Abstract
Objective
The widespread use of pharmaceuticals prescribed by different physicians has caused the Swedish government to propose a new legislation with registration of all prescriptions dispensed at the Swedish pharmacies. In the present study, we wanted to examine the frequency, distribution and determinants of potential drug interactions.
Methods
The prescriptions from all individuals (n=8,214) with two or more prescriptions during October 2003 to December 2004 were collected from the ongoing Jämtland cohort study of a total of about 11,000 individuals. Potential drug–drug interactions were detected with a computerized interaction detection system and classified according to clinical relevance (types A–D).
Results
On average each individual filled 14.6 (men 14.3, women 14.8) prescriptions during the study period. 3.6% of the individuals used more than 15 different drugs. The number of detected potential drug interactions type A–D was 4,941 (men 1,949, women 2,992). The risk of receiving a potential interaction type A–D was estimated as the cumulative incidence 0.26 (2,116/8,214) overall, 0.22 (748/3,467) for men and 0.29 (1,368/4,747) for women during the 15-month study period. The age adjusted risk, RRadj, for women was estimated as 1.30. Excluding sex hormones and modulators of the genital system, the RRadj was 0.96, with no elevated risk for women. For potential interactions type D, that might have serious clinical consequences, 167 (cumulative incidence 0.0203) individuals (72 men, cumulative incidence 0.0208, 95 women cumulative incidence 0.0200) were detected. The risk of receiving a combination of potentially interacting drugs was positively correlated to age and polypharmacy. The cumulative incidence for elderly was estimated as 0.36 (65–84 years) and 0.39 (85 years and above). The relative risk for individuals with 15 drugs or more was estimated as 3.67 (95% CI 3.46–3.90).
Conclusion
In a general population there were relatively few severe potential drug interactions. The new Swedish national pharmacy register will provide health care professionals with a powerful tool to systematically review all prescriptions. An alert system should focus on the more potential drug interactions, type C–D, with close monitoring of elderly and patients with polypharmacy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Drugs can be used in combinations to obtain a desired therapeutic objective or to treat coexisting diseases. Such combinations may result in undesired interactions of a pharmacokinetic or pharmacodynamic nature resulting in undertreatment or toxic effects. The problems of polypharmacy and interactions are well known phenomena in general health care. However, the frequency of significant adverse drug interactions in the general population is unknown. Many individuals use multiple drugs (polypharmacy) which may multiply the effect in an unintended direction. The widespread use of pharmaceuticals, prescribed by several physicians unaware of each other, increases the risk of polypharmacy and drug–drug interactions, not at least among the elderly [14, 29, 36].
The Swedish government has approached the problems arising with the increasing use of drugs in the society. The development within the pharmaceutical arena has been very dynamic during the last 50 years. New chemical entities represent major therapeutic progress within many health care sectors. More diseases can be cured or alleviated resulting in an increase in quality of life. However, the new pharmaceutical therapies also have disadvantages. Adverse effects can lead to distrust, reduced compliance and even impaired symptoms and health status [1]. Furthermore, drug interactions are recognized as a cause for admissions to hospitals, especially for the elderly [9, 18].
A new individual-based national pharmacy register in Sweden is an attempt to manage the complexity of the problems [1]. The purpose of the national pharmacy register is to provide conditions for safer prescribing by making prescription purchase information available for the registered individuals, and also for all prescribers and pharmacists at all pharmacies after conditioned consent from the registered individual.
The national pharmacy register will contain the name and social security number of the registered individual along with day of purchase, product, prescribed amount and dosage. The information will be available for prescribers, pharmacists and the registered individual for 15 months. After that period, the material will be available for research only. The mandatory registration is in action as of July 2005.
The present study, based on an ongoing cohort study in the county of Jämtland, was conducted in order to examine the frequency, distribution and determinants of potential drug interactions. Most studies of drug interaction in clinical practice are limited to the elderly [30, 42], a short period [25, 30] or to particular health care settings [7, 22]. With a random sample of subjects of all ages, representative of the general population, for an extended period of time, our study was designed to mimic the new national pharmacy register, as it will be presented for prescribers and pharmacists in Swedish health care.
