Abstract
We investigated whether darker interviewer-ascribed skin color is associated with worse cardiometabolic health among young adult Blacks and Hispanics in the United States. Our sample was comprised of 2,128 non-Hispanic Blacks and 1603 Hispanics aged 24-32, who were in high school in the United States in 1994. We used logistic and OLS regression to predict obesity, hypertension, diabetes, and cardiometabolic risk. We tested the interaction between Hispanic immigrant generation and ascribed skin color. Darker ascribed skin color predicted worse cardiometabolic health among both young adult Blacks and Hispanics. Among Hispanics, the associations were strongest among third and higher generation respondents. Our findings suggest that among US Blacks and Hispanics how individuals are perceived by others via their skin color is significantly associated with their health and well-being. Gradients in cardiometabolic health in young adulthood will likely contribute to gradients in cardiovascular disease and all-cause mortality later in life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Cardiometabolic health, which refers to a constellation of conditions that are collectively associated with the onset of metabolic syndrome, higher risk of cardiovascular disease, and higher all-cause mortality, has worsened dramatically in the United States since the 1990s [1–4]. Extensive research has revealed key disparities in cardiometabolic health across racial/ethnic groups [3]. Non-Hispanic Blacks (Blacks) and Hispanics, the country’s two largest racial/ethnic groups, experience high age-adjusted rates of three important indicators of poor cardiometabolic health—obesity (49.5 and 39.1 %), hypertension (40.4 and 26.1 %), and diabetes (13.2 and 12.8 %) [5–7]. Whites, by contrast, experience lower rates of obesity (34.3 %) and diabetes (7.6 %) than both Blacks and Hispanics, and hypertension (27.4 %) at a rate lower than Blacks, but similar to Hispanics. Although personal lifestyle factors including diet and exercise are important cardiometabolic risk (CMR) factors, medical practitioners and policy makers must also consider structural inequalities and differential stress exposures when addressing racial/ethnic health disparities.
We employ the terms race/ethnicity and racial/ethnic because Hispanics do not fall within US racial categories [8, 9]. Self-reported race/ethnicity, the most common indicator of racial/ethnic disparities used in health research, reflects individuals’ shared cultural and ancestral backgrounds, their perceptions of social position, and their beliefs about how others perceive them [10]. Explanations of racial/ethnic health disparities generally emphasize disparities in factors such as socioeconomic status (SES), which affect access to resources such as health care, creating health disparities that widen across the life course [11, 12]. Additionally, racial/ethnic discrimination can incur chronic stress and initiate physiological changes, leading to elevated blood sugar and blood pressure [8, 11, 13, 14].
Racial/ethnic groups are very heterogeneous. How researchers conceptualize and measure race/ethnicity has implications for how we understand and address racial/ethnic inequalities in health [15]. In particular, wide skin color variation exists US Blacks and Hispanics [16, 17]. Despite the frequent treatment of Blacks and Hispanics as homogenous racial/ethnic groups, scholars have found that how Blacks and Hispanics are perceived by others affects their SES, exposure to racial discrimination, and health [18–22]. Skin color represents a salient indicator of the association between appearance and experience among US Blacks and Hispanics. Darker skin color is associated with fewer years of education, lower household income, greater exposure to racist events, and poorer mental health [18–20, 22]. Among Blacks darker skin color is also associated with higher blood pressure and body-mass-index (BMI) [22, 23]. One study conducted among Puerto Ricans found that darker interviewer-ascribed skin color, but not actual skin pigmentation measured with a narrow-band reflectometer, was associated with higher blood pressure [21].
Following Gravlee et al., we argue that externally-ascribed skin color captures a critical aspect of how individuals are perceived by others, which we expect to be associated with physical health [21]. Studies that have measured the association between skin color and one or more aspects of cardiometabolic health, using geographically limited, non-nationally representative samples of US Blacks, have found that darker skin color is associated with higher blood pressure and BMI [23, 24]. Although less is known about the association between skin color and cardiometabolic health among US Hispanics, darker skin color is associated with poorer self-rated health among Hispanics in the United States and four Latin American countries [15, 25].
