Abstract
Prior investigations have examined risk factors associated to postpartum depression in immigrant women, but depression during pregnancy has received less attention. This study describes the prevalence and early determinants of antenatal depression among recent (≤ 5 years) and long-term immigrants (> 5 years), compared to Canadian-born women. 503 women completed standardized self-report questionnaires measuring sociodemographics and psychosocial factors. Multivariate logistic regressions identified first trimester risk factors for depression in each immigrant group. The prevalence of depressive symptoms was highest for recent immigrant (25.3–30.8%) compared to long-term immigrant (16.9–19.2%) and Canadian-born women (11.7–13.8%). Among recent immigrants, multiparity, higher stress and pregnancy-specific anxiety in early pregnancy increased the risk of antenatal depression. Among long-term immigrants, stress in the first trimester was significantly associated with antenatal depressive symptoms. Knowledge of modifiable risk factors (pregnancy-specific anxiety and stress) may help improve antenatal screening and inform the development of tailored interventions to meet the mental health needs of immigrant women during the perinatal period.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Background
In addition to regular parental demands, parents who have migrated experience various stressors, such as migratory stress, minority discrimination, language barriers and social isolation [1,2,3]. Immigrant women’s experience of psychological distress during pregnancy may be exacerbated because of their lower use of maternity-care services and mental health services due to various barriers, including their unfamiliarity with the health system, cultural beliefs or preferences, language barriers, lack of culturally tailored therapies, and the fear of being perceived as an unfit mother [1, 4, 5].
A growing body of research has demonstrated that postpartum depression (PPD) is highly prevalent in women who have immigrated, with a prevalence of 20% reported in high-income countries [3, 6], and of 6 to 37% reported in Canadian studies [7,8,9,10,11,12,13]. In fact, studies have shown higher risks for both elevated antenatal and postnatal depressive symptoms associated with immigrant status compared to native-born counterparts (for meta-analysis, [6]), which has similarly been reported in several Canadian studies [3, 8, 14].
Although prior research has largely focused on postnatal mental health, a growing body of literature suggests that the prevalence of depression during pregnancy is comparably high or greater than PPD [15,16,17]. While antenatal depression has been shown to be one of the strongest determinants of PPD [17,18,19,20], few studies have examined depression throughout pregnancy among immigrant women. A recent meta-analysis of sixteen studies, among immigrant women, reported a high prevalence (12%–45%) of clinically significant antenatal depressive symptoms (measured with self-report questionnaires) [3].
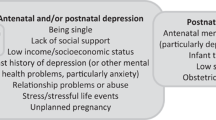
While a growing number of studies have examined risk factors associated to PPD in immigrant women [8, 13, 14], determinants of depression during pregnancy have received less attention. To date, risk factors that have been identified for antenatal depression in immigrant women have included younger age, shorter stay in host country, ethnicity (Black, Latin American, or Asian), poor social support, lower educational attainment, poor couple adjustment, obstetric problems, perceived stress, and stressful life events [21,22,23,24,25,26]. Pregnancy-specific anxiety has not been examined as a risk factor for antenatal depression among immigrant populations, however some evidence in a non-immigrant sample suggests it may be a risk factor for PPD [27], and general anxiety has been identified as a risk factor for antenatal depression among non-immigrant populations [18, 25]. Unplanned pregnancy, non-white ethnicity, lower educational attainment, lower income, food insecurity, perceived stress or stressful life events have also been reported as risk factors for antenatal depression in previous studies of non-immigrant women [25, 28,29,30,31,32,33,34].
Given the growing size of the immigrant population in Canada and this group’s vulnerability to psychological distress during the perinatal period which in turn may increase the risk of adverse maternal and infant outcomes, research into the risk factors associated with antenatal depression in this population warrants further study. While the findings to date suggest high prevalence rates for antenatal and postnatal depression among immigrant women, the course of antenatal depression throughout pregnancy and its risk factors have received relatively little attention in this population. Most studies have examined antenatal depression only in the third trimester of pregnancy [18, 35]. More prospective studies are needed to examine potential predictors of antenatal depressive symptoms as many previous investigations have been cross-sectional in design (for systematic review, [18, 30, 35]).
The current investigation sought to describe the prevalence and early determinants of depression during pregnancy among recent immigrant (≤ 5 years) and long-term immigrant women (> 5 years), compared to Canadian-born women. Similar to what has previously been reported for maternal PPD, we expected that recent immigrant women would be at elevated risk of experiencing depression during pregnancy compared to Canadian-born women. Unplanned pregnancy, non-white ethnicity, lower educational attainment, lower income, and food insecurity were expected risk factors for antenatal depression, as they have been reported in previous studies. Based on prior evidence, we expected that perceived stress and pregnancy-specific anxiety in the first trimester would be associated with depressive symptoms during at least one trimester of pregnancy for both immigrant and Canadian-born women.
Methods
The current study is part of a larger investigation to better understand the role of psychosocial factors associated with gestational weight gain and postpartum weight retention.
Participants
Pregnant women were recruited by a research assistant from community and hospital-affiliated obstetrical clinics within 2 McGill University affiliated hospitals (McGill University Health Centre–MUHC and St. Mary’s) (2014–2017). Women were eligible to participate if they (a) were at least 18 years of age; (b) were ≤ 12 weeks gestation; (c) were able to communicate in French or English; and (d) had access to the internet. Exclusion criteria included pre-existing medical conditions (i.e. type 1 or type 2 diabetes), gestational diabetes in a previous pregnancy, and multiple gestation (i.e. twins). These exclusion criteria were selected as these are factors known to influence gestational weight gain, which was part of the larger study. Eligible participants that indicated an interest in participating were given a secured website address to enter and provide informed consent and complete the standardized self-report questionnaires measuring sociodemographic and psychosocial variables in each trimester of pregnancy (weeks 13, 24, 36 of pregnancy). An e-mail prompt to the password secured website was sent to participants at each follow up with the battery of questionnaires (www.fluidsurveys.com). Ethics approval was granted by McGill Faculty of Medicine Institutional Review Board and the ethics review boards of the participating hospitals.