Methods
Study design and participants
The present study enrolled individuals from the Jämtland cohort study [5]. Jämtland is a small county (1.4% of the Swedish population) in the northwest part of Sweden. The proportion of persons aged 65 years and older was 20% in Jämtland in year 2004 as compared to 17% in all of Sweden. The county is mainly rural with one large town. The cohort contained all inhabitants born on the same 4 days each month. During the study period, 11,216 individuals were included (9% of the total population) in the cohort. All individuals included are informed and may leave the cohort whenever desired. However, the drop-out from the cohort is very low. Since year 1970, all ordinary prescriptions dispensed at pharmacies within the county are registered. In year 2004, 81% of all drugs prescribed to persons in Jämtland were dispensed as ordinary prescriptions at pharmacies in Jämtland and thereby available for the data collection. Data recorded included the social security number (giving age and gender), the drug and amount dispensed, the dosage and the time of dispensing. Data were recorded through Apoteket AB, the national corporation of Swedish pharmacies. In the present study, all individuals in the Jämtland cohort who collected two or more ordinary prescriptions at pharmacies within the county of Jämtland during the period October 2003–December 2004 were included. The age distribution in the Jämtland cohort was 0–14 (10%), 15–64 (64%), 65–84 (22%) and 85+ (3%) years as compared to 0–14 (9%), 15–64 (61%), 65–84 (26%) and 85+ (4%) years for the study population.
The chosen study variables and the length of the study period, October 2003 to December 2004, were intended to mimic the new national pharmacy register which will make prescriptions of an individual available for 15 months for prescribers, pharmacists and the registered individual. By including similar information as the national pharmacy register will do, the design of the present study provides a model to study the new register. During the 15-month study period, the included subjects’ prescriptions were recorded with date of sales, the drugs named by trade name and by the Anatomical Therapeutic Chemical (ATC) Classification System [39], along with information about the individual, including blinded individual number, gender and age. The criteria for inclusion in our study was that each individual in the cohort had filled two or more prescriptions during the study period at the pharmacies in the county of Jämtland, Sweden.
Each individual may be subject to one or more potential drug interactions by two or more drugs in combination. An individual may also fill prescriptions with the same generic entity several times during the study period. One single drug combination may also give rise to multiple interactions of different mechanisms. In the present study, we have registered the above mentioned interactions as one potential interaction for each individual.
Individuals residing in hospitals or in nursing homes without ordinary prescriptions were not included in the study.
The drug–drug interaction has been defined as ‘when the effects of one drug are changed by the presence of another drug’ [36] or more explicitly when a ‘pharmacological or clinical response to the administration of a drug combination is different from that anticipated from the known effects of the two agents given alone’ [38]. In the present study, we did not evaluate the actual outcome, but rather the risk of receiving prescriptions with potential drug interactions. We refer to the term ‘potential drug interaction’ as ‘the possibility that one drug may alter the intensity of pharmacological effects of another drug given concurrently. The net result may be enhanced or diminished effects of one or both of the drugs or the appearance of a new effect that is not seen with either drug alone’ [14].
In the present study, the definition of the general expression ‘drug’, was defined as the chemical entity or substance, which is the 5th level in the ATC classification [39].
Interaction detection
Potential drug–drug interactions were detected with a computerized interaction detection system, based on the interaction database published in Pharmaceutical Specialities in Sweden 2003. The drugs were matched by ATC code for each subject using an interaction classification system [35]. Each potential interaction was classified by type A, B, C or D (Table 1) according to the clinical relevance.
Statistical analysis
The frequencies of potential drug interactions in the study were compiled both for the subjects and the number of interactions. The distribution of potential drug interactions was stratified for age groups, gender and number of drugs on an individual basis. If not stated otherwise, the age strata used were 0–14, 15–64, 65–84 and 85 years and above.
