more than 50 % of women in our study had more than one birth during the study period, we used GEE to adjust for correlated data. The models included all variables which were significantly associated with ethnic origin in the univariate analysis. The models for the EI group included maternal age, prim parity, history of obstetric failure, severe preeclampsia and LOPC. The models of FSUI included maternal age, prim parity, severe preeclampsia and diabetes.
EIs, compared to JNB, were at a significantly higher adjusted risk for all adverse birth outcomes. FSUIs adjusted risk for adverse birth outcomes was much more similar to JNB. FSUI had higher adjusted risk for LGA, but significantly lower adjusted risk for LBW and SGA. While there was no higher risk among FSUI for neonatal postpartum death, the adjusted risk of fetal death was significantly higher.
Discussion
According to the UN report of 2013, about half of the migrants to developed countries were women at the peak of reproductive age (20–34) [28]. Birth outcomes are therefore often used as markers to assess the health status of migrants in comparison to native-born [2]. Birth outcomes of migrants in the receiving country reflect their genetics, environmental exposures and medical treatment in their home country, and their living conditions, socioeconomic position, as well as accessibility, quality and utilization of health services in the receiving country [29].
Our study took place in Israel where all citizens are covered by universal health care insurance, thus all women in our study population had access to health services, prenatal care and maternity services. Our study population included only women who had started their child-bearing in Israel and had used the same birth hospital. Women who were multipara at their first birth in soroka were not included in the analysis as their obstetric history was not complete. They all live in the same geographical area with no cost access to prenatal care services. However, other barriers to access to health services, caused by a complex of societal, cultural and structural factors, may exist [30].
Our main hypothesis regarding immigrants status was based on findings of studies conducted in the US and in Europe, most of which have shown that the incidence of adverse birth outcomes among immigrants from less developed countries was often worse than that of the receiving country, but better than in their country of origin [18]. This observation has some exceptions [11], explained by the “healthy migrant hypothesis” [31, 32], a concept that was challenged by recent studies [16, 33].
Our findings support our hypotheses; the two groups of immigrants had higher PM than JNB women, but the largest gap was, as expected, between JNB and the immigrants from Ethiopia. Our results confirm other studies [34] which found greater risk among EI of preterm, SGA, and stillbirths [21]. In our study the two immigrant groups had higher rates of pregnancy complications, such as severe preeclampsia, than JNB, but while FSUI had significantly higher rates of both mild and severe preeclampsia, EI had only significantly higher rates of severe, but not mild or moderate preeclampsia. This might suggest a lower rate of early detection of preeclampsia among immigrants from Ethiopia. Higher rates of diabetes were found in the FSUI group, but not in the EI group, suggesting either lower prevalence of diabetes among the immigrants from Ethiopia or lower detection rates. However, other studies have shown a high prevalence of diabetes in the Ethiopian population, increasing with longer duration of stay in the country [35, 36], supporting the hypothesis of lower rates of detection, due to suboptimal use of prenatal care services. The excess rates of caesarian section (CS) may also reflect low utilization of prenatal care. A recent meta-analysis [37] which examined the international excess of CS among immigrants in Western countries, found that immigrants from Eastern Europe had reduced rates of CS while immigrants from Africa had higher rates, particularly emergency CS. This was attributed to cultural-behavioral factors, preexisting maternal medical conditions and gestational risk factors. In our study, both immigrant groups had higher rates of CS, compared to JNB but the gap between EI and native born was much greater than between FSUI and native born.
These patterns of differences are consistent with the findings that EI were less likely to use prenatal care, as well to give birth out of hospital, compared to both FSUI and JNB. Not using prenatal care at all or suboptimal use of available and free services by immigrants from Asia and Africa has been documented in other European countries [38, 39] and in the US [40]. Suboptimal use of prenatal services may delay the timely detection of modifiable risk factors such as hypertension, diabetes, threatening preterm labor, all of which, if timely detected and treated, may improve birth outcomes. Essen et al [41] noted that hospitalization in neonatal intensive care units of newborns of African immigrants was significantly lower than that of non-immigrants, and suggested that it may be indicative of poorer prenatal care leading, to higher PM observed among immigrants from Africa to Sweden.
