Abstract
Colorectal cancer (CRC) is the second leading cause of cancer-related deaths in the US, yet screening rates remain low among minority populations. The purpose of the current study was to identify differences in the endorsement of barriers to CRC screening and to evaluate the association between provider recommendation and CRC screening adherence among Hispanic, Pacific Islander and White patients. This study utilized a cross sectional survey design to identify patient-reported barriers to CRC screening. Logistic regression was utilized to evaluate the association between patient demographic characteristics (race/ethnicity, gender, age), having received provider recommendation, and patient awareness of CRC screening. The study sample was comprised of a diverse population (N = 197); 48% Hispanic, 25% White, 10% Pacific Islander, 4% Black and 13% other races/ethnicity. The median age of participants was 58, yet fewer than 30% were up-to-date for CRC screening. The most commonly cited barriers included fear of test results (27.6%), inability to leave work for a CRC screening appointment (26.9%), being unaware of the need for colonoscopy (25.4%), and lack of provider recommendation for CRC screening (24.9%). Only 16.2% of participants reported that a provider had discussed CRC screening options with them. After adjusting for age and gender, Hispanic patients were less likely to report having had a provider discuss CRC screening options compared to White patients (OR = 0.24, 95% CI: 0.09–0.68, p < 0.05). The findings from this study indicate that patient’s perceived screening barriers, lack of awareness and a lack of provider communication about CRC screening options may contribute to low screening rates among minority populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is the fourth most common type of cancer in the United States, and it is estimated that 134,490 new cases will be diagnosed in 2016 [1]. The U.S. Preventive Services Task Force (USPSTF) recommends that adults aged 50–75 undergo CRC screening, with test options including fecal stool blood test yearly, flexible sigmoidoscopy every 5 years, or a colonoscopy every 10 years [2]. Screening reduces the incidence and mortality of CRC [2, 3]. For example, proactive screening efforts may reduce mortality by approximately 15–33% [2, 3].
Despite the availability of effective screening tests, CRC screening rates remain low, especially among minority populations. For instance, approximately 44% of Hispanics are up-to-date for CRC screening compared to 61% of non-Hispanic Whites [4]. Additionally, little is known about CRC screening rates among Pacific Islanders, making it difficult to know whether barriers to screening exist in this population. Due to disparities in cancer screening among minority populations, it is important to identify predictors of CRC screening adherence, such as perceived barriers to screening and the role of provider screening recommendations [4].
Although common barriers to receiving CRC screening have been studied extensively in some populations (e.g., non-Hispanic Whites), there is comparatively little data on screening rates and barriers among certain minority groups (e.g., Pacific Islander and Hispanic patients). Previous studies indicate that patients’ commonly endorsed barriers to CRC screening include fear of test results, lack of provider recommendation, and logistical barriers such as cost and lack of transportation [5–13]. Additionally, patients’ lack of awareness regarding the importance of CRC screening and different screening options have been reported in some studies [9–11, 14–16]. However, few studies have evaluated potential differences in barriers endorsed between racial or ethnic groups. Initial evidence suggests that barriers to CRC screening may differ between racial and ethnic groups. For example, Hispanic patients were more likely to report embarrassment from screening tests and fear of test results compared to non-Hispanic White patients [17]. Identifying barriers unique to racial and ethnic groups could inform culturally-sensitive, tailored interventions aimed at improving adherence to CRC screening.
In recent years, the role of physician recommendation in the uptake of CRC screening has been examined as an important predictor of CRC screening [5, 16, 18]. Most notably, studies have found that minority patients (e.g., African American and Hispanic patients) are less likely to receive a provider recommendation for CRC screening than White patients [10, 16, 19]. Thus, lack of provider recommendation among minority populations could contribute to the low screening rates in these populations. No studies, to our knowledge, have evaluated the role of provider recommendation for CRC screening within a Pacific Islander clinic population.