The cumulative incidence was used as a measurement of the occurrence of potential drug interactions in the study population. The cumulative incidence can be seen as a measurement of the average risk on an individual level, conditioned that the risk is defined as the probability of an individual obtaining drugs with a potential interaction during the study period. The cumulative incidence was calculated as cumulative incidence =n/N where n denotes the number of individuals receiving drugs with potential interactions during the study period, and N all the subjects at risk (all included individuals with two or more prescriptions) at the beginning of the study.
The cumulative incidence always ranges from 0 to 1. It should be observed that the cumulative incidence was applied to the time period 15 months. The relative risk, RR, for one group compared to another was estimated as the rate ratio between cumulative incidences, RR=cumulative incidence1/cumulative incidence0. Cumulative incidence1 denotes the cumulative incidence of a potential drug interaction in the observed group, and cumulative incidence0 refers to the cumulative incidence in the cohort less the observed group. The relative risk was used as an effect measure of the strength of the association. When RR equals unity (=1) there is no difference between the compared groups [31]. RR with a 95% confidence interval (95% CI) including 1 was considered not statistically significant. Episheet (http://members.aol.com/krothman/episheet.xls) was used to calculate RR with 95% CI.
Statistix 8 (Analytical Software, Fla., USA) was used for descriptive statistics and all p-values were tested with two-sample t-test. Standard deviations, SD, were two sided. p<0.01 was regarded significant.
Results
Descriptive statistics
During the study period, October 2003 to December 2004, 8,214 individuals (Table 2) were included, filling two or more prescriptions, at pharmacies in the county of Jämtland. Of the individuals, 58% (n=4,747) were women and 42% (n=3,467) were men. The mean age of the study population was 50.1 years (SD 22.9). There was no difference (p=0.25) between the mean age for men (49.9, SD 22.6) and women (50.5, SD 23.3).
A total of 119,920 prescriptions were recorded during the 15-month study period and each individual filled on average 14.6 (SD 16.5) (men 14.3, SD 15.6, women 14.8, SD 17.1) prescriptions, without any difference (p=0.16) between men and women. We were not able to process 857 prescriptions lacking ATC classification, mostly extemporaenous preparations.
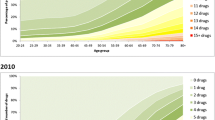
The frequency distribution showed that most individuals (54.5%) filled prescriptions for four or less different drugs during the study period; the mean number was 5.53, SD 4.22 (men 5.32, SD 4.01, women 5.69, SD 4.36). On average, women used a larger variety of drugs than men (p=0.0001). 11.3% of the individuals filled prescriptions for more than ten different drugs, and 3.6% used more than fifteen different drugs. The most extreme individual used 53 different drugs during the period. The mean number of drugs per individual increased with age from 3.4, 4.8, 7.6 to 8.0 in the respective age strata.
The number of detected potential drug interactions type A–D were 4,941 (men 1,949, women 2,992). Of the 8,214 individuals at risk, 2,116 individuals (748 men, 1,368 women) filled prescriptions with potential drug interactions type A–D during the period, i.e. each individual could have more than one potential drug interaction.
For potential interactions type D, that might have serious clinical consequences, 167 individuals (72 men, 95 women) were detected.
Risk estimation
Age
The mean age of the study population was 50.1 years (SD 22.9). The mean age of individuals with detected potential drug interactions was 62.8 (SD 17.4). The cumulative incidence for each age group were cumulative incidence0–14 0.032 (23/718), cumulative incidence15–64 0.24 (1,189/5,028), cumulative incidence65–84 0.36 (788/2,167), cumulative incidence≥85 0.39 (116/301). The estimated relative risk RR was increasing with age for each strata RR0–14 0.11 (95% CI: 0.077–0.172), RR15–64 0.81 (95% CI: 0.76–0.87), and RR65–84 1.66 (95% CI: 1.54–1.78). For the strata 85 years of age and above RR≥85 1.52 (95% CI: 1.32–1.77) there was a slight decline. The cumulative incidence for type D interactions were estimated as cumulative incidenceD 0–14 0.001 (1/718), cumulative incidenceD 15–64 0.014 (72/5,028), cumulative incidenceD 65–84 0.038 (82/2,167), and cumulative incidenceD ≥85 0.040 (12/301) (Table 3).