Use of prenatal health services is affected not only by availability and geographical and financial accessibility but also by cultural and lingual accessibility, as exemplified by the significantly higher rates of out of hospital delivery among EIs compared with the two other groups. Most of the study population lives in close geographical proximity to the hospital and as there were no geographical or financial barriers to hospital delivery, out of hospital birth may reflect a cultural choice, indicating that health care services in Israel were more culturally accessible to the FSUI than to EI. One very likely reason for this was that many health care providers in those years were themselves immigrants from the FSU, but only few were of Ethiopian origin [42]. It is reasonable to assume that the presence of Russian speaking physicians and nurses in hospitals and community clinics made these services more culturally accessible to FSUI than to immigrants from Ethiopia. Immigrant-related factors such as language have been shown to influence access to health services [43–45].
A recent analysis of the perinatal health of migrants in Europe by Bollini et al. [4]. Suggests that differences in prenatal health of migrants is associated not only with the country of origin but also, and mainly with the integration policies of the receiving countries, which according to Koopmans et al. [46]. (2005) include equal opportunities (in school, in the labour market), and actions to combat socioeconomic disadvantage, to protect of immigrant culture, religion and identity, and to promote antidiscrimination legislation. While the official Israeli absorption policy of Jewish immigrants does not differ according to the country of origin, in fact the absorption of the EIs has been less successful than that of the immigrants from the FSU. About 40 % of the EIs of working age in 2005 had an elementary school education or less, and many had no required vocational skills, resulting in high rates of unemployment or low paying, unskilled jobs. Large families, high dependency ratio, and low income, are reflected in a high proportion of poverty (52 %) and lower than average standard of living of EI compared to Jewish population as a whole [25]. Immigrants from the FSU were of higher educational level and many had professional skills, enabling them to achieve better paying jobs, and, as mentioned before, they had a noticeable impact on the health care system [47]. Our findings are consistent with a previous study published in 2007 in Israel [48] which has shown that the general population received more preventive recommendations and treatment than did Ethiopian women. The authors suggested lack of communication between the service providers and the recipient as the main reason.
Lu and Halfon [49] suggested that adverse birth outcomes are not determined only by prenatal exposures, but by life experience of risk factors associated with low socioeconomic position, stress and sense of discrimination. The life-course approach is particularly relevant to migrants’ life experience and provides a theoretical support to our empirical evidence of disparity between native born and migrants from two different backgrounds. While Israeli policy toward Jewish immigrants is no doubt integrative, the daily life experience of different groups of immigrants, as well as their experience of interaction with the health care system may not be the same for a variety of reasons (language, skin color, cultural affinity, literacy, etc.). While both immigrant groups have experienced stress associated with migration and adjusting to a new culture, the process of absorption of the EI has been less successful than that of the FSU immigrants, partially explaining the disparity in birth outcomes of the two groups of immigrants [50, 51].
Our study has several strengths: it is a population based study, in a context of full coverage of perinatal services, eliminating financial barriers to care or differential quality of services, as explanatory factors of disparity in outcomes. The information is based on a computerized data base which enabled us to examine and control for important clinical characteristics. However, it has several limitations: we were not able to control for important variables such as: time since migration, education, utilization pattern of MCHCs, smoking, drinking and nutrition, which were not documented in the database. It should be noted that the effect of time since migration was examined in the recent work of Calderon-Margalit et al. [21] on birth outcomes of immigrants from Ethiopia which found no improvement with duration of stay.
In conclusion, universal health care insurance and free access to perinatal services are not enough to eliminate gaps in birth outcomes between immigrants and native-born, nor do they eliminate differences between immigrants from the FSU and Ethiopia.
References
Gissler M, et al. Stillbirths and infant deaths among migrants in industrialized countries. Acta Obstet Gynecol Scand. 2009;88:134–48.
Gagnon AJ, Zimbeck M, Zeitlin J. Migration to western industrialised countries and perinatal health: a systematic review. Soc Sci Med. 2009;69:934–46.
Sosta E, et al. Preterm delivery risk in migrants in Italy: an observational prospective study. J Travel Med. 2008;15:243–7.
Bollini P, Pampallona S, Wanner P, Kupelnick B. Pregnancy outcome of migrant women and integration policy: a systematic review of the international literature. Soc Sci Med. 2009;68:452–61.
Malin M, Gissler M. Maternal care and birth outcomes among ethnic minority women in Finland. BMC Public Health. 2009;9:84.
Zanconato G, Iacovella C, Parazzini F, Bergamini V, Franchi M. Pregnancy outcome of migrant women delivering in a public institution in Northern Italy. Gynecol Obstet Investig. 2011;72:157–62.
Zeitlin J, Combier E, de Caunes F, Papiernik E. Socio-demographic risk factors for perinatal mortality. A study of perinatal mortality in the French district of Seine-Saint-Denis. Acta Obstet. 1998;77:826–35.
