Abstract
Aprocitentan is a novel, potent, dual endothelin receptor antagonist that recently demonstrated efficacy in the treatment of difficult-to-treat (resistant) hypertension. The aim of this study was to develop a population pharmacokinetic (PK) model describing aprocitentan plasma concentration over time, to investigate relationships between subject-specific factors (covariates) and model parameters, and to quantify the influence of the identified covariates on the exposure to aprocitentan via model-based simulations, enabling judgment about the clinical relevance of the covariates.
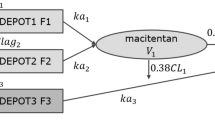
PK data from 902 subjects in ten Phase 1, one Phase 2, and one Phase 3 study were pooled to develop a joint population PK model. The concentration-time course of aprocitentan was described by a two-compartment model with absorption lag time, first-order absorption and elimination, and reduced relative bioavailability following very high doses of 300 and 600 mg.
The population PK model described the observed data well. Volume and clearance parameters were associated with body weight. Renal function as reflected by estimated glomerular filtration rate (eGFR), hepatic impairment, and sex were identified as relevant covariates on clearance.
The subject-specific characteristics of body weight, eGFR, hepatic impairment, and sex were shown to influence exposure parameters area under the concentration-time curve and maximum concentration in steady state to a limited extent, i.e., not more than 25% different from a reference subject, and therefore do not warrant dose adjustments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
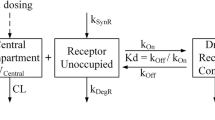
Aprocitentan (ACT-132577) is a once-daily, orally active, dual endothelin (ET) receptor antagonist that recently demonstrated efficacy in the treatment of difficult-to-treat (resistant) hypertension [1, 2]. The compound targets a different pathophysiological pathway than current treatments, as it inhibits the binding of endothelin, a potent vasoconstrictor peptide, to ETA and ETB receptors [3,4,5]. Blocking this pathway could therefore represent a new mode of action to lower blood pressure in patients who do not achieve blood pressure control with the currently available treatments. Aprocitentan decreased blood pressure without affecting heart rate in different animal models of hypertension with various renin levels and demonstrated an effect in renin-salt-sensitive models in which it also improved renal hemodynamics and cardiac remodeling [6]. In humans, orally administered aprocitentan at doses of 10, 25, and 50 mg produced clinically meaningful reduction in blood pressure in patients with mild to moderate hypertension [7] and at doses of 12.5 and 25 mg o.d. in difficult-to-treat (resistant) hypertension in subjects who concomitantly received at least three other drugs of various drug classes in the recently completed Phase 3 PRECISION study [1].
Aprocitentan was found safe and well tolerated in male and female subjects without hypertension, showing favorable pharmacokinetic (PK) properties for once-daily dosing based on a half-life of 44 h [8]. Aprocitentan is primarily eliminated via urine (52%) and feces (25%), with metabolism mostly via glucosidation and hydrolysis [9]. Subjects with severe renal or moderate hepatic impairment were found to have lower clearance, leading to 32% and 22% higher exposure (area under the curve over a dosing interval) with no need for dose adjustments [10, 11].
Aprocitentan has no active metabolites and no known relevant interactions with other drugs [9], including CYP3A and BCRP substrates [12, 13]. After multiple dosing, accumulation at steady state was 3-fold, and only minor differences in exposure between females and males were observed [8]. Additionally, no clinically relevant PK differences were found between Japanese and Caucasian subjects, and therefore no significant differences in PK are anticipated in other ethnicities [14]. These pharmacokinetic properties support use in a resistant hypertensive patient population in which adherence to antihypertensive medications, a key component to control blood pressure levels, has proven difficult [15]: with the long half-life and moderate accumulation at steady state, missed doses are not expected to immediately impact exposure to aprocitentan.
The Phase 1 program included a safety study in subjects on a high-sodium diet, investigating whether aprocitentan may cause fluid retention and edema as these are concerns with ET receptor antagonists. Only a moderate body weight increase without obvious sodium retention was observed and PK were similar as observed in other studies in subjects not receiving a high sodium-diet [16]. As anticipated for ET receptor antagonists, edema or fluid retention was the most common adverse event reported with aprocitentan within 4 weeks of treatment in the PRECISION study, though this was clinically manageable with the addition or up-titration of diuretic therapy [1].