Gender
The risk of receiving drugs with a potential interaction type A–D was estimated as the cumulative incidence 0.26 (2,116/8,214) overall, 0.22 (748/3,467) for men and 0.29 (1,368/4,747) for women (Table 2). The RR for women was estimated as 1.34 (women/men 0.29/0.22) (95% CI: 1.24–1.44). Adjusted for age the RRadj for women was 1.30. The stratified analysis revealed that there was a difference only in the age strata 15–64; RR was estimated as 1.61 (95% CI: 1.44–1.80). With the ATC group G03 (sex hormones and modulators of the genital system) excluded, none of the age strata showed a different risk of receiving drugs with a potential interaction type A–D for women relative men. The age adjusted RRadj with G03 excluded was estimated as 0.96.
For clinically relevant interactions type D, that might have serious clinical consequences, the cumulative incidence was estimated as 0.0203 (167/8,214), 0.0208 (72/3,467) for men and 0.0200 (95/4,747) for women. RR for women compared to men was 0.96 (women/men 0.0200/0.0208) (95% CI: 0.72–1.30). None of the age strata showed a difference between men and women in the risk of obtaining drugs with potential interactions type D.
Polypharmacy
The risk of receiving drugs with a potential drug interaction showed a proportional positive linear relationship (coefficient of determination, R 2=0.97) with the number of drugs used during the study period. For individuals with two drugs the cumulative incidence was estimated as 0.05 (98/1,989) compared to individuals with more than 15 drugs 0.86 (254/294). The RR for individuals using more than 15 drugs was estimated as 3.67 (95% CI: 3.46–3.90).
Type C interactions
The most frequent potential drug interaction was of the type C (Fig. 1), which may modify the effect of another drug (Table 1). The age distribution of potential interactions type C displayed a bimodal distribution. In the age strata 15–64 years, 369 women had a potential interaction with drugs in the ATC group G03, of these women 318 (86%) had a type C interaction. After excluding G03, the curve was normal, negatively skewed and the residual peak showed a mean of 64.7 years of age (median 66 years, Q1 56 years, Q3 77 years) (Fig. 2).
For the age group 56–77 years, the most common potential type C interactions were nonsteroidal antiinflammatory drugs, NSAID, in combination with β-blocking agents (228 individuals), diuretics (172 individuals), and ACE-inhibitors (94 individuals). ACE-inhibitors also interacted with furosemide (147 individuals), insulins (76 individuals) and metformin (69 individuals).
Type D interactions
Potential drug interactions of the clinically significant type D (Table 1), were less frequent and constituted a minor portion at 7.9% (167/2,116) of the potential interactions detected. The age distribution showed the same distribution as the type C interactions adjusted for G03, with a median at 66 years (Q1 57 years, Q3 77 years). The most common potential type D interactions for the age group 57–77 was ipratropium with β2- adrenoreceptor agonists (30 individuals), NSAID with methotrexate (16 individuals) and with warfarin (10 individuals), β-blocking agents with verapamil (7 individuals), and organic nitrates with sildenafil (5 individuals).
Discussion
In a general population there were relatively few severe potential drug interactions. The risk of receiving drugs with a clinically relevant potential interaction type D is only present for 2 of 100 patients with two or more drugs. The potential drug interaction type C, which can be avoided by adjusting the dose and monitoring the effect or the plasma concentration, was ten times more frequent than the type D interaction.
Reports on actual drug interactions are not always well documented and can be based on animal data, in vitro data, small samples or case reports, and controlled studies are often restricted to healthy volunteers [34]. As a model for a national pharmacy register, our study only evaluated potential drug interactions and were not designed to estimate the incidence of actual drug interaction events.
Limitations
The potential drug interactions detected in the present study were probably slightly underestimated since only prescribed medications were included, but not over-the-counter nonprescription medications, herbal or home remedies [12, 16, 19, 37, 40, 41]. Moreover, drugs dispensed in hospitals and nursing homes without ordinary prescriptions were not included in the study.
