Abstract
The current study is an example of drug–disease interaction modeling where a drug induces a condition which can affect the pharmacodynamics of other concomitantly taken drugs. The electrophysiological effects of hypokaliemia and heart rate changes induced by the antiasthmatic drugs were simulated with the use of the cardiac safety simulator. Biophysically detailed model of the human cardiac physiology—ten Tusscher ventricular cardiomyocyte cell model—was employed to generate pseudo-ECG signals and QTc intervals for 44 patients from four clinical studies. Simulated and observed mean QTc values with standard deviation (SD) for each reported study point were compared and differences were analyzed with Student’s t test (α = 0.05). The simulated results reflected the QTc interval changes measured in patients, as well as their clinically observed interindividual variability. The QTc interval changes were highly correlated with the change in plasma potassium both in clinical studies and in the simulations (Pearson’s correlation coefficient > 0.55). The results suggest that the modeling and simulation approach could provide valuable quantitative insight into the cardiological effect of the potassium and heart rate changes caused by electrophysiologically inactive, non-cardiological drugs. This allows to simulate and predict the joint effect of several risk factors for QT prolongation, e.g., drug-dependent QT prolongation due to the ion channels inhibition and the current patient physiological conditions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The aging of societies [1, 2] and a consequent increase in burden of morbidity inevitably leads to the higher medicines consumption as the patients require multiple drugs regimens [3, 4]. Drug combinations are used not only to treat single or coexisting diseases, but also to elicit drug–drug interactions (DDI) which will maximize the effectiveness of therapy, or prevent side effects and improve the safety of pharmacotherapy [5]. However, when unintended, they may result in treatment failure or risk of harmful adverse effects [6,7,8,9]. Indeed, multidrug regimens and DDIs are significant causes of adverse effects and drug-related morbidity and mortality. Given the potential societal, individual and economical consequences of DDIs, the topic of DDI has been receiving a lot of attention from regulatory, industry and academia and much effort has been devoted to identifying, predicting and preventing of DDIs [10, 11]. The less investigated, but potentially equally significant, issue is a problem and consequences of interactions between drug and disease (DDisI) [12]. A drug-disease interaction occurs when an existing medical condition makes certain drugs harmful, or a drug exacerbates pre-existing conditions, or a drug induces a condition or change in physiology which affects pharmacokinetics (PK) or pharmacodynamics (PD) of its own, or another concomitantly taken drug. In many conditions, the PK and/or PD interactions with a disease impose restrictions in use of a certain medicine. Examples include, among many others: (1) liver diseases with their complex effects on drug clearance, biotransformation, and pharmacokinetics (e.g., elevated plasma drug concentrations and related toxicity) or pharmacodynamics [13]; (2) renal insufficiency and toxic drug concentrations resulting from impaired renal elimination, changes in absorption, distribution, protein binding, or non-renal clearance [14]; (3) altered absorption and pharmacokinetics in coeliac disease [15, 16]; (4) altered pharmacodynamics and reduced drug metabolism in diseases with inflammation process (e.g., rheumatoid arthritis, Crohn’s disease) due to the inhibitory action of some cytokines [17,18,19]; (5) pharmacodynamic interaction of beta-blockers and asthma or COPD, corticosteroids and diabetes, tricyclic antidepressants and arrhythmias, or nonaspirin NSAIDs and hypertension [20].
Drug–disease interactions are also important in cardiovascular problems, which are our primary research area. As mentioned before, inflammatory conditions play a role in the pathogenesis of cardiovascular diseases and their complications, which may alter the response to cardiac pharmacotherapy [19]. Some drugs and conditions may also favor the occurrence of cardiac side effects of pharmacotherapy, such as QT prolongation and TdP risk, via disturbances of electrolyte balance or heart rate changes. Bradycardia, an important factor increasing the risk of QT prolongation, was reported to be associated with anorexia and eating disorders [21], hypothyroidism, Hashimoto disease [22, 23], or autoimmune rheumatic diseases [24].