Measures
Socio-demographic information included age, ethnicity, education, marital status, income, work-status, parity, and food security.
Health information included medical history, current health, use of medications, date of last menstrual period.
The Edinburgh Postpartum Depression Scale (EPDS; 36]) is a widely used 10-item scale that assesses depressed mood in the past week. This scale was developed and validated for antenatal use [36, 37]. EPDS total scores range from 0 to 30, with higher scores indicating greater levels of depressive symptoms. A cut-off score of 12 or greater suggests a clinically significant level of depression and has been shown to have a sensitivity of 86 to 100% and a specificity of 78% to 94% [36,37,38]. The EPDS has been validated in diverse countries and ethnic groups [39,40,41,42,43,44].
Prenatal Distress Questionnaire Revised (PDQ-R; [45, 46]) is a 17-item measure assessing stress specific to pregnancy (medical care, physical symptoms, parenting, bodily changes and infants’ health). The PDQ-R has good psychometric properties and has been associated with poor health behaviours including smoking, unhealthy eating, and poorer physical activity, which are associated with poorer mental health [46]. The PDQ-R has been translated and validated across different cultural contexts [47,48,49,50].
Perceived Stress Scale (PSS; [51]) is a 10-item scale assessing the extent to which situations are appraised as stressful within the past month. The PSS has been shown to have adequate psychometric properties and is positively correlated with several self-report and behavioral measures of stress in adults [52]. The PSS has been translated into many languages and has demonstrated good psychometric properties in a wide range of cultures [53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68].
Analysis
Chi-square analyses and one-way ANOVAs were performed to determine whether the groups differed with respect to participant characteristics (see Table 1).
EPDS scores were dichotomized into a binary variable, using the clinical cut-off score of 12 or more to determine those with elevated depressive symptoms in at least one trimester (refer to Measures section for information on cut-off). Chi-square analyses were performed on this dichotomous variable representing elevated depressive symptoms to examine group (recent immigrant, long-term immigrant, Canadian-born) differences at each time point.
Three multivariate logistic regressions were performed to identify first trimester risk factors for elevated depressive symptoms for each group (recent immigrant, long-term immigrant, Canadian-born). Direct entry of the following variables was used to predict elevated depressive symptoms during pregnancy: parity (“one child” or “two or more children”), food security (insecurity in the past 12 months defined as sometimes or often you and other household members did not have enough to eat because there wasn't enough money to buy food, sometimes or often you had enough to eat, but not always the kinds of food you wanted because you couldn't afford it), education (“high school and less” or “more than high school (e.g. specialized training school, CEGEP, university”), pregnancy intention (“trying to get pregnant?” yes or no), ethnicity (white or other [i.e. South Asian, South East Asian, West Asian, Chinese, Korean, Japanese, Black, Filipino, Latin American, Arab, Inuit, Cree, Meti, Other]), income (0–40 K, 41–80 K, 81 K or more), pregnancy-specific anxiety, and perceived stress. Statistical significance was set at 0.05. Data were analyzed using SPSS version 25 (IBM Corp, 2017).
Results
Participant Characteristics
At study entry, 751 women fully completed the baseline on-line questionnaires and 503 (65.9%) fully completed all three on-line assessments (n = 91 recent immigrant; n = 130 long-term immigrant, n = 282 Canadian-born) (See Table 1 in Supplementary material for characteristics of participants missing and not missing data). No significant differences were found between participants with complete and incomplete data for parity, language spoken, marital status, education, working status, pregnancy intention, food security, pregnancy-specific anxiety, and elevated depression in at least one trimester. Participants with incomplete data were younger (32.5 (SD = 4.45) vs 33.21 (SD = 4.24), p = 0.035), more likely to be nonwhite (46.5% vs 63.4%, X2 = 20.01, p < 0.001), more likely to be in the lowest income level and less likely to be in the highest income level (25.0% vs 16.9%, X2 = 7.12, p = 0.008 and 45.8% vs 56.3%, X2 = 7.57, p = 0.006, respectively), less likely to have consulted a professional for emotional difficulties (20.5% vs 28.0%, X2 = 5.08, p = 0.024), and reported higher perceived stress (16.26 (SD = 6.59) vs 15.24 (SD = 5.96), p = 0.033) than participants with complete data. The following analyses were conducted using the subset of participants who completed all three assessments.
Table 1 shows participant characteristics of the final sample. Significantly more Canadian-born women (80.1%) were of white ethnicity compared to both recent (44.7%; X2 = 44.04, p < 0.001) and long-term (41.1%; X2 = 63.10; p < 0.001) immigrants. Significantly more Canadian-born women (80.1% vs 52.7%; X2 = 26.48; p < 0.001) and long-term immigrants (73.1% vs 52.7%; X2 = 9.69; p = 0.002) reported being employed at baseline compared to recent immigrants. Recent immigrant women were significantly more likely to be in the lowest income level (< $40,000) than long-term immigrants (37.2% vs 16.5%; X2 = 12.54; p < 0.001) and Canadian-born women (38.5% vs 9.9%; X2 = 39.90; p < 0.001). Long-term immigrants were also significantly more likely to be in the lowest income level compared to Canadian-born women (16.9% vs 9.9%; X2 = 4.08; p = 0.043). Concerning the highest level of income (> $81,000), long-term immigrants (53.1% vs 30.8%; X2 = 10.82, p = 0.001) and Canadian-born women (66.0% vs 30.8%; X2 = 34.83, p < 0.001) were significantly more likely to be in this group compared to recent immigrants. Canadian-born women were also significantly more likely to be in the higher income level than long-term immigrants (66.0% vs 53.1%; X2 = 6.26, p = 0.012). Significantly more recent immigrants (11% vs 4.3%; X2 = 5.62; p = 0.018) reported food insecurity at baseline compared to Canadian-born women. Canadian-born women (35.1%) were significantly more likely to have consulted a health professional for emotional difficulties compared to both recent (15.4%; X2 = 12.67, p < 0.001) and long-term (21.5%; X2 = 7.68; p = 0.006) immigrants. No significant group differences were found for age, parity, marital status, or education.