Our study makes four contributions. First, we expand the research on skin color and health among Blacks by evaluating a wider variety of cardiometabolic health indicators within a nationally representative sample. Second, we provide one of the first assessments of the association between skin color and cardiometabolic health among Hispanics. Third, we identify gradients in CMR by skin color. Fourth, we explore whether the association between skin color and cardiometabolic health varies by immigrant generation among Hispanics—the data did not contain sufficient first/second generation Blacks to conduct similar analyses. Among first and second generation Hispanic immigrants, who interact primarily with co-ethnics, there is evidence that darker skin color may provide a sense of “ethnic legitimacy” [26]. Ayers et al. found that “indigenous appearance” was associated with lower substance abuse among second generation Mexican youth, but higher substance use within the third generation [27]. Thus, we expect that perceived skin color may be a more salient risk factor among later-generation Hispanics.
Methods
Data
We conducted cross-sectional analyses using data from the National Longitudinal Study of Adolescent to Adult Health (Add Health). Add Health used a multistage, stratified sampling design that randomly selected 80 high schools and their feeder schools in different communities across the United States, creating a baseline sample of 20,745. Three follow-up interviews have been administered, most recently in 2008–2009. We used data from Blacks and Hispanics who participated in Waves I (1994–1995), III (2001–2002), and IV (2008–2009). Wave I interviews provided basic demographic information: self-identified race/ethnicity, gender, and immigrant generation; interviewers recorded perceived skin color at Wave III; all other variables, including cardiometabolic health, were measured at Wave IV.
For this analysis, we included those respondents who self-identified as “Black or African American” and did not select Hispanic ethnicity (Blacks) and those respondents who self-identified as ethnically Hispanic regardless of race (Hispanics). The response rates at Waves III and IV were 77 and 80 % respectively. Analysis of non-response at Wave IV revealed little bias on health measures after sample weights were applied [28]. Thus, our results are representative of cardiometabolic health among Black and Hispanic young adults, aged 24–32, who were attending middle or high school in the United States in 1994–1995.
There were 2491 non-Hispanic Blacks and 1913 Hispanics who were interviewed at Waves I, III, and IV with non-missing sampling weights. We excluded 5 % of Blacks who were either first or second generation immigrants. We deleted observations with missing data on cardiometabolic health measures (13 %) and on independent variables (2 %), leaving an analytic sample of 2128 third-generation non-Hispanic Blacks and 1603 Hispanics. Table 1 summarizes our variables among Blacks and Hispanics.
Measures
Cardiometabolic Health Measures
At Wave IV, trained interviewers collected anthropometric measures, cardiovascular indicators, and glucose homeostasis. We included three clinical indicators of cardiometabolic health—obesity, hypertension, and diabetes. We identified respondents with a BMI (kg/m2) of 30 or higher as obese. We identified all individuals with systolic blood pressure of at least 140, diastolic blood pressure of at least 90, a previous hypertension diagnosis, or prescribed blood pressure medication as hypertensive. We identified diabetes based on a continuous measure of HbA1c (blood sugar) that was derived using dried capillary whole blood spots. We categorized respondents with blood sugar greater than 6.4, those who reported a prior diagnosis, and those currently taking diabetes medications as diabetic.
We used principal components analysis (PCA) to create a composite measure of CMR based on three continuous indicators of cardiometabolic risk—BMI, systolic blood pressure, and blood sugar. PCA weights the different measures to capture the greatest possible proportion of variation in disease risk [29]. The composite variable had an eigenvalue of 1.3 and explained 44 % of the variance across the three measures. Because the PCA did not incorporate prescribed medications or prior diagnoses, it reflects gradients in uncontrolled CMR, unlike the clinical indicators described above. Assessing gradients in risk within a population of young adults provides a forecast of future disparities, which can inform targeted interventions. We standardized composite CMR with a mean of zero and a standard deviation of one. Thus, a value below zero indicates below average CMR, while a value above zero indicates above average CMR.
Skin Color
At Wave III, interviewers ascribed respondents’ skin colors on a five-point scale: black, dark-brown, medium-brown, light-brown, white. Interviewers were mostly non-Hispanic White (71 %) or non-Hispanic Black (21 %) and college educated (91 %). Only 5 % were Hispanic. The results were substantively unchanged when we included an interviewer fixed effect (available upon request). Like other studies that use similar measures, we treat skin color as a categorical variable [16, 18]. Even in studies that utilize melatonin or color palettes to measure skin color continuously, researchers often group values into nominal categories that accord with societally ascribed racial/ethnic profiles [21, 25].
