Abstract
Background
Aprocitentan is an orally active dual endothelin receptor antagonist that targets a novel pathway in the treatment of difficult-to-control (resistant) hypertension. The drug–drug interaction potential of aprocitentan on cytochrome P450 (CYP) 3A enzymes was investigated in this open-label, two-treatment single-sequence study.
Objectives
The primary and main secondary objectives were to study the pharmacokinetics of midazolam in the absence and presence of aprocitentan and the safety and tolerability of combined administration, respectively.
Methods
Nineteen healthy male subjects received a single dose of 8 mg midazolam. Thereafter, they started aprocitentan treatment (loading dose of 150 mg followed by 50 mg once daily) and received another single dose of midazolam with aprocitentan at steady state. Pharmacokinetics and tolerability of midazolam and its metabolite 1-hydroxy midazolam were assessed over 24 h after each midazolam administration.
Results
At steady state, aprocitentan did not affect the area under the plasma concentration-time curve and maximum plasma concentration (Cmax) of midazolam and 1-hydroxy midazolam, with a geometric means ratio (GMR) of midazolam + aprocitentan/midazolam alone close to 1 and 90% confidence intervals (CI) between 0.88 and 1.23. For the Cmax of 1-hydroxy midazolam the GMR (90% CI) was 0.86 (0.70–1.05). Somnolence, a known side-effect of midazolam, was reported as the most frequent adverse event. There were no relevant differences in tolerability parameters between treatments.
Conclusion
Aprocitentan does not alter the pharmacokinetics of midazolam to a clinically relevant extent and was well tolerated when administered concomitantly. Therefore, aprocitentan can be administered together with drugs that are substrates of CYP3A without dose adjustments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The results of this drug–drug investigation study did not show clinically relevant differences in pharmacokinetics, safety, and tolerability of the CYP3A substrate midazolam in the presence and absence of aprocitentan, a dual endothelin receptor antagonist. |
Based on the results, aprocitentan can be concomitantly administered with drugs that are substrates of CYP3A. |
1 Introduction
Aprocitentan is a dual endothelin receptor antagonist (ERA) that potently inhibits the binding of endothelin (ET)-1 to both ETA and ETB receptors [1]. ET-1 is one of the most potent vasoconstrictor peptides known and is formed by the vascular endothelium to maintain vascular tone and blood pressure (BP) [2,3,4]. Hypertension is one of the leading risk factors of cardiovascular disease mortality [5]. Five major drug classes are recommended for the treatment of hypertension either as monotherapy or in combination until BP control is achieved—angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, beta-blockers, calcium channel blockers, and diuretics [6, 7]. However, an important proportion of patients will continue to have uncontrolled BP despite lifestyle modifications and three-drug combination therapy at optimal doses including a diuretic. In the absence of a secondary cause of hypertension, such patients are classified as having difficult-to-control (resistant) hypertension. Despite specialist treatment, more drugs with a different mode of action are needed [8].
As difficult-to-control (resistant) hypertension is associated with volume expansion, which is a feature of salt-sensitive hypertension, treatment with ERAs could be of particular benefit for this patient population since ET-1 regulates BP in response to salt [9]. Indeed, in animals, aprocitentan showed greater efficacy in salt-dependent/low renin models of hypertension than in high/normal renin models [1]. In these models, aprocitentan also had a synergistic effect on lowering BP when given together with the renin–angiotensin system (RAS) blocking drugs, valsartan and enalapril. In contrast, spironolactone only had an additive effect when given together with such RAS-blockers [1].
In humans, aprocitentan was well tolerated up to single and multiple doses of 600 mg and 100 mg once daily, respectively [10]. Its pharmacokinetic profile was dose proportional up to these doses and was compatible with a once-daily dosing regimen based on a half-life (t½) of 44 h. Accumulation at steady-state was approximately 3-fold and no clinically relevant differences in pharmacokinetics for sex, age, and food intake were observed. Measurement of plasma ET-1 confirmed ETB antagonism at doses ≥ 25 mg after multiple-dose administration [10]. Preliminary information indicated that the majority of aprocitentan and its metabolites is eliminated in urine (52.1% of the administered radioactive dose) while 24.8% of the radioactive dose is recovered in feces. Metabolism of aprocitentan identified two main elimination pathways that were independent of cytochrome P450 (CYP) enzymes and relied on glucosidation by uridine 5′-diphospho-glucuronosyltransferase and chemical hydrolysis [11].
