Abstract
We implemented a pharmacokinetic/pharmacodynamic (PK/PD) based optimization algorithm recommending intraoperative Remifentanil and Propofol infusion rates to minimize time to emergence and maximize the duration of analgesia in a clinical setting. This feasibility study tested the clinical acceptance of the optimization algorithm’s recommendations during scoliosis surgical repair for 14 patients. Anesthesiologist accepted 359/394 (91%) of the recommendations given on the basis of the optimization algorithm. While following the optimization’s recommendations the anesthesiologist decreased Propofol infusions from an average of 164–135 mcg/kg/min [p = 0.002] and increased Remifentanil infusions from an average of 0.22–0.30 mcg/kg/min [p = 0.004]. The anesthesiologists appeared to accept and follow the recommendations from a PK/PD based optimization algorithm.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
During general anesthesia, anesthesiologists titrate their anesthetic with an immediate focus on the intraoperative requirements of providing adequate analgesia and maintaining unresponsiveness, while also seeking the postoperative targets of a rapid emergence and postoperative analgesia. Dosing anesthetics to meet these intraoperative requirements and postoperative targets is challenging when the surgical procedure is complicated and associated with high pain intensity, as with spine surgery [1]. A potential dosing regimen to increase postoperative analgesia includes the intraoperative use of methadone, but high doses of opiates may also prolong emergence times [2, 3].
Incorporation of pharmacokinetic and pharmacodynamic (PK/PD) models may enable anesthesiologists to achieve their intraoperative requirements and postoperative targets [4]. Based on PK/PD technology, we developed an optimization algorithm to recommend intraoperative dosing regimens that not only focus on intraoperative sedation and analgesia requirements but also target a rapid emergence and prolonged postoperative analgesia [5].
The optimization algorithm was modified to recommend both Propofol and Remifentanil infusion rates in the presence of a one-time methadone bolus. The aim of this study was to test the feasibility of a PK/PD based optimization algorithm. We hypothesized that the optimization algorithm will be considered acceptable, defined as a rate of agreement of more than 80% between the recommendations of the optimization algorithm and the applied adjustments by the attending anesthesiologists. To test this hypothesis, we performed a preliminary open label cohort study of 14 patients who underwent surgery for adolescent idiopathic scoliosis repair.
2 Methods
With IRB approval, the optimization algorithm was implemented in 14 adolescents who underwent idiopathic scoliosis repair surgery and the University of Florida Hospital from 6/2015 until 9/2016. The primary outcome measured was the anesthesiologist’s rate of agreement with the optimization’s recommendations of Remifentanil and Propofol intraoperative infusion rates; intended to determine whether anesthesiologists accept the recommendations of the algorithm. Secondary outcome measures were the observed time to emergence, time to first postoperative opioid administered, postoperative opioid consumption, and postoperative pain scores. The time to emergence was defined as the time from the end of surgery (skin closure) until the patient could respond by moving their feet. Feet movement was the hospital’s emergence requirement following scoliosis surgical repair. The postoperative pain scores were collected per hospital format; VAS on a scale from 0 to 10 recorded by the nurse in the electronic medical record every 4–6 h.
Inclusion criteria for all patients were ASA class I-II status, a diagnosis of adolescent idiopathic scoliosis and age between 10 and 19 years. A single surgical team at the University of Florida hospital (UF Health) provided care for all patients. Subjects were excluded if they were being treated with drugs known to alter anesthetic requirements (e.g., opiates, alpha2 agonists, anticonvulsants, antidepressants) or restrictive lung disease. No female subjects either pregnant or breast feeding were included in the study. Inclusion criteria for the study required the anesthesiologists to only use Propofol, Fentanyl, Remifentanil, and methadone. The methadone was administered as one bolus between 0.25 and 0.40 mcg/kg at the beginning of surgery.
