Abstract
Prenatal care coordination programs direct pregnant Medicaid beneficiaries to medical, social, and educational services to improve birth outcomes. Despite the relevance of service context and treatment level to investigations of program implementation and estimates of program effect, prior investigations have not consistently attended to these factors. This study examines the reach and uptake of Wisconsin’s Prenatal Care Coordination (PNCC) program among Medicaid-covered, residence occurrence live births between 2008 and 2012. Data come from the Big Data for Little Kids project, which harmonizes birth records with multiple state administrative sources. Logistic regression analyses measured the association between county- and maternal-level factors and the odds of any PNCC use and the odds of PNCC uptake (> 2 PNCC services among those assessed). Among identified Medicaid-covered births (n = 136,057), approximately 24% (n = 33,249) received any PNCC and 17% (n = 22,680) took up PNCC services. Any PNCC receipt and PNCC uptake varied substantially across counties. A higher county assessment rate was associated with a higher odds of individual PNCC assessment but negatively associated with uptake. Mothers reporting clinical risk factors such as chronic hypertension and previous preterm birth were more likely to be assessed for PNCC and, once assessed, more likely to received continued PNCC services. However, most mothers reporting clinical risk factors were not assessed for services. Estimates of care coordination’s effects on birth outcomes should account for service context and the treatment level into which participants select.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Women who are poor, less educated, and/or Black are more likely to experience adverse pregnancy outcomes, including infant death, than their more affluent, educated, and White peers [1,2,3]. Despite decades of scholarly attention and targeted policy changes, disparities in birth outcomes persist and—in some cases—appear to be worsening [4,5,6]. Thus, the development, implementation, and evaluation of programs designed to reduce adverse birth outcomes and disparities therein remains a national priority [7].
Care coordination programs are among the strategies that state Medicaid (MA) agencies have adopted to improve birth outcomes [8,9,10]. While care coordination is widely viewed as a promising strategy for supporting maternal and infant health [11], barriers to accurately estimating program effects remain.
This paper contextualizes extant estimates of care coordination’s effect on birth outcomes by examining variation in the reach and uptake of Wisconsin’s Prenatal Care Coordination (PNCC) program. PNCC, which was initiated in 1993 and connects pregnant women to medical, educational, and social services [12], provides a good case example for this exercise. Wisconsin’s PNCC assessment is intended to be universally implemented among MA-covered women and was designed so that most women meet eligibility criteria [13]. Wisconsin is also home to some of the largest Black-White racial health disparities in the nation [14] and is characterized by extremes of variation in geographic rurality, racial/ethnic segregation, and health care infrastructure. Finally, PNCC is primarily managed by providers at the county level (e.g., county health departments), thus allowing for within-state service context variation.
Prenatal Care Coordination Programs: A Brief History and Summary of Evidence
In the late 1980s, federal and state authorities asserted the advantageous effects of early and comprehensive prenatal care on birth outcomes and initiated policy changes that expanded prenatal care access. These changes came largely in the form of broadening the reach and scope of MA-covered care among pregnant women, including funding care coordination programs during the prenatal and postpartum periods. Although these programs vary by state, the broad purpose of prenatal care coordination is to connect pregnant women to health-promoting information and services [8,9,10].
Early evaluations of prenatal care coordination’s effect on birth outcomes produced mixed results. Some studies indicated that state programs reached the intended population and improved birth outcomes, while others reported conflicting conclusions [15,16,17,18,19]. Aside from Reichman and Florio [19], who used instrumental variable techniques to examine the effects of an enriched prenatal care program on birth outcomes in New Jersey, a majority of early studies did not sufficiently address selection bias, however. Because women who receive care coordination services are likely to differ in important and systematic ways from women who do not, simply comparing recipients to non-recipients will result in biased estimates.
