Abstract
Among the potential range of irrational beliefs that could be used as predictors of physical and mental health, catastrophizing is the process that has received most attention in chronic pain research. Other irrational processes such as demandingness, low frustration tolerance, and self-downing have rarely been studied. The goal of this study was to explore whether this wider range of beliefs is associated with health in chronic pain patients beyond catastrophizing. A total of 492 chronic pain patients completed a measure of irrational beliefs, a measure of physical and mental health, and a numerical rating scale designed to assess pain intensity and interference. Irrational processes were more strongly associated with mental than with physical health. Low frustration tolerance and self-downing were found to be significantly related to mental health even after controlling for the effect of catastrophizing. Processes other than catastrophizing appear to have potentially important relationships with the mental health of people with chronic pain. These results may offer new intervention targets for practitioners.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Albert Ellis (1962) argued that irrational beliefs, which are considered to be inconsistent with reality and illogical, play a fundamental role in the interpretation of life events. Now, more than 50 years after Ellis used the term catastrophizing for the first time, this irrational belief has proved to be a key variable in the prediction of pain- related outcomes (Agar-Wilson & Jackson, 2012; Flink, Boersma, MacDonald, & Linton, 2012; Lee, Wu, Lee, Cheing, & Chan, 2008; Wade, Riddle, & Thacker, 2012).
Contemporary categorizations of irrational beliefs distinguish four belief processes (i.e., inferences about an event): demandingness, catastrophizing/awfulizing, low frustration tolerance (LFT), and a global evaluation or self-downing (Lega & Ellis, 2001). However, with the exception of catastrophizing, there has been relatively little study of these four belief processes in chronic pain. It may be useful, therefore, to look further at whether these variables are also worth of study in future research.
Demandingness refers to inflexible requirements expressed in terms of “musts,” “should,” “have to,” and “oughts” (e.g., “I should not have difficulties;” Bridges, 2010). In pain research it appears that demandingness, in the form of perfectionism, has a direct correlation with pain interference and negative affect (Hadjistavropoulos, Dash, Hadjistavropoulos, & Sullivan, 2007).
Catastrophizing can be defined as evaluation of a negative event as worse than it should actually be (e.g., “It would be terrible to fail at something that is important to me;” Bridges, 2010). As exposed above, catastrophizing has been repeatedly associated with a wide range of consequential outcomes in chronic pain, including pain intensity and interference (Ferreira-Valente, Pais Ribeiro, Jensen, & Almeida, 2011; Ramírez Maestre, Esteve Zarazaga, & López Martínez, 2001), physical disability (Agar-Wilson & Jackson, 2012; George, Calley, Valencia, & Beneciuk, 2011), depression (Nieto, Miró, Huguet, & Saldaña, 2011; Wade et al., 2012; Wong, Williams, Mak, & Fielding, 2011), and anxiety (Hirsh, George, Riley, & Robinson, 2007; Moix, Kovacs, Martín, Plana, & Royuela, 2011).
When it comes to LFT, pain studies have tended to focus on the affective component of this variable (Muris et al., 2007; Wade, Dougherty, Archer, & Price, 1996). However, LFT also implies a cognitive evaluation of certain circumstances as being unbearable (e.g., “I can’t function when I have difficulties;” Bridges, 2010). Although this irrational belief has not been a focus of study in chronic pain, McCracken and Eccleston (2003) have suggested that frustration, such as when attempts to control pain fail, can worsen the pain experience. Therefore, we would expect LFT to have a negative association with pain-related outcomes.
Self-downing is a defensive (i.e., it can prepare for failure) self-critical belief related to occasions when achievements are not experienced as satisfactory. It has also been associated with worse outcomes, such as severity of depression, in clinical studies (Luyten et al., 2011). In addition, this tendency to be excessively critical and to make global negative evaluations of oneself (e.g., “I am useless if I have difficulties;” Bridges, 2010) has been shown to have a greater association with distress, pain interference, and activity level than do traditional pain-related beliefs, such as the belief that pain is permanent or the belief that one is to blame for one’s pain (Stroud, Thorn, Jensen, & Boothby, 2000).
The previous studies have increased our understanding of how irrational beliefs can influence health outcomes in the presence of pain, which is encouraging. However, to our knowledge no study has assessed all these irrational processes together in relation to chronic pain. Furthermore, while pain catastrophizing has been shown to have a considerable association with pain-related outcomes, it is not known whether the other irrational processes may also contribute to the prediction of health beyond catastrophizing. Hence, the main aim of this study is to explore the relation between irrational processes and health in a sample of chronic pain patients when controlling for catastrophizing. As each irrational process addresses a different component of irrational thinking, we expect that demandingness, LFT, and self-downing will be significantly associated with health, above and beyond catastrophizing.
Methods and Materials
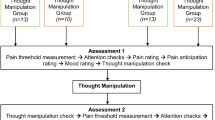
Participants and Procedure
The sample comprised 492 consecutive patients (63.6% women) who attended the Pain Clinic at the Vall d'Hebron Hospital for the first time. Data collection started during the second half of 2010 and finished by the end of 2012. The mean age for the whole sample was 58.49 years (SD = 15.12). Most patients were married at the time of assessment (60.5 %). The remaining patients were widowed (14.2 %), single (13.0 %), or divorced (12.3 %). More than half of participants (54.2 %) presented low educational levels (i.e., less than 12 years of education). The majority of participants were not working at the time of assessment. Specifically, 53.5 % of patients were retired and 12.4 % were unemployed. Duration of pain ranged from 4 months to 53 years, with a mean duration of pain of approximately 7 years (SD = 10 years) and a median of 3 years. Pain diagnoses were provided by expert physicians working at the Pain Clinic. Diagnoses were made on the basis of prior medical records and the observations made by the physicians during the first interview with the patient at the Pain Clinic. Main pain diagnoses were low back pain (59 %), neck pain (9.3 %), post-surgery pain (6.3 %), and osteoarthritis (5.5 %). Regarding the type of pain, 30.2 % of patients suffered from nociceptive pain, 6.3 % from neuropathic pain, and 63.4 % from mixed pain.
Nociceptive pain refers to pain caused by damage to body tissue, such as bones, muscles, or joints. In contrast, neuropathic pain is a result of damage to the nervous system, such as spinal cord, peripheral nerves, and certain central nervous system regions. Mixed pain is a combination of nociceptive and neuropathic pain (Woolf, 2004). Certain diseases, such as osteoarthritis, inflammatory arthropathies, and musculoskeletal pain, can present with nociceptive pain only. Other conditions, such as diabetic polyneuropathy, trigeminal neuralgia, post-stroke pain, and post-herpetic neuralgia, tend to be preferably accompanied by neuropathic pain (Erdemoglu & Koc, 2013). However, it is very frequent to find a combination of both pain etiologies. For example, musculoskeletal disorders include neck and low back pain. Despite in the previous lines we defined musculoskeletal disorders as predominantly nociceptive, a mixed etiology including neuropathic pain is frequent due to the degeneration of discs and the compression of nerves (Freynhagen & Baron, 2009).
A percentage of the patients included in the current study also participated in a previous investigation published elsewhere (Suso-Ribera, Camacho-Guerrero, McCracken, Maydeu-Olivares, & Gallardo-Pujol, 2014). The aim of the aforementioned study was to explore the relationship between problem-solving components and the health status of chronic pain patients. The sample was comprised of 369 participants. Together with a measure of problem solving and health, these patients also provided data on irrational thinking. This data on irrational thinking was not included in the previous investigation. After finishing the recruitment process for the previous study, we continued to recruit more participants for the current investigation. This resulted in 123 new participants. The same recruitment procedure, which will be detailed in the next section, was used in both studies.