Following the successful Phase 2 dose-finding study in patients with essential hypertension (NCT02603809), doses of 12.5 and 25 mg aprocitentan are currently being tested in a Phase 3 study (NCT03541174). In this prospective, multi-center, blinded, randomized, parallel-group study the efficacy and safety of aprocitentan for difficult-to-control (resistant) hypertension in adults are investigated. As these patients often have co-morbidities and receive other pharmacological treatments, it was important, prior to initiation of this Phase 3 study, to understand whether aprocitentan would have an effect on drugs whose metabolism is dependent on CYP3A. In vitro studies investigating the inhibitory effect of aprocitentan on different CYP families indicated that aprocitentan inhibited metabolism of two markers of CYP3A, i.e., midazolam and testosterone, with a 50% inhibitory concentration of 7.3 µM and 11 µM, respectively. In vitro induction studies showed that aprocitentan increased CYP3A4 mRNA and enzyme activity in a concentration-dependent manner. It was therefore warranted to further investigate the drug–drug interaction potential of aprocitentan and substrate drugs of CYP3A in a clinical setting. At the time of conducting the study, doses for Phase 3 had not yet been selected. Therefore, a dose of 50 mg aprocitentan was chosen as this corresponded to the highest dose tested in Phase 2. Midazolam was selected as the index substrate, in line with regulatory guidance [12, 13]. A dose of 8 mg was selected based on prior published data and anticipation of possible induction of CYP3A4 leading to lower plasma concentrations of midazolam [14, 15].
2 Methods
The study (NCT02841761) followed the principles of the Declaration of Helsinki, its amendments, and good clinical practice, and the protocol was approved by an Independent Review Board (Integreview IRB, Austin, TX, USA). The study was conducted at Biotrial Inc., Newark, NJ, USA and ran from August 2016 to October 2016. All subjects provided written informed consent prior to screening.
2.1 Study Design
This study was a single-center, open-label, single-sequence Phase 1 study to investigate the effect of multiple oral doses of aprocitentan on the pharmacokinetics of midazolam and 1-hydroxy midazolam. Screening occurred from 3 to 21 days before first study treatment administration. After eligibility was established, the subjects returned to the clinic on Day 1. On Day −1, they received a single oral dose of 8 mg midazolam followed by a 24-h observation of pharmacokinetics, safety, and tolerability and subjects stayed overnight in the clinic. On Day 2, the subjects received a single oral loading dose of 150 mg aprocitentan after which they were released from the clinic. Thereafter, single oral doses of 50 mg aprocitentan were administered on the morning on Days 3, 4, and 5. Pharmacokinetics, safety, and tolerability assessments were performed on an ambulatory basis during this time. The subjects returned to the clinic on the evening of Day 5 and stayed there until the morning of Day 7. On the morning of Day 6, the subjects received a single oral dose of 8 mg midazolam together with 50 mg aprocitentan followed by a 24-h observation of pharmacokinetics, safety, and tolerability. An end-of-study (EOS) visit was performed 16–18 days after administration of the first study treatment.
It was anticipated that 20 subjects would be needed to achieve 16 evaluable subjects who would be required based on sample size calculations. During the study, it became clear that the number of 16 evaluable subjects would easily be reached and recruitment was therefore halted at 19 subjects.
2.2 Study Population
This study included 19 healthy male subjects. Subjects were eligible if they were between 19 and 45 years of age, had a body mass index of 18–30 kg/m2, were non-smokers and healthy based on a medical check including clinical laboratory tests, and did not have any known hypersensitivity to aprocitentan, midazolam, or their excipients. Previous treatment with any prescribed or over-the counter medication within 3 weeks prior to study treatment administration was not allowed.
2.3 Treatments
Three treatments were investigated. Treatment A consisted of a single oral dose of 8 mg midazolam on Day 1. Treatment B1 consisted of a single oral loading dose of 150 mg aprocitentan on Day 2 followed by oral doses of 50 mg aprocitentan on Days 3, 4, and 5.
Treatment B2 consisted of a single oral dose of 8 mg midazolam and 50 mg aprocitentan on Day 6. Midazolam was given as midazolam hydrochloride syrup (2 mg/mL, Roxane Laboratories Inc, Columbus, OH, USA).