Pharmacodynamics of proarrhythmic drugs may also be substantially influenced by disruptions of ion homeostasis. The electrolyte imbalance may occur due to the various reasons including complication of certain illnesses, or medications intake [29,30,31,32,33,34,35].
Hypocalcaemia, hypomagnesemia, and especially hypokalemia lead to prolongation of cardiac repolarization [25,26,27,28], and carry additional risk for arrhythmias, especially in patients with inherent risk for rhythm disorder and those using drugs with QT-prolonging potential. Plasma ion imbalance should, therefore, be accounted for during simulation of drug effects on the ECG. The current study aimed at using the mechanistic modeling and simulation to assess the drug dependent physiology modification (i.e., potassium concentration changes), and its influence on QT interval.
The assessment of the QT prolongation risk of a drug candidate which does not have ion channel inhibition potency may not be straightforward. Testing all hypotheses in clinical and/or animal studies may be unfeasible. Therefore, modeling and simulation methods can complement experimental studies reducing the number of performed experiments. The concept of virtual twin known from the PBPK modeling has been recently utilized for the cardiac safety assessment [36]. In brief, the individual patient characteristics was linked to his or her virtual twin within a PBPK modeling framework to provide safe and effective individualized dosage as a component of truly personalized drug therapy at the point of care [37].
Materials and methods
Clinical data from the literature
A literature search was performed to identify potential sources of clinical data for the simulation study. The PubMed, Medline, and Google Scholar databases were screened for papers reporting QT interval changes in line with plasma potassium concentrations. The “QT”, “QTc”, “plasma potassium”, “depletion”, “drug” and their combinations were used as keywords. Four studies met the inclusion criteria, namely information about the drug concentration-dependent plasma potassium level, drug concentration-dependent heart rate level, and QT/QTc [38,39,40,41]. All the reports, where QTc length, potassium plasma concentration and heart rate at different time points of a clinical study with variability (SD—standard deviation or CV—cofficient of variation) were reported, were used for the simulation study.
Biophysically detailed models of the human cardiac physiology—CSS
The ten Tusscher ventricular cardiomyocyte cell model [42] was used to form a one-dimensional (1D) string mimicking the cross-section of the ventricular wall. The above mentioned model has been implemented in the Cardiac Safety Simulator (CSS) version 2.1 (Simcyp, Sheffield, UK, a Certara company), together with the database of human physiological, genotypic, and demographical data [43]. Therefore CSS platform allows generation of a realistic virtual population for the cardiac physiology during simulations, including accounting for circadian variability in heart rate, plasma concentration of electrolytes Na+, K+ and Ca2+ using covariate models derived from actual clinical data [44, 45]. Epidemiological models which take into account the effect of gender and age on ventricular heart wall thickness, cardiomyocyte volume/capacitance and sarcoplasmic reticulum are also built into the CSS platform [46]. The 1D string of cells (ventricular wall thickness) paced at the endocardial side used the 50:30:20 distribution of the endo, mid-, and epi-cardium cells respectively, with an average diffusion coefficient of 0.0016 cm2/ms. The forward Euler method was used to integrate the model equations with a space step and a time step of 0.01 mm and 0.01 ms respectively. Total simulation time was set to 10,000 ms, and during simulation, multiple beats were added at the beginning to reach a steady state and then withdrawn from the final analysis to assure stability and to avoid computation bias.
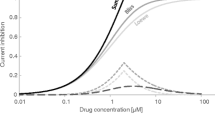
Physiological parameters modification
A heart-rate-corrected QT interval length was measured from reconstructed pseudo-ECG signals generated with the use of the CSS. The QT correction method employed was the same as in the relevant clinical trial, i.e., Bazett’s correction [47] in Clifton [40], Lecailon [39], and Tveskov [41] studies and Karjalainen correction [48] in Kuusela [38] study. The simulation scenario followed study methodology in the identified clinical trials regarding study population (number of participants, age, and gender) and data acquisition time. The data was extracted from the papers and used further to construct input files for the cardiac model. Each time point (or study phase) was simulated separately to account for the observed variability of potassium concentration and HR (converted to RR). The mean value and parameter variation expressed as CV were introduced into the model and constituted the basis for random sampling of values for individuals in the virtual study population. If the mean drug concentration was reported, the individual drug concentrations were randomly generated upon the mean and SD values for each time point, and drug dependent inhibition of ion channels was established using IC50 and Hill coefficient values. Neither for formoterol nor for the terbutaline in vitro data on their inhibitory potential against hERG ion channel was available. Thus IC50 values were predicted with the use of CSS built-in QSAR model [49]. Hill coefficient was assumed to be 1. Clifton and colleagues [40] did not report the terbutaline concentrations thus its influence on QT interval via ion channels inhibition was assumed negligible.