Juárez SP, Ortiz-Barreda G, Agudelo-Suárez AA, Ronda-Pérez E. Revisiting the healthy migrant paradox in perinatal health outcomes through a scoping review in a recent host country. J Immigr Minor Health. 2015. doi:10.1007/s10903-015-0317-7.
Forna F, Jamieson DJ, Sanders D, Lindsay MK. Pregnancy outcomes in foreign-born and US-born women. Int J Gynecol Obstet. 2003;83:257–65.
Alexander GR, et al. US birth weight/gestational age-specific neonatal mortality: 1995–1997 rates for whites, hispanics, and blacks. Pediatrics. 2003;111:e61–6.
Guendelman S, et al. Birth outcomes of immigrant women in the United States, France, and Belgium. Matern Child Health J. 1999;3:177–87.
Cervantes A, Keith L, Wyshak G. Adverse birth outcomes among native-born and immigrant women: replicating national evidence regarding Mexicans at the local level. Matern Child Health J. 1999;3:99–109.
Small R, et al. Somali women and their pregnancy outcomes postmigration: data from six receiving countries. BJOG An Int J Obstet Gynaecol. 2008;115:1630–40.
Urquia ML, Frank JW, Moineddin R, Glazier RH. Immigrants’ duration of residence and adverse birth outcomes: a population-based study. BJOG. 2010;117:591–601.
Gould JB, Madan A, Qin C, Chavez G. Perinatal outcomes in two dissimilar immigrant populations in the United States: a dual epidemiologic paradox. Pediatrics. 2003;111:e676–82.
Puthussery S. Perinatal outcomes among migrant mothers in the United Kingdom: is it a matter of biology, behaviour, policy, social determinants or access to health care? Best Pract Res Clin Obstet Gynaecol. 2015. doi:10.1016/j.bpobgyn.2015.09.003.
Pimentel VM, Eckardt MJ. More than interpreters needed: the specialized care of the immigrant pregnant patient. Obstet Gynecol Surv. 2014;69:490–500.
Cacciani L, et al. Perinatal outcomes among immigrant mothers over two periods in a region of central Italy. BMC Public Health. 2011;11:294.
Spallek J, Lehnhardt J, Reeske A, Razum O, David M. Perinatal outcomes of immigrant women of Turkish, Middle Eastern and North African origin in Berlin, Germany: a comparison of two time periods. Arch Gynecol Obstet. 2014;289:505–12.
Ceballos M. Simulating the effects of acculturation and return migration on the maternal and infant health of Mexican immigrants in the United States: a research note. Demography. 2011;48:425–36.
Calderon-Margalit R, Sherman D, Manor O, Kurzweil Y. Adverse perinatal outcomes among immigrant women from Ethiopia in Israel. Birth. 2015;42:125–31.
Zilber N, Lerner Y. Psychological distress among recent immigrants from the former Soviet Union to Israel, I. correlates of level of distress. Psychol Med. 1996;26:493–501.
Mortality rate, neonatal (per 1,000 live births)|Data|Table. http://data.worldbank.org/indicator/SH.DYN.NMRT.
The Immigration of Ethiopian Jews to Israel. ministry of immigrant http://www.moia.gov.il/Hebrew/FeelingIsrael/AboutIsrael/Pages/mivtzaShlomo.aspx.
Bank of Israel–Press Releases–The Bank of Israel publishes an excerpt from its 2006 Annual Report, due to be published 11 April 2007 http://www.boi.org.il/en/NewsAndPublications/PressReleases/Pages/070404e.aspx.
Central Bureau of Statisyics. Period of Immigration, country of birth, last country of Residence. Israel Statistical Yearbook (2014). http://www.cbs.gov.il/shnaton66/st04_04.pdf.
Immigrants (1), by first district of residence in Israel under the last country selected of residence. (2014). doi:CBS, Statistical abstract of Israel 2014, Table 4.9.
United Nations(a). International Migration Policies. Population Division (2013). doi:10.4135/9781412952446.n605.
Naimy Z, Grytten J, Monkerud L, Eskild A. Perinatal mortality in non-western migrants in Norway as compared to their countries of birth and to Norwegian women. BMC Public Health. 2013;13:37.
Jacobs B, Ir P, Bigdeli M, Annear PL, Van Damme W. Addressing access barriers to health services: an analytical framework for selecting appropriate interventions in low-income Asian countries. Health Policy Plan. 2012;27:288–300.
