Abstract
Objectives Antenatal and postnatal depression can lead to poor outcomes for women and their children. The aim of this study was to explore whether risk factors differ for depression symptoms that are present during pregnancy and/or after childbirth. Methods An ethnically and socioeconomically diverse sample of 5301 women completed interviews during the third trimester of pregnancy and 9 months after childbirth. Depression symptoms were measured using the Edinburgh Postnatal Depression Scale (EPDS). Depression symptoms (defined as EPDS >12) among participants and associations with pre-pregnancy and pregnancy maternal characteristics were explored using logistic regression. Results The rate of antenatal depression symptoms (ADS) only was 8.5, 5% of women had depression symptoms at 9 months postpartum (PDS) only and 3% experienced depression symptoms at both time points. Perceived stress and Pacific or Asian ethnicity were risk factors for ADS and PDS. Anxiety during and before pregnancy was a risk factor for ADS only while having a pre-pregnancy diagnosis of depression was a risk factor for PDS only. Having ADS increased the odds ratio of PDS by 1.5 (95% CI 1.01–2.30). Conclusions The results supported evidence from previous longitudinal studies that depression symptoms appear to be higher during pregnancy than in the first year following childbirth. The study found that PDS may often be a continuation or recurrence of ADS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Significance
Few studies have looked at the extent to which factors associated with postnatal depression symptoms (PDS) first impact on risk for antenatal depression symptoms (ADS) (a known predictor of PDS). Our study included a comprehensive range of pre-pregnancy and pregnancy variables. We found that women who experience stress are at risk throughout the perinatal period. Those with a history of depression may be most at risk of developing PDS rather than ADS while those with anxiety may be most at risk of ADS. In our study, Asian and Pacific Island women living in New Zealand were at higher risk of perinatal depression.
Introduction
It is estimated that up to one in five women experience depression at some point in their lives (Kessler et al. 1997). Women are particularly vulnerable to depressive symptoms during pregnancy (ADS) and up to a year after childbirth (PDS). Depression symptoms during these perinatal periods are associated with negative impacts on maternal health, pregnancy outcomes, child health and child development (National Institute for Health and Clinical Excellence 2014). However, the effect of perinatal depression symptoms on women and their children can be reduced if they are identified early, successfully treated or prevented from occurring in the first place (Dennis and Dowswell 2013).
Several meta-analyses have reported the prevalence of ADS among pregnant women and PDS among new mothers (Bennett et al. 2004; Gavin et al. 2005; O’Hara and Swain 1996). They largely included data from cross-sectional studies that assessed women for depression either in pregnancy or during the postnatal period (Hein et al. 2014). As such, we know less about: depression symptoms that persist throughout the perinatal period; women who recover from ADS and do not experience PDS; and women who experience depression symptoms with onset in the postnatal period.
Previous longitudinal studies with samples up to over 8000 women have reported ADS rates ranging from 7 to 25% and PDS rates from 6 to 20% (see Underwood et al. 2016). Most of these studies report lower rates of depression during the postnatal period, compared with during pregnancy, with 13–54% of women with depression during pregnancy going on to experience postnatal depression. Understanding which groups of women are more likely to experience perinatal depression symptoms and improving recognition are crucial for timely and effective prevention/intervention. Significant risk factors for ADS found by reviews of the evidence are shown in Fig. 1 (see Beck 2001; Lancaster et al. 2010; O’Hara and Swain 1996; Robertson et al. 2004; Schmied et al. 2013).
Figure 1 shows the overlap of identified risk factors for depression symptoms in each perinatal period. Many risk factors for PDS are present during or before pregnancy (Beck 2001; Robertson et al. 2004). A recent systematic review supported the view that the phenomenology of and risk factors for ADS and PDS are similar to those for non-perinatal depression (Howard et al. 2014). Specifically, the risk factors that were characterised as ‘strong’ for ADS were (1) social: domestic violence; absence of social or relationship support; intention to get pregnant; and (2) psychological: prior history of psychopathology. Risks that were characterised as ‘strong’ for PDS included (1) social: Domestic violence; low socio-economic status; (2) psychological: neuroticism; substance misuse; and (3) biological: increased parity; multiple births; chronic illness or medical illness (Howard et al. 2014). This mainly cross-sectional evidence does not clarify the extent to which risk factors differ for each period. Nor does it provide evidence on risk factors associated with chronic or recurring depression symptoms. There is some existing evidence that different groups have different risk factors depending on the onset of their symptoms (Sidebottom et al. 2014). However, longitudinal studies that take onset and persistence into account are needed (Banti et al. 2011; Halbreich and Karkun 2006).
As described above, ADS are known to be a significant predictor of PDS. However, Underwood et al. (2016) report that there has been a lack of longitudinal research on how ADS interact with other pre-pregnancy or pregnancy risk factors for PDS (Robertson et al. 2004). This paper builds on our previous report on ADS (Waldie et al. 2015) by exploring the extent to which these factors are associated with PDS and depression symptoms are present both during pregnancy and after childbirth.