We observed substantial variation in skin color among both Blacks and Hispanics (Table 1). Among Blacks, interviewers ascribed a white or light-brown skin color to 11 % of respondents and a black skin color to 28 % of respondents, with the remainder in the middle. Among Hispanics, interviewers ascribed 42 % white, 42 % light-brown, and 17 % medium-brown to black. Because there were relatively few Blacks (0.48 %) who interviewers reported as having a “white” skin color, we combined the white and light-brown skin colors among Blacks. Similarly, we combined Hispanic respondents who were ascribed black or dark-brown skin-colors (3 %) with those who were classified as medium-brown.
Discrimination and SES
Because others have found that exposure to racial discrimination and access to resources vary by skin color, we adjusted for these factors in our regression models. We adjusted for perceived discrimination using the following item: “In your day-to-day life, how often do you feel you have been treated with less respect or courtesy than other people: never, rarely, sometimes, or often?” We coded respondents who reported sometimes or often as having experienced discrimination. Add Health does not include a multi-item discrimination scale [30]. Thus, we may not fully capture the prevalence of discrimination experiences in our sample.
We adjusted for three aspects of SES—educational attainment (college graduation), annual household income (reported on a 12-point scale from $5000 to $150,000), and economic hardship. Respondents indicated if at any time during the previous 12-months they were: without phone service, unable to pay rent, evicted, unable to pay utilities, lost access to utilities, and/or worried about food shortage. Consistent with prior studies, we coded respondents who experienced at least one aspect of hardship as experiencing economic hardship [31].
Demographic Factors
All regressions controlled for gender, age, married or cohabiting, urban residence, US region (West, Midwest, South, or West), and health insurance coverage. We defined immigrant generation: first-generation (born outside the United States), second-generation (at least one parent born outside the United States), and third-generation (both parents born in the United States). Because Hispanics’ ethnic origin is associated with health and varies by skin color, we adjusted for ethnic origin among Hispanics: Mexican, Cuban, Central-South American, Puerto Rican, other.
Analytic Approach
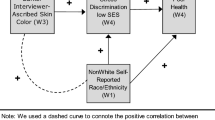
We first present weighted bivariate bar graphs of the associations between skin color and our cardiometabolic measures separately for Blacks and Hispanics (Fig. 1). We next assess the statistical association between skin color and cardiometabolic health among Blacks (Table 2) and Hispanics (Table 3) using ordinary-least-squares regression for CMR and logistic regression for obese, hypertensive, and diabetic. All the regression models were adjusted for demographic characteristics, perceived discrimination, and SES. Results (not shown) revealed no substantive differences between unadjusted models and those presented.
Prevalence of obesity, hypertension, diabetes, and composite CMR among young adult Blacks and Hispanics (aged 24–32) living in the US: Add Health, 2008. LB light brown, MB medium brown, DB dark brown, Black Black. Means and percentages were weighted to provide nationally representative estimates for Blacks. (n = 2128) and Hispanics (n = 1603) living in the U.S. who were in 7th–12th grade in 1994. a Composite CMR was calculated using principal components analysis of BMI, systolic blood pressure, and blood sugar
To assess whether immigrant generation modifies the association between skin color and cardiometabolic health, we included an interaction term between native born (third-generation-plus) and skin color among Hispanics. We computed the full effect of skin color among first/second generation and third and higher generation Hispanics and present these results in Table 3. We used Wald tests to assess the interaction coefficients’ joint significance.
All regressions were weighted and standard errors were adjusted for Add Health’s complex design [32]. We imputed missing income values for 9 % of cases using chained equations.
Results
Skin Color and Cardiometabolic Health
We observed gradients in cardiometabolic health by skin color among Blacks and Hispanics. Among Blacks, the prevalence of each clinical outcome was greatest for those ascribed black skin color (Fig. 1a–c). The percent obese and the percent diabetic both increased with darker ascribed skin color, but they exhibited non-linear trends. Among Hispanics, we observed linear increases associated with darker skin color for hypertension and diabetes, but not obesity (Fig. 1d–f).
We observed strong gradients in CMR among Blacks (Fig. 1g) and Hispanics (Fig. 1h). Within both groups, CMR increased among those ascribed darker skin colors.
Regression Results Among Blacks
We found that among young adult Blacks (Table 2), darker skin color was significantly associated with the risk of obesity and diabetes, but not hypertension.