On the other hand, the study might also have overestimated potential interactions since the time relationship for the concurrent use of drug combinations has not been evaluated during the study period.
The fact that the population in the Jämtland cohort is older than in Sweden in general might also imply an overestimation of the cumulative incidence of potential interactions among the elderly. However, it did not have any effect on the risk estimates. The validity of the Jämtland cohort was explored by comparing the 20 most common classes of drugs, at the 2nd level in the ATC-system, measured as defined daily doses, DDD/1,000 inhabitants/day in the cohort with the 20 most common classes for all of Sweden. The same groups were the most common in both cohorts but some differences in the level of use were found.
Incidences and Polypharmacy
The cumulative incidence 0.0203 of potential drug interactions type D in our study was lower than previously reported in the range 4–8% [4, 13, 29, 36]. The differences might be explained by the choice of study design, study population, frequency measures, classification system and inclusion criteria, e.g. age and health status, and the actual setting of the study with higher incidences for studies in high risk settings like emergency departments and lower incidences for the general elderly population. When comparing severe and clinically potential drug interactions often considerably lower incidences have been reported in the magnitude of 1.4% [25], or even lower incidences when taking into account concurrent use of the drug combinations; 1.9/1,000 patient year [7], supporting the findings in our study.
We found that the risk of receiving drugs with a potential drug interaction was strongly correlated to the number of drugs dispensed, which is supported by previous studies [20].
The elderly
In our study, the two elderly groups used on average 7.6 (65–84 years) and 8.0 (85 and above) different drugs during the 15-month study period. The level of the estimated cumulative incidence65–84 0.36 and cumulative incidence≥85 0.39 for potential drug interactions type A–D were well in accordance with other studies [2, 4, 8, 21], indicating an increased risk (RR65–84=1.66 and RR≥85=1.52) for elderly.
For the more severe type D interactions the cumulative incidences were estimated as 0.038–0.040 for the two groups of elderly, which were similar as previous findings; 3% [2], 4.4% [30] and 8% [4] .
The elderly, who may have an increased susceptibility due to an impaired function of several vital organ systems, frequently use multiple drugs [6, 8, 23, 24, 42]. Drug interactions in the elderly are often predictable and therefore represents avoidable health care costs and patients sufferings [33].
Potential drug interactions for elderly patients occur at a high rate 22% [22], 31% [2], 46% [4]. In a Danish study of the elderly, one-third were exposed to polypharmacy and, of these, 25% (age 60–79) and 36% (≥80 years) were exposed to potential drug interactions, of which diuretics, NSAIDs, ACE-inhibitors, digoxin, oral antidiabetics, calcium channel blockers, anticoagulants and β-blockers accounted for the highest number of potential interactions. When focusing only on major drug interactions, potassiumsparing diuretics and oral anticoagulants were the most frequently involved drugs [3]. The elderly at an outpatient medical clinic population had an incidence of potential interactions of 27% [21].
Gender
From our study we found no reason to expect that women are more exposed to potential drug interactions than men, sex hormones/modulators excluded. The 30% higher age adjusted risk of receiving drugs with a potential drug interaction type A–D for the women compared to the men was fully explained by women’s use of oral contraceptives and other gynecological drugs. After excluding all detected interactions with sex hormones and modulators of the genital system (ATC group G03), the original bimodal distribution frequency distribution showed a negatively skewed normal distribution and the adjusted RR was 0.96 (Fig. 2).
Interactions and hospitals
It is relevant to systematically monitor not only the type D interactions, but also the type C interactions in order to reduce drug interaction events and hospitalization. Drug interactions in the general population caused, in a study in 1993, admissions to hospitals with an incidence in the range of 0–2.8% [17]. The awareness of interactions may since then have been improved. A nested case-control study showed that the odds ratios for the association between hospital admission and drug toxicity for three specific drug combinations were 6, 12 and 20 times, respectively, more likely to have been exposed to the drug combination during the week preceding admission than controls [18]. Medication use prior to admission to an emergency unit was evaluated for the elderly; 538 of 1,000 patients were exposed to potential drug interactions. The number of side effects did not differ between the contraindicated drug associations and the associations that only required precautionary use [9].
