Abstract
To compare infant injuries in the first year of life between Maternal Infant Health Program (MIHP) participants and matched comparison groups. The population was the cohort of Medicaid-insured singleton infants born in 2011 in Michigan who had continuous Medicaid insurance and survived the first year after birth (N = 51,078). Propensity score matching was used to compare participants in MIHP to matched comparison groups from among the nonparticipants. Injury episodes were defined based on Medicaid claims in the first year of life. Matched comparisons were performed using McNemar, Bowker, and Wilcoxon signed rank tests to assess the effects of program participation on infant injuries. Infants of MIHP participants were more likely to have injury episodes (11.7 vs. 10.4 %, p < 0.01) and a higher rate of episodes (126.9/1,000 infants vs. 109.6/1,000) compared to matched nonparticipants. Infants of MIHP participants were more likely to have superficial injuries (4.9 vs. 3.9 %, p < 0.01) and a higher rate of episodes related to superficial injuries (49.7/1,000 vs. 39.6/1,000), which mainly accounted for the difference in injury visits between groups. Similar results were found among those enrolled and risk-screened in the program by the 2nd pregnancy trimester and who received a dosage of at least three additional MIHP contacts when compared to matched nonparticipants. MIHP participants did not experience reductions in infant injuries in the first year of life compared to matched nonparticipants. Possible explanations may include increased health-seeking behavior of the mothers participating in MIHP or improved recognition of infant injuries that warrant medical attention.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prenatal and early infancy home visiting programs provide a broad set of services to address issues such as access to services, maternal and child health, safe home environments, parenting, and child development [1]. In general, these programs support underserved, low-income populations, and other at-risk groups [2, 3]. The federal 2010 Patient Protection Affordable Care Act supports the expansion of evidence-based home visitation programs [4, 5] and reaffirmed the need for evidence of the effectiveness of home-visitation programs [6].
While there is consistent evidence that home visiting improves child health, maternal health, parenting practices, and child development, the evidence on the effects of home visiting programs on the incidence of infant injuries is mixed [6]. Some prior randomized controlled trials (RCT) found that nurse home visiting reduced the infant injury-related encounters during the first 2 years of life [7, 8]. Another RCT found that a home visiting enhanced intervention did not reduce the risk of infant injury during the first 3 years of life [9, 10]. A recent quasi-experimental evaluation revealed that children participating in a statewide initiative providing nurse home visitation to high-risk first time mothers were more likely to have injury visits during the first 2 years of life compared to a propensity score matched group of non-participants [11].The study found that significantly higher rates of superficial injuries mainly accounted for the difference in injury visits between the two groups.
The Maternal and Infant Health Program (MIHP) is a population-based enhanced prenatal and postnatal care (EPC) program that includes home-visitation available to all Medicaid-eligible pregnant women and infants aged ≤1 year in Michigan. MIHP is the largest EPC program in Michigan, with participants and providers in all counties. While overall approximately a third of all Medicaid-eligible pregnant women in Michigan enroll in the MIHP program during pregnancy, there is geographic diversity in participation across the state. The MIHP enrollment rate varies along the entire range across counties, with two-thirds of the 83 Michigan counties experiencing rates between 20 and 63 % in 2011 (authors calculations). Medicaid-insured pregnant women may enroll in the program at any time during their pregnancy. While some women self-refer, most women are referred to the MIHP program either through physician offices, the Special Supplemental Nutrition Program for Women, Infants and Children (WIC), Medicaid health plans, or other social service community programs. MIHP supplements medical prenatal, postnatal, and infant care through home-based care coordination, referrals, and risk-specific interventions with the aims of promoting healthy pregnancies, positive birth outcomes, and healthy infants. The MIHP program includes specific components focusing on infant safety, including safe sleep, not shaking the baby, child proofing the home, and other infant safety education. Approximately 45 % of the infants born in Michigan and 40 % of all US infants are Medicaid-insured at birth [12, 13]. Medicaid-insured women and their infants are at higher risk, including having a higher likelihood of unintended pregnancies, initiating prenatal care later than the first trimester, smoking during pregnancy, adverse birth outcomes, infant mortality, and infant injury compared to women with private insurance [14–17].
