Abstract
The adherence to the CDC guideline on screening non-U.S. born persons for hepatitis B virus infection was assessed. A retrospective cohort study was conducted at University of Washington primary care clinics using the electronic medical records. Persons from hepatitis B virus prevalent countries were identified using country of origin and language. Of 2329 eligible for screening, only 617 (26.5%) were screened. The prevalence of HBsAg was 35 (5.7%). Among women of reproductive age (18–44 years, n = 906), 238 (26.3%) were screened, and 7 (2.9%) were HBsAg positive. Low screening practice for chronic hepatitis B infection, and high infection prevalence among those screened was noted. The findings indicate that potentially three out of every one detected case may be missed. Urgent efforts are needed to scale up and consistently implement HBV screening at primary care clinics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2015, an estimated 257 million people were living with chronic hepatitis B (HBV) infection, the majority of whom reside in low-and-middle-income countries (LMICs), particularly in Africa and Asia [1,2,3,4]. Because most individuals with chronic HBV infection are asymptomatic, many remain undiagnosed, and the World Health Organization (WHO) estimates that only 9% of persons living with chronic HBV have received a diagnosis [1]. Due to an ongoing lack of timely diagnosis among many individuals with chronic HBV, HBV-related hepatocellular carcinoma (HCC), as well as cirrhosis and its complications remain significant causes of morbidity and mortality worldwide [1, 5].
In the United States (U.S.), the majority of persons living with chronic HBV are foreign-born. Despite guidance, issued in 2008, from the U.S. Centers for Disease Control and Prevention (CDC) recommending one-time HBV screening for persons born in countries with an HBV prevalence ≥ 2% [6], data indicate that adherence to screening guidelines for non-U.S. born individuals remains low, particularly in primary care [7,8,9,10].
In Seattle and King County, Washington, more than 22% of residents are non-U.S. born, many of whom immigrated from countries in Southeast Asia and Eastern African, where hepatitis B surface antigen (HBsAg) seroprevalence often exceeds 8% [2, 9,10,11]. The proportion of individuals from HBV-endemic countries who have been screened for chronic HBV is not known. In this study, we estimated the proportion of individuals from intermediate (≥ 2%) and high (≥ 8%) HBV prevalence countries who were screened for chronic HBV at University of Washington (UW) affiliated primary care clinics between 2016 and 2019, and evaluated factors associated with HBV screening in this population.
Methods
Study design and population
We completed a retrospective cohort analysis of HBV screening among patients receiving care at all UW affiliated primary care clinics. The study population included individuals ≥ 18 years of age, originating from intermediate or high HBV-endemic countries, defined by the WHO and CDC as those with an HBsAg seroprevalence ≥ 2% [12]. Individuals were included in the analysis if they established care at one of the UW primary care clinics in the year 2016, and if they had at least one additional follow-up visit by the end of 2019. Birthplace and preferred spoken language, as documented in the electronic medical record system (EMR), were used to determine eligibility criteria by country of origin. Individuals with documented HBV screening results (HBsAg or HBV DNA testing) prior to 2016 were excluded from our cohort.
Data collection, variables, and analysis
Demographic information and laboratory values were extracted from the EMR for all patients who met the inclusion criteria. Key variables of interest included: HBsAg, HBV DNA, age, sex, race, ethnicity, clinic site (grouped into categories based on hospital and network), number of clinic encounters and health insurance status.
Our main outcome of interest was screening for chronic HBV infection, defined as receipt of a HBsAg test anytime during the study period (2016 and 2019). For patients who were found to be HBsAg-positive, we evaluated the proportion who underwent liver function testing or liver imaging (Ultrasound or CT scan), as well as the proportion linked to HBV specialty care, defined as completion of a hepatology clinic visit. HBV screening and linkage to care was similarly evaluated among women of reproductive age within our cohort, defined as women between the ages of 18 and 44 years.
Descriptive statistics were used to compare patients who had and had not received HBV screening. Wald Chi-square test was used to identify correlates and calculate relative risk ratios (RR) of HBV screening along with 95% confidence intervals for all study participants and among the subgroup of reproductive age women. Analyses were performed using R (version 4.0.3, Vienna, Austria).
This study was approved by the human subjects division at the University of Washington.
Results
We identified 2473 patients from intermediate to high HBV prevalence countries who established care across 42 UW primary care clinics in 2016 and had at least one additional clinic visit by the end of 2019. Of these, 144 were excluded due to prior HBsAg or HBV DNA testing, resulting in an analytic cohort of 2329 (Fig. 1).