The New Zealand Context
The current research was carried out in New Zealand with mothers of babies who were due between April 2009 and March 2010. The New Zealand Public Health and Disability Act (Section 88) requires that midwives assess for the risk of PDS during their postnatal visits up until 6 weeks after the birth (New Zealand Gazette 2007). However, there is no such screening for ADS depression. According to Barber (2009), “There is no coordinated policy in New Zealand that dictates universal screening for perinatal emotional disorders—the new guidelines for primary care come closest, in recommending that caregivers ask about depression (New Zealand Guidelines Group, 2008), but there is no guarantee that any woman will receive this basic screening” (p 34). Internationally, there is a lack of active screening for depression across the perinatal period despite the fact that there are increasing calls for including universal screening as part of best practice (Milgrom and Gemmill 2014) and to increase clinicians awareness of psychosocial risks (Austin et al. 2008).
The current study’s research questions were: (1) What pre-pregnancy and pregnancy factors are associated with the onset and persistence (or recurrence) of depression symptoms during the third trimester of pregnancy and at 9 months after childbirth? (2) To what extent do depression symptoms in pregnancy increase the likelihood of a woman experiencing depression symptoms at 9 months after childbirth once other pre-pregnancy and pregnancy factors are taken into account?
Method
Participants and General Procedure
Participants in this study were drawn from a cohort of women enrolled during pregnancy in Growing Up in New Zealand; a longitudinal, multidisciplinary study designed to explore the determinants of child developmental trajectories (Morton et al. 2015). In brief, the aim of Growing Up in New Zealand was to recruit a child cohort that was broadly generalizable to current New Zealand births (Morton et al. 2012). A broad sampling strategy was used to directly and indirectly approach as many pregnant women as possible who met the inclusion criteria: a due date between 25th April 2009 and 25th March 2010 and living in a specific geographical area covered by three contiguous District Health Board regions (where about 33% of the New Zealand population lives). Recruitment methods included referral by health professionals, visits to antenatal classes and clinic rooms, community events and media publicity. Ethical approval was obtained from the New Zealand Ministry of Health Northern Y Regional Ethics Committee. Written informed consent was obtained from all participating women.
Interviews were carried out during pregnancy for 5664 women who consented to themselves and their child/children taking part in Growing Up in New Zealand. Selected sociodemographic characteristics of these women and the sample used in the analyses are shown in Table 1.
For the antenatal data collection, participants were visited by interviewers at their homes during the third trimester of pregnancy to complete a face-to-face computer-assisted interview. All interviews were carried out in English. Initial data collection waves, in addition to the antenatal interview, were designed to provide timely information about the children in the study and their development (at 9 months, 2 years and 54 months of age). Since the children have been born, data have been simultaneously collected from the cohort’s parents to provide concurrent information on the child’s family/home environment.
Postnatal data collection was carried out 9 months after childbirth using the same method as the antenatal data collection. Participants were included in the longitudinal analyses for this study if (1) they were the biological mother of the child and (2) they provided data during the third trimester of their pregnancy and at 9 months after childbirth. A total of 5301 women were included in the analyses. There were 358 women (6.3% of the antenatal sample) who were lost to follow-up (i.e., they provided data during pregnancy but not 9 months after childbirth). There were no missing data for any of the EDS/EPDS items at either the antenatal or postnatal interview.
Compared with those included, the participants who were excluded from the longitudinal analyses were significantly: younger; more likely to be Māori, Pacific or Asian; less likely to have a degree; more likely to be unemployed during pregnancy; more likely to be in a low socioeconomic group; and less likely to be cohabiting with a partner or married. Nonetheless, participants included in the longitudinal analyses were similar to NZ national birth data in terms of maternal age and were sufficiently ethnically and socioeconomically diverse to allow for meaningful multilevel analyses.
Participants excluded from the longitudinal analyses were significantly more likely to have reached the study criteria for antenatal depression. Thus, the rate of depression during pregnancy in these longitudinal analyses was slightly lower than the prevalence in our previous report (11.9%) (Waldie et al. 2015).
Measures
ADS and PDS were measured using the Edinburgh Postnatal Depression Scale (EPDS) (Cox et al. 1987); a tool that has also been validated for use in pregnancy and is referred to as the Edinburgh Depression Scale (EDS) when used outside of the postnatal period (Cox et al. 1996). The EDS/EPDS has ten items scored 0–3 and a maximum score of 30. Rates of ADS and PDS were calculated using a cut-off of 12/13. Sensitivity/specificity for major depression at this cut-off are estimated to be 0.83/0.90 and 0.80/0.93 in the antenatal and postnatal periods respectively (National Institute for Health and Clinical Excellence 2014). Participants were divided into four groups defined as follows: ADS only (antenatal interview EDS >12 and postnatal interview EPDS ≤12); PDS only (antenatal interview EDS ≤12 and postnatal interview EPDS >12); ADS + PDS (antenatal interview EDS >12 and postnatal interview EPDS >12); and ‘no depression’ (antenatal interview EDS <12 and postnatal interview EPDS <12).
Socio-demographic variables collected by self-report during the antenatal interview included maternal age, workforce participation, relationship status, educational qualifications, socioeconomic status and ethnicity. The latter was defined as the woman’s self-prioritised ethnicity. External prioritisation was carried out (as utilised by Statistics New Zealand 2004) for mothers who identified with more than one ethnicity and did not provide a self-prioritised main ethnicity. New Zealand has six broad ethnic groups: New Zealand European; Māori; Pacific Peoples; Asian; Middle Eastern, Latin American and African (MELAA); and other (Statistics New Zealand 2004). In this study participants identifying as MELAA or other were grouped together as Other ethnicities. The term New Zealand European (the largest ethnic group making up 69% of the population) refers to New Zealanders of European descent. Around 23% of people living in New Zealand were born overseas, with most immigrants coming from the United Kingdom, China, the Pacific Islands, Australia, India, South Africa and Korea. In the Growing Up in New Zealand study, the proportion of mothers born in New Zealand for each ethnic group was: 98% for Māori; 80% for New Zealand European; 47% for Pacific Peoples; 6% for Asian; and 6% for other.
