Abstract
Background
Colonoscopy is an effective modality for colorectal cancer screening. The objectives of this study were to identify colorectal cancer knowledge and barriers to screening colonoscopy in the general US population.
Methods
Data was obtained from the health information national trends survey (HINTS I). The dataset (n = 6369) examined the influence of age, race, gender, education, income, media usage, and interactions with health care providers on knowledge, attitudes, and behavior regarding colonoscopic screening for colorectal cancer.
Results
The term ‘colonoscopy’ was recognized by 80% of participants (over the age of 35), however only 35% of respondents perceived it as a major method for colon cancer screening. Hispanics had the least awareness of colonoscopic screening (16% versus 39% non-Hispanic). Female gender, education, and income all correlated with knowledge and use of colonoscopic screening. There was a positive correlation between media usage and having a colonoscopy (r = 0.095, p < 0.01). Having a health care provider was strongly correlated with having undergone a colonoscopy (r = 0.249, p < 0.01). Reasons for not having a colonoscopy were ‘no reason’ (29%), ‘doctor didn’t order it’ (24%), and ‘didn’t know I needed the test’ (15%). Personalized materials were the preferred media for receiving cancer-related information.
Conclusions
Knowledge of and participation in screening colonoscopy is low in the US population, especially among Hispanics. The most important immediate action is to increase physician referral for screening colonoscopy. Education materials focused on specific sociodemographic segments and targeted communication campaigns need to be developed to encourage screening.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Colorectal cancer is the fourth most common cancer in the United States. In 2005 approximately 50,000 people died from colorectal cancer and over 140,000 cases were diagnosed [1]. The survival rate for stage I cancers is good, with over 90% 5-year survival. However, advanced stage colorectal cancers have a survival rate of less than 10% [2]. This high mortality and large incidence makes colorectal cancers the second leading cause of cancer death in the United States. Screening methods are widely available for colorectal cancer. These include fecal occult blood test (FOBT), barium enema, sigmoidoscopy, colonoscopy, and even newer techniques including virtual colonoscopy and fecal deoxyribonucleic acid (DNA) testing. Currently, colonoscopy remains the preferred modality of colorectal screening by the American Society for Gastrointestinal Endoscopy and the American College of Gastroenterology [3, 4]. It is currently the most sensitive method for finding cancer precursors (polyps) and can be therapeutic.
Routine colonoscopy can reduce the incidence of colorectal cancer by 76–90% [5, 6, 7]. This large decrease in incidence has not been realized in the general population. The incidence of colon cancer has decreased little since the introduction of colonoscopy. The reason for this is that, despite the high success of colonoscopy to prevent colon cancer, many patients do not undergo the screening examination. In 2002, approximately 77 million people in the United States were over the age of 50. Of these, an estimated 42 million had not had colon cancer screening of any kind. Approximately 18 million (23%) people over the age of 50 years have had screening colonoscopy. This figure does not include high-risk patients, who may need screening more frequently and before the age of 50 years [8].
If colorectal screening is so effective at detecting and treating lesions before they become invasive cancers, why is the general population not being screened? To answer this question, the public’s attitude towards colorectal cancer screening needs to be investigated. In this study we examined the general public’s view of colorectal cancer screening by looking at the health information national trends survey (HINTS 1). This survey was completed in 2003. It is comprised of a survey administered to a representative population of the United States collected to monitor the public’s knowledge and use of health information in the mass media. We created a database of patient demographics, attitudes, and knowledge of colorectal screening to find if any variable could define why this highly successful screening technique is not more widely adopted. The aim was to identify barriers to screening colonoscopy in eligible patients. The hypotheses were that poor knowledge of colon cancer and colon cancer screening are major barriers to obtaining screening colonoscopy.