Results
There were four papers found to be eligible for the simulation study [38,39,40,41] (Table 1).
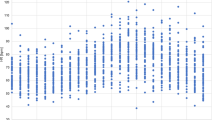
The mean potassium level and QT interval change profiles, and HR changes profiles if feasible, were digitized from the graphs presented in the clinical trials reports. Individual parameter values were then assigned randomly in the CSS for each reported study point. The report by Tveskov [41] provides baseline and maximal HR values only. Thus HR values for other time points were estimated based on linear interpolation between minimal and maximal HR time points. The results of HR and potassium concentration sampling are shown in Fig. 1. The results prove the correctness of the random sampling process.
Potassium concentration (SD) and HR (SD) sampling results in the reported study points. OBS values observed in a clinical study, SAM values sampled from the distribution defined by the coefficient of variation. X axis reported study points, Y axis potassium concentration [mmol/L] or HR [bpm], P placebo session, T terbutaline infusion session
The pseudo-ECG signals generated based on individually assigned potassium level and HR values were analyzed, and individual QTc interval length was calculated for each study participant as well as the study mean with standard deviation. The same QT interval correction method as in the reported clinical studies was applied for virtual trials. The mean values of simulated QTc intervals for occasions reported in study reports included placebo, different drug concentrations, or both, depending on the study. All virtual trial results are summarized in Fig. 2. The simulated QTc values were compared with the observed ones (Fig. 2 left panel), and differences were analyzed with Student’s t test with a 0.05 significance level.
The correlation of potassium level and QTc interval length is shown in Fig. 2 panel B. Table 2 presents Pearson’s correlation coefficients for QTc duration and potassium concentration.
Discussion
Potassium homeostasis is essential for the normal functioning of cardiac cells. Its derangement, both to hypo- and hyperkalemia, can lead to the cardiac rhythm abnormalities. Potassium level below the normal range has been identified as the risk factor for QT prolongation, a condition that may evoke Torsade de pointes and cause sudden cardiac death [27, 50]. Hypokalemia usually occurs as a complication of certain illnesses or medications (examples were given in the introductory section). Hypokalemia prevalence in the healthy general population is estimated at less than 1% but increases with age to 2–3% and with morbidity. Of patients with cardiovascular disease, 7–17% suffer from hypokalemia. Moreover, hypokalemia is present in up to 20% of psychiatric or hospitalized patients, and up to 40% of patients on diuretics [50,51,52,53,54].
This study aimed to assess the drug dependent potassium concentration changes and their consequences on QT interval. Plasma potassium concentration is an element of the whole body homeostasis. Its variation, including diurnal rhythmicity, influences and is combined with other ions level in plasma and other body fluids. At the same time potassium is an inevitable element of cell metabolic activity as presented in multiple sources [55,56,57]. Based on that it can be expected that the drug triggered plasma potassium level disruption will modify the cell homeostasis at various levels. In our study only electrical phenomena were accounted for and the approach has to be considered as the simplified version of reality.
Four clinical studies have been identified eligible for the study simulated. They considered bronchodilating agents, namely β2-adrenergic agonists, known to affect cardiac ventricular repolarization and increase the risk of ventricular arrhythmias by lowering plasma potassium concentration and affecting the beta-adrenergic system. The QSAR predicted IC50 values for compounds in question were 0.49 and 53.35 µM for formoterol and terbutaline, respectively. As plasma drug concentrations achieved during studies were at least two orders of magnitude lower than their IC50 values, no hERG channel-mediated influence on QT was expected. There was no current inhibition predicted by the model, accordingly. Therefore observed QT changes were linked solely with drug-induced potassium concentration alterations.