Lu Y. Test of the ‘healthy migrant hypothesis’: a longitudinal analysis of health selectivity of internal migration in Indonesia. Soc Sci Med. 2008;67:1331–9.
McGlade MS, Saha S, Dahlstrom ME. The latina paradox: an opportunity for restructuring prenatal care delivery. Am J Public Health. 2004;94:2062–5.
Juárez SP, Revuelta-Eugercios BA. Too heavy, too late: investigating perinatal health outcomes in immigrants residing in Spain. a cross-sectional study (2009–2011). J Epidemiol Community Health. 2014;68:863–8.
Press F, Katz M, Leiberman JR, Shoham I, Glezerman M. Obstetric performance in Ethiopian immigrants compared with Israeli parturients. Isr J Med Sci. 1993;29:403–7.
Rubinstein A, Graf E, Villa Y. Prevalence of diabetes mellitus in Ethiopian immigrants: comparison of Moses and Solomon immigrations. Isr J Med Sci. 1993;29:344–6.
Zung A, et al. Type 1 diabetes in Jewish Ethiopian immigrants in Israel: HLA class II immunogenetics and contribution of new environment. Hum Immunol. 2004;65:1463–8.
Merry L, Small R, Blondel B, Gagnon AJ. International migration and caesarean birth: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2013;13:27.
Alderliesten ME, Vrijkotte TGM, Van Der Wal MF, Bonsel GJ. Late start of antenatal care among ethnic minorities in a large cohort of pregnant women. BJOG An Int J Obstet Gynaecol. 2007;114:1232–9.
Essén B, et al. Are some perinatal deaths in immigrant groups linked to suboptimal perinatal care services? BJOG An Int J Obstet Gynaecol. 2002;109:677–82.
Fuentes-Afflick E, Hessol NA. Immigration status and use of health services among Latina women in the San Francisco Bay Area. J. Womens. Health (Larchmt). 2009;18:1275–80.
Essén B, et al. Increased perinatal mortality among sub-Saharan immigrants in a city-population in Sweden. Acta Obstet Gynecol Scand. 2000;79:737–43.
Remennick LI, Shtarkshall RA. Technology versus responsibility: immigrant physicians from the former Soviet Union reflect on Israeli health care. J Health Soc Behav. 1997;38:191–202.
Bischoff A, Perneger TV, Bovier PA, Loutan L, Stalder H. Improving communication between physicians and patients who speak a foreign language. Br J Gen Pract. 2003;53:541–6.
Andrulis D, Goodman N, Pryor C. What a difference an interpreter can make: health Care experiences of uninsured with limited english proficiency. 9 Sep 2011 (2002).
Bowen JM. Bridging the multicultural gap. Minn Med. 2000;83:10–3.
Koopmans R, Statham P, Giugni M, Passy F. Contested Citizenship—University of Minnesota Press. (2005) http://www.upress.umn.edu/book-division/books/contested-citizenship.
The main effects of FSU immigrants from 1990 onward on Israeli economy. https://www.knesset.gov.il/mmm/data/pdf/m03149.pdf, accessed Dec 5 2014.
Tandeter H, Masandilov I, Kemerly I, Biderman A. Ethnic differences in preventive medicine: the example of Jewish Ethiopian women in Israel. Isr Med Assoc J. 2007;9:452–6.
Lu MC, Halfon N. Racial and ethnic disparities in birth outcomes: a life-course perspective. Matern Child Health J. 2003;7:13–30.
Fenster T. Ethnicity, citizenship, planning and gender: the case of Ethiopian immigrant women in Israel. Gend, Place Cult. 1998;5:177–89.
Kahan-Strawczynski P, Amiel S, Levi D, VK. First and second generations of immigrant youth from Ethiopia and the Former Soviet Union–similarities and differences. (2012). http://brookdale.jdc.org.il/?CategoryID=192&ArticleID=288.
Acknowledgments
This study was not funded by any factor and was part of the academic studies of the first author.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants performed by any of the authors. The Institutional Review Board of SUMC (in accordance with the Declaration of Helsinki) approved the study.
Rights and permissions
About this article
Cite this article
Lubotzky-Gete, S., Shoham-Vardi, I. & Sheiner, E. Comparing Pregnancy Outcomes of Immigrants from Ethiopia and the Former Soviet Union to Israel, to those of Native-Born Israelis. J Immigrant Minority Health 19, 1296–1303 (2017). https://doi.org/10.1007/s10903-016-0484-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-016-0484-1