Methods
All data used in the statistical analysis was gathered through the health information national trends survey (HINTS I) conducted by the National Cancer Institute. This survey was completed in December 2003. There were 6349 respondents who either completed the entire survey or only the health communication and general cancer questions only. From these surveys, the 34 questions specific to colorectal cancer screening were extracted and entered into the database. The analysis of this data assessed demographic data for comparison and was used to created hypotheses about the barriers to colorectal cancer screening.
From the 34 specific colorectal screening questions (Appendix A) and the background information provided by each participant, perception about colorectal screening could be analyzed with the follow eight independent variables: age, ethnic background, gender, education, employment status, income, media usage, and interactions with health care providers. In addition, those who had undergone colorectal screening were compared against those who had not. Finally, subjects with knowledge of colorectal cancer screening were compared to those without this knowledge.
There were five major questions to be addressed by the data set:
-
1.
What is the general knowledge about colon cancer within the general population?
-
2.
How widespread is accurate and correct knowledge about colonoscopy and sigmoidoscopy within the general population?
-
3.
What are the possible reasons for not having a colonoscopy/sigmoidoscopy?
-
4.
Are attitudes of those who had a colonoscopy/sigmoidoscopy different from those who did not have one regarding the procedure?
-
5.
What are the most frequently used media channels of those who had a colonoscopy/sigmoidoscopy?
To better evaluate the influence of media, a media load index was constructed by adding individual volumes for daily hours watching TV, daily hours of radio listening, days reading newspapers per week, and days reading magazines per week. Values were normalized (n = 6309) and a random sample of 1500 was selected.
All observations were assumed to be independent. SPSS 13/0 was used to perform the statistical analysis. Variables were assessed for normality and logarithmic transformations were applied to normalize those that had skewness and/or kurtosis outside of the +3/–3 range. Descriptive statistics were conducted on all variables; correlations, t-tests, and analysis of variance (ANOVA) were used to test for statistically significant effects of independent variables.
Results
Of the 6349 participants 60% were female and the largest age group was 35–49 years (30.9%), followed by 18–34 years (26.1%), and 50–64 years (23.5%). Of this population most felt their risk for colon cancer was very low (30%) or somewhat low (31%). They also felt they were less likely (45%) or about as likely (39%) to get cancer as the average person and they rarely or never worry about getting colon cancer (74%).
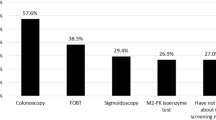
Understanding of colon cancer screening tests is shown in Table 1. Most thought that nothing detects colon cancer (43%), and only 36% correctly identified colonoscopy as a colon cancer screening test. Other possible answers included digital rectal exams, computed tomography CT/ magnetic resonance imaging (MRI) scans, and fecal occult blood tests. Fecal occult blood test was the third most common answer for detection of colon cancer (7%). Most patients had heard of a stool blood test (61%) but only 44% of eligible patients had actually had a stool blood test in the past year. The most common reasons for not having a stool blood test were “no reason” and “doctor didn’t say I needed it.” Only 21% of patients had thought about having an initial or subsequent stool blood test.
The term colonoscopy was familiar to 80% while only 30% had heard of sigmoidoscopy. Of patients over the age of 50 years, 38% indicated they had undergone a colonoscopy in the past. Of those, 90% were performed in the last 10 years. Table 2 shows responses to why eligible subjects had not had a colonoscopy in the past. The most common answer was “no reason” (29%) followed by “doctor did not order it or did not say I needed it” (24%).
The perception of the age at which the average person should begin colorectal cancer screening with a colonoscopy was highly variable (Table 3). There is also considerable misunderstanding of the interval between colonoscopies (Table 4).
Most subjects felt that arranging a colonoscopy is easy (44%) or somewhat easy (32%). Half of patients responded that they were afraid of finding colon cancer if they were checked. Most patients (89%) agreed that regular colon checks improved the chances of finding treatable colon cancer. Only 28% of patients thought colon cancer screening was too expensive. Most subjects thought the highest risk of colon cancer was 40–60 years of age. Only 29% realized that your risk of colon cancer is greatest over 60 years of age.