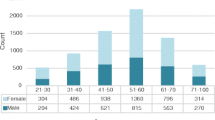
Demographic characteristics are outlined in Table 1. The median age of the study population was 36 years (interquartile range [IQR]: 25–57); 62% (n = 1446) were female, 63% (n = 1455) Asian/Pacific Islanders and 15% (n = 354) Black persons. HBsAg screening was performed in 617 of 2329 (26.5%) individuals during the timeframe of interest, and 35 (5.7%) were found to be HBsAg positive. Most of the patients were screened in their first year (2016) of establishing care, 414/617 (67.1%). Among women of reproductive age (n = 906), 26.3% (n = 238) were screened for HBsAg, and 2.9% (n = 7) were HBsAg positive (Supplementary table 1).
In a univariate analysis, individuals who were Black (RR 2.07, 95% confidence interval [CI] 1.81–2.37, p < 0.001), without health insurance, or identified as self-paying or receiving charity assistance (RR 1.38, 95% CI 1.21–1.58, p < 0.001), and those seen at one of the clinics affiliated with the county hospital (Harborview) (RR 3.02, 95% CI 2.66–3.43, p < 0.001) were more likely to have undergone screening for HBV. Additionally, patients with a higher number of clinic visits during the study period were more likely to have been screened for HBV when compared with those with fewer clinic visits (median of 8 vs. 4 clinic visits, p < 0.001). (Table 2 and Supplementary Table 2).
Of the 35 patients found to have chronic HBV infection, 31 (88.6%) had follow up liver aminotransferase testing and 26 (74.3%) had liver imaging studies. Twenty (57.1%) were subsequently evaluated in hepatology clinic, and 9 (25.7%) received treatment during the study period (Table 3).
Discussion
Despite guidelines from the CDC recommending one-time screening for all persons born in countries with a ≥ 2% prevalence for HBV, we found that only a quarter of the 2329 eligible patients were screened for chronic HBV in this contemporary primary care cohort.
Our findings are in keeping with other published studies, which have shown that provider adherence to accepted national guidelines for health screening and vaccination recommendations among immigrant and refugee populations is generally low within the U.S. [13]. Specifically, screening rates for chronic hepatitis B infection among non-U.S. born persons have been reported as low as 7–36% in the literature, including in an academic primary care setting [14,15,16]. A study from Mayo Clinic Rochester indicated that only 31% of Asian Americans were screened for chronic HBV infection at their health center, with screening mostly occurring during pregnancy, pre-employment evaluations, and rarely in the setting of routine primary care [15]. In a similar study from the Mayo Clinic, authors found a baseline HBV screening rate of 7.2% within primary care, which increased to 31.4% after providers were sent reminder emails regarding HBV screening a week prior to scheduled visits with eligible patients [14]. Collectively, the findings, paired with our current study, suggest that HBV screening is not consistently implemented in most primary care practices, and many cases of chronic infection are likely going undiagnosed. Majority of the screening occurred on initial visit when the patients established care. This might be because of relatively longer time allotted for initial patient visits allowing more patient-physician contact than subsequent follow up visits.
The prevalence of HBV among screened individuals in our study was 5.7%. This is consistent with the prevalence of chronic HBV in intermediate and high prevalence countries, including countries with a large immigrant population in King County such as Vietnam, China, Philippines, and Ethiopia [1]. Comparably high rates of HBV infection have also been described among foreign-born individuals in studies from other high-income countries such as Canada (5.4%) [3], Germany (3.6%) [4], Italy (9.6%) [16], as well as in other cities/states within the US such as Baltimore (3.7%-6.1%) [17] and Minnesota (8.5%) [15]. If this HBV prevalence held true for our clinic population as a whole, there were potentially as many as 133 (5.7% of 2329) individuals with chronic HBV that could have been identified. Current screening practices may have resulted in as many as 98 missed chronic HBV diagnoses.
Perinatal transmission is the main route of HBV transmission in endemic areas, and as such, screening women of reproductive age for HBV infection is a crucial step in HBV prevention and linkage to care [18]. In this study, the proportion of reproductive age women who were screened for chronic HBV was similarly low (26.3%). Nevertheless, the prevalence of the infection among reproductive aged women was lower, 2.9%, when compared to the total population. While the reasons for this are not addressed in this study, owing to their younger age, it is possible that women of reproductive age were more likely than older women to have been vaccinated against HBV at birth or in early childhood.