Procedure
Patients were contacted by letter 1 month before their first scheduled visit at the Pain Clinic. The protocol they were sent included an explanation of the purpose, procedures and risks of the study, as well as contact information for the lead researcher, an informed consent form, and the questionnaires they were required to complete. The completed questionnaires were returned to the physicians the day of the patients’ first appointment, so all questionnaires were completed before patients reached the Pain Clinic for the first time.
Questionnaires
Irrational Beliefs
The General Attitudes and Beliefs Scale (GABS) describes beliefs presumed to underlie human behaviour and well-being from the perspective of rational emotive behaviour therapy (Burgess, 1986; DiGiuseppe, Leaf, Exner, & Robin, 1988). As opposed to other measures of irrational thinking, the GABS fulfils recent recommendations for the measurement of irrational beliefs: it distinguishes rational and irrational items, considers processes (i.e., interpretations of an event) and contents (i.e., the event themes), and assesses cognition rather than behaviour (David, Lynn, & Ellis, 2010). In addition, its items are considered not to include affective wording, which is in line with validity criteria for belief measures (Bernard, 1998).
The present study used a Spanish adaptation of the GABS-SV, a shortened version of the GABS (Caballo, Lega, & González, 1996). Half of the 48 items are rational, so they are not considered for the analysis of irrationality (Lega, Caballo, & Ellis, 2002). Participants are asked to rate to what extent they agree with a series of statements using a 5-point Likert-type scale. The response options are 0 = strongly disagree, 1 = disagree, 2 = neither agree nor disagree, 3 = agree, and 4 = strongly agree. The scale includes seven subscales, corresponding to four processes (demandingness, catastrophizing, LFT, and self-downing) and three contents (success, affiliation, and comfort). Each irrational item loads on a process and a content. Thus, for the purpose of this study, and to reduce multicollinearity, we only focused on the four processes. To simplify, from now we will use the term “irrational belief” to refer to the “process of irrational thinking” only, so both terms will be used indistinctively.
The number of items included in each scale is six for the processes (score range = 0–24). Two typical items are provided here for each irrational process in the GABS-SV, that is: Demandingness (“I must do well at important things” and “I must have a pleasant, comfortable life most of the time”); Catastrophizing (“It is a catastrophe to be hassled in life” and “It is awful to be disliked by certain people”); Low Frustration Tolerance (“I cannot tolerate to fail at important tasks” and “I can’t stand being disliked by other people who are important to me”); and Self-downing (“When I experience discomfort in my life, I tend to think that I am not a good person” and “I would be a worthless person if I achieved poorly at tasks that are important to me”). A reduced 55-item version of the GABS has been previously used (Sava, 2009), where its scales showed moderate to good levels of consistency (.59 < α < .70). However, the refined and shorter 48-item Spanish version (Caballo et al., 1996) obtained better internal consistency estimates in our sample (.69 < α < .86). Psychometric properties of the short version of the GABS will be presented in detail below.
The Spanish adaptation of the GABS-SV was created using a back-translation method (Chen & Boore, 2010). Specifically, the original scale in English was first translated to Spanish by the research team. Then, a professional linguist translated the Spanish version back to English. Finally, this back-translated English version was compared against the original English scale.
Health
The Spanish adaptation of the Short Form-36 Health Survey (SF-36; Alonso et al., 1998) was used to assess physical and mental health. The scale comprises 8 dimensions of health: Physical Functioning evaluates the limitations on daily activities (i.e., self-care, walking, climbing stairs, carrying weight, bending) due to health problems. Sample items include “Does your health now limit you in performing vigorous activities, such as running, lifting heavy objects, or participating in strenuous sports?” and “Does your health now limit you in climbing several flights of stairs?” This scale is comprised of 10 items ranging from 1 = yes, limited a lot to 3 = no, not limited at all, yielding a maximum score of 30. Role Physical measures the degree to which health interferes at work or other regular daily physical activities. Sample items include “During the past 4 weeks, have you had to cut down the amount of time you spent on work or other regular daily activities as a result of your physical health?” and “During the past 4 weeks, were you limited in the kind of work or other activities as a result of your physical health?” Role Physical is composed of 4 items, with items ranging from 1 = yes to 2 = no, and a maximum scale score of 8. Bodily Pain assesses the intensity of pain and its interference on daily functioning (e.g., “How much bodily pain have you had during the past 4 weeks?”). Bodily Pain has 2 items, one ranging from 1 = none to 6 = very severe, and another ranging from 1 = not at all to 5 = extremely. Therefore, scores for Bodily Pain range from 2 to 11. General Health reflects the perception of overall health, including current health status and expectations of future health. Sample items include “Compared to 1 year ago, how would you rate your health in general now?” and “I am as healthy as anybody I know.” General Health includes 5 items, each ranging from 1 to 5, resulting in a maximum scale score of 25. For General Health, response scales for four of the five items range from 1 = definitely true to 5 = definitely false. The remaining item ranges from 1 = excellent to 5 = poor. Vitality describes the level of energy, as opposed to tiredness. Sample items include “During the past 4 weeks, how often did you feel tired?” and “During the past 4 weeks, how often did you have a lot of energy?” Vitality is composed of 4 items, each ranging from 1 = all of the time to 6 = none of the time. Scores for this scale range from 1 to 24. Social Functioning refers to the extent to which health problems interfere with social activities, such as visiting with friends and relatives (e.g., “During the past 4 weeks, to what extent has your physical health or emotional problems interfered with your normal social activities with family, friends, neighbours, or groups?”). Social Functioning has 2 items, both ranging from 1 to 5. However, verbal anchors differ between items. For one item, the anchors range from 1 = not at all to 5 = extremely, while for the other item, anchors range from 1 = all of the time to 5 = none of the time. Role Emotional explores the impact of emotional problems on daily functioning, including a reduction in the time devoted to regular activities, as well as an impact on performance and motivation (e.g., “During the past 4 weeks, have you accomplished less than you would like at work or other regular daily activities as a result of any emotional problems, such as feeling depressed or anxious?”). Emotional Role includes 3 items using 1 = yes and 2 = no as anchors. Therefore, the maximum score for this scale is 6. Finally, Mental Health taps into aspects related to general well-being, such as depressive and anxiety symptoms, behaviour control, and overall distress. Sample items include “During the past 4 weeks, how often have you felt so down in the dumps that nothing could cheer you up?” and “During the past 4 weeks, how often have you felt calm and peaceful?” Mental Health contains 5 items. Each item ranges from 1 = all of the time to 6 = none of the time, so the scale has a maximum range score of 30.
For the sake of clarity and interpretability, each SF-36 scale score is converted to a 0-100 range (Bergman, Jacobsson, Herrström, & Petersson, 2004; McHorney, Ware, & Raczek, 1993). Higher scores indicate better health (i.e., higher scores in Bodily Pain should be interpreted as lower levels of pain and less interference of pain on functioning). A composite score can be obtained for physical (PCS) and mental health (MCS) using the aforementioned subscales. Both composite scores are linear combinations of the eight subscales (i.e., all subscales are summed). However, subscales present different weights for each composite score. For example, the subscales showing high weights on the PCS (>.3) are Physical Functioning, Role Physical, and Bodily Pain. In contrast, the subscales showing high weights on the Mental Composite Score (>.3) are Role Emotional and Mental Health. Because General Health, Vitality, and Social Functioning refer to both dimensions of health, their factor weights on each composite score are lower (Bergman et al., 2004; Vilagut et al., 2008). The PCS and the MCS have a 0-100 range, with higher scores meaning better health. Although the SF-36 has eight subscales, only the two composite scores will be used to capture patients’ experiences of overall health in the regression analyses. The reason for doing this is that the use of the PCS and the MCS reduces the number of statistical comparisons and eliminates floor and ceiling effects (Ware, Kosinski, Bayliss, McHorney, Rogers, & Raczek, 1995). The PCS should be interpreted as a measure of the individual’s perception of physical health status, as well as how physical health impacts on daily activities and social functioning. In contrast, the MCS taps into aspects of emotional well-being, including how emotional well-being influences daily activities and social functioning. The PCS and the MCS are separate but interrelated factors.