Analysis
Gender played a major role in colon cancer knowledge. Women (42%) were more likely than men (27%) to understand that colonoscopy tests were for colon cancer. More women than men were aware of colonoscopy (64% versus 36%). Age did not play a major role in cancer knowledge. Older patients were more likely to know that colonoscopy detects colon cancer (50–64 years 45%, 35–49 years 33%). The youngest age group (18–34 years, 65%) was less likely to have heard of colonoscopy (cf. 82–88% in the older age groups). Employment status did not influence colon cancer knowledge.
Ethnic background also had a significant influence on cancer knowledge. Hispanics had the lowest degree of recognition as to what a colonoscopy was and its purpose. Overall only 48% of Hispanic individuals answered “Yes” to knowing what a colonoscopy is (compared to the average of 85%), and only 16% could correctly identify its use (compared to 39% of other ethnic groups). Of all ethnic backgrounds Hispanic individuals had the lowest percentage of participants who had actually undergone a colonoscopy (9%), compared to the overall average (38%). More white people (40%) knew that colonoscopy detected colon cancer than non-white people (25%).
Education level had a strong influence on knowledge of colonoscopy. A higher education level was correlated with the proportion of participants who had heard of a colonoscopy or knew of its use for cancer screening. Over 90% of those with a college degree or higher level of education were knowledgeable, compared to 15% of those who reported having less than a high school diploma or being illiterate. Over 50% of the group with the highest level of education knew that a colonoscopy was a screening test for colorectal cancer, while 69% of those with less than a high school education answered that “nothing” was a screening test for colorectal cancer. In a manner similar to education, income level showed a direct correlation between higher income and greater knowledge about screening for colorectal cancers. Income level however did not significantly impact on the percentage of participants who had actually undergone a colonoscopy. Participants who had previously undergone an endoscopic procedure (either colonoscopy or sigmoidoscopy) were found to have a more positive attitude towards colorectal cancer screening. Of these participants, 58% who had previously had a colonoscopy or sigmoidoscopy indicated that “arranging to get tested for colon cancer would be easy”. This is in direct contrast to 39% of those who had not undergone an endoscopic screening exam.
Those who had previously undergone an endoscopic procedure were more likely to answer that “regular colon cancer checks increase changes of finding treatable cancer” compared to those who have not undergone an examination (84% versus 71%). Also those who have undergone a colonoscopy were less likely to consider it an expensive procedure than those who have not undergone an endoscopy (p = 0.047).
A major factor between the groups who had undergone a colonoscopy and the group which had not was having a health care provider. Of those who had undergone endoscopic screening, over 30% indicated that they had regular health care provider, compared to only 9% of those who had not been screened. There was also a direct correlation between the number of times a participant had visited a physician and the likelihood that they had undergone a colonoscopy (p = 0.01). Also a majority of those who underwent an endoscopic screening had some level of health care coverage.
Media usage was correlated with whether a participant had undergone colonoscopy/sigmoidoscopy. Those who had undergone an endoscopic examination previously tended to be more likely to trust the information delivered by a physician than those who had not undergone endoscopic screening (p = 0.007). Also it was noted that those who had not undergone endoscopic screening were more trusting of cancer information from radio and Internet sources than those who had been screened (p = 0.001). Finally, patients who had undergone a colonoscopy listen to less radio per day (2 hours versus 2.5 hours) and read newspapers more days of the week (4.7 days versus 3.0 days).
The influence of the media load index was compared to colon cancer knowledge and knowledge seeking. Those with a lower media load thought they needed more information on colon cancer screening (p = 0.01), while those with a high media load placed more trust in the Internet (p = 0.038). Those who had colonoscopy correlated strongly with a high media load index (p < 0.0001).
