Abstract
Intraoperative neurophysiological monitoring (IONM) is widely used in spinal cord tumors (SCTs) removal surgery. This study mainly hypothesized that patients with prolonged latency of preoperative somatosensory evoked potentials (preSEPLat) would have more deteriorated intraoperative evoked potentials. Among 506 patients who underwent SCTs removal surgery, 74 underwent both preSEPs and IONM. The correlation between preSEPLat and intraoperative SEPs (ioSEPs) was mainly analyzed, and subgroup analysis according to anatomical type was also conducted. Secondly, whether preSEPLat related to intraoperative motor evoked potentials (ioMEPs) or postoperative motor deterioration (PMD) was analyzed. In addition, risk factors for PMD were examined among anatomical factors, including operation level, tumor-occupying area ratio, and anatomical type, as well as electrophysiological factors, such as preSEPLat, ioSEPs, and ioMEPs. Changes in ioSEP and ioMEP were considered significant even if they were recovered before the end of the monitoring. Patients with prolonged preSEPLat were more likely to have significant ioSEP changes for intradural-extramedullary (IDEM) but not for intramedullary or extradural tumors. The anatomical type and tumor-occupying area ratio were prognostic factors for transient PMD, while the ioSEPs were the only prognostic factor for persisted PMD over 4 weeks after surgery. PreSEPs are helpful in predicting the significant changes in ioSEPs during IDEM tumor removal surgery. The tumor-occupying area ratio and anatomical type are contributing factors for the transient PMD, whereas ioSEPs are prognostic factors in predicting the PMD that persists over 4 weeks after SCTs removal surgery. To our knowledge, this is the first study that mainly focused on the correlations of preoperative and intraoperative evoked potentials.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Patients with spinal cord tumors (SCTs) usually undergo surgical tumor removal, and preoperative electrodiagnostic studies can provide functional information of these patients. Since compromised somatosensory evoked potentials (SEPs) imply myelopathy in the absence of a brain or peripheral nerve lesion, neurosurgeons often refer to the result of preoperative electrodiagnosis to decide whether to proceed with the operation. Particularly, in cases in which the clinical symptoms do not correlate with the lesions confirmed in imaging studies, the results of the preoperative evoked potentials (EPs) may play an important role in determining whether to perform the operation.
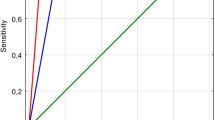
Intraoperative neurophysiological monitoring (IONM) is widely used in spinal surgery to reduce iatrogenic damage. As preoperative EPs are known to reflect the preoperative neurologic condition, many studies have shown that changes in intraoperative EPs can predict the postoperative neurological deterioration. However, in this relation chain, the link between preoperative and intraoperative EPs has not been studied (Fig. 1). Thus, to the best of our knowledge, this is the first study planned to test the hypothesis that patients with compromised preoperative EPs would have more significant deterioration in intraoperative EPs. If this hypothesis is substantiated, stricter enforcement of IONM will be recommended to give a warning in cases where intraoperative EPs are expected to show significant changes. In addition, preoperative EPs can also be regarded as one of the contributing factors for postoperative motor deterioration (PMD).
Study aims to reveal the correlations between preoperative and intraoperative evoked potentials. As preoperative evoked potentials (Eps) are known to reflect the preoperative neurologic condition, many studies have shown that changes in intraoperative EPs can predict the postoperative neurological deterioration. However, in this relation chain, the link between preoperative and intraoperative EPs has not been studied. Thus, this is the first study planned to test the hypothesis that patients with compromised preoperative EPs would have more significant deterioration in intraoperative EPs
Since the anatomical type of SCTs is one of the important factors in determining the postoperative neurological prognosis, we made a sub-analysis by anatomical type to reveal the correlation of preoperative EPs with intraoperative EPs and PMD. Moreover, as the prognosis may vary depending on the tumor size even within the same anatomical type, the tumor size was also considered for the statistical analysis.