A one-way ANOVA showed a significant difference in scores for pregnancy-specific anxiety during the first trimester (F (2, 500) = 4.17; p = 0.016), with recent immigrant women reporting significantly more pregnancy-specific anxiety than Canadian-born women (p = 0.013).
The prevalence of depressive symptoms defined as an EPDS score ≥ 12 was highest for recent immigrant (25.3–30.8%) compared long-term immigrant (16.9%–19.2%) and Canadian-born women (11.7–13.8%). Recent immigrant women reported significantly more clinical levels of depressive symptoms than Canadian-born women during the first (25.3% vs 12.8%; X2 = 8.08; p = 0.004), second (25.3% vs 11.7%; X2 = 9.93; p = 0.002), and third (30.8% vs 13.8%; X2 = 13.40; p < 0.001) trimester. A significantly greater proportion of recent immigrant women reported elevated depressive symptoms during the third trimester compared to long term immigrants (30.8% vs 16.9%; X2 = 5.86; p = 0.015).
First Trimester Risk Factors for Elevated Depressive Symptoms for each Immigrant Group
Three logistic regression models were computed to identify first trimester risk factors for elevated antenatal depressive symptoms for each group. The results are presented in Table 2.
Among recent immigrants, the final model significantly predicted depressive symptom status, correctly identifying 79.1% of cases. Among recent immigrants, multiparity, higher pregnancy-specific anxiety and perceived stress in early pregnancy increased the risk of depressive symptoms during pregnancy (R2 = 0.39 (Cox & Snell), χ2(10) = 44.51, p < 0.001). More specifically, a one-unit increase in PDQ-R and PSS total score in the first trimester of pregnancy was associated with a 19% (OR 1.19, 95% CI [1.06, 1.33] and 26% (OR 1.26, 95% CI [1,08, 1.47]) greater odds, respectively of clinical depressive symptoms.
Among long-term immigrants, the final model significantly predicted depressive symptom status, correctly identifying 84.6% of cases. Among long-term immigrant women, perceived stress in the first trimester was significantly associated with depressive symptoms during pregnancy (R2 = 0.29 (Cox & Snell), χ2(10) = 43.72, p < 0.001). A one-unit increase in PSS total score in the first trimester of pregnancy was associated with 16% greater odds of clinical depressive symptoms (OR 1.16, 95% CI [1.06, 1.27]).
Among Canadian-born women, the final model significantly predicted depressive symptom status, correctly identifying 83% of cases. Among Canadian-born women, ethnicity (non-white), higher pregnancy-specific anxiety and perceived stress in the first trimester was significantly associated with depressive symptoms during pregnancy (R2 = 0.30 (Cox & Snell), χ2(10) = 99.20, p < 0.001). A one-unit increase in PDQ-R and PSS total score in the first trimester of pregnancy was associated with an 8% (OR 1.08, 95% CI [1.01, 1.17] and 29% (OR 1.29, 95% CI [1.19, 1.40]) greater odds of clinical depressive symptoms. Food insecurity, education, pregnancy intention and income were not significant independent predictors of depressive symptoms in any of the regression models.
Discussion
We sought to determine the prevalence and early determinants of depression during pregnancy among recent and long-term immigrant women, compared to Canadian-born women. The prevalence of depression was found to be particularly elevated throughout pregnancy among recent immigrant women compared to their Canadian-born counterparts. Our findings point to unique and common factors associated to depressive symptoms in immigrant and Canadian-born women.
As expected, recent immigrant women were more likely to report clinically elevated symptoms of depression during pregnancy compared to Canadian-born women throughout every trimester. The prevalence of depressive symptoms among our immigrant groups are similar to estimates that have previously been reported in studies examining antenatal depressive symptoms in this population with self-report measures (16.5–30.1% vs 12%–45% respectively [3]). Furthermore, the greater prevalence of depressive symptoms during pregnancy among immigrant women compared to their Canadian counterparts has similarly been found in a Canadian study by Miszkurka et al. [22]. While we only found significant differences in the prevalence of depressive symptoms for recent immigrant women when comparing to Canadian-born women, Miszkurka et al. [22] reported a higher prevalence of antenatal depressive symptoms regardless of time since immigration. However, in the latter study women were assessed for depression only in mid-pregnancy, and with the Center for Epidemiologic Studies Depression Scale which has not been validated for use among pregnant women.
While certain sociodemographic factors previously identified as predictors of antenatal depression, such as lower income, lower educational attainment, unintended pregnancy, and food insecurity, were not related to antenatal depressive symptoms in our study, modifiable psychosocial risk factors including perceived stress and pregnancy-specific anxiety were significant predictors among all women despite migrant status. These results are similar to previous findings in studies of risk factors for antenatal depression in both immigrant and non-migrant populations [23,24,25,26]. While general anxiety has previously been identified as a risk factor for antenatal depression in non-immigrant populations [18, 25], our study is the first to our knowledge to examine pregnancy-specific anxiety as a risk factor for antenatal depression among immigrant women.