For all studies sampled and used for the simulations, values of HR and potassium concentrations closely reflected those which were measured in the reported studies (Fig. 1). The simulated results reflect the QTc interval changes measured in patients and their interindividual variability. Simulated QTc values were compared with those measured in the clinical studies usingStudent’s t-test. For four occasions (7.4%) in all the studies, the difference between predicted and observed QTc values was statistically significant (marked with the asterisk in the Fig. 2 panel A).
The change in QTc interval was highly correlated with the change in plasma potassium both in clinical studies and in the simulations (correlation coefficient, r > 0.60, with the exception of simulation of Lecaillon study with r = 0.55). This evidences that the model is able to properly replicate the anticipated mechanism of electrocardiograph abnormalities, i.e., effects of the decline in plasma potassium. As our model does not account for metabolic changes nor gene expression elicit by potassium level changes, the reasonably good prediction of the clinical endpoints of interest indirectly prove the negligible role of those components in the observed effect. In most cases, the mean QTc values and QTc changes resulting from lowering plasma potassium level were below thresholds of particular concern, i.e., QTc duration of < 500 ms and change < 30 or 60 ms [58, 59]. However, considering important interindividual variation of QTc values, it is possible that there are individuals with QTc prolongation above the safety limit within the group with acceptable mean QT value. Moreover, even moderate effects of hypokalemia when accompanied by other risk factors independently affecting the QT interval and the heart rate, especially the administration of strong hERG inhibitor or polytherapy with several QT-prolonging drugs, may put a patient at substantial cardiac risk.
Conclusions
The current study is an example of drug-disease interaction modeling where a drug induces a condition which can affect the pharmacodynamics of another concomitantly taken drugs. The results suggest that the modeling and simulation approach could provide valuable quantitative insight into the cardiological effect of the potassium and heart rate changes caused by electrophysiologically inactive, non-cardiological drugs. It can be assumed that changes resulting from other reasons, like a disease, dietary habits or gastrointestinal fluid loss would be simulated successfully. This allows to simulate and predict the joint effect of several risk factors for QT prolongation, e.g., drug-dependent QT prolongation due to the ion channels inhibition and the current patient physiological conditions.
References
Divo MJ, Martinez CH, Mannino DM (2014) Ageing and the epidemiology of multimorbidity. Eur Respir J 44:1055–1068. https://doi.org/10.1183/09031936.00059814
WHO Facts about ageing. In: WHO. http://www.who.int/ageing/about/facts/en/. Accessed 6 Oct 2017
Payne RA (2016) The epidemiology of polypharmacy. Clin Med 16:465–469. https://doi.org/10.7861/clinmedicine.16-5-465
Moen J, Antonov K, Larsson CA, Lindblad U, Nilsson JLG, Råstam L, Ring L (2009) Factors associated with multiple medication use in different age groups. Ann Pharmacother 43:1978–1985. https://doi.org/10.1345/aph.1M354
St. Louis EK (2009) Truly “rational” polytherapy: maximizing efficacy and minimizing drug interactions, drug load, and adverse effects. Curr Neuropharmacol 7:96–105. https://doi.org/10.2174/157015909788848929