Combined motor evoked potentials (MEPs) and D-waves monitoring has been recommended in SCT removal surgery for long-term outcomes [1,2,3]. When D-wave monitoring is unavailable, MEP monitoring should be performed for favorable outcomes [2, 4, 5]. Previous studies have suggested that intraoperative monitoring of MEPs, which electrophysiologically represent the corticospinal tract, are superior to the monitoring of SEPs in predicting PMD [6]. However, the intraoperative somatosensory evoked potential (ioSEP) has been also suggested as a supportive tool for predicting the motor outcomes after neurosurgery [7,8,9]. Studies have reported that the ioSEP is a sensitive modality for indirectly monitoring the corticospinal tract, as it can monitor the somatosensory tract directly, suggesting that the conduction blocks of the corticospinal tract and somatosensory tract mostly occur together during SCT surgery [10,11,12]. A recent meta-analysis of studies on IONM during SCT removal surgery revealed that the MEPs have higher specificity than the SEPs for assessing postoperative neurological deterioration; however, the SEPs have similar sensitivity to the MEPs [13]. Although the SEPs do not basically reflect the neurophysiological function of the corticospinal tract, case reports have discussed postoperative motor weakness even if there was only a change in the ioSEPs [14,15,16]. Moreover, conducting a simple comparative analysis between the preoperative and intraoperative MEPs is difficult, since the stimulating methods for invoking MEPs differ for each evaluating situation. Transcranial magnetic stimulation was used for the preoperative evaluation, and transcranial electrical stimulation was used for the evaluation of the intraoperative MEPs (ioMEPs). In addition, invoking the MEPs in the lower extremities is difficult using magnetic stimulation, and a specialized stimulating coil is required to induce the MEPs in the muscles of the lower extremities. Therefore, we decided to analyze mainly the SEPs rather than the MEPs for assessing the correlations between the preoperative and intraoperative EPs to determine the relevance of whether preoperative electrodiagnosis can predict the IONM outcomes.
2 Methods
2.1 Study design
This retrospective cohort study was performed in a tertiary hospital. The study protocol was approved by the institutional review board (IRB) (3-2019-0108) and conducted in accordance with the Declaration of Helsinki. The IRB confirmed that informed consent is not required because this study complies with standard practice and does not expose patient-identifiable information.
2.2 Study population
Between January 2013 and April 2017, patients with SCTs who underwent tumor removal surgery under IONM were screened. Among 506 screened patients, 89 had preoperative electrodiagnostic data, including preoperative SEPs (preSEPs). Among these, 15 patients were not included based on the following exclusion criteria: patients who were monitored only for a single modality, i.e., either ioMEPs or ioSEPs (n = 13), and patients who did not survive until 4 weeks after surgery (n = 2). Finally, the medical records of 74 patients were reviewed and collected data were analyzed, including the preSEPs, ioSEPs, ioMEPs, preoperative motor scores, postoperative motor scores, preoperative magnetic resonance imaging (MRI), operation notes, anesthesia records, and outpatient clinical notes.
2.3 PreSEPs, ioSEPs, and ioMEPs
A day before surgery, preSEPs were evaluated in an electromagnetically shielded room with Medelec Synergy electromyogram equipment (Oxford Instrument Medical Ltd., Surrey, UK) by a skilled physiatrist. Prior to the SEP evaluation, nerve conduction studies of the extremities were performed to exclude possible peripheral nerve lesions. The motor and sensory nerves of the bilateral median, ulnar, peroneal, or tibial nerves were included. The preSEPs were obtained by stimulating the bilateral median or ulnar nerves at the wrists or by stimulating the bilateral peroneal or posterior tibial nerves at the ankles (duration, 0.2 ms; repetition rate, 5 Hz), recording at C3 (right median or ulnar nerve); C4 (left median or ulnar nerve); and Cz (right and left peroneal or tibial nerve), and referencing FPz according to the international 10–20 EEG system. Considering the age and the height of the patients, the prolonged latency of preSEPs (preSEPLat) in any side of any examined nerve was considered “prolonged preSEPLat,” and acceptable preSEPLat in all examined nerves were considered “acceptable preSEPLat [17].” The amplitudes of preSEPs were not accounted for since the absolute values of the SEP amplitudes considerably vary for each individual.
All surgical procedures were performed with a posterior approach in the prone position. The ioSEPs were elicited by the same protocol of preSEPs using Cascade® IONM system (Cadwell Industries Inc., Kennewick, WA, USA). Prolongation of latency of > 10% from the baseline latency or amplitude reduction of > 50% from the baseline peak-to-peak amplitude in any side of any examined nerve was indicative of significantly deteriorated ioSEPs. When the ioSEPs changed beyond these criteria during the surgery, this change was considered a significant deterioration even if some recovery was made at the end of the surgery.
