Abstract
Recruitment of immigrants and racial and ethnic minorities with first-episode psychosis (FEP) for research studies presents numerous challenges. We describe methods used to recruit 43 U.S. Latinos with FEP and their family caregivers (n = 41) participating in a study to reduce duration of untreated psychosis. A key challenge was that patients were not continuing treatment at an outpatient clinic, as initially expected. To facilitate identification of patients prior to outpatient care, we collaborated with clinic and hospital administrators. Many patients and families were grappling with the aftermath of a hospitalization or adjusting to a diagnosis of a serious mental illness. A considerable amount of time was devoted to addressing participants’ concerns and when possible, facilitating needed services. Our experience underscores the importance of establishing long-term relationships through multiple contacts with patients, families, and stakeholders to address recruitment barriers among underserved groups with FEP.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Interest is growing in both the study of early psychosis and its treatment [1, 2]. Research has indicated that early intervention can lead to less burden for patients and families. Studies have found that reducing duration of untreated psychosis (DUP), the time it takes to access services following illness onset, contributes to improved patient outcomes [3, 4]. Researchers are investigating how best to encourage families to seek services early for their loved ones to avoid involuntary hospitalization [5]. Local governments are also funding services for persons in the early stages of illness [6]. Overall, the view of psychotic disorders as inherently chronic conditions is changing [1, 2], with evidence supporting the benefits of timely treatment [3, 4].
It is important that the shift toward studying and treating early psychosis reaches all communities. To date, little attention has been given to addressing the needs of immigrant and minority communities. Immigrant communities are particularly important because studies have found that they are at greater risk of developing schizophrenia and other psychotic disorders than native-born communities [7, 8]. Minority status may also be a risk factor. For example, native-born Māori in New Zealand have higher incidence rates of schizophrenia compared to non-Māori [9]. The needs of immigrant and minority communities are important given that they tend not to access services to the same degree as nonminority communities [10,11,12,13], placing them at risk of longer DUP. For example, Mexican-origin and Spanish-speaking adults, a minority immigrant group, use mental health services to a significantly lesser degree than other ethnic and racial groups in the United States [11]. Although this research focused on nonpsychotic disorders, it is likely to extend to psychotic disorders.
Importantly, efforts to understand and improve treatment that may contribute to the reduction of DUP for Latinos and other immigrant minority groups experiencing first-episode psychosis (FEP) are hampered by research recruitment challenges. The early phase of a psychotic illness is often a period of instability during which patients and families begin to learn about the illness and symptom management. Consequently, they may not be prepared to engage in research, given their other immediate priorities [14, 15]. These challenges are compounded when recruiting immigrants and minorities with FEP. Although studies examining recruitment of immigrant and minority participants are informative [16,17,18,19], they may not address the unique challenges of recruiting immigrant and minority patients with early psychosis in community settings. Even though some studies have recruited racial and ethnic minority individuals with FEP, little information was provided on recruitment strategies or cultural considerations [20,21,22,23]. Studies examining the recruitment of individuals with psychotic disorders have tended to focus on individuals well into their illness course or participating in clinical trials [14, 24]. Some exceptions exist; a recent study described recruitment of individuals with FEP by clinicians in early psychosis clinics [15]. However, these findings may not translate to settings outside of specialty FEP clinics, where access to patients and organizational support may be limited.
In the current study, we share the lessons we have learned in recruiting Latinos, both immigrants and U.S. born, to a study assessing DUP in this immigrant and ethnic minority group. We present a case study depicting major recruitment issues and associated strategies, then discuss possible implications for providing services to this hard-to-reach segment of the community.
Methods
Study Overview
The parent study seeks to increase psychosis literacy in the San Fernando Valley in Southern California through a communication campaign developed for Latinos using various media formats described elsewhere [5, 25, 26] to reduce DUP among Latinos with FEP. Data were collected during the baseline period (May 2014 through August 2015) before the communication campaign began. By comparing DUP among individuals experiencing early psychosis and their caregivers before the launch of the campaign to DUP of other individuals identified after the launch, we will be able to assess whether the campaign contributed to a reduction in DUP. We are particularly interested in assessing the delay persons with FEP experience in seeking mental health treatment and adhering to their medication. Findings related to the communication campaign and DUP will be presented elsewhere.