In another Canadian study, similar demographic factors (education and occupational status) were not related to depressive symptoms during pregnancy among immigrant women, while psychosocial risk factors (i.e. stressful life events, lack of social support and unsatisfactory marital relations) were found to be predictive of antenatal depression [26]. Social support may be a key confounding factor that may explain the lack of association between demographic factors and depressive symptoms during pregnancy in our study. Poor social support [69, 70] and disadvantaged socioeconomic position [19, 30, 71] are both important determinants of perinatal mental health. Some evidence suggests that social support may be a protective factor against maternal distress related to lower socioeconomic position and food insecurity during pregnancy [72, 73]. Given the high levels of educational attainment and income reported in the women from our sample, it is possible that the participants had access to instrumental support that was not measured and accounted for.
The impact of pregnancy-specific anxiety and stress may be mediated by poor social support among immigrant women, particularly among women who have recently immigrated and have not had the time to rebuild an extensive social network. In women’s country of origin, the support of family and friends during the perinatal period may be culturally expected and valued [74,75,76]. While we did not have data on social support, other studies with immigrant women have identified poor social support as a risk factor for antenatal depression [21, 23, 24, 26]. A study by Zelkowitz et al. [26], identified smaller social networks and lower satisfaction with social support among immigrant women with greater PPD. In our study, a significantly greater proportion of recent immigrant women reported elevated depressive symptoms during the third trimester compared to long term immigrants. Similarly, some studies have suggested a mediating effect of marital adjustment and social support on the relationship between stress or stressful life events and antenatal depressive symptoms among immigrant women [26, 77, 78]. Future investigations should include measures of social support and couple adjustment in order to confirm the impact of these social factors on sociodemographic and psychological risk factors for antenatal depression.
Most of the women in the recent immigrant group reported many potential risk factors of distress including not working at baseline and lower income. This differentiates this group of women to the long-term immigrant and Canadian-born women. While we controlled for income level and working status, it is possible that these factors had a cumulative effect as we do not know whether they also had these factors prior to their move to Canada.
Our study has several strengths, including the ethnic diversity in our sample of women. Another strength is the prospective design, which allows for examination of determinants of antenatal depressive symptoms over time during the pregnancy. While most studies have examined antenatal depression only in the third trimester of pregnancy [18, 35], we included measures of distress throughout pregnancy. Importantly, this study expands our understanding of risk factors that place immigrant women at a higher risk for depressive symptoms during pregnancy. These findings highlight the importance considering modifiable psychological risk factors for the development of depressive symptoms such as perceived stress and pregnancy-specific anxiety.
Our study has limitations, including the use of convenience sampling, which may result in selection bias. Moreover, participants had generally greater educational attainment and higher income relative to the Canadian population. In particular, our Canadian-born group was comprised of primarily White and highly educated women. These factors limit the generalizability of results to all pregnant women in Canada. While approximately 16% of families in Canada are led by lone-mothers [79], this group of women are under-represented in this sample as only 6% reported being single or not cohabitating with a partner. Therefore, the results may not be generalizable to this population of women giving birth. Women who were not fluent in either English or French, which may include very recent immigrant women or women with low levels of acculturation [80], were not represented in this sample. However, according to data from the 2016 Census of the Canadian population, the proportion of immigrants with knowledge of at least one of Canada’s official languages is very high (93.2%) [81]. Previous investigations have reported a higher prevalence of mental disorders and symptoms among immigrant women with low host country language ability during the perinatal period compared to immigrant women who do not lack this ability [3, 82, 83]. The elimination of a language barrier as stressor in our study may have a protective effect and we could expect even greater rates of PPD among women with language barriers. Compared to participants with complete data, participants with missing data reported significant differences on certain variables that could be related with greater symptoms of depression (i.e. younger age, nonwhite ethnicity, lower income, higher perceived stress). However, the regression controlled for these variables within the model. Furthermore, symptoms of depression were measured by self-report questionnaires, rather than clinical interviews. However, the relevance of psychological distress symptoms to wellbeing for mothers and their infants has been shown in individuals meeting clinically significant cut-offs on self-report questionnaires [84,85,86,87]. The use of self-report questionnaires for data collection may also limit the reliability of participant responses due to the social desirability biases implicated in self-report measures. A history of mental illness has previously been identified as a risk factor for antenatal depression in the general population [88]. We did not inquire about whether depressive symptoms were present prior to pregnancy, therefore we cannot determine whether symptoms may have been a continuation, exacerbation, or whether it was a new onset. However, we included participants history of consulting a health professional for emotional difficulties as a covariate. Other factors that may influence mental health and help-seeking behaviours such as culturally based stigma towards mental illness, low social support, and poor marital adjustment were not assessed. Given these limitations, we cannot suggest that immigration is the cause of a greater level of depression. However, since there have been few studies examining associated factors of antenatal depression in immigrant women, this data provides an important basis for future studies.
Clinical implications and Conclusions
The high prevalence of depressive symptoms in pregnancy underline the need for a greater access to screening and follow-up of women’s mental health during pregnancy. Enduring depressive symptoms may negatively impact both the relationship with the partner and infant. Given the growing size of the immigrant population in Canada and this group’s vulnerability to greater psychological distress during pregnancy, greater attention to the modifiable risk factors associated with antenatal depression in this population is important. The implications of pregnancy-specific anxiety and stress as modifiable risk factors for the development of antenatal depression may help to improve antenatal screening and inform the development of tailored interventions to better meet the mental health needs of immigrant women during the perinatal period.