After adjustment for demographic characteristics, perceived discrimination, and SES, ascribed black skin color was associated with an increase in CMR of 0.39 standard deviations (95 % CI 0.21–0.58) relative to respondents ascribed light-brown or white skin color. The robust linear increase in CMR, which drew upon related, but not identical, measures of cardiometabolic health, suggests that incorporating multiple aspects of disease risk, may provide a stronger indication of overall cardiometabolic health risk than testing multiple outcomes separately. Similar measures may provide important insights to researchers and policymakers interested in long-term health risk within younger populations.
Regression Results Among Hispanics
Among young adult Hispanics (Table 3 ), darker ascribed skin color was significantly associated with greater risk of obesity and diabetes and greater CMR among third or higher generation respondents. At the same time, among third and higher generation respondents, white ascribed skin color had a significant protective effect on CMR (−0.21). By contrast, skin color was not significantly associated with cardiometabolic health or CMR among first and second generation Hispanics.
We found mixed evidence in support of the hypothesized interaction between skin color and immigrant generation among Hispanics. In our regressions for obesity, hypertension, and diabetes, the interactions effects were not jointly significant. However, all of the odds ratios for the interaction effects were in the expected direction. Moreover, the results revealed a robust interaction between ascribed skin color and nativity as they relate to CMR (p < 0.05).
We also estimated separate models (not shown) among first and second generation and the third and higher generation Hispanic young adults. Among first and second generation Hispanic respondents, ascribed skin color was not significantly associated with any of our outcomes and the direction of the coefficients varied. In contrast, among third and higher generation Hispanics, darker ascribed skin color was strongly and significantly associated with poorer cardiometabolic health for all of our outcome measures.
Discussion and Conclusion
We assessed the association between interviewer-ascribed skin color and three clinically defined indicators of cardiometabolic health—obesity, hypertension, and diabetes. Skin color was positively associated with these three outcomes, but the size and robustness of the associations varied across the three measures. Our nationally representative results are consistent with research on skin color and health, which has found gradients in hypertension and BMI among Blacks in geographically limited samples [23, 24]. Ours was the first study to incorporate diabetes, an important indicator of cardiometabolic syndrome. Among both Blacks and Hispanics, we found the strongest associations between ascribed skin color and diabetes risk. Diabetes is an essential consideration in studies of cardiometabolic health as cardiometabolic syndrome with diabetes is associated with higher all-cause mortality, relative to cardiometabolic syndrome without diabetes [4].
Exposure to stress and racial discrimination associated with darker perceived skin color, as well as economic insecurity, which is highest among darker skinned Blacks and Hispanics, may contribute to the elevated diabetes risk. In response to perceived threats and stressors, the brain activates the sympathetic nervous system (SNS) and the hypothalamic–pituitary–adrenal axis (HPA axis) [33, 34]. The SNS triggers the release of glucose and fats for immediate energy. The HPA axis releases the stress hormone cortisol, which also increases glucose and inhibits insulin production. Thus, frequent stress and perceived threat due to skin color among darker skinned Blacks and Hispanics may create a glucose-insulin imbalance, leading to poorer cardiometabolic health.
Additionally, we demonstrated that using a composite indicator to capture variance across related, but not identical, indicators of cardiometabolic health, provides an important indication of the association between how individuals are perceived by others and their cardiometabolic risk. Unlike our clinical measures, which incorporated doctors’ diagnoses and prescriptions, our risk indicator captures uncontrolled CMR. We found a strong and linear association between darker ascribed skin color and greater CMR among third and higher generation Blacks and Hispanics. In contrast, we found no association between ascribed skin color and CMR among first and second generation Hispanics. These findings suggest that how individuals are perceived by others has significant implications for their cardiometabolic health.
We also found that the association between skin color and cardiometabolic health is modified by immigrant generation among Hispanics. Consistent with prior research on substance use across Mexican immigrant generations [27], we found that the association between darker ascribed skin color and cardiometabolic health was significantly stronger among later-generation Hispanic immigrants. These findings suggest that greater “ethnic legitimacy,” which is associated with darker skin color among first and second generation Hispanics, might buffer newer Hispanic immigrants against the consequences associated with darker ascribed skin color that are prevalent among third and higher generation Hispanics [17].