Self-reported health data collected during the antenatal interview included perceived general health before pregnancy using a 5-point Likert scale from excellent to poor from the SF-36 general health questionnaire (Ware et al. 1994); whether participants had a long-term disability and to what extent they experienced nausea during pregnancy. Participants reported their smoking behavior and alcohol consumption before and during pregnancy. Participants were asked whether they had ever at any time in their life had any of the following illnesses diagnosed by a doctor: asthma; anaemia; depression; either heart disease or high blood pressure; diabetes; either anxiety or panic attacks. For each condition participants were asked to choose one of the following options: never; before this pregnancy but not during this pregnancy; before this pregnancy and during this pregnancy; only during this pregnancy. Participants were asked the following questions about before they became pregnant, during the first 3 months of pregnancy and since the first 3 months of pregnancy: how many days per week (0–7) did you do vigorous activity; how long on average did you do this type of activity on these days (<30, 30–60, >60 min). These questions were repeated for moderate activity. For this study, ‘exercise’ was defined as moderate or vigorous activity for at least 30 min on five (or more) days a week (Ministry of Health 2003). Participants reported whether or not their pregnancy was planned and whether they had any previous pregnancies/children.
At the antenatal interview, participants completed the 10-item Perceived Stress Scale (PSS; Cohen et al. 1983). A higher score on the PSS indicates higher levels of perceived stress. Participants’ scores on a 9-item Warmth and Hostility Scale (Melby et al. 1993) and 6-item Conflict scale (Pryor 2004) were summed to produce a composite relationship environment score. A family environment composite score was calculated by summing a 6-item Family Stress scale (specifically developed for the Growing Up in New Zealand study) and six items on informal family support from the Family Support Scale (Dunst et al. 1984). An external environment score was calculated by summing a 10-item Neighbourhood Integration scale (Turrell et al. 2006) and six items on external support from the Family Support Scale (Dunst et al. 1984). Higher scores on the relationship, family and external environment scores indicate a better environment.
Data Analysis
Chi square/t test analyses were used to determine univariable associations between ADS/PDS and categorical/continuous variables. A broad range of variables were explored and many were found to have significant univariable associations with ADS/PDS. In order to reduce the number of variables in the multivariable analyses and reduce the probability of making type 1 errors, only factors associated with depression status at p < 0.01 at univariable level were included in the multinomial and binary logistic regression analyses. Statistical significance in the multivariable analyses were given at p < 0.05. Analyses were carried out using version 22.0 IBM SPSS Statistics.
Results
The mean total score on the EDS measured at the antenatal interview was 6.10 (SD = 4.9; range 0–28) compared with a mean of 5.25 (SD = 4.6; range 0–30) on the EPDS at 9 months after childbirth. Median total scores at each time point were 5 and 4, respectively, and the mode total score at each time was zero (accounting for 11.7% of the sample at the antenatal interview and 14.2% at postnatal interview). Total EDS scores at the antenatal interview were significantly correlated with total EPDS scores at the postnatal interview (r = 0.46, p < 0.001).
Rates of Depression Symptoms
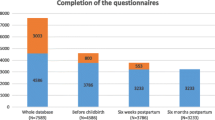
As reported by Waldie et al. (2015), 672 (11.9%) of the 5664 women who provided data at the antenatal interview met the criteria for ADS (total score ≥13). Rates of depression symptoms, according to the EDS/EPDS, for participants with longitudinal data are illustrated in Fig. 2. Over the perinatal period, 16.5% of women (n = 875) experienced significant levels of either ADS (measured during the third trimester of pregnancy) or PDS (at 9 months after childbirth) while 83.5% (n = 4426) were not experiencing depression at either of these time points.
At the time points measured, rates of ADS and PDS were 11.5% (n = 611) and 8% (n = 422), respectively. Almost 26% of women (n = 158) who experienced ADS also had PDS, while 37% of those who had PDS had also experienced ADS. A higher proportion of women experienced ADS only (8.5%) than PDS only (5%). A smaller group of women (3% of the total sample) experienced depression symptoms during the third trimester of pregnancy and were also depressed 9 months after childbirth (ADS + PDS). There were 295 women (5.6% of the total) who experienced ADS that had resolved by the postnatal data collection.
Factors Associated with Depression Status
Table 2 shows the rates of APD/PDS among different groups within the cohort, indicates where differences between depression statuses were significant at univariable level and provides the odds ratios (and 95% confident intervals) for variables that were entered into multivariable analyses. Table 3 shows the means scores of continuous variables for each depression group and provides the odds ratios (and 95% confident intervals) for variables that were entered into multivariable analyses.
The variables that were not associated with depression symptoms (at p < 0.01) at univariable level were: being born in or outside of New Zealand, living in a rural area, parity, exercise in the 1st trimester and 2nd–3rd trimesters of pregnancy. As such, all other variables were included in two multinomial logistic regression analyses exploring the following outcomes: (1) no depression at either time point vs. ADS only, PDS only and ADS + PDS; and (2) ADS only vs. PDS only and ADS + PDS.