Dechanont S, Maphanta S, Butthum B, Kongkaew C (2014) Hospital admissions/visits associated with drug-drug interactions: a systematic review and meta-analysis. Pharmacoepidemiol Drug Saf 23:489–497. https://doi.org/10.1002/pds.3592
Astrand B, Astrand E, Antonov K, Petersson G (2006) Detection of potential drug interactions—a model for a national pharmacy register. Eur J Clin Pharmacol 62:749–756. https://doi.org/10.1007/s00228-006-0143-x
McDonnell PJ, Jacobs MR (2002) Hospital admissions resulting from preventable adverse drug reactions. Ann Pharmacother 36:1331–1336. https://doi.org/10.1345/aph.1A333
Shad MU, Marsh C, Preskorn SH (2001) The economic consequences of a drug-drug interaction. J Clin Psychopharmacol 21:119–120
Hennessy S, Leonard CE, Gagne JJ, Flory JH, Han X, Brensinger CM, Bilker WB (2016) Pharmacoepidemiologic methods for studying the health effects of drug–drug interactions. Clin Pharmacol Ther 99:92–100. https://doi.org/10.1002/cpt.277
Lorberbaum T, Sampson KJ, Chang JB, Iyer V, Woosley RL, Kass RS, Tatonetti NP (2016) Coupling data mining and laboratory experiments to discover drug interactions causing QT prolongation. J Am Coll Cardiol 68:1756–1764. https://doi.org/10.1016/j.jacc.2016.07.761
Lau MHM, Tenney JW (2017) Evaluation of drug–disease interactions and their association with unplanned hospital readmission utilizing STOPP Version 2 criteria. Geriatrics 2:33. https://doi.org/10.3390/geriatrics2040033
Schenker S, Martin RR, Hoyumpa AM (1999) Antecedent liver disease and drug toxicity. J Hepatol 31:1098–1105
Nolin TD, Naud J, Leblond FA, Pichette V (2008) Emerging evidence of the impact of kidney disease on drug metabolism and transport. Clin Pharmacol Ther 83:898–903. https://doi.org/10.1038/clpt.2008.59
Wang I, Hopper I (2014) Celiac disease and drug absorption: implications for cardiovascular therapeutics. Cardiovasc Ther 32:253–256. https://doi.org/10.1111/1755-5922.12094
Tran TH, Smith C, Mangione RA (2013) Drug absorption in celiac disease. Am J Health-Syst Pharm 70:2199–2206. https://doi.org/10.2146/ajhp120689
Aitken AE, Richardson TA, Morgan ET (2006) Regulation of drug-metabolizing enzymes and transporters in inflammation. Annu Rev Pharmacol Toxicol 46:123–149. https://doi.org/10.1146/annurev.pharmtox.46.120604.141059
Schmitt C, Kuhn B, Zhang X, Kivitz AJ, Grange S (2011) Disease–drug–drug interaction involving tocilizumab and simvastatin in patients with rheumatoid arthritis. Clin Pharmacol Ther 89:735–740. https://doi.org/10.1038/clpt.2011.35
Sanaee F, Clements JD, Waugh AWG, Fedorak RN, Lewanczuk R, Jamali F (2011) Drug–disease interaction: crohn’s disease elevates verapamil plasma concentrations but reduces response to the drug proportional to disease activity. Br J Clin Pharmacol 72:787–797. https://doi.org/10.1111/j.1365-2125.2011.04019.x
Lindblad CI, Hanlon JT, Gross CR, Sloane RJ, Pieper CF, Hajjar ER, Ruby CM, Schmader KE (2006) Clinically important drug-disease interactions and their prevalence in older adults. Clin Ther 28:1133–1143. https://doi.org/10.1016/j.clinthera.2006.08.006
Casiero D, Frishman WH (2006) Cardiovascular complications of eating disorders. Cardiol Rev 14:227–231. https://doi.org/10.1097/01.crd.0000216745.96062.7c
Shojaie M, Eshraghian A (2008) Primary hypothyroidism presenting with Torsades de pointes type tachycardia: a case report. Cases J 1:298. https://doi.org/10.1186/1757-1626-1-298
Ker J (2012) Thyroxine and cardiac electrophysiology—a forgotten physiological duo? Thyr Res 5:8. https://doi.org/10.1186/1756-6614-5-8