Around half (47%) of the population had searched on their own for cancer information. Of those who said somebody else had looked for them for cancer information (17%), the vast majority used a family member (72%) or friend (20%). Very few used an information specialist (librarian) or a cancer organization. If given a choice, 49% would go to a physician first for cancer information, but a significant minority (33%) would go to the Internet first. Of those who had sought information on colon cancer, the actual first source of information was the Internet (47%) and the physician was first in only 11%.
Discussion
Colorectal cancer decreases life expectancy by up to 292 days per person (aged 50–54 years) in the United States. For patients aged from 50–79 years, it is estimated that the number of colonoscopies needed to save 1 year of expected life is between three and six [9]. This fact shows the amazing capabilities of a colonoscopy to decrease the incidence of colon cancer. Colonoscopy is also cost effective, with most estimates between $10,000 and $20,000 per life year saved [10].
Five major questions were addressed in this study. The first analyzed general knowledge about colon cancer within the general population. The data shows that there is a general lack of knowledge regarding colon cancer. Knowledge is especially poor in men, Hispanics, and the young. Age and income level showed less of an influence. The poor general knowledge about colon cancer appears to contribute to the low use of screening colonoscopy in the population. In addition, most subjects could be classified as optimists, as they did not have an accurate view of their risk of colon caner and seldom worried about it.
Knowledge regarding colon cancer screening testing was especially poor. Nearly half of the population did now know of anything that detects colon cancer. Knowledge of fecal occult blood testing was also poor, with only 7% of the population realizing that this was used for detecting colon cancer. This startling lack of knowledge of colon cancer screening techniques is a major failure of health care education in this country.
Most people think that the highest risk of colon cancer is in the 40–60-year-old age group. This is probably because screening is recommended to start at the age 50. These attitudes show a fundamental misunderstanding of colon cancer formation via the adenoma–colon cancer continuum. Most did not understand that the primary benefit of screening colonoscopy is to remove adenomatous polyps that may become cancerous ten or more years in the future. Better education regarding colon cancer information will likely improve screening compliance.
The second question dealt with accurate and current knowledge about colonoscopy. Again, overall knowledge was quite poor. Most (64%) did not realize that colonoscopy is a screening test for colon cancer. Knowledge of colonoscopy as a diagnostic or screening procedure was especially low among men and Hispanics. Education level strongly correlated with colonoscopy knowledge and understanding of colonoscopy as a screening test. Specific screening colonoscopy knowledge such as age to start and recommended intervals was poor in the general population. While 36% of patients understood that colonoscopy detects colon cancer, the question did not identify how many subjects understood that this was true for symptomatic and asymptomatic individuals. The concept of screening colonoscopy in an asymptomatic patient is not well understood.
The third question looked at reasons for not having colonoscopy. Of patients recommended to have colonoscopy (over age 50 years) 38% had actually had one. This is fairly typical of other studies on this subject [11, 12]. Most patients had “no reason”, which is too generic to help define colonoscopy barriers. The second reason was that a doctor did not tell me to. This could be a major clue to how to improve compliance for screening colonoscopy. A change in primary care physician attitude to this detail may greatly increase compliance with colonoscopies. In a similar way, those without a primary care provider (PCP) had lower colonoscopy usage.
Of those without a PCP, only 9% of respondents had undergone a colonoscopy. This fact can be attributed to both lack of knowledge and lack of physician guidance. Those who do not have a PCP might not have the regular opportunity to discuss health concerns and issues with a physician. Also, if these patients are rarely seen by a physician, the concentration of the visit would probably not be on health maintenance and prevention, leading to colorectal screening [13]. This study also concluded that specific barriers to colorectal screening were lack of screening policy, poor motivation for colorectal screening by the PCP, and inadequate insurance coverage of the screening procedure [13]. A study by Farraye et al. [14] looked at barriers to sigmoidoscopy by sending surveys to 998 patients. It was found that the odds of having an endoscopic procedure were increased by 3.7 if they had a long-term relationship with a PCP. In a separate study of colorectal screening in rural communities by Greiner et al. [15] 801 patients and 36 rural physicians were surveyed to find barriers to colonoscopy. They concluded that the primary barrier to colonoscopy in rural populations is inadequate discussion between physicians and patients.