To date, PK data following oral aprocitentan administration have been collected in ten Phase 1 studies [8,9,10,11,12,13,14, 16,17,18], one Phase 2 dose-finding study [7], and one Phase 3 study [1]. The objective of this study was to develop a population PK model describing aprocitentan plasma concentration over time, to investigate the relationship between subject-specific factors (covariates) and model parameters, and to quantify the influence of identified covariates on the PK of aprocitentan via model-based simulations, enabling judgment about the clinical relevance of the covariates and guiding of dosing recommendations.
Methods
Data
PK data following oral aprocitentan administration were pooled from ten Phase 1 studies, a Phase 2 dose-finding study in subjects with essential hypertension, and a Phase 3 study in subjects with resistant hypertension. The doses administered ranged from 5 mg to 600 mg (single dose) and 100 mg (multiple doses). Ethics approval for each study was obtained from the respective local ethics committee(s), and all subjects gave written informed consent. The Phase 1 studies included a three-part single ascending dose and multiple ascending dose (SAD/MAD) study including assessment of the effect of age and food on PK; a mechanistic study in subjects on a high sodium diet; two drug-drug interaction (DDI) studies with the CYP3A4 substrate midazolam and the BCRP substrate rosuvastatin; an absorption, distribution, metabolism, and excretion study; two special population studies in subjects with severe renal function impairment (eGFR 15–29 mL/min/1.73 m2) and moderate hepatic impairment; an ethnic sensitivity study in Japanese compared to Caucasian subjects; a thorough QT study; and a bioequivalence study with two aprocitentan tablet formulations in which the active pharmaceutical ingredient had different drug particle size distributions. Eight Phase 1 studies collected data in a dense sampling scheme with at least 12 PK samples per subject and two studies collected data sparsely. The Phase 2 and 3 studies provided 1–7 samples per subject taken at steady-state trough times (Table S1).
In the population PK modeling, measurements below the lower limit of quantification (LLOQ) were set to the LLOQ of 5 ng/mL and treated as censored with simulation from a distribution restricted to the range 0.05 - LLOQ, as per M4 method [19]. Records with missing information including time of measurement or dosing event, drug concentration, or amount of dose were discarded. Missing continuous covariates were imputed by the population median, and missing categorical covariates were imputed by the most frequent category. Subjects with no creatinine measurement available were excluded based on a predefined protocol deviation specification.
Given the wealth of data, a conservative approach was taken regarding inclusion of data. Highly implausible measurements were excluded from the analysis, following pre-specified criteria. These included PK data from subjects for whom concentration measurements were below the LLOQ with no indication of non-compliance or dosing interruption in the dosing history and PK measurements from subjects that were low at time points at which concentrations were expected to be high, e.g., at the time when the maximum plasma concentration (tmax) is usually reached. These data originated mostly from the Phase 2/3 studies. Additionally, PK measurements from subjects excluded from PK analysis due to predefined protocol deviations including missing creatinine data and data collected on days at which subjects received comedication in the DDI studies were not included.
Model development
Population PK modeling was performed using nonlinear mixed effects modeling with Monolix 2021R1 [20]. The Stochastic Approximation Expectation-Maximization (SAEM) algorithm was used for parameter estimation [21]. The population PK model was developed in a stepwise manner. (1) Selection of the structural model that best described aprocitentan plasma concentration over time based on data from Phase 1 studies with dense PK sampling. Evaluated structural models included zero- and first-order absorption with lag time, one-, two-, and three-compartment distribution, and first-order elimination. (2) Combination of all PK data, i.e., data from all Phase 1 studies as well as Phase 2 and Phase 3 studies in subjects with essential hypertension and resistant hypertension, respectively, and re-estimation of model parameters. If re-estimation was inaccurate when combining all data, absorption rate and lag time were to be fixed to the estimates from subjects with dense PK data (Step 1), assuming that dense well-controlled single-center PK data from Phase 1 studies would be suited best to characterize the absorption phase. (3) Covariate analysis was conducted in three steps. First, body size measures including body weight, body mass index (BMI), lean body weight, and fat mass were assessed as covariates for volume and clearance parameters. BMI, lean body weight and fat mass were only to replace allometric scaling based on body weight if the model fit would improve.