Transcranial electrical stimulation MEPs were obtained from the bilateral abductor pollicis brevis and tibialis anterior muscles. Train stimuli which consisted of six square-wave stimuli (duration, 0.5 ms; interstimulus interval, 5 ms; repetition rate, 2 Hz; stimulating intensity gradually escalated, from 50 to 400 mV) (Cascade; Cadwell Industries Inc., Kennewick, WA, USA) were delivered through needle electrodes placed at C1 and C2, according to the international 10–20 EEG system. C1/C2 and C2/C1 montage were used to measure ioMEPs of the right and left extremities, respectively. A reduction of > 50% in the ioMEP amplitude compared with the baseline ioMEPs was considered a significant change. When the amplitude of the ioMEPs decreased by > 50% during the surgery, the decrease was considered a significant deterioration even if some recovery was made at the end of the surgery.
Changes in ioSEP and ioMEP over the alarm criteria were considered significant even if they were recovered before the end of the monitoring. Complete recovery of ioEPs occurred when the ioEP exceeded the alarm criteria and recovered within the criteria at the end of the monitoring. Partial recovery of ioEPs occurred when ioEP recovered but exceeded the alarm criteria at the end of the monitoring.
2.4 PMD
Neurologic examination was performed a day before, 48 h after, and 4 weeks after the operation. Since this study focused on motor deterioration, sensory function was not considered. The Medical Research Council scale for muscle strength was applied to measure the strength of the ten key muscles of the International Standards for Neurological Classification of Spinal Cord Injury. Any decline in the motor score compared with the preoperative state was considered PMD.
2.5 Tumor size measurement
Based on the axial view of the MRI taken before surgery, the spinal canal area and tumor-occupying area were measured at the maximal tumor-occupying spinal level by an experienced radiologist using a picture archiving and communication system (Centricity PACS Radiology RA1000 Workstation, GE Healthcare, Barrington, IL, USA) [18]. The tumor-occupying area ratio was calculated as follows: tumor-occupying area/spinal canal area.
2.6 Anesthesia
Patients were administered intravenous midazolam (1.0–2.0 mg) as a pre-anesthetic medication. Rocuronium sodium was intravenously adjusted for tracheal intubation. A train-of-four stimulus at the ankle was applied to determine the level of neuromuscular blockage. Total intravenous anesthesia with remifentanil (0.15–2 μg/kg/min) and propofol (6–8 mg/kg/h) was continued throughout the surgical procedure. All patients were maintained normothermic and normotensive.
2.7 Statistical analysis
The basic characteristics of the two groups (acceptable preSEPLat, acceptable preSEPLat in all examined nerves; prolonged preSEPLat, prolongation of the preSEPLat in any examined nerve) were analyzed using an independent t-test and chi-squared test. Correlations between the preSEPLat and ioSEPs were analyzed using the chi-squared test and Fisher’s exact test. Fisher’s exact test was used in analyzing the correlations of preSEPLat or ioSEPs to PMD. To determine the risk factors for PMD at 48 h (PMD48hrs) or 4 weeks (PMD4wks) after the operation, multiple regression analysis was performed with the following variables: sex, age, height, operation level, anatomical type, tumor-occupying area ratio, preSEPLat, ioSEPs, and ioMEPs. Independent t-test was used in determining the correlations of the tumor-occupying area ratio to the preSEPLat, ioSEPs, PMD48hrs, or PMD4wks. The receiver operating characteristics (ROC) curve was used to analyze the cutoff of the tumor-occupying area ratio for significant changes in preSEPLat, ioSEPs, ioMEPs, PMD48hrs, and PMD4wks. In this study, the ioSEPs were classified as ioSEPLat, ioSEPAmp, and ioSEP (latency or amplitude) to determine whether latency or amplitude are mainly associated with the preSEPs or PMD. In actual monitoring, the generally consensus is that the amplitude and latency of the ioSEPs should be considered together. Therefore, only the ioSEP (latency or amplitude) was included as an independent variable for multiple regression analysis performed to identify the risk factors for PMD. SPSS version 20.1 (IBM, Armonk, NY, USA) was used for analysis. Two-sided P-values of < 0.05 were considered statistically significant.