The purpose of the current study was to identify differences in the endorsement of barriers to CRC screening and to evaluate the association between provider recommendation and CRC screening adherence among Hispanic, Pacific Islander and White patients. The goal of this analysis is to contribute to the understanding of factors that may impact disparities in CRC screening rates among minority populations, and to inform the development of culturally-tailored interventions for these diverse populations.
Methods
Participants
Participants in the current study were recruited from a safety-net clinic in the Intermountain West that provides free medical services for uninsured and low-income individuals. Participants were eligible to participate in the current study if they were aged 50–75 and had a scheduled medical appointment (for any reason) at the clinic. This study was approved by the Institutional Review Board (IRB) at Westminster College.
Measures
Participants were asked to complete a self-report questionnaire assessing barriers to, awareness of, and occurrence of provider recommendation for CRC screening. To address language barriers and low health literacy among participants, the questionnaire was modified from a previous questionnaire used to identify barriers to CRC screening in a predominately Black population [9]. For example, to address potential lack of knowledge about screening tests, a brief definition of each screening test was added to the survey. Following the description of each screening test, awareness of colonoscopy and blood stool test was assessed by asking “are you aware of what a colonoscopy/blood stool test is?”
Barriers were assessed using a list of potential barriers (operationalized as yes/no responses) for colonoscopy and blood stool test, separately. Barriers to sigmoidoscopy were not assessed because the clinic did not offer this procedure. In addition, participants were asked to report on their lifetime screening status (ever had colonoscopy/fecal stool blood test and year of last screening). Provider recommendation for CRC screening was assessed by asking patients if their provider had ever discussed CRC options with them and if so, which option(s). The questionnaire also contained items assessing patient demographic information, including gender, age, race/ethnicity, and previous history of cancer. Participants were provided with a Spanish or English form of the survey based on their documented preferred language in the medical chart.
Procedure
Study recruitment occurred over a 2-month period in 2015. Clinic staff invited all eligible participants to complete the questionnaire during the triage portion of their appointment (prior to meeting with their healthcare provider). In total, 770 surveys were attached to medical charts for recruitment, and 197 were returned (response rate = 26%).
Statistical Analysis
Data were analyzed using STATA 14.1. Frequencies and percentages were calculated to summarize participant demographic characteristics, screening rates and endorsement of barriers to CRC screening. A one-way analysis of variance (ANOVA) with post-hoc analysis was performed to assess the difference in the number of endorsed barriers between Hispanic, Pacific Islander and White participants. Logistic regression was performed to investigate the extent to which provider recommendation was predicted by race/ethnicity. Logistic regression was also performed to assess the association between race/ethnicity and awareness of screening tests.
Results
A total of 197 participants completed the questionnaire (Table 1). Half (50%) of the sample completed the English survey and the remainder completed the Spanish survey. The median age of participants was 58 years and the sample was 58% female. Participants self-reported their race/ethnicity as Hispanic (48%), White (25%), Pacific Islander (10%), Black (4%) and Other (13%).
Screening Rates
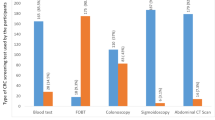
Less than 30% of participants were currently up-to-date for colonoscopy or fecal stool blood test based on the USPSTF recommendations (Table 2). Approximately half (56%) reported never having completed either test and 12% reported having had a past screening test but being currently overdue. Hispanic participants were less likely to report having completed a colonoscopy compared to White participants (OR = 0.33; 95% CI: 0.15–0.72; p < 0.05). Hispanic participants were also less likely to report having completed a fecal stool blood test compared to White participants (OR = 0.38; 95% CI: 0.16–0.89; p < 0.05). Similarly, Pacific Islander participants were less likely to report having completed a colonoscopy compared to White participants (OR = 0.08; 95% CI: 0.02–0.44; p < 0.05). There was no significant difference in completion of fecal stool blood tests between Pacific Islander and White patients.