A dose level of aprocitentan of 50 mg was selected in this study as this was the highest dose investigated in a dose-finding Phase 2 study. As steady-state conditions using a once-daily dosing regimen would only be attained around Day 8 based on the pharmacokinetic profile of aprocitentan, simulation of multiple-dose profiles applying a loading dose was performed using Phoenix WinNonlin 6.4 (Pharsight Corp., Mountain View, CA, USA) to shorten the time to steady state [10]. The mean absorption rate constant (ka), the mean elimination rate constant (ke), and the mean apparent volume of distribution (V/F) were estimated using data from the multiple ascending dose study [10] and model 3 (first-order input and elimination, 1-compartment model) was selected to simulate multiple-dose dosing regimens. Simulations using a loading dose of 150 mg followed by once daily doses of 50 mg suggested that steady-state conditions would be obtained by Day 5 with similar peak and total aprocitentan exposure as a dosing regimen of 50 mg aprocitentan once daily without a loading dose (data on file).
2.4 Pharmacokinetic Assessments and Bioanalysis
Blood samples for determination of midazolam and 1-hydroxy midazolam plasma concentrations were taken at 0 h (pre-dose), 10, 20, 30, and 45 min and 1, 1.5, 2, 3, 4, 6, 8, 10, 12, 16, and 24 h after midazolam administration on Days 1 and 6. Per time point, a volume of approximately 6 mL blood was drawn of which 2.5 mL and, for time points relevant to measurement of aprocitentan, 500 µL plasma was used for determination of plasma concentrations. A valid liquid chromatography coupled to tandem mass spectrometry (LC–MS/MS) (ACC GmbH Analytical Clinical Concepts, Leidersbach, Germany) was applied. The limit of quantification (LOQ) was 0.1 ng/mL for both analytes. The inter-batch coefficient of variation (precision) was ≤ 5.3 and 4.7% for midazolam and 1-hydroxy midazolam, respectively. The inter-batch accuracy ranged from − 6.0 to 6.0% for midazolam and − 6.0% to 5.0% for 1-hydroxy midazolam.
Plasma concentrations of aprocitentan were measured at trough on Days 2 (prior to first dosing of aprocitentan), 3, 4, 5, 6, and 7 (24 h after last aprocitentan administration). An LC–MS/MS method as previously described [10] was employed. The LOQ was 5.0 ng/mL. The inter-batch precision was ≤ 4.3%, whereas the inter-batch accuracy ranged from − 1.4 to 2.6%.
Pharmacokinetic parameters of midazolam and 1-hydroxy midazolam were determined by noncompartmental analysis using Phoenix WinNonlin 6.4. The measured individual plasma concentrations of aprocitentan were used to directly obtain maximum plasma concentration (Cmax) and time to Cmax (tmax). The area under the plasma concentration–time curve from time 0 to the last measurable concentration (AUC0–t) was calculated according to the linear trapezoidal rule using the measured concentration–time values above the LOQ. Values below the LOQ were set to zero. The area under the plasma concentration–time curve from time 0 to infinity (AUC0–∞) was calculated combining AUC0–t and AUCextra, where AUCextra represented an extrapolated value obtained by Ct/λz (Ct, the last measured plasma concentration above LOQ; λz, the elimination rate constant determined by log-linear regression of the plasma concentrations of the terminal phase). The t½ was calculated as 0.693/λz.
2.5 Tolerability Assessments
At screening, a medical history (including the recording of previous and concomitant medications), physical examination, and clinical laboratory tests were performed. All adverse events (AEs) that occurred after study treatment administration up to EOS were recorded. The study investigator assessed the relationship to study treatment and intensity of the AE. Other safety assessments included vital signs, body weight, 12-lead electrocardiogram (ECG), and clinical laboratory tests, which were performed from Day 1 to EOS.
2.6 Statistical Analysis
A precision estimate approach was applied for comparison of Cmax and AUC0–∞ between treatments. Assuming a within-group log standard deviation (SD) of 0.36 and 0.44 for Cmax and AUC0–∞, respectively, for midazolam, it was estimated that with a sample size of 16 subjects the lower and upper bounds of the 90% confidence interval (CI) of the geometric means ratio (GMR) Treatment B2 (midazolam + aprocitentan)/Treatment A (midazolam alone) would be 0.66−1.52 if the estimated ratio was 1. For 1-hydroxy midazolam, for a sample size of 16 subjects, assuming a within-group log SD of 0.44 and 0.41 for Cmax and AUC0–∞, respectively, the lower and upper bounds of the 90% CI of the GMR would also be 0.66–1.52 if the estimated ratio was 1.