To address this problem, researchers have increasingly turned to quasi-experimental methods that allow for more accurate definitions of untreated comparison groups. To date, researchers have used propensity score analysis to investigate state care coordination programs in Iowa, North Carolina, and Michigan. Specifically, Slaughter et al. used propensity score analysis to examine the effects of Iowa’s prenatal case management (PCM) program on 2005–2006 birth outcomes [20]. They found that while a dichotomous indicator of PCM receipt was not associated with prematurity or birthweight, receiving a moderate to high amount of PCM services (defined according to length, breadth, and contact time of services) was associated with lower rates of premature birth and LBW. Similarly, Hillemeier et al. used 2008–2010 MA birth data and propensity score analysis to examine North Carolina’s maternity care coordination (MCC) program [21, 22]. They found that MCC was associated with more prenatal care as well as a 20% reduction in the preterm birth rate, but was not associated with birthweight. Finally, Meghea et al. and Roman et al. used 2009–2011 MA birth data and propensity score analysis to examine the effects of Michigan’s Maternal and Infant Health Program (MIHP) on health care receipt and birth outcomes [23,24,25]. MIHP was associated with higher rates of prenatal care and lower rates of prematurity and LBW, and its impact extended past delivery: MIHP was associated with higher rates of well-child visits and injury-related health care visits among children in the first year of life.
Although quasi-experimental analysis has improved rigor in terms of estimating program effects, methods that correct for selection bias rely on (1) modeling all selection factors and (2) appropriately identifying the treatment condition upon which to model the selection process. Risk for adverse birth outcomes is usually described in terms of mothers’ characteristics, so most studies have adjusted for individual-level factors associated with service receipt. However, care coordination services are not determined by maternal characteristics alone. A long history of research documenting healthcare service variation by contextual factors, including service supply [26], demonstrates that context (i.e. place) often plays a role in service receipt and related outcomes. Nonetheless, researchers have not consistently investigated care coordination program reach or accounted for how context affects uptake (exceptions include Reichman and Florio [19], Hillemeier et al. [21, 22]). Overlooking contextual variation is relevant when, for example, researchers examine the effect of a statewide care coordination program in a state characterized by within-state (e.g., county-level) differences in program infrastructure.
Prior research has also not consistently attended to whether the factors that predict assessment for services differ from those that predict service uptake. This oversight is notable because defining treatment in terms of assessment is likely to identify a comparison group that differs from the group that would be identified if treatment was defined as, for example, taking up ongoing services. Context matters here as well: care coordination programs in some settings may be better at reaching and assessing pregnant women than they are at engaging women in ongoing services, whereas the opposite may be true in other settings. Overlooking such distinctions could result in misidentifying a comparison group and thus misestimating a program’s effectiveness.
Methods
Sample
Data for this study come from the Big Data for Little Kids (BD4LK) project, which merges and harmonizes data from multiple administrative sources. This study’s dataset includes: (1) all Wisconsin resident in-state birth records from 2007 to 2012; (2) Medicaid (MA) claims and encounters (hereafter “claims”) associated with mother–infant dyads; (3) social program participation data and employment earnings between 2005 and 2015 drawn from the Multi-Sample Person File (MSPF) [27]; and (4) county- and zip code-level contextual information from public data sources (described below). We limited our sample to MA-covered births between 2008 and 2012 because we could not account for PNCC receipt prior to 2007, and to births to women covered by non-emergency forms of MA at delivery because these women were most likely eligible for PNCC.
Dataset construction involved several stages of matching. First, each child’s birth record was matched to a unique mother in the MSPF. Approximately 70% of all mothers matched to an MSPF record, reflecting the fact that a sizable proportion of mothers and/or their children were involved in the social programs and types of employment monitored in the MSPF (e.g., unemployment insurance). Because MA and the MSPF rely on similar identification strategies, nearly 99% of mothers and children with MA claims matched uniquely to an MSPF record.
Duplicate observations occurred in a small number of cases (n = 1136, or < 1% of births), which we handled by randomly selecting one duplicate and dropping all others. We used list-wise deletion to manage the small amount of missing data on other variables of interest (n = 1567 or 1.14% of births), resulting in a final sample size of 136,057 births.
Measures
PNCC Services
We measured PNCC using MA codes indicating a paid PNCC service claim associated with a specific birth. We recorded claim type (i.e. assessment [H1000], care plan [H1002 U2 until October 1, 2012 and H1002 thereafter], education [H1003], home visit [H1004], case management [H1002 until October 1, 2012 and T1016 TH thereafter]) and defined PNCC receipt in two ways: (1) any PNCC (0 = none; 1 = any); and (2) PNCC uptake (0 = PNCC assessment and/or care plan only; 1 = assessment, care plan, and at least one additional service).