Barriers
Across the entire sample, the most commonly cited barriers to colonoscopy included fear of test results (28%), unable to leave work for appointment (27%), being unaware of the need for colonoscopy (25%), and lack of provider recommendation (25%). When barriers were evaluated for each racial/ethnic group separately, the most common barriers were different. For instance, Hispanics most commonly endorsed lack of trust in their provider (51%), whereas Pacific Islander participants cited not having a family member who has had CRC as their most common barrier (34%) (Table 3). Hispanics reported a significantly higher average number of barriers than White participants [F(3,190) = 4.82, p < 0.05]. On average, Hispanics reported nearly two more barriers than White participants. Hispanic participants were less likely to report being aware of what colonoscopy is (OR = 0.19; 95% CI: 0.05–0.71; p < 0.05) and what a fecal stool blood test is than White participants (OR = 0.38; 95% CI: 0.17–0.81; p < 0.05). Pacific Islander participants were also less likely to be aware of what a colonoscopy is (OR = 0.05; 95% CI: 0.01–0.24, p < 0.05) than White participants (Table 4).
Provider Recommendation
Only 16.2% of participants reported ever receiving a provider recommendation for CRC screening. Of the people who reported having received a provider recommendation, colonoscopy was the most commonly discussed screening option (75%). Race/ethnicity was a predictor of receiving a provider recommendation (Table 4). Specifically, after adjusting for age and gender, Hispanic participants were 76% less likely to report having received a provider recommendation compared to White participants (OR = 0.24; 95% CI: 0.09–0.68; p < 0.05). There was no significant association for Pacific Islander participants. Also, after adjusting for age and gender, participants across all racial and ethnic groups who received a provider recommendation were 3.7 times more likely to report having completed a colonoscopy (OR = 3.72; 95% CI: 1.59–8.86; p < 0.05) and 3.9 times more likely to report having completed a fecal stool blood test (OR = 3.90; 95% CI: 1.56–9.74; p < 0.05) than those who reported no provider recommendation.
Discussion
Consistent with national data, minority participants in the current study had suboptimal screening rates for both colonoscopy and fecal stool blood test and were less likely to have reported any prior CRC screening compared with White participants [4]. CRC screening adherence among all participants within this safety-net clinic was low. This result is particularly notable given participants attending the clinic have access to free fecal stool blood tests and low cost screening colonoscopies.
Similar to previous studies, commonly endorsed barriers included fear of test results, being unable to afford to leave work for screening appointments, being unaware of the need for colonoscopy, and lack of provider recommendation [5–12, 20]. However, the current study found that the most common barriers for each racial/ethnic group were different. For example, Hispanics commonly endorsed a lack of trust in their provider while Pacific Islanders reported not having a family member who has had CRC as their most common barrier. Hispanic participants endorsed statistically significantly more barriers on average than White and Pacific Islander participants. This indicates that Hispanic participants may be affected by a wider range of barriers, which could lead to reduced adherence to CRC screening recommendations. Lack of awareness was also an important barrier in the current study. Awareness of CRC screening was low for both Hispanic and Pacific Islander participants when compared to White participants.
Similar to previous studies, race/ethnicity was a predictor of the receipt of a provider recommendation for CRC screening [5, 16, 18]. In the current study, Hispanic participants were less likely to report receiving a provider recommendation for CRC screening compared with White participants. Of particular concern was the overall lack of provider recommendation among all study participants. Only 16% of participants reported receiving a provider recommendation, yet those who reported receiving a provider recommendation for CRC screening were more likely to have completed a colonoscopy and a fecal stool blood test. This emphasizes the integral role of provider recommendations in CRC screening adherence and the importance of effective provider communication with patients. For example, a prior study found that patients who receive information about CRC screening from providers may not fully understand what has been communicated to them [21]. In diverse safety-net clinics where health literacy may be particularly low, increasing the effectiveness of provider-patient communication may help to increase awareness among minority populations [21–24].