The SF-36 scales have good psychometric properties (.78 < α < .94; Alonso et al., 1998) and has been widely used in chronic pain populations. Internal consistency estimates were similar in our sample (.74 < α < .93). The Bodily Pain and the Social Functioning scales showed the smallest reliability estimates (.74 and .78, respectively), which may be due to the fact that they are the scales with the lowest number of items, only 2 each. The scale has also shown to have good construct validity. Specifically, the scales to best represent physical health (i.e., Physical Health, Role Physical, and Bodily Pain) were most valid in detecting the severity of problems in patients with medical conditions. In contrast, Role Emotional and Mental Health best distinguished between groups differing in the presence and severity of psychiatric disorders (McHorney et al., 1993).
Pain Intensity and Interference
Here we used a separate numerical rating scale to assess both its perceived intensity and interference of pain in the daily activities. This is a standard instrument in the measurement of pain (Farrar, Young, LaMoreaux, Werth, & Poole, 2001). Patients were asked to rate their current pain intensity and interference on a scale from 0 = no pain or interference to 10 = worst possible pain or interference. Even though pain intensity and pain interference are reflected in the Bodily Pain dimension from the SF-36, they refer to average pain intensity and pain interference, which can differ from current pain intensity and pain interference (Harris, Li, Flynn, & Chow, 2007), and these are frequently defined as separate assessment domains. Therefore, we decided to include the assessment of both current and average pain intensity and pain interference.
Data Analysis
First, we provide descriptive statistics (means and standard deviations) for all variables. In so doing we also explore the presence of gender differences in irrational beliefs using t tests. We provide correlations between irrational beliefs and health components.
Because, to our knowledge, the General Attitudes and Beliefs Scale has not been used in chronic pain populations, a confirmatory factor analysis (CFA) was conducted to verify that it successfully captured the original GABS constructs in our sample (construct validity). Specifically, we explored the fit of a seven-factor model, corresponding to four processes (demandingness, catastrophizing, LFT, and self-downing) and three contents (success, affiliation, and comfort). Each irrational item loaded on a process and content. The CFA was conducted with Mplus version 7.31 (Muthén & Muthén, 2015), using maximum likelihood estimation with robust standard errors to control for non-normality. Several fit indices were calculated to evaluate the adequacy of the seven-factor model (Burgess, 1986; DiGiuseppe et al., 1988): the root mean square error of approximation (RMSEA; Steiger, 1990), the comparative fit index (CFI; Bentler, 1990), and the Tucker-Lewis index (TLI; Tucker & Lewis, 1973). CFI and TLI values above .90 indicate adequate fit, while a RMSEA lower than .05 suggests good fit (Hu & Bentler, 1999). The model was estimated using maximum likelihood with robust standard errors and goodness of fit tests (Satorra & Bentler, 1994).
Then, two hierarchical regression analyses were conducted to evaluate the core aim of this article, namely, the multivariate relation between irrational processes, beyond catastrophizing, and either the PCS or the MCS. In the hierarchical regression, gender, age, and duration of pain were entered in the first step, while in the second step we added pain intensity, pain interference, and either the MCS, or the PCS. Catastrophizing was entered in the third step, while in the final step we added the remaining irrational processes (i.e. demandingness, LFT, and self-downing).
Due to the large number of statistical tests performed, we used a Bonferroni-adjusted significance level. No serious problem of multicollinearity was observed when conducting the regression analyses, since tolerance was >.25 and the variance of inflation factor (VIF) was <4 for all independent variables. Mplus v7.11 was used for the confirmatory factor analysis. SPSS 21 was used for all remaining analyses.
Results
Descriptive Statistics and Gender Differences in Pain and Health Outcomes
Overall, men reported having better health and lower pain intensity and pain interference than women (Table 1). Most of the gender differences reached significance, except for General Health and Social Functioning.
Physical and mental composite scores in our sample were comparable (between −1SD and +1SD) to those of other studies (Dysvik, Vinsnes, & Eikeland, 2004; Lamé, Peters, Vlaeyen, Kleef, & Patijn, 2005; Townsend et al., 2008). However pain ratings in this study may be high, approximately +1SD when compared to other investigations (Bendayan, Esteve, & Blanca, 2012; Gómez-Pérez, López-Martínez, & Ruiz-Párraga, 2011).
Factor Structure of the GABS-SV
The CFA replicated the original factor structure of the GABS-SV, consisting of four irrational processes (demandingness, catastrophizing, LFT, and self-downing) and three contents (success, affiliation, and comfort). Table 2 summarizes the goodness-of-fit indices of the seven-factor model, as well as the Cronbach’s alpha coefficients for the process scales. Specifically, obtained goodness-of-fit indices were: χ 2 = 383.02, df = 207, CFI = .950, TLI = .934, and RMSEA = .045. These values suggested an adequate fit of the seven-factor model. In the present dataset, the internal consistency for each of the process scales, which are the focus of this study, was .67 for demandingness, .86 for catastrophizing, .81 for LFT, and .77 for self-downing.
Gender Differences in Irrational Beliefs
Table 3 provides descriptive statistics for the GABS-SV processes, including an analysis of gender differences in irrational thinking. There were no significant differences between men and women on the measures of irrational processes; values of t ranged from −0.93 to −1.42, p > .05 in all cases.
Intercorrelations Between Study Variables
As a preliminary step in conducting the hierarchical regression analyses, we calculated the bivariate associations between study variables (Table 4). Health components of the SF-36 were significantly intercorrelated. Significant associations were also revealed between these components and the composite scores. Physical Functioning (r = .76, p < .001), Role Physical (r = .66, p < .001), and Bodily Pain (r = .65, p < .001) correlated most highly with the Physical Composite Score. Their correlation with the Mental Composite Score was significant but weaker (.22 ≤ r ≤ .35, p < .001). General Health, Vitality, and Social Functioning were related to both composite scores. Specifically, General Health correlated moderately with the Physical (r = .47, p < .001) and the Mental (r = .45, p < .001) Composite Scores. Vitality (r = .47, p < .001) and Social Functioning (r = .36, p < .001) were moderately associated with the Physical Composite Score, but strongly (.64 ≤ r ≤ .69, p < .001) linked to the Mental Composite Score. Role Emotional (r = .87, p < .001) and Mental Health (r = .88, p < .001) were highly correlated with the Mental Composite Score. Neither Role Emotional (r = −.16, p < .001) nor Mental Health (r = −.01, p > .003) were positively correlated with the Physical Composite Score. Pain intensity and pain interference were linked to poorer health ratings across all the components of the SF-36. Older people reported lower levels of Physical Functioning (r = −.38, p < .001), General Health (r = −.15, p < .001), and Physical Composite Scores (r = −.29, p < .001). Age and pain duration were also correlated (r = .15, p < .001). Additionally, pain duration was linked to decreased Physical Functioning (r = −.12, p < .003) and General Health (r = −.14, p < .003).
Table 4 also shows that irrational beliefs were significantly intercorrelated, and most of these correlations were high (.48 ≤ r ≤ .81, p < .001), although there was one notable exception, a low (albeit significant) correlation between demandingness and self-downing (r = .18, p < .001). Irrational beliefs were not associated with age, pain duration, pain intensity, or pain interference.