Next, the candidate covariates for clearance and volume parameters (age, sex, race, disease) and for clearance only (renal impairment, creatinine clearance, eGFR as defined by the MDRD formulaFootnote 1 [22, 23] (Modification of Diet in Renal Disease Study), hepatic impairment, diabetes) were investigated with an automated covariate search algorithm, COSSAC, using a forward-backward methodology with thresholds of p < 0.05 for inclusion and p < 0.01 for backward deletion [24].
Third, time-varying covariates were evaluated as covariates for absorption rate and lag time separately after automated covariate search for technical reasons. These covariates were food status (fed, fasted, uncontrolled) and formulation. The formulations were capsule and film-coated tablets A and B containing drug substance with different particle size distributions.
The categorical covariates food status and formulation and their respective model parameters were included into the model if the parameter estimate for at least one category was statistically significantly different from 0.
Categorical covariate-parameter terms were implemented as power relationships, i.e., Parameter = θ * exp(βθ,cov) where θ is the population parameter for the reference covariate category, and βθ,cov is the covariate effect parameter. Categorical covariates were investigated versus a specified reference category, typically the most frequent.
Continuous covariate-parameter terms were included in the model as power relationships, i.e., Parameter = θ*(cov/referencecov)βθ,cov where θ is the population parameter for the reference covariate value, and βθ,cov is the parameter estimate for the covariate effect. Reference values for centering were chosen as round values close to observed medians.
The model was evaluated based on the precision of the parameter estimation using relative standard errors (%RSE), goodness-of-fit plots of observations vs. predictions, and residuals vs. time and vs. predictions. Predictive model performance was assessed based on visual predictive checks (VPCs) stratified by dose group. In addition, a statistical criterion, the corrected Bayesian Information Criterion (BICc) was used as the preferred measure for the goodness of fit of the model to the data [25]. The BICc is a composite of log-likelihood and penalty terms for the complexity of the model, i.e., the number of fixed-effect and random-effect parameters. Lower values indicate a better fit with respect to balancing goodness of fit vs. model complexity, i.e., number of parameters.
Simulations
Based on the final PK model, population-typical predictions were performed to visualize the impact of covariates on exposure parameters including steady-state maximum plasma concentrations within a dosing interval (Cmax,SS) and area under the plasma concentration-time curve for a steady-state dosing interval (AUCτ,SS). These predictions included varying covariate scenarios, with 10th and 90th percentiles compared to the median value for continuous covariates and each category compared for categorical covariates, and an anticipated high clinical exposure scenario (with each covariate contributing to increased aprocitentan concentrations) compared to a reference subject with body weight of 87 kg (median of all subjects), eGFR of 90 mL/min/1.73 m2 (close to the overall median of 89 mL/min/1.73 m2) female, in fasted state, and without hepatic impairment. Predictions were performed in Berkeley Madonna version 10.2.8 [26, 27].
R versions 3.6.1 and 4.0.4 [28] with additional R packages were used for data processing and exploratory analyses and visualization of results, respectively.
Results
Data
A total of 902 subjects was included in the PK modeling data set, of which 251 subjects participated in Phase 1, 226 subjects with essential hypertension in Phase 2, and 425 subjects with resistant hypertension in Phase 3 studies. The modeling data set comprised of 8450 concentration measurements, of which most (7413, 87.7%) were collected in the Phase 1 program. 498 records (5.6%) were excluded from the analysis based on predefined criteria. Subjects had a median (10th–90th percentile) age of 55 (30–71) years, body weight of 87 (67–120) kg, eGFR of 89 (59–122) mL/min/1.73 m2, included males (63%) and females (37%), and were predominantly Caucasian (75%), Black or African American (20%), or Asian (4%). More details are provided in the Supplementary Information (Tables S2 and S3).
Dose-normalized concentrations vs. time indicated dose proportionality up to 100 mg (Fig. 1). Lower dose-normalized concentrations over the dosing interval were observed following administration of 300 mg or 600 mg such that dose-dependent absorption models for rate and time lag were explored.