The per-protocol set was used for pharmacokinetic evaluations. Pharmacokinetic parameters were summarized using geometric mean and two-sided 95% CI, or the median and range values for tmax. Mean plasma concentration–time profiles were plotted on both linear and semi-logarithmic scales. Differences between Treatment B2 (midazolam + aprocitentan) and A (midazolam alone) were explored using GMR and 90% CI (Treatment A as reference). Differences between treatments for tmax were explored using the Wilcoxon rank-sum test using the median difference and its 90% CI.
The all-treated set was used for the analysis of tolerability variables that were summarized descriptively by treatment. Treatment-emergent AEs (TEAEs) were defined as—treatment-emergent to Treatment A = from midazolam administration on Day 1 up to 24 h thereafter; treatment-emergent to aprocitentan = from first administration on Day 2 up to EOS; treatment-emergent to Treatment B2 = from midazolam administration on Day 6 up to 24 h thereafter.
3 Results
3.1 Subject Disposition
A total of 19 healthy male subjects were enrolled, received study treatment, and completed the EOS visit. Demographic information is displayed in Table 1. None of the subjects had a medical history that affected eligibility of participation to the study. Only minor deviations from the protocol occurred (e.g., delay in pharmacokinetic blood sampling, missing physical examination at EOS), that had no influence on the analysis of pharmacokinetics and safety.
3.2 Pharmacokinetic Evaluations
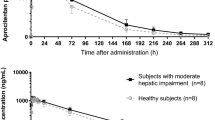
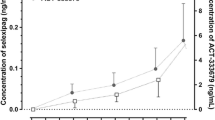
The plasma concentration–time profiles of midazolam and 1-hydroxy midazolam in the presence and absence of aprocitentan are shown in Fig. 1. After administration of midazolam alone, the Cmax of midazolam and 1-hydroxy midazolam was reached after 0.5 h. Thereafter, plasma concentrations declined rapidly with a geometric mean t½ of 4.2 and 5.8 h for midazolam and 1-hydroxy midazolam, respectively. Visual inspection of plasma concentrations of aprocitentan indicated that steady-state concentrations were achieved rapidly (i.e., by Day 3) following the loading dose of 150 mg. Therefore, on Day 6 co-administration of midazolam and aprocitentan was performed with subjects in a steady-state condition (Fig. 2). In the presence of aprocitentan, plasma concentrations of midazolam were generally slightly higher with a Cmax of 46.0 ng/mL compared to 44.2 ng/mL when given alone (Table 2). AUC0–t and AUC0–∞ were also minimally increased by approximately 14% (Table 3). Plasma concentrations of 1-hydroxy midazolam were similar in the presence and absence of aprocitentan, although a lower Cmax could be observed when midazolam was administered together with aprocitentan (Cmax of 21.9 ng/mL vs 25.6 ng/mL with and without aprocitentan, respectively). T½ increased from 5.7 to 8.8 h in the presence of aprocitentan (Table 2). Overall, no relevant impact was observed on AUC0–t and AUC0–∞.
Arithmetic mean (± standard deviation) plasma concentration–time profiles of midazolam (upper) and 1-hydroxy midazolam (lower) in healthy male subjects (n = 19) after administration of midazolam alone (Treatment A) or midazolam + aprocitentan (Treatment B2). Data on a semi-logarithmic scale are shown in an insert
When comparing the GMR and 90% CIs for Cmax, AUC0–t, AUC0–∞, and t½ to the interval of 0.80–1.25 that is commonly used in bioequivalence studies [16, 17], all 90% CIs of midazolam parameters were contained within this interval, as well as the 90% CI for AUC0–t and AUC0–∞ for 1-hydroxy midazolam (Table 3). The 90% CI of Cmax and t½ of 1-hydroxy midazolam were only partially contained (0.70, 1.05 and 1.11, 1.58 for Cmax and t½, respectively) (Table 3).
3.3 Tolerability
All treatments were well tolerated; no deaths, serious AEs or AEs leading to study treatment discontinuation occurred. During the study, 2 subjects received medications (i.e., paracetamol, nasal sodium chloride spray) for the treatment of AEs. A total of 60 TEAEs were reported in 19 (100%) subjects (Table 4). Somnolence was the most frequently reported TEAE which is an expected pharmacodynamic effect of midazolam. Headache was predominantly reported by subjects after treatment with aprocitentan (15 TEAEs in 9 subjects), while another headache was reported after aprocitentan and midazolam co-administration. All TEAEs were of mild or moderate intensity and resolved by EOS.