In a study at an emergency department, 47% of patients (above 50 years) were found with drug interactions. The risk for a potential drug interaction rose from 13% for patients with two medications to 82% for those with seven medications and more [11]. Of 500 discharged medical patients, 60% had a potential drug interaction. Of those, more than 50% were new at the time of discharge due to a change of the medication during the hospital stay. 9% of the patients had a potential drug interaction of major severity [10].
Physician awareness
A national pharmacy register has the potential to alert prescribers on potential drug interactions. Experiences, however, are that alerts may generate little or no change in prescribing patterns [27]. The same was seen in a study with an automated system in which about 90% of the physicians overrode a computerized alert for high-severity drug interactions [28]. It seems necessary for an automated drug interaction alert system to differentiate between the different classes of drug interactions based on documentation and clinical relevance in order not to be neglected by the prescribers. One reason that clinicians do not react to alerts may be that their clinical experience is not align with the interaction system. In the present study some of the most common potential C and D interactions detected were detected for patients with ACE-inhibitors receiving blood glucose lowering drugs, heart failure patients receiving diuretics, patients with ipratropium (relevant only for nebulisers) and beta agonists and NSAIDS patients with methotrexate. These are all examples of common potential interactions that most clinicians find safe in daily use. In order to be useful tools the interaction systems must be clinically relevant. Furthermore, the prescribers should be offered relevant information and education.
The national pharmacy register can facilitate for the pharmacists to monitor for improper drug combinations. Pharmacists at community pharmacies intervened in one study to resolve prescribing-related problems in 1.9% of new prescription orders. A panel of three expert evaluators concluded that 28% of the prescribing problems identified during the study could have caused patient harm if the pharmacist had not intervened to correct the problem [32]. Of patients with potential drug interactions detected at a pharmacy, 44% had the dose changed and 75% were monitored for adverse clinical effects, after contact with the physician [15]. As pharmacists are mostly not in the position to evaluate if prescribers have monitored or adjusted the dose for potential type C interactions it seems relevant to monitor only for the more severe and clinically relevant interactions, type D, at pharmacies. With an automated system this represents an interaction in about 2 of every 100 patients per 15-month period. Furthermore, the clinical importance of drug interactions may vary depending on genetic and pathophysiological factors unknown to the pharmacist. Prior to alerting the prescriber of potentially interacting drug combinations, the actual time relationship and concurrency in use need to be evaluated by the pharmacist in dialogue with the patient.
The national pharmacy register has the potential to offer a new tool for prescribers and pharmacists to increase the quality in medication, avoiding improper use of polypharmacy and subsequent risk of drug interaction events. To obtain this, the register has to be timely updated and readily accessible, taking patient privacy into account.
Future studies
The new Swedish pharmacy register is not only intended to be of value for prescribers, pharmacists and the registered individuals, but also as a resource for researchers to study the individual based consumption of prescription medications. In combination with other health related databases it can be a powerful tool in risk assessment and pharmacoepidemiological studies. Utilization of the register always has to control for age, gender and the concurrent use of multiple pharmaceuticals. In order to establish a casual inference between an exposure of a drug and a drug related effect it is, however, important to evaluate the true health effects, not only the theoretical, potential risks.
The present study gave ideas for future studies evaluating the interaction risk for individual drugs [26], changes in pattern of drug interaction over time and evaluations of the true health effects of drug interactions.
Conclusion
By using the national pharmacy register prescribers will detect potential drug interactions type C-D in about 22 patients out of 100, with two or more prescription drugs. Considering only the more clinically relevant interactions type D, about 2 patients out of 100 may have a risk of experiencing a severe drug interaction. The risk for drug interactions is most emphasized for elderly patients with polypharmacy. We suggest that prescribers systematically monitor type C and type D interactions and that dispensing pharmacists examine type D interactions on a regular basis.