The fourth question compared those who had had a colonoscopy versus those who had not. The attitude of those who had undergone colonoscopy was generally better than those who had not. Of those having had a colonoscopy 58% thought that having colon cancer screening was easy, compared to 39% in others. These patients better understood that colonoscopy contributed to finding early treatable cancer (84% versus 71%). This data shows that the primary barriers are to the first colonoscopy. Patients who have had a colonoscopy are more aware of its importance and more likely to comply with colonoscopy recommendations in the future.
The final question concerned the use of media in promoting colonoscopy. The use of media is strongly correlated with undergoing colonoscopy. 49% of respondants indicated they would chose to go to a physician first for any health information. However, most subjects (47%) actually reported going to the internet first for health information, and only 11% reported seeking information from a physician first. This likely has to do with the ubiquitous access to the Internet in our society. Most media appears to have a minor influence on screening colonoscopy, but the Internet is a highly significant information source.
The HINTS I data for barriers to colonoscopy revealed two major findings. There is a general lack of understanding of colonoscopy as a screening test for colon cancer. The second major finding is that the primary care physician is the most important gateway to screening colonoscopy. Both of these factors can be barriers to colonoscopy and could likely be improved with educational campaigns. Patients need to learn colon cancer concepts and understand the great value that colonoscopy provides. It is important to explore means to motivate PCPs to recommend screening colonoscopy.
The strength of this study is that it is based on a robust and representative sample of the US population. Some selection bias may be present as only those willing to fill out the questionnaire were included. The data is relatively recent (2003) but current trends such as Internet usage may have already changed. The data given was not cross-checked with other sources so a recall bias is likely present. The survey was constructed to evaluate the public’s use of cancer-related information and not specifically designed to address barriers to colonoscopy.
Probably the major research question that emerges from this data is that the most important reason for not having colonoscopy is “no reason”. It is important that we try to dig down and uncover the real reasons in this large group. This is probably best done with focus groups using qualitative research techniques. Once qualitative studies have revealed possible reasons, a random telephone survey might be helpful in quantitating and evaluating results. Tailored educational materials will likely be needed for maximum penetration of the screening colonoscopy message. We believe a concentrated media campaign has the potential to increase the use of screening colonoscopy especially if it is available on the Internet.
References
Jemal A, Murry T, Ward E, et al. (2005) Cancer Statistics, CA Cancer J Clin 55:10–30
O’Connell JB, Maggard MA, Ko CY (2004) Colon cancer survival rates with the new American Joint Committee on Cancer sixth edition staging. J Natl Cancer Inst 96:1420–5
ASGE guideline (2006) Colorectal cancer screening and surveillance. Gastrointestinal Endo; 63:546–558
Rex DK, ACG board of Trustees (2004) American College of Gastroenterology Action plan for colorectal cancer prevention. Am J Gastroenterology 99(4):574–7
Winawer SJ, Zauber AG, Ho MN, et al. (1993) Prevention of colorectal cancer by colonoscopic polypectomy: the National Polyp Study Workgroup. N Engl J Med 329:1977–81
Citarda F, Tomaselli G, Capocaccia R, et al. (2001) Efficacy in standard clinical practice of colonoscopic polypectomy in reducing colorectal cancer incidence. Gut 48:812–5