While the overall proportion of patients screened for HBV in our study was low, a few groups were more likely to be screened than others; although no subgroup had a screening rate higher than 50%. These included Black persons and uninsured individuals. The reasons for this cannot be ascertained by our study data; however, it is possible that some of the providers had higher awareness of HBV prevalence among African-born persons when compared to other similarly at-risk groups, or that systemic racial bias contributes to altered perceptions of patients’ risk for certain infectious diseases. Unfortunately, we did not come across similar studies addressing this issue or preferential screening among persons of different races. The presence of a dedicated clinic for international communities at Harborview Medical Center, King County’s public hospital, which is run by UW, may also account for higher rates of HBV screening among county hospital clinics and among uninsured individuals, as a higher proportion of patients seen within Harborview’s primary care clinics are uninsured, when compared to other primary care clinics across the UW system [9].
It is perhaps not surprising that patients screened for HBV were more likely to have a greater number of clinic visits during the timeframe of interest (median of 8 versus 4). Patients with more frequent clinic visits might have been sicker and had greater opportunity to undergo screening for infections including HBV. It is probable that the increased frequency of physician–patient contacts facilitated more complete health care maintenance plans. Nevertheless, it is notable that the median number of clinic visits for patients not screened was four, i.e., a follow-up rate of approximately once a year for this cohort. This finding further accentuates that guideline-based HBV screening has been inadequately incorporated into routine primary care, as yearly follow-up over the course of four years should have provided sufficient time to complete routine infectious diseases screening.
Patients with HBV infection need regular lifelong follow up because they are at increased risk of progression to liver cirrhosis and hepatocellular cancer [19]. While most patients diagnosed with chronic HBV in this cohort were subsequently followed in their primary clinic with liver enzymes and imaging, linkage to hepatology clinic was only completed by 20 (57%). It is important to note, however, that immediate referral to specialty care may not be necessary, as specialty care needs depend on the stage of chronic HBV, and the proportion of patients linked to care in our study is relatively consistent with that of HBV infected patients from other domestic studies, including cohorts from Denver (29% linked to care) and Philadelphia (53% linked to care) [20]. However, the importance of regular follow up, monitoring of disease activity as well as health education, which can be done at primary care level, cannot be over emphasized. Adherence to longitudinal monitoring of patients with chronic HBV at the provider level is particularly important given several studies which indicate low awareness regarding HBV transmission and care needs among immigrant communities [2, 11, 14, 21].
There are certain limitations worth noting in our study. Birthplace and primary language were not always complete in the medical record system and we may have missed certain groups of eligible patients, including English speakers originating from countries of high HBV prevalence. Additionally, patients who were screened for HBV in other healthcare settings might have been misclassified as unscreened in this study due to our inability to access outside facility records. We required that patients have a minimum of two clinic visits during the intended study period for this study. This was taking into consideration that all the routine healthcare screening tests (including the HBV screening) might not be completed on a single visit, but this might have introduced some selection bias into our sample. Finally, these data come from a single healthcare system and may not be generalizable to other clinical settings.
Conclusions
This study found a low frequency of screening and high prevalence of chronic HBV infection among people from HBV endemic countries seen in a network of primary care clinics. For each diagnosed hepatitis B case, potentially three cases were missed within our cohort. There is an urgent need to prioritize, scale up and consistently implement HBV screening among persons from intermediate to high HBV prevalent countries to prevent the transmission and long-term complications of chronic HBV infection. Additional efforts are needed to understand how best to simplify, implement and adhere to HBV screening guidelines within primary care.
Data availability
The author confirms that all data generated or analysed during this study are included in this article.
Code availability
Not applicable.
References
World Health Organization. Global hepatitis report, (2017). Geneva; 2017. Retrieved March 21, 2020, from https://creativecommons.org/%0Alicenses/by-nc-sa/3.0/igo
Upadhyaya, N., Chang, R., Davis, C., Conti, M. C., Salinas-Garcia, D., & Tang, H. (2010). Chronic hepatitis B: Perceptions in Asian American communities and diagnosis and management practices among primary care physicians. Postgraduate Medicine, 122(5), 165–175.
Pottie, K., Janakiram, P., Topp, P., & McCarthy, A. (2007). Prevalence of selected preventable and treatable diseases among government-assisted refugees: Implications for primary care providers. Canadian Family Physician, 53(11), 1928–1934.
Heidrich, B., Cetindere, A., Beyaz, M., et al. (2014). High prevalence of hepatitis markers in immigrant populations: A prospective screening approach in a real-world setting. European Journal of Gastroenterology and Hepatology, 26(10), 1090–1097.
McMahon, B. J., Block, J., Haber, B., et al. (2012). Internist diagnosis and management of chronic hepatitis b virus infection. The American Journal of Medicine, 125(11), 1063–7. https://doi.org/10.1016/j.amjmed.2012.03.010
Weinbaum, C. M., Williams, I., Mast, E. E., et al. (2008). Recommendations for identification and public health management of persons with chronic hepatitis B virus infection. MMWR Recommendations and Reports, 57(RR-8), 1–20.