Some research in the US has demonstrated the efficacy of using culturally and linguistically tailored psychotherapy (e.g. IPT and CBT) [89,90,91], or a healthy lifestyle intervention (that is community-planned, and culturally and linguistically tailored) [92] to treat symptoms of antenatal depression in immigrant women. However, Canadian data has recognized the underutilization of mental health services in both perinatal and non-perinatal immigrants compared to Canadian-born populations due to their unfamiliarity with the health system, systemic discrimination, language barriers, financial barriers, lack of culturally tailored therapies, lack of awareness about mental ill health, and cultural beliefs or preferences, such as significant stigma and shame towards mental illness [4, 5, 93,94,95,96,97]. A recent study, using data from the Canadian Community Health Survey, reported a significantly lower likelihood for recent and long-term immigrants to consult a health professional for emotional difficulties compared to Canadian-born women [98]. Psychological interventions can be delivered in the context of antenatal and maternity care by healthcare providers [99], which may improve accessibility. Previous evidence has shown that the integration of mental health and primary care services have been successful in immigrant populations [100]. Collaborating with community services to provide psychoeducation on mental health that is acceptable to community members and tapping into religious organizations as a resource for social support could be valuable sectors of intervention among immigrants [101]. However, much research has suggested the need for the further development and delivery of mental health services in immigrant populations [102].
The results of this study provide further evidence that women are at risk for antenatal depression, particularly recent immigrant women. Given that immigrant women are less likely to seek help for mental health issues due to various social barriers, there is a need to target women at risk by providing culturally tailored support resources and follow-ups during the perinatal period.
References
Tobin CL, Di Napoli P, Beck CT. Refugee and immigrant women’s experience of postpartum depression: a meta-synthesis. J Transcult Nurs. 2018;29(1):84–100.
Jayaweera H, Quigley MA. Health status, health behaviour and healthcare use among migrants in the UK: evidence from mothers in the Millennium Cohort Study. Soc Sci Med. 2010;71(5):1002–10.
Anderson FM, Hatch SL, Comacchio C, Howard LM. Prevalence and risk of mental disorders in the perinatal period among migrant women: a systematic review and meta-analysis. Arch Womens Ment Health. 2017;20(3):449–62.
Higginbottom GM, Hadziabdic E, Yohani S, Paton P. Immigrant women’s experience of maternity services in Canada: a meta-ethnography. Midwifery. 2014;30(5):544–59.
Higginbottom GM, Morgan M, Alexandre M, Chiu Y, Forgeron J, Kocay D, et al. Immigrant women’s experiences of maternity-care services in Canada: a systematic review using a narrative synthesis. Syst Rev. 2015;4:13.
Falah-Hassani K, Shiri R, Vigod S, Dennis C-L. Prevalence of postpartum depression among immigrant women: a systematic review and meta-analysis. J Psychiatr Res. 2015;70:67–82.
Dennis CL, Merry L, Stewart D, Gagnon AJ. Prevalence, continuation, and identification of postpartum depressive symptomatology among refugee, asylum-seeking, non-refugee immigrant, and Canadian-born women: results from a prospective cohort study. Arch Womens Ment Health. 2016;19(6):959–67.
Dennis CL, Merry L, Gagnon AJ. Postpartum depression risk factors among recent refugee, asylum-seeking, non-refugee immigrant, and Canadian-born women: results from a prospective cohort study. Soc Psychiatry Psychiatr Epidemiol. 2017;52(4):411–22.
Mechakra-Tahiri S, Zunzunegui MV, Seguin L. Self-rated health and postnatal depressive symptoms among immigrant mothers in Québec. Women Health. 2007;45(4):1–17.
Stewart DE, Gagnon A, Saucier JF, Wahoush O, Dougherty G. Postpartum depression symptoms in newcomers. Can J Psychiatry. 2008;53(2):121–4.
Sword W, Watt S, Krueger P. Postpartum health, service needs, and access to care experiences of immigrant and Canadian-born women. J Obstetr Gynecol Neonatal Nurs. 2006;35(6):717–27.
Zelkowitz P, Saucier JF, Wang T, Katofsky L, Valenzuela M, Westreich R. Stability and change in depressive symptoms from pregnancy to two months postpartum in childbearing immigrant women. Arch Womens Ment Health. 2008;11(1):1–11.
Ganann R, Sword W, Thabane L, Newbold B, Black M. Predictors of postpartum depression among immigrant women in the year after childbirth. J Womens HEALTH. 2016;25(2):155–65.
Alhasanat D, Fry-McComish J. Postpartum depression among immigrant and Arabic women: literature review. J Immigr Minor Health. 2015;17(6):1882–94.
World Health Organization, United Nations Population Fund. Mental health aspects of women's reproductive health: a global review of the literature. Geneva: World Health Organization; 2009.
Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol. 2005;106(5 Pt 1):1071–83.
Underwood L, Waldie K, D’Souza S, Peterson ER, Morton S. A review of longitudinal studies on antenatal and postnatal depression. Arch Womens Ment Health. 2016;19(5):711–20.
Underwood L, Waldie KE, D’Souza S, Peterson ER, Morton SM. A Longitudinal Study of Pre-pregnancy and Pregnancy Risk Factors Associated with Antenatal and Postnatal Symptoms of Depression: Evidence from Growing Up in New Zealand. Matern Child Health J. 2017;21(4):915–31.
Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen Hosp Psychiatry. 2004;26(4):289–95.
Verreault N, Da Costa D, Marchand A, Ireland K, Dritsa M, Khalifé S. Rates and risk factors associated with depressive symptoms during pregnancy and with postpartum onset. Journal of psychosomomatic obstetrics & gynaecology. 2014;35(3):84–91.
Diaz MA, Le HN, Cooper BA, Muñoz RF. Interpersonal factors and perinatal depressive symptomatology in a low-income Latina sample. Cultur Divers Ethnic Minor Psychol. 2007;13(4):328–36.