Patients met study criteria if they (a) self-identified as Latino; (b) were 15–64 years old; and (c) had a clinical diagnosis of a psychotic disorder including mood disorders with psychotic features. Exclusion criteria consisted of having a diagnosis of a psychotic disorder due to a general medical condition or prior treatment for psychosis consisting of more than 1 year of continuous antipsychotic medication at any time. Once patients agreed to participate in the study, they identified a primary caregiver who could also be contacted for study participation. Written informed consent was obtained from all participants and written assent was secured from those younger than 18 years of age. The study was approved by the Institutional Review Board of the University of Southern California.
Participant Eligibility and Enrollment
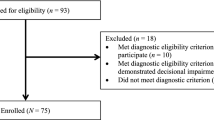
Eighty-four patients were referred for study participation. Eighteen individuals did not meet study inclusion criteria. Specifically, nine had taken antipsychotic medication continuously for more than 1 year and the other nine did not have a relevant diagnosis—seven were diagnosed with a drug-induced psychotic episode and two with a mood disorder without psychotic symptoms. In addition, we were unable to assess eligibility for 21 patients because we could not contact 12 and nine declined to participate after initially agreeing to do so. Some who declined expressed concern that recalling their psychotic episode might trigger symptoms, and others stated they did not believe they had an illness. As a result, 45 of the referred patients were found eligible for the study. However, two of these 45 patients dropped out after they consented to participate in the study but before completing the baseline assessment. Therefore, our final sample consisted of 43 patients, representing 96% of those who met study criteria and enrolled in the study.
Table 1 provides demographic data of our baseline sample of 43 patients and 41 caregivers. Data were collected by bilingual and bicultural research staff members using established measures such as the Structured Clinical Interview for DSM-IV [27] to determine diagnosis. A semistructured interview was also conducted with participants that included questions related to pathways to care and family relations. Two-thirds of patient interviews (n = 29, 67%) were conducted in English, although their self-reported Spanish speaking proficiency was good, suggesting that most patients were bilingual. However, caregiver interviews were primarily conducted in Spanish (n = 27, 66%), and caregivers reported significantly higher Spanish proficiency than English proficiency, t(39) = − 4.67, p < .01 (Spanish proficiency: M = 3.65, SD = 0.70; English proficiency: M = 2.53, SD = 1.13).
Results
Recruitment Site Administrative Support
Recruitment began at a community outpatient mental health clinic. The clinic is located in a large urban county featuring variability in services. Specialty services are generally not provided for patients with FEP, as was the case for the recruitment clinic site. Based on a review of the clinic’s administrative database, census data from the targeted catchment area, and the estimated incidence rate of psychotic disorders, we expected to identify approximately four patients per month who met study criteria. A key factor in our recruitment efforts was close collaboration with the clinic administrative leadership. In particular, the clinic medical director, a psychiatrist and study co-investigator, played a critical role in identifying potential participants. He acted as a gatekeeper among patients, our research team, which consisted of professionals in the fields of psychology, psychiatry, nursing, and social work, and the clinic staff. In addition, we had the support of a bilingual and bicultural research coordinator, a registered nurse, whose office was in the clinic. He was an important asset to the project given his extensive research and clinical experience working with Latinos with serious mental illness and their families in addition to his knowledge of community services. The medical director attended weekly disposition meetings during which discussions took place regarding newly enrolled patients who had consented to receive outpatient treatment. Based on this knowledge, case managers contacted potential participants to inform them about the study, obtain permission for the study team members to contact them, and assess if they were interested in participating in the study.
During the study recruitment period, 1232 new patients sought treatment at the clinic, of whom 627 (51%) were Latino. Of these Latino patients, 202 (32%) had a psychotic disorder; however, most did not meet our study criteria because they had received antipsychotic medication for more than 1 year and thus were not considered patients with FEP. During the first 6 months of the study, we recruited 15 participants, well below our recruitment goals.