References
Prop. 2004/05:70 Ökad patientsäkerhet på läkemedelsområdet (Improved patient safety within the pharmaceutical arena). Socialdepartementet (Swedish Ministry of Health and Social Affairs), http://www.regeringen.se/sb/d/108/a/38890 2004-07-01
Bergendal L, Friberg A, Schaffrath A (1995) Potential drug-drug interactions in 5,125 mostly elderly out-patients in Gothenburg, Sweden. Pharm World Sci 17:152–157
Bjerrum L, Andersen M, Petersen G, Kragstrup J (2003) Exposure to potential drug interactions in primary health care. Scand J Prim Health Care 21:153–158
Bjorkman IK, Fastbom J, Schmidt IK, Bernsten CB (2002) Drug-drug interactions in the elderly. Ann Pharmacother 36:1675–1681
Boethius G, Wiman F (1977) Recording of drug prescriptions in the county of Jamtland, Sweden. I. Methodological aspects. Eur J Clin Pharmacol 12:31–35
Cadieux RJ (1989) Drug interactions in the elderly. How multiple drug use increases risk exponentially. Postgrad Med 86:179–186
Chen YF, Avery AJ, Neil KE, Johnson C, Dewey ME, Stockley IH (2005) Incidence and possible causes of prescribing potentially hazardous/contraindicated drug combinations in general practice. Drug Saf 28:67–80
Costa AJ (1991) Potential drug interactions in an ambulatory geriatric population. Fam Pract 8:234–236
Doucet J, Chassagne P, Trivalle C, Landrin I, Pauty MD, Kadri N, Menard JF, Bercoff E (1996) Drug-drug interactions related to hospital admissions in older adults: a prospective study of 1000 patients. J Am Geriatr Soc 44:944–948
Egger SS, Drewe J, Schlienger RG (2003) Potential drug-drug interactions in the medication of medical patients at hospital discharge. Eur J Clin Pharmacol 58:773–778
Goldberg RM, Mabee J, Chan L, Wong S (1996) Drug-drug and drug-disease interactions in the ED: analysis of a high-risk population. Am J Emerg Med 14:447–450
Gugler R, Allgayer H (1990) Effects of antacids on the clinical pharmacokinetics of drugs. An update. Clin Pharmacokinet 18:210–219
Hansten PD (2003) Drug interaction management. Pharm World Sci 25:94–97
Hardman JG, Limbird LE (2001) Goodman&Gilman’s The Pharmacological Basis of Therapeutics 10th International edn. McGraw-Hill Professional, New York, pp 54–56
Haumschild MJ, Ward ES, Bishop JM, Haumschild MS (1987) Pharmacy-based computer system for monitoring and reporting drug interactions. Am J Hosp Pharm 44:345–348
Henry D, Dobson A, Turner C (1993) Variability in the risk of major gastrointestinal complications from nonaspirin nonsteroidal anti-inflammatory drugs. Gastroenterology 105:1078–1088
Jankel CA, Fitterman LK (1993) Epidemiology of drug-drug interactions as a cause of hospital admissions. Drug Saf 9:51–59
Juurlink DN, Mamdani M, Kopp A, Laupacis A, Redelmeier DA (2003) Drug-drug interactions among elderly patients hospitalized for drug toxicity. Jama 289:1652–1658
Koch-Weser J, Greenblatt DJ (1977) Drug interactions in clinical perspective. Eur J Clin Pharmacol 11:405–408
Kohler GI, Bode-Boger SM, Busse R, Hoopmann M, Welte T, Boger RH (2000) Drug-drug interactions in medical patients: effects of in-hospital treatment and relation to multiple drug use. Int J Clin Pharmacol Ther 38:504–513
Kurfees JF, Dotson RL (1987) Drug interactions in the elderly. J Fam Pract 25:477–488
Linnarsson R (1993) Drug interactions in primary health care. A retrospective database study and its implications for the design of a computerized decision support system. Scand J Prim Health Care 11:181–186
Lipton HL, Bero LA, Bird JA, McPhee SJ (1992) The impact of clinical pharmacists′ consultations on physicians’ geriatric drug prescribing. A randomized controlled trial. Med Care 30:646–658