Dose-normalized aprocitentan concentration vs. time by dose. A subset of the modeling data set is visualized: data from subjects with a dense sampling scheme, in fasted state, without renal or hepatic impairment, and not on a high-sodium diet following a single dose or the first day of multiple doses in a study period. Open bullets indicate individual measurements, lines a nonparametric regression line (dose groups are indicated by colors)
Model development
Aprocitentan concentration-time data were best described by a two-compartment model with absorption lag time tlag, first-order absorption ka and first-order clearance CL for doses up to 100 mg. In absence of data following intravenous administration, the model was parameterized in terms of apparent volume of distribution and apparent clearance. A parameter for relative bioavailability (F) was introduced, fixed at 1 with estimated interindividual variability (IIV) to allow estimation of differences in F between subjects. F was estimated to be lower following administration of 300 and 600 mg and included as covariate for these two dose levels only.
Estimation of inter-individual variability based on only 6 subjects per dose indicated high uncertainty (3026% and 1501% for F and 9126% and 126,157% for tlag for 300 and 600 mg, respectively) such that model development was continued with fixed parameter estimates without inter-individual variability for F and no separate estimation of tlag for the highest doses. The estimated parameters for F were 0.78 and 0.56 for doses of 300 and 600 mg, respectively (21.7% and 43.6% lower than for doses up to 100 mg, respectively). Due to the high parameter uncertainty, covariate analysis was not conducted for these model parameters.
A continuous Emax function to capture F as function of dose was explored and rejected due to instability in parameter estimation.
Allometric scaling adequately captured the relationship of body weight to clearance and volume parameters. Including lean body weight and fat mass as covariates instead of allometric scaling based on body weight resulted in a slightly better model fit, however, the estimated effects on Q and Vp were approaching 0, indicating no pronounced relationship, and were estimated with low precision reflected by high RSEs (38.3% and 34.4%, respectively).
Diabetes was found to not have any impact on aprocitentan PK. The COSSAC approach identified race as covariate on Vc, and eGFR, hepatic impairment, disease status, and sex as covariates on clearance. Of these, eGFR, hepatic impairment, and sex were retained. Race on Vc was considered physiologically implausible, and the impact of disease was more likely to be attributed to study design with sparse sampling vs. dense sampling or to the expected lower compliance in Phase 2/3 studies compared to a controlled Phase 1 setting rather than disease status. Compared to subjects without hepatic impairment and without hypertension, subjects with moderate hepatic impairment had a 20.7% lower clearance, and male subjects had a 3.5% lower clearance than females (all other characteristics remaining identical).
Lastly, inter-occasional variability (IOV) was introduced to evaluate the time-varying covariates formulation and food status (data from cross-over studies) on tlag and ka. The covariate effect estimates for formulation approached 0, indicating limited impact on tlag and ka, and were associated with high RSEs indicating that inclusion did not improve the model fit. Food status was included, with most pronounced differences observed between fasted and fed status (tlag increased from 0.593 h [36 min] to 1.61 h, and ka decreased from 0.657 /h to 0.484 /h). Only minor differences were observed in subjects with uncontrolled food status (tlag and ka of 0.700 h [RSE 136%] and 0.586 /h [RSE 164%], respectively), but parameters in these groups were estimated with low precision as reflected by the high RSEs.
Food status was included into the model as covariate on tlag and ka. Clearance and volume parameters were found to increase with body weight, and clearance was also impacted by eGFR, hepatic impairment, and, to a smaller extent, sex. Aprocitentan clearance for a female subject vs. a male reference subject of 87 kg, without hepatic impairment and eGFR of 90 mL/min/1.73 m2 were estimated as 0.342 and 0.354 L/h, respectively. Parameter estimates of the final model are displayed in Table 1 and show high precision (low RSEs). Most RSEs were below 25%, indicating good precision of parameter estimates. RSEs above 25% were observed for the impact of Food status on ka (96% and 164% for fed and uncontrolled, respectively), food on tlag (136% for uncontrolled), sex on clearance (68.8%), and hepatic impairment on clearance (45.2%).