Miszkurka M, Goulet L, Zunzunegui MV. Contributions of immigration to depressive symptoms among pregnant women in Canada. Can J Public Health. 2010;101(5):358–64.
Shin H, Shin Y. Life Stress, Social Support, and Antepartum Depression among Married Immigrant Women from Southeast Asia. J Korean Acad Community Health Nurs. 2015;26:108.
Small R, Lumley J, Yelland J. Cross-cultural experiences of maternal depression: associations and contributing factors for Vietnamese, Turkish and Filipino immigrant women in Victoria. Australia Ethnicity & health. 2003;8(3):189–206.
Truijens SEM, Spek V, van Son MJM, Guid Oei S, Pop VJM. Different patterns of depressive symptoms during pregnancy. Arch Womens Ment Health. 2017;20(4):539–46.
Zelkowitz P, Schinazi J, Katofsky L, Saucier JF, Valenzuela M, Westreich R, et al. Factors associated with depression in pregnant immigrant women. Transcult Psychiatry. 2004;41(4):445–64.
Rwakarema M, Premji SS, Nyanza EC, Riziki P, Palacios-Derflingher L. Antenatal depression is associated with pregnancy-related anxiety, partner relations, and wealth in women in Northern Tanzania: a cross-sectional study. BMC Womens health. 2015;15:68.
Bekele D, Worku A, Wondimagegn D. Prevalence and associated factors of mental distress during pregnancy among antenatal care attendees at Saint Paul’s Hospital. Addis Ababa Obstetr Gynecol Int J. 2017;7:00269.
Marcus SM, Flynn HA, Blow FC, Barry KL. Depressive symptoms among pregnant women screened in obstetrics settings. J Womens Health. 2003;12(4):373–80.
Lancaster CA, Gold KJ, Flynn HA, Yoo H, Marcus SM, Davis MM. Risk factors for depressive symptoms during pregnancy: a systematic review. Am J Obstet Gynecol. 2010;202(1):5–14.
Rubertsson C, WaldenstrÖm U, Wickberg B, Rådestad I, Hildingsson I. Depressive mood in early pregnancy and postpartum: prevalence and women at risk in a national Swedish sample. J Reprod Infant Psychol. 2005;23(2):155–66.
Rubertsson C, Wickberg B, Gustavsson P, Rådestad I. Depressive symptoms in early pregnancy, two months and one year postpartum-prevalence and psychosocial risk factors in a national Swedish sample. Arch Womens Ment Health. 2005;8(2):97–104.
Augusto ALP, de Abreu Rodrigues AV, Domingos TB, Salles-Costa R. Household food insecurity associated with gestacional and neonatal outcomes: a systematic review. BMC Pregnancy Childbirth. 2020;20:1–11.
Richards M, Weigel M, Li M, Rosenberg M, Ludema C. Household food insecurity and antepartum depression in the National Children’s Study. Ann Epidemiol. 2020;44:38–44.
Waldie KE, Peterson ER, D’Souza S, Underwood L, Pryor JE, Carr PA, et al. Depression symptoms during pregnancy: evidence from growing up in New Zealand. J Affect Disord. 2015;186:66–73.
Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–6.
Murray D, Cox JL. Screening for depression during pregnancy with the Edinburgh Depression Scale (EDDS). J Reprod Infant Psychol. 1990;8(2):99–107.
Murray L, Carothers AD. The validation of the Edinburgh Post-natal Depression Scale on a community sample. Br J Psychiatry. 1990;157:288–90.
O’Connor E, Rossom RC, Henninger M, Groom HC, Burda BU. Primary care screening for and treatment of depression in pregnant and postpartum women: evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2016;315(4):388–406.
Gibson J, McKenzie-McHarg K, Shakespeare J, Price J, Gray R. A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatr Scand. 2009;119(5):350–64.
Adewuya AO, Ola BA, Dada AO, Fasoto OO. Validation of the Edinburgh Postnatal Depression Scale as a screening tool for depression in late pregnancy among Nigerian women. J Psychosom Obstet Gynecol. 2006;27(4):267–72.
Eberhard-Gran M, Eskild A, Tambs K, Opjordsmoen S, Ove SS. Review of validation studies of the Edinburgh Postnatal Depression Scale. Acta Psychiatr Scand. 2001;104(4):243–9.
Carpiniello B, Pariante C, Serri F, Costa G, Carta M. Validation of the Edinburgh postnatal depression scale in Italy. J Psychosom Obstet Gynecol. 1997;18(4):280–5.
Hewitt CE, Gilbody SM, Mann R, Brealey S. Instruments to identify post-natal depression: which methods have been the most extensively validated, in what setting and in which language? Int J Psychiatry Clin Pract. 2010;14(1):72–6.
Yali AM, Lobel M. Coping and distress in pregnancy: an investigation of medically high risk women. J Psychosom Obstetr Gynaecol. 1999;20(1):39–52.
Lobel M, Cannella DL, Graham JE, DeVincent C, Schneider J, Meyer BA. Pregnancy-specific stress, prenatal health behaviors, and birth outcomes. Health Psychol. 2008;27(5):604–15.
Caparros-Gonzalez RA, Perra O, Alderdice F, Lynn F, Lobel M, García-García I, et al. Psychometric validation of the Prenatal Distress Questionnaire (PDQ) in pregnant women in Spain. Women Health. 2019;59(8):937–52.
Penengo C, Colli C, Garzitto M, Driul L, Cesco M, Balestrieri M. Validation of the Italian version of the Revised Prenatal Coping Inventory (NuPCI) and its correlations with pregnancy-specific stress. BMC Pregnancy Childbirth. 2020;20(1):1–14.