Therefore, we decided to expand our recruitment efforts to another site. Because the clinic’s medical director was also the chief of psychiatry at a local safety-net hospital (with a psychiatric emergency room and inpatient psychiatric unit), he had knowledge of patients who might be eligible for study participation but not engaged in treatment at the community mental health center. Many such patients were informed about study participation and agreed to be contacted by the research coordinator. Most (n = 21, 75%) of the remaining 28 patients were recruited from the inpatient unit or psychiatric emergency facility. Expanding to the hospital site proved beneficial, otherwise we would have only recruited seven participants during this period.
Prolonged Relationship and Engagement
We used the initial contact at the hospital (and to some extent at the outpatient clinic) as an opportunity to engage participants in treatment. The research coordinator usually met briefly with the patient at the hospital and then followed up with the patient and family caregiver once the patient was discharged to provide further study information. We understood that patients and families might still be grappling with the aftermath of a hospitalization or acknowledging a diagnosis of a serious mental illness. The period after an initial psychotic episode is a stressful time for patients and families, and they likely have many priorities other than participation in research [14, 15]. The research coordinator considered these issues when contacting participants and spent a considerable amount of time listening to and addressing their concerns and referring them to their treatment provider as needed. As illustrated in the case study below, the research coordinator usually met with participants on more than one occasion. Many expressed a lack of knowledge regarding available clinical programs, which served as an opportunity to introduce them to the clinic and its services. It is important to note that unlike other studies [15] in which clinicians act as recruiters and thus may have frequent contact with patients, our research coordinator, although housed in the clinic, was not employed by the clinic. Therefore, he had limited access to patients, requiring additional effort to establish a relationship with potential participants.
The research team members also spent time providing psychoeducation about the illness with the purpose of supporting illness management. To further address the needs of study participants, we introduced a monthly drop-in family support group at the outpatient clinic to provide a forum for participants to receive additional information and support without registering as service recipients. The group was primarily composed of study participants; however, it was also open to unenrolled patients and families. The group had the added benefit of helping with study retention, allowing the research team to maintain contact with some families for continued data collection.
Case Study
The following is an example of the strategies used to recruit a patient and his family caregiver. The patient, a 28-year-old single Latino man, was taken to the hospital by law enforcement for involuntary treatment after he was found confronting a man on the street because of severe delusions. The patient agreed to be contacted by the research coordinator, who contacted the patient and his mother after several attempts to reach them by phone during a period of 2 months. He later learned that the mother used a prepaid cellular phone that was often not in service due to her inability to afford payment. The family of four experienced several barriers due to their low socioeconomic status, including renting a room that they all shared and relying on public transportation, which made it difficult for the patient to access services. In addition, the patient relied on his mother to communicate with providers, which was difficult due to her limited English-speaking skills. The research coordinator arranged to meet with the patient and his mother at a location near their home. During this initial meeting, the research coordinator took the time to listen to the patient and learn about his concerns. He helped the patient connect with outpatient care, obtain a local bus pass at a reduced rate, and access other social services. Through direct patient feedback and information gathered from the semistructured interview, the research coordinator understood that what mattered most to the patient was his economic situation. Therefore, by providing practical information on how to address this issue, the research coordinator began to engage with the patient, who had previously been reluctant toward treatment and study participation. In addition, because the patient and his mother expressed a lack of understanding regarding the patient’s illness, the research coordinator provided them with psychoeducation and informed them about a Spanish-speaking family support group.
Discussion
The initial difficulties encountered in recruiting participants at the outpatient clinic led to modifications in recruitment methods. Although hospitalized patients were encouraged to seek outpatient care after discharge, many were not seeking service. Our efforts to reach out to patients in the hospital or soon after discharge allowed us to connect with them earlier in the process. Individuals with early psychosis, particularly immigrants [28], have low rates of treatment engagement and therefore may not attend follow-up care [29]. Connecting with patients during the early phase of the illness requires an understanding of their vulnerable situation. As in our case study, most patients had been involuntarily hospitalized after contact with law enforcement, which may have added to their concern about ongoing treatment due to fear that it would lead to another hospitalization. Therefore, our first contact with patients regarding study participation often began with questions about follow-up care, not participation in research. Some level of psychoeducation and case management support was frequently required.