Irrational Beliefs and Physical Aspects of Health
Irrational processes were not significantly associated with pain intensity, pain interference, or with the physical components of health assessed by the SF-36 (Table 5). Only self-downing was associated with physical health components from the SF-36, namely, Physical Functioning (r = −.14, p < .005) and Role Physical (r = −.15, p < .001).
In the regression analyses, none of the irrational processes were significantly associated with the PCS (Table 6). The first block explained 7.9 % of the variance (F change = 13.36, p < .001), with only age (β = −.28, p < .001) being a significant predictor. In the second block, the inclusion of pain intensity, interference, and the MCS added a significant 25.7 % increment in R 2 (F change = 56.56, p < .001), with age (β = −.23, p < .001), interference (β = −.43, p < .001), and the MCS (β = −.30, p < .001) being significantly associated with the PCS. The third (F change = 0.04, p = .83) and fourth blocks (F change = 1.51, p = .21), which involved the irrational processes, were not statistically significant.
Because irrational beliefs and the MCS appeared to share a significant amount of variance (Table 7), we explored whether the lack of association between irrational beliefs and PCS was due to the inclusion of the MCS before the irrational beliefs. Therefore, we repeated the regression analysis shown in Table 6 excluding the MCS from the analyses. The relation between irrational beliefs and the PCS remained non-significant after the exclusion of the MCS.
Irrational Beliefs and Mental Components of Health
The correlation analyses showed that all irrational processes, except for demandingness, were significantly and at least moderately correlated with all components related to mental health (Table 7). By comparison, demandingness was only weakly correlated with levels of Vitality (r = −.17, p < .001), Role Emotional (r = −.14, p < .005), Mental Health (r = −.20, p < .001), and the Mental Composite Score (r = −.19, p < .001). The remaining processes of irrational thinking (i.e., catastrophizing, LFT, and self-downing) had patterns of association with mental components of health that closely paralleled one another, and which tended to be somewhat stronger than the pattern for demandingness. That is, catastrophizing, LFT, and self-downing had a weak but significant association with General Health (−.26 ≤ r ≤ −.29, p < .001), Vitality (−.26 ≤ r ≤ −.30, p < .001), and Social Functioning (−.23 ≤ r ≤ −.25, p < .001), and a moderate correlation with Role Emotional (-.39 ≤ r ≤ -.41, p < .001), Mental Health (-.44 ≤ r ≤ -.47, p < .001), and the Mental Composite Score (−.45 ≤ r ≤ −.47, p < .001).
In the final regression model (Table 8), age, gender, pain duration, pain intensity, pain interference, and the Physical Composite Score accounted for more than 21 % of the variance in the Mental Composite Score. Irrational processes added a significant 19.6 % to the prediction of the Mental Composite Score. Specifically, the inclusion of catastrophizing (β = −.40, p < .001) in the third block led to an additional 15.1 % of the variance in the Mental Composite Score being explained. In the final step, LFT (β = −.21, p < .005) and self-downing (β = −.20, p < .001) produced a further and significant 4.5 % increase in the model’s predictive power and catastrophizing ceased to contribute to the Mental Composite Score (β = −.13, p = .056). Of the covariates, only pain interference (β = −.33, p < .001) and the Physical Composite Score (β = −.29, p < .001) significantly contributed to the Mental Composite Score in the final step of the model.
Discussion
The main goal of this study was to investigate whether a wider range of irrational belief processes would have a significant association with health when controlling for catastrophizing in a sample of chronic pain patients. We expected that the irrational processes of demandingness, LFT, and self-downing would explain significant additional variance in the prediction of health.
Our results provide partial support for this hypothesis. As expected, not only catastrophizing but a broader range of irrational belief variables, notably LFT and self-downing, appear to be significantly related to mental health in chronic pain patients, even after controlling for catastrophizing. However, demandingness showed weaker associations than did the other irrational beliefs, and the significant relationship between most irrational beliefs and mental health did not extend to physical health.
The limited relation between demandingness and mental health has already been noted in previous studies (Kelly, Joyce, & Greaves, 1998), suggesting that this variable is not a core process of irrational thinking as Ellis (1962) suggested. Our results appear to provide further evidence in this direction. However, the fact that demandingness had the poorest internal consistency scores (α = .67) may have also influenced the results. Before drawing further conclusions, future investigations should address this issue by improving the psychometric properties of this scale.
In our study, irrational beliefs were more strongly related to mental than to physical aspects of health. Previous studies have shown that pain catastrophizing has a stronger correlation with mental components of health when compared to physical components (Severeijns, Vlaeyen, van den Hout, & Weber, 2001). Interestingly, however, we found no significant associations between our general measure of catastrophizing and physical aspects of health, a result that contrasts with other studies (Agar-Wilson & Jackson, 2012; de Boer, Struys, & Versteegen, 2012; Ferreira-Valente et al., 2011; Kendell, Saxby, Farrow, & Naisby, 2001; Wong et al., 2011). Pain intensity in the present sample was more intense than in other pain populations (Bendayan et al., 2012; Gómez-Pérez et al., 2011). Therefore, one possible explanation for the discrepancy between our results and previous findings is that, in the presence of intense pain, the effect of general catastrophizing is not revealed. However, it is also possible that a measure of irrational beliefs which does not specifically address pain, as in the General Attitudes and Beliefs Scale, helps explain the weak relationship between catastrophizing and physical health in the present study. In line with the latter hypothesis, there is growing evidence to suggest that the strong relationship between pain catastrophizing and pain-related physical outcomes could be partly due to the fact that pain catastrophizing is situational and pain-dependant, which would explain why changes in pain intensity can lead to changes in pain catastrophizing (Sullivan, 2012; Wade et al., 2012). Indeed, a typical pain catastrophizing item (i.e., “My pain is terrible and I feel it’s never going to get any better”) has a greater focus on pain intensity than a general catastrophizing item in the General Attitudes and Beliefs Scale (e.g., “It is terrible to have difficulties in life”), which is likely to explain the overlap between pain catastrophizing, pain intensity, and physical limitations due to pain that previous research has found. Therefore, the use of a broader, dispositional conceptualization of catastrophizing, as found in the General Attitudes and Beliefs Scale, might reduce the overlap with sensory aspects of pain (i.e., pain intensity), which are known to correlate more strongly with physical health than with mental health (Leeuw et al., 2007). As such, the non-significant association between irrational processes and pain intensity and physical health might as well be interpreted as a positive finding. Although we did not assess whether changes in pain would lead to variations in irrational beliefs, the fact that GABS-SV scores were not significantly associated with pain intensity and its physical aspects is encouraging as it provides support for the hypothesis that the GABS has a reduced overlap with sensorial aspects of pain (i.e., pain intensity). Despite this, physical health is more than a sensory dimension. Therefore, positive interpretations of the lack of relationship between irrational beliefs and physical health in the present study should be interpreted with caution.
Despite the aforementioned discrepancies in the relationship between catastrophizing and physical aspects of health, our study provides consistent support for the significant association between this irrational process and mental aspects of health. The large amount of explained variance (15.1 %) that this variable added to the prediction of the mental health composite (above and beyond the contribution of age, gender, pain duration, and physical aspects of health) provides further evidence for the relevance of this irrational process, in line with the current literature (Hanley, Raichle, Jensen, & Cardenas, 2008; Vervoort, Goubert, Eccleston, Bijttebier, & Crombez, 2006).
In addition to our findings supporting the key role of catastrophizing, our study also explored the role of other irrational processes on chronic pain. Here the results provide evidence for the relevance of two other processes: LFT and self-downing.