Incidental values outside the normal range were observed for clinical laboratory, vital signs, and ECG parameters. No treatment-related pattern could be discerned, and these excursions were not considered clinically significant by the principal investigator.
4 Discussion
Aprocitentan is a dual ERA that has the potential to be used in hypertensive subjects with multiple co-morbidities and co-medications. As such, it was important to investigate the effect of aprocitentan on substrates of CYP3A, as metabolism of many drugs is dependent on this enzyme [13, 18]. To test whether aprocitentan had a relevant effect on CYP3A, midazolam was selected as the index substrate. Midazolam has consistently been shown to be impacted to a clinically relevant extent by CYP3A inhibitors or inducers and is recommended by regulatory agencies [12, 13, 19,20,21]. The effect of 50 mg aprocitentan after multiple doses was investigated, which allowed observation of the net-effect on CYP3A under aprocitentan steady-state conditions, which is important as aprocitentan is intended for chronic use. At the time of conducting the study, the highest dose for Phase 3 studies had not been selected. Given that in patients with difficult-to-control (resistant) hypertension (NCT03541174) doses of 12.5 and 25 mg are studied, the results of this study cover aprocitentan exposure at its future intended use. In this study, a loading dose was applied to reach steady-state conditions earlier than 8 days, which would shorten the study duration for each subject and would require fewer ambulatory visits. Measurement of trough plasma concentrations of aprocitentan indicated that steady-state levels were achieved by Day 3, which was earlier than the model-predicted Day 5. A visual review of the arithmetic mean plasma concentrations measured at trough revealed some fluctuation during the study. However, as these levels fluctuated approximately only 10% between Days 5, 6, and 7, and the standard deviations of the arithmetic means overlap, this was not considered clinically relevant. Thus, the loading dose approach is an option to optimize study designs.
In this study, multiple-dose administration of aprocitentan did not impact the pharmacokinetics of midazolam and 1-hydroxy midazolam to a clinically relevant extent. Most of the 90% CI of the GMR were within the commonly used bioequivalence range of 0.80–1.25. Cmax and t½ of 1-hydroxy midazolam were partially contained within that range and were slightly lower and higher, respectively.
Overall, the most commonly reported TEAE was somnolence, which is an expected pharmacodynamic effect of midazolam. The most frequently reported TEAE associated with aprocitentan was headache, which is in line with previously published data [10]. The safety profiles of midazolam with and without aprocitentan did not differ and were in line with previous observations in clinical studies of both midazolam and aprocitentan.
5 Conclusion
The results of this drug–drug interaction study showed that multiple-dose administration of aprocitentan did not affect the pharmacokinetics and safety of the CYP3A substrate midazolam and its metabolite 1-hydroxy midazolam to a clinically relevant extent. Therefore, aprocitentan does not affect CYP3A and aprocitentan can be administered without any dose adjustment with drugs whose metabolism is dependent on this enzyme.
References
Trensz F, Bortolamiol C, Kramberg M, Wanner D, Hadana H, Rey M, Strasser DS, Delahaye S, Hess P, Vezzali E, Mentzel U, Menard J, Clozel M, Iglarz M. Pharmacological characterization of aprocitentan, a dual endothelin receptor antagonist, alone and in combination with blockers of the renin angiotensin system, in two models of experimental hypertension. J Pharmacol Exp Ther. 2019;368(3):462–73.
Dhaun N, Webb DJ. Endothelins in cardiovascular biology and therapeutics. Nat Rev Cardiol. 2019;16(8):491–502.
Haynes WG, Webb DJ. Contribution of endogenous generation of endothelin-1 to basal vascular tone. Lancet. 1994;344(8926):852–4.
Yanagisawa M, Kurihara H, Kimura S, Tomobe Y, Kobayashi M, Mitsui Y, Yazaki Y, Goto K, Masaki T. A novel potent vasoconstrictor peptide produced by vascular endothelial cells. Nature. 1988;332(6163):411–5.
Jagannathan R, Patel SA, Ali MK, Narayan KMV. Global updates on cardiovascular disease mortality trends and attribution of traditional risk factors. Curr Diab Rep. 2019;19(7):44.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):1269–324.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I, Group ESCSD. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–104.
FDA (2018) U.S. Food and Drug Administration, Center for Drug Evaluation and Research (CDER). Guidance for industry: hypertension: conducting studies of drugs to treat patients on a background of multiple antihypertensive drugs. Silver Spring, MD, USA. Draft Guidance, July, 2018.