For each anesthetic administration a study investigator was present to employ the algorithm, present the algorithm’s recommendations, and record data. To employ the algorithm, the study investigator recorded doses and times of administration of anesthetics, and the patient demographics (age, height, gender, and weight). The first recommendation for each patient was given approximately 30 min after induction, which was when the anesthesiologists’ work load lessened. After the first recommendation was given, recommendations were shared every 10 min until the end of surgery. Specifically, the study investigator shared the algorithm’s recommended Propofol and Remifentanil infusion rates with the anesthesiologist. The anesthesiologist was found compliant with the recommendation if they changed infusions rates as recommended within 2 min. The adherence to the recommendations and reason for non-compliance were recorded by the study investigator. The patient time to emergence, time of first postoperative opioid administered, postoperative opioid consumption, and visual analog scale pain scores (the first 24 h following surgery) were recorded by the hospital staff in the electronic medical record as per their normal documenting process.
The rate of agreement was determined by the total number of times the clinician agreed with the algorithm divided by the total number of times the recommendations were given. If the overall rate of agreement exceeded 80% the algorithm would be determined accepted. A student t-test statistic was performed to compare the changes of the Propofol and Remifentanil infusion rates before and after optimization recommendations were given.
2.1 Optimization overview
The optimization algorithm is a PK/PD based mathematical model we have previously developed [5]. For this application the optimization algorithm was modified to also include methadone. The include methadone in the algorithm it’s predicted effect site concentrations were converted to remifentanil equivalents [6, 7]. The inputs into the optimization algorithm are the patient demographics (age, height, weight, and gender), the time and duration of each dose administered, and the rate (infusion) or size (bolus) of that dose, and the estimated remaining duration of surgery. The outputs of the optimization algorithm are the predicted time to emergence and duration of analgesia for the current dosing regimen and the predicted time to emergence and duration of analgesia for the optimized dosing regimen. The optimization algorithm attempts to maintain the ‘level’ of anesthesia based off the assumption that the current dosing regimen is adequate and appropriate. The goal of the optimization algorithm is to recommend the intraoperative dosing regimen to maintain the ‘level’ of anesthesia while minimizing the time to emergence and maximizing the duration of analgesia.
2.2 Presurgical introduction to the optimization algorithm
Prior to the study, each of the board certified anesthesiologists were individually introduced to the optimization algorithm. This introduction was intended to explain the concept of using pharmacokinetic (PK) and pharmacodynamic (PD) models to optimize anesthetic dosing. PK models were introduced as mathematical estimations of the anesthetic concentrations in the patient and the PD models estimate the effect anesthetic concentrations have on the patient [8]. These models were described to be population based with limited reliability when applied to individuals [9]. At this phase of the introduction the optimization algorithm program was shown to the anesthesiologist to illustrate the mathematical modeling, Fig. 1.
Optimization algorithm MATLAB GUI. MATLAB GUI with the optimization algorithm programmed software. The top left is the box for the study investigator to enter the patient demographics and estimated surgery length. The surgery length can change as the estimation becomes more certain. The algorithm requires initialization where it simulates a wide range of possible Propofol and Remifentanil infusions rates, as done with the ‘initialize button’. After initialization the optimization can optimize the infusion rates, the ‘Optimization current admin’ button searches the combinations of Propofol and Remifentanil infusion rates finding the one forecasted to have the best postoperative emergence and analgesia responses. The upper middle box displays the recommended Propofol and Remifentanil infusion rates after the algorithm is executed. Also when the optimization is run, the PK and PD estimations for the optimized infusion rates are illustrated through the display. The effect site concentrations are shown in the top right panel; Remifentanil in red, Propofol in blue, and induction Fentanyl and bolus methadone in green. The solid lines indicate the effect site concentrations for administrations proceeding the current implementation of the optimization algorithm and the projected effect site concentrations for maintained infusion rates. The dotted lines indicate the effect site concentrations if the infusion rates recommendations are followed. In this example the recommendation simulation was run at the 85 min mark. The Remifentanil infusion rate was recommended to increase to 0.29 mcg/kg/min and the Propofol infusion rate was recommended to decrease to 145 mcg/kg/min. Also displayed on the PK box display are two solid black vertical lines indicating the estimated end of surgery and emergence time. The emergence and analgesia predictions are calculated and displayed in the box in the left middle panel. The bottom panel displays the pharmacodynamics estimations laid upon the pharmacodynamics response surface. The solid green line is the current trajectory administration, while the red line indicates the optimized trajectory. For the first phase of the surgery the red and green line track each other, near the middle of the graph the two lines diverge, which is indicative of the point when the optimization was run
2.3 Intraoperative operation of the optimization algorithm
After the anesthesiologist had viewed the display they were reminded that the PK/PD optimization did not account for other variables that might affect their decision making process: heart rate, blood pressure, and BIS value. The anesthesiologist was informed the PK/PD optimization algorithm would not determine the ‘level’ or ‘depth’ of anesthesia; but rather, that it would find the best post-operative outcomes while maintaining their set level. The anesthesiologist was expected to make the clinical decision determining if the recommended infusion rates were safe and appropriate for the patient. Furthermore, after each given recommendation, if they deemed the infusion rates inappropriate they would be queried why. The study investigator recorded the infusion rates administered, the recommendations, compliance to the recommendations, and any reason for not following the recommended change of infusion rates. When the anesthesiologist rejected the infusion rate recommendation the actual infusion rates were input into the algorithm, at the next time interval the algorithm was implemented again.