Inclusion of the covariates was evaluated visually, indicating the model adequately captured the variability between subjects (Figure S5). Most RSEs were below 25% indicating good precision of parameter estimates. Exceptions were RSEs for the impact of food status on ka (RSE 96% and 164% for fed and uncontrolled, respectively) and on tlag (RSE 136% for uncontrolled), and the impact of sex and hepatic impairment on clearance (RSE 68.6% and 45.2%, respectively). The residual error was low (14.6%).
The model was evaluated graphically with observations vs. predictions (Fig. 2) and a Visual Predictive Check (Figures S1 and S2), indicating the model described aprocitentan concentrations well in subjects from Phase 1 studies without hypertension and subjects with essential and resistant hypertension (from studies in Phases 2 and 3).
Simulations
Population-typical predictions based on the final population PK model were employed to enable judgment about the clinical relevance of the covariates identified in the model development process. Aprocitentan concentration-time profiles were derived from model predictions and compared to a reference subject of 87 kg with an eGFR of 90 mL/min/1.73 m2, female, and without hepatic impairment. Higher body weight corresponded to lower aprocitentan concentrations, lower eGFR corresponded to higher concentrations, moderate hepatic impairment corresponded to higher concentrations, and male sex corresponded to similar but slightly lower concentrations compared to the reference subject (Fig. 3).
Impact of covariates on aprocitentan concentration-time profiles following administration of 25 mg aprocitentan o.d. for 10 days. Lines: model-prediction of aprocitentan concentration vs. time for a reference subject with different body weight, food status, estimated glomerular filtration rate (eGFR), hepatic impairment (HI), and sex
The largest effects on exposure were seen in subjects with low eGFR (AUCτ,SS 23% and 35% higher and Cmax,SS 19% and 30% higher for 30 and 17 mL/min/1.73 m2, respectively) and moderate hepatic impairment (22% higher AUCτ,SS and 19% higher Cmax,SS). Only minor differences in PK parameters between subjects with different body weight, hepatic impairment, food status, or sex were observed (median less than 25% change compared to the reference subject). There was low variability in tmax of 4.3 h, except for subjects in fed state (6.2 h). Compared to fasted state, a slightly higher tmax of 4.7 h was observed in subjects with food status uncontrolled, of which most subjects were in Phase 2 and 3 programs with sparse PK sampling and in particular no samples around tmax.
For the high clinical exposure scenario, for a subject with a low body weight of 67 kg, in fed state, with moderate HI, and renal function impairment reflected by an eGFR of 17 mL/min/1.73 m2, steady state was achieved later, and exposure was higher, with a relative AUCτ,SS of 2.18 and Cmax,SS of 2.05 (Fig. 4).
Visualization of reference and anticipated high clinical exposure scenarios for aprocitentan concentration-time profiles following administration of 25 mg aprocitentan o.d. for 20 days. Green dashed line: prediction of aprocitentan concentration over time for a reference female subject of 87 kg, in fasted state, without HI, and an eGFR of 90 mL/min/1.73 m2. Red solid line: prediction of aprocitentan concentration over time for the anticipated high clinical exposure scenario in a female subject of 67 kg, in fed state, with moderate HI, and an eGFR of 17 mL/min/1.73 m2
eGFR = estimated glomerular filtration rate; HI = hepatic impairment; o.d. = once daily
Discussion
In this study, the first PK model describing aprocitentan concentration over time was developed based on a robust dataset pooling data from 902 subjects from 12 clinical studies. The large number of subjects with a wide age and body weight range, including males and females, subjects without hypertension, or subjects with (essential or resistant) hypertension allowed for identification of covariates and evaluation of the impact of these subject characteristics on aprocitentan PK. The model described the aprocitentan concentration data well across the dose range from 5 to 600 mg as indicated by observations vs. predictions (Fig. 2) and simulations from the model that were similar to the observed data (Figure S1 and S2). A future step could be linking PK to PD outcomes in subjects with and without hypertension.
Parameter estimates of the PK model based on this pooled dataset with all aprocitentan data available to date were in agreement with previously reported PK parameters from non-compartmental analyses based on individual study data (included in the pooled data set). The population model-based CL/F of 0.291 L/h for a 70 kg subject is similar compared to the previously reported CL/F of 0.293 L/h [10] and 0.309 L/h [11] and the population model-based apparent volume of 19.3 L (Vc + Vp) is similar compared to the previously reported Vz/F of 20.0 L [10] and 21.5 L [11]. The simulated time to reach steady state (Fig. 3) was in agreement with the previously reported results of the MAD study with steady state being reached by Day 8 [8].