Lazzerini PE, Acampa M, Guideri F, Capecchi PL, Campanella V, Morozzi G, Galeazzi M, Marcolongo R, Laghi-Pasini F (2004) Prolongation of the corrected QT interval in adult patients with anti-Ro/SSA-positive connective tissue diseases. Arthritis Rheum 50:1248–1252. https://doi.org/10.1002/art.20130
Franjic L, House SL, Vitkovitsky I, Halcomb SE (2012) QTc prolongation is associated with hypokalemia and hypocalcemia in emergency department patients. Conference abstracts and posters. Paper 12
Huang TC, Cecchin FC, Mahoney P, Portman MA (2000) Corrected QT interval (QTc) prolongation and syncope associated with pseudohypoparathyroidism and hypocalcemia. J Pediatr 136:404–407. https://doi.org/10.1067/mpd.2000.103447
Kallergis EM, Goudis CA, Simantirakis EN, Kochiadakis GE, Vardas PE (2012) Mechanisms, risk factors, and management of acquired long QT syndrome: a comprehensive review. Sci World J 2012:212178. https://doi.org/10.1100/2012/212178
Efstratiadis G, Sarigianni M, Gougourelas I (2006) Hypomagnesemia and cardiovascular system. Hippokratia 10:147–152
Rothenbuhler A, Marchand I, Bougnères P, Linglart A (2010) Risk of corrected QT interval prolongation after pamidronate infusion in children. J Clin Endocrinol Metab 95:3768–3770. https://doi.org/10.1210/jc.2009-2814
Oiwa H, Mokuda S (2015) Severe hypocalcemia and prolonged QT interval due to denosumab in an elderly woman with rheumatoid arthritis and chronic kidney disease. Letter to Editor. Eur J Rheumatol. https://doi.org/10.5152/eurjrheum.2015.0049
Veltri KT, Mason C (2015) Medication-induced Hypokalemia. Pharm Ther 40:185–190
Liljeqvist JA, Edvardsson N (1989) Torsade de pointes tachycardias induced by overdosage of zimeldine. J Cardiovasc Pharmacol 14:666–670
Kumar V, Khosla S, Stancu M (2017) Torsade de pointes induced by hypokalemia from imipenem and piperacillin. Case Rep Cardiol 2017:4565182. https://doi.org/10.1155/2017/4565182
Zeuli JD, Wilson JW, Estes LL (2013) Effect of combined fluoroquinolone and azole use on QT prolongation in hematology patients. Antimicrob Agents Chemother 57:1121–1127. https://doi.org/10.1128/AAC.00958-12
Albert RK, Schuller JL, COPD Clinical Research Network (2014) Macrolide antibiotics and the risk of cardiac arrhythmias. Am J Respir Crit Care Med 189:1173–1180. https://doi.org/10.1164/rccm.201402-0385ci
Patel N, Wiśniowska B, Jamei M, Polak S (2018) Real patient and its virtual twin: application of quantitative systems toxicology modelling in the cardiac safety assessment of citalopram. Am Assoc Pharm Sci J 20:6
Tucker GT (2017) Personalized drug dosage—closing the loop. Pharm Res 34:1539–1543. https://doi.org/10.1007/s11095-016-2076-0
Kuusela TA, Jartti TT, Tahvanainen KU, Kaila TJ (2005) Prolongation of QT interval by terbutaline in healthy subjects. J Cardiovasc Pharmacol 45:175–181
Lecaillon JB, Kaiser G, Palmisano M, Morgan J, Cioppa GD (1999) Pharmacokinetics and tolerability of formoterol in healthy volunteers after a single high dose of Foradil dry powder inhalation via Aerolizer. Eur J Clin Pharmacol 55:131–138
Clifton GD, Hunt BA, Patel RC, Burki NK (1990) Effects of sequential doses of parenteral terbutaline on plasma levels of potassium and related cardiopulmonary responses. Am Rev Respir Dis 141:575–579. https://doi.org/10.1164/ajrccm/141.3.575
Tveskov C, Djurhuus MS, Klitgaard NA, Egstrup K (1994) Potassium and magnesium distribution, ECG changes, and ventricular ectopic beats during beta 2-adrenergic stimulation with terbutaline in healthy subjects. Chest 106:1654–1659
ten Tusscher KH, Noble D, Noble PJ, Panfilov AV (2004) A model for human ventricular tissue. Am J Physiol Circ Physiol 286:H1573–H1589. https://doi.org/10.1152/ajpheart.00794.2003