County Characteristics
PNCC in Wisconsin is primarily managed by county entities, making mothers’ residence county a natural level of aggregation to examine contextual effects. We used data from the Health Resources and Service Administration (HRSA) warehouse [28] to characterize county urbanicity by Core-Based Statistical Area (CBSA) status [29], whether the county was a primary medical care Health Professional Shortage Area (HPSA) during the year of birth, the number of obstetrics and gynecology physicians per 1000 live births in 2010, and the presence of Federally Qualified Health Centers (FQHC) and/or Rural Health Clinics (RHC) in 2010 (categorical variable, 0 = no FQHC or RHC; 1 = FQHC or RHC; 2 = both FQHC and RHC). We also considered measures of social context, including the child poverty rate in 2010, the percentage of Black residents in 2010, and the percentage of adults with less than a high school education in 2010–2014 (averaged). Finally, we documented yearly county fertility rates using the Wisconsin Interactive Statistics on Health database [30].
Maternal and Household Characteristics
We drew mothers’ sociodemographic characteristics (i.e. age, education, race/ethnicity, marital status, and nativity status) and clinical characteristics (i.e. parity, plurality, previous preterm birth, cigarette use during pregnancy, chronic hypertension, and prepregnancy diabetes) from birth records. We used the MSPF to construct a measure of each woman’s income (wage earnings and other forms of monetary income, such as child support) during the year spanning 18 months prior to birth to 6 months prior to birth. Lastly, we used the MSPF to generate an indicator of a woman’s receipt of any Supplemental Nutrition Assistance Program (SNAP) benefits in the 6 months prior to the child’s estimated conception date (defined using a child’s birth date and the physician’s estimate of gestational age at birth).
Analytic Approach
After summarizing bivariate differences and county- and individual-level characteristics by PNCC status, we estimated a series of descriptive logistic regression models estimating the odds of a mother (1) receiving any PNCC service, relative to no services and (2) taking up PNCC (i.e. receiving services beyond assessment and a care plan), conditional on being assessed. We estimated these models in two steps, first regressing individual-level PNCC participation on county-level factors, and then adding individual characteristics. All analyses were completed using Stata Statistical Software, version 15 [31] and all study procedures were approved by the University of Wisconsin-Madison's Minimal Risk Institutional Review Board.
Results
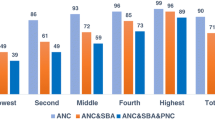
Summary statistics show that few mothers participated in PNCC between 2008 and 2012 and that PNCC receipt varied considerably across counties (see Fig. 1; Table 1). Approximately 25% of MA-covered mothers received any PNCC, and this percentage varied by county of residence, from < 5% to > 60%. The proportion of assessed mothers who took up PNCC also varied by county, from < 25% to > 90%. Statewide, roughly 17% of MA-covered mothers were assessed for and took up PNCC between 2008 and 2012.
Rates of PNCC participation remained relatively stable across years (see Table 1). The PNCC assessment rate was highest in metropolitan counties, and uptake among those assessed was highest in non-CBSA (i.e. rural) counties. The assessment rate was also higher in higher-poverty counties as well as in counties where > 5% of the population was Black.
Results from logistic models that regressed individual-level PNCC receipt on county characteristics show few significant associations between county factors and the odds of receiving any PNCC or the odds of uptake (results not shown), with one exception. The county-level PNCC assessment rate during the year of birth (i.e. percent any PNCC) was associated with the odds of PNCC receipt: each 1% increase in the county assessment rate was associated with an approximately 5% higher odds of a mother being assessed for PNCC (odds ratio [OR] 1.05; confidence interval [CI] 1.05–1.06), and an approximately 4% lower odds of taking up services (OR 0.96; CI 0.95–0.98).
The significant associations between the county PNCC assessment rate and PNCC receipt remained robust to conditioning on maternal characteristics (see Figs. 2, 3). In line with previous research examining the association between maternal characteristics and care coordination receipt, younger, less educated, lower income, Black, Hispanic, unmarried, first-time mothers, and mothers reporting clinical risk factors were more likely to receive any PNCC and, once assessed, more likely to take up services.