The first model included 5173 participants and was significant (−2LL = 4560.29; R2 = 0.29 (Cox and Snell), 0.41 (Nagelkerke), 0.28 (McFadden); Model χ2 (105) = 1743.69, p < 0.001) (see Tables 2, 3). The second model included 844 participants (participants without ADS and/or PDS were removed from the sample) and was significant (−2LL = 1444.99; R2 = 0.26 (Cox and Snell), 0.30 (Nagelkerke), 0.15 (McFadden); Model χ2 (70) = 256.43, p < 0.001) (see Table 4).
As shown in Tables 2 and 3, factors significantly associated with ADS only (compared with no depression at either time point) at multivariable level analyses were: perceived stress score, being in a difficult relationship environment during pregnancy, being of Pacific or Asian ethnicity, not being employed in a paid job during pregnancy, self-reported anxiety before and during pregnancy, unplanned pregnancy and moderate-severe nausea during pregnancy.
Factors significantly associated with PDS at 9 months after childbirth only (compared with no depression at either time point) at multivariable level analyses were: perceived stress score, being of Pacific or Asian ethnicity, not being employed in a paid job during pregnancy and self-reported pre-pregnancy diagnosis of depression.
Factors significantly associated with having ADS + PDS (compared with no depression at either time point) at multivariable level analyses were: perceived stress score, having a difficult relationship environment or difficult family environment during pregnancy, being of Pacific or Asian ethnicity, not being employed in a paid job during pregnancy, self-reported anxiety before and during pregnancy, self-reported anxiety before but not during pregnancy, and one or more alcoholic drinks a week during pregnancy.
PDS vs. ADS Only
The only pre-pregnancy or antenatal factor associated with participants who experienced PDS only rather than ADS only was having a diagnosis of depression pre-pregnancy (see Table 4). Having higher stress scores during the third trimester of pregnancy, a diagnosis of anxiety before and during pregnancy and moderate-severe nausea were associated with an increased likelihood of having antenatal only rather than postnatal only depression symptoms. Pre-pregnancy or antenatal factors associated with participants who were more likely to experience ADS + PDS rather than ADS only were higher perceived stress, difficult relationship environment, difficult family environment (all during the third trimester of pregnancy) and not exercising before pregnancy.
Pre-pregnancy and ADS Impact on PDS
Factors with a significant univariable association (p < 0.01) with depression status were entered into a binary logistic regression alongside ADS with PDS as the dependent variable (see model 3, Table 5). The model included 5178 participants and was significant (−2LL = 2319.58; R2 = 0.1 (Cox and Snell), 0.22 (Nagelkerke); Model χ2(36) = 512.12, p < 0.001). Pre-pregnancy depression and meeting the criteria for depression symptoms at the antenatal interview raised the odds ratio of having depression symptoms 9 months after childbirth by 1.7 (95% CI: 1.28–2.27) and 1.5 (95% CI: 1.15–2.02), respectively.
The analysis was repeated, substituting presence/absence of ADS with antenatal EDS total score (see model 4, Table 5). The model included 5178 participants and was significant (−2LL = 2286.46; R2 = 0.1 (Cox and Snell), 0.24 (Nagelkerke); Model χ2(36) = 545.23, p < 0.001). For each additional point on the EDS measured during the third trimester pregnancy the odds of having PDS were raised by 10% (OR = 1.098, 95% CI: 1.067–1.129, p < 0.001).
Impact of Ethnicity
Pacific or Asian women accounted for 26% of the entire sample but this group accounted for 37.7% of the 875 women who had depression symptoms at the antenatal interview or 9 months after childbirth (according to the EDS/EPDS) and 46.5% of the 158 women who had significant depression symptoms at both time points.
Discussion
Our study of 5301 women from the Growing Up in New Zealand study cohort found that 16.5% reported significant depression symptoms either at their antenatal interview or at 9 months after childbirth. Like previous large longitudinal studies, more women met the criteria for probable depression as measured at the antenatal interview than did at the postnatal interview (Bowen et al. 2012; Cankorur et al. 2015; Evans et al. 2001; Rich-Edwards et al. 2006). A small but significant group who had ADS at the antenatal interview also met the criteria for depression 9 months after childbirth. We also found that higher EDS scores at the antenatal interview were associated with an increased likelihood of PDS. This appears to suggest that, in our sample, the more severe a participant’s ADS were the more likely they were to experience PDS at 9 months postpartum. It may not be just that the presence of significant ADS increases the risk of depression symptoms at 9 months post-delivery but that severity of ADS matters and women with more severe ADS should be particularly closely monitored and supported after childbirth.
Postnatal depression studies that neglect to account for depression during pregnancy and its antecedents run the risk of ignoring a significant source of variance (Cankorur et al. 2015; Haas et al. 2005). Women who have PDS are not the exact same group of women who experienced antenatal depression. Furthermore, there are differing risk factors for depression symptoms during each of these perinatal period. For example, women who have been depressed in the past, but do not experience antenatal depression, may be most at risk of postnatal depression.