Elijovich F, Laffer CL, Amador E, Gavras H, Bresnahan MR, Schiffrin EL. Regulation of plasma endothelin by salt in salt-sensitive hypertension. Circulation. 2001;103(2):263–8.
Sidharta PN, Melchior M, Kankam MK, Dingemanse J. Single- and multiple-dose tolerability, safety, pharmacokinetics, and pharmacodynamics of the dual endothelin receptor antagonist aprocitentan in healthy adult and elderly subjects. Drug Des Devel Ther. 2019;13:949–64.
Sidharta PN, Fischer H, Delahaye S, Dingemanse J. Absorption, distribution, metabolism and excretion of aprocitentan, a dual endothelin receptor antagonist, in humans (Abstract). Clin Pharmacol Drug Dev. 2019;8(S1):14–5.
EMA (2012) European Medicines Agency (EMA) – Committee for Medicinal Products for Human use (CHMP): Guideline on the investigation of drug interactions. (CPMP/EWP/560/95/Rev.1 Corr. 2). London, UK. 21 June 2012.
FDA (2017) U.S. Food and Drug Administration, Center for Drug Evaluation and Research (CDER): Guidance for industry: clinical drug interaction studies- study design, data analysis, and clinical implications. Silver Spring, MD.
Bornemann LD, Min BH, Crews T, Rees MM, Blumenthal HP, Colburn WA, Patel IH. Dose dependent pharmacokinetics of midazolam. Eur J Clin Pharmacol. 1985;29(1):91–5.
Juif PE, Boehler M, Donazzolo Y, Bruderer S, Dingemanse J. A pharmacokinetic drug-drug interaction study between selexipag and midazolam, a CYP3A4 substrate, in healthy male subjects. Eur J Clin Pharmacol. 2017;73(9):1121–8.
FDA (2017) U.S. Food and Drug Administration, Center for Drug Evaluation and Research (CDER): Waiver of in vivo bioavailability and bioequivalence studies for immediate-release solid oral dosage forms based on a biopharmaceutics classification system. Guidance for Industry. Silver Spring, MD: December 2017.
EMA (2010) European Medicines Agency (EMA) – Committee for Medicinal Products for Human use (CHMP): Guideline on the investigation of bioequivalence. (CPMP/EWP/QWP/1401/98 Rev.1 Corr). London, UK. 01 August 2010.
Zanger UM, Schwab M. Cytochrome P450 enzymes in drug metabolism: regulation of gene expression, enzyme activities, and impact of genetic variation. Pharmacol Ther. 2013;138(1):103–41.
Olkkola KT, Backman JT, Neuvonen PJ. Midazolam should be avoided in patients receiving the systemic antimycotics ketoconazole or itraconazole. Clin Pharmacol Ther. 1994;55(5):481–5.
Gorski JC, Jones DR, Haehner-Daniels BD, Hamman MA, O’Mara EM Jr, Hall SD. The contribution of intestinal and hepatic CYP3A to the interaction between midazolam and clarithromycin. Clin Pharmacol Ther. 1998;64(2):133–43.
Bjorkhem-Bergman L, Backstrom T, Nylen H, Ronquist-Nii Y, Bredberg E, Andersson TB, Bertilsson L, Diczfalusy U. Comparison of endogenous 4beta-hydroxycholesterol with midazolam as markers for CYP3A4 induction by rifampicin. Drug Metab Dispos. 2013;41(8):1488–93.
Acknowledgements
This study was conducted by Biotrial Inc, Newark, NJ, USA. The authors would like to thank Michael Dobrow, DO who served as principal investigator and JP Jones, PhD who was the Clinical Pharmacologist involved in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by Actelion Pharmaceuticals Ltd.
Conflicts of Interest
PNS and JD are current employees of Idorsia Pharmaceuticals Ltd and former employees of Actelion Pharmaceuticals Ltd, the company that funded the study. The authors report no other conflict of interest in this work.
Ethics Approval
The study (NCT02841761) followed the principles of the Declaration of Helsinki, its amendments, and good clinical practice, and the protocol was approved by an Independent Review Board (Integreview IRB, Austin, TX, USA).
Informed Consent
All subjects provided written informed consent prior to screening.
Rights and permissions
About this article
Cite this article
Sidharta, P.N., Dingemanse, J. Effect of Multiple-Dose Aprocitentan Administration on the Pharmacokinetics of Midazolam in Healthy Male Subjects. Eur J Drug Metab Pharmacokinet 45, 227–234 (2020). https://doi.org/10.1007/s13318-019-00590-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-019-00590-8