Forest plot displaying the odds of any PNCC receipt by mothers’ residence county and maternal characteristics. n = 136,057, Pseudo R2 = 0.163. Estimated odds ratios and 95% confidence intervals displayed. The model includes year fixed effects. Standard errors clustered by mothers’ residence county. PNCC Prenatal Care Coordination, HS high school, NH non-Hispanic, AI American Indian, AN Alaskan native, SNAP Supplemental Nutrition Assistance Program. Reference (“ref.”) groups: CBSA ref. “non-CBSA”; HPSA ref. “not HPSA, year of birth”; FQHC/RHC ref. “no FQHC or RHC, 2010”; child poverty ref. “0–10% child poverty”; % Black ref. “Black < 5%, 2010”; age ref. “20–29 years”; education ref. “HS grad/GED”; race/ethnicity ref. “White NH”; unmarried ref. “married”; foreign-born ref. “native-born”; SNAP receipt ref. “no SNAP receipt”; first birth ref. “second or later birth”; plural birth ref. “single birth”; previous preterm birth ref. “no previous preterm birth”; tobacco use ref. “no tobacco use reported”; chronic hypertension ref. “no chronic hypertension reported”; prepregnancy diabetes ref. “no prepregnancy diabetes reported”. Note to Editors: Excel forest plot file available upon request
Forest plot displaying the odds of PNCC uptake (> 2 services among those assessed) by mothers’ residence county and maternal characteristics. n = 33,249, Pseudo R2 = 0.159. Estimated odds ratios and 95% confidence intervals displayed. The model includes year fixed effects. Standard errors clustered by mothers’ residence county. PNCC Prenatal Care Coordination, HS high school, NH non-Hispanic, AI American Indian, AN Alaskan native, SNAP Supplemental Nutrition Assistance Program. Reference (“ref.”) groups: CBSA ref. “non-CBSA”; HPSA ref. “not HPSA, year of birth”; FQHC/RHC ref. “no FQHC or RHC, 2010”; child poverty ref. “0–10% child poverty”; %Black ref. “Black <5%, 2010”; age ref. “20–29 years”; education ref. “HS grad/GED”; race/ethnicity ref. “White NH”; unmarried ref. “married”; foreign-born ref. “native-born”; snap receipt ref. “no snap receipt”; first birth ref. “second or later birth”; plural birth ref. “single birth”; previous preterm birth ref. “no previous preterm birth”; Tobacco use ref. “no tobacco use reported”; chronic hypertension ref. “no chronic hypertension reported”; prepregnancy diabetes ref. “no prepregnancy diabetes reported. Note to Editors: Excel forest plot file available upon request
Figure 3 also shows that the strongest predictor of PNCC uptake was Black non-Hispanic race/ethnicity. Many studies have acknowledged the important role of race and ethnicity in care coordination programs, particularly when programs are designed to address racial disparities in birth outcomes, [19, 23,24,25] and our finding that Black non-Hispanic mothers were more likely to participate in PNCC aligns with this literature. It is important to note, however, that Black mothers in Wisconsin are highly geographically concentrated. More than 75% of Black mothers live in Milwaukee County and an additional 20% live in five other primarily southeastern counties, leaving 5% of Black mothers in the balance of the state. To investigate the stability of the association between race/ethnicity and PNCC receipt, we completed subgroup analyses, dividing the sample by (1) residence in the six counties with the highest concentration of Black mothers and (2) residence in the balance of the state.
Results of the subgroup analyses align with results from the full sample (see Table 2), with a few notable exceptions. First, in the six counties with the highest concentration of Black mothers, Black non-Hispanic race/ethnicity was associated with a roughly 50% higher odds of receiving any PNCC and nearly three times the odds of PNCC uptake, relative to white non-Hispanic race/ethnicity. Outside of the six counties, however, Black mothers were not more likely to receive PNCC. Rather, Laotian/Hmong and Hispanic race/ethnicity was associated with a higher odds of receiving any PNCC, relative to white non-Hispanic race/ethnicity, and there was no difference in the odds of PNCC uptake by race/ethnicity among assessed mothers.
Furthermore, we found that the associations between parity, clinical risk, and PNCC receipt varied by county group. Outside of the six counties, first-time motherhood was associated with nearly three times the odds of receiving any PNCC, relative to second- or later pregnancies, compared to an approximately 50% higher odds inside the six counties. Whereas chronic hypertension and pre-pregnancy diabetes were not associated with the odds of receiving any PNCC in the six counties, mothers with either of these conditions who lived in the balance of the state experienced a 40% higher odds of being assessed for PNCC, relative to their peers.