These issues may have been common in our sample given that all patients were Latinos and family members were primarily monolingual Spanish-speaking individuals of Mexican origin. Studies have found that Mexican-origin Latinos who are monolingual Spanish speakers are less likely to use mental health services than other Latino groups [11]. Although participants had recently initiated treatment, they may have delayed seeking continued treatment and required case management support. Recruitment often involved additional effort not only because patients and caregivers were dealing with early psychosis, but also because of contextual issues that required multiple contacts with participants to develop trust, establish study eligibility, and proceed with data collection. Importantly, most studies examining FEP have excluded participants who are not English speaking [4, 22, 23, 30], thereby limiting our knowledge of the needs of non-English-speaking individuals with early psychosis and their families.
Gaining an understanding of what is at stake for patients and caregivers during the initial phase of the illness is essential to recruitment and may also have relevant clinical implications [31]. Most patients were young adults in their early to late 20s with an average age of 28 years. They were adjusting to a serious mental illness diagnosis during a critical time in their lives, when individuals are usually establishing themselves with respect to their work, financial independence, and social relationships. Therefore, recruitment efforts needed to consider patients’ immediate concerns (e.g., financial) to ensure they could participate in the study.
Our recruitment experience may have implications for engaging this hard-to-reach community in mental health services. Service engagement could be enhanced by recognizing the unique needs of patients and families during the initial phase of the illness, particularly through specialty mental health services developed for young adults experiencing psychosis. As services for early psychosis grow, our experience demonstrates that building a prolonged relationship is a key component of recruitment that may also translate to engagement in clinical services.
We found that engaging caregivers was important because they were highly involved in providing support to patients. Studies have found that Latinos with serious mental illness are more likely to live with their family compared to other groups [12]; therefore, engaging family members is critical to recruitment efforts. As seen in our case study, family support was a contributing factor in recruiting the patient to the study. The early phase of the illness can be difficult for family members as they learn to adjust to their loved one’s illness [32, 33], and it may be even more challenging for non-English-speaking family members. These factors needed to be addressed to move forward with recruitment.
It is not possible to generalize our findings based on largely Mexican-origin families to other Latinos or other racial and ethnic groups in different U.S. communities. Nevertheless, our findings may inform recruitment efforts among other underserved groups. For example, trust may be critical to other immigrant and minority group members who have high rates of involuntary admissions [34, 35]. We recognize that providing support to patients may inadvertently shorten patients’ DUP and potentially affect our overall study’s aim, which is to reduce DUP. In addition, our findings should be considered in light of the large public mental health system where this study took place. Recruitment in other mental health systems with linked inpatient and outpatient units, for example, may allow for centralized recruitment at one site.
New Contribution to the Literature
We acknowledge that recruitment barriers among individuals with FEP are not limited to Latinos. However, our study adds to the literature by describing critical issues that can undermine recruitment of immigrants and minorities with FEP and presenting strategies that need to be considered with this and other vulnerable groups. Recruitment of individuals with FEP requires understanding what is salient to them as people experiencing early psychosis. Understanding participants’ local social world [31] is particularly important when recruiting underserved groups such as Latinos, who may present with additional recruitment challenges including contextual factors such as low English language proficiency and low socioeconomic status [36]. Our recruitment methods addressed participants’ concerns by taking the time to learn about their needs, which built trust and contributed to research participation. Our experience also highlights the importance of support from on-site administrators to gain access to participants and address difficulties that may arise during the recruitment process. Finally, because recruitment involves building trust and relationships, which are necessary for treatment engagement, these findings may also have implications for the growing interest in FEP intervention services in the United States and may be particularly relevant among immigrants and minorities with early psychosis.
References
Addington J. The promise of early intervention. Early Interv Psychiatry. 2007;1(4):294–307.
Lieberman JA, Dixon LB, Goldman HH. Early detection and intervention in schizophrenia: a new therapeutic model. JAMA. 2013;310(7):689–90.