3 Results
Of the 74 patients, 31 showed acceptable preSEPLat of all examined nerves and the remaining 43 showed prolonged preSEPLat in any of the examined nerves. All 74 patients had stable baseline waves of ioSEPs and ioMEPs. Age (P = 0.09), sex (P = 0.16), and height (P = 0.77) were not significantly different between the two groups. The anatomical type (P = 0.06), including intramedullary (IM), intradural-extramedullary (IDEM), or extradural (ED) tumors, operation level (P = 0.59), or pathologic type (P = 0.93), were not significantly different between the two groups (Table 1).
Among 36 patients who showed significant changes in any ioSEPAmp or ioSEPLat, 22 (61.1%) showed complete recovery, 5 (13.9%) showed partial recovery, and 9 (25.0%) showed no recovery. Among 47 patients who showed significant changes in ioMEPAmp, 8 (17.0%) showed complete recovery, 21 (44.7%) showed partial recovery, and 18 (38.3%) showed no recovery.
3.1 Correlations between preSEPs and ioSEPs
The chi-squared test for all 74 patients revealed no significant correlation between preSEPs and ioSEPs (P = 0.36). However, the subgroup analysis by anatomical type revealed that patients with prolonged preSEPLat were more likely to have deteriorated ioSEPs (P = 0.04) for IDEM tumors but not for IM (P = 0.67) or ED tumors (P = 0.17). Fisher’s exact test showed a significant correlation between preSEPLat and the latency of the ioSEPs (ioSEPLat) for IDEM tumors (P = 0.03) but not for IM (P = 0.67) or ED tumors (P = 0.17) (Table 2).
3.2 Correlation between preSEPs and PMD
Prior to surgery, 34 patients had neurological weakness. A chi-squared test revealed a significant correlation between preSEPLat and preoperative motor deficits (P = 0.003). However, the preSEPLat showed no significant correlation with PMD (PMD48hrs, P = 0.77; PMD4wks, P = 0.73) (Table 3). Even by subgroup analysis, the preSEPLat did not significantly correlate with PMD for any anatomical type of SCTs.
3.3 Correlation between ioSEPs and PMD
The ioSEP changes showed significant correlations with PMD48hrs (P = 0.003) and PMD4wks (P = 0.01). In more detail, changes in ioSEPLat were significantly correlated with PMD48hrs (P = 0.03), and changes in ioSEPAmp significantly correlated with both PMD48hrs (P < 0.01) and PMD4wks (P < 0.01). Changes in the amplitude of ioMEP (ioMEPAmp) significantly correlated with PMD48hrs (P = 0.03) but not with PMD4wks (P = 0.70). By the subgroup analysis for IM tumors, the decreased ioSEPAmp significantly correlated with PMD48hrs (P = 0.03) and had a tendency to correlate with PMD4wks (P = 0.05). For IDEM tumors, ioSEPAmp showed a tendency to correlate with PMD48hrs (P = 0.05) and PMD4wks (P = 0.05). In ED tumors, no correlation was found between any parameter of intraoperative EPs and PMD (Table 3).
3.4 Risk factors for PMD
Since no statistically significant correlations were noted between preSEPs and PMD48hrs and PMD4wks, we performed a logistic regression analysis to determine the contributing factors for PMD. The anatomical type (P = 0.04), tumor-occupying area ratio (P = 0.01), and significant changes in ioSEPs (P = 0.001) were statistically significant risk factors for PMD48hrs. The ioSEPs were the only statistically significant factor affecting PMD4wks (P = 0.004) (Fig. 2).
Correlations between preoperative, intraoperative SEPs, and postoperative motor deterioration. ED extradural, IDEM intradural-extramedullary, IM intramedullary, IONM intraoperative neurophysiological monitoring, ioMEPs intraoperative motor evoked potentials, ioSEPs intraoperative somatosensory evoked potentials, preSEPs preoperative somatosensory evoked potentials. *Statistically significant with P-value < 0.05
3.5 Cutoff of the tumor-occupying area ratio for significant changes in ioSEP, ioMEP, and PMD
As the tumor-occupying area ratio was found to be one of the contributing factors for PMD, significant correlations of the tumor-occupying area ratio to the preSEPLat (P = 0.045) and PMD48hrs (P = 0.03) were also revealed (Table 4). Based on these correlations, we further analyzed the cutoff of the tumor-occupying area ratio for several variables using ROC curve analysis. The cutoff of the tumor-occupying area ratio for the significant changes in preSEPLat, ioSEPs, ioMEPAmp, PMD48hrs, and PMD4wks were 0.67, 0.67, 0.68, 0.69, and 0.69, respectively.