Discussion
The reach of Wisconsin’s PNCC program between 2008 and 2012 was modest, and mothers’ receipt of PNCC depended on contextual and individual-level factors. We found that the county-level assessment rate was a consistent and stable correlate of individual-level PNCC receipt, controlling for a number of maternal and county characteristics, and that the county-level assessment rate was negatively associated with PNCC uptake. These findings imply that a mother’s residence county contributed to her likelihood of receiving PNCC, and in a manner such that a higher odds of being assessed was associated with a lower odds of taking up services.
We conjecture that these findings may reflect county-level differences in access to and/or prioritization of PNCC resources. For example, high assessment/low uptake counties may devote substantial resources to assessing the need for PNCC in the county population, but then target resources at mothers deemed at highest risk of adverse birth outcomes. Low assessment/high uptake counties, on the other hand, may target most of their resources at women they assume—prior to assessment—to be in most need. That our subgroup analyses show that the association between race/ethnicity, parity, clinical risk factors (i.e. chronic hypertension, prepregnancy diabetes), and the odds of PNCC participation differed by county group provides some support for this conjecture. That is, it is possible that counties differentially target assessment resources at mothers of color (e.g., Black, Hispanic, Laotian/Hmong mothers) and/or at first-time mothers because of some a priori determination of the mothers’ level of risk. The reasonableness of such targeting is not clear, however. In fact, that some counties appear to prioritize first-time mothers contradicts the PNCC assessment directives, which state that, “women with multiple previous pregnancies may have increased risks for a poor birth outcome” [13].
Our results also suggest that assuming identical determinants of selection into PNCC assessment and selection into PNCC uptake may produce inaccurate comparison groups and thus inaccurate estimates of program effect. We found that mothers reporting clinical risk factors were, on the whole, more likely to participate in PNCC, which aligns with previous work as well as program intent. The favorable nature of this finding is tempered by the fact that (1) most mothers reporting clinical and other risks were not assessed for PNCC and thus could not have taken up services and (2) the subgroup analyses revealed differences in the association between risk factors and PNCC receipt by county group. This pattern of findings raises concerns. First, if previous preterm birth is the strongest predictor of subsequent preterm birth [1], our results demonstrate that PNCC resources did not reach most of the mothers who were at pronounced risk of an adverse birth outcome between 2008 and 2012. Second, these findings call into question implementation fidelity and thus the validity of any estimates of program effect on individuals and populations. Finally, our results raise questions about whether methods such as propensity score analysis can sufficiently account for the host of selection processes that determine when and to whom assessment for care coordination services occurs, and thus who can take up services.
Limitations
This analysis was limited to in-state live births among Wisconsin resident mothers. As a result, we did not consider PNCC receipt among mothers who experienced a miscarriage or fetal death. We also were unable to distinguish between pregnancies that ended versus live births that occurred in a state other than Wisconsin, and so could not consider PNCC claims associated with out-of-state live births to Wisconsin residents. Our reliance on MA claims means that we were unable to determine the extent to which PNCC services were provided absent reimbursement.
We expect that our findings are relevant to other states, given that prior analyses found limited program enrollment [21] as well as geographic variation in service uptake [19]. Nonetheless, Wisconsin is likely characterized by idiosyncracies that preclude comprehensive generalization to other settings. The observational nature of our analysis does not allow for causal assertions, and the risk of omitted variable bias is pronounced as the documented variability in PNCC receipt across counties does not reflect the program’s formal intent or design.
Implications
Obtaining accurate estimates of a statewide care coordination program’s effect on birth outcomes requires careful model specification. Relying exclusively on maternal factors in propensity score models, for example, is likely insufficient. In fact, in states where care coordination implementation varies substantially within-state (e.g., across counties), as is the case in Wisconsin, the value of reporting statewide program effect estimates may be limited.
Scholars and practitioners have recognized the relevance of systems of care approaches in addressing adverse birth outcomes and disparities therein [32, 33]. The primary purpose of such approaches is to effectively approach resource constraints by matching high-risk mothers and infants to health care services that are capable of responding to their needs. A similar framing of care coordination services may be beneficial. Our results suggest that Wisconsin’s strategy of providing PNCC has historically been suboptimal, such that most mothers reporting risks were not assessed for or provided PNCC. The extent to which this was true varied across counties and for reasons that were not immediately clear. A systems approach, defined to match mothers’ needs to services, merits consideration, particularly if care coordination providers tend to operate amidst important resource constraints.