Although frustration tolerance has not been a focus of interest in chronic pain research, there are similarities between high frustration tolerance and acceptance. Both concepts can be considered as based on the acknowledgement of reality, regardless of whether one attempts to change this reality (Ellis & Robb, 1994; McCracken, 1998). Notably, there are certain parallels between high frustration tolerance items from the General Attitudes and Beliefs Scale (e.g., “Even though some situations are displeasing and uncomfortable, I can still function despite them”) and items used to assess acceptance (e.g., “My life is going well, even though I have chronic pain;” Wicksell, Olsson, & Melin, 2009). Congruent with our results, acceptance seems to have a positive association with pain-related outcomes (Feinstein et al., 2011; McCracken & Keogh, 2009; Wicksell et al., 2009). However, while in our study LFT had a larger correlation with mental health than did catastrophizing, acceptance seems to have a smaller association with mental health when compared to catastrophizing (Richardson et al., 2009; Vowles, McCracken, & Eccleston, 2008). The fact that LFT and acceptance are defined in opposing terms may explain such discrepancies. Thus, dysfunctional thinking (e.g., LFT) could have a stronger association with health when compared to a functional stance (e.g., acceptance). It is also possible, though, that both concepts are not two ends of the same spectrum, but potentially two distinct but related phenomena. Further studies should test these hypotheses.
The discussion about acceptance and LFT raises the question whether demandingness might also be inversely related to acceptance. Demandingness items in the GABS-SV (e.g., “I should not experience discomfort in life”) bear similarities with acceptance items (e.g., “It is OK to experience pain;” Wicksell et al., 2009). As suggested above, we encourage researchers to explore how acceptance is related to these irrational beliefs. However, as noted above, the measurement of demandingness in the GABS-SV should be refined before a comparison with acceptance is made.
From this point we move the discussion forward to the remaining irrational process, namely, self-downing. Self-downing was the only GABS-SV scale to be significantly correlated with physical health components (i.e., Physical Functioning and Role Physical). A relationship between self-downing and physical health outcomes is consistent with previous findings relating this variable to lower activity engagement (Stroud et al., 2000). One possible explanation for the relation between self-downing and physical health is that physical limitations lead to a global devaluation of the individual (i.e., “I am a useless person if I cannot achieve my goals”). It may also be that the use of self-downing statements also increases physical limitations through inactivity, which could be triggered by a self-fulfilling prophecy type of belief that has the form: “I am a useless person; therefore, it’s not worth trying to achieve my goals”. Further research is needed in order to test both hypotheses as causal associations cannot be drawn from the present investigation.
It is unclear why self-downing was the only irrational belief to correlate to physical components of health. Previous research has shown that self-downing was more intensely associated with a measure of physical functioning (e.g., activity level) when compared with other pain-related beliefs, e.g., the belief that pain is permanent, or the belief that one is to blame for one’s pain (Stroud et al., 2000). However, no study had combined self-downing together with other measures of irrational thinking in the context of pain. Several factors may explain why self-downing was the only belief to correlate with physical components of health in the current study. First, it is important to note that self-downing was only moderately associated with the remaining beliefs in the present study (i.e., demandingness, catastrophizing, and LFT). This suggests that self-downing taps into aspects of irrational thinking that are not shared by the remaining irrational beliefs. Specifically, self-downing is a component of irrational thinking that puts more emphasis on an individual’s self-evaluation, e.g., a belief such as “I am useless,” as opposed to evaluations of the situation, e.g., beliefs such as “The situation is awful,” or “The situation is unbearable.” To our understanding, this focus on one’s self rather than the situation might be an important factor explaining why self-downing was the only irrational belief to correlate with physical health outcomes. However, this hypothesis should be tested in future studies. In addition to the relation between self-downing and physical health outcomes, findings in the present investigation are also in line with previous findings suggesting that this belief has a negative association with mental health (Luyten et al., 2011; Stroud et al., 2000). Furthermore, in our study, the relation of self-downing with mental health seems to be independent of other pain-related beliefs, catastrophizing and LFT, which is again consistent with the report by Stroud et al. (2000).
Our results suggest that both LFT and self-downing should be considered together with catastrophizing when exploring the relation between beliefs and mental health. Note that these three irrational beliefs, as a group, explained a non-negligible 19.7 % of the variance of mental health, even when controlling for the contribution of physical outcomes.
An interesting finding in the present study is that men presented with higher self-rated mental health than females despite the absence of gender differences in irrational beliefs. Therefore, even though we found that irrational beliefs correlated with mental health, irrational beliefs do not seem to explain gender differences in mental health in our sample. As other researchers sometimes report, robust gender differences may often be found (Afifi, 2007). However, the reasons for such differences are complex and not easily understood (Fanous, Gardner, Prescott, Cancro, & Kendler, 2002; Kendler, Kuhn, & Prescott, 2004; Piccinelli & Wilkinson, 2000).
Our study does have certain limitations. Although we found that irrational beliefs are related to self-reports of one’s health, the fact that we used a cross-sectional design prevents us from establishing any causal relationships. Therefore, while our results might be interpreted as irrational beliefs impacting on beliefs about one’s health status, it is also possible that health has an influence on irrational thinking. For example, as an individual’s health worsens, he or she may become more self-critical and be more likely to catastrophize. While acknowledging that health status can impact irrational thinking, psychological treatment addressing irrational beliefs has already been shown to have positive effects on various health-related outcomes in hypertensive asthma, and breast cancer patients (David et al., 2010), suggesting that irrational beliefs have the potential to influence health status. People with chronic pain might well benefit from these interventions, too. We therefore encourage researchers to conduct studies of treatment process and outcome in order to explore whether a reduction in these irrational beliefs would indeed lead to an improvement in mental health and general functioning.
Also, our results may not be generalizable to all pain populations given the heterogeneity of our sample. While acknowledging this limitation, the fact that pain diagnosis distributions (Lamé et al., 2005; De Boer et al., 2012) and physical and mental health ratings (Dysvik et al., 2004; Lamé et al., 2005; Townsend et al., 2008) were comparable to those reported in other similar studies suggests that our sample may nonetheless be representative of chronic pain populations attending pain clinics. Another limitation refers to the pain levels presented by patients in the present investigation. As previously noted, the mean pain intensity reported in our sample was approximately one standard deviation higher than in other similar studies. If the relationship between irrational beliefs and health varied across different levels of pain intensity (i.e., if pain was a moderator), the associations found in the present investigation might be different in populations with lower pain levels. If, indeed, pain was a moderator, we believe that the strength of the relationship between irrational beliefs and health would increase when assessing a sample with lower levels of pain. This hypothesis comes from research showing that the influence of personality characteristics increases when situational factors are less compelling determinants of behavior (Higgins & Scholer, 2008). Finally, the impact of co-morbid anxiety and mood disorders was not tested in the present investigation. Depression and anxiety levels are known to impact self-reported health status (Huijnen et al., 2010; Meredith, Strong, & Feeney, 2006). Further research should explore how co-morbidity influences the relationship between irrational beliefs and health status.
Despite these limitations, we did avoid a number of shortcomings that are frequent in the literature, such as small sample sizes or uncorrected significance levels when performing multiple comparisons (Asghari & Nicholas, 1999), and this makes our findings potentially more robust. In addition, the fact that the General Attitudes and Beliefs Scale uses item content that is independent of behaviour and emotion should help to overcome a critical drawback of some measures currently used in this area. Specifically, and as noted by Affleck, Tennen, Urrows, & Higgins (1992), some measures of pain catastrophizing may be focusing too heavily on emotional aspects of pain rather than on cognitive processes. In addition, we believe that current measures of pain catastrophizing are too dependent on pain intensity scores (Sullivan, 2012; Wade et al., 2012), and so favor the use of a broader conceptualization of pain catastrophizing as is found in GABS-SV items. This would be congruent with other findings that emphasize the importance of general metacognitive processes in chronic pain (Yoshida et al., 2012).