4 Discussion
4.1 Relationship between preSEPs and ioSEPs: proof of the hypothesis
The main hypothesis, “the patient with prolonged preSEPLat would have more deterioration in intraoperative EPs,” started from a reliable presumption that the surgical procedure would be more invasive for the somatosensory tract for lesions with greater involvement of the dorsal column. However, an opposing hypothesis can be also raised, that is, a patient with prolonged preSEPLat would exhibit less deterioration of ioSEPs, since the neural tract is already compromised so much preoperatively that any additional iatrogenic neural insult could not cause further deterioration. Although the main hypothesis became insignificant when it was applied for all 74 cases, regardless of anatomical types, the subgroup analysis obtained a significantly reliable result for IDEM tumors. Unlike IDEM tumors, IM tumors with deteriorated preSEPs showed less significant electrophysiological changes during surgery. As IM tumors can compress the spinal cord within the pia mater, more directly than IDEM tumors, it would cause more severe neurophysiological deterioration preoperatively, and this supports the opposing hypothesis mentioned above. In the same context, some previous studies suggested that SEP monitoring might be less sensitive to detection of acute insults in the presence of preexisting white matter lesions [9, 19].
Although the usefulness of IONM has been demonstrated mostly in IM tumors, the efficacy of IONM in IDEM tumors is still being debated. Since IDEM tumors can compress the spinal cord from outside the pia mater rather than invade the spinal cord axon itself, we can hypothesize that IDEM tumors would cause neuropraxia first rather than axonotmesis or neurotmesis according to Seddon’s classification [20]. Although this classification was originally based on peripheral nerves, some studies have adjusted this concept to explain the mechanisms of spinal cord injury [21,22,23]. The significant correlations between the latencies of preSEPs and ioSEPs in patients with IDEM tumors would be a clue that the conduction block is a major mechanism of SEP changes. Otherwise, IM tumors, which grow with time and affect nearby axons, would cause axonotmesis or neurotmesis and lead to greater changes in parameters than those caused by IDEM tumors.
The topographically involved anatomical lesion appears to be important for intraoperative SEP changes [24,25,26,27]. The larger the tumor-occupying area ratio, the larger the ioSEP change is likely to be. Howerver, in case of preexisting electrophysiological deterioration before surgery, the cutoff value of the tumor-occupying area ratio for ioSEP change may not be applied, regardless of whether it is an IDEM or IM tumor. Among five IM ependymoma patients with prolonged preSEPLat, patients with a relatively lower tumor-occupying area ratio (0.68–0.86; Patients 1, 2, 3, 7, and 9 in Table 5) showed significant deterioration in ioSEPs, while a patient with a higher tumor-occupying area ratio (0.94; Patient 4 in Table 5) showed no significant ioSEP changes. Likewise, among patients with IDEM tumors presenting with prolonged preSEPLat, patients with a relatively lower tumor-occupying area ratio (0.31 and 0.52; Patients 5 and 6, respectively, in Table 5) showed a significant change in ioSEPs, while a patient with a larger tumor-occupying area ratio (0.71; Patient 8 in Table 5) and severe invasion of the somatosensory tract showed no significant changes in ioSEPs, as did the severely invasive IM tumor. These findings suggested that a topographically severely compromised spinal cord before operation would not yield significant changes in ioSEP. These cases support those of a previous study which demonstrated that rats with preexisting demyelination showed less SEP vulnerability to ischemia and anoxia [9].
4.2 Contributing factors for PMD
4.2.1 Topographical vs electrophysiological value
Based on the analyzed risk factors for the PMD, topographical values including tumor-occupying area ratio and anatomical type are considered significant risk factors for transient PMD, which would resolve within 4 weeks. However, the electrophysiological parameter, ioSEPs, was found to be a significant risk factor for PMD that persisted over 4 weeks. These results of regression analyses imply that the PMD would be restored soon after surgery if the ioSEPs did not change significantly even if the tumor-occupying area ratio is higher. With closer observation, the average tumor-occupying area ratio of patients with IM tumors who showed transient PMD was 0.81 and that of patients with PMD that persisted over 4 weeks was 0.78. This also suggests that the topographical data itself is not enough for predicting the persistence of PMD, and the electrophysiological value should be considered to predict a more reliable prognosis. In addition, the possible reason that the ioMEPAmp was not analyzed to be a prognostic factor for PMD would lie on the strict alarm criteria of this study on ioMEPAmp, which was set as 50% reduction from baseline, not 80% reduction as recently reviewed [3].