Yuksel F, Akin S, Durna Z. The Turkish adaptation of the" Revised Prenatal Distress Questionnaire": a reliability/validity and factor analysis study/" Prenatal Distres Olcegi" nin Turkce’ye uyarlanmasi ve faktor analizi. J Educ Res Nursing. 2011;8(3):43–52.
Esfandiari M, Faramarzi M, Gholinia H, Omidvar S, Nasiri-Amiri F, Abdollahi S. Psychometric properties and factor structure of the Persian version of revised prenatal distress questionnaire in second and third trimesters. Iran J Nurs Midwifery Res. 2020;25(5):431.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–96.
Cohen S, Williamson G, editors. Psychological stress in a probability sample of the United States. Newbury Park, CA: Sage Publications, Inc; 1988.
Eskildsen A, Dalgaard VL, Nielsen KJ, Andersen JH, Zachariae R, Olsen LR, et al. Cross-cultural adaptation and validation of the Danish consensus version of the 10-item Perceived Stress Scale. Scand J Work Environ Health. 2015;41:486–90.
Andreou E, Alexopoulos EC, Lionis C, Varvogli L, Gnardellis C, Chrousos GP, et al. Perceived stress scale: reliability and validity study in Greece. Int J Environ Res Public Health. 2011;8(8):3287–98.
Baik SH, Fox RS, Mills SD, Roesch SC, Sadler GR, Klonoff EA, et al. Reliability and validity of the Perceived Stress Scale-10 in Hispanic Americans with English or Spanish language preference. J Health Psychol. 2019;24(5):628–39.
Lee J, Shin C, Ko Y-H, Lim J, Joe S-H, Kim S, et al. The reliability and validity studies of the Korean version of the Perceived Stress Scale. Korean J Psychosomat Med. 2012;20(2):127–34.
Huang F, Wang H, Wang Z, Zhang J, Du W, Su C, et al. Psychometric properties of the perceived stress scale in a community sample of Chinese. BMC Psychiatry. 2020;20(1):1–7.
Lesage F-X, Berjot S, Deschamps F. Psychometric properties of the French versions of the Perceived Stress Scale. Int J Occup Med Environ Health. 2012;25(2):178–84.
Mimura C, Griffiths P. A Japanese version of the Perceived Stress Scale: cross-cultural translation and equivalence assessment. BMC Psychiatry. 2008;8(1):1–7.
Nordin M, Nordin S. Psychometric evaluation and normative data of the Swedish version of the 10-item perceived stress scale. Scand J Psychol. 2013;54(6):502–7.
Chaaya M, Osman H, Naassan G, Mahfoud Z. Validation of the Arabic version of the Cohen Perceived Stress Scale (PSS-10) among pregnant and postpartum women. BMC Psychiatry. 2010;10(1):1–7.
Jovanović V, Gavrilov-Jerković V. More than a (negative) feeling: validity of the Perceived Stress Scale in Serbian clinical and non-clinical samples. Psihologija. 2015;48(1):5–18.
Klein EM, Brähler E, Dreier M, Reinecke L, Müller KW, Schmutzer G, et al. The German version of the Perceived Stress Scale–psychometric characteristics in a representative German community sample. BMC Psychiatry. 2016;16(1):1–10.
Dao-Tran T-H, Anderson D, Seib C. The Vietnamese version of the Perceived Stress Scale (PSS-10): translation equivalence and psychometric properties among older women. BMC Psychiatry. 2017;17(1):1–7.
Siqueira RR, Ferreira HAA, Romélio RAC. Perceived stress scale: reliability and validity study in Brazil. J Health Psychol. 2010;15(1):107–14.
Wongpakaran N, Wongpakaran T. The Thai version of the PSS-10: an investigation of its psychometric properties. BioPsychoSocial Med. 2010;4(1):1–6.
Remor E. Psychometric properties of a European Spanish version of the Perceived Stress Scale (PSS). Span J Psychol. 2006;9(1):86.
Örücü MÇ, Demir A. Psychometric evaluation of perceived stress scale for Turkish university students. Stress Health. 2009;25(1):103–9.
Milgrom J, Hirshler Y, Reece J, Holt C, Gemmill AW. Social support—a protective factor for depressed perinatal women? Int J Environ Res Public Health. 2019;16(8):1426.
Saad M. Examining the social patterning of postpartum depression by immigration status in Canada: an exploratory review of the literature. J Racial Ethn Health Disparities. 2019;6(2):312–8.
Goyal D, Gay C, Lee KA. How much does low socioeconomic status increase the risk of prenatal and postpartum depressive symptoms in first-time mothers? Womens Health Issues. 2010;20(2):96–104.
Nakamura A, Lesueur FE-K, Sutter-Dallay A-L, Franck J-È, Thierry X, Melchior M, et al. The role of prenatal social support in social inequalities with regard to maternal postpartum depression according to migrant status. J Affect Disorders. 2020;272:465–73.
Quintanilha M, Mayan MJ, Thompson J, Bell RC. Contrasting “back home” and “here”: how Northeast African migrant women perceive and experience health during pregnancy and postpartum in Canada. Int J Equity Health. 2016;15(1):1–8.
Landale NS, Oropesa RS. Migration, social support and perinatal health: an origin-destination analysis of Puerto Rican women. J Health Soc Behav. 2001;42(2):166–83.
Martinez-Schallmoser L, MacMullen NJ, Telleen S. Social support in Mexican American childbearing women. J Obstetr Gynecol Neonatal Nurs. 2005;34(6):755–60.
Martinez-Schallmoser L, Telleen S, MacMullen NJ. The effect of social support and acculturation on postpartum depression in Mexican American women. J Transcult Nurs. 2003;14(4):329–38.