Kane JM, Robinson DG, Schooler NR, Mueser KT, Penn DL, Rosenheck RA, Addington J, Brunette MF, Correll CU, Estroff SE, et al. Comprehensive versus usual community care for first-episode psychosis: 2-year outcomes from the NIMH RAISE Early Treatment Program. Am J Psychiatry. 2016;173(4):362–72.
Srihari VH, Tek C, Kucukgoncu S, Phutane VH, Breitborde NJK, Pollard J, Ozkan B, Saksa J, Walsh BC, Woods SW. First-episode services for psychotic disorders in the U.S. public sector: a pragmatic randomized controlled trial. Psychiatr Serv. 2015;66(7):705–12.
López SR, Lara Mdel C, Kopelowicz A, Solano S, Foncerrada H, Aguilera A. La CLAve to increase psychosis literacy of Spanish-speaking community residents and family caregivers. J Consult Clin Psychol. 2009;77(4):763–74.
Essock SM, Goldman HH, Hogan MF, Hepburn BM, Sederer LI, Dixon LB. State partnerships for first-episode psychosis services. Psychiatr Serv. 2015;66(7):671–3.
Cantor-Graae E, Selten JP. Schizophrenia and migration: a meta-analysis and review. Am J Psychiatry. 2005;162(1):12–24.
Bourque F, van der Ven E, Malla A. A meta-analysis of the risk for psychotic disorders among first- and second-generation immigrants. Psychol Med. 2011;41(5):897–910.
Kake TR, Arnold R, Ellis P. Estimating the prevalence of schizophrenia among New Zealand Māori: a capture–recapture approach. Aust N Z J Psychiatry. 2008;42(11):941–9.
Alegría M, Canino G, Ríos R, Vera M, Calderón J, Rusch D, Ortega AN. Mental health care for Latinos: inequalities in use of specialty mental health services among Latinos, African Americans, and non-Latino Whites. Psychiatr Serv. 2002;53(12):1547–55.
Alegría M, Mulvaney-Day N, Woo W, Torres M, Gao S, Oddo V. Correlates of past-year mental health service use among Latinos: results from the National Latino and Asian American Study. Am J Public Health. 2007;97(1):76–83.
Barrio C, Yamada AM, Hough RL, Hawthorne W, Garcia P, Jeste DV. Ethnic disparities in use of public mental health case management services among patients with schizophrenia. Psychiatr Serv. 2003;54(9):1264–70.
Vega WA, Kolody B, Aguilar-Gaxiola S, Catalano R. Gaps in service utilization by Mexican Americans with mental health problems. Am J Psychiatry. 1999;156(6):928–34.
Furimsky I, Cheung AH, Dewa CS, Zipursky RB. Strategies to enhance patient recruitment and retention in research involving patients with a first episode of mental illness. Contemp Clin Trials. 2008;29(6):862–6.
Patterson S, Duhig M, Connell M, Scott J. Successful recruitment to a study of first-episode psychosis by clinicians: a qualitative account of outcomes and influences on process. J Ment Health. 2014;23(5):225–30.
Areán PA, Alvidrez J, Nery R, Estes C, Linkins K. Recruitment and retention of older minorities in mental health services research. Gerontologist. 2003;43(1):36–44.
Loue S, Sajatovic M. Research with severely mentally ill Latinas: successful recruitment and retention strategies. J Immigr Minor Health. 2008;10(2):145–53.
Shedlin MG, Decena CU, Mangadu T, Martinez A. Research participant recruitment in Hispanic communities: lessons learned. J Immigr Minor Health. 2011;13(2):352–60.
Aponte-Rivera V, Dunlop BW, Ramirez C, Kelley ME, Schneider R, Blastos B, Larson J, Mercado F, Mayberg H, Craighead WE. Enhancing Hispanic participation in mental health clinical research: development of a Spanish-speaking depression research site. Depress Anxiety. 2014;31(3):258–67.
Chong SA, Mythily S, Verma S. Reducing the duration of untreated psychosis and changing help-seeking behaviour in Singapore. Soc Psychiatry Psychiatr Epidemiol. 2005;40(8):619–21.