References
Butler, A. S., & Behrman, R. E. (Eds.), (2007). Preterm birth: Causes, consequences, and prevention. Washington, DC: National Academies Press.
Mathews, T. J., & MacDorman, M. F. (2013). Infant mortality statistics from the 2010 period linked birth/infant death data set. National Vital Statistics Report, 62(8), 1–26.
Schempf, A. H., Branum, A. M., Lukacs, S. L., & Schoendorf, K. C. (2007). The contribution of preterm birth to the black–white infant mortality gap, 1990 and 2000. American Journal of Public Health, 97(7), 1255–1260.
Martin, J. A., Hamilton, B. E., & Osterman, M. J. K. (2016). Births in the United States, 2015 (NCHS Data Brief, No 258). Hyattsville: National Center for Health Statistics.
MacDorman, M. F., & Mathews, T. J. (2008). Recent trends in infant mortality in the United States (NCHS Data Brief. No 9). Hyattsville: National Center for Health Statistics.
Riddell, C. A., Harper, S., & Kaufman, J. S. (2017). Trends in differences in US mortality rates between black and white infants. JAMA Pediatr, 171(9), 911–913.
Lu, M. C. (2014). Improving maternal and child health across the life course: Where do we go from here? Maternal and Child Health Journal, 18(2), 339–343.
Gallagher, J., Botsko, C., & Schwalberg, R. (2004). Influencing interventions to promote positive pregnancy outcomes and reduce the incidence of low birth weight and preterm infants. Washington, DC: Health Systems Research Inc.
Hill, I. T. (1990). Improving state Medicaid programs for pregnant women and children. Health Care Financing Review, 1990(Suppl), 75–87.
Van Dijk, J. W., Anderko, L., & Stetzer, F. (2011). The impact of prenatal care coordination on birth outcomes. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 40(1), 98–108.
Kroll-Desrosiers, A. R., Crawford, S. L., Simas, T. A. M., Rosen, A. K., & Mattocks, K. M. (2016). Improving pregnancy outcomes through maternity care coordination: A systematic review. Women’s Health Issues, 26(1), 87–99.
Wisconsin Department of Health Services. (2017). Prenatal care coordination. Retrieved from https://www.dhs.wisconsin.gov/mch/pncc.htm.
Wisconsin Department of Health Services. (2009). Forward health: Prenatal care coordination pregnancy questionnaire. Retrieved from https://www.forwardhealth.wi.gov/WIPortal/Subsystem/KW/Print.aspx?ia=1&p=1&sa=54&s=4&c=13&nt=Prenatal+Care+Coordination+Pregnancy+Questionnaire.
U.S. Department of Health and Human Services. (2017). 2016 national healthcare quality and disparities report. Rockville: Agency for Healthcare Research and Quality.
Middleton, B. H., Middleton, R., & Jakpor, K. M. (1992). Evaluation of the Wisconsin Prenatal Care Coordination projects. Madison: Wisconsin Department of Health & Social Services.
Baldwin, L. M., Larson, E. H., Connell, F. A., Nordlund, D., Cain, K. C., Cawthon, M. L., et al. (1998) The effect of expanding Medicaid prenatal services on birth outcomes. American Journal of Public Health, 88(11), 1623–1629.
Buescher, P. A., Roth, M. S., Williams, D., & Goforth, C. M. (1991). An evaluation of the impact of maternity care coordination on Medicaid birth outcomes in North Carolina. American Journal of Public Health, 81(12), 1625–1629.
Piper, J. M., Mitchel, E. F. Jr, & Ray, W. A. (1996). Evaluation of a program for prenatal care case management. Family Planning Perspectives. https://doi.org/10.2307/2136126.
Reichman, N. E., & Florio, M. J. (1996). The effects of enriched prenatal care services on Medicaid birth outcomes in New Jersey. Journal of Health Economics, 15(4), 455–476.
Slaughter, J. C., Issel, L. M., Handler, A. S., Rosenberg, D., Kane, D. J., & Stayner, L. T. (2013). Measuring dosage: A key factor when assessing the relationship between prenatal case management and birth outcomes. Maternal and Child Health Journal, 17(8), 1414–1423.