Given that irrational beliefs may act as cognitive vulnerability factors for distress in the presence of negative situations (Cristea, Montgomery, Szamoskozi, & David, 2013) such as pain, we suggest that addressing these dispositions towards irrationality rather than focusing on specific distortions related to a stressor (i.e., pain) might help patients to generalize changes to a wider range of conditions. Pain is probably not the only stressful situation that patients go through, and, therefore, interventions that address their general schemas might promote better functioning and lead to less suffering in various settings. Note that irrational beliefs were not associated with pain intensity in our study. Therefore, the use of such general schemas might help to detect risk factors for mental health problems even when pain is significantly reduced.
The aforementioned issues in existent measures of catastrophizing have been a major topic of debate recently, and these preliminary findings suggest that the General Attitudes and Beliefs Scale can satisfactorily overcome some of the shortcomings of other current methods. Hence, we suggest that this scale might offer an alternative way of measuring general catastrophizing in chronic pain patients. The fact that we were able to replicate the factor structure of the GABS in our chronic pain sample is an important step in this regard.
In summary, our results are consistent with previous research supporting the importance of irrational beliefs in the assessment of general personal functioning (Harrington, 2011). Also congruent with a vast literature in the field, catastrophizing correlated considerably with mental health in chronic pain patients. In addition to replicating existent results, our study extends findings from previous research demonstrating that two additional processes, LFT and self-downing, also appear to be significantly associated with mental health, above and beyond catastrophizing. This points to potential new targets in the psychological treatment of chronic pain patients.
References
Affleck, G., Tennen, H., Urrows, S., & Higgins, P. (1992). Neuroticism and the pain-mood relation in rheumatoid arthritis: Insights from a prospective daily study. Journal of Consulting and Clinical Psychology, 60(1), 119–126. doi:10.1037/0022-006X.60.1.119.
Afifi, M. (2007). Gender differences in mental health. Singapore Medical Journal, 48(5), 385–391. doi:10.1177/0020764010390431.
Agar-Wilson, M., & Jackson, T. (2012). Are emotion regulation skills related to adjustment among people with chronic pain, independent of pain coping? European Journal of Pain, 16(1), 105–114. doi:10.1016/j.ejpain.2011.05.011.
Alonso, J., Regidor, E., Barrio, G., Prieto, L., Rodrigues, C., & de la Fuente, L. (1998). Valores poblacionales de referencia de la versión española del Cuestionario de Salud SF-36 [Population-based reference values for the Spanish version of the health Survey SF-36]. Medicina Clinica (Barc), 111, 410–416.
Asghari, A., & Nicholas, M. K. (1999). Personality and adjustment to chronic pain. Pain Reviews, 6, 85–97.
Bendayan, R., Esteve, R., & Blanca, M. J. (2012). New empirical evidence of the validity of the Chronic Pain Acceptance Questionnaire: The differential influence of activity engagement and pain willingness on adjustment to chronic pain. British Journal of Health Psychology, 17(2), 314–326. doi:10.1111/j.2044-8287.2011.02039.x.
Bentler, P. M. (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107(2), 238–246. doi:10.1037/0033-2909.107.2.238.
Bergman, S., Jacobsson, L. T. H., Herrström, P., & Petersson, I. F. (2004). Health status as measured by SF-36 reflects changes and predicts outcome in chronic musculoskeletal pain: A 3-year follow up study in the general population. Pain, 108(1–2), 115–123. doi:10.1016/j.pain.2003.12.013.
Bernard, M. E. (1998). Validation of the General Attitude and Belief Scale. Journal of Rational-Emotive & Cognitive-Behavior Therapy, 16(3), 183–196. doi:10.1023/A:1024911014579.
Bridges, K. R., & Harnish, R. J. (2010). Role of irrational beliefs in depression and anxiety: A review. Health, 02(08), 862–877. doi:10.4236/health.2010.28130.
Burgess, P. M. (1986). Belief systems and emotional disturbance: evaluation of the rational-emotive model. (Unpublished doctoral dissertation). University of Melbourne, Parkville, Melbourne, Australia.
Caballo, V. E., Lega, L. I., & González, S. (1996). A factor analysis of a back translated Spanish version of the Scale of Attitudes and Beliefs (SAB). New York.
Chen, H. Y., & Boore, J. R. P. (2010). Translation and back-translation in qualitative nursing research: Methodological review. Journal of Clinical Nursing, 19(193), 234–239. doi:10.1111/j.1365-2702.2009.02896.x.
Cristea, I. A., Montgomery, G. H., Szamoskozi, S., & David, D. (2013). Key constructs in “ Classical ” and “ New Wave ” cognitive behavioral psychotherapies : Relationships among each other and with emotional distress. Journal of Clinical Psychology, 69(6), 584–599. doi:10.1002/jclp.21976.
David, D., Lynn, S. J., & Ellis, A. (2010). Rational and irrational beliefs (I. N. Y. Oxford University Press, Ed.). New York: Oxford University Press Inc.
De Boer, M. J., Struys, M. M. R. F., & Versteegen, G. J. (2012). Pain-related catastrophizing in pain patients and people with pain in the general population. European Journal of Pain, 16(7), 1044–1052. doi:10.1002/j.1532-2149.2012.00136.x.
DiGiuseppe, R., Leaf, R., Exner, T., & Robin, M. V. (1988). The development of a measure of rational/irrational thinking. Paper presented at the World Congress of Behavior.
Dysvik, E., Vinsnes, A. G., & Eikeland, O.-J. (2004). The effectiveness of a multidisciplinary pain management programme managing chronic pain. International Journal of Nursing Practice, 10(5), 224–234. doi:10.1111/j.1440-172X.2004.00485.x.
Ellis, A. (1962). Reason and emotion in psychotherapy. New York: Lyle Stuart.
Ellis, A., & Robb, H. (1994). Acceptance in rational emotive therapy. In S. C. Hayes, N. S. Jacobson, V. M. Follette, & M. J. Dougher (Eds.), Acceptance and change: Content and context in psychotherapy. Reno, NV: Context Press.
Erdemoglu, Â. K., & Koc, R. (2013). Brief Pain Inventory score identifying and discriminating neuropathic and nociceptive pain. Acta Neurologica Scandinavica. doi:10.1111/ane.12131.
Fanous, A., Gardner, C. O., Prescott, C. A., Cancro, R., & Kendler, K. S. (2002). Neuroticism, major depression and gender: A population-based twin study. Psychological Medicine, 32(04), 719–728. doi:10.1017/S003329170200541X.
Farrar, J. T., Young, J. P., LaMoreaux, L., Werth, J. L., & Poole, R. M. (2001). Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain, 94(2), 149–158. doi:10.1016/S0304-3959(01)00349-9.
Feinstein, A. B., Forman, E. M., Masuda, A., Cohen, L. L., Herbert, J. D., Moorthy, L. N., & Goldsmith, D. P. (2011). Pain intensity, psychological inflexibility, and acceptance of pain as predictors of functioning in adolescents with juvenile idiopathic arthritis: A preliminary investigation. Journal of Clinical Psychology in Medical Settings, 18(3), 291–298. doi:10.1007/s10880-011-9243-6.
Ferreira-Valente, M. A., Pais Ribeiro, J. L., Jensen, M. P., & Almeida, R. (2011). Coping with chronic musculoskeletal pain in Portugal and in the United States: A cross-cultural study. Pain Medicine, 12(10), 1470–1480. doi:10.1111/j.1526-4637.2011.01208.x.
Flink, I. K., Boersma, K., MacDonald, S., & Linton, S. J. (2012). Understanding catastrophizing from a misdirected problem-solving perspective. British Journal of Health Psychology, 17(2), 408–419. doi:10.1111/j.2044-8287.2011.02044.x.