Though this investigation advances our understanding of disparities in cardiometabolic health among Blacks and Hispanics, it also highlights the need for further investigation in several areas. First, because Add Health only measured cardiometabolic health at a single point in time, we were unable to assess the association between ascribed skin color and change in cardiometabolic health across the life course. Second, although our measure provided a strong indicator of how individuals are perceived by others, it did not provide the same precision or flexibility as more complex color scales, such as that designed by Telles and Steele [35]. Third, while researchers recommend multi-item measures of perceived discrimination, the best available indicator was a single question measuring perceived discriminatory treatment [30]. A more robust indicator may have revealed greater attenuation in the association between ascribed skin color and cardiometabolic health. It is our hope that these important findings will stimulate further analysis of ascribed skin color and other factors that may affect cardiometabolic health among Blacks and Hispanics to better understand disparities in health within these large and heterogeneous racial/ethnic groups.
This study has provided an important contribution to the examination of health disparities among Blacks and the first analysis (to our knowledge) of the association between ascribed skin color and objectively measured physical health among Hispanics. We found significant gradients in cardiometabolic health by skin color among Blacks and Hispanics. These results support more widespread measurement of ascribed skin color and other aspects of how individuals are perceived by others, as scholars, policymakers, and medical practitioners move beyond race/ethnicity to better understand and address health disparities in the United States.
References
Mozumdar A, Liguori G. Persistent increase of prevalence of metabolic syndrome among U.S. adults: NHANES III to NHANES 1999–2006. Diabetes Care. 2011;34(1):216–9. doi:10.2337/dc10-0879.
Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among us adults: FINDINGS from the third national health and nutrition examination survey. JAMA. 2002;287(3):356–9. doi:10.1001/jama.287.3.356.
Grundy SM, Brewer HB, Cleeman JI, Smith SC, Lenfant C. Definition of metabolic syndrome report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004;109(3):433–8. doi:10.1161/01.CIR.0000111245.75752.C6.
Malik S, Wong ND, Franklin SS, et al. Impact of the metabolic syndrome on mortality from coronary heart disease, cardiovascular disease, and all causes in United States adults. Circulation. 2004;110(10):1245–50. doi:10.1161/01.CIR.0000140677.20606.0E.
Flegal K, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307(5):491–7. doi:10.1001/jama.2012.39.
Yoon SS, Burt V, Louis T, Carroll MD. Hypertension among adults in the United States, 2009–2010. NCHS Data Brief. 2012;107:1–8.
Centers for Disease Control and Prevention. National diabetes statistics report: estimates of diabetes and its burden in the United States. Atlanta, GA: US Department of Health and Human Services; 2014. http://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf. Accessed 9 Jan 2016.
Borrell LN. Racial identity among Hispanics: implications for health and well-being. Am J Public Health. 2005;95(3):379–81. doi:10.2105/AJPH.2004.058172.
Roth WD. The multiple dimensions of race. Ethn Racial Stud. 2016;39(8):1310–38. doi:10.1080/01419870.2016.1140793.
Nagel J. Constructing ethnicity: creating and recreating ethnic identity and culture. Soc Probl. 1994;41(1):152–76. doi:10.2307/3096847.
Dressler WW, Oths KS, Gravlee CC. Race and ethnicity in public health research: models to explain health disparities. Annu Rev Anthropol. 2005;34(1):231–52. doi:10.1146/annurev.anthro.34.081804.120505.
Stringhini S, Batty GD, Bovet P, et al. Association of lifecourse socioeconomic status with chronic inflammation and type 2 DIABETES risk: the Whitehall II Prospective cohort study. PLoS Med. 2013;10(7). doi:10.1371/journal.pmed.1001479.
Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health. 2011;32:381–98. doi:10.1146/annurev-publhealth-031210-101218.
Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32(1):20–47. doi:10.1007/s10865-008-9185-0.
Garcia JA, Sanchez GR, Sanchez-Youngman S, Vargas ED, Ybarra VD. Race as lived experience. Bois Rev Soc Sci Res Race. 2015;12(2):349–73. doi:10.1017/S1742058X15000120.
Golash-Boza T, Darity W. Latino racial choices: the effects of skin colour and discrimination on Latinos’ and Latinas’ racial self-identifications. Ethn Racial Stud. 2008;31(5):899–934. doi:10.1080/01419870701568858.