Prior evaluations of the MIHP using propensity score matching found that the program was effective in improving healthcare utilization for mothers and infants and in reducing the risk of adverse birth outcomes [18, 19]. This study builds upon our previous work, with the goal of assessing program effectiveness in reducing infant injuries in the first year of life.
Methods
Study Design
This study used a quasi-experimental cohort design to assess the effects of participation in MIHP on infant injuries. The study compared the outcomes of MIHP participants with a matched group selected from among the Medicaid beneficiaries who did not participate in MIHP. The study received IRB exempt status from the Michigan State University IRB because it was considered research not involving human subjects due to the use of retrospective de-identified data.
Study Population and Data Sources
The study population was represented by the cohort of Medicaid-insured singleton-born infants born between January 1, 2011 and December 31, 2011 in Michigan who survived the first year after birth and had continuous Medicaid insurance during the first year of life (N = 51,078). Infants and mothers were linked based on unique Michigan Department of Community Health (MDCH) master record numbers (linking rate >95 %), with all data available through the data warehouse from MDCH. Continuous Medicaid was defined based on monthly infant Medicaid eligibility in each month of the first year of life. Data for this cohort of infants consisted of all birth and death records, Medicaid maternal and infant medical claims during pregnancy and during the first year after birth, and monthly Medicaid eligibility from 3 months prior to conception until 1 year after birth. Data also included other program participation (such as cash assistance). Over 99 % of the infants in the study population were linked to Medicaid claims in the first year of life (Tables 1, 2).
Measures
Outcomes
We identified injury episodes based on the primary diagnoses recorded on the Medicaid claims (the ICD-9 codes are presented in Tables 3, 4). Following Spady and Saunders [20] and Lestina, Miller, and Smith [21], to avoid over-counting injury events due to follow-up visits, we defined an injury episode as follows: (1) within 180 days, different injury diagnoses (of primary diagnosis) that fall into the same category of injury were counted as one episode, assuming that the same category of injury does not occur more than one time within 180 days; or (2) within 7 days, primary diagnoses that fell into different injury categories. We then categorized the injury episodes into 17 categories, following Spady and Saunders [21] (Tables 3, 4).
MIHP Participation
A first MIHP participation indicator was coded “yes” if at least one maternal claim with MIHP CPT or HCPCS codes submitted by an MIHP provider was present during pregnancy, otherwise it was coded “no” [22]. Previous studies showed dosage effects of home visiting programs improving birth outcomes [18, 23]. To capture the effects of MIHP enrollment timing and dosage, a second MIHP participation indicator was coded one if women enrolled in MIHP and were screened in the 1st or 2nd trimester and had at least three additional MIHP contacts at any time during pregnancy and 0 if not participating in MIHP. Prior work revealed that pregnancies of those enrolled in MIHP in the 3rd trimester were more likely to be carried full-term, potentially biasing our analyses, and offering another reason to exclude those with 3rd trimester MIHP enrollment from the 2nd MIHP definition [18].
Program eligibility is based on prenatal Medicaid coverage, as all pregnant women with Medicaid coverage qualify for services, and MIHP and Medicaid eligibility continue through pregnancy and 60 days after birth for all mothers. Medicaid-insured infants are eligible for MIHP for the entire first year of life. We chose to define MIHP based on prenatal participation only, and excluded from among participants those who enrolled in MIHP after birth, so that MIHP pre-dates the infant injury analyzed outcomes, and therefore avoiding the potential issue of selection into MIHP related to infant injury. The vast majority of those enrolled in MIHP during pregnancy continue in the program during the infant’s first year of life.