Coburn SS, Gonzales NA, Luecken LJ, Crnic KA. Multiple domains of stress predict postpartum depressive symptoms in low-income Mexican American women: the moderating effect of social support. Arch Womens Ment Health. 2016;19(6):1009–18.
Glazier RH, Elgar FJ, Goel V, Holzapfel S. Stress, social support, and emotional distress in a community sample of pregnant women. J Psychosom Obstetr Gynecol. 2004;25(3–4):247–55.
Statistics Canada. Labour Force Survey. 2014.
Maria-da-Conceição FS, Figueiredo MH. Immigrant women’s perspective on prenatal and postpartum care: systematic review. J Immigr Minor Health. 2015;17(1):276–84.
Statistics Canada. Census in Brief: Linguistic integration of immigrants and official language populations in Canada. 2017.
Chen HH, Hwang FM, Wang KL, Chen CJ, Lai JCY, Chien LY. A structural model of the influence of immigrant mothers’ depressive symptoms and home environment on their children’s early developmental outcomes in Taiwan. Res Nurs Health. 2013;36(6):603–11.
Zelkowitz P, Tamara HM. Screening for post-partum depression in a community sample. Can J Psychiatry. 1995;40(2):80–6.
Cheng C-Y, Fowles ER, Walker LO. Postpartum maternal health care in the United States: a critical review. J Perinat Educ. 2006;15(3):34.
Kingston D, Tough S, Whitfield H. Prenatal and postpartum maternal psychological distress and infant development: a systematic review. Child Psychiatry Hum Dev. 2012;43(5):683–714.
Staneva A, Bogossian F, Pritchard M, Wittkowski A. The effects of maternal depression, anxiety, and perceived stress during pregnancy on preterm birth: a systematic review. Women Birth. 2015;28(3):179–93.
Wisner KL, Sit DK, McShea MC, Rizzo DM, Zoretich RA, Hughes CL, et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiat. 2013;70(5):490–8.
Freeman MP. Perinatal depression: recommendations for prevention and the challenges of implementation. JAMA. 2019;321(6):550–2.
Spinelli MG, Endicott J. Controlled clinical trial of interpersonal psychotherapy versus parenting education program for depressed pregnant women. Am J Psychiatry. 2003;160(3):555–62.
Muñoz RF, Le H-N, Ippen CG, Diaz MA, Urizar GG Jr, Soto J, et al. Prevention of postpartum depression in low-income women: Development of the Mamás y Bebés/Mothers and Babies Course. Cogn Behav Pract. 2007;14(1):70–83.
Le H-N, Perry DF, Stuart EA. Randomized controlled trial of a preventive intervention for perinatal depression in high-risk Latinas. J Consult Clin Psychol. 2011;79(2):135.
Kieffer EC, Caldwell CH, Welmerink DB, Welch KB, Sinco BR, Guzmán JR. Effect of the healthy MOMs lifestyle intervention on reducing depressive symptoms among pregnant Latinas. Am J Community Psychol. 2013;51(1):76–89.
Kirmayer LJ, Weinfeld M, Burgos G, du Fort GG, Lasry J-C, Young A. Use of health care services for psychological distress by immigrants in an urban multicultural milieu. Can J Psychiatry. 2007;52(5):295–304.
Whitley R, Kirmayer LJ, Groleau D. Understanding immigrants’ reluctance to use mental health services: a qualitative study from Montreal. Can J Psychiatry. 2006;51(4):205–9.
Tiwari SK, Wang J. Ethnic differences in mental health service use among White, Chinese, South Asian and South East Asian populations living in Canada. Soc Psychiatry Psychiatr Epidemiol. 2008;43(11):866.
Merry LA, Gagnon AJ, Kalim N, Bouris SS. Refugee claimant women and barriers to health and social services post-birth. Can J Public Health. 2011;102(4):286–90.
Ahmed A, Bowen A, Feng CX. Maternal depression in Syrian refugee women recently moved to Canada: a preliminary study. BMC Pregnancy Childbirth. 2017;17(1):1–11.
Nwoke CN, Okpalauwaekwe U, Bwala H. Mental health professional consultations and the prevalence of mood and anxiety disorders among immigrants: multilevel analysis of the Canadian community health survey. JMIR Mental Health. 2020;7(9):e19168.
Matvienko-Sikar K, Flannery C, Redsell S, Hayes C, Kearney PM, Huizink A. Effects of interventions for women and their partners to reduce or prevent stress and anxiety: a systematic review. Women and Birth. 2020;34(2): e97–e117.
Giacco D, Matanov A, Priebe S. Providing mental healthcare to immigrants: current challenges and new strategies. Curr Opin Psychiatry. 2014;27(4):282–8.
Guruge S, Thomson MS, George U, Chaze F. Social support, social conflict, and immigrant women’s mental health in a Canadian context: a scoping review. J Psychiatr Ment Health Nurs. 2015;22(9):655–67.
Thomson MS, Chaze F, George U, Guruge S. Improving immigrant populations’ access to mental health services in Canada: a review of barriers and recommendations. J Immigr Minor Health. 2015;17(6):1895–905.
Acknowledgements
This research was supported by a grant awarded to Dr Deborah Da Costa by the Canadian Institutes of Health Research (CIHR; #299916).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest.
Ethics Approval
Ethics approval was granted by McGill Faculty of Medicine Institutional Review Board and the ethics review boards of the participating hospitals. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vaillancourt, M., Lane, V., Ditto, B. et al. Parity and Psychosocial Risk Factors Increase the Risk of Depression During Pregnancy Among Recent Immigrant Women in Canada. J Immigrant Minority Health 24, 570–579 (2022). https://doi.org/10.1007/s10903-021-01284-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-021-01284-7