Polak S, Wisniowska B, Fijorek K, Glinka A, Mendyk A (2014) In vitro-in vivo extrapolation of drug-induced proarrhythmia predictions at the population level. Drug Discov Today 19:275–281. https://doi.org/10.1016/j.drudis.2013.10.009
Fijorek K, Patel N, Klima L, Stolarz-Skrzypek K, Kawecka-Jaszcz K, Polak S (2013) Age and gender dependent heart rate circadian model development and performance verification on the proarrhythmic drug case study. Theor Biol Med Model. https://doi.org/10.1186/1742-4682-10-7
Fijorek K, Puskulluoglu M, Polak S (2013) Circadian models of serum potassium, sodium, and calcium concentrations in healthy individuals and their application to cardiac electrophysiology simulations at individual level. Comput Math Methods Med 2013:429037. https://doi.org/10.1155/2013/429037
Polak S, Fijorek K (2012) Inter-individual variability in the pre-clinical drug cardiotoxic safety assessment analysis of the age-cardiomyocytes electric capacitance dependence. J Cardiovasc Transl Res 5:321–332. https://doi.org/10.1007/s12265-012-9357-8
Bazett H (1997) An analysis of the time-relations of electrocardiograms. Ann Noninvasive Electrocardiol 2:177–194
Karjalainen J, Viitasalo M, Mänttäri M, Manninen V (1994) Relation between QT intervals and heart rates from 40 to 120 beats/min in rest electrocardiograms of men and a simple method to adjust QT interval values. J Am Coll Cardiol 23:1547–1553
Wiśniowska B, Mendyk A, Szlęk J, Kołaczkowski M, Polak S (2015) Enhanced QSAR models for drug-triggered inhibition of the main cardiac ion currents. J Appl Toxicol JAT 35:1030–1039. https://doi.org/10.1002/jat.3095
Kjeldsen K (2010) Hypokalemia and sudden cardiac death. Exp Clin Cardiol 15:e96–e99
Liamis R, Rodenburg E, Hofman A, Zietse R, Stricker B, Hoorn E (2013) Electrolyte disorders in community subjects: prevalence and risk factors. Am J Med 126:256–263
Lam MH, Chau SW, Wing Y (2009) High prevalence of hypokalemia in acute psychiatric inpatients. Gen Hosp Psychiatry 31:262–265. https://doi.org/10.1016/j.genhosppsych.2009.02.007
Widodo D, Setiawan B, Chen K, Nainggolan L, Santoso WD (2006) The prevalence of hypokalemia in hospitalized patients with infectious diseases problem at Cipto Mangunkusumo Hospital, Jakarta. Acta Med Indones 38:202–205
Bardak S, Turgutalp K, Koyuncu MB, Harı H, Helvacı I, Ovla D, Horoz M, Demir S, Kıykım A (2017) Community-acquired hypokalemia in elderly patients: related factors and clinical outcomes. Int Urol Nephrol 49:483–489. https://doi.org/10.1007/s11255-016-1489-3
Takahashi S, Driscoll BF, Law MJ, Sokoloff L (1995) Role of sodium and potassium ions in regulation of glucose metabolism in cultured astroglia. Proc Natl Acad Sci USA 92:4616–4620
Kones RJ (1976) Potassium metabolism in the normal and ischemic heart cell. Int J Clin Pharmacol Biopharm 13:269–291
Palmer BF (2015) Regulation of potassium homeostasis. Clin J Am Soc Nephrol 10:1050–1060. https://doi.org/10.2215/CJN.08580813
Kannankeril P, Roden DM, Darbar D (2010) Drug-induced long QT syndrome. Pharmacol Rev 62:760–781. https://doi.org/10.1124/pr.110.003723
Food and Drug Administration HHS (2005) International conference on harmonisation; guidance on E14 clinical evaluation of QT/QTc interval prolongation and proarrhythmic potential for non-antiarrhythmic drugs; availability. Notice. Fed Regist 70:61134-5
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wiśniowska, B., Polak, S. Drug–physiology interaction and its influence on the QT prolongation-mechanistic modeling study. J Pharmacokinet Pharmacodyn 45, 483–490 (2018). https://doi.org/10.1007/s10928-018-9583-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10928-018-9583-z