A previous study revealed that the topographical degree of spinal cord involvement correlated with the latencies of tibial SEPs in patients with cervical ossification of posterior longitudinal ligament (OPLL) [18]. Recently, diffusion tensor tractography revealed significant correlations of the topographical alteration of pyramidal tract to MEPs and PMD [28]. In the present study, the cutoff values of the tumor-occupying area ratio for preSEPLat and ioSEP deterioration in SCTs (cutoff values, 0.67 and 0.67, respectively) were higher than those for preSEPLat in OPLL (cutoff value, 0.36) [18]. These differences may result from the hardness difference between tumor and ossification.
4.2.2 PreSEPs not enough to predict PMD
Even though the preSEPLat did not show a direct correlation with PMD in this study, the prolongation of preSEPLat could be a deductive basis for predicting the postoperative functional changes by noting that the ioSEPs are significantly related to preSEPLat, especially in patients with IDEM tumors. Additional data can be accumulated and analyzed to verify whether preSEPs can be used as an index for predicting PMD considering the collinearity with ioSEPs.
4.2.3 Tumor growth rate may not be a prognostic factor for PMD
Epidemiologically, IM tumors comprise 20–30% of primary intradural SCTs, and IDEM tumors comprise the remaining 70–80% [29, 30]. Ependymomas, which are known to grow slowly, account for up to 25% of IM tumors. Among the 24 patients with IM tumors, nine (37.5%) had ependymoma. Among ten patients with IM tumors who had PMD, eight (80.0%) had ependymoma. We first assumed that this slowly growing IM ependymoma would not deteriorate or cause less deterioration of the neural tract because the nerves had enough time to adapt to the slowly increasing intradural pressure, so that maintaining the neurophysiological function would be relatively easier over the long time of tumor growth. However, in this study, many cases of ependymoma with prolonged preSEPs have already shown PMD (Table 5). An animal study which compared the imaging and neurological outcomes of rat models under the varying speeds of spinal cord compression revealed that the speed of cord compression is not a significant factor for neurological deterioration [31]. In addition, to the best of our knowledge, no previous experimental study has examined the degree of the restoration of neurophysiological function after decompression depending on the duration of neural compression of any peripheral nerve or spinal cord. Moreover, in an actual clinical setting, accurate prediction of the initial onset of tumor development is usually impossible; even neurosurgeons would regard this kind of study unnecessary because they mostly promptly make plans to remove the tumor once it is detected.
4.3 Limitations
In addition to the small sample size, this study has several other limitations. We did not match each median, ulnar, peroneal, or tibial SEPs by the preoperative and intraoperative evaluations, and we did not match the motor outcomes by each nerve. Since we analyzed the overall preSEPs, ioSEPs, and motor grades, we could not provide specific statistical data on each nerve and its focal functional outcomes. Further, the postoperative neurologic prognosis was not analyzed based on the degree of recovery of IONM parameters. D-wave testing was not available because it has not yet been approved by the Korea Food and Drug Administration. Despite the SEP studies, the patient’s sensory function was not considered because of the difficulty in obtaining reports of subtle sensory changes. Additionally, this study did not unify the pathologic type of tumors, which usually contributes to the prognosis. Further analysis with a bigger sample size of each pathological type would provide more useful information to neurosurgeons.
5 Conclusions
In this study, the preSEPs and ioSEPs showed significant correlation in patients with IDEM tumors. Preoperative electrodiagnosis including preSEPs are useful not only in determining the preoperative neurophysiological function, but also in predicting the results of IONM, especially in IDEM tumors. Topographical values, including tumor-occupying area ratio and anatomical type, were found to be contributing factors for the transient PMD, whereas the ioSEPs were identified as the significant prognostic factors for predicting postoperative weakness that persists over 4 weeks.
Data availability
Data are not available according to the guideline of our Institutional Review Board.
References
Sala F, Palandri G, Basso E, Lanteri P, Deletis V, Faccioli F, Bricolo A. Motor evoked potential monitoring improves outcome after surgery for intramedullary spinal cord tumors: a historical control study. Neurosurgery 2006;58(6):1129–43. https://doi.org/10.1227/01.neu.0000215948.97195.58
Ghadirpour R, Nasi D, Iaccarino C, Romano A, Motti L, Sabadini R, Valzania F, Servadei F. Intraoperative neurophysiological monitoring for intradural extramedullary spinal tumors: predictive value and relevance of D-wave amplitude on surgical outcome during a 10-year experience. J Neurosurg Spine. 2018;30(2):259–67. https://doi.org/10.3171/2018.7.spine18278.