Manchon ND, Bercoff E, Lemarchand P, Chassagne P, Senant J, Bourreille J (1989) [Incidence and severity of drug interactions in the elderly: a prospective study of 639 patients]. Rev Med Interne 10:521–525
Merlo J, Liedholm H, Lindblad U, Bjorck-Linne A, Falt J, Lindberg G, Melander A (2001) Prescriptions with potential drug interactions dispensed at Swedish pharmacies in January 1999: cross sectional study. Bmj 323:427–428
Molden E, Garcia BH, Braathen P, Eggen AE (2005) Co-prescription of cytochrome P450 2D6/3A4 inhibitor-substrate pairs in clinical practice. A retrospective analysis of data from Norwegian primary pharmacies. Eur J Clin Pharmacol 61:119–125
Morera T, Gervasini G, Carrillo JA, Benitez J (2004) Early detection of drug interactions utilizing a computerized drug prescription handling system-focus on cerivastatin-gemfibrozil. Eur J Clin Pharmacol 59:917–921
Morera T, Gervasini G, Carrillo JA, Benitez J (2004) Using a computerized drug prescription screening system to trace drug interactions in an outpatient setting. Ann Pharmacother 38:1301–1306
Quinn D (1997) Clinically Important Drug Interactions. In: Speight TM, Holford N.H. (ed) Avery’s Drug Treatment, 4th edn. ADIS International, Auckland, Philadelphia, pp 301–328
Rosholm JU, Bjerrum L, Hallas J, Worm J, Gram LF (1998) Polypharmacy and the risk of drug-drug interactions among Danish elderly. A prescription database study. Dan Med Bull 45:210–213
Rothman KJ (1986) Modern Epidemiology. Little, Brown, Boston, Toronto, p 37
Rupp MT, DeYoung M, Schondelmeyer SW (1992) Prescribing problems and pharmacist interventions in community practice. Med Care 30:926–940
Seymour RM, Routledge PA (1998) Important drug-drug interactions in the elderly. Drugs Aging 12:485–494
Sjöqvist F (1997) Fundamentals of Clinical Pharmacology. In: Speight TM, Holford N.H. (ed) Avery’s Drug treatment, 4th edn. ADIS International, Auckland, Philadelphia, pp 52–53
Sjöqvist F (1997) A new classification system of drug interactions. Eur J Clin Pharmacol 52 (suppl.) Abstract 377
Stockley IH (2002) Stockley’s Drug Interactions, 6 edn. The Pharmaceutical Press, London, p 1
Strom BL (1994) Adverse reactions to over-the-counter analgesics taken for therapeutic purposes. Jama 272:1866–1867
Tatro DS, Olin BR (1992) Drug Interaction Facts. Facts and Comparisons, 3rd edn. Lippincott, St Louis
W.H.O. ATC Index. W.H.O. (2005) Collaborating Centre for Drug Statistics Methodology, http://www.whocc.no/atcddd/ 07–20
Vestal RE, Norris AH, Tobin JD, Cohen BH, Shock NW, Andres R (1975) Antipyrine metabolism in man: influence of age, alcohol, caffeine, and smoking. Clin Pharmacol Ther 18:425–432
Whitcomb DC, Block GD (1994) Association of acetaminophen hepatotoxicity with fasting and ethanol use. Jama 272:1845–1850
Zhan C, Correa-de-Araujo R, Bierman AS, Sangl J, Miller MR, Wickizer SW, Stryer D (2005) Suboptimal prescribing in elderly outpatients: potentially harmful drug-drug and drug-disease combinations. J Am Geriatr Soc 53:262–267
Acknowledgements
We are indebted to Sten-Erik Öhlund for developing the interaction detection software, to Mats Nordlöf for construction of Figs. 1 and 2 and to Apoteket AB for providing the crude data from the Jämtland study. The study was supported financially by Apoteket AB, including support to the E-Health Institute.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Åstrand, B., Åstrand, E., Antonov, K. et al. Detection of potential drug interactions – a model for a national pharmacy register. Eur J Clin Pharmacol 62, 749–756 (2006). https://doi.org/10.1007/s00228-006-0143-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-006-0143-x