The parameters were all estimated with reasonable accuracy as judged by the RSE. Food status uncontrolled is presumably a mixture of fed and fasted, i.e., a bimodal distribution. The high RSE might therefore just reflect the inhomogeneity of the category.
The RSEs for food status fed were 29.1% for tlag and 96% for ka, supported by p-values of < 0.001 and 0.125 using a correlation test. This finding despite the low number of subjects, 5, is possibly due to the well-controlled clinical Phase 1 environment.
The effect of hepatic impairment on clearance is similarly based on only 8 subjects in a dedicated Phase 1 study, resulting in an RSE of 45.2% and a p-value of 0.007. The high RSE for estimating the effect of sex on CL appears to be driven by the estimated small effect that is possibly only significant due to the large number of observations and the fact that RSE as the ratio of uncertainty and parameter estimate becomes large with a small nominator.
The relative change in PK parameters was compared to a female reference subject of 87 kg, with an eGFR of 90 mL/min/1.73 m2, and without hepatic impairment. Overall, the impact of the identified covariates is of limited clinical relevance. Even a combination of covariates leading to the anticipated high clinical exposure scenario resulted in only approximately doubling the exposure: a 25 mg dosing regimen in the extreme scenario would yield exposure equivalent to 50 mg, a dose found to be safe and well tolerated in the Phase 2 study. This scenario includes the very low eGFR value of 17 mL/min/1.73 m2. It is noted though that the population of treatment-resistant hypertension includes subjects with diabetes and renal failure and eGFR as low as 15 mL/min/1.73 m2 at times. A clinically more realistic eGFR level of 30 mL/min/1.73 m2 results in even smaller differences in exposure.
In comparison to the unexplained random IIV, the impact of covariates is small. As aprocitentan is developed for the treatment of difficult-to-control (resistant) hypertension, an indication that typically includes older patients with several comorbidities and multiple concomitant medications, the low variability in PK and the previously reported absence of effect of other drugs on aprocitentan [9] is favorable.
To account for the relatively lower concentrations following the highest doses of 300 and 600 mg (Fig. 1), dose was included as categorical covariate on relative bioavailability. A continuous function with an exponential relationship led to a worse fit, and an Emax model correlating dose with relative bioavailability was found to be not identifiable. Once parameters for Emax and the Hill factor were fixed to 1, the estimated ED50 still had a very high RSE and was therefore not preferred over a categorical covariate for doses of 300 and 600 mg only (i.e., substantially higher than the therapeutic dose and of limited clinical relevance).
The absorption component of the model showed that presence of food corresponded to delayed and slower absorption (higher tlag and lower ka). The parameters tlag and ka for uncontrolled food status were estimated between the parameter estimates for fed and fasted, i.e., showing consistency. Estimation precision was low, in particular for the uncontrolled food status that was presumably a mixture of fed and fasted such that low precision can be expected.
The final model included a lag time of 0.593 h (36 min). To account for the absorption delay, a transit compartment model with estimated mean transit time and transit rate was evaluated as well, showing improvement in BICc, however not in the goodness-of-fit plots and VPCs. Additionally, this model was numerically less stable, and both models (lag time and transit compartments) resulted in similar parameter estimates for clearance and volume parameters and therefore inclusion of a lag time was preferred.
In the automated search with the COSSAC algorithm [24], eGFR was identified as categorical covariate. However, to allow simulations across a wide range of eGFR values, eGFR was also evaluated as continuous covariate which improved the fit and was therefore preferred. Additionally, race as covariate on Vc was considered physiologically implausible, based on limited data (Table S3), and body weight was already included accounting for body size.