Matching Maternal Baseline Characteristics
Maternal age at birth, marital status, race/ethnicity, county of residence, smoking status during pregnancy, first-time pregnancy, and repeat pregnancy within 18 months were available and used as baseline characteristics potentially associated with MIHP participation. Two SES measures were also included. The first binary indicator identified pregnant women with income at ≤33 % of the federal poverty level (FPL) based on their participation in the Low-Income Family Program and receipt of cash assistance. The second indicator distinguished between: (1) Medicaid-eligible pregnant women who had Medicaid before pregnancy (qualifying income ≤63 % FPL if aged >19 years, the majority in this study; and ≤150 % FPL if aged ≤19 years); and (2) higher-income women who became eligible after confirming the pregnancy, with qualifying income of ≤185 % FPL regardless of age [24]. Three binary indicators for maternal chronic conditions were also included, coded 1 if any relevant claims during pregnancy were identified based on diagnostics and procedure codes, and 0 otherwise. To minimize the likelihood of measuring disease onset after MIHP enrollment during pregnancy, some of the most prevalent conditions were selected: asthma (ICD9; 250), diabetes (ICD9, 401–405), and hypertension (ICD9; 491–493).
Analytic Approach
Comparability between the MIHP participants and all nonparticipants was first assessed using appropriate bivariate statistical tests (Table 1). Then, the expected probability of MIHP participation (the propensity score) was estimated for all participants and non-participants as a function of all the above baseline characteristics using logistic regression [25, 26]. Next, 1:1 random-sort nearest-neighbor matching without replacement was used within race (Black and others), within a ±0.05 SD caliper, where SD was the standard deviation of the linear predictor (the logit-transformed propensity score), to select comparison groups. Further, matched comparisons were performed to assess MIHP effects on infant injuries and baseline equivalence across all covariates between the MIHP participants and the matched comparison groups according to both MIHP indicators (Table 2). Paired comparisons were performed using McNemars test, Bowker’s test, and t test, as appropriate.
To test whether MIHP has favorable effects in reducing injury visits in specific injury categories, paired comparisons were made between the MIHP participants and the matched comparison groups, within each injury category, using Wilcoxon signed rank tests and McNemar tests (Tables 3, 4). Injury episodes counts and rates per 1,000 infants, as well as counts and rates of infants with injuries were compared. All analyses were performed by using the SAS version 9.3, Cary, NC: SAS Institute Inc.
Results
Significant differences were observed between MIHP participants and non-participants along all the baseline characteristics, according to both MIHP participation indicators. More mothers in MIHP identified as Black (38 vs. 21 %); were first time mothers (37 vs. 31 %); had a family income <33 % FPL (29 vs. 16 %); and were more likely to have chronic disease (Table 1).
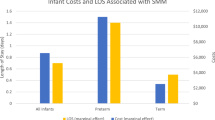
Table 2 shows that after selecting a matched comparison group using the propensity score method, we established baseline equivalence on all the characteristics included in our analyses using both MIHP participation indicators (except on the individual county of residence, unreported results). Table 2 also shows that infants whose mothers participated in MIHP were more likely to have injury episodes compared to a matched group of non-participants, both among those with any MIHP participation (11.7 vs. 10.4 %, p < 0.01) and among those who enrolled and risk-screened in the program by the 2nd trimester and who received at least three additional MIHP contacts (12.1 vs. 10.6 %, p < 0.01).
When defining MIHP participation as “any MIHP contact during pregnancy” (Table 3), there were more superficial injury episodes among the infants in MIHP (679 episodes, 49.7/1,000 infants, p < 0.01) versus the matched non-participant infants (538 episodes, 39.6/1,000, p < 0.01). There were also more open wounds (16.8 vs. 13.3/1,000, p < 0.01), foreign body injuries (13.6 vs. 10.3/1,000, p < 0.01), and intracranial injuries (6.2 vs. 4.4/1,000, p = 0.04).