Hunter M. The persistent problem of colorism: skin tone, status, and inequality. Sociol Compass. 2007;1(1):237–54. doi:10.1111/j.1751-9020.2007.00006.x.
Klonoff EA, Landrine H. Is skin color a marker for racial discrimination? explaining the skin color–hypertension relationship. J Behav Med. 2000;23(4):329–38. doi:10.1023/A:1005580300128.
Frank R, Akresh IR, Lu B. Latino immigrants and the U.S. racial order: how and where do they fit in? Am Sociol Rev. 2010;75(3):378–401.
Monk EP Jr. Skin tone stratification among Black Americans, 2001–2003. Soc Forces. 2014;sou007. doi:10.1093/sf/sou007.
Gravlee CC, Dressler WW, Bernard HR. Skin color, social classification, and blood pressure in southeastern Puerto Rico. Am J Public Health. 2005;95(12):2191–7. doi:10.2105/AJPH.2005.065615.
Monk EP Jr. The cost of color: skin color, discrimination, and health among African–Americans. Am J Sociol. 2015;121(2):396–444. doi:10.1086/682162.
Armstead CA, Hébert JR, Griffin EK, Prince GM. A question of color: the influence of skin color and stress on resting blood pressure and body mass among African American women. J Black Psychol. 2014;40(5):424–50. doi:10.1177/0095798413494404.
Klag MJ, Whelton PK, Coresh J, Grim CE, Kuller LH. The association of skin color with blood pressure in US Blacks with low socioeconomic status. JAMA. 1991;265(5):599–602. doi:10.1001/jama.1991.03460050053019.
Perreira KM, Telles EE. The color of health: skin color, ethnoracial classification, and discrimination in the health of Latin Americans. Soc Sci Med. 2014;116(0):241–50. doi:10.1016/j.socscimed.2014.05.054.
Vargas ED, Sanchez GR, Kinlock BL. The enhanced self-reported health outcome observed in Hispanics/Latinos who are socially-assigned as White is dependent on nativity. J Immigr Minor Health. 2014;1–8. doi:10.1007/s10903-014-0134-4.
Ayers SL, Kulis S, Marsiglia FF. The impact of ethnoracial appearance on substance use in Mexican heritage adolescents in the southwest United States. Hisp J Behav Sci. 2013;35(2):227–40. doi:10.1177/0739986312467940.
Brownstein N, Kalsbeek WD, Tabor J, Entzel P, Daza E, Harris KM. Non-response in wave IV of the national longitudinal study of adolescent health. Chapel Hill, NC: Carolina Population Center, University of North Carolina; 2011. http://www.cpc.unc.edu/projects/addhealth/data/guides/W4_nonresponse.pdf.
Dunteman GH. Principal components analysis. Vol. 69. Newbury Park, CA: Sage Publications; 1989.
Krieger N, Smith K, Naishadham D, Hartman C, Barbeau EM. Experiences of discrimination: validity and reliability of a self-report measure for population health research on racism and health. Soc Sci Med. 2005;61(7):1576–96. doi:10.1016/j.socscimed.2005.03.006.
Hardie JH, Lucas A. Economic factors and relationship quality among young couples: comparing cohabitation and marriage. J Marriage Fam. 2010;72(5):1141–54. doi:10.1111/j.1741-3737.2010.00755.x.
Chen P, Chantala K. Guidelines for analyzing add health data. Chapel Hill, NC: Carolina Population Center, University of North Carolina at Chapel Hill; 2014.
McEwen BS, Lasley EN. The end of stress as we know it. Washington, DC: Joseph Henry Press; 2004.
Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7(7):e1000316. doi:10.1371/journal.pmed.1000316.
Telles EE, Steele L. Pigmentocracy in the Americas: how is educational attainment related to skin color. Nashville, TN: Vanderbilt University; 2012. http://www.vanderbilt.edu/lapop/insights/IO873en.pdf. Accessed 27 May 2015.
Acknowledgments
The funding were provided by UNC Gillings School of Public Health and National Institute of Child Health and Human Development (US) (Grant No. T32 HD007168 and R24 HD050924).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wassink, J., Perreira, K.M. & Harris, K.M. Beyond Race/Ethnicity: Skin Color and Cardiometabolic Health Among Blacks and Hispanics in the United States. J Immigrant Minority Health 19, 1018–1026 (2017). https://doi.org/10.1007/s10903-016-0495-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-016-0495-y