Conclusions
A population PK model for aprocitentan was developed with subject-specific characteristics of body weight, eGFR, hepatic impairment, sex, and food status included as covariates. These covariates were shown to influence PK parameters AUCτ,SS and Cmax,SS to a limited extent, i.e., not more than 25% different from a reference subject and approximately twice as high in a high clinical exposure scenario (e.g., female, low body weight, low eGFR, and moderate HI all contributing to an increased aprocitentan concentration). The clinical implications of differences in aprocitentan concentration between subjects with different characteristics are therefore practically negligible, which is favorable for a chronic treatment to be used for patients who frequently have several comorbidities and are treated with multiple concomitant medications.
Notes
eGFR = 186*CR− 1.154 * age− 0.203 * Fsex * Frace with CR creatinine concentration in serum (mg/dL), Fsex = 0.742 for sex female and 1 for sex male, and Frace = 1.210 for race black and 1 otherwise.
References
Schlaich MP, Bellet M, Weber MA et al (2022) Dual endothelin antagonist aprocitentan for resistant hypertension (PRECISION): a multicentre, blinded, randomised, parallel-group, phase 3 trial. Lancet 400:1927–1937. https://doi.org/10.1016/S0140-6736(22)02034-7
Clozel M (2022) Aprocitentan and the endothelin system in resistant hypertension. Can J Physiol Pharmacol 100:573–583. https://doi.org/10.1139/cjpp-2022-0010
Yanagisawa M, Kurihara H, Kimura S et al (1988) A novel potent vasoconstrictor peptide produced by vascular endothelial cells. Nature 332:411–415. https://doi.org/10.1038/332411a0
Iglarz M, Clozel M (2010) At the heart of tissue: endothelin system and end-organ damage. Clin Sci 119:453–463. https://doi.org/10.1042/CS20100222
Schiffrin EL (2001) Role of endothelin-1 in hypertension and vascular disease. Am J Hypertens 14. https://doi.org/10.1016/s0895-7061(01)02074-x. :83S-89S
Trensz F, Bortolamiol C, Kramberg M et al (2019) Pharmacological characterization of Aprocitentan, a dual endothelin receptor antagonist, alone and in combination with blockers of the Renin Angiotensin System, in two models of experimental hypertension. J Pharmacol Exp Ther 368:462–473. https://doi.org/10.1124/jpet.118.253864
Verweij P, Danaietash P, Flamion B et al (2020) Randomized dose-response study of the new dual endothelin receptor antagonist aprocitentan in hypertension. Hypertension 75:956–965
Sidharta P, Melchior M, Kankam MK, Dingemanse J (2019) Single- and multiple-dose tolerability, safety, pharmacokinetics, and pharmacodynamics of the dual endothelin receptor antagonist aprocitentan in healthy adult and elderly subjects. Drug Des Devel Ther Volume 13:949–964. https://doi.org/10.2147/DDDT.S199051
Sidharta PN, Fischer H, Dingemanse J (2021) Absorption, distribution, metabolism, and excretion of Aprocitentan, a dual endothelin receptor antagonist, in humans. Curr Drug Metab 22:399–410. https://doi.org/10.2174/1389200222666210204202815
Sidharta PN, Ulč I, Dingemanse J (2019) Single-dose pharmacokinetics and tolerability of Aprocitentan, a dual endothelin receptor antagonist, in subjects with severe renal function impairment. Clin Drug Investig 39:1117–1123. https://doi.org/10.1007/s40261-019-00837-x
Fontes MSC, Dingemanse J, Halabi A et al (2022) Single-dose pharmacokinetics, safety, and tolerability of the dual endothelin receptor antagonist aprocitentan in subjects with moderate hepatic impairment. Sci Rep 12:19067. https://doi.org/10.1038/s41598-022-22470-z
Sidharta PN, Dingemanse J (2020) Effect of multiple-dose Aprocitentan Administration on the pharmacokinetics of midazolam in healthy male subjects. Eur J Drug Metab Pharmacokinet 45:227–234. https://doi.org/10.1007/s13318-019-00590-8
Sidharta PN, Dingemanse J (2020) Effects of multiple-dose administration of Aprocitentan on the pharmacokinetics of Rosuvastatin. Clin Pharmacol Drug Dev 9:995–1002. https://doi.org/10.1002/cpdd.815