3 Results
The optimization algorithm was implemented on 14 patients to generate 394 recommendations. The anesthesiologist accepted and followed 359/394 (91%) of the recommendations given. Partial acceptance occurred twice when the anesthesiologist changed the infusion rates half of the distance to the recommended infusion rate amounts. There were three reasons for non-compliance; (1) lowering the Propofol infusion rate would cause an unsafe rise in patient intraoperative awareness evidenced by rising BIS values, (2) raising the Remifentanil infusion rate would cause hypotension, and (3) wanting to focus solely on decreasing the patient’s emergence time because the methadone administration was expected to provide sufficient postoperative analgesia.
The majority (79%) of naïve recommendations, recommendations after the anesthesiologist changed infusion rates or at the beginning of the anesthetic, were to increase Remifentanil while simultaneously decreasing the Propofol infusion rates. The anesthesiologists reached the optimal infusion rates and generally maintained those doses during the maintenance phase, the majority of the algorithm’s recommendations (81%) were to maintain the Propofol and Remifentanil infusion rates. During the course of the maintenance phase the algorithm guided clinicians to decrease the Propofol infusion rate to 135 ± 28 mcg/kg/min a decrease of 29 ± 31 mcg/kg/min [tstat = − 3.4, p = 0.004, 95% CI = − 44 to − 10] and increase the remifentanil infusion rate to 0.30 ± 0.07 mcg/kg/min an increase of 0.08 mcg/kg/min [tstat = 3.9, p = 0.002, 95% CI = 0.05–0.19].
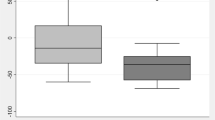
Patients emerged 20 min [7–33; 25–75% quartile] after surgery, required the first rescue opioid administration 54 [20–128] min after entrance to the recovery unit, and received the equivalent of 10 [4–17] mg of morphine during the first 24 h during which time their average VAS pain score was 3.4 ± 1.8. There were no adverse events observed or recorded when the anesthesiologist followed the optimization recommendations.
3.1 Discussion
The anesthesiologists positively accepted the recommendations from the optimization algorithm as indicated by the agreement rate of 91%. The high agreement rate indicates that anesthesia providers felt the recommended dosing rates were within their clinical scope. Furthermore, it appears that a PK/PD based optimization algorithm may be an intraoperative tool anesthesiologists are willing to use.
However, the high rate of agreement might be elevated by the education given pre-operatively associated with the intra-operative presence of a study investigator. The anesthesiologist might have conformed to the recommendations of the study investigator because of a perceived aggrandizement of the PK/PD optimization algorithm. Additionally, the workload for the anesthesiologist workload might have diminished since the anesthesiologist only had to determine the ‘level’ or ‘depth’ of anesthesia but did not have to worry about postoperative emergence or analgesia.