Freynhagen, R., & Baron, R. (2009). The evaluation of neuropathic components in low back pain. Current Pain and Headache Reports, 13(3), 185–190. doi:10.1007/s11916-009-0032-y.
George, S. Z., Calley, D., Valencia, C., & Beneciuk, J. M. (2011). Clinical investigation of pain-related fear and pain catastrophizing for patients with low back pain. The Clinical Journal of Pain, 27(2), 108–115. doi:10.1097/AJP.0b013e3181f21414.
Gómez-Pérez, L., López-Martínez, A. E., & Ruiz-Párraga, G. T. (2011). Psychometric properties of the Spanish Version of the Tampa Scale for Kinesiophobia (TSK). The Journal of Pain, 12(4), 425–435. doi:10.1016/j.jpain.2010.08.004.
Hadjistavropoulos, H., Dash, H., Hadjistavropoulos, T., & Sullivan, T.-L. (2007). Recurrent pain among university students: Contributions of self-efficacy and perfectionism to the pain experience. Personality and Individual Differences, 42(6), 1081–1091. doi:10.1016/j.paid.2006.09.013.
Hanley, M. A., Raichle, K., Jensen, M. P., & Cardenas, D. D. (2008). Pain catastrophizing and beliefs predict changes in pain interference and psychological functioning in persons with spinal cord injury. The Journal of Pain, 9(9), 863–871. doi:10.1016/j.jpain.2008.04.008.
Harrington, N. (2011). Frustration intolerance: Therapy issues and strategies. Journal of Rational-Emotive & Cognitive-Behavior Therapy, 29(1), 4–16. doi:10.1007/s10942-011-0126-4.
Harris, K., Li, K., Flynn, C., & Chow, E. (2007). Worst, average or current pain in the Brief Pain Inventory: Which should be used to calculate the response to palliative radiotherapy in patients with bone metastases? Clinical Oncology (Royal College of Radiologists (Great Britain), 19(7), 523–527. doi:10.1016/j.clon.2007.04.007.
Higgins, E. T., & Scholer, A. A. (2008). When is personality revealed? A motivated cognition approach. In O. P. John, R. W. Robins, & L. A. Pervin (Eds.), Handbook of personality. Theory and research (3rd ed., p. 862). New York: The Guilford Press.
Hirsh, A. T., George, S. Z., Riley, J. L., & Robinson, M. E. (2007). An evaluation of the measurement of pain catastrophizing by the coping strategies questionnaire. European Journal of Pain, 11(1), 75. doi:10.1016/j.ejpain.2005.12.010.
Hu, L., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. doi:10.1080/10705519909540118.
Huijnen, I. P. J., Verbunt, J. a, Peters, M. L., Delespaul, P., Kindermans, H. P. J., Roelofs, J., … Seelen, H. A. M. (2010). Do depression and pain intensity interfere with physical activity in daily life in patients with Chronic Low Back Pain? Pain, 150(1), 161–6. doi: 10.1016/j.pain.2010.04.021.
Kelly, M. O., Joyce, M. R., & Greaves, D. (1998). The primacy of the “shoulds”: Where is the evidence? Journal of Rational-Emotive & Cognitive-Behavior Therapy, 16(4), 223–234. doi:10.1023/A:1024960402090.
Kendell, K., Saxby, B., Farrow, M., & Naisby, C. (2001). Psychological factors associated with short-term recovery from total knee replacement. British Journal of Health Psychology, 6(Pt 1), 41–52. doi:10.1348/135910701169043.
Kendler, K. S., Kuhn, J., & Prescott, C. A. (2004). The interrelationship of neuroticism, sex, and stressful life events in the prediction of episodes of major depression. American Journal of Psychiatry, 161(4), 631–636. doi:10.1176/appi.ajp.161.4.631.
Lamé, I. E., Peters, M. L., Vlaeyen, J. W. S., Kleef, M. V., & Patijn, J. (2005). Quality of life in chronic pain is more associated with beliefs about pain, than with pain intensity. European Journal of Pain, 9(1), 15–24. doi:10.1016/j.ejpain.2004.02.006.
Lee, E.-J., Wu, M.-Y., Lee, G. K., Cheing, G., & Chan, F. (2008). Catastrophizing as a cognitive vulnerability factor related to depression in workers’ compensation patients with chronic musculoskeletal pain. Journal of Clinical Psychology in Medical Settings, 15(3), 182–192. doi:10.1007/s10880-008-9118-7.
Leeuw, M., Goossens, M. E. J. B., Linton, S. J., Crombez, G., Boersma, K., & Vlaeyen, J. W. S. (2007). The fear-avoidance model of musculoskeletal pain: Current state of scientific evidence. Journal of Behavioral Medicine, 30, 77–94. doi:10.1007/s10865-006-9085-0.
Lega, L. I., Caballo, V. E., & Ellis, A. (2002). Teoría y práctica de la terapia racional emotivo-conductual [Theory and practice of rational emotive behavior therapy] (2nd ed.). Madrid: Siglo XXI.
Lega, L. I., & Ellis, A. (2001). Rational Emotive Behavior Therapy (REBT) in the new millenium: A cross-cultural approach. Journal of Rational-Emotive & Cognitive-Behavior Therapy, 19(4), 201–222. doi:10.1023/A:1012537814117.
Luyten, P., Kempke, S., Van Wambeke, P., Claes, S., Blatt, S. J., & Van Houdenhove, B. (2011). Self-critical perfectionism, stress generation, and stress sensitivity in patients with chronic fatigue syndrome: Relationship with severity of depression. Psychiatry, 74(1), 21–30. doi:10.1521/psyc.2011.74.1.21.
McCracken, L. M. (1998). Learning to live with the pain: Acceptance of pain predicts adjustment in persons with chronic pain. Pain, 74(1), 21–27. doi:10.1016/S0304-3959(97)00146-2.
McCracken, L. M., & Eccleston, C. (2003). Coping or acceptance: What to do about chronic pain? Pain, 105(1–2), 197–204. doi:10.1016/S0304-3959(03)00202-1.
McCracken, L. M., & Keogh, E. (2009). Acceptance, mindfulness, and values-based action may counteract fear and avoidance of emotions in chronic pain: An analysis of anxiety sensitivity. The Journal of Pain, 10(4), 408–415. doi:10.1016/j.jpain.2008.09.015.
McHorney, C. A., Ware, J. E., & Raczek, A. E. (1993). The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Medical Care, 31(3), 247–63. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8450681.
Meredith, P., Strong, J., & Feeney, J. A. (2006). Adult attachment, anxiety, and pain self-efficacy as predictors of pain intensity and disability. Pain, 123(1–2), 146–154. doi:10.1016/j.pain.2006.02.025.
Moix, J., Kovacs, F. M., Martín, A., Plana, M. N., & Royuela, A. (2011). Catastrophizing, state anxiety, anger, and depressive symptoms do not correlate with disability when variations of trait anxiety are taken into account: A study of chronic low back pain patients treated in Spanish pain units [NCT00360802]. Pain Medicine (Malden, Mass.), 12(7), 1008–1017. doi:10.1111/j.1526-4637.2011.01155.x.
Muris, P., Meesters, C., van den Hout, A., Wessels, S., Franken, I., & Rassin, E. (2007). Personality and temperament correlates of pain catastrophizing in young adolescents. Child Psychiatry and Human Development, 38(3), 171–181. doi:10.1007/s10578-007-0054-9.
Muthén, L. K., & Muthén, B. O. (1998–2015). Mplus User’s Guide. Seventh Edition. Los Angeles: Muthén & Muthén.
Nieto, R., Miró, J., Huguet, A., & Saldaña, C. (2011). Are coping and catastrophising independently related to disability and depression in patients with whiplash associated disorders? Disability and Rehabilitation, 33(5), 389–398. doi:10.3109/09638288.2010.491576.