Infants whose mothers enrolled in MIHP in the first two pregnancy trimesters and had at least three MIHP prenatal contacts in addition to the enrollment risk screening (Table 4) had more superficial injury episodes (484 vs. 360 episodes, 54.3 vs. 40.4/1,000, p < 0.01) compared to infants in the matched non-participant group.
Discussion
The propensity score matched analyses found that MIHP participation did not reduce risk of injury-related visits for infants in their first year of life. The odds of having any injury and the injury episode rates in the first year of life were higher among infants of MIHP participants compared to matched non-participants. The finding was mostly explained by higher rates of superficial injury episodes among children born to MIHP participants.
While some randomized trials showed reductions in encounters for injury in the first 2 years of life for children participating in home visiting programs [7, 8], others, focusing on the first 3 years of life, did not [9, 10]. A recent evaluation of a statewide initiative providing nurse home visitation to high-risk first-time mothers used propensity score matching and found that participating children were more likely to have at least one injury visit, and had more overall injury visits in the first 2 years of life than comparison children [11]. The study concluded that the finding was explained mostly by more superficial injuries among children participating in NFP, and that visit rates for more serious injuries were similar.
While similar in methodology and findings with the study described above [11], our analyses add to the research literature in several ways. Our study population was a statewide birth cohort of Medicaid-insured infants and their mothers, and, unlike other programs, MIHP is available to all Medicaid beneficiaries regardless of age, gravidity, or other characteristics. With population-based program eligibility, the results of the study are more generalizable compared to other programs’ evaluations as the Michigan population is racially heterogeneous, including rural and large metropolitan areas. Another benefit of the population-based eligibility was the significantly larger sample size compared to prior studies. As randomized trials or lotteries are, in general, not feasible with programs with population-based eligibility, the quasi-experimental propensity score matching approach used here relied on the most rigorous available methods to reduce selection bias. Our analyses also accounted for the timing of enrollment in the program and for the dosage of services to test whether the participants who enrolled early during pregnancy and were more engaged experienced different program effects. While comparable to these studies, it is relevant to note that our analyses focused on the infants’ first year of life, when the rates and sources of injuries may be different than in the toddler years.
The early enrollment and a dosage of prenatal MIHP was shown to improve prenatal care and reduced risk of adverse birth outcomes [18, 19], which in turn may have influenced infant injuries. To test whether birth outcomes and their relationship with MIHP influenced our analyses, we replicated the infant injuries paired comparisons in conditional logistic regressions adjusted for indicators of preterm birth and low birth weight, with virtually unchanged results (unreported results available from the authors).
Noting that the approach used in this study made use of the best available methods to account for potential selection bias, several limitations are to be mentioned. The analysis balanced on selection factors expected to influence participation in MIHP, yet, as with other observational studies, our matching was limited to observable characteristics. Other unobserved selection factors may impact our findings. For example, women who enroll in MIHP may have higher psychosocial resources, have greater readiness to engage in services, and have a more active health-seeking behavior, which may explain our findings. Additional unobserved sources of potential bias due to imbalances between those in MIHP and the matched nonparticipants include maternal involvement with child protective services, mother’s status as primary caregiver, and availability of childcare. As a specific example, the higher rates of intracranial injuries in the MIHP group may be due to child protective services becoming more involved with the MIHP families due to the increased surveillance by the home visitors, as these injuries could suggest maltreatment in children of this age. While overall, only 7 % occur in the neonatal period (first 4 weeks), injuries in some categories do occur at significantly higher rates in the neonatal period, and could be due to birth trauma. As an example, over 40 % of the upper limb fractures (by far the largest share within any category, authors’ calculations) occurred in the first 4 weeks of life. These injuries may not have been preventable by MIHP participation. The exclusion of infants who died in the first year of life from our study population reduced the potential of including non-preventable (by MIHP) injuries due to birth defects/injuries. However, a possible limitation is the fact that infants whose death was due to maltreatment may have had injuries that were potentially unobserved. We acknowledge this may be a limitation if the MIHP and matched nonparticipant groups were imbalanced in this regard.