Hillemeier, M. M., Domino, M. E., Wells, R., Goyal, R. K., Kum, H.C., Cilenti, D., et al. (2015). Effects of maternity care coordination on pregnancy outcomes: Propensity-weighted analyses. Maternal and Child Health Journal, 19(1), 121–127.
Hillemeier, M. M., Domino, M. E., Wells, R., Goyal, R. K., Kum, H.C., Cilenti, D., et al. (2017). Does maternity care coordination influence perinatal health care utilization? Evidence from North Carolina. Health Services Research. https://doi.org/10.1111/1475-6773.12742.
Meghea, C. I., Raffo, J. E., Zhu, Q., & Roman, L. (2013). Medicaid home visitation and maternal and infant healthcare utilization. American Journal of Preventive Medicine, 45(4), 441–447.
Meghea, C. I., You, Z., & Roman, L. A. (2015). A statewide Medicaid enhanced prenatal and postnatal care program and infant injuries. Maternal and Child Health Journal, 19(10), 2119–2127.
Roman, L., Raffo, J. E., Zhu, Q., & Meghea, C. I. (2014). A statewide Medicaid enhanced prenatal care program: Impact on birth outcomes. JAMA Pediatrics, 168(3), 220–227.
The Dartmouth Institute for Health Policy and Clinical Practice. (2017). Atlases and reports. Retrieved from http://www.dartmouthatlas.org/publications/reports.aspx.
Brown, P. A., Ross, D., Smith, J. A., Thornton, K., & Wimer, L. (2011). Technical report on lessons learned in the development of the Institute for Research on Poverty's Multi-Sample Person File (MSPF) data system. Madison, WI: Instititue for Research on Poverty.
U.S. Department of Health and Human Services. (2017). Data. Retrieved from https://datawarehouse.hrsa.gov/data/data.aspx.
U.S. Census Bureau. (2016). Core-based statistical areas. Retrieved from https://www.census.gov/topics/housing/housing-patterns/about/core-based-statistical-areas.html.
Wisconsin Department of Health Services. (2016). WISH query: fertility module. Retrieved from https://www.dhs.wisconsin.gov/wish/fertility/form.htm.
StataCorp. (2017). Stata statistical software: Release 15. College Station, TX: StataCorp LLC.
March of Dimes, Committee on Perinatal Health. (1976). Toward improving the outcome of pregnancy: Recommendations for the regional development of maternal and perinatal health services. White Plains: March of Dimes National Foundation.
American Academy of Pediatrics Committee on Fetus and Newborn. (2012). Levels of neonatal care. Pediatrics, 130(3), 587–597.
Acknowledgements
Support was provided by the University of Wisconsin-Madison Clinical and Translational Science Award (CTSA) program, through the National Institutes of Health (NIH) National Center for Advancing Translational Sciences (NCATS), Grant UL1TR00427, as well as the University of Wisconsin-Madison School of Medicine and Public Health’s Wisconsin Partnership Program (WPP) and the Institute for Research on Poverty. We are grateful for excellent data access and programming assistance provided by Steven T. Cook, Dan Ross, Jane A. Smith, Kristen Voskuil, and Lynn Wimer. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or WPP. The authors would like to thank the Wisconsin Department of Children and Families, Department of Health Services and Department of Workforce Development for the use of data for this analysis, but these agencies do not certify the accuracy of the analyses presented.
Funding
Support was provided by the University of Wisconsin-Madison Clinical and Translational Science Award (CTSA) program, through the National Institutes of Health (NIH) National Center for Advancing Translational Sciences (NCATS), Grant UL1TR00427, as well as the University of Wisconsin-Madison School Medicine and Public Health’s Wisconsin Partnership Program (WPP). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or WPP.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Research Involving Human Participants and/or Animals
The study did not directly involve human participants and/or animals. All study procedures were approved by an institutional review board.
Rights and permissions
About this article
Cite this article
Larson, A., Berger, L.M., Mallinson, D.C. et al. Variable Uptake of Medicaid-Covered Prenatal Care Coordination: The Relevance of Treatment Level and Service Context. J Community Health 44, 32–43 (2019). https://doi.org/10.1007/s10900-018-0550-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-018-0550-9