Foster, T., Hon, H., Kanwal, F., Han, S., & Spiegel, B. (2011). Screening high risk individuals for hepatitis B: Physician knowledge, attitudes, and beliefs. Digestive Diseases and Sciences, 56(12), 3471–3487.
Liu, C. Y., Chandrasekar, P. H., Masood, A., & Schiffer, C. A. (2013). Adherence to hepatitis B screening and prophylactic lamivudine for prevention of rituximab-associated hepatitis B reactivation. Journal of Oncology Pharmacy Practice, 19(1), 18–23.
Terasaki, G., Desai, A., McKinney, C. M., & Haider, M. Z. (2017). Seroprevalence of hepatitis B infection among immigrants in a primary care clinic: A case for granular ethnicity and language data collection. Journal of Immigrant and Minority Health, 19(4), 987–990.
Burke, N. J., Jackson, J. C., Thai, H. C., et al. (2004). “Honoring tradition, accepting new ways”: Development of a hepatitis B control intervention for Vietnamese immigrants. Ethnicity & Health, 9(2), 153–169.
Chu, J. N., Le, P. V., Kennedy, C. J., et al. (2017). Factors associated with hepatitis B knowledge among Vietnamese Americans: A population-based survey. Journal of Immigrant and Minority Health, 19(4), 801–808.
World Health Organization D of communicable diseases surveillance and response.(2020). Hepatitis. WHO/CDS/CSR/LYO/2002.2:Hepatitis B. Retrieved August 20, 2020, from http://www.who.int/emc
Waldorf, B., Gill, C., & Crosby, S. S. (2014). Assessing adherence to accepted national guidelines for immigrant and refugee screening and vaccines in an urban primary care practice: A retrospective chart review. Journal of Immigrant and Minority Health, 16(5), 839–845.
Eneh, P. N., Mady, M., Schmidt, M. A., et al. (2021). Hepatitis B screening of at-risk immigrants seen at primary care clinics: A quality improvement project. Mayo Clinic Proceedings: Innovations, Quality & Outcomes, 5(3), 635–44. https://doi.org/10.1016/j.mayocpiqo.2021.04.002
Loo, N. M., Kim, W. R., Larson, J. J., Wieland, M. L., & Chaudhry, R. (2012). Hepatitis B screening in a US academic primary care practice. Archives of internal medicine, 172(19), 1517. https://doi.org/10.1001/archinternmed.2012.3647
Coppola, N., Alessio, L., Gualdieri, L., et al. (2017). Hepatitis B virus infection in undocumented immigrants and refugees in Southern Italy: Demographic, virological, and clinical features. Infectious Diseases of Poverty, 6(1), 1–9. https://doi.org/10.1186/s40249-016-0228-4
Juon, H. S., Ha, E., Kim, F., Trang, A., Pan, J., & Blanchard, J. (2019). Prevalence of viral hepatitis in foreign-born populations in the Baltimore-Washington Metropolitan area, 2009–2015. Journal of Community Health, 44(2), 203–207.
Nelson, N. P., Jamieson, D. J., & Murphy, T. V. (2014). Prevention of perinatal hepatitis B virus transmission. Journal of the Pediatric Infectious Diseases Society, 3(SUPPL1), 7–12.
McMahon, B. J. (2014). Chronic hepatitis B virus infection. Medical Clinics of North America, 98(1), 39–54. https://doi.org/10.1016/j.mcna.2013.08.004
Young, J., Payton, C., Walker, P., et al. (2020). Evaluation of a program to improve linkage to and retention in care among refugees with hepatitis B virus infection—three US cities, 2006–2018. MMWR. Morbidity and Mortality Weekly Report, 69(21), 647–650.
Freeland, C., Bodor, S., Perera, U., & Cohen, C. (2020). Barriers to hepatitis B screening and prevention for African immigrant populations in the United States: A qualitative study. Viruses, 12(3), 305.
Funding
No funds, grants or other support was received.
Author information
Authors and Affiliations
Contributions
ED and HNK: Conceptualization and protocol development. AG and HNK: data collection. ED, HNK, MAC, KL: study design and data analysis. All the authors contributed to interpretation of results. ED: drafted the first manuscript. All authors contributed to reviewing, preparing and approving the final draft for publication.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Ethical approval
This study was approved by the human subjects division at the University of Washington.
Consent to participate
Not applicable, retrospective record analysis.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Diro, E., Corcorran, M.A., Lan, K. et al. Adherence to chronic hepatitis B screening guidelines for persons from intermediate to high prevalence Countries. J Community Health 47, 704–709 (2022). https://doi.org/10.1007/s10900-022-01102-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-022-01102-7