Our prior program of research revealed that MIHP participation increased appropriate use of maternal and infant health care, including receiving appropriate well-child visits through the first year of life. It is plausible that MIHP participation could increase the general health-seeking behavior of mothers, resulting in more encounters with the health system. A potential mechanism may be that MIHP participation improves the ability to navigate the health system. Another possibility is that MIHP participation improves the parental recognition of infant injuries that may need medical attention, as a result of the direct interaction with MIHP home visitors or participation in parenting education group classes. Both increased health-seeking behavior and improved parental recognition of infant injuries needing medical attention could have resulted in increased medical episodes related to infant injuries and are supported by our finding of higher rates of superficial injuries among program participants [17].
To conclude, participants in a state Medicaid-sponsored population-based EPC program did not experience reductions in infant injuries in the first year of life compared to matched nonparticipants. The majority of the infant injuries were superficial and accounted for most of the difference in injury episodes between MIHP participants and the matched controls. Potential mechanisms explaining the increased infant injury among MIHP participants include better recognition of injuries that need medical attention, improved ability to navigate the health system, and increased maternal health-seeking behavior. Further research, including qualitative reviews of the program delivery and fidelity, may confirm these mechanisms of MIHP effect or suggest alternative explanations. Our findings are especially relevant as Medicaid covers a large proportion of pregnancies and births in the US and Medicaid-insured mothers and infants represent a disadvantaged group.
References
Avellar, S., & Paulsell, D. (2011). Lessons learned from the home visiting evidence of effectiveness review office of planning, research and evaluation, administration for children and families. Washington, DC: U.S. Department of Health and Human Services. http://homvee.acf.hhs.gov/Lessons_Learned.pdf.
Agency for healthcare research and quality. (2012). 2011 national healthcare disparities report. www.ahrq.gov/research/findings/nhqrdr/nhdr11/index.html.
Blumenshine, P., Egerter, S., Barclay, C. J., Cubbin, C., & Braveman, P. A. (2010). Socioeconomic disparities in adverse birth outcomes: A systematic review. American Journal of Preventive Medicine, 39(3), 263–272.
Health Care and Education Affordability Reconciliation Act of 2010. http://www.hhs.gov/healthcare/rights/law/reconciliation-law.pdf.
Iglehart, J. K. (2010). Historic passage—reform at last. New England Journal of Medicine, 362(14), e48.
Paulsell, D., Avellar, S., Sama-Miller, E., Del Grosso, P. (2014). Home visiting evidence of effectiveness review: Executive summary. Washington, DC: Office of planning, research and evaluation, administration for children and families, DHHS. http://homvee.acf.hhs.gov/HomVEE_Executive_Summary_2013.pdf. Accessed on August 8, 2014.
Kitzman, H., Olds, D. L., Henderson, C. R, Jr, Hanks, C., Cole, R., Tatelbaum, R., et al. (1997). Effect of prenatal and infancy home visitation by nurses on pregnancy outcomes, childhood injuries, and repeated childbearing. A randomized controlled trial. Journal of the American Medical Association, 278(8), 644–652.
Olds, D. L., Henderson, C. R, Jr, Chamberlin, R., & Tatelbaum, R. (1986). Preventing child abuse and neglect: A randomized trial of nurse home visitation. Pediatrics, 78(1), 65–78.
Campbell, K. I., & Silva, P. A. (1997). Parents as first teachers pilot programme evaluation: Age three assessments. Final report to the ministry of education on the dunedin and Gisborne/East coast areas. Wellington: Ministry of Education.
Wagner, M., Clayton, S., Gerlach-Downie, S., & McElroy, M. (1999). An evaluation of the northern California parents as teachers demonstration. Menlo Park, CA: SRI International.