Compton MT, Chien VH, Leiner AS, Goulding SM, Weiss PS. Mode of onset of psychosis and family involvement in help-seeking as determinants of duration of untreated psychosis. Soc Psychiatry Psychiatr Epidemiol. 2008;43(12):975–82.
Krstev H, Carbone S, Harrigan SM, Curry C, Elkins K, McGorry PD. Early intervention in first-episode psychosis—the impact of a community development campaign. Soc Psychiatry Psychiatr Epidemiol. 2004;39(9):711–9.
Morgan C, Dazzan P, Morgan K, Jones P, Harrison G, Leff J, Murray R, Fearon P, AESOP Study Group. First episode psychosis and ethnicity: initial findings from the AESOP study. World Psychiatry. 2006;5(1):40–6.
Jørgensen R, Munk-Jørgensen P, Lysaker PH, Buck KD, Hansson L, Zoffmann V. Overcoming recruitment barriers revealed high readiness to participate and low dropout rate among people with schizophrenia in a randomized controlled trial testing the effect of a guided self-determination intervention. BMC Psychiatry. 2014;14:28.
Calderon V, Mejia Y, del Carmen Lara-Muñoz M, Segoviano J, Castro Q, Casados A, López SR. Towards the sustainability of information campaigns: training promotores to increase the psychosis literacy of Spanish-speaking communities. Soc Psychiatry Psychiatr Epidemiol. 2015;50(4):665–9.
Hernandez MY, Mejia Y, Mayer D, Lopez SR. Using a narrative film to increase knowledge and interpersonal communication about psychosis among Latinos. J Health Commun. 2016;21(12):1236–43.
First MB, Spitzer RL, Gibbon M, Williams, J. Structured clinical interview for DSM-IV axis I disorders. Washington, DC: American Psychiatric Press; 1997.
Ouellet-Plamondon C, Rousseau C, Nicole L, Abdel-Baki A. Engaging immigrants in early psychosis treatment: a clinical challenge. Psychiatr Serv. 2015;66(7):757–9.
Lal S, Malla A. Service engagement in first-episode psychosis: current issues and future directions. Can J Psychiatry. 2015;60(8):341–5.
Kane JM, Schooler NR, Marcy P, Correll CU, Brunette MF, Mueser KT, Rosenheck RA, Addington J, Estroff SE, Robinson J, et al. The RAISE early treatment program for first-episode psychosis: background, rationale, and study design. J Clin Psychiatry. 2015;76(3):240–6.
López SR, Guarnaccia P. Cultural psychopathology: uncovering the social world of mental illness. Annu Rev Psychol. 2000;51:571–98.
Barton K, Jackson C. Reducing symptoms of trauma among carers of people with psychosis: pilot study examining the impact of writing about caregiving experiences. Aust N Z J Psychiatry. 2008;42(8):693–701.
Hernandez M, Barrio C. Perceptions of subjective burden among Latino families caring for a loved one with schizophrenia. Community Ment Health J. 2015;51(8):939–48.
Compton MT, Esterberg ML, Druss BG, Walker EF, Kaslow NJ. A descriptive study of pathways to care among hospitalized urban African American first-episode schizophrenia-spectrum patients. Soc Psychiatry Psychiatr Epidemiol. 2006;41(7):566–73.
Morgan C, Mallett R, Hutchinson G, Leff J. Negative pathways to psychiatric care and ethnicity: the bridge between social science and psychiatry. Soc Sci Med. 2004;58(4):739–52.
Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annu Rev Public Health. 2006;27:1–28.
Funding
This research was supported by a grant from the National Institute of Mental Health (R01MH103830) awarded to Steven Regeser López.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors certify their responsibility for the research presented and they report no known conflict of interest.
Ethical Approval
All applicable institutional guidelines for human participants were followed.
Rights and permissions
About this article
Cite this article
Hernandez, M., Franco, R., Kopelowicz, A. et al. Lessons Learned in Clinical Research Recruitment of Immigrants and Minority Group Members with First-Episode Psychosis. J Immigrant Minority Health 21, 123–128 (2019). https://doi.org/10.1007/s10903-018-0704-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-018-0704-y