The findings from the current study support the notion that interventions to increase CRC screening among diverse patients, including from Hispanic and Pacific Islander communities, may be more effective if they address barriers specific to each racial and ethnic group. Patient interventions should address the specific needs of Hispanic and Pacific Islander patients, including the differences in barriers and low levels of awareness. For example, since Hispanic participants endorsed a lack of trust in their provider as a common barrier, it may be beneficial for future studies to gain an understanding of reasons behind this, so providers can improve their relationship building. Since the provider plays an important role in CRC screening, interventions targeting awareness may be most effective if they are implemented at both the individual patient and provider levels.
The current study had several limitations. The study included a relatively small sample size and had a low response rate, both likely due to the high no-show rate in the clinic. Another limitation of this study is the use of self-report for completion of CRC screening and provider recommendation of CRC screening. In the case of provider recommendation, patient report of recommendation occurrence could be an underestimate due to language barriers or other communication challenges. Future studies should replicate the findings of this study using a larger sample size, including a larger sample of Pacific Islanders, an understudied group. Future studies may also benefit from using patient chart review as a way to confirm CRC screening completion and potentially, provider recommendation.
The findings from this study helped to elucidate racial/ethnic differences in the endorsement of barriers and receipt of provider recommendation. Specifically, this study described barriers to CRC screening unique to Hispanic populations and addressed the lack of data on screening rates, barriers and provider CRC screening recommendation among Pacific Islander patients. Results from the current study emphasize the importance of evaluating salient barriers for each racial/ethnic group separately and the need for tailored educational interventions, especially in racially diverse clinics.
References
SEER Cancer Statistics Factsheets: Colon and rectum cancer (2016). http://seer.cancer.gov/statfacts/html/colorect.html.
US Preventive Services Task Force (2016). Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA, 315(23), 2564–2575. doi:10.1001/jama.2016.5989.
Winawer, S., et al. (2003). Colorectal cancer screening and surveillance: Clinical guidelines and rationale-update based on new evidence. Gastroenterology, 124(2), 544–560. doi:10.1053/gast.2003.50044.
Cancer Trends Progress Report: Colorectal cancer screening (2015). http://progressreport.cancer.gov/detection/colorectal_cancer.
Geiger, T. M., et al. (2008). Improving rates for screening colonoscopy: Analysis of the health information national trends survey (HINTS I) data. Surgical Endoscopy and Other Interventional Techniques, 22(2), 527–533. doi:10.1055/s-0029-1242460.
Cameron, K. A., et al. (2007). Investigating Hispanic/Latino perceptions about colorectal cancer screening: A community-based approach to effective message design. Patient Education and Counseling, 68(2), 145–152. doi:10.1016/j.pec.2007.04.004.
Green, A. R., et al. (2008). Barriers to screening colonoscopy for low-income Latino and white patients in an urban community health center. Journal of General Internal Medicine, 23(6), 834–840. doi:10.1007/s11606-008-0572-6.
Honein-AbouHaidar, G. N., et al. (2016). Systematic review and meta-study synthesis of qualitative studies evaluating facilitators and barriers to participation in colorectal cancer screening. Cancer Epidemiology Biomarkers and Prevention, 25(6), 907–917. doi:10.1158/1055-9965.epi-15-0990.
Jones, R. M., et al. (2010). The relative importance of patient-reported barriers to colorectal cancer screening. American Journal of Preventive Medicine, 38(5), 499–507. doi:10.1016/j.amepre.2010.01.020.
Klabunde, C. N., Schenck, A. P., & Davis, W. W. (2006). Barriers to colorectal cancer screening among Medicare consumers. American Journal of Preventive Medicine, 30(4), 313–319. doi:10.1016/j.amepre.2005.11.006.
McLachlan, S. A., Clements, A., & Austoker, J. (2012). Patients’ experiences and reported barriers to colonoscopy in the screening context—A systematic review of the literature. Patient Education and Counseling, 86(2), 137–146. doi:10.1016/j.pec.2011.04.010.