Matone, M., O’Reilly, A. L., Luan, X., Localio, A. R., & Rubin, D. M. (2012). Emergency department visits and hospitalizations for injuries among infants and children following statewide implementation of a home visitation model. Maternal and Child Health Journal, 16(9), 1754–1761.
The Henry Kaiser J. Family Foundation. (2011). Medicaid matters: Understanding Medicaid’s role in our health care system. www.kff.org/medicaid/upload/8165.pdf.
The Annie E. Casey Foundation. (2013). Data center, kids count, Michigan. http://datacenter.kidscount.org/data/bystate/Rankings.aspx?state=MI&ind=1716.
Michigan Department of Community Health. (2010). PRAMS report 2008, Edited by Christin M. Larder and Violanda Grigorescu. http://www.michigan.gov/documents/mdch/MI_PRAMS_2008_Annual_Repot_9_28_2010_340775_7.pdf.
Blumenshine, P., Egerter, S., Barclay, C. J., Cubbin, C., & Braveman, P. A. (2010). Socioeconomic disparities in adverse birth outcomes: A systematic review. American Journal of Preventive Medicine, 39(3), 263–272.
Brintnell, D., Peterson-Hickey, M., Stroud, D., Castellano, S., Fogarty, C. The birth certificate and medicaid data match project: Initial findings in infant mortality. http://www.health.state.mn.us/divs/fh/mch/mortality/documents/mortalityfindings.pdf. Accessed on May 29, 2014.
Leventhal, J. M., Martin, K. D., & Gaither, J. R. (2012). Using US data to estimate the incidence of serious physical abuse in children. Pediatrics, 129(3), 458–464. doi:10.1542/peds.2011-1277.
Roman, L. A., Raffo, J. E., Zhu, Q., & Meghea, C. I. (2014). A statewide medicaid enhanced prenatal care program: Impact on birth outcomes. JAMA Pediatrics, 168(3), 220–227.
Meghea, C. I., Raffo, J. E., Zhu, Q., & Roman, L. (2013). Medicaid home visitation and maternal and infant healthcare utilization. American Journal of Preventive Medicine, 45(4), 441–447.
Spady, D. W., Saunders, D. L., Schopflocher, D. P., & Svenson, L. W. (2004). Patterns of injury in children: A population-based approach. Pediatrics, 113(3), 522–529.
Lestina, D. C., Miller, T. R., & Smith, G. S. (1998). Creating injury episodes using medical claims data. Journal of Trauma, 45(3), 565–569.
Michigan Department of Community Health. Maternal infant health program (MIHP). http://www.michigan.gov/mdch/0,4612,7-132-2943_4672-106183–,00.html. Accessed on May 9, 2014.
Slaughter, J., Issel, L. M., Handler, A., Rosenberg, D., Kane, D., & Stayner, L. (2013). Measuring dosage: A key factor when assessing the relationship between prenatal case management and birth outcomes. Maternal and Child Health Journal, 17(8), 1414–1423.
The Henry Kaiser J. Family Foundation. Medicaid matters: Understanding Medicaid’s role in our health care system. Kaiser Commission on Key Facts. http://kaiserfamilyfoundation.files.wordpress.com/2013/01/8165.pdf. Accessed May 8, 2014.
Rosenbaum, P. R., & Rubin, D. B. (1983). The central role of the propensity score in observational studies for causal effects. Biometrika, 70(1), 41–55.
Rubin, D. B. (1997). Estimating causal effects from large data sets using propensity scores. Annals of Internal Medicine, 127(Part2), 757–763.
Acknowledgments
This project was supported by a grant from the Michigan Department of Community Health. We thank the Michigan Department of Community Health for facilitating the access to the data.
Conflict of interest
The authors report no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Meghea, C.I., You, Z. & Roman, L.A. A Statewide Medicaid Enhanced Prenatal and Postnatal Care Program and Infant Injuries. Matern Child Health J 19, 2119–2127 (2015). https://doi.org/10.1007/s10995-015-1724-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-015-1724-z