Thiis-Evenen E, Hoff GS, Sauar J, et al. (1999) Population-based surveillance by colonoscopy: effect on the incidence of colorectal cancer. Telemark Polyp Study I. Scand J Gastroenterol 34:414–20
Seef LC, Manninen DL, Dong FB, et al. (2004) Is there endoscopic capacity to provide colorectal cancer screening to the unscreened population in the United States? Gastroenterol 127:1661–9
Inadomi JM, Sonnenberg A (2000) The impact of colorectal cancer screening on life expectancy. Gastrointest Endo 51:517–23
Pignone M, Saha S, Hoerger T, et al. (2002) Cost-effectiveness analysis of colorectal cancer screening: A systematic review for the U.S Preventive Services Task Force. Ann Intern Med 137(2):96–106
Centers for Disease Control, Prevention. Screening for colorectal cancer- United States (1997) Morbidity and Mortality Weekly Report, 1999. 48:116–121
Centers for Disease Control, Prevention. Colorectal cancer test use among persons aged ≥50 years- United States, 2001. Morbidity and Mortality Weekly Report (2003). 289(19): 2492–2493
Wender RC (2002) Barriers to screening for colorectal cancer. Gastrointest Endo Clin North Am 12:145–69
Farraye FA, Wong M, Hurwitz S, et al. (2004) Barriers to endoscopic colorectal cancer screening: are women different than men? Am J Gastroenterol 341–9
Greiner KA, Engelman KK, Hall MA, et al. (2004) Barriers to colorectal cancer screening in rural primary care. Prevent Med 38:269–75
Author information
Authors and Affiliations
Corresponding author
Appendix 1. Colorectal cancer knowledge questions.
Appendix 1. Colorectal cancer knowledge questions.
-
1.
How likely are you to get colon cancer?
-
2.
Compared to an average person, how likely are you to get colon cancer?
-
3.
How often do you worry about getting colon cancer?
-
4.
What tests detect colon cancer?
-
5.
Have you ever heard of a stool blood test?
-
6.
In the last year, has a doctor advised you to have a home stool blood test?
-
7.
Have you every done a stool blood test at home?
-
8.
When was your most recent home stool blood test?
-
9.
Before the most recent, when was your last home stool blood test?
-
10.
Any reason why you have not had a home stool blood test?
-
11.
Have you thought about having another stool blood test?
-
12.
Do you plan to have another stool blood test?
-
13.
When do you expect to have another home stool blood test?
-
14.
What age should people start having home stool blood tests?
-
15.
Once people start, how often should they have home stool blood tests?
-
16.
Specify how often people should have home stool blood tests?
-
17.
Ever heard of sigmoidoscopy or colonoscopy?
-
18.
Ever had a sigmoidoscopy?
-
19.
Ever had a colonoscopy?
-
20.
Were you ever advised to have a sigmoidoscopy?
-
21.
Were you every advised to have a colonoscopy?
-
22.
When was your most recent sigmoidoscopy/colonoscopy?
-
23.
Before the most recent, when was your last sigmoidoscopy/colonoscopy?
-
24.
Any reason why you have not had a sigmoidoscopy/colonoscopy?
-
25.
Have you thought about having another sigmoidoscopy/colonoscopy?
-
26.
Do you plan to get another sigmoidoscopy/colonoscopy?
-
27.
When do you expect to have another sigmoidoscopy/colonoscopy?
-
28.
At what age are people supposed to start having sigmoidoscopy/colonoscopy?
-
29.
Once they start, how often is it recommended to have a sigmoidoscopy/colonoscopy?
-
30.
Arranging to get tested for colon cancer would be easy?
-
31.
Are you afraid of finding colon cancer if you got checked?
-
32.
Do regular colon checks increase the chances of finding treatable cancer?
-
33.
Getting checked for colon cancer is too expensive?
-
34.
What age is the highest risk for colon cancer?
Rights and permissions
About this article
Cite this article
Geiger, T.M., Miedema, B.W., Geana, M.V. et al. Improving rates for screening colonoscopy: Analysis of the health information national trends survey (HINTS I) data. Surg Endosc 22, 527–533 (2008). https://doi.org/10.1007/s00464-007-9673-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-007-9673-2