Results from previous longitudinal studies reflect some of our findings that perinatal depression symptoms are associated with relationship issues, unemployment, unplanned pregnancy, pre-pregnancy exercise, nausea and alcohol use (Bowen et al. 2012; Haas et al. 2005; Kim et al. 2008; Rich-Edwards et al. 2006; Schmied et al. 2013). Systematic reviews have found that the strongest predictors of ADS are life stress and lack of social support (Lancaster et al. 2010) while PDS are related to a history of depression, ADS, anxiety and stress, and low levels of social support during pregnancy (Robertson et al. 2004). Other common factors from previous studies were not significantly associated with depression symptoms in our study e.g. age, marital status, parity, education and socioeconomic status (Banti et al. 2011; Hein et al. 2014; Robertson et al. 2004). Evidence on the impact of age, parity and relationship status has been found to be inconsisent (Lancaster et al. 2010).
Many of the pre-pregnancy and pregnancy risk factors associated with depression symptoms in our study were related to the women’s mental health; pre-pregnancy depression, anxiety before and during pregnancy and perceived stress during the third trimester of pregnancy. This adds to extensive existing evidence that there are high levels of comorbidity between depression, anxiety and stress (Lancaster et al. 2010; O’Hara and Swain 1996; Robertson et al. 2004; Schmied et al. 2013). Further research is needed on the extent to which women experiencing psychological distress during pregnancy seek and receive appropriate assessment/intervention (Bowen et al. 2012). This is important because there is evidence that emotional problems during pregnancy are associated with obstetric complications (Chung et al. 2001). Antenatal stress can also influence foetal neurodevelopment resulting in cognitive and behavioural problems throughout childhood and adolescence (Lamb et al. 2014; Slykerman et al. 2014; Thompson et al. 2012).
Previous research has indicated that the EDS/EPDS may comprise two factors: depression symptoms and anxio-depressive symptoms. It is possible that scores of each factor contribute to the total score differently during pregnancy compared with after childbirth. Particularly, in this study where the data were collected during the third trimester of pregnancy which is known to be a period of increase stress and anxiety. More detailed analyses of this and the relationship between depression symptoms, anxiety and stress is needed.
Risk factors identified in our study suggest that encouraging women who are trying to get pregnant to exercise and those who are pregnant to avoid alcohol may reduce the risk of perinatal depression. Linking alcohol intake to maternal mental health would reinforce messages that mothers currently receive about the negative impact of alcohol on foetal/child health. Targeted interventions for alcohol abuse before, during and after pregnancy may also reduce the risk of ADS and/or PDS.
Compared with alcohol intake, there is very little promotion on the benefits of physical exercise with respect to perinatal mental health. A recent systematic review on the effectiveness of exercise for the prevention and treatment of antenatal depression found some evidence that exercise during pregnancy can help ADS, but the finding came with the caveat that they were based on a small number of studies and low-moderate quality trials, with significant heterogeneity and wide confidence intervals (Daley et al. 2015). With respect to postnatal depression, Teychenne and York’s (2013) review on physical activity, sedentary behaviour, and PDS found that studies in this area were also limited. They concluded that there is some indication that physical activity prior to, during and after pregnancy may help reduce the risk of PDS, with more research needed to explore the optimal exercise dose and type of activity. Our findings have contributed to the limited amount of research in this field and suggest that it is only exercise prior to becoming pregnant rather than exercise during pregnancy that is associated with a reduced likelihood of depression symptoms.
Our findings suggest that women may need extra support during pregnancy if they are unemployed, their pregnancy was not planned, they experience moderate to severe nausea, have anxiety or panic attacks before and during pregnancy and they have a difficult relationship or family environment. Women who have difficult relationships and family environments are also most at risk of being in the persistent depression group and these mothers could be more carefully monitored and supported. Women who report relationship difficulties may be experiencing domestic abuse. As such, maternity service providers should be aware of interventions for domestic abuse during pregnancy and after childbirth that may be of help to women at risk of ADS and/or PDS.
Future research should further explore the impact of the factors identified in this study on antenatal and/or postnatal depression. In particular, more evidence is needed on prevention tools and interventions that target modifiable factors such as relationship and family issues, stress, exercise, and alcohol use.
New Zealand is a developed country with a predominantly urban population and a relatively high fertility rate. Of the 4.5 million people who live in New Zealand, over 25% were born overseas. The major ethnic groups are New Zealand European, Māori, Asian, and Pacific peoples. In our study, Pacific and Asian women were disproportionally represented among those with ADS only, PDS only and depression symptoms at both time points. This did not appear to be related to immigration from outside of NZ since country of birth was not significantly associated with ADS or PDS at a univariate level. Furthermore, this association persisted when socioeconomic/demographic factors such as deprivation, education, employment status and relationship status were taken into account.
Other studies have found high rates of perinatal depression among Pacific women (Onoye et al. 2009) and in Asian countries (Imran and Haider 2010). These increased rates could be a result of the methods used (e.g., the screening tool) or underlying high levels of perinatal depression among different ethnic groups (Halbreich and Karkun 2006). The Pacific Islands Family Study found that postnatal psychological distress among Pacific women in New Zealand was associated with intimate partner physical violence and, to some extent, smoking and alcohol behaviours (Gao et al. 2010). More research is needed on risk factors for these women and differences between those from different countries/Pacific islands.