MacDonald DB. Overview on criteria for MEP monitoring. J Clin Neurophysiol. 2017;34(1):4–11. https://doi.org/10.1097/wnp.0000000000000302.
Macdonald DB, Skinner S, Shils J, Yingling C. Intraoperative motor evoked potential monitoring—a position statement by the American Society of Neurophysiological Monitoring. Clin Neurophysiol. 2013;124(12):2291–316. https://doi.org/10.1016/j.clinph.2013.07.025.
Kothbauer KF. Intraoperative neurophysiologic monitoring for intramedullary spinal-cord tumor surgery. Neurophysiol Clin. 2007;37(6):407–14. https://doi.org/10.1016/j.neucli.2007.10.003.
Sala F, Bricolo A, Faccioli F, Lanteri P, Gerosa M. Surgery for intramedullary spinal cord tumors: the role of intraoperative (neurophysiological) monitoring. Eur Spine J. 2007;16(Suppl 2):S130–139. https://doi.org/10.1007/s00586-007-0423-x.
Li C, Houlden DA, Rowed DW. Somatosensory evoked potentials and neurological grades as predictors of outcome in acute spinal cord injury. J Neurosurg. 1990;72(4):600–9. https://doi.org/10.3171/jns.1990.72.4.0600.
Perot PL Jr, Vera CL. Scalp-recorded somatosensory evoked potentials to stimulation of nerves in the lower extremities and evaluation of patients with spinal cord trauma. Ann NY Acad Sci. 1982;388:359–68.
Seyal M, Mull B. Mechanisms of signal change during intraoperative somatosensory evoked potential monitoring of the spinal cord. J Clin Neurophysiol. 2002;19(5):409–15.
Kearse LA Jr, Lopez-Bresnahan M, McPeck K, Tambe V. Loss of somatosensory evoked potentials during intramedullary spinal cord surgery predicts postoperative neurologic deficits in motor function [corrected]. J Clin Anesth. 1993;5(5):392–8.
Glassman SD, Johnson JR, Shields CB, Backman MH, Paloheimo MP, Edmonds HL Jr, Linden RD. Correlation of motor-evoked potentials, somatosensory-evoked potentials, and the wake-up test in a case of kyphoscoliosis. J Spinal Disord. 1993;6(3):194–8.
Chang SH, Park YG, Kim DH, Yoon SY. Monitoring of motor and somatosensory evoked potentials during spine surgery: intraoperative changes and postoperative outcomes. Ann Rehabil Med. 2016;40(3):470–80. https://doi.org/10.5535/arm.2016.40.3.470.
Rijs K, Klimek M, Scheltens-de Boer M, Biesheuvel K, Harhangi BS. Intraoperative neuromonitoring in patients with intramedullary spinal cord tumor: a systematic review, meta-analysis, and case series. World Neurosurg. 2019;125:498–510.e2. https://doi.org/10.1016/j.wneu.2019.01.007.
Krassioukov AV, Sarjeant R, Arkia H, Fehlings MG. Multimodality intraoperative monitoring during complex lumbosacral procedures: indications, techniques, and long-term follow-up review of 61 consecutive cases. J Neurosurg Spine. 2004;1(3):243–53. https://doi.org/10.3171/spi.2004.1.3.0243.
Park T, Park J, Park YG, Lee J. Intraoperative neurophysiological monitoring for spinal cord tumor surgery: comparison of motor and somatosensory evoked potentials according to tumor types. Ann Rehabil Med. 2017;41(4):610–20. https://doi.org/10.5535/arm.2017.41.4.610.
Sandalcioglu IE, Gasser T, Asgari S, Lazorisak A, Engelhorn T, Egelhof T, Stolke D, Wiedemayer H. Functional outcome after surgical treatment of intramedullary spinal cord tumors: experience with 78 patients. Spinal Cord. 2005;43(1):34–41. https://doi.org/10.1038/sj.sc.3101668.
Chiappa KH. Short-latency somatosensory evoked potentials: methodology. In: Chiappa KH, editor. Evoked potentials in clinical medicine. 3rd ed. Philadelphia, New York: Lippincott-Raven; 1997. p. 283–340.