Fontes MSC, Dingemanse J, Sidharta PN (2021) Multiple-dose pharmacokinetics, Safety, and tolerability of Aprocitentan, a dual endothelin receptor antagonist, in healthy Japanese and caucasian subjects. Clin Pharmacol Drug Dev 10:718–725. https://doi.org/10.1002/cpdd.881
Raebel MA, Ellis JL, Carroll NM et al (2012) Characteristics of patients with primary non-adherence to medications for hypertension, diabetes, and lipid disorders. J Gen Intern Med 27:57–64. https://doi.org/10.1007/s11606-011-1829-z
Gueneau de Mussy P, Sidharta PN, Wuerzner G et al (2021) Effects of the dual endothelin receptor antagonist Aprocitentan on Body Weight and Fluid Homeostasis in healthy subjects on a high Sodium Diet. Clin Pharmacol Ther 109:746–753. https://doi.org/10.1002/cpt.2043
Sidharta PN, Brussee JM, Schultz A et al (2022) ACCP Abstract Booklet. Clin Pharmacol Drug Dev 11:1–112. https://doi.org/10.1002/cpdd.1151
Idorsia Pharmaceuticals Ltd (2022) Bioequivalence Study of Different Aprocitentan Tablet Formulations. In: ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT05196399. Accessed 26 Jun 2023
Beal SL (2001) Ways to fit a PK model with some data below the quantification limit. J Pharmacokinet Pharmacodyn 28:481–504. https://doi.org/10.1023/A:1012299115260
Lixoft (2021) Monolix documentation
Delyon B, Lavielle M, Moulines E (1999) Convergence of a stochastic approximation version of the EM algorithm. Ann Stat 27:94–128
Levey AS, Bosch JP, Breyer Lewis J et al (1999) A more Accurate Method to Estimate glomerular filtration rate from serum creatinine: a New Prediction equation. Ann Intern Med 130:461. https://doi.org/10.7326/0003-4819-130-6-199903160-00002
Levey AS, Coresh J, Greene T et al (2006) Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. https://doi.org/10.7326/0003-4819-145-4-200608150-00004
Ayral G, Si Abdallah J, Magnard C, Chauvin J (2021) A novel method based on unbiased correlations tests for covariate selection in nonlinear mixed effects models: the COSSAC approach. CPT Pharmacometrics Syst Pharmacol 10:318–329. https://doi.org/10.1002/psp4.12612
Delattre M, Lavielle M, Poursat MA (2014) A note on BIC in mixed-effects models. Electron J Stat 8:456–475. https://doi.org/10.1214/14-EJS890
Krause A, Lowe P (2014) Visualization and communication of pharmacometric models with Berkeley Madonna. CPT Pharmacometrics Syst Pharmacol 3:116. https://doi.org/10.1038/psp.2014.13
Marcoline FV, Furth J, Nayak S et al (2022) Berkeley Madonna Version 10–A simulation package for solving mathematical models. CPT Pharmacometrics Syst Pharmacol 11:290–301. https://doi.org/10.1002/psp4.12757
R (2020) R: a Language and Environment for Statistical Computing. Version 3.6.1 and 4.0.4, 2002, R Foundation for Statistical Computing
Acknowledgements
The authors would like to thank all study participants, all study teams, and specifically Denis Boutin for supporting the project with data science activities and Chih-hsuan Hsin for valuable discussions supporting the analysis.
Funding
All studies were funded by Idorsia Pharmaceuticals Ltd or Actelion Pharmaceuticals Ltd, Allschwil, Switzerland.
Author information
Authors and Affiliations
Contributions
J.M.B. and A.K. wrote the manuscript. P.S. and J.D. designed the research. J.M.B., P.S., J.D., and A.K. performed the research. J.M.B. and A.K. analyzed the data.
Corresponding author
Ethics declarations
Conflict of interest
At the time of analysis conduct, J.M.B., P.S., J.D., and A.K. were employees and/or shareholders of Idorsia Pharmaceuticals Ltd which develops aprocitentan as treatment for resistant hypertension.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Brussee, J.M., Sidharta, P.N., Dingemanse, J. et al. Population pharmacokinetics of the dual endothelin receptor antagonist aprocitentan in subjects with or without essential or resistant hypertension. J Pharmacokinet Pharmacodyn 51, 243–252 (2024). https://doi.org/10.1007/s10928-024-09902-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10928-024-09902-1