Piccinelli, M., & Wilkinson, G. (2000). Gender differences in depression. Critical review. The British Journal of Psychiatry, 177(6), 486–492. doi:10.1192/bjp.177.6.486.
Ramírez Maestre, C., Esteve Zarazaga, R., & López Martínez, A. E. (2001). Neuroticismo, afrontamiento y dolor crónico [Neuroticism, coping, and chronic pain]. Anales de Psicología, 17(1), 129–137.
Richardson, E. J., Ness, T. J., Doleys, D. M., Baños, J. H., Cianfrini, L., & Richards, J. S. (2009). Depressive symptoms and pain evaluations among persons with chronic pain: Catastrophizing, but not pain acceptance, shows significant effects. Pain, 147(1–3), 147–152. doi:10.1016/j.pain.2009.08.030.
Satorra, A., & Bentler, P. M. (1994). Corrections to test statistics and standard errors in covariance structure analysis. In A. von Eye & C. C. Clogg (Eds.), Latent variable analysis: Applications for developmental research (pp. 399–419). Thousand Oaks, CA: Sage.
Sava, F. A. (2009). Maladaptive schemas, irrational beliefs, and their relationship with the five-factor personality model. Journal of Cognitive and Behavioral Psychotherapies, 9(2), 135–147.
Severeijns, R., Vlaeyen, J. W. S., van den Hout, M. A., & Weber, W. E. J. (2001). Pain catastrophizing predicts pain intensity, disability, and psychological distress independent of the level of physical impairment. The Clinical Journal of Pain, 17(2), 165–172. doi:10.1097/00002508-200106000-00009.
Steiger, J. H. (1990). Structural model evaluation and modification: An interval estimation approach. Multivariate Behavioral Research, 25(2), 173–180. doi:10.1207/s15327906mbr2502_4.
Stroud, M. W., Thorn, B. E., Jensen, M. P., & Boothby, J. L. (2000). The relation between pain beliefs, negative thoughts, and psychosocial functioning in chronic pain patients. Pain, 84(2–3), 347–52. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10666540.
Sullivan, M. J. L. (2012). The communal coping model of pain catastrophising: Clinical and research implications. Canadian Psychology/Psychologie Canadienne, 53(1), 32–41. doi:10.1037/a0026726.
Suso-Ribera, C., Camacho-Guerrero, L., McCracken, L.M., Maydeu-Olivares, A., & Gallardo-Pujol, D. (2014). Social problem solving in chronic pain: An integrative model of coping predicts mental health in chronic pain patients. Journal of Health Psychology. doi.10.1177/1359105314544133.
Townsend, C. O., Kerkvliet, J. L., Bruce, B. K., Rome, J. D., Hooten, W. M., Luedtke, C. A., & Hodgson, J. E. (2008). A longitudinal study of the efficacy of a comprehensive pain rehabilitation program with opioid withdrawal: Comparison of treatment outcomes based on opioid use status at admission. Pain, 140(1), 177–189. doi:10.1016/j.pain.2008.08.005.
Tucker, L. R., & Lewis, C. (1973). A reliability coefficient for maximum likelihood factor analysis. Psychometrika, 38, 1–10. doi:10.1007/BF02291170.
Vervoort, T., Goubert, L., Eccleston, C., Bijttebier, P., & Crombez, G. (2006). Catastrophic thinking about pain is independently associated with pain severity, disability, and somatic complaints in school children and children with chronic pain. Journal of Pediatric Psychology, 31(7), 674–683. doi:10.1093/jpepsy/jsj059.
Vilagut, G., María Valderas, J., Ferrer, M., Garin, O., López-García, E., & Alonso, J. (2008). Interpretación de los cuestionarios de salud SF-36 y SF-12 en España: componentes físico y mental [Interpretation of the SF-36 and the SF-12 questionnaires in Spain: Physical and mental components]. Medicina Clínica, 130(19), 726–735. doi:10.1157/13121076.
Vowles, K. E., McCracken, L. M., & Eccleston, C. (2008). Patient functioning and catastrophizing in chronic pain: The mediating effects of acceptance. Health Psychology, 27(2 Suppl), S136–S143. doi:10.1037/0278-6133.27.2(Suppl.).S136.
Wade, J. B., Dougherty, L. M., Archer, C. R., & Price, D. D. (1996). Assessing the stages of pain processing: A multivariate analytical approach. Pain, 68(1), 157–167. doi:10.1016/S0304-3959(96)03162-4.
Wade, J. B., Riddle, D. L., & Thacker, L. R. (2012). Is pain catastrophizing a stable trait or dynamic state in patients scheduled for knee arthroplasty? The Clinical Journal of Pain, 28(2), 122–128. doi:10.1097/AJP.0b013e318226c3e2.
Ware, J., Kosinski, M., Bayliss, M., McHorney, C., Rogers, W., & Raczek, A. (1995). Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. Medical Care, 33(4 Suppl), AS264–AS279.
Wicksell, R. K., Olsson, G. L., & Melin, L. (2009). The Chronic Pain Acceptance Questionnaire (CPAQ)-further validation including a confirmatory factor analysis and a comparison with the Tampa Scale of Kinesiophobia. European Journal of Pain, 13(7), 760–768. doi:10.1016/j.ejpain.2008.09.003.
Wong, W. S., Williams, D. A., Mak, K. H., & Fielding, R. (2011). Assessing attitudes toward and beliefs about pain among Chinese patients with chronic pain: Validity and reliability of the Chinese version of the Pain Beliefs and Perceptions Inventory (ChPBPI). Journal of Pain and Symptom Management, 42(2), 308–318. doi:10.1016/j.jpainsymman.2010.10.263.
Woolf, C. J. (2004). Pain: Moving from symptom control toward mechanism-specific pharmacologic management. Annals of Internal Medicine, 140(6), 441–451. doi:10.7326/0003-4819-140-8-200404200-00010.
Yoshida, T., Molton, I. R., Jensen, M. P., Nakamura, T., Arimura, T., Kubo, C., & Hosoi, M. (2012). Cognitions, metacognitions, and chronic pain. Rehabilitation Psychology, 57(3), 207–213. doi:10.1037/a0028903.
Acknowledgments
Funding for this study was provided by Ministerio de Educación y Cultura (Spanish Government, FPU-AP2010-5585), Ministerio de Economía y Competitividad (Spanish Government, PSI2012-33601), AGAUR (Catalan Government, 2009-SGR-74), Fundació Pedro i Pons (University of Barcelona, Spain), and Society of Multivariate Experimental Psychology.
Author contributions
Carlos Suso-Ribera, Montsant Jornet-Gibert, Maria Victoria Ribera-Canudas, David Gallardo-Pujol and Alberto Maydeu-Olivares designed the project. Carlos Suso-Ribera gathered the data and conducted the analysis. Lance M. McCracken helped with the interpretation of data. Carlos Suso-Ribera wrote the first draft and all the authors then critically revised it. The final manuscript was read and approved by all named authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Carlos Suso-Ribera, Montsant Jornet-Gibert, Maria Victoria Ribera Canudas, Lance M. McCracken, Alberto Maydeu-Olivares, and David Gallardo-Pujol declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Rights and permissions
About this article
Cite this article
Suso-Ribera, C., Jornet-Gibert, M., Ribera Canudas, M.V. et al. There’s More Than Catastrophizing in Chronic Pain: Low Frustration Tolerance and Self-Downing Also Predict Mental Health in Chronic Pain Patients. J Clin Psychol Med Settings 23, 192–206 (2016). https://doi.org/10.1007/s10880-016-9454-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10880-016-9454-y