Limitations and Strengths
Due to the large sample size of the Growing Up in New Zealand study it was not possible to carry out follow-up assessment of those with high scores to determine how many met the diagnostic criteria for depression. We were also unable to carry out any standardised assessment of pre-pregnancy depression and relied on self-reported diagnosis for this and for levels of anxiety before and during pregnancy. We were unable to determine whether the women in our sample who reported a pre-pregnancy diagnosis, ADS or depression symptoms at 9 months postpartum had sought or were receiving treatment. Neither were we able to ascertain whether any of the women had been diagnosed with postnatal depression. The accuracy of our data on pre-pregnancy and early pregnancy variables may have been adversely affected by recall bias. Data were collected at only two time points thus our results may not be generalizable to the first and second trimesters of pregnancy or the weeks and months immediately following childbirth; all time periods associated with the risk of developing depression. More research on identifying depression earlier in pregnancy or following childbirth is needed.
Loss to follow-up in the study was relatively small (6.3%). However, those excluded from the longitudinal analyses were significantly different from those in the original antenatal sampling suggesting some selection bias. The results of the study may have differed if more women had taken part in both the antenatal and postnatal interviews. There were missing data for some of the variables (with up to 19 cases missing) and a complete case analysis was used for the multivariable models resulting in up to 128 missing cases; this may have led to some additional bias.
The mode EDS/EPDS score for women included in the sample was zero. Some researchers have suggested that zero scores on the EDS/EPDS indicate a pathological score or a sign of high social desirability. It was not possible to explore the former concept but the latter may be an issue when carrying out face-to-face interviews as was the case in this study.
The main strength of the study was the use of a large, population-based, sample sourced from a cohort with high participation and low attrition rates that has good representation of minority ethnic groups and those with low socio-economic status. Further, we used a standardised, validated measure of ADS and depression symptoms at 9 months postpartum. The breadth of data collected during the antenatal interview allowed us to take into account a very broad range of pre-pregnancy and pregnancy factors. A conservative criterion was used to determine which variables were included multivariable analyses. Only variables which were significantly associated with depression symptoms at p < 0.01 were entered.
Conclusion
The perinatal period can be a time of psychological distress for women that has both short and long-term negative effects. Effective prevention, identification and treatment of depression symptoms prior to, during and post-pregnancy are vital. Suggested strategies include: discussing pregnancy with women who experience or are at risk of experiencing mental health problems; providing support to women with a history of mental health problems who are pregnant or planning to get pregnant; mental health screening and promotion for women throughout pregnancy (particularly those in at-risk groups); and additional support for women after childbirth if they have experienced pre-pregnancy or antenatal mental health problems.
Abbreviations
- ADS:
-
Antenatal depression symptoms
- CI:
-
Confidence interval
- EDS:
-
Edinburgh Depression Scale
- EPDS:
-
Edinburgh Postnatal Depression Scale
- PDS:
-
Postnatal depression symptoms
- M:
-
Mean
- ND:
-
No data
- PSS:
-
Perceived Stress Scale
- REF:
-
Reference
- SD:
-
Standard deviation
References
Austin, M. -P, Priest, S. R., Sullivan, E. A., & Cochrane Collaboration (2008). Antenatal psychosocial assessment for reducing perinatal mental health morbidity. New York: Wiley.
Banti, S., Mauri, M., Oppo, A., Borri, C., Rambelli, C., Ramacciotti, D., & Cassano, G. B. (2011). From the third month of pregnancy to 1 year postpartum. Prevalence, incidence, recurrence, and new onset of depression. Results from the Perinatal Depression-Research and Screening Unit study. Comprehensive Psychiatry, 52(4), 343–351.
Barber, C. C. (2009). Perinatal mental health care in New Zealand: The promise of beginnings. New Zealand Journal of Psychology, 38, 32–38.
Beck, C. T. (2001). Predictors of postpartum depression. An update. Nursing Research, 50(5), 275–285.
Bennett, H. A., Einarson, A., Taddio, A., Koren, G., & Einarson, T. R. (2004). Prevalence of depression during pregnancy: Systematic review. Obstetrics and Gynecology, 103(4), 698–709.
Bowen, A., Bowen, R., Butt, P., Rahman, K., & Muhajarine, N. (2012). Patterns of depression and treatment in pregnant and postpartum women. Canadian Journal of Psychiatry, 57(3), 161–167.
Cankorur, V. S., Abas, M., Berksun, O., & Stewart, R. (2015). Social support and the incidence and persistence of depression between antenatal and postnatal examinations in Turkey: A cohort study. BMJ Open, 5, e006456.
Chung, T. K. H., Lau, T. K., Yip, A. S. K., Chiu, H. F. K., & Lee, D. T. S. (2001). Antenatal depressive symtpomatology is associated with adverse obstetric and neonatal outcomes. Psychosomatic Medicine, 63, 830–834.
Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health Social Behavior, 24, 385–396.
Cox, J. L., Chapman, G., Murray, D., & Jones, P. (1996). Validation of the Edinburgh postnatal depression scale (EPDS) in non-postnatal women. Journal of Affective Disorders, 39, 185–189.
Cox, J. L., Holden, J. M., & Sagovsky, R. (1987). Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. The British Journal of Psychiatry, 150(6), 782–786.
Daley, A. J., Foster, L., Long, G., Palmer, C., Robinson, O., Walmsley, H., & Ward, R. (2015). The effectiveness of exercise for the prevention and treatment of antenatal depression: Systematic review with meta-analysis. BJOG: An International Journal of Obstetrics & Gynaecology, 122(1), 57–62.
Dennis, C. L., & Dowswell, T. (2013). Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database of Systematic Reviews (Online), 28(2), CD001134.
Dunst, C. J., Jenkins, V., & Trivette, C. M. (1984). Family support scale: Reliability and validity. Journal of Individual, Family and Community Wellness, 1, 45–52.