Taylor, V., et al. (2003). Colorectal cancer screening among African Americans: The importance of physician recommendation. Journal of the National Medical Association, 95(9), 806–812. https://www.scopus.com/inward/record.uri?eid=2-s2.00141818420&partnerID=40&md5=63a426d8372d31ae99bf3167629a9f38.
Tessaro, I., et al. (2006). Knowledge, barriers, and predictors of colorectal cancer screening in an Appalachian church population. Preventing Chronic Disease, 3(4). http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1779287/.
Berkowitz, Z., et al. (2008). Beliefs, risk perceptions, and gaps in knowledge as barriers to colorectal cancer screening in older adults. Journal of the American Geriatrics Society, 56(2), 307–314. doi:10.1111/j.1532-5415.2007.01547.x.
O’Malley, A. S., et al. (2004). Patient and provider barriers to colorectal cancer screening in the primary care safety-net. Preventive Medicine, 39(1), 56–63. doi:10.1016/j.ypmed.2004.02.022.
Shokar, N. K., Carlson, C. A., & Weller, S. C. (2008). Factors associated with racial/ethnic differences in colorectal cancer screening. The Journal of the American Board of Family Medicine, 21(5), 414–426. doi:10.3122/jabfm.2008.05.070266.
Walsh, J. M. E., et al. (2004). Barriers to colorectal cancer screening in Latino and Vietnamese Americans. Journal of General Internal Medicine, 19(2), 156–166. doi:10.1111/j.1525-1497.2004.30263.x.
Brawarsky, P., et al. (2004). Effect of physician recommendation and patient adherence on rates of colorectal cancer testing. Cancer Detection and Prevention, 28(4), 260–268. doi:10.1016/j.cdp.2004.04.006.
Wee, C. C., McCarthy, E. P., & Phillips, R. S. (2005). Factors associated with colon cancer screening: The role of patient factors and physician counseling. Preventive Medicine, 41(1), 23–29. doi:10.1016/j.ypmed.2004.11.004.
Tessaro, I., et al. (2006). Knowledge, barriers, and predictors of colorectal cancer screening in an Appalachian church population. Preventing Chronic Disease, 3(4), 123–134. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1779287/.
Davis, T. C., et al. (2001). The role of inadequate health literacy skills in colorectal cancer screening. Cancer Investigation, 19(2), 193–200. doi:10.1081/CNV-100000154.
Arora, N. K. (2003). Interacting with cancer patients: The significance of physicians’ communication behavior. Social Science and Medicine, 57(5), 791–806. doi:10.1016/S0277-9536(02)00449-5.
Bredart, A., Bouleuc, C., & Dolbeault, S. (2005). Doctor-patient communication and satisfaction with care in oncology. Current Opinion in Oncology, 17(4), 351–354.
Fallowfield, L., & Jenkins, V. (1999). Jenkins, effective communication skills are the key to good cancer care. European Journal of Cancer, 35(11), 1592–1597. doi:10.1016/S0959-8049(99)00212-9.
Acknowledgements
We greatly appreciate feedback from Dr. Natalie Stillman-Webb from the University of Utah, in addition to Dr. John Contreras and Dr. Kristine Lynch from Westminster College on earlier versions of this manuscript.
Funding
This work was supported, in part, by the National Cancer Institute (NCI) of the National Institutes of Health (NIH) K07CA196985 (to YW), American College of Gastroenterology Junior Faculty Development award (to NJS) and the Huntsman Cancer Institute and Huntsman Cancer Foundation. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Samadder has received a speaker honorarium from Cook Medical Inc. All other co-authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Nagelhout, E., Comarell, K., Samadder, N.J. et al. Barriers to Colorectal Cancer Screening in a Racially Diverse Population Served by a Safety-Net Clinic. J Community Health 42, 791–796 (2017). https://doi.org/10.1007/s10900-017-0319-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-017-0319-6