Yoon SY, Park TH, Eun NL, Park YG. The cutoff value of ossification of posterior longitudinal ligament (OPLL) for early diagnosis of myelopathy using somatosensory evoked potential in cervical OPLL patients. Spinal Cord. 2017;55(6):606–11. https://doi.org/10.1038/sc.2017.15.
Follis F, Scremin OU, Blisard KS, Scremin AM, Pett SB, Scott WJ, Kessler RM, Wernly JA. Selective vulnerability of white matter during spinal cord ischemia. J Cereb Blood Flow Metab. 1993;13(1):170–8. https://doi.org/10.1038/jcbfm.1993.20.
Seddon HJ. Peripheral nerve injuries. Glasg Med J. 1943;139(3):61–75.
Asan Z. Spinal concussion in adults: transient neuropraxia of spinal cord exposed to vertical forces. World Neurosurg. 2018;114:e1284–e9. https://doi.org/10.1016/j.wneu.2018.03.198.
Bernsen HJ, Koetsveld A, Frenken CW, van Norel GJ. Neuropraxia of the cervical spinal cord following cervical spinal cord trauma: a report of five patients. Acta Neurol Belg. 2000;100(2):91–5.
Dailey A, Harrop JS, France JC. High-energy contact sports and cervical spine neuropraxia injuries: what are the criteria for return to participation? Spine (Phila Pa 1976). 2010;35(21 Suppl):S193–S201. https://doi.org/10.1097/BRS.0b013e3181f32db0.
Yanni DS, Ulkatan S, Deletis V, Barrenechea IJ, Sen C, Perin NI. Utility of neurophysiological monitoring using dorsal column mapping in intramedullary spinal cord surgery. J Neurosurg Spine. 2010;12(6):623–8. https://doi.org/10.3171/2010.1.spine09112.
Manzano G, Green BA, Vanni S, Levi AD. Contemporary management of adult intramedullary spinal tumors-pathology and neurological outcomes related to surgical resection. Spinal Cord. 2008;46(8):540–6. https://doi.org/10.1038/sc.2008.51.
Quinones-Hinojosa A, Gulati M, Lyon R, Gupta N, Yingling C. Spinal cord mapping as an adjunct for resection of intramedullary tumors: surgical technique with case illustrations. Neurosurgery. 2002;51(5):1199–206.
Smith MC, Deacon P. Topographical anatomy of the posterior columns of the spinal cord in man. The long ascending fibres. Brain. 1984;107:671–98.
Czernicki T, Maj E, Podgorska A, Kunert P, Prokopienko M, Nowak A, Cieszanowski A, Marchel A. Diffusion tensor tractography of pyramidal tracts in patients with brainstem and intramedullary spinal cord tumors: relationship with motor deficits and intraoperative MEP changes. J Magn Reson Imaging. 2017;46(3):715–23. https://doi.org/10.1002/jmri.25578.
Samartzis D, Gillis CC, Shih P, O’Toole JE, Fessler RG. Intramedullary spinal cord tumors: part I—epidemiology, pathophysiology, and diagnosis. Glob Spine J. 2015;5(5):425–35. https://doi.org/10.1055/s-0035-1549029.
Celano E, Salehani A, Malcolm JG, Reinertsen E, Hadjipanayis CG. Spinal cord ependymoma: a review of the literature and case series of ten patients. J Neurooncol. 2016;128(3):377–86. https://doi.org/10.1007/s11060-016-2135-8.
Long HQ, Li GS, Lin EJ, Xie WH, Chen WL, Luk KD, Hu Y. Is the speed of chronic compression an important factor for chronic spinal cord injury rat model? Neurosci Lett. 2013;545:75–80. https://doi.org/10.1016/j.neulet.2013.04.024.
Acknowledgements
We would like to thank Editage (https://www.editage.co.kr) for English language editing.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol was approved by the institutional review board of Gangnam Severance Hospital (3-2019-0108) and conducted in accordance with the Declaration of Helsinki.
Research involving human participants and/or animals
This retrospective cohort study was based on the preexisting medical data review, and did not prospectively include human participants or animals.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Park, J., Cho, Y.E., Park, M. et al. Correlation between preoperative somatosensory evoked potentials and intraoperative neurophysiological monitoring in spinal cord tumors. J Clin Monit Comput 35, 979–991 (2021). https://doi.org/10.1007/s10877-020-00584-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-020-00584-x