A feasibility study testing the implementation on this cohort was chosen because we were unsure if positive results could be found amidst the study limitations. One study limitation is the clinical application of PK/PD models which have inherent variability around their predictions [9, 10].We were unsure if anesthesiologists would be willing to follow an intraoperative PK/PD tool; while intraoperative PK/PD tools are available on the market but are not common in an operating room setting. Previously the SmartPilot® and Navigator® have been shown to visualize the anesthetic PK/PD landscape intraoperatively and have decreased the anesthetics used [11]. Other PK/PD tools, such as target controlled infusion pumps, are becoming more common in Europe. Target controlled infusion pump technology has advanced to feature EEG based closed loop control of sedative/hypnotic agents [12]. These PK/PD tools available on the market are focused on establishing the depth of anesthesia and the intraoperative anesthetic. Thus, the feasibility of good acceptance for an intraoperative PK/PD tool in the US was suspect. The technology implemented in this project could be an excellent companion to the PK/PD display technology to allow them the freedom to adjust the ‘level’ of anesthesia as needed while allowing the technology to target optimal post-operative outcomes. A second limitation of the study was implementing the PK/PD models in a pediatric population. The PK/PD models were developed using adult populations [8] thus their accuracy in a pediatric population is questionable [13]. A third study limitation is the conversion of opioids, fentanyl and methadone, into remifentanil equivalents. While it is generally understood that opioids have pharmacodynamic similarities the conversion between opioids is not well definied [6].
This feasibility study successfully determined that the anesthesiologists accepted the dosing rate recommendations from the optimization algorithm. Further feasibility studies should be performed on the optimization algorithm; determine if the optimization algorithm will operate successfully in different patient populations (adult, elderly), or with different surgery types, or with inhaled agents. If product development is desired then the feasibility of the operation of the optimization algorithm in an anesthesia monitor, without a study investigator, should be designed.
References
Gornitzky AL, Flynn JM, Muhly WT, Sankar WN. A rapid recovery pathway for adolescent idiopathic scoliosis that improves pain control and reduces time to inpatient recovery after posterior spinal fusion. Spine Deformity. 2016;4:288–95.
Gottschalk A, Durieux M, Nemergut E. Intraoperative methadone improves postoperative pain control in patients undergoing complex spine surgery. Anesth Analg. 2011;112:218–23.
Nicholson A. Methadone for cancer pain. Cochrane Database Syst Rev. 2007;17: (4) CD003971.
Struys M, Sahinovic M, Lichtenbelt B, Vereeck H, Absalom A. Optimizing intravenous drug administration by applying pharmacokinetic/pharmacodynamic concepts. Br J Anaesth. 2011;107(1):38–47.
Tams C, Syroid N, Johnson K. J Clin Comput Monit. 2019; 8230.
Pereira J, Lawlor P, Vigano A, Dorgan M, Bruera E. Equianalgesic dose ratios for opioids: a critical review and proposals for long-term dosing. J Pain Symptom Manage. 2001;22(2):672–87.
Berdine H, Nesbit S. Equianalgesic dosing of opioids. J Pain Palliat Care Pharmacother. 2006; 20(4): 79–84.
Minto C, Schnider T, Shafer S. Pharmacokinetics and pharmacodynamics of remifentanil II model application. Anesthesiology. 1997;86(1):24–33.
Shafer S. All models are wrong. Anesthesiology. 2012;116(2):240–1.
Tams C, Johnson K. Prediction variability of combined pharmacokinetic pharmacodynamic models: a simulation study of Propofol in combination with remifentanil and fentanyl. J Anesth Clin Res. 2014;5:3.
Cirillo, et al. Navigator® and SmarPilot ® View are helpful in guiding anesthesia and reducing anesthetic drug dosing. Minerva Anesthiol. 2015;81:1163–9.
Kuizenga M, Hugo V, Struys M. Model-based drug administration: current status of target-controlled infusion and closed-loop control. Curr Opin Anaesthesiol. 2016;29(4):475–81.
Chidambaran V, Costandi A, D’Mello A. Propofol: a review of its role in pediatric anesthesia and sedation. CNS Drugs. 2015;29(7):543–63.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tams, C., Johnson, K. & Seubert, C. Acceptance of a propofol and remifentanil infusion dosing algorithm to optimize postoperative emergence and analgesia. J Clin Monit Comput 33, 953–957 (2019). https://doi.org/10.1007/s10877-019-00295-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-019-00295-y