Evans, J., Heron, J., Francomb, H., Oke, S., & Golding, J. (2001). Cohort study of depressed mood during pregnancy and after childbirth. British Medical Journal, 323(7307), 257–260.
Gao, W., Paterson, J., Abbott, M., Carter, S., Iusitini, L., & McDonald-Sundborn, G. (2010). Impact of current and past intimate partner violence on maternal mental health and behaviour at 2 years after childbirth: Evidence from the Pacific Islands Families Study. Australian and New Zealand Journal of Psychiatry, 44(2), 174–182.
Gavin, N. I., Gaynes, B. N., Lohr, K. N., Meltzer-Brody, S., Gartlehner, G., & Swinson, T. (2005). Perinatal depression: A systematic review of prevalence and incidence. Obstetrics and Gynecology 106(5, Part 1), 1071.
Haas, J. S., Jackson, R. A., Fuentes-Afflick, E., Stewart, A. L., Dean, M. L., Brawarsky, P., & Escobar, G. J. (2005). Changes in the health status of women during and after pregnancy. Journal of General Internal Medicine: Official Journal of the Society for Research and Education in Primary Care Internal Medicine, 20(1), 45–51.
Halbreich, U., & Karkun, S. (2006). Cross-cultural and social diversity of prevalence of postpartum depression and depressive symptoms. Journal of Affective Disorders, 91(2–3), 97–111.
Hein, A., Rauh, C., Engel, A., Haberle, L., Dammer, U., Voigt, F., Fasching, P. A., Faschingbauer, F., Burger, P., Beckmann, M. W., Kornhuber, J., & Goecke, T. W. (2014). Socioeconomic status and depression during and after pregnancy in the Franconian Maternal Health Evaluation Studies (FRAMES). Archives of Gynecology and Obstetrics, 289(4), 755–763.
Howard, L. M., Molyneaux, E., Dennis, C. L., Rochat, T., Stein, A., & Milgram, J. (2014). Perinatal mental health 1: Non-psychotic mental disorders in the perinatal period. Lancet, 384, 1775–1788.
Imran, N., & Haider, I. I. (2010). Screening of antenatal depression in Pakistan: Risk factors and effects on obstetric and neonatal outcomes. Asia-Pacific Psychiatry, 2(1), 26–32.
Kessler, R. C., Zhao, S., Blazer, D. G., Swartz, M. (1997). Prevalence, correlates, and course of minor depression and major depression in the national comorbidity survey. Journal of Affective Disorders, 45, 19–30.
Kim, Y. -K., Hur, J. -W., Kim, K. -H., Oh, K. -S., & Shin, Y. -C. (2008). Prediction of postpartum depression by sociodemographic, obstetric and psychological factors: A prospective study. Psychiatry and Clinical Neurosciences, 62(3):331–340.
Lamb, Y. N., Thompson, J. M., Murphy, R., Wall, C., Kirk, I. J., Morgan, A. R., et al. (2014). Perceived stress during pregnancy and the catechol-O-methyltransferase (COMT) rs165599 polymorphism impacts on childhood IQ. Cognition, 132(3), 461–470. doi:10.1016/j.cognition.2014.05.009.
Lancaster, C. A., Gold, K. J., Flynn, H. A., Yoo, H., Marcus, S. M., & Davis, M. M. (2010). Risk factors for depressive symptoms during pregnancy: A systematic review. American Journal of Obstetrics and Gynecology, 202(1), 5–14.
Melby, J. N., Conger, R. D., Book, R., Rueter, M., Lucy, L., Repinski, D., et al. (1993). The Iowa family interaction rating scales (4th ed.). Coding manual. Ames, Iowa State University, Institute for Social and Behavioral Research.
Milgrom, J. & Gemmill, A. W. (2014). Screening for perinatal depression. Best Practice & Research Clinical Obstetrics & Gynaecology, 28, 13–23.
Ministry of Health. (2003). District Health Board toolkit: Physical Activity. Wellington: New Zealand Ministry of Health.
Morton, S. M. B., Atatoa Carr, P. E., Grant, C. C., Lee, A. C., Bandara, D. K., Mohal, J., Kinloch, J., Schmidt, J. M., Hedges, M. R., Ivory, V. C., Kingi, T. K., Liang, R., Perese, L. M., Peterson, E. R., Pryor, J. E., Reese, E., Robinson, E. M., Waldie, K. E. & Wall, C. (2012). Growing Up in New Zealand: A longitudinal study of New Zealand Children and their families. Report 2: Now we are born. Auckland: Growing Up in New Zealand
Morton, S. M. B., Ramke, J., Kinloch, J., Grant, C. C., Atatoa Carr, P., Leeson, H., Lee, A. C., & Robinson, E. (2015). Growing Up in New Zealand cohort alignment with all New Zealand births. Australian and New Zealand Journal of Public Health, 39(1), 82–87.
National Institute for Health and Clinical Excellence. (2014). Antenatal and postnatal mental health. Clinical management and service guidance. London: National Insitute of Health and Clinical Excellence.
New Zealand Gazette. (2007). http://www.health.govt.nz/system/files/documents/publications/s88-primary-maternity-services-notice-gazetted-2007.pdf.
O’Hara, M. W., Swain, A. M. (1996). Rates and risk of postpartum depression-a meta-analysis. International Review of Psychiatry, 8, 37–54.
Onoye, J. M., Goebert, D., Morland, L., Matsu, C., & Wright, T. (2009). PTSD and postpartum mental health in a sample of Caucasian, Asian, and Pacific Islander women. Archives of Women’s Mental Health, 12(6), 393–400.
Pryor, J. E. (2004). Stepfamilies and resilience. Final report. Prepared for Centre for Social Research and Evaluation/Te Pokapū Rangahau Arotaki Hapori. Roy McKenzie Centre for the Study of Families, Wellington, Victoria University.
Rich-Edwards, J. W., Kleinman, K., Abrams, A., Harlow, B. L., McLaughlin, T. J., Joffe, H., & Gillman, M. W. (2006). Sociodemographic predictors of antenatal and postpartum depressive symptoms among women in a medical group practice. Journal of Epidemiology and Community Health, 60(3), 221–227.
Robertson, E., Grace, S., Wallington, T., & Stewart, D. E. (2004). Antenatal risk factors for postpartum depression: A synthesis of recent literature. General Hospital Psychiatry, 26(4), 289–295.
Schmied, V., Johnson, M., Naidoo, N., Austin, M. P., Matthey, S., Kemp, L., et al. (2013). Maternal mental health in Australia and New Zealand: A review of longitudinal studies. Women and Birth: Journal of the Australian College of Midwives, 26(3), 167–178.
Sidebottom, A. C., Hellerstedt, W. L., Harrison, P. A., & Hennrikus, D. (2014). An examination of prenatal and postpartum depressive symptoms among women served by urban community health centers. Archives of Womens Mental Health, 17, 27–40.
Slykerman, R. F., Thompson, J., Waldie, K., Murphy, R., & Mitchell, E. A. (2014). Maternal stress during pregnancy is associated with moderate to severe depression in 11-year-old children. Acta Paediatrica. doi:10.1111/apa.12787.
Statistics New Zealand. (2004). Report of the review of the measurement of ethnicity. Wellington: Statistics New Zealand
Teychenne, M., & York, R. (2013). Physical activity, sedentary behavior, and postnatal depressive symptoms: A review. American Journal of Preventive Medicine, 45(2), 217–227.
Thompson J. M. D, Sonuga-Barke, E. J., Morgan, A. R., Cornforth, C., Ferguson, L. R., Mitchell, E. A., & Waldie, K. E. (2012). The catechol-O-methyltransferase (COMT) Val158Met polymorphism moderates the effect of antenatal stress on behavioural problems. Developmental Medicine and Child Neurology, 54(2), 148–154.
Turrell, G., Kavanagh, A., & Subramanian, S. V. (2006). Area variation in mortality in Tasmania (Australia): The contributions of socioeconomic disadvantage, social capital and geographic remoteness. Health & place, 12(3), 291–305.
Underwood, L., Waldie, K. E., Peterson, E. R., D’Souza, S., & Morton, S. M. B. (2016). A review of longitudinal studies on antenatal and postnatal depression. Archives of Women’s Mental Health, 19(5), 711–720.
Waldie, K. E., Peterson, E. R., D’Souza, S., Underwood, L., Pryor, J. E., Carr, P. A., Grant, C., & Morton, S. M. B. (2015). Depression symptoms during pregnancy: Evidence from Growing Up in New Zealand. Journal of Affective Disorders, 186, 66–73.
Ware, J. E., Kosinski, M., & Keller, S. K. (1994). SF-36 physical and mental health summary scales: A user’s manual. Boston, MA: The Health Institute.
Acknowledgements
The Growing Up in New Zealand study has been funded by the New Zealand Ministries of Social Development, Health, Education, Justice and Pacific Island Affairs; the former Ministry of Science Innovation and the former Department of Labour (now both part of the Ministry of Business, Innovation and Employment); the former Ministry of Women’s Affairs (now the Ministry for Women); the Department of Corrections; the Families Commission (now known as the Social Policy Evaluation and Research Unit); Te Puni Kokiri; New Zealand Police; Sport New Zealand; the Housing New Zealand Corporation; and the former Mental Health Commission, The University of Auckland and Auckland UniServices Limited. Other support for the study has been provided by the New Zealand Health Research Council, Statistics New Zealand, the Office of the Children’s Commissioner and the Office of Ethnic Affairs.
Funding
The study has been designed and conducted by the Growing Up in New Zealand study team, led by the University of Auckland. The authors acknowledge the contributions of the original study investigators: Susan M.B. Morton, Polly E. Atatoa Carr, Cameron C. Grant, Arier C. Lee, Dinusha K. Bandara, Jatender Mohal, Jennifer M. Kinloch, Johanna M. Schmidt, Mary R. Hedges, Vivienne C. Ivory, Te Kani R. Kingi, Renee Liang, Lana M. Perese, Elizabeth Peterson, Jan E. Pryor, Elaine Reese, Elizabeth M. Robinson, Karen E. Waldie and Clare R. Wall. The views reported in this paper are those of the authors and do not necessarily represent the views of the Growing Up in New Zealand study investigators.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Underwood, L., Waldie, K.E., D’Souza, S. et al. A Longitudinal Study of Pre-pregnancy and Pregnancy Risk Factors Associated with Antenatal and Postnatal Symptoms of Depression: Evidence from Growing Up in New Zealand. Matern Child Health J 21, 915–931 (2017). https://doi.org/10.1007/s